Abstract
Objective
To determine various morphometric parameters like transverse and sagittal pedicle width; interpedicular distance; antero-posterior and transverse canal diameter and canal surface area at thoracolumbar junction (T11, T12, L1, L2) in central Indian population and compare results with similar studies available in literature.
Material and methods
A prospective, computerized tomography scan based morphometric analysis of thoracolumbar junction was conducted at medical college and tertiary care centre in central India. All asymptomatic cases more than 18 years age with normal lateral radiograph and CT scan of thoracolumbar junction and free from any spinal pathology or trauma were included in the study. Parameters measured were transverse and sagittal pedicle width; interpedicular distance; antero-posterior and transverse canal diameter and canal surface area at thoracolumbar junction (T11, T12, L1, L2).
Results
Mean transverse pedicle width was maximum at T11 and minimum at L1 in both males and females, whereas sagittal width was maximum at T11 and minimum at L2 in both the groups. Interpedicular distance was largest at L1 in both the groups. All the measurements were significantly different (P < 0.05) in males and females. Mean antero-posterior and transverse diameter was maximum at T12 and L2 respectively in both male and female study population. Canal surface area was maximum at L1 among males (230.10 mm2) as well as females (209.02 mm2).
Conclusion
There is significant variation in morphometric parameters of thoracolumbar junction in different races and population. Thorough knowledge of morphometry of a particular population is essential for dealing with pathology or trauma of thoracolumbar junction.
Keywords: Thoracolumbar junction, Pedicle morphometry, Canal measurements, Central Indian population
Source of support
Nil.
1. Introduction
Thoracolumbar spine (T11, T12, L1, and L2) is the transition point between the more rigid thoracic spine and the more flexible lumbar spine. This region is subsequently predisposed to unique patterns of pathology.1 Unfortunately, in adults the part of the spinal cord that terminates at the mechanically vulnerable thoracolumbar junction encompasses the primary efferents for all the lumbosacral roots, and hence canal encroachment can lead to cataclysmic neurological sequelae. Sagittal alignment and pedicle and vertebral canal morphometry of thoracolumbar junction are the crucial parameters which can assist in better perception and management of thoracolumbar ailments.2, 3, 4
Notwithstanding the diversified studies available of thoracic and lumbar vertebral morphometry separately or in groups,5,6 studies pertaining to thoracolumbar junction morphometry employing Computerized Tomography (CT) scan are few and far between. Also, there are very few studies from India. As per author’s knowledge, this is the first study from central India population with maximum number of vertebrae studied.
The intent of this study was to inspect pedicle morphometry and canal measurements of thoracolumbar junction using Computerized Tomography (CT) Scan in the normal population of this region and to thereby construe a normal range.
2. Material and methods
2.1. Inclusion criteria
-
1.
All subjects older than 18 years with normal neurological examination.
-
2.
Lateral radiograph and CT scan of thoracolumbar junction (T11, T12, L1 and L2) reported as normal by radiologist and neurosurgeons.
2.2. Exclusion criteria
-
•
Age <18 years
-
•
Major trauma (such as a motor vehicle collision)
-
•
Diseases of the vertebral column, spinal canal, paravertebral soft tissues or retroperitoneum; traumatic vertebral fractures; and Osteoporotic vertebral collapse.
-
•
Segmentation anomalies at thoracolumbar junction.
2.3. Protocol
A plain CT scan (Bright Speed, GE Healthcare) of thoracolumbar junction (T11,T12,L1,L2) was done for all the subjects included in study and following parameters were measured:
- 1.
- 2.
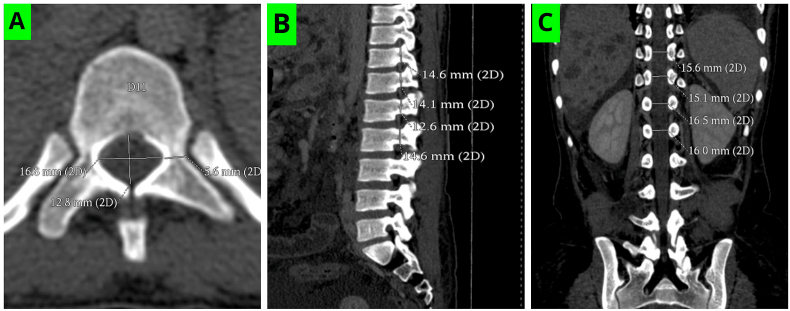
Fig. 1.
Showing (A) Transverse pedicle width,.Anteroposterior and transverse canal diameter (B) Sagittal pedicle width and (C) Interpedicular distance at thoracolumbar junction.
Fig. 2.
Vertebral canal surface area at T11 level.
3. Results
A total of 200 patients were included in the study of which 109 (54.5%) were males and rest were females. More than half of the subjects aged between 31 and 50 years. Mean height in males and females were 158.02 cms and 147.8 cms respectively. Mean weight in males and females were 68.7 kgs and 56.9 kgs respectively (Table 1).
Table 1.
Demographic profile of patients.(n = 200).
| Variables | |
|---|---|
| 1. Sex distribution: Males- Females- |
109 91 |
| 2. Age distribution:(years) <20 21-30 31-40 41-50 51-60 61-70 >70 |
08 35 53 51 36 16 01 |
| 3. Mean height: Males- Females- |
158.02 cms 147.8 cms |
| 4. Mean weight: Males- Females- |
68.7 kgs. 56.9 kgs. |
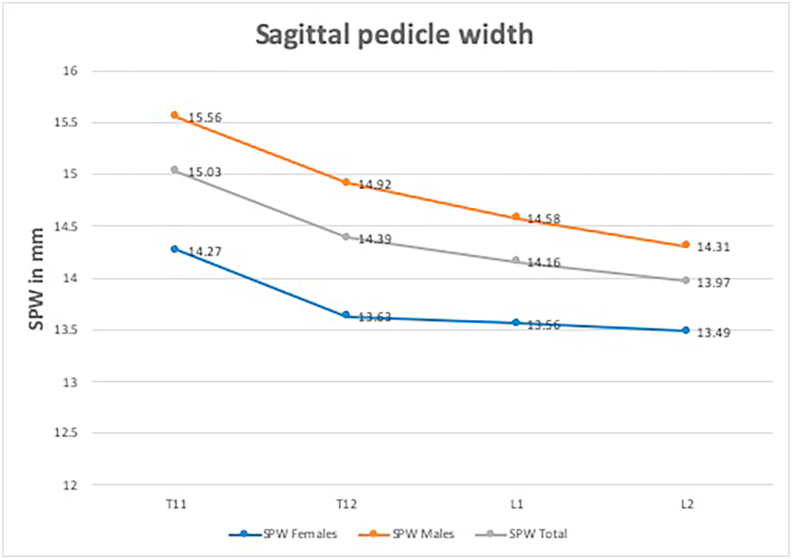
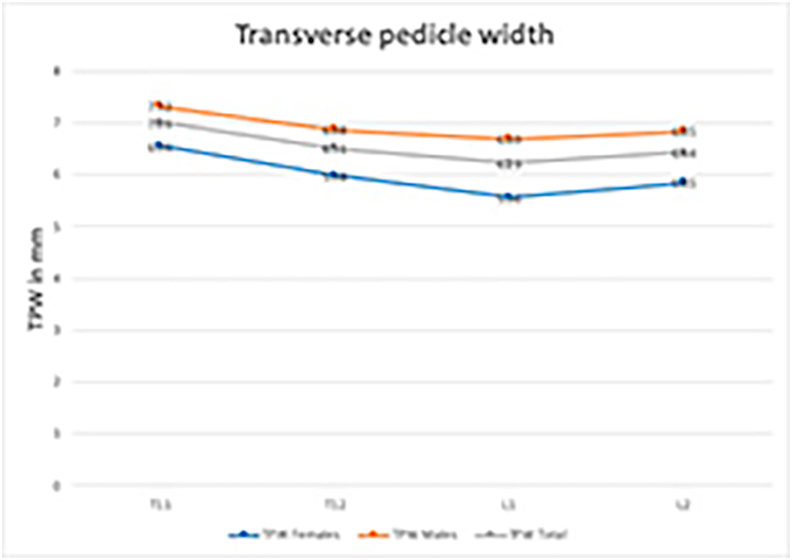
Mean (SD) transverse and sagittal pedicle width and interpedicular distance in mm were measured based on CT image (Table 2). Mean transverse pedicle width was maximum at T11 and minimum at L1 in both males and females (Fig. 3), whereas sagittal width was maximum at T11 and minimum at L2 in both the groups (Fig. 4). Interpedicular distance was largest at L1 in both the groups. All the measurements were significantly different (P < 0.05) in males and females (Table 2).
Table 2.
Mean (SD) of TPW, SPW and IPD of pedicles.
| Pedicle Measurements in CT (mm) | Females |
Males |
Total |
P value |
|||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | (Male vs female) | |
| TPW T11 | 6.56 | 1.45 | 7.32 | 1.38 | 7.01 | 1.45 | 0.009 |
| TPW T12 | 5.98 | 1.47 | 6.88 | 1.39 | 6.51 | 1.49 | 0.004 |
| TPW L1 | 5.56 | 1.34 | 6.69 | 1.43 | 6.23 | 1.50 | <0.001 |
| TPW L2 | 5.85 | 1.26 | 6.85 | 1.49 | 6.44 | 1.48 | 0.001 |
| SPW T11 | 14.27 | 1.95 | 15.56 | 1.88 | 15.03 | 2.00 | 0.001 |
| SPW T12 | 13.63 | 2.15 | 14.92 | 1.90 | 14.39 | 2.09 | 0.002 |
| SPW L1 | 13.56 | 1.79 | 14.58 | 1.60 | 14.16 | 1.74 | 0.004 |
| SPW L2 | 13.49 | 1.85 | 14.31 | 2.15 | 13.97 | 2.06 | 0.016 |
| IPD T11 | 14.98 | 2.07 | 16.17 | 1.64 | 15.68 | 1.91 | 0.002 |
| IPD T12 | 17.15 | 2.28 | 18.39 | 2.17 | 17.88 | 2.29 | 0.005 |
| IPD L1 | 17.95 | 2.01 | 19.27 | 2.45 | 18.73 | 2.36 | 0.007 |
| IPD L2 | 17.17 | 2.31 | 18.56 | 2.51 | 17.99 | 2.51 | 0.006 |
TPW- Transverse pedicle width, SPW-Sagittal pedicle width, IPD- Inter pedicular distance.
Fig. 3.
Transverse pedicle width (TPW) at T11, T12, L1 and L2 level in males and females.
Fig. 4.
Sagittal pedicle width (SPW) at T11, T12, L1 and L2 level in males and females.
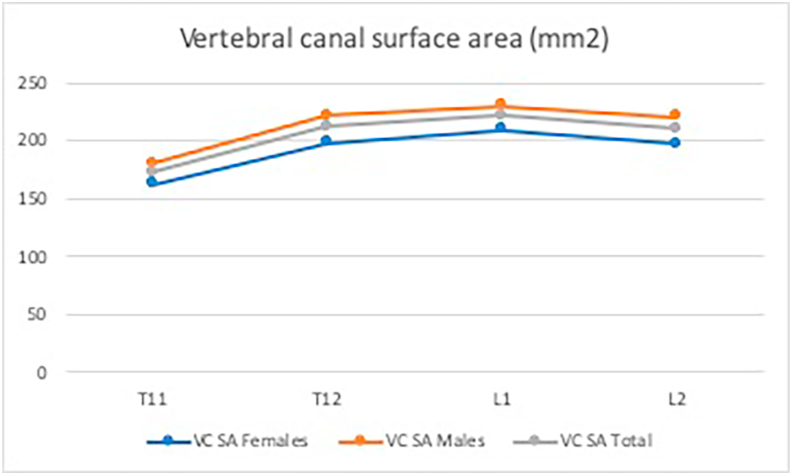
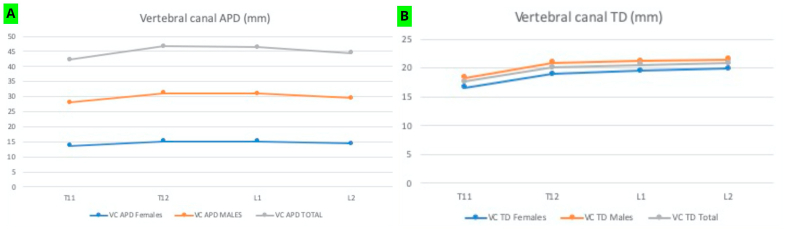
Table 3 shows mean (SD) antero-posterior diameter, transverse diameter and canal surface area of T11 to L2 vertebrae. Mean antero-posterior and transverse diameter was maximum at T12 and L2 respectively in both male and female study population (Fig. 5). Canal surface area was maximum at L1 among males (230.10 mm2) as well as females (209.02 mm2) (Fig. 6). Difference in all measurements between males and females was statistically significant (P < 0.05). (Table 3).
Table 3.
Mean (SD) of antero-posterior diameter, transverse diameter and surface area of vertebral canal. VC APD- Vertebral canal anteroposterior diameter.
| Vertebral canal Measurements CT Scan (MM & MM2) | Female |
Males |
Total |
P Value |
|||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | (Males vs Females) | |
| VC APD T11 | 13.61 | 1.53 | 14.49 | 1.44 | 14.13 | 1.54 | 0.004 |
| VC APD T12 | 15.22 | 1.46 | 15.90 | 1.31 | 15.62 | 1.41 | 0.017 |
| VC APD L1 | 15.12 | 1.23 | 15.81 | 1.25 | 15.53 | 1.28 | 0.007 |
| VC APD L2 | 14.37 | 1.37 | 15.19 | 1.69 | 14.85 | 1.61 | 0.011 |
| VC TD T11 | 16.61 | 1.53 | 18.31 | 2.35 | 17.61 | 2.21 | <0.001 |
| VC TD T12 | 18.98 | 1.75 | 20.92 | 1.99 | 20.12 | 2.11 | <0.001 |
| VC TD L1 | 19.54 | 2.07 | 21.25 | 1.98 | 20.55 | 2.18 | <0.001 |
| VC TD L2 | 19.85 | 1.88 | 21.47 | 2.13 | 20.81 | 2.17 | <0.001 |
| VC SA T11 | 161.85 | 37.72 | 180.41 | 38.60 | 172.80 | 39.14 | 0.019 |
| VC SA T12 | 198.20 | 34.94 | 221.61 | 39.01 | 212.01 | 38.97 | 0.003 |
| VC SA L1 | 209.02 | 32.40 | 230.10 | 37.99 | 221.46 | 37.12 | 0.005 |
| VC SA L2 | 196.80 | 37.08 | 220.12 | 48.54 | 210.56 | 45.48 | 0.011 |
VC TD- Vertebral canal transverse diameter.
VC SA- Vertebral canal surface area.
Fig. 5.
Vertebral canal anteroposterior (A) and transverse diameter (B) at different levels in male and female population.
Fig. 6.
Vertebral canal surface area at T11, T12, L1 and L2 level in males and females.
4. Discussion
Thoracolumbar spine is the transition point between the more rigid thoracic spine and the more flexible lumbar spine and, is resultantly susceptible to unique patterns of pathology in this region.7 The anatomy of the rib cage significantly influences the biomechanical properties of the thoracolumbar spine. Above T10, ribs 3 through 8 articulate anteriorly with the sternum and posteriorly with their associated vertebral body and transverse process, as well as with the vertebral body above via an inferior demi facet. This configuration stabilizes the thoracic spine and increases its rigidity twofold to threefold.8 Below this level, the rigidity of the thoracic spine is reduced as the anatomy evolves into the configuration of the more mobile lumbar spine. Thoracolumbar spinal pathology places the conus medullaris and cauda equina at risk, and injury to these neurological structures has profound functional consequences. The conus medullaris and cauda equina mark the transition between the central and peripheral nervous systems. Injury results in a constellation of upper and lower motor neuron symptoms, depending on the exact site of the lesion. The location of the conus medullaris varies by developmental stage. At birth, the cord fills the vertebral canal and terminates at the lumbosacral junction.9 The distal tip of the spinal cord then ascends with infant development, probably because of the differential growth between the spinal column and spinal cord. In adults, the tip usually terminates at the mid aspect of the first lumbar vertebra. However, its position varies between the lower 11th thoracic and upper 3rd lumbar vertebrae.10 Traditionally, it has been taught that the termination also varies with the position of the spine, although a recent study by Bauer and colleagues found no change in the position of the conus with flexion.11 However, they did demonstrate that the cauda equina displaces medially over the conus with flexion.
A comprehensive knowledge of anatomy and normal spectrum of parameters like sagittal and transverse pedicle width and vertebral canal anteroposterior and transverse diameter of this region are imperative tools in proper devising of management. These measurements diversify in consonance with age, gender, body habitus and race of the subjects. Geographical and genetic considerations leading to these variations are well recognized. Despite plentiful studies in literature, describing normal measurements of thoracic and lumbar region, there is still a dearth of data analyzing the thoracolumbar vertebral dimensions, especially from central India. Therefore, we panned the present study to determine pedicle morphometry and canal measurements of thoracolumbar junction. We have included measurements of T11 to L2 vertebrae in the present study. Various parameters measured and compared in the present study are discussed below.
4.1. Transverse pedicle width
This is the most important parameter in determining the pedicle screw diameter which can be safely placed. In the present study, TPW of thoracic vertebrae [T 11 (7.01 ± 1.45) and T 12 (6.51 ± 1.49)] is more than lumbar vertebrae L 1 (6.23 ± 1.50). On moving from L1 to L2, it again increases (Fig. 3). A similar trend of TPW was seen even if we analyze measurements in males and females separately. It is inferred that TPW is higher among males in comparison to females. In a study by Kim et al. it was shown that the average diameters of T11 and T12 vertebrae were higher than that of L1and L2 and transverse diameter of the pedicle was wider in males as compared to females at all the vertebral levels.12 In a study by Zindrick et al., TPW of T11 was more than T12 and it progressively increased to L2.13 In an Indian study done by Singel et al.,14 they found diameter of lumbar vertebrae more in female than males, which is in contrast to our findings. Based on our results, at all the four levels studied, safe screw diameter in male and female patients is 6.5 mm and 5.5 mm respectively. TPW values were slightly lower in our study in comparison to western literature and comparable to results of most of the studies conducted on Indian population.
4.2. Sagittal pedicle width and interpedicular distance
In the present study, we found that SPW showed a decreasing trend as we move down from T11 to L2. At all levels, it was significantly higher in males as compared to females (Fig. 4). We share the similarity of findings with the study done by Mitra et al.15 A similar observation was also made in a study by Zindrick et al.13 where in case of thoracic vertebrae SPW of T11 was greater than T12 (17.4 vs 15.8) whereas Datir et al.16 and Pai et al.17 found SPW of T12 > T11. In their study on lumbar measurements, Singel et al. found SPW of L1 was more in females (15.7 vs 14.7) than males while SPW of L2 was lower in females.14 In our study, IPD increased from above downwards except at L 2 in both the genders which were analogous to a study by Datir et al.16 and Mitra et al.15
4.3. Vertebral canal APD, TD and SA
Canal measurements influence the chances of developing neurological deficits in spine injury as well as degenerative pathologies. So, It is important to know the baseline values of canal diameters and surface area of a particular population.
Marchesi et al. performed radiological and cadaveric canal measurements from T6 to L5. At thoracolumbar junction, they found maximum VC APD at T12 followed by L1 and minimum VC APD at T11.18 In their study, VC TD was maximum at L1 and L2 and minimum at T11. At all levels, they noted higher TD as compared to APD. We also found similar trends in the present study (Fig. 5). In present study, male and female population was separately analyzed. Although the measurement trends were similar in both sex, males have significantly larger diameters in comparison to females. In the present study, vertebral canal surface area increased from T11 (172.80) to L1 (221.46) and then decreased at L2 (210.56) (Fig. 6). Similar trend was noted in both sex and values in males were significantly higher.
All the parameters measured in our study differ from other studies done in different population groups, which proves the importance of morphometric studies in different population groups. A thorough anatomical knowledge and morphometric orientation of spine of that particular population is necessary for planning and execution of successful spine surgery. Table 4, Table 5, Table 6 shows comparison of TPW, SPW and VC APD respectively in different studies conducted in different geographical population.
Table 4.
Transverse pedicle width (TPW) in different studies.
Table 5.
Sagittal pedicle width (SPW) in different studies.
Table 6.
Vertebral canal Antero-posterior diameter (VC APD) in different studies.
| Studies | T 11 |
T 12 |
L 1 |
L 2 |
||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | |
| Present | 14.49 | 13.61 | 15.90 | 15.22 | 15.81 | 15.12 | 15.19 | 14.37 |
| Gupta and Singla | 16.86 | 17.71 | 17.48 | 16.91 | ||||
| Marchesi et al.18 | 16.3 | 17.7 | 17.8 | 16.8 | ||||
Although our study provides important information regarding thoracolumbar junction morphometry, it has certain strengths and limitations. A large sample size is the cardinal strength of our study. We performed the meticulous morphometric analysis by using CT scan which is precise and unerring as compared to conventional radiograph. With CT we are able to calculate the accurate transverse diameter and surface area which are equally vital in predicting the spinal stenosis. As anomalies of this region are well known in pediatric population but they are not analyzed in this study. We calculated dimensions at mid vertebral level while the degenerative pathology are commonly found to affect the inter-body level. A comparative analysis with patients of thoracolumbar stenosis is required for better correlation.
5. Conclusion
-
•
CT scan is more precise in anatomic morphometric measurement of thoracolumbar spine in normal asymptomatic population.
-
•
These morphometric dimensions show ethnic, racial and geographical discrepancies and hence normal reference values of the population of a particular region is of paramount importance.
-
•
These reference values can be of assistance in preoperative management; surgical planning and post-operative follow up of patients with thoracolumbar stenosis.
-
•
Data comparison with patients of thoracolumbar stenosis results in proficient analysis of result.
-
•
Similar study in pediatric population is required for veracious assessment of congenital anomalies.
Contributor Information
Ketan Hedaoo, Email: drketan14@gmail.com.
Ambuj Kumar, Email: drambuj21@gmail.com.
Brijesh Kumar Singh, Email: brijeshkumarsinghssmc04@gmail.com.
Raghavendra Kumar Sharma, Email: sdr.raghavendra@gmail.com.
Mallika Sinha, Email: mallikaneuro@gmail.com.
Yadram Yadav, Email: yadavyrns@gmail.com.
References
- 1.Abdel M.P., Bodemer W.S., Anderson P.A. Supine thoracolumbar sagittal spine alignment: comparing computerized tomography and plain radiographs. Spine. 2012;37(4):340–345. doi: 10.1097/BRS.0b013e31821946d1. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardt M., Bridwell K.H. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14(7):717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 3.McCormack B.M., Benzel E.C., Adams M.S., Baldwin N.G., Rupp F.W., Maher D.J. Anatomy of the thoracic pedicle. Neurosurgery. 1995;37(2):303–308. doi: 10.1227/00006123-199508000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Kunkel M.E., Schmidt H., Wilke H.-J. Prediction of the human thoracic and lumbar articular facet joint morphometry from radiographic images. J Anat. 2011;218(2):191–201. doi: 10.1111/j.1469-7580.2010.01323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crawford M.B., Toms A.P., Shepstone L. Defining normal vertebral angulation at the thoracolumbar junction. Am J Roentgenol. 2009;193(1):W33–W37. doi: 10.2214/AJR.08.2026. [DOI] [PubMed] [Google Scholar]
- 6.Acharya S., Dorje T., Srivastava A. Lower dorsal and lumbar pedicle morphometry in Indian population: a study of four hundred fifty vertebrae. Spine. 2010;35(10):E378–E384. doi: 10.1097/BRS.0b013e3181cb7f2b. [DOI] [PubMed] [Google Scholar]
- 7.Vaccaro A.R., An H.S., Lin S., Sun S., Balderston R.A., Cotler J.M. Noncontiguous injuries of the spine. J Spinal Disord. 1992;5(3):320–329. doi: 10.1097/00002517-199209000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Andriacchi T., Schultz A., Belytschko T., Galante J. A model for studies of mechanical interactions between the human spine and rib cage. J Biomech. 1974;7(6):497–507. doi: 10.1016/0021-9290(74)90084-0. [DOI] [PubMed] [Google Scholar]
- 9.Malas M.A., Salbacak A., Büyükmumcu M., Seker M., Köylüoğlu B., Karabulut A.K. An investigation of the conus medullaris termination level during the period of fetal development to adulthood. Kaibogaku Zasshi. 2001;76(5):453–459. [PubMed] [Google Scholar]
- 10.Soleiman J., Demaerel P., Rocher S., Maes F., Marchal G. Magnetic resonance imaging study of the level of termination of the conus medullaris and the thecal sac: influence of age and gender. Spine. 2005;30(16):1875–1880. doi: 10.1097/01.brs.0000174116.74775.2e. [DOI] [PubMed] [Google Scholar]
- 11.Bauer D.F., Shoja M.M., Loukas M., Oakes W.J., Tubbs R.S. Study of the effects of flexion on the position of the conus medullaris. Childs Nerv Syst. 2008;24(9):1043–1045. doi: 10.1007/s00381-008-0640-6. [DOI] [PubMed] [Google Scholar]
- 12.Kim N.H., Lee H.M., Chung I.H., Kim H.J., Kim S.J. Morphometric study of the pedicles of thoracic and lumbar vertebrae in Koreans. Spine. 1994;19(12):1390–1394. doi: 10.1097/00007632-199406000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Zindrick M.R., Wiltse L.L., Doornik A. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12(2):160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Tc S., Mm P., Dv G. Published online; 2004. A Study of Width and Height of Lumbar Pedicles in Saurashtra Region; p. 6. [Google Scholar]
- 15.Mitra S.R., Datir S.P., Jadhav S.O. Morphometric study of the lumbar pedicle in the Indian population as related to pedicular screw fixation. Spine. 2002;27(5):453–459. doi: 10.1097/00007632-200203010-00004. [DOI] [PubMed] [Google Scholar]
- 16.Datir S.P., Mitra S.R. Morphometric study of the thoracic vertebral pedicle in an Indian population. Spine. 2004;29(11):1174–1181. doi: 10.1097/00007632-200406010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Pai B.S., Gangadhara Nirmala S., Muralimohan S., Varsha S.M. Morphometric analysis of the thoracic pedicle: an anatomico-radiological study. Neurol India. 2010;58(2):253–258. doi: 10.4103/0028-3886.63808. [DOI] [PubMed] [Google Scholar]
- 18.Marchesi D., Schneider E., Glauser P., Aebi M. Morphometric analysis of the thoracolumbar and lumbar pedicles, anatomo-radiologic study. Surg Radiol Anat. 1988;10(4):317–322. doi: 10.1007/BF02107905. [DOI] [PubMed] [Google Scholar]