Abstract
A lumbar herniation disc appears as a major cause of lumbar pain and sciatica. The purpose of the present systematic review is to examine the effectiveness of such exercise programs on pain, disability, quality of life, strength and the assessed time required to return to work/normal activities after undergoing lumbar discectomy surgery. PubMed, MEDLINE, and Google Scholar were used for the selection of randomized controlled trials (RCTs). The PEDro scale was chosen to assess the methodological quality of the included studies. Seven RCTS met the inclusion criteria. According to the evaluation of the PEDro scale, one was considered as « high quality», five as « moderate quality» and one as « low quality». The mean score of the studies was 5.14. The results showed that after such exercise there was an improvement in pain, disability, quality of life, muscle strength and in time required to return to work. The exercise programs have a positive impact on the reduction of pain, disability, time required to return to work/normal activities as well as an increase in quality of life and muscle strength in patients with lumbar discectomy surgery.
Keywords: exercise, Strength, Discectomy, Pain, Disability, Quality of life
1. Introduction
A lumbar herniated disc is characterized by a rupture of the annulus fibrosus that leads to an effusion of the nucleus pulposus. Clinical symptoms include lower extremity hypoesthesia, paresthesias, weakness and radiating pain that is described as sharp, dull, or burning.1
Conservative and surgical methods are being used for the treatment of lumbar disc herniation. Discectomy and microdiscectomy are the most common surgical procedures for lumbar disc herniation.2 Although surgical procedures report high success rates in the early postoperative phase, its long-term positive results are less favorable.3 Surgical treatment compared to conservative treatments was observed to have quicker rehabilitation and was more effective in improving disability in long term and also improved quality of life.4 The most consistent complaints after surgery include continual low back pain, sciatica and hernia recurrence.5
In addition to pain, patients, which are diagnosed with lumbar spine herniation, have unbalanced and weakened flexor and extensor body muscles, therefore, it is necessary to follow an appropriate exercise program.1 Previous studies have found that exercise programs, which are implemented after lumbar disc herniation surgery, effectively reduce postoperative pain, disability, and improve strength of back muscles, return to work and patient-reported outcome functional scores.6, 7, 8, 9 Post-operative exercise programs, that begin early, at 4–6 weeks after surgery, are mostly recommended, although there is not a consensus on the best reported time to begin the program.3,10
The purpose of this systematic review is to examine the effectiveness of such exercise programs on strength, pain, disability, quality of life and time required to return to work in patients who have undergone lumbar discectomy. There is no other recent systematic review to our knowledge, which includes all these measurable variables. Furthermore, there are three other similar systematic reviews which include studies which have been published up to 20136,7,11, whereas the current study includes studies up to 2020. In addition, the Scopic Review of Marchand et al.12 has not included only RCTS and they have not undergone any assessment of risk of bias of their RCTs. In addition, the present study can be clinically significant in terms of health-economics. This is due to lumbar intervertebral disc herniations being the most common causes for individuals of working-age to undergo lumbar spine surgery. Therefore, such conditions are a major public health problem owing to their prevalence and health-care expenditure.13
2. Method
2.1. Searching strategy
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) directions have been followed.14 RCTs were chosen from three different databases: PubMed, MEDLINE and Google Scholar. The key words for this systematic review were: “lumbar discectomy”, “lumbar microdiscectomy”, “lumbar open discectomy”, “lumbar endoscopic discectomy”, “surgery”, “operation”, “surgical back pain”, “strength exercise”, “core stabilization”, “pain”, “disability”, “quality of life”, “strength”, “time work loss” and “returning to work/activities”. According to Mesh terms, the key words were: “diskectomy”, “exercise”, “pain”, “disability evaluation”, “quality of life”, “muscle strength”, “return to work”. Thus, the final key words, that we have used, were: “discectomy”, “microdiscectomy”, “exercise”, “pain”, “disability”, “quality of life”, “muscle strength”, “return to work” which were used with a certain combination using Boolean operators (Table 1). The studies had to be published between January 2010 to June 2020. Two of the authors individually performed the searches, screened the titles and abstracts, and assessed them for inclusion. Any disagreement was resolved by mutual discussion and consultation with the third author. Furthermore, the references of the articles were cross-checked and examined for any additional related articles.
Table 1.
Search strategy.
| No | Key words |
|---|---|
| 1 | “discectomy” OR “microdiscectomy” |
| 2 | “exercise” |
| 3 | “pain” OR “disability” OR “quality of life” OR “muscle strength” OR “return to work” |
| Final search | 1 AND 2 AND 3 |
2.2. Inclusion and exclusion criteria
The inclusion and exclusion criteria were applied by three independent researchers.
Studies that did not meet the inclusion criteria were excluded. All researchers were in agreement concerning the final selection of the included RCTs.
The inclusion criteria were:
-
a)
RCTs published in full text in English
-
b)
Patients underwent lumbar discectomy
-
c)
Patients in the experimental group participated in an exercise rehabilitation program and were compared with another control group
-
d)
Subjects of both genders who were 18 years old and over
-
e)
Examining variables were at least one of the following: pain, disability, quality of life, muscle strength, return to work.
The exclusion criteria were:
-
a)
The control group following a particular exercise rehabilitation program supervised by a physiotherapist
-
b)
The experimental group, besides the exercise rehabilitation program, had an additional intervention which the control group did not have.
2.3. Methodological quality
The PEDro scale was chosen to assess the methodological quality of the included studies. This scale is responsible for the evaluation of RCTs and it is widely used as a valid and reliable tool.15 According to the PEDro scale, a clinical trial study can have a score range of 0–10: 0–3 poor quality, 4–6 moderate quality, and 7–10 high quality. Each research was rated separately by two independent individuals and the results were compared to one another. No differences in scoring were detected between the two raters.
2.4. Measurable variables
The measurable variables examined in this review were pain, disability, quality of life, muscle strength and return to work.
3. Results
3.1. Search and selection of studies
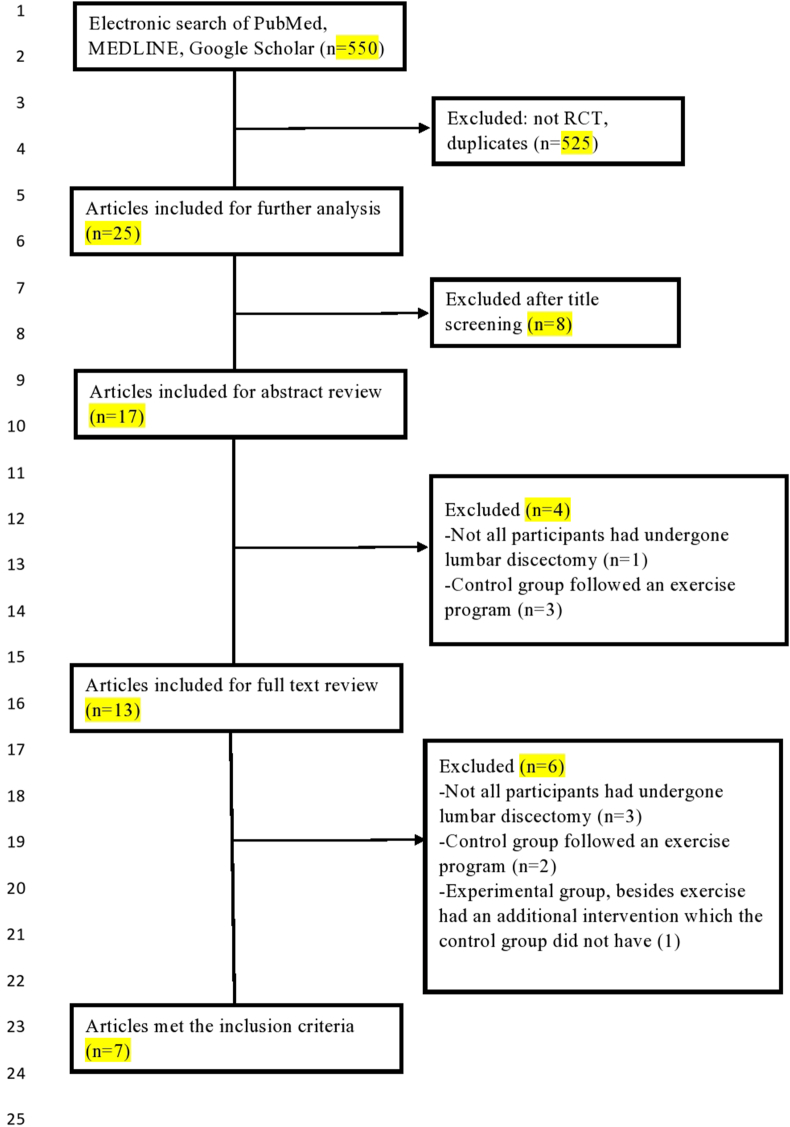
The initial search found 550 studies. Non RCTs and duplicates were excluded. As a result, 25 RCTs, published from 2010 to 2020, were collected. Out of 25 RCTs, 8 studies were excluded after title screening, 4 studies were excluded after abstract review and 6 studies were excluded after full text review. The flow chart of the included studies is presented in Fig. 1. Seven articles met the inclusion criteria and were evaluated with the PEDro scale.
Fig. 1.
Flow chart of the included studies.
3.2. Methodological quality
According to the evaluation of the PEDro scale, out of seven studies that met the inclusion criteria, one was considered as « high quality»,16 five as « moderate quality»17, 18, 19, 20, 21 and one as « low quality».1 The mean score of the evaluation of the studies was 5.14 (Table 2).
Table 2.
Evaluation of the included studies with the PEDro Scale.
| Articles | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Beneck et al.18 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 |
| 2 | Ju et al.1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3/10 |
| 3 | Kim et al.17 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4/10 |
| 4 | Oosterhuis et al.16 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 |
| 5 | Ogutluler Ozkara et al.19 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 6/10 |
| 6 | Rushton et al.20 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6/10 |
| 7 | Jentoft et al.21 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 |
| Mean score: 5.14 | ||||||||||||
3.3. Pain
Five studies examined the effectiveness of exercise programs on pain. Two instruments were used to evaluate neck pain, the Visual Analogue Scale (VAS/PVAS).1,19,20 and the Numeric Pain Rating Scale (NPRS/NRS).16,21 All five studies found an improvement in pain, but the results were considered statistically significant in three of them (Table 3). Among the three statistically significant studies, two were evaluated as « moderate quality»19,21 and one as « low quality».1 The other two studies which evaluated pain, even though they showed an improvement to this variable, the results were not statistically significant. Out of these, one was of «high quality»16 and the other was of «moderate quality».20
Table 3.
General characteristics of the included studies.
| Articles | Sample (drop out) | Intervention | Duration, frequency and intensity of intervention | Outcomes | Evaluation/reassessment | Results |
|---|---|---|---|---|---|---|
| Beneck et al.18 | 98(21) A:51(6) B:47(15) |
A: education & exercise (lumbar extensor strength, endurance training, trunk and lower extremity training) B: education |
3 times a week for 12 weeks | -Quality of life (SF-36) | -At baseline (4–6 weeks postoperatively) -After the therapeutic intervention (12 weeks) |
- Statistically significant improvement on SF-36 role physical and SF-36 bodily pain in group A comparison to group B. |
| Jentoft et al.21 | 70 A:33 B:37 |
A: Information (advise, education) & standard post-operative mobilization. Exercise program (hospital & home): mobility, strength, stretching B: Information (advise, education) & standard post-operative mobilization. |
For 12 weeks 2-6 treatments, 10–30′, 7 exercises, 8–10 repetitions, gradually increase, twice a day (hospital) and 11 exercises (home) |
-Pain: back/hip pain, leg pain (NPRS) -Disability (ODI) |
-At baseline - 6–8 weeks after surgery −12 months after surgery |
-Statistically significant improvement in leg pain in both groups after 12 months. Group A had also statistically significant improvement between 6 and 8 weeks and 12 months. There was not a statistically significant improvement for back/hip pain in both groups. Between both groups group A had statistically significant better results after 12 months for leg pain. -Statistically significant improvement in disability in both groups after 12 months. Group A had also statistically significant improvement between 6 and 8 weeks and 12 months Between both groups, group A had statistically significant better results after 12 months. |
| Ju et al.1 | 14 A:7 B:7 |
A: Medx lumbar extension program and progressive resistance exercise PRE (torso flexion, hip extension, torso rotation, leg extension, seated leg curl, leg press, abdominal press, overhead press) Β: no exercise rehabilitation program |
70′ 3 times a week for 12 weeks Medx: 40–50% maximal isometric strength. Intensity gradually increased by increasing the weight by 5–10% PRE: exercise intensity 40–50% of the participants’ one repetition maximum, 18–20 repetitions per set |
- Pain: back pain, night pain, exercise pain, handicap (VAS) -Strength (Med, USA) |
-At baseline -After the therapeutic intervention for group A (12 weeks) -After resting for weeks for group B |
-Statistically significant improvements in all four types of pain in group A. Group B did not show any statistically significant improvements. -Group A showed statistically significant improvement in strength, whereas group B did not. |
| Kim et al.17 | 34(4) A:11(1) B:12(2) C:11(1) |
A: After 6 weeks of rest the participants followed a progressive resistance exercise (stretching, aerobic exercise, lumbar extension training with the MedX machine) Β: After 6 weeks of rest the participants followed an aquatic backward locomotion exercise (stretching and water exercises) C: After 6 weeks of rest the participants were instructed to maintain everyday activities without any intensive training exercise |
60′ After 6 weeks of rest, exercise program was performed 2 times a week for 12 weeks followed by a period of detraining and then retraining Stretching: 40% HRmax A: aerobic exercise 40–60% HRmax, lumbar extension training 2 sets 15–20 repetitions 50–60% 1 RM B: ranging between 40 and 70% HRmax |
-Strength: isometric lumbar extension strength (MedX) | -At baseline (before surgery) −6 weeks after surgery −12 weeks after surgery (first 6th week exercise program) −18 weeks after surgery (second 6th week exercise program) -after detraining -after retraining |
-Group A and B had greater increases in strength after the first 6th week exercise program in comparison to group C. Statistically significant improvement was shown after the second 6th week exercise in group A and in group B. After the detraining period in both A and B group, the lumbar extension strength decreased similar and became about the same with group C. After the retraining period, group A an B had statistically significant better strength than group C. |
| Ogutluler Ozkara et al.19 | 30 A:15 Β:15 |
Α: instructions (lying, standing, sitting, walking) and an exercise program (strengthening, stretching, passive-active movement, mobilization) Β: instructions (lying, standing, sitting, walking) |
3 times a week, for 12 weeks. 2 sets of each exercise, first week 10 repetitions and after the first week 5–10 repetitions |
-Pain (VAS) -Disability (ODI) -Quality of life (SF-360 -Resume to work |
- At baseline -Reassessment at 6 weeks - After the therapeutic intervention (12 weeks) |
-Statistically significant improvement on VAS in both groups. Between both groups group A had statistically significant better results. -Statistically significant improvement on ODI in both groups. Between both groups, group A had statistically significant better results. -For group A there was statistically significant improvement in SF-36 virality and SF-36 emotional role, whereas in group B only for SF- virality. Between both groups, group A had statistically significant better results in physical functioning of the SF-36, including body pain and social functioning sub-parameters. -Between both groups there was not a statistically significant difference for the term of returning to normal life. |
| Oosterhuis et al.16 | 173 Α:92(12) Β:77(7) |
Α: 1–2 days postoperative care. Advice and instructions for transfers and performing daily living activities. At discharge they were given a booklet providing advice and suggestions for exercises. The therapist focused his treatment on the ability for personal care activities. Exercises were taught with gradually increasing intensity. Β:1–2 days postoperative care. Advice and instructions for transfers and performing daily living activities. At discharge they were given a booklet providing advice and suggestions for exercises |
30′ per week 1 or 2 times a week for 6–8 weeks |
-Pain: leg pain, back pain (NRS) -Disability (ODI) -quality of life: general physical and mental health (SF-12) |
-At baseline -After 3,6,9,12 and 26 weeks |
There was an improvement in all of these variables in both groups but they were not characterized as statistically significant. Between both groups the results were not statistically significant different. |
| Rushton et al.20 | 59 A:29(12) Β:30(11) |
Α:Physiotherapy & leaflet: education, advice, mobility exercises, core stability exercises, progressive approach to exercise Β:Patient leaflet |
For 8 weeks, 8 physiotherapy sessions | -Pain: beck pain, leg pain (VAS) -Disability (RMDQ) -quality of life (EQ-5D) -return to work/function |
-At baseline (4 weeks after surgery) -After the therapeutic intervention (12 weeks after surgery) -Follow-up assessment (26 weeks after surgery) |
-In all the variables there was an improvement in both groups but it wasn’t characterized as statistically significant. |
3.4. Disability
Disability was examined in four studies. The most common instrument for this evaluation was the Oswestry Disability Index which was used in three studies.16,19,21 Furthermore, one study used the Roland Morris Disability Questionnaire (RMDQ) for the evaluation.20 In all four studies there was an improvement in disability. Furthermore, in two of these the reduction of disability was characterized as statistically significant (Table 3) and the evaluation of the PEDro scale showed that it was of «moderate quality».19,21 For the remaining two, which showed an improvement in disability but not significant, one was of «high quality»,16 and the other was of «moderate quality».20
3.5. Quality of life
Four studies assessed the effectiveness of exercise programs on the quality of life. The instruments used were the Short Form Health Survey (SF-36),18,19 the Short Form Health Survey (SF-12),16 and the 5-level EQ-5D version (EQ-5D-5L).20 According to the PEDro scale, three studies were of «moderate quality»,18, 19, 20 and one was of «high quality».16 In all studies there was an increase in quality of life. Particularly, Ogutluler Ozkaria et al.19 found a statistically significant improvement in SF-36 vitality and SF-36 emotional role in the experimental group of the intervention exercise. The other three studies which evaluated quality of life, even though they showed an improvement to this variable, the results were not statistically significant.16,18,20
3.6. Muscle strength
Two studies examined the effectiveness of the exercise programs on maximum isometric lumbar extension strength. Both studies used the MedX Machine for this evaluation.1,17 Both studies reported a statistically significant increase in muscle strength. The evaluation of the PEDro scale showed that one was of «moderate quality»17 and one was of «low quality».1
3.7. Return to work
Two studies assessed the effectiveness of the exercise programs on the time required to return to work/normal activities.19,20 Rushton et al.20 found that at 12 weeks, 59% of participants on the experimental group had returned to work and 65% had returned to normal activities, whereas in the study of Ogutluler Ozkaria et al.19 all the participants had returned to normal life at 12 weeks. Both studies were evaluated as « moderate quality».19,20
3.8. Sample
The sample of our study consisted of 474 patients who had undergone lumbar discectomy or microdiscectomy (males: 65.4%, females: 34.6%) with a mean age of 43 years old (range 18–70 years old).
3.9. Intervention
Patients after surgery in the lumbar region followed an exercise program. The exercise program included stretching, strengthening, passive-active movement, core stabilization, balance exercises, etc. Particularly in Ju’s et al.1 and Kim’s et al.17 studies, part of their rehabilitation program was using the Medx for lumbar extension dynamometer for 15 to 20 repetitions per set. Kim et al.17 had two exercise groups: (a) an aerobic program with lumbar extension training with the MedX machine and (b) a stretching aquatic program. In another study,16 the exercises of the experimental group were adapted for activities concerning personal care and for movement within the house. In Beneck et al.‘s study18 the participants undertook an exercise program of three times a week for 12 weeks which included back extensor and endurance training using a variable-angle Roman chair, accompanied by trunk and lower extremity exercise training. In Ogutluler Ozkaria et al.‘s study19 the experimental group followed an exercise program consisting of pelvic tilt, abdominal exercises, quadriceps and thigh extensor strengthening, stretching and low back strengthening and mobilization. The exercises given during the first week were ten repetitions and exercises after that period, were five repetitions which eventually increased to ten repetitions. Another study20 reported that the exercise group followed mobility and core stability exercises with a progressive approach to exercise for a time period of eight weeks, including one physiotherapy session each week. Lastly, in Jentoft et al.‘s study21 the participants in the experimental group followed seven exercises for 10–30 min of 8–10 repetitions, twice a day in a total of two to six treatments during their time in the hospital depending on the time of their stay and they were also instructed to follow 11 exercises when returning home.
Besides the exercise program, some participants were given verbal instructions, education, and an advising booklet.16,18,19,21 The duration of most RCTs was twelve weeks,1,17, 18, 19,21 but in two trials, the duration was between six and eight weeks.16,20 The frequency of the exercise program varied and ranged from one to three times a week, with the most common frequency being three times a week (Table 3).
4. Discussion
The purpose of the present systematic review was to examine the effectiveness of an exercise program on pain, disability, quality of life, muscle strength and on the time, which was required for the patients to return to work/normal activities after lumbar discectomy surgery. Although diversity, intensity, duration of exercise therapy varied among different included studies, the results revealed that there was a positive impact in all of these measurable variables.
Similar results were found in the systematic review of Snowdon et al.22 which provided moderate quality evidence regarding early physiotherapy rehabilitation after spinal surgery. Particularly, they reported that early physiotherapy rehabilitation is effective and reduces pain significantly, in comparison to the control group. In contrast to these findings, Oosterhuis et al.‘s11 systematic review states that immediate physiotherapy is not more effective when compared to the control group. However, this finding should be interpreted with caution due to the low quality of the results in this study.11 Also, according to Marchand et al.12 significant improvements were found in the experimental intervention groups for pain, disability, strength and for the time required for patients to return to work.
Postoperative pain in and around the area where the operation is carried out usually exists. According to Johansen et al.23 the interventions, which specifically target the mechanisms of pain chronification, could be more effective for the reduction of pain and may be associated with central changes in pain processing and related to comorbid chronic pain. In addition, it has been found that lumbar pain is closely related to lumbar extension strength.24 As a result, the intervention programs place an emphasis on improving these muscles through exercise. Cailliet et al.25 stated that exercise positively enhanced joint capsules, ligaments, tendons, and increased blood flow, thereby contributing to the recovery of injured regions. Furthermore, after an isometric lumbar extension exercise or a resistance exercise program by increasing the cross-sectional areas of the muscles, there was an improvement in muscle strength and function, thus resulting in the prevention and treatment of pain.25,26
The role of the paraspinal muscles in static or dynamic balance and optimum function of the spine as a whole, has extensively been investigated after lumbar discectomy surgery.27,28 A study using MRI scanning showed atrophy in multifidus muscle in patients with disc herniation.29 The weakness of these muscles may contribute to further instability and dysfunction and thus creates a need for active training to improve local capacity after discectomy.26 Overall, lumbar extension exercises enhanced strength and stability in the lumbar region. In particular, Kim et al.30 noted that lumbar extensor muscle exercises significantly improved lumbar muscle strength. Nevertheless, in the study of Kim et al.17 pseudorandomization was used, which may have affected their results. Furthermore, Choi et al.26 showed that the integration of exercise for lumbar extensor muscles leads to increased cross-sectional areas of the multifidus and longissimus muscles and improved lumbar extension strength. Similarly, our study provides evidence that the exercise programs are effective in increasing lumbar extension strength for patients who were operated on for lumbar disc herniation. Particularly, our included studies used for both exercise and assessment the MedX system which is an isokinetic system that allows specific stabilization of the pelvis, thus efficiently training the spinal extensor muscles and isolating them from the hip extensors.31
The present results showed an improvement in disability and in quality of life after an exercise program. Jentoft et al.21 stated that even after 12 months from surgery the improvement in disability was statistically significant. In Oosterhuis et al.‘s16 study there was mentioned that the positive effects are possibly due to the treatment consisting of isolated exercises. Nevertheless, Oosterhuis et al.‘s16 included both patients with lumbar disc herniation and patients with stenosis, thus a more homogenous sample was needed. Rushton et al.20 reported that attention should be placed on comprehending the natural clinical process of disability following lumbar discectomy but their sample size was purposely small to draw valid conclusions.
The positive effects from the exercises were also determined by the evaluation of the time required for the patients to return to work. Individuals of working-age with lumbar intervertebral disc herniation are prone to undergo lumbar spine surgery. Because the financial burden as a consequence of the time-loss from work is considerable, time to return to work has a critical economic value. So the sooner this population returns to work the lower the costs of the health-care system. In the current review, two studies reported participants’ successful return to work or normal activities at 12 weeks after surgery.19,20 Rushton et al.20 found that 59% of participants in the experimental group had successfully returned to work and 65% had returned to normal activities, whereas Ogutluler Ozkaria et al.19 reported that all the participants had returned to normal life at 12 weeks. Similarly, Choi et al.26 demonstrated that 87% of patients in the exercise group returned to work within four months. However, Ogutluler Ozkaria et al.’ study19 had a small number of participants and a follow-up period of only three months. Finally, Sharma et al.32 stated that all patients returned to daily activities and work within a time span of five weeks.
The present review has a few limitations. Only studies that were published in English were included. One major limitation of the present review is that the sample size in most of the selected studies was small in each of the groups. Such small samples may not quantify accurately the effectiveness of the exercise program after lumbar discectomy. Furthermore, the number of studies that evaluate muscle strength and return to work are not enough to draw a conclusion for these measurable variables. Finally, pain, disability, quality of life and strength were examined only on the basis of their statistical significance and not on their clinical significance.
Further consideration of trial design and interventions is required. Future studies are required to include at least one longer-term assessment that considers the long-term effects of the exercise programs. More RCTs with higher methodological quality should be conducted and any treatment exercise protocol for patients who have undergone lumbar discectomy should be justified with further studies. Also, cost-effectiveness studies should be considered. Additional research could focus on evaluating muscle strength and time required to return to work/normal activities to draw valid conclusions. Lastly, multi-center studies should compare the exercise group to a ‘no intervention group’ with a protocol that includes more patients and discusses the duration and the intensity of the exercise which is needed.19, 20
5. Conclusions
The current systematic review revealed that the methodological quality of the included studies using PEDro scale is considered moderate. The results showed that there was an improvement in pain, disability, quality of life, muscle strength and return to work following exercise program, thus exercise programs are recommended for patients who have undergone lumbar discectomy.
Submission declaration
This manuscript has not been published elsewhere and that it has not been simultaneously submitted for publication elsewhere. Its submission is approved by all authors and if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright holder.
Declaration of originality
All tables and figures are your original work and no permissions are required.
Author contributions
Nafsika Atsidakou contributed to the investigation, data curation, writing (original draft).
Aikaterini Evangelia Matsi contributed to the investigation, data curation, writing (original draft). Anna Christakou contributed to the conceptualization, visualization of the work, data curation, writing (original draft and review/editing) and supervision of the work.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
There is no conflict of interest.
References
- 1.Ju S., Park G., Kim E. Effects of an exercise treatment program on lumbar extensor muscle strength and pain of rehabilitation patients recovering from lumbar disc herniation surgery. J Phys Ther Sci. 2012;24(6):515–518. [Google Scholar]
- 2.Rasouli M.R., Rahimi-Movaghar V., Shokraneh F., Moradi-Lakeh M., Chou R. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 2014;9 doi: 10.1002/14651858.CD010328.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ostelo R.W., Costa L.O., Maher C.G., de Vet H.C., van Tulder M.W. Rehabilitation after lumbar disc surgery: an update Cochrane review. Spine. 2009;34:1839–1848. doi: 10.1097/BRS.0b013e3181abbfdf. [DOI] [PubMed] [Google Scholar]
- 4.Chen B.L., Guo J.B., Zhang H.W. Surgical versus non-operative treatment for lumbar disc herniation: a systematic review and meta-analysis. Clin Rehabil. 2018;32(2):146–160. doi: 10.1177/0269215517719952. [DOI] [PubMed] [Google Scholar]
- 5.Yilmaz F., Yilmaz A., Merdol F., Parlar D., Sahin F., Kuran B. Efficacy of dynamic lumbar stabilization exercise in lumbar microdiscectomy. J Rehabil Med. 2003;35:163–167. doi: 10.1080/16501970306125. [DOI] [PubMed] [Google Scholar]
- 6.Ostelo R.W.J.G., Costa L.O.P., Maher C.G., de Vet H.C.W., van Tulder M.W. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev. 2008;4 doi: 10.1002/14651858.CD003007.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Rushton A., Wright C., Goodwin P., Calvert M., Freemantle N. Physiotherapy rehabilitation post first lumbar discectomy. Spine. 2011;36(14):961–972. doi: 10.1097/BRS.0b013e3181f0e8f8. [DOI] [PubMed] [Google Scholar]
- 8.Demir S., Dulgeroglu D., Cakci A. Effects of dynamic lumbar stabilization exercises following lumbar microdiscectomy on pain, mobility and return to work. Randomized controlled trial. Eur J Phys Rehabil Med. 2014;50:627–640. [PubMed] [Google Scholar]
- 9.Hebert J.J., Fritz J.M., Thackeray A., Koppenhaver S.L., Teyhen D. Early multimodal rehabilitation following lumbar disc surgery: a randomised clinical trial comparing the effects of two exercise programmes on clinical outcome and lumbar multifidus muscle function. Br J Sports Med. 2015;49:100–106. doi: 10.1136/bjsports-2013-092402. [DOI] [PubMed] [Google Scholar]
- 10.Erdogmus C.B., Resch K.L., Sabitzer R. Physiotherapy-based rehabilitation following disc herniation operation. Spine. 2007;32:2041–2049. doi: 10.1097/BRS.0b013e318145a386. [DOI] [PubMed] [Google Scholar]
- 11.Oosterhuis T., Costa L.O.P., Maher C.G., de Vet H.C.W., van Tulder M.W., Ostelo R.W.J.G. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev. 2014;3 doi: 10.1002/14651858.CD003007.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marchand A.A., O’Shaughnessy J., Châtillon C.É., Sorra K., Descarreaux M. Current practices in lumbar surgery perioperative rehabilitation: a scoping review. J Manip Physiol Ther. 2016;39(9):668–692. doi: 10.1016/j.jmpt.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Schroeder G.D., Guyre C.A., Vaccaro A.R. The epidemiology and pathophysiology of lumbar disc herniations. Semin Spine Surg. 2016;28(1):2–7. [Google Scholar]
- 14.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Maher C.G., Sherrington C., Herbert R.D., Moseley A.M., Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 16.Oosterhuis T., Ostelo R.W., van Dongen J.M. Early rehabilitation after lumbar disc surgery is not effective or cost-effective compared to no referral: a randomized trial and economic evaluation. J Phys. 2017;63(3):144–153. doi: 10.1016/j.jphys.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 17.Kim Y.S., Park J., Shim J.K. Effects of aquatic backward locomotion exercise and progressive resistance exercise on lumbar extension strength in patients who have undergone lumbar diskectomy. Arch Phys Med Rehabil. 2010;91(2):208–214. doi: 10.1016/j.apmr.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Beneck G.J., Popovich J.M., Selkowitz D.M., Azen S., Kulig K. Intensive, progressive exercise improves quality of life following lumbar microdiskectomy: a randomized controlled trial. Clin Rehabil. 2014;28(9):892–901. doi: 10.1177/0269215514525059. [DOI] [PubMed] [Google Scholar]
- 19.Ogutluler Ozkara G.O., Ozgen M., Ozkara E., Armagan O., Arslantas A., Atasoy M.A. Effectiveness of physical therapy and rehabilitation programs starting immediately after lumbar disc surgery. Turk Neurosurg. 2015;25(3):372–379. doi: 10.5137/1019-5149.JTN.8440-13.0. [DOI] [PubMed] [Google Scholar]
- 20.Rushton A., Heneghan N.R., Calvert M., Heap A., White L., Goodwin P.C. Physiotherapy post lumbar discectomy: prospective feasibility and pilot randomized controlled trial. PloS One. 2015;10(11) doi: 10.1371/journal.pone.0142013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jentoft E.S., Kvåle A., Assmus J., Moen V.P. Effect of information and exercise programmes after lumbar disc surgery: a randomized controlled trial. Physiother Res Int. 2020:e1864. doi: 10.1002/pri.1864. [DOI] [PubMed] [Google Scholar]
- 22.Snowdon M., Peiris C.L. Physiotherapy commenced within the first four weeks post–spinal surgery is safe and effective: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2016;97(2):292–301. doi: 10.1016/j.apmr.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Johansen A., Schirmer H., Stubhaug A., Nielsen C.S. Persistent post-surgical pain and experimental pain sensitivity in the Tromsø study: comorbid pain matters. Pain. 2014;155:341–348. doi: 10.1016/j.pain.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 24.Mayer T., Gatchel R., Betancur J., Bovasso E. Trunk muscle endurance measurement. Isometric contrasted to isokinetic testing in Control subjects. Spine. 1995;20:920–927. [PubMed] [Google Scholar]
- 25.Cailliet R. Philadelphia Daves Company; 1998. Low Back Pain Syndrome; pp. 156–178. [Google Scholar]
- 26.Choi G., Raiturker P.P., Kim M.J., Chung D.J., Chae Y.S., Lee S.H. The effect of early isolated lumbar extension exercise program for patients with herniated disc undergoing lumbar discectomy. Neurosurgery. 2005;57(4):764–772. doi: 10.1093/neurosurgery/57.4.764. [DOI] [PubMed] [Google Scholar]
- 27.Panjabi M.M. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5:383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Goel V.K., Kong W., Han J.S., Weinstein J.N., Gilbertson L.G. A combined finite element and optimization investigation of lumbar spine mechanics with and without muscles. Spine. 1993;18:1531–1541. [PubMed] [Google Scholar]
- 29.Sun D., Liu P., Cheng J., Ma Z., Liu J., Qin T. Correlation between intervertebral disc degeneration, paraspinal muscle atrophy, and lumbar facet joints degeneration in patients with lumbar disc herniation. BMC Muscoskel Disord. 2017;18(1):167. doi: 10.1186/s12891-017-1522-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim Y.S., Park J., Hsu J., Cho K.K., Kim Y.H., Shim J.K. Effects of training frequency on lumbar extension strength in patients recovering from lumbar discectomy. J Rehabil Med. 2010;42(9):839-845. doi: 10.2340/16501977-0607. [DOI] [PubMed] [Google Scholar]
- 31.Graves J.E., Webb D.C., Pollock M.L., Matkozich J., Leggett S.H., Carpenter D.M. Pelvic stabilization during resistance training: its effect on the development of lumbar extension strength. Arch Phys Med Rehabil. 1994;75:210–215. [PubMed] [Google Scholar]
- 32.Sharma S.B., Lin G.X., Jabri H. Radiographic and clinical outcomes of huge lumbar disc herniations treated by transforaminal endoscopic discectomy. Clin Neurol Neurosurg. 2019;185:105485. doi: 10.1016/j.clineuro.2019.105485. [DOI] [PubMed] [Google Scholar]