Abstract
Osteomyelitis (OM) is the most frequent infection associated with diabetic foot ulcers (DFU) that typically involve the forefoot, the most common location of DFU.
Conservative surgical procedures could be attractive alternative that reduces minor and major amputations and avoid future recurrence thus preserving the functionally of the foot. This review aimed to analyze and describe the current evidence on conservative diabetic foot osteomyelitis (DFO) surgical procedures depending on DFU location and indications.
A narrative revision of the evidence was carried out by searching Medline through PubMed databases from inception to late July 2020 to identify retrospective, prospective, and randomized controlled trials pertaining to conservative DFO procedures on the forefoot.
Seven types of conservative surgical procedures for DFO treatment in the forefoot are described in this review: (1) partial or total distal phalangectomy, (2) arthroplasty of the proximal or distal interphalangeal joint, (3) distal Syme amputation, (4) percutaneous flexor tenotomy, (5) sesamoidectomy, (6) arthroplasty of the metatarsophalangeal joint, and (7) metatarsal head resection.
When indicated, conservative surgery for DFUs in patients with chronic forefoot OM is a safe and effective option that increases the chances of healing and reduces the possibility of limb loss and death compared with radical amputation procedures.
Since a lack of sufficient evidence supporting this procedure exists, future investigations should be focused on the random clinical trial (RCT) design. The results of prospective trials could help surgeons select the appropriate procedure in each case in order to minimize complications.
Keywords: Diabetic foot, Conservative surgery, Surgical approach, Osteomyelitis
1. Introduction
Osteomyelitis (OM) is the most common infection associated with diabetic foot ulcers (DFU). OM occurs in more than 20% of moderate infections and between 50% and 60% of severe infections and is associated with high rates of amputation.1 Over 50% of DFU are located in the forefoot, the most frequent location of diabetic foot osteomyelitis (DFO).2
Traditionally, DFO has been considered a complex and difficult-to-treat infection with a high rate of relapse3 and is one of the most challenging issues when dealing with diabetic foot syndrome.4 Surgical resection of infected bone has long been the standard osteomyelitis treatment.2 Several criteria in which surgery should be the first therapeutic option have been recommended: (1) bone is visible at the bottom of the ulcer, (2) the presence of necrosis in soft tissues, (3) the need for drainage of abscesses or collections, (3) failure (after 90 days) of antibiotic treatment (4) joint exposure (especially the first metatarsophalangeal), (5) need for offloading surgery, (6) advanced bone destruction, and (7) patients at high risk of ATB toxicity (especially in patients with nephropathy).5
Standard diabetic foot surgery has been amputation in many departments6 however, during the last decades it has noticeably changed from radical surgery to a more complex discipline focusing on conservative and planned procedures.7 Previous studies have demonstrated that this trend has had an important impact the type of selected surgery with a progressively increasing focus on proactive and conservative, rather than reactive and ablative, foot procedures.8
Amputations are devastating and radical procedures compared with conservative surgery, which is the type of surgery in which only the infected bone is removed without the need for amputation.9 The advantages of conservative surgery consist of several parameters that mainly include lowering the rates of minor and major amputation5 and reducing urgent procedures.8 In addition, conservative surgery allows surgical technique planning in order to avoid future recurrences by analyzing foot biomechanics ensuring a more stable foot functionality.5
The International Working Group on the Diabetic Foot (IWGDF) recognizes that DFO is an area in which guidelines for treatment is needed.2 Different conservative surgical techniques for DFO of the forefoot can be found; however conservative techniques described in the literature are heterogeneous and present small variations depending mainly on the surgeon’s skills and resources.
The aim of this review was to analyze and describe the current evidence addressing conservative DFO surgical procedures depending on the DFU location that would allow clinicians to establish therapeutic criteria in the approach to DFO in the forefoot.
2. Material and methods
A narrative revision of the evidence was carried out focusing on conservative DFO surgical techniques in patients with foot ulcers located in the forefoot.
The databases PubMed (Medline) database was searched from inception to late July 2020 to identify retrospective, prospective and randomized controlled trials pertaining to conservative DFO procedures on the forefoot.
The key words used during the search were: “diabetic foot”, “partial hallux amputation”, “interphalangeal arthroplasty”, “metatarsal head resection” and “sesamoidectomy”. Searches were filtered for studies published in English.
The literature review was performed independently by two authors (EGM and MGM) who screened all titles and abstracts for eligibility on predefined inclusion criteria. Any discrepancies between the two reviewers were discussed with a third reviewer (JLM).
Inclusion criteria were studies enrolling patients with DFO in different forefoot areas who were treated by conservative surgery depending on ulcer location. We limited our review to researches that define the surgical technique in the methods section for a specific DFU location. We did not limit the care setting of the included studies. Reference lists of all retrieved studies were cross-checked for additional reports.
Exclusion criteria were non-original articles, including letters or comments and studies without data available for analysis. Additionally, references of narrative and systematic reviews were scrutinized for additional articles including the last update of IWGDF Guidelines.2
A total of 55 records were identified by the literature research. At the end of the screening process, 14 studies met the inclusion criteria.
After selection of the articles, the review was divided into sections based on analysis of the evidence with surgical approaches depending on the location of the forefoot DFO as described in the literature.
2.1. Conservative surgical techniques for forefoot diabetic foot osteomyelitis
2.1.1. DFU location: hallux
2.1.1.1. Plantar or distal hallux DFU. Osteomyelitis of the distal phalanx of the hallux
Patients with diabetic peripheral neuropathy are at high risk of plantar and distal hallux ulcerations associated with the presence of digital deformities, such as hammertoe, excessive digit length of the toe or biomechanical abnormalities (such as limited first metatarsophalangeal joint [MTPJ]), and ankle joint mobility.10,11
Usually, a DFU located in the plantar surface of the big toe is the most common point of entry of OM of the distal phalanx of the hallux; in addition to this location, the tip of the hallux becomes another site of DFU complicated with OM as shown in Fig. 1.11
Fig. 1.
1a: Plantar diabetic foot ulcer (DFU) on the hallux. 1b: DFU on the tip of the big toe.
Surgical treatment of bone infection at this level involves partial or complete phalangectomy or treatment by Distal Syme Hallux Amputation (DSHA) technique depending on the spread of the infection.10, 11 Partial hallux amputations are performed by distal phalangectomy. The hallux is approached through the plantar or distal ulcer using a fish-mouth type incision used to create a durable plantar flap, which is then rotated dorsally for primary closure (Fig. 2, Fig. 3).10
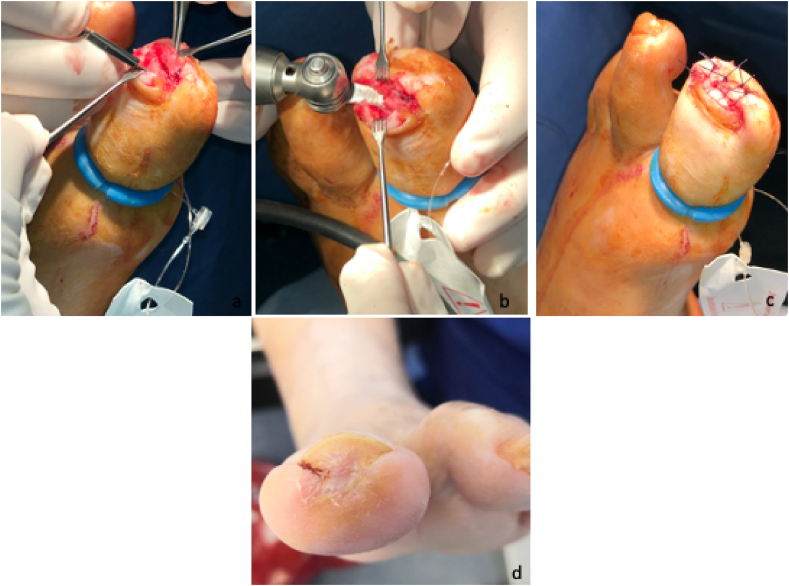
Fig. 2.
Partial distal phalangectomy performed in DFU in the tip of the toe approached through the ulcer and closure via primary intention. 2a: Soft tissue anatomical dissection and bone exposure using a fish-mouth type incision. 2b: tip of the distal phalanx removal with sagittal saw. 2c: primary closure with simple suture. 2d: wound closure at 7 weeks.
Fig. 3.
3a:Pre-operative X-ray. 3b: Post-surgical X-ray.
In cases of bone infections that affect the total integrity of the distal phalanx, the DSHA procedure would be selected.11 This surgical technique involves a transverse dorsal incision that extends directly into the interphalangeal joint to allow for easy disarticulation of the distal phalanx. Dorsal incision is followed by a plantar incision to create a plantar flap that will be advanced dorsally to cover the wound defect after bone excision. The tip of the proximal phalanx can then be remodeled to remove the bony prominence after which it is finally closed with a suture (Fig. 4, Fig. 5).11
Fig. 4.
Distal Syme Hallux Amputation (DSHA) procedure and primary closure with suture. 4a-4b: transverse dorsal incision that extends directly into the interphalangeal joint. 4c:distal phalanx disarticulation. 4d:primary closure with simple suture. 4e,f: plantar and dorsal vision after wound closure after 10 weeks.
Fig. 5.
5a: Pre-operative X-ray. 5b: Post-surgical X-ray.
2.1.1.2. Medial-plantar or dorsal hallux DFU. Osteomyelitis of the interphalangeal joint of the hallux
Ulcers involving the interphalangeal joint of the hallux are often chronic and recurrent and frequently become complicated by osteomyelitis,12 preceded by DFU located on the plantar or dorsal surface of the interphalangeal joint (IPJ). Arthroplasty of the IPJ without fixation when possible can prevent hallux amputation.13
In case of a plantar ulcer, the procedure consists of a plantar approach via an ellipsoidal excision through the ulcer. After the ulcerectomy is performed in the location of the infected bone, resection of the bone is performed by removal of the head of the proximal phalanx and the base of the distal phalanx as shown in Fig. 6, Fig. 7.6,14,15
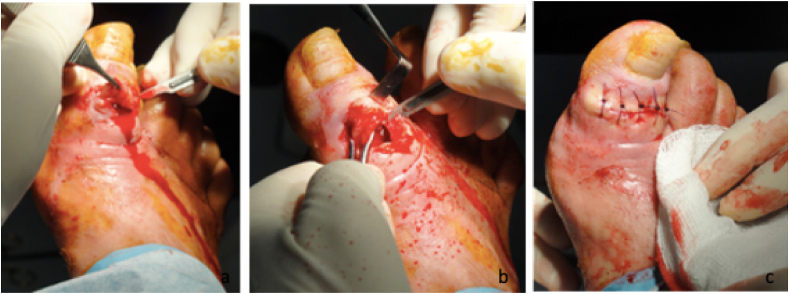
Fig. 6.
Hallux interphalangeal joint (IPJ) arthroplasty via a plantar approach through the ulcer followed by a secondary closure. 6a: plantar approach via ellipsoidal incision and soft tissue dissection with bone exposure. 4b,4c: removal of the head of the proximal phalanx and the base of the distal phalanx. 4d:primary closure of the extremes of the incision leaving open the central part of the surgical wound to be managed by conservative treatment. 4e: wound closure after 9 weeks.
Fig. 7.
7a; Preoperative X-ray. 5b; Postsurgical X-ray.
For a dorsal IPJ ulcer, the approach occurs via a dorsal longitudinal incision through the ulcer followed by a retraction of the extensor hallucis longus or if necessary exposure, transection, or lengthening, and later repairing followed by the bone removal (Fig. 8).6,14,16 Bone cartilage should not be left exposed due to the avascular characteristic of this tissue, which may not generate bone coverage with granulation tissue and favors dehiscence and/or reinfection. The choice of closure will depend on the possible co-existence of a soft tissue infection.17
Fig. 8.
IPJ arthroplasty by dorsal approach and closure via primary intention. 8a: dorsal approach via transverse incision and soft tissue dissection with bone exposure. 8b: bone extraction. 8c:primary closure with simple suture.
2.1.2. DFU location: lesser toes
2.1.2.1. Plantar and distal DFU. Osteomyelitis of the distal phalanx of the lesser toes
The apical and plantar aspect of the lesser toes are a frequent location of DFU appearance and involve the distal phalanx due to the presence of deformities, such as claw and hammer toe.18,19 Surgical approach of DFO at this level is an easy procedure performed by a distal phalangectomy that could involves the removal of part or the totally of the distal phalanx.6 The procedure will be performed using a fish-mouth type incision through the ulcer and consecutively, the removal of the infected bone followed by a curettage of the middle phalanx (Fig. 9). In case of bone infection that affects the total integrity of the distal phalanx, the DSHA procedure would be selected.20
Fig. 9.
Partial distal phalangectomy of the second toe. 9a: fish-mouth incision. 9b: tip of the distal phalanx removal with sagittal saw. 9c: curettage of the distal phalanx. 9d:primary closure with simple suture. 9e: wound closure after 2 weeks.
Additionally, a percutaneously flexor tenotomy combined with bone removal has been described as an effective and safe procedure that could be performed curatively in order to minimize recurrence rates.21 The procedure is advocated for flexible toe deformities, and recent literature has highlighted the importance of an etiopathogenic diagnosis of toe deformities.22 A certain proportion of patients have an extensor substitution deformity, and the flexor tenotomy could not be indicated. Therefore, patients may be subject to a biomechanical assessment. First, the flexibility of the deformity should be evaluated. This evaluation will be performed using the Kellikian push-up test. If the deformity corrects by the application of pressure at the base of the metatarsophalangeal joint (MTPJ), it is then considered flexible; in contrast, the persistence of clawing indicates a rigid deformity.23
Etiopathogenic of the deformity is then stratified following the assessment previously described24; flexor stabilization is stratified when a toe deformity is evident in the late phase of gait. Flexor substitution will be identified when the deformity is visible in the heel lift phase of gait. Finally, extensor substitution can be identified when the deformity is apparent during the swing phase of gait. When indicated, the procedure consists of locating the tendon by placing it under tension followed by a subsequent transversal incision. The wound following the tenotomy will be sutured (Fig. 10).25
Fig. 10.
Plantar phalangectomy closed by suture combined with percutaneously flexor tenotomy of the second toe.
2.1.2.2. Dorsal or interdigital DFU. Osteomyelitis of the proximal or distal interphalangeal joint
DFUs complicated with OM that involve the IPJ of lesser toes are frequently located on the dorsal or interdigital (medial or lateral) aspect of the lesser toes. Dorsal DFUs located in the lesser toes are associated with the presence of claw or hammer toes deformities involving almost all of the dorsum of the proximal or distal IPJ,18 while interdigital ulcers are associated with the presence of deformities over the condyle of the phalanx and usually due to the use of unfitted footwear (Fig. 11).26
Fig. 11.
11a: Dorsal DFU in the second toe. 11b: Interdigital DFU (lateral aspect of the fourth toe).
Resection arthroplasty is the surgical procedure used to manage fixed forms of claw or hammer toe deformities. It includes the removal of any IPJ.6
When a dorsal DFU is present, an ulcerectomy will be performed via the dorsal approach in the original wound, while if an interdigital DFU is present, a longitudinal incision in the dorsum will be made.17 The infected bone will be removed, and the surgical wound will be closed. In case of DFUs located on distal IPJs, the procedure consists of resecting the base of the distal and the head of the middle phalanxes. If the DFU is located in the proximal IPJ, the part of bone that is removed will be the base of the middle and the head of the proximal phalanxes (Fig. 12, Fig. 13). In addition, a flexor tenotomy can be performed as has been previously mentioned in the text and is preceded by a biomechanical assessment.22
Fig. 12.
Arthroplasty of proximal interphalangeal joint of the fourth toe in a DFU located in the dorsal aspect of the toe. 12a: dorsal approach via ellipsoidal incision and soft tissue dissection with bone exposure. 12b: removal of the head of the proximal phalanx and the base of the middle phalanx. 12c: primary closure with simple suture.12d: wound closure after 3 weeks.
Fig. 13.
a: Pre-operative X-ray. 13b: Post-surgical X-ray.
2.1.3. DFU location: sesamoids. Osteomyelitis of sesamoids and/or metatarsophalangeal joint
Sesamoid bones are frequently involved in DFU located in the plantar surface of the first metatarsal head.27 The surgical decision should focus on avoiding first ray amputation in order to preserve the functionality of the foot.28
Sesamoidectomy has been described as removal of one or both sesamoid bones depending of the infection extent. Surgical procedure could be associated with an arthroplasty of the first metatarsal head in those cases in which affectation of the first metatarsal head that does not require a metatarsal head resection.6
The procedure consists of a medial incision to approach the joint or a plantar approach through the DFU.29, 30 After opening the capsule, removal of the sesamoids is performed, and if necessary, a Keller arthroplasty procedure will follow the sesamoidectomy procedure. First, resection of the plantar surface of the first metarsal head is followed by removal of the medial deformity, condyle of the metatarsal head, and the base of the proximal phalanx if that structure is involved. Arthroplasty of the first metatarsophalangeal joint can be fixed with an external fixation device such as Kirschnner wire (KW).29 Primary closure will be performed in the medial approach,29 and in cases in which a plantar approach is selected, the ulcer will be managed using conservative treatment that is capable of benefitting from negative pressure wound therapy (NPWT) treatment (Fig. 14, Fig. 15).30,31
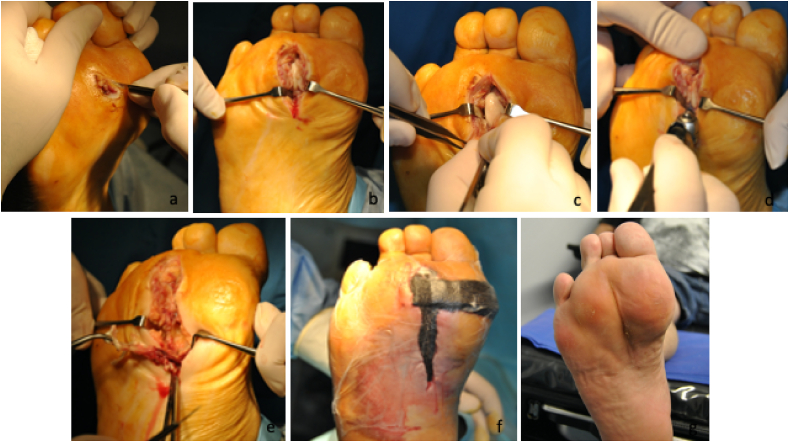
Fig. 14.
Sesamoidectomy of medial and lateral sesamoids combined with a Keller arthroplasty. 14a: medial approach incision and capsule exposure. 14b; medial sesamoidectomy. 14c,d: plantar and medial metatarsal head condilectomy. 14e: resection of the proximal phalanx base. 14f: primary closure with simple suture and fixation with KW.14 g,h: wound closure after 12 weeks.
Fig. 15.
15a: Pre-operative X-ray. 15b: Post-surgical X-ray.
2.1.4. DFU location: metatarsal heads. Osteomyelitis of metatarsal heads
Metatarsal head resection (MHR) is a common and standardized procedure that is indicated as part of the surgical treatment of metatarsal head osteomyelitis.32
The procedure was defined by Griffiths et al.32 as a bone osteotomy at the surgical neck of the metatarsal from which the metatarsal head is removed via a dorsal approach and primary closure with sutures is performed. Despite this standard procedure, technique procedure has suffered from changes over the years that have yielded different results.33 In that respect, recent literature34 has demonstrated the importance of a surgical approach that depends on the ulcer’s characteristics in order to minimize short- and long-term complications. Two types of approaches are described: (1) plantar or (2) dorsal. The selection of the appropriate procedure for these patients should be determined based on the consideration of several underlying factors.35
The dorsal approach consists of a skin incision on the dorsal surface that extends from the base of the toe to the midpoint of the metatarsal shaft; the extensor tendon will be protected by retraction, while the incision will reach deep down to the bone. In this case, the dorsal incision will be closed by primary suturing (Fig. 16, Fig. 17).35
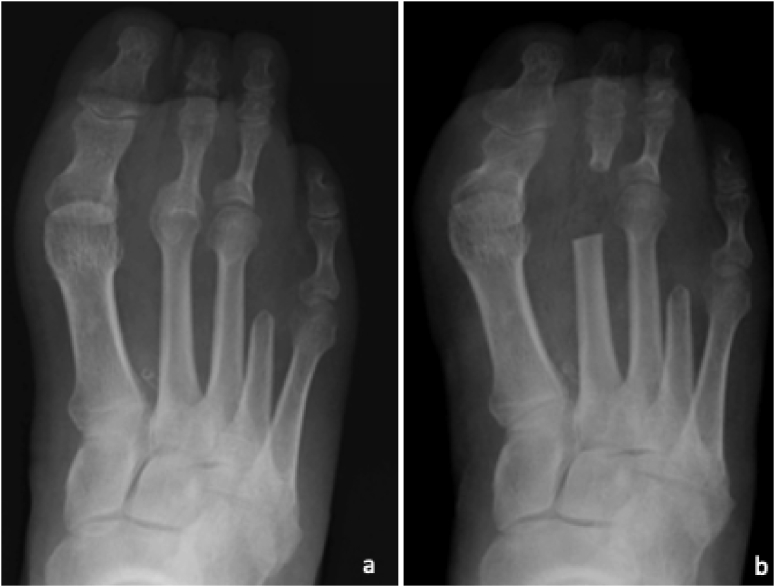
Fig. 16.
Metatarsal head resection by dorsal approach of the second and third metatarsal heads. 16a:soft tissue dissection with metatarsal head exposure. 16b: resection of the second head with sagittal saw. 16c: removal of the second metatarsal head. 16d: primary closure with simple suture. 16e,f: wound closure of the plantar DFU after 1 week and wound closure of the dorsal incision after 3weeks.
Fig. 17.
17a: Pre-operative X-ray. 17b: Post-surgical X-ray.
This approach is indicated in case of a small DFU (<1 cm2) and shallower ulcers.35
The plantar approach consists of an incision on the plantar surface through which the ulcer by means of conic ulcerectomy is removed; this process also removes both walls and the bottom of the lesion after which an MHR will be performed. Plantar postsurgical ulcera are allowed to heal by secondary intention.35 International guidelines recommend the use of NPWT in cases of post-operative wounds; therefore, NPWT is indicated in patients who underwent an MHR via the plantar approach in which the resulting cavity and postsurgical bone exposure may have benefitted from its effects (Fig. 18, Fig. 19).36
Fig. 18.
Second metatarsal head resection by plantar approach. 18a: conic ulcerectomy 18b,c:.metatarsal head exposure. 18d: resection of the second head with sagittal saw. 18e: soft tissue debridement. 18f: negative wound pressure therapy application. 18g: wound closure after 11 weeks.
Fig. 19.
19a: Pre-operative X-ray. 19b: Post-surgical X-ray.
This approach is indicated in patients with bigger ulcers (>1 cm2, equal or greater in size than the metatarsal head) and those ulcers that involve deep structures, such as tendon or bone.35
3. Discussion
The current review describes a total of seven types of conservative surgical procedures for the treatment of DFO in the forefoot. Small technical variations have been found between surgical procedures in different studies. In that respect, recent literature indicates that surgical techniques will depend mainly on the surgeon’s skills.38 We tried to summarize surgical procedures described on the literature depending on OM location in order to achieve surgical techniques standardization to prevent late complications.
Conservative surgical treatment of diabetic foot osteomyelitis has demonstrated to be safe and effective.34,38 During the last several decades, the DFO surgical approach has been based on conservative surgery, which could be an attractive alternative to amputations, with better results with respect to wound-healing, infection control9,39 and mortality.7 The surgical technique must be based on an OM approach for that removes the part of infected bone and maintaining the functionality of the foot.26
Healing rates derived from conservative surgery showed in different ranges from 80%,784.6%,40 86.3%,41 to 100%40 depending on the procedures and the profiles of evaluated patients. Despite these interesting results, outcomes derived from conservative surgery are largely related to several factors, such as the presence of ischemia,42 co-morbid soft tissue infections,43 or the amount of resected bone,44 all of which are factors that must be taken into account.
Piaggesi et al.7 showed recently that conservative surgery performed by a multidisciplinary team reduces healing times and mortality rates. This positive trend from radical surgery to conservative and especially to reconstructive surgery was observed over a period of fifteen years.
The evidence base for conservative surgery management of forefoot OM in people with diabetes is weak, and good quality research studies, especially relating to studies of direct relevance to routine clinical care, are needed. Jeffcoate et al.45 summarized the core details required in the planning and reporting of intervention studies in the prevention and management of diabetic foot ulcers, including studies that focus on infection. Most of the papers included in the current review are comparative with a low level of evidence (3–5). In the future, researchers must focus on performing randomized clinical trials (RCT) to show the clinical efficacy of conservative techniques. A summary of conservative techniques and its levels of evidence are showed in Table 1.
Table 1.
Summary of surgical approaches of DFO in forefoot locations with their respective Sackett’s levels of evidence.37
| DFU location: HALLUX | |||
|---|---|---|---|
| Anatomical location | Surgery Technique | Surgical Approach | Level of evidence |
| Plantar or distal (“Tip of the toe”) | Partial hallux amputation | Plantar (fish mouth incision) | Level 3b |
| Distal Syme Hallux Amputation | Transverse dorsal incision + plantar incision flap | Level 4 | |
| Dorsal or plantar-medial | Interphalangeal joint arthroplasty | Dorsal/medial (through the ulcer) | Level 3b-4 |
| DFU location: LESSER TOES (2nd to 5th) | |||
| Plantar or distal (“Tip of the toe”) | Partial phalangectomy | Plantar (fish mouth incision) | Level 4 |
| Dorsal or plantar-medial | Interphalangeal joint arthroplasty | Dorsal | Level 4 |
| DFU location: PLANTAR SURFACE METATARSAL HEADS | |||
| Sesamoids | Sesamoidectomy | Plantar (through the ulcer)/medial. | Level 4 |
| Metatarsal Heads | Metatarsophalangeal joint arthroplasty | Plantar or Dorsal | Level 4 |
| Metatarsal head resection | Plantar or Dorsal | Level 2a | |
The current review has some limitations. First, due to selection bias, it may not have included some publications. However, most of the frequently used techniques are included in the manuscript. Further systematic reviews are needed to summarize the surgical outcomes of conservative techniques.
Additionally, the decision of the included articles has been partially biased by our personal preferences and surgical experience.
4. Conclusions
This review describes seven conservative surgical procedures for the treatment of DFO in the forefoot. When indicated, conservative surgery for DFUs in patients with chronic forefoot OM is a safe and effective option that increases the chances of healing and reduces the possibility of limb loss and death compared with radical amputation procedures. Since a lack of high level of evidence exists, future investigations should be focused on RCT designs. The results of prospective trials could help surgeons select the appropriate procedure in each case in order to minimize surgery-related complications.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
No conflict of interest has been declared by the author(s).
Contributor Information
José Luis Lázaro-Martínez, Email: diabetes@ucm.es.
Marta García-Madrid, Email: magarc28@ucm.es.
Yolanda García-Álvarez, Email: yolienf3@hotmail.com.
Francisco Javier Álvaro-Afonso, Email: fraalv@hotmail.com.
Irene Sanz-Corbalán, Email: iresanzcorbalan@hotmail.com.
Esther García-Morales, Email: esthergarciamorales@yahoo.es.
References
- 1.Lipsky B.A. Bone of contention: diagnosing diabetic foot osteomyelitis. Clin Infect Dis. 2008;47(4):528–530. doi: 10.1086/590012. [DOI] [PubMed] [Google Scholar]
- 2.Lipsky B.A., Senneville E., Abbas Z.G. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update) Diabetes Metab Res Rev. 2020;36(1) doi: 10.1002/dmrr.3280. [DOI] [PubMed] [Google Scholar]
- 3.Berendt A.R., Peters E.J., Bakker K. Diabetic foot osteomyelitis: a progress report on diagnosis and a systematic review of treatment. Diabetes Metab Res Rev. 2008;24(1):145–161. doi: 10.1002/dmrr.836. [DOI] [PubMed] [Google Scholar]
- 4.Lipsky B.A., Berendt A.R., Deery H.G. Diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2004;39(7):885–910. doi: 10.1086/424846. [DOI] [PubMed] [Google Scholar]
- 5.Lipsky B.A. Treating diabetic foot osteomyelitis primarily with surgery or antibiotics: have we answered the question? Diabetes Care. 2014;37(3):593–595. doi: 10.2337/dc13-2510. [DOI] [PubMed] [Google Scholar]
- 6.Aragon-Sanchez J., Lazaro-Martinez J.L., Alvaro-Afonso F.J., Conservative Molines-Barroso R. Surgery of diabetic forefoot osteomyelitis: how can I operate on this patient without amputation? Int J Low Extrem Wounds. 2015;14(2):108–131. doi: 10.1177/1534734614550686. [DOI] [PubMed] [Google Scholar]
- 7.Piaggesi A., Iacopi E., Pieruzzi L., Coppelli A., Goretti C. Diabetic foot surgery "Made in Italy". Results of 15 years of activity of a third-level centre managed by diabetologists. Diabetes Res Clin Pract. 2020;167:108355. doi: 10.1016/j.diabres.2020.108355. [DOI] [PubMed] [Google Scholar]
- 8.Armstrong D.G., Bharara M., White M. The impact and outcomes of establishing an integrated interdisciplinary surgical team to care for the diabetic foot. Diabetes Metab Res Rev. 2012;28(6):514–518. doi: 10.1002/dmrr.2299. [DOI] [PubMed] [Google Scholar]
- 9.Aragon-Sanchez J. Treatment of diabetic foot osteomyelitis: a surgical critique. Int J Low Extrem Wounds. 2010;9(1):37–59. doi: 10.1177/1534734610361949. [DOI] [PubMed] [Google Scholar]
- 10.Oliver N.G., Attinger C.E., Steinberg J.S., Evans K.K., Vieweger D., Kim P.J. Influence of hallux rigidus on reamputation in patients with diabetes mellitus after partial hallux amputation. J Foot Ankle Surg. 2015;54(6):1076–1080. doi: 10.1053/j.jfas.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Boffeli T.J., Goss M.S. Distal Syme hallux amputation for tip of toe wounds and gangrene complicated by osteomyelitis of the distal phalanx: surgical technique and outcome in consecutive cases. J Foot Ankle Surg. 2018;57(3):456–461. doi: 10.1053/j.jfas.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 12.Nube V.L., Molyneaux L., Yue D.K. Biomechanical risk factors associated with neuropathic ulceration of the hallux in people with diabetes mellitus. J Am Podiatr Med Assoc. 2006;96(3):189–197. doi: 10.7547/0960189. [DOI] [PubMed] [Google Scholar]
- 13.Rosenblum B.I., Giurini J.M., Chrzan J.S., Habershaw G.M. Preventing loss of the great toe with the hallux interphalangeal joint arthroplasty. J Foot Ankle Surg. 1994;33(6):557–560. [PubMed] [Google Scholar]
- 14.Stephens H.M. The diabetic plantar hallux ulcer: a curative soft tissue procedure. Foot Ankle Int. 2000;21(11):954–955. doi: 10.1177/107110070002101111. [DOI] [PubMed] [Google Scholar]
- 15.Tamir E., Finestone A.S., Avisar E., Agar G. Toe-sparing surgery for neuropathic toe ulcers with exposed bone or joint in an outpatient setting: a retrospective study. Int J Low Extrem Wounds. 2016;15(2):142–147. doi: 10.1177/1534734616636311. [DOI] [PubMed] [Google Scholar]
- 16.Lew E., Nicolosi N., McKee P. Evaluation of hallux interphalangeal joint arthroplasty compared with nonoperative treatment of recalcitrant hallux ulceration. J Foot Ankle Surg. 2015;54(4):541–548. doi: 10.1053/j.jfas.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 17.Kim J.Y., Kim T.W., Park Y.E., Lee Y.J. Modified resection arthroplasty for infected non-healing ulcers with toe deformity in diabetic patients. Foot Ankle Int. 2008;29(5):493–497. doi: 10.3113/FAI-2008-0493. [DOI] [PubMed] [Google Scholar]
- 18.Isakov E., Budoragin N., Shenhav S., Mendelevich I., Korzets A., Susak Z. Anatomic sites of foot lesions resulting in amputation among diabetics and non-diabetics. Am J Phys Med Rehabil. 1995;74(2):130–133. [PubMed] [Google Scholar]
- 19.Cowley M.S., Boyko E.J., Shofer J.B., Ahroni J.H., Ledoux W.R. Foot ulcer risk and location in relation to prospective clinical assessment of foot shape and mobility among persons with diabetes. Diabetes Res Clin Pract. 2008;82(2):226–232. doi: 10.1016/j.diabres.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 20.Boffeli T.J., Abben K.W., Hyllengren S.B. In-office distal Symes lesser toe amputation: a safe, reliable, and cost-effective treatment of diabetes-related tip of toe ulcers complicated by osteomyelitis. J Foot Ankle Surg. 2014;53(6):720–726. doi: 10.1053/j.jfas.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 21.Bonanno D.R., Gillies E.J. Flexor tenotomy improves healing and prevention of diabetes-related toe ulcers: a systematic review. J Foot Ankle Surg. 2017;56(3):600–604. doi: 10.1053/j.jfas.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Sanz-Corbalan I., Lazaro-Martinez J.L., Garcia-Alvarez Y., Garcia-Morales E., Alvaro-Afonso F., Molines-Barroso R. Digital deformity assessment prior to percutaneous flexor tenotomy for managing diabetic foot ulcers on the toes. J Foot Ankle Surg. 2019;58(3):453–457. doi: 10.1053/j.jfas.2018.09.015. [DOI] [PubMed] [Google Scholar]
- 23.Muscarella V.BSAotFaA. first ed. vol. 29. Elsevier Health Sciences; Philadelphia: 2012. (An Issue of Clinics in Podiatric Medicine and Surgery). No. 1. [Google Scholar]
- 24.McGlamry E.D.J.A., Green D.R. Deformities of the intermediate digits and metatarsophalangeal joint. In: Banks A.S., Downey M.S., Martin D.E., Millers S.J., editors. third ed. vol. 1. Lippincott Williams & Wilkins; Philadelphia: 2001. pp. 253–304. (McGlamry’s Comprehensive Textbook of Foot and Ankle Surgery). [Google Scholar]
- 25.Tamir E., McLaren A.M., Gadgil A., Daniels T.R. Outpatient percutaneous flexor tenotomies for management of diabetic claw toe deformities with ulcers: a preliminary report. Can J Surg. 2008;51(1):41–44. [PMC free article] [PubMed] [Google Scholar]
- 26.Lazaro-Martinez J.L., Aragon-Sanchez J., Alvaro-Afonso F.J., Garcia-Morales E., Garcia-Alvarez Y., Molines-Barroso R.J. The best way to reduce reulcerations: if you understand biomechanics of the diabetic foot, you can do it. Int J Low Extrem Wounds. 2014;13(4):294–319. doi: 10.1177/1534734614549417. [DOI] [PubMed] [Google Scholar]
- 27.Molines-Barroso R.J., Lazaro-Martinez J.L., Aragon-Sanchez J., Garcia-Morales E., Beneit-Montesinos J.V., Alvaro-Afonso F.J. Analysis of transfer lesions in patients who underwent surgery for diabetic foot ulcers located on the plantar aspect of the metatarsal heads. Diabet Med. 2013;30(8):973–976. doi: 10.1111/dme.12202. [DOI] [PubMed] [Google Scholar]
- 28.Giurini J.M., Chrzan J.S., Gibbons G.W., Habershaw G.M. Sesamoidectomy for the treatment of chronic neuropathic ulcerations. J Am Podiatr Med Assoc. 1991;81(4):167–173. doi: 10.7547/87507315-81-4-167. [DOI] [PubMed] [Google Scholar]
- 29.Lin S.S., Bono C.M., Lee T.H. Total contact casting and Keller arthoplasty for diabetic great toe ulceration under the interphalangeal joint. Foot Ankle Int. 2000;21(7):588–593. doi: 10.1177/107110070002100711. [DOI] [PubMed] [Google Scholar]
- 30.Stone C., Smith N. Resection arthroplasty, external fixation, and negative pressure dressing for first metatarsophalangeal joint ulcers. Foot Ankle Int. 2011;32(3):272–277. doi: 10.3113/FAI.2011.0272. [DOI] [PubMed] [Google Scholar]
- 31.Rayman G., Vas P., Dhatariya K. Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update) Diabetes Metab Res Rev. 2020;36(1) doi: 10.1002/dmrr.3283. [DOI] [PubMed] [Google Scholar]
- 32.Griffiths G.D., Wieman T.J. Metatarsal head resection for diabetic foot ulcers. Arch Surg. 1990;125(7):832–835. doi: 10.1001/archsurg.1990.01410190024003. [DOI] [PubMed] [Google Scholar]
- 33.Sanz-Corbalan I., Tardaguila-Garcia A., Garcia-Alamino J.M. Resections in diabetic foot patients: a systematic review. J Clin Med. 2020;9(6) doi: 10.3390/jcm9061845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aragon-Sanchez J., Lipsky B.A. Modern management of diabetic foot osteomyelitis. The when, how and why of conservative approaches. Expert Rev Anti Infect Ther. 2018;16(1):35–50. doi: 10.1080/14787210.2018.1417037. [DOI] [PubMed] [Google Scholar]
- 35.Tardaguila-Garcia A., Sanz-Corbalan I., Molines-Barroso R.J., Alvaro-Afonso F.J., Garcia-Alvarez Y., Lazaro-Martinez J.L. Complications associated with the approach to metatarsal head resection in diabetic foot osteomyelitis. Int Wound J. 2018;16(2):467–472. doi: 10.1111/iwj.13055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rayman G., Vas P., Dhatariya K. Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update) Diabetes Metab Res Rev. 2020;36(1) doi: 10.1002/dmrr.3283. [DOI] [PubMed] [Google Scholar]
- 37.Sackett D.L. How are we to determine whether dietary interventions do more good than harm to hypertensive patients? Can J Physiol Pharmacol. 1986;64(6):781–783. doi: 10.1139/y86-133. [DOI] [PubMed] [Google Scholar]
- 38.Lazaro Martinez J.L., Garcia Alvarez Y., Tardaguila-Garcia A., Garcia Morales E. Optimal management of diabetic foot osteomyelitis: challenges and solutions. Diabetes Metab Syndr Obes. 2019;12:947–959. doi: 10.2147/DMSO.S181198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aragon-Sanchez F.J., Cabrera-Galvan J.J., Quintana-Marrero Y. Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement. Diabetologia. 2008;51(11):1962–1970. doi: 10.1007/s00125-008-1131-8. [DOI] [PubMed] [Google Scholar]
- 40.Fujii M., Terashi H., Yokono K. Surgical treatment strategy for diabetic forefoot osteomyelitis. Wound Repair Regen. 2016;24(2):447–453. doi: 10.1111/wrr.12418. [DOI] [PubMed] [Google Scholar]
- 41.Lazaro-Martinez J.L., Aragon-Sanchez J., Garcia-Morales E. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: a randomized comparative trial. Diabetes Care. 2014;37(3):789–795. doi: 10.2337/dc13-1526. [DOI] [PubMed] [Google Scholar]
- 42.Armstrong D.G., Cohen K., Courric S., Bharara M., Marston W. Diabetic foot ulcers and vascular insufficiency: our population has changed, but our methods have not. J Diabetes Sci Technol. 2011;5(6):1591–1595. doi: 10.1177/193229681100500636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aragon-Sanchez J. Clinical-pathological characterization of diabetic foot infections: grading the severity of osteomyelitis. Int J Low Extrem Wounds. 2012;11(2):107–112. doi: 10.1177/1534734612447617. [DOI] [PubMed] [Google Scholar]
- 44.Sanz-Corbalan I., Lazaro-Martinez J.L., Aragon-Sanchez J., Garcia-Morales E., Molines-Barroso R., Alvaro-Afonso F.J. Analysis of ulcer recurrences after metatarsal head resection in patients who underwent surgery to treat diabetic foot osteomyelitis. Int J Low Extrem Wounds. 2015;14(2):154–159. doi: 10.1177/1534734615588226. [DOI] [PubMed] [Google Scholar]
- 45.Jeffcoate W.J., Bus S.A., Game F.L. Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: required details and markers of good quality. Lancet Diabetes Endocrinol. 2016;4(9):781–788. doi: 10.1016/S2213-8587(16)30012-2. [DOI] [PubMed] [Google Scholar]