Abstract
Introduction
In order to enhance cost-effectiveness, shorter hospital stays have been adopted following hip or knee replacement surgery. This study seeks to describe the incidence of morbidity and mortality, five days after patients were taken to surgery with an expected hospital stay of four days.
Methods
Utilizing an Institutional Joint Replacement database, a descriptive study was carried out using a retrospective cohort of 1233 procedures in 1100 patients between 2012 and 2016. These were followed up for three months to evaluate morbidity and mortality in the postoperative period.
Results
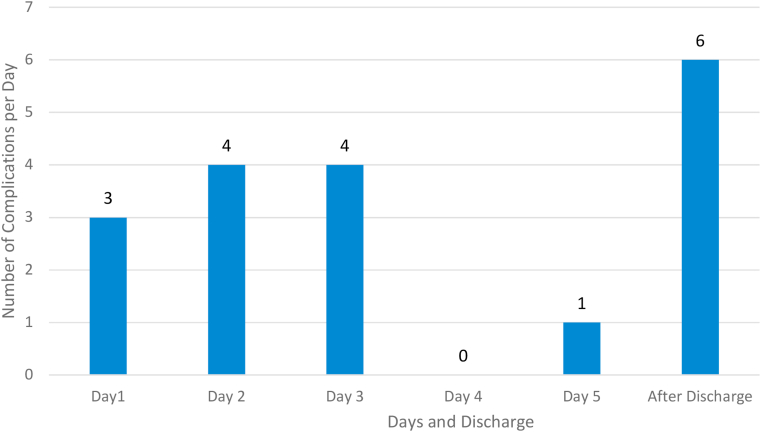
Complications were classified as minor or major (these were defined as any adverse event that can threaten a patient’s life or had the potential to result in readmission). Of the cohort, 18 (1.5%) patient procedures presented one or more major complications. On the first postoperative day 3 major complications occurred (including one death). On the second and third day, 4 major complications were registered each day. On the fourth day after surgery, there were no major complications. On the fifth day 1 major complication was identified. After patient discharge there were 6 major complications reported.
Discussion
The balance between early discharge and out-of-hospital morbidity as well as the frequency of hospital readmission must be the basis to determine whether a patient’s hospital stay should be reduced. According to our results, it seems to be safe to shorten hospital stay in young and healthy patients. Furthermore, only orthopedic teams that have minimal rates of outpatient complications and adhere to high standards of care should consider reducing hospital stay.
Keywords: Early discharge, Postoperative complications, Arthroplasty, Morbidity, Mortality
1. Introduction
Total joint replacement and patient rehabilitation have improved significantly over the years and it is considered nowadays a safe and effective procedure for severe osteoarthritis of the hip or knee.1, 2, 3 Current trends have moved towards minimally invasive procedures and shortened hospital stay with the objective of accelerating patient recovery, this makes relevant to take in account the temporality and characteristics of complications associated with joint replacement after hospital discharge.4,5 In the standard practice following total knee or hip replacement it has been described a hospital stay up to 3 weeks, however, those new trends have led clinical protocols to a regular hospital stay of 2–4 days.6,7 Therefore accelerated discharge has been introduced to care protocols in a widespread manner,6 nevertheless, it is relevant to highlight that this is more a popular trend to shorten in-hospital stay than a standard definition for early discharge.
Even though there is no clear definition of early discharge, some studies have described it as a length of hospital stay between 1 and 3 days.6, 7, 8, 9 In order to give early discharge to patients, thus reducing costs, it is necessary to ensure a low rate of adverse events.3,10, 11, 12, 13, 14, 15 However, complications that may arise after discharge are rarely taken into account2, 3, 4; although major complications and death following these procedures are sporadic,16 some studies suggest that patient readmission is on the rise, it has been reported as frequent as 10% during the first and second month after a joint arthroplasty due to related complications17, 18, 19
Furthermore, a second element to be considered is the previous condition of the patients who undergo total joint arthroplasty. These conditions and associated comorbidities vary among patients and this natural variation could impact complication and re-admission rates.3,4,20,21 A better understanding and consideration of these differences would yield better short term results.
Several studies have approached not only the impact of individual risk factors on length of stay and morbidity or mortality rates but also the timing of appearance of these adverse events, however these studies have yielded contradictory reports.14,22,23 Therefore, it is pivotal to determine the moment when adverse events occur during the early perioperative period and evaluate risk variation produced by each patient’s individual characteristics. If early complications do not increase and can be diagnosed in a timely manner during a reduced hospital stay (one to two days), then outpatient protocols can reduce costs related to this type of procedures without increasing morbidity thus increasing patient satisfaction.24, 25, 26, 27
This study seeks to describe the temporary course of post-operative complications in the early perioperative period of elective hip and knee replacement with an emphasis on major complications that could threaten a patient’s life and lead to readmission if the patient had been, theoretically, subjected to early discharge. Furthermore, it describes the day when intra or extra hospital complications occurred, which were the most common complications and their final outcomes, in order to determine the safest moment for patient discharge.
2. Methods
In order to achieve this study’s objectives, a descriptive quantitative study was constructed using the Institutional Joint Replacement Registry. This Registry keeps demographic data, performance indicators and clinical outcomes of all patients who undergo elective arthroplasties. A cohort description was designed utilizing information that was collected in a prospective manner from patients who underwent primary hip or knee replacement between 2012 and 2016. This database permitted the identification of postoperative patient complications, their characteristics and their temporality. Patients were followed for complications occurring within in-hospital time and then after discharge during the first 12 weeks after surgery.
Although patients were treated by different surgeons, all of them were treated according to the same standardized clinical care protocol, including risk mitigation and screening surgery contraindications. All patients were planned to stay in hospital for three nights, and this length of stay could be modified according to the judgment of the surgeon, based on the clinical progress of the patient. All hip surgeries were carried out using a Posterolateral Mini-Incision approach and all knee arthroplasties were carried out using a midvastus or medial parapatellar approach with the use of a tourniquet. During the postoperative period patients received pharmacological and mechanical prophylaxis in order to avoid venous thromboembolism (VTE) according to NICE guidelines.
2.1. Inclusion criteria
-
1.
Patients that had undergone elective primary hip or knee surgery between 2012 and 2016 with at least three months of post-operative follow-up.
-
2
Patients 18 years or older.
2.2. Exclusion criteria
-
1.
Patients who were programmed for additional surgical procedures.
-
2.
Patients with an incomplete medical record.
Once patients were selected according to the aforementioned criteria, demographic variables and relevant outcomes were extracted from the database for the study.
2.3. Demographic variables
The demographic variables included in this study were: sex, age, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, patient history, type of surgery and hospital stay.
2.4. Study outcomes were
-
1.
Anemia which required transfusions: Defined as the administration of any allogeneic blood component during the post-operative period. In our institutional protocol, blood transfusion was administered when symptoms occurred in the presence of a haemoglobin level below 9 mg/dL.
-
2.
Complications: appearance of a major or minor complication.
-
3.
Days before complications: number of days before the manifestation of a complication (major or minor).
-
4.
In-Hospital Falls: if the patient fell during hospital stay.
-
5.
Damage due to hospital falls: repercussions due to a patient’s fall.
-
6.
Readmission during the following three months: if a patient was readmitted to the hospital or to an emergency service after discharge due to a condition related to the index surgery.
-
7.
Time from surgery until readmission: time before readmission after discharge.
-
8.
In-Hospital mortality: if a patient died after surgery while staying in the hospital.
-
9.
Mortality three months after surgery: Death within three months after discharge.
-
10.
Death in days: Days between surgery and death.
This study used a study carried out by Parvizi et al. in order to define major complications as any adverse event that can threaten a patient’s life.1
As such, major complications according to the Institutional Joint Replacement Registry were classified as:
-
●
Stable or unstable angina
-
●
Pulmonary embolism
-
●
Coronary event
-
●
Renal failure
-
●
Death
In addition to these complications, anemia which required a blood transfusion was included since our study group considered it as a relevant outcome for patients.
The frequency and the moment when each complication occurred were measured and calculated in proportions (over the total number of minor or major complications). Each type of complication, days before onset, age and patient age were also quantified and then converted into proportions and separated according to minor or major complications. Demographic and pathological reports of the patients were also described. Subsequently, the frequency of complications in the following five days after surgery were described, these results were then discriminated for outcomes following any type of complication and major complications. Moreover, a hypothetical threshold was adjusted for hospital discharge and reduced to three and two days. The purpose of this calculation was to estimate the proportion of complications that would occur after discharge if the number of days before the patient left the hospital were progressively reduced and therefore estimate a hypothetical readmission rate for each day.
This study was evaluated by the institutional ethics committee and due to its retrospective characteristics (only past medical records were included in the study); it was considered a low risk investigation and did not require a consent form. Patient data and clinical history was handled under strict confidentiality and was only reviewed by the research team.
3. Results
The Institutional Joint Replacement Registry included 1332 procedures carried out during the study period, and after applying inclusion and exclusion criteria a total of 1233 procedures in 1100 patients were reviewed. The overall loss of records for any reason accounts for 7.4%. Most of the patients of the study were women (70.3%) and hip arthroplasty was the most common type of joint replacement surgery (54%). Average age and BMI were 67.8 ( ±10.6) and 24.1 ( ±3) respectively (Table 1). On average 61.2% of patients were classified as ASA 2 by anesthesiologists and average hospital stay was of 4.1 days ( ±1.2). Previous patient history is described on Table 2. After reviewing all procedures, 215 patients (17.4%) had at least one complication during their stay. A total of 307 complications occurred, of those 289 (94.1%) were classified as minor and 18 (5.9%) were classified as major according to the studies aforementioned classification criteria.
Table 1.
Patient demographic data.
| Male | 327 (29.7%) |
|---|---|
| Female | 773 (70.3%) |
| Average Age | 67.8 years (SD±10.6) |
| Average BMI | 24.1 (SD±3) |
| ASA 1 | 4.1% |
| ASA 2 | 61.2% |
| ASA 3 | 34.6% |
| ASA 4 | 0.1% |
| Hospital Stay | 4.1 days (SD±1.2) |
| Knee Replacement | 567 (46%) |
| Hip Replacement | 666 (54%) |
Table 2.
Electronic patient records: History of comorbidities and definition.
| History | N | Definition |
|---|---|---|
| Metabolic diseases | 911 (32.1%) | Hypothyroidism, dyslipidemia, osteoporosis, hyperuricemia and/or diabetes |
| Hypertension | 645 (22.7%) | Systolic pressure > 140 mmHg and diastolic pressure > 90 mmHg |
| Gastrointestinal disease | 282 (9.9%) | Inflammatory bowel disease, bleeding of the digestive tract, polyps and/or diverticulitis |
| Past Cardiovascular Event | 162 (5.7%) | Miocardial infarction, stenosis and/or valvular insufficiencies |
| Neoplasia | 142 (5%) | All breast cancers, prostate and/or benign tumors except prostatic hyperplasia |
| Musculoskeletal disorders | 119 (4.2%) | Osteoarthritis, meniscus injury and/or previous fractures |
| Pulmonary disease | 117 (4.1%) | Chronic Obstructive Pulmonary disease (COPD) and/or pulmonary hypertension |
| Rheumatologic diseases | 116 (4.1%) | Arthritis, lupus, sclerosis and/or Sjogren’s syndrome |
| Genitourinary diseases | 88 (3.1%) | Chronic kidney disease, urinary tract infections and/or incontinence |
| Psychiatric disorders | 70 (2.5%) | Depression, anxiety and/or bipolar disorder |
| Neurological disorders | 68 (2.4%) | Peripheral neuropathies |
| Thrombo-embolic disease | 59 (2.1%) | Stroke, Deep Vein Thrombosis or Pulmonary embolism |
| Vascular disorders | 22 (0.8%) | Venous insufficiency |
| Hematologic diseases | 20 (0.7%) | Deficiency of coagulation factors, Von Willebrand disease, hypercoagulability and/or blood dyscrasias |
| Immunological disease | 2 (0.1%) | Liver transplant and/or immunosuppressed patients |
| Avascular necrosis | 13 (0.5%) | Avascular necrosis of the femoral head and/or Perthes disease |
| Total | 2836 (100%) | Total |
3.1. Minor complications
Of the 289 minor complications, the most common was anemia that required a transfusion with a total of 112 cases (38.8%). The following five most common minor complications were: 15 (5.2%) gastrointestinal alterations, 14 (4.8%) cases of atelectasis, 13 (4.5%) patients had some form of delirium, and 12 (4.2%) cases of electrolyte imbalance and respiratory altercations were found. Other minor complications can be found on Table 3. There were 3 cases of patient falls (1%), but none had any repercussions on the patient and occurred after discharge. Although falls are part of international security goals determined by Joint Commission International (which has certified both the hospital and service as centers of excellence), these were not taken into consideration as a major complication for this study.
Table 3.
Minor complications per day and total∗.
| Days of presentation Minor complication or events |
1 | 2 | 3 | 4 | 5 | After discharge | Total |
|---|---|---|---|---|---|---|---|
| Symptomatic anemia | 31 (10.7%) | 46 (15.9%) | 23 (8%) | 10 (3.5%) | 1 (0.3%) | 1 (0.3%) | 112 (38.75%) |
| Gastrointestinal disorders | 3 (1%) | 4 (1.4%) | 2 (0.7%) | 1 (0.3%) | 1 (0.3%) | 4 (1.4%) | 15 (5.19%) |
| Atelectasis | 1 (0.3%) | 2 (0.7%) | 0 (0%) | 6 (2.1%) | 4 (1.4%) | 1 (0.3%) | 14 (4.84%) |
| Delirium | 6 (2.1%) | 6 (2.1%) | 0 (0%) | 1 (0.3%) | 0 (0%) | 0 (0%) | 13 (4.5%) |
| Respiratory disorders | 2 (0.7%) | 1 (0.3%) | 0 (0%) | 5 (1.7%) | 1 (0.3%) | 3 (1%) | 12 (4.15%) |
| Symptomatic electrolyte imbalance | 5 (1.7%) | 2 (0.7%) | 1 (0.3%) | 2 (0.7%) | 1 (0.3%) | 1 (0.3%) | 12 (4.15%) |
| Surgical site infection | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 8 (2.8%) | 8 (2.77%) |
| Urinary infection | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.3%) | 1 (0.3%) | 6 (2.1%) | 8 (2.77%) |
| Hypotension | 4 (1.4%) | 4 (1.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 8 (2.77%) |
| Other complicationsa | 14 (4.8%) | 17 (5.9%) | 11 (3.8%) | 5 (1.7%) | 5 (1.7%) | 35 (12.1) | 87 (30.10%) |
| General | 66 (22.8%) | 82 (28.4%) | 37 (12.8%) | 31 (10.7%) | 14 (4.8%) | 59 (20.4%) | 289 (100%) |
∗Percentages are calculated over the total number of minor complications.
Chest pain, prothesis luxation, associated dermatological disorders, pneumonia, alterations associated with the management of pain and anesthesia, fever, lipotimia or syncope due to orthostatism, behavior disturbances, arrhythmia, fall, uncontrolled Postoperative pain, hematoma, other surgical procedures, stroke, renal colic, bleeding that required surgical intervention, neurological disorders, uncontrolled hypertension, seizures, epistaxis, delay in rehabilitation goals, deep vein thrombosis, vertebral fracture, pleural effusion, anxiety, cellulitis, decompensated chronic obstructive pulmonary disease, pulmonary hypertension, femoral neuropraxia by catheter, rhinopharyngitis, gastrointestinal bleeding, thrombocytopenia and femoral catheter infection.
3.2. Major complications
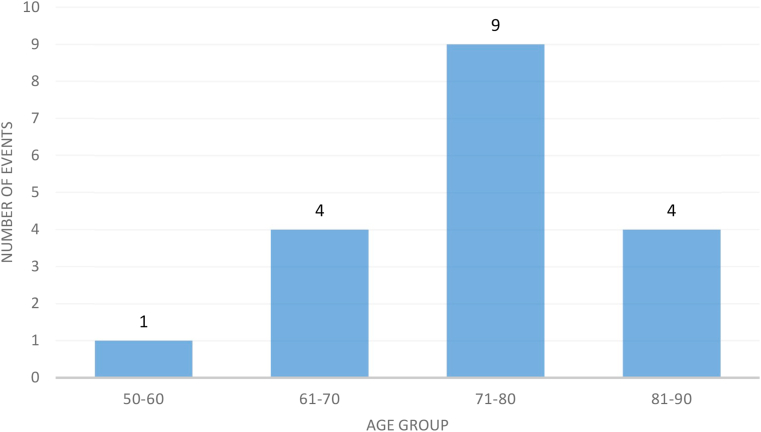
A total of 18 (1.5%) patients in 1233 procedures presented a major complication, these were only observed in patients older than 50 (Table 4) or in patients classified as ASA 2 or 3 (Table 5). In regards to age, 13 (72.2%) patients were older than 70 and the rest were between 70 and 50. Occurrence of complications for each age group is shown in Graph 1. As for ASA classification, 6 (33.3%) patients were classified as ASA 2 and 12 (66.7%) were classified as ASA 3. Coronary events were the most common major complication with 9 (50%) incidents followed by pulmonary thromboembolism and death with 5 (27.8%) and 3 (16.7%) events respectively (Table 6). Regarding patient death, one died on day one after surgery following a stroke and the other two deaths came 66 and 90 days after discharge. However, their medical record does not report cause of death.
Table 4.
Age range and day of major complication onset.
| Age | 1 | 2 | 3 | 4 | 5 | After discharge | Total |
|---|---|---|---|---|---|---|---|
| 50–70 | 1 (5.6%) | 2 (11.1%) | 1 (5.6%) | 0 (0%) | 0 (0%) | 1 (5.6% | 5 (27.8%) |
| >70 | 2 (11.1%) | 2 (11.1%) | 3 (16.7%) | 0 (0%) | 1 (5.6%) | 5 (27.8%) | 13 (72.2%) |
| General | 3 (16.7%) | 4 (22.2%) | 4 (22.2%) | 0 (0%) | 1 (5.6%) | 6 (33.3%) | 18 (100%) |
Table 5.
ASA classification and day of major complication onset.
| ASA | 1 | 2 | 3 | 4 | 5 | After Discharge | Total |
|---|---|---|---|---|---|---|---|
| 1 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| 2 | 0 (0%) | 2 (11.1%) | 1 (5.6%) | 0 (0%) | 1 (5.6%) | 2 (11.1%) | 6 (33.3%) |
| 3 | 3 (16.7%) | 2 (11.1%) | 3 (16.7%) | 0 (0%) | 0 (0%) | 4 (22.2%) | 12 (66.7%) |
| 4 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
Graph 1.
Number of major complications per age group.
Table 6.
Major complication incidence and day of onset.
| Complication | 1 | 2 | 3 | 4 | 5 | After Discharge | Total |
|---|---|---|---|---|---|---|---|
| Coronary Event | 2 (11.1%) | 3 (16.7%) | 2 (11.1%) | 0 (0%) | 0 (0%) | 2 (11.1%) | 9 (50%) |
| Death | 1 (5.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (11.1%) | 3 (16.7%) |
| Pulmonary Embolism | 0 (0%) | 0 (0%) | 2 (11.1%) | 0 (0%) | 1 (5.6%) | 2 (11.1%) | 5 (27.8%) |
| Angina | 0 (0%) | 1 (5.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (5.6%) |
| General | 3 (0%) | 4 (22.2%) | 4 (22.2%) | 0 (0%) | 1 (5.6%) | 6 (33.3%) | 18 (100%) |
∗Percentages are calculated over the total number of major complications.
There were a total of 4 major complications on the second day and third day after surgery. On the fourth day after surgery however, there were no major complications. There was one major complication (a case of pulmonary embolism) on the fifth day; after discharge there were 6 major complications (Graph 2).
Graph 2.
Number of major complications per day.
The most common causes for readmission were infection of the surgical site, urinary tract infection and prosthesis dislocation with 8 (2.8%), 8 (2.8%) and 6 (1.9%) cases respectively. Due to the fact that some complications are related to hospital stay, complications such as delirium and atelectasis do not necessarily correspond to a cause for readmission. As such, to estimate a theoretical readmission rate if patients had been subjected to an early discharge protocol, the researchers determined that major complications would be the only complications capable of leading to a theoretical patient readmission.
Consequently, if hospital stay was reduced to 3 days for all patients, 45 minor complications and 1 major complication would have occurred after discharge. This would raise the readmission rate associated to joint replacement to 5%. If hospital stay was reduced to 2 days, 82 minor complications and 5 major complications would occur after discharge and therefore the associated surgical readmission rate would increase to 6%.
4. Discussion
In order to lower costs and due to the need to mitigate high surgical volumes, and the desire to be more efficient, hospitals and surgeons have started to reduce hospital stay for patients. This, in theory, should also reduce risks and increase the cost-effectiveness of procedures as well as patient satisfaction4, 10, 13, 27.
Previous studies have used similar methodologies as ours1,2,5,16,28,29 utilizing a cohort of patients with an extended follow-up registry, and although our population demographics are similar (Table 1), complications were only identified in the first five days to determine the safety of surgery with a reduced hospital stay modality.1,2,5,19,28,29
Furthermore, few studies use an institutional patient registry that spans several years as was done in this study or evaluate the immediate complications following surgery and characterize their temporal and individual patient demographics. For example, there are reports that utilize ten29 or six1 years as a study period, however these were written some time ago and may not be currently suitable or applicable due to surgical advances in reconstructive surgery. Other studies focus on a socioeconomic perspective which emphasizes on readmission for insurance companies and/or governmental policy strategies, this was not taken into account for this study.10,19,27 Previous studies also coincide with our study in patient sex and type of surgery distribution, being hip replacement the most common procedure and women the most common gender.5,16,25
Despite the fact that over the past century hospital stay has been reduced, rates of readmission have increased.25,27 Concomitantly, patients who undergo joint replacement surgery are becoming more complex in nature and pressure from healthcare stakeholders to give them early discharge has exacerbated the debate.25,27 This pressure is due to the fact that short hospital stays lower readmission rates on the long run19 due to the fact that patients with a hospital stay longer than five days are more likely to be readmitted.2 However, these do not take into account the individual risk factors for morbidity and mortality patients may be exposed to in the first five days after surgery. For instance, pulmonary embolism was the second most common major complication in our study (29.4%) and it has been proven that this complication is more common in the first seven days after surgery.30,31 Similarly, there is evidence that shows that the risk for cardiac and pulmonary disease after joint replacement must be adjusted according to each patient in order to reduce the risk of complications.29 Other factors such as sex, ASA classification and type of surgery have been associated with a higher risk of morbimortality in the postoperative period.5,19 However, it has not been possible to demonstrate the capacity of solely depending on a patient’s medical history to predict the onset of complications,5 as in the case of our study. According to our results, it seems to be safe to shorten hospital stay in young and healthy individuals. It is relevant to highlight the low frequency of complications in ASA 4 patients, this could be the result of limited sample size (2 patients, 0.1%) for this particular group in our study.
Given the low incidence of complications in ASA 1 and 2 groups, this study supports the need to continue with individual patient evaluation and the use of prophylactic measures to diminish the risk of morbidity and mortality.14,16,22,23,32 It also supports optimizing patient care through risk factor individualization (or utilizing a case-by-case approach when determining early discharge) and utilizing readmission rates as a quality benchmark.22 Although formal risk stratification protocols for patients are necessary and useful in order to determine early discharge and the risk for post discharge complications14 only experienced orthopedic teams with high standards of quality and safety should aggressively reduce hospital stay. These types of strategic hospital initiatives should be continuously monitored with performance indicators and metrics. This way, hospitals and their surgical teams can study their individual patient populations (as well as continuously improve their performance) in order to determine the best day for early discharge. Individual studies carried out by Parvizi et al. and Pulido et al. describe a rise in the increase for mortality during the first five postoperative days5 and report similar results as ours such as: a significant increase of morbimortality risk because of major complications in the first two days after surgery, mostly related to coronary events and pulmonary embolism.1,5
In regards to the onset of the aforementioned complications, the first and second day are the days when there were more cases of anemia that required transfusion (77 cases/26.6%), delirium (12 cases/4.2%), and gastrointestinal altercations and electrolyte imbalances (7 cases respectively/2.4%) occurred. On the other hand, atelectasis and respiratory altercations peaked on the fourth day. Surgeons and their teams must be aware of patients with risk factors that could lead to a coronary event due to their frequency on those four days during the first three postoperative days in 38.9% of all cases. Furthermore, pulmonary embolisms occurred between the third and fifth day and after discharge in 16.7% of all cases. The incidence of other major complications can be seen in Table 6. Despite stratifying and tabulating patients in whom a complication occurred; there was no way to predict the moment of onset of major complications. This lack of predictability concurs with previous studies.1 Prevention of these major complications will be subject of further research since it is beyond the scope of this study.
It is expected that from 2014 to 2030 primary total hip arthroplasties will increase by 71% and total knee arthroplasties will increase by 85% in the United States (other countries have also projected an increase in the number of surgeries).21,22 Keeping this demographic trend and the data that was recollected in mind, hospitals must start to develop risk stratification and early discharge protocols that reflect their standards of care and lightens the burden of higher volumes of surgeries. In order to modify this, readmission and complication rates can be used as benchmarking tools for early discharge in line with a case-by-case assessment of each individual patient based on their surgeons criteria.3 Adequate strategic profiling of patients based on correctly structured protocols, could help avoid early complications and associated pitfalls and lead to increased satisfaction, decreased costs and improved outcomes.13,14 The study’s results may be ideal in the sense that the hip and knee replacement program at the hospital is certified as a center of excellence and thereby not reflect complication/readmission rates in many hospitals. Other institutions may have higher complication rates or an inadequate system to measure performance indicators and supervise surgical performance. Although this may be a limitation, it also highlights the need for continuous measurement of readmission and complication rates, especially before adopting a protocol such as early discharge that may compromise patient-centered care. A second limitation is the fact that hips and knees were considered in a pooled analysis, therefore the differences between procedures could have impacted our results. Another potential limitation of this study is the fact that data were collected through an institutional arthroplasty register which is not designed for this particular study, however the impact of this shortcoming has been minimized including only the outcomes that were previously recorded in a prospective manner. It is still possible that some relevant outcomes are not included since they were not recorded prospectively. Finally, it is important to highlight that these results cannot be extrapolated to patients in whom an arthroplasty is performed due to a proximal femoral fracture since this study only included elective procedures.
By studying and adequately recording data in registries, hospitals can achieve best practices in care by avoiding adverse events, managing patient needs/expectations and effectively managing resources while optimizing patient and surgical team outcomes after total hip or knee arthroplasty.
5. Conclusions
In conclusion, with these results, surgeons (that have adequate risk stratification tools, performance indicators and high standards of care at their disposal) may consider shortening hospital stay to 3 days due to the fact that although joint replacement surgeries are safe, there is still a risk for major complications in the postoperative period that can be overlooked by aggressively reducing hospital stay. Therefore, the balance between early discharge and extra-hospital morbidity and mortality, as well as the frequency of readmission must be the cornerstone and a quality benchmark for decision making when it comes to reducing hospital stay. According to these results 3-days hospital stay (2 nights) could be safe as a general rule in patients younger than 70 years old without major comorbidities. However, as previously mentioned shortening this stay demands strict patient selection, individual risk factor assessment and a carefully structured/supervised early discharge protocol.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Local IRB did not request the consent form patients as per the study design.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
Camilo Gutiérrez Rodríguez MD: declares that he has no conflict of interest.
Maria Alejandra Asmar Murgas MD: declares that she has no conflict of interest.
Abelardo Camacho Uribe MD: declares that he has no conflict of interest.
Valeria Barrios MD: declares that she has no conflict of interest.
Guillermo Bonilla León MD: has participated as paid speaker for Boehringer-Ingelheim, Pfizer, Sanofi and DePuy Synthes (Orthopedics); has received other financial support from DePuy Synthes (Orthopedics), has received research support from a company or supplier as a Principal researcher for Grunenthal and Johnson & Johnson, outside this work.
Adolfo Llinás Volpe MD: has received royalties from Innomed, Novamed and 3 M; has participated as paid speaker for Zimmer, Shire, Novonordisk, Novartis, Johnson & Johnson, Medtronic and Procaps; has participated as paid consultant for Zimmer and Medtronic, outside this work.
Contributor Information
Camilo Gutiérrez Rodríguez, Email: gutierrezcamilo757@gmail.com.
María Alejandra Asmar Murgas, Email: ma.asmar293@uniandes.edu.co.
Abelardo Camacho Uribe, Email: abecamachouribe@gmail.com.
Valeria Barrios Diaz, Email: valeria.barrios2311@gmail.com.
Guillermo Bonilla León, Email: guillermobonilla.md@gmail.com.
Adolfo Llinás Volpe, Email: adolfo.llinas@fsfb.org.co.
References
- 1.Pulido L., Parvizi J., Macgibeny M. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23(6 Suppl 1):139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 2.Schairer W.W., Sing D.C., Vail T.P., Bozic K.J. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):464–470. doi: 10.1007/s11999-013-3121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tay K., Tang A., Fary C., Patten S., Steele R., Steiger R.D. The effect of surgical approach on early complications of total hip arthoplasty. Arthroplasty. 2019;1(1) doi: 10.1186/s42836-019-0008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Courtney P.M., Boniello A.J., Berger R.A. Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplasty. 2017;32(5):1426–1430. doi: 10.1016/j.arth.2016.11.055. [DOI] [PubMed] [Google Scholar]
- 5.Parvizi J., Mui A., Purtill J.J., Sharkey P.F., Hozack W.J., Rothman R.H. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89(1):27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 6.Marsh J., Somerville L., Howard J.L., Lanting B.A. Significant cost savings and similar patient outcomes associated with early discharge following total knee arthroplasty. Can J Surg. 2019;62(1):20–24. doi: 10.1503/cjs.002118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metcalfe S., Ji H., Molodianovitsh K., Sidhom P., Faye L., Webster G. Canadian Institute for Health Information; 2015. Hip and Knee Replacements in Canada: Canadian Joint Replacement Registry 2015 Annual Report.https://secure.cihi.ca/free_products/CJRR_2015_Annual_Report_EN.pdf Accessed 2020. [Google Scholar]
- 8.Kraus K.R., Buller L.T., Caccavallo P.P., Ziemba-Davis M., Meneghini R.M. Is there benefit in keeping early discharge patients overnight after total joint arthroplasty? [published online ahead of print, 2020 jul 16] J Arthroplasty. 2020;S0883–5403(20):30778–30786. doi: 10.1016/j.arth.2020.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Otero J.E., Gholson J.J., Pugely A.J., Gao Y., Bedard N.A., Callaghan J.J. Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplasty. 2016;31(12):2714–2725. doi: 10.1016/j.arth.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 10.Larsen K., Hansen T.B., Thomsen P.B., Christiansen T., Søballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91(4):761–772. doi: 10.2106/JBJS.G.01472. [DOI] [PubMed] [Google Scholar]
- 11.O’ Reilly M., Mohamed K., Foy D., Sheehan E. Educational impact of joint replacement school for patients undergoing total hip and knee arthroplasty: a prospective cohort study. Int Orthop. 2018;42(12):2745–2754. doi: 10.1007/s00264-018-4039-z. [DOI] [PubMed] [Google Scholar]
- 12.Paredes O., Ñuñez R., Klaber I. Successful initial experience with a novel outpatient total hip arthroplasty program in a public health system in Chile. Int Orthop. 2018;42(8):1783–1787. doi: 10.1007/s00264-018-3870-6. [DOI] [PubMed] [Google Scholar]
- 13.Mayer M.A., Pirruccio K., Sloan M., Sheth N.P. Discharge home is associated with decreased early complications following primary total joint arthroplasty. J Arthroplasty. 2019;34(11):2586–2593. doi: 10.1016/j.arth.2019.06.049. [DOI] [PubMed] [Google Scholar]
- 14.Yao D.H., Keswani A., Shah C.K., Sher A., Koenig K.M., Moucha C.S. Home discharge after primary elective total joint arthroplasty: postdischarge complication timing and risk factor Analysis. J Arthroplasty. 2017;32(2):375–380. doi: 10.1016/j.arth.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Masaracchio M., Hanney W.J., Liu X., Kolber M., Kirker K. Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: a systematic review with meta-analysis. PLoS One. 2017;12(6) doi: 10.1371/journal.pone.0178295. 2017 Jun 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunt L.P., Ben-Shlomo Y., Clark E.M. 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet. 2013;382(9898):1097–1104. doi: 10.1016/S0140-6736(13)61749-3. [DOI] [PubMed] [Google Scholar]
- 17.Kee J.R., Edwards P.K., Barnes C.L., Foster S.E., Mears S.C. After-hours calls in a joint replacement practice. J Arthroplasty. 2019;34(7):1303–1306. doi: 10.1016/j.arth.2019.02.067. [DOI] [PubMed] [Google Scholar]
- 18.Nedza S.M., Fry D.E., DesHarnais S., Spencer E., Yep P. Emergency department visits following joint replacement surgery in an era of mandatory bundled payments. Acad Emerg Med. 2017;24(2):236–245. doi: 10.1111/acem.13080. [DOI] [PubMed] [Google Scholar]
- 19.Zmistowski B., Restrepo C., Hess J., Adibi D., Cangoz S., Parvizi J. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013;95(20):1869–1876. doi: 10.2106/JBJS.L.00679. [DOI] [PubMed] [Google Scholar]
- 20.Tulic G., Dubljanin-Raspopovic E., Tomanovic-Vujadinovic S., Sopta J., Todorovic A., Manojlovic R. Prolonged pre-operative hospital stay as a predictive factor for early outcomes and mortality after geriatric hip fracture surgery: a single institution open prospective cohort study. Int Orthop. 2018;42(1):25–31. doi: 10.1007/s00264-017-3643-7. [DOI] [PubMed] [Google Scholar]
- 21.Roger C., Debuyzer E., Dehl M. Factors associated with hospital stay length, discharge destination, and 30-day readmission rate after primary hip or knee arthroplasty: retrospective Cohort Study. Orthop Traumatol Surg Res. 2019;105(5):949–955. doi: 10.1016/j.otsr.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Ricciardi B.F., Oi K.K., Daines S.B., Lee Y.Y., Joseph A.D., Westrich G.H. Patient and perioperative variables affecting 30-day readmission for surgical complications after hip and knee arthroplasties: a matched cohort study. J Arthroplasty. 2017;32(4):1074–1079. doi: 10.1016/j.arth.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 23.Slullitel P.A., Estefan M., Ramírez-Serrudo W.M. Re-admissions treble the risk of late mortality after primary total hip arthroplasty. Int Orthop. 2018;42(9):2015–2023. doi: 10.1007/s00264-018-3876-0. [DOI] [PubMed] [Google Scholar]
- 24.Radzak K.N., Wages J.J., Hall K.E., Nakasone C.K. Rate of transfusions after total knee arthroplasty in patients receiving lovenox or high-dose aspirin. J Arthroplasty. 2016;31(11):2447–2451. doi: 10.1016/j.arth.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 25.Tarity T.D., Swall M.M. Current trends in discharge disposition and post-discharge care after total joint arthroplasty. Curr Rev Musculoskelet Med. 2017;10(3):397–403. doi: 10.1007/s12178-017-9422-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grosso M.J., Neuwirth A.L., Boddapati V., Shah R.P., Cooper H.J., Geller J.A. Decreasing length of hospital stay and postoperative complications after primary total hip arthroplasty: a decade analysis from 2006 to 2016. J Arthroplasty. 2019;34(3):422–425. doi: 10.1016/j.arth.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 27.Cram P., Lu X., Kaboli P.J. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991-2008. J Am Med Assoc. 2011;305(15):1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Vries L.M., Sturkenboom M.C., Verhaar J.A., Kingma J.H., Stricker B.H. Complications after hip arthroplasty and the association with hospital procedure volume. Acta Orthop. 2011;82(5):545–552. doi: 10.3109/17453674.2011.618907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mantilla C.B., Horlocker T.T., Schroeder D.R., Berry D.J., Brown D.L. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty [published correction appears in Anesthesiology 2002 Aug. Anesthesiology. 2002;96(5):1140–1146. doi: 10.1097/00000542-200205000-00017. 97(2):531] [DOI] [PubMed] [Google Scholar]
- 30.Sweetland S., Green J., Liu B. Duration and Magnitude of the Postoperative Risk of Venous Thromboembolism in Middle Aged Women: Prospective Cohort Study [published Correction Appears in BMJ. BMJ. 2010;vol. 340:c417. doi: 10.1136/bmj.b4583. 2009;339:b4583. 2009 Dec 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Finch D.J., Martin B.I., Franklin P.D., Magder L.S., Pellegrini V.D., Jr. PEPPER Investigators. Patient-reported outcomes following total hip arthroplasty: a multicenter comparison based on surgical approaches. J Arthroplasty. 2020;35(4):1029–1035. doi: 10.1016/j.arth.2019.10.017. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lizaur-Utrilla A., Gonzalez-Navarro B., Vizcaya-Moreno M.F., Miralles Muñoz F.A., Gonzalez-Parreño S., Lopez-Prats F.A. Reasons for delaying surgery following hip fractures and its impact on one year mortality. Int Orthop. 2019;43(2):441–448. doi: 10.1007/s00264-018-3936-5. [DOI] [PubMed] [Google Scholar]