Abstract
The choice of anaesthetic in shoulder surgery is an evolving field of research which has important implications for patient outcomes. We have performed a prospective study to assess the usability of an interscalene brachial plexus block (ISBPB) with sedation as the primary anaesthetic and analgesic for arthroscopic shoulder surgery. Our study assessed the requirements of analgesia peri-operatively and post operatively and found that patients had no requirement (n = 30) and minimal requirements with a low pain score (visual analogue score; mean 2.4, range 2–5) respectively. We also found that patients spent a short amount of time in recovery (31 min mean, range 21–48 min) and were able to be discharged on the same day. Our findings suggest that ISBPB with sedation is a viable option in arthroscopic shoulder surgery for a variety of procedures with positive effects for patient outcomes and mobility.
Keywords: Interscalene, Brachial, Plexus, Block, Arthroscopy, Arthroscopic, Shoulder, Surgery, Anaesthesia, Analgesia, Pain
1. Introduction
Shoulder surgery is an evolving field of orthopaedics which is proving to be increasingly beneficial to a wide spectrum of patients from young to old. As research advances in this field the possibilities of improving quality of life, function and pain for patients with shoulder pathology increases. Arthroscopic and minimally invasive surgical techniques are becoming more common and there is evidence which show benefit in hospital stay6 and functional outcome2 in adopting these methods. A common burden of shoulder surgery is severe post-operative pain and prolonged recovery time associated with general anaesthesia. It is pertinent that the anaesthetic technique should be optimised for shoulder surgery to enable the best possible patient outcomes for all patients undergoing a shoulder procedure.
General anaesthesia is currently the mainstay for patients receiving shoulder surgery. There are numerous negative implications associated with this including deep vein thrombosis, pulmonary embolism, pneumonia, and delirium alongside others.8,9 During the covid-19 pandemic, having a general anaesthesia has been associated with other negative implications as an aerosol generating procedure (AGP), and avoided when possible. As AGPs are associated with risk of infection, added precautions are routinely being taken during intubation and extubation, resulting in prolonged turn-around times between cases and increased risk to patients and staff.5
Due to this situation, anaesthetists have been looking increasingly at alternative methods of perioperative anaesthesia. A few examples of alternative perioperative anaesthesia include; abdominal and lower limb procedures being given a spinal anaesthesia with sedation; hand procedures being performed under Wide Awake Local Anaesthesia No Tourniquet (WALANT) and shoulder procedures being given an Interscalene Brachial Plexus Block with sedation (ISBPB). These modalities have historically been used to manage post-operative pain and not as the main anaesthetic for the procedure.
ISBPB is best performed with ultrasound guidance. The patient is prepared in supine position and the head turned away from the side receiving the block. The groove between scalenus anterior and medius is identified above the clavicle at the level of C6 as the brachial plexus is superficial at this level. Local anaesthetic is initially inserted followed by a nerve block needle with the anaesthetic of choice for the block. A minimum of ten minutes is given to assess the success of the block using motor and sensory examination.4 A catheter may or may not be inserted for further supplementation of anaesthetic depending on operative requirements.
A practitioner with experience in ISBPB should deliver the anaesthetic. Although extremely uncommon, there have been historically reported cases of anaesthetic being inserted into the spinal cord leading to permanent cervical spinal cord damage.1 There are also potential unwanted prolonged anaesthetic effects including respiratory complications in the form of phrenic nerve paralysis.7 For this reason, it is generally ill advised to perform a bilateral ISBPB and caution should be advised in patients with existing respiratory illness.
The objective of this paper is to assess whether interscalene block anaesthesia is a viable anaesthetic and analgesic in arthroscopic shoulder surgery. We will look at several outcomes to see whether ISBPB can be routinely used as the main anaesthetic in an awake patient (Awake Surgery) and whether a general anaesthetic can be avoided altogether. Our secondary aim is to assess how ISBPB affects post-operative pain and its management. We hypothesise that ISBPB has significant potential benefits in arthroscopic shoulder surgery both intraoperatively and postoperatively. Whilst the data collected was prior to the coronavirus pandemic, it has greater relevance now.
2. Methods
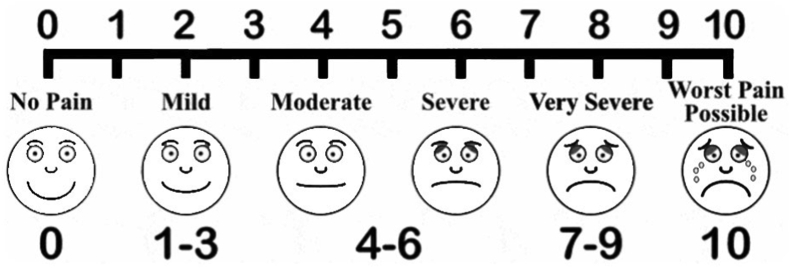
This was a prospective cohort study. We collected data on 30 consecutive patients whom underwent various arthroscopic procedures by the same orthopaedic surgeon over a period of 8 months in 2018. All patients had a full pre-assessment clinic to optimise their medical condition. The inclusion criteria were patients undergoing any arthroscopic shoulder surgery with ISBPB, concurrent sedation in the beech chair position. We did not exclude any patients if they met the inclusion criteria. The blocks were performed by an anaesthetist with ultrasound guidance. A mixture of 10 ml 0.5% chirocaine with 10 ml 2% lignocaine were prepared, of which 15–17 ml was administered. No catheter for further supplementation was inserted nor required. All patients received sedation in the form of midazolam or propofol. Our primary outcome was intra-operative and post-operative analgesic requirements for the duration of hospital stay. Our secondary outcomes were post-operative pain score on the visual analogue scale (Fig. 1) recorded prior to discharge from the hospital, time spent in recovery and operative times. For our purposes, time spent in recovery is the duration the patient received 1 to 1 nursing in the recovery bay after transfer from the operating bed to their inpatient bed and prior to transfer to the ward. Operative time is the time recorded after the WHO time-out checklist is completed to completion of skin closure to the arthroscopic ports. A pain score above 5 is against discharge from hospital criteria.
Fig. 1.
The visual analogue scale.
3. Results
Data was collected from 30 patients over a period of 8 months. The age range of the patients was 28–74 years, with 12 being males and 18 females. The procedures undertaken are listed in Table 1. The mean operative time was 38 min (range, 28–56 min). Mean time spent in recovery was 31 min (range, 21–48 min). The mean VAS score in recovery being 2.4 (range, 2–5). All patients were discharged on the same day with a length of stay ranging between 3 and 8 h. No further intra-operative analgesia was administered. No patients were abandoned to a general anaesthetic. During the post-operative period in hospital 14 patients required 1 dose of 1 g oral paracetamol, 12 required 1 dose of 400 mg ibuprofen and 6 required 1 dose of morphine administration with a mean of four milligrams utilised (range 2–10 mg).
Table 1.
Arthroscopic procedures undertaken using ISBPB with sedation.
| Rotator cuff repairs | 12 |
| Subacromial decompression with acromio-clavicular joint excision | 10 |
| Labral repairs | 4 |
| Calcific tendoinitis debridement | 4 |
4. Discussion
Our principle finding is that ISBPB with sedation is effective as an analgesic and anaesthetic for a range of arthroscopic shoulder procedures without the need for a general anaesthetic. Our patients benefitted from a low pain score, minimal requirements of post-operative analgesics and no usage of intra-operative opioids. Transfer from recovery to the ward was quicker and all of our patients were discharged on the same day as their procedure. This is an important finding in arthroscopic shoulder surgery given the historically poor immediate post-operative pain management.7
During the covid-19 pandemic, hospital theatres are burdened by AGP wait-times, deep cleaning and delayed theatre efficiency. ISBPB with sedations offers an alternative solution in optimising theatre flow in this field of surgery. This study has confirmed the use of ISBPB as the sole anaesthetic and analgesic for arthroscopic shoulder procedures and paves the way for its future use. Many patients routinely undergoing shoulder surgery are offered ISBPB prior to induction for a general anaesthetic as post-operative pain management. These patients may benefit significantly by being able to forego the general anaesthetic altogether.
Our study is limited by sample size and it would be pertinent to perform a larger scale study on this topic. It is also limited by being a single surgeon consecutive series in one institution with no control group and so our results may have been affected by selection bias. We have not evaluated long-term adverse effects of ISBPB in this patient cohort however no acute adverse effects were noted. Whilst we did not encounter an unsuccessful block, contingency plans should be made for if this were to occur. This should be considered on an individual basis and would likely require conversion to a general anaesthetic.
There is the potential that patients may have anxious feelings towards having their procedure whilst awake. We recommend this is addressed through patient education and information-giving with an emphasis on the benefits of using ISBPB as shown by our study. It would be pertinent to explain that the patient will receive sedation and that the procedure will not continue if they have any sensation of pain in the operating site at any point.
Our study lays the groundwork for more extensive research in the use of ISBPB with sedation as an alternative to general anaesthesia and can pave the way for numerous potential benefits to hospitals and patients willing to use this technique for routine elective patients. Our study supports the findings of previous research showing effective post-operative analgesic effects.3
We have shown that ISBPB can be used as the main intra-operative anaesthetic for arthroscopic shoulder surgery. Whilst, the beneficial role of ISBPB has been demonstrated by this study, it remains part of a multi-modal approach to peri-operative anaesthesia. Future research could confirm the usability in utilising this method in non-arthroscopic shoulder procedures so more patients could benefit from the trend towards Awake Surgery.
5. Conclusion
This study provides evidence that ISBPB with sedation is an effective tool as an anaesthetic and analgesic for patients requiring a variety of arthroscopic shoulder procedures. These patients benefitted from no intra-operative analgesia requirements, no prolongation of operative time, low pain scores post operatively, minimal time spent in recovery and early discharge from hospital.
Declaration of competing interest
None.
References
- 1.Benumof J.L. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anaesthesia. Anaesthesiology. 2000;93:1541–1544. doi: 10.1097/00000542-200012000-00033. [DOI] [PubMed] [Google Scholar]
- 2.Blonna D., Bellato E., Caranzano F., Assom M., Rossi R., Castoldi F. Arthroscopic Bankart repair versus open Bristow-Latarjet for shoulder instability: a matched-pair multicenter study focused on return to sport. Am J Sports Med. 2016;44(12):3198–3205. doi: 10.1177/0363546516658037. [DOI] [PubMed] [Google Scholar]
- 3.Bosco L., Zhou C., Murdoch J.A.C. Pre- or postoperative interscalene block and/or general anesthesia for arthroscopic shoulder surgery: a retrospective observational study. Can J Anaesth. 2017;64(10):1048–1058. doi: 10.1007/s12630-017-0937-6. [DOI] [PubMed] [Google Scholar]
- 4.Christina L.B., David M.C. Anaesthesia for shoulder surgery. Cont Educ Anaesth Crit Care Pain. 2008;8(6):193–198. doi: 10.1093/bjaceaccp/mkn040. [DOI] [Google Scholar]
- 5.Cook T.M., Harrop-Griffiths W. Aerosol clearance times to better communicate safety after aerosol-generating procedures. ICM Anaesthesia. 2020;75(8):1122–1123. doi: 10.1111/anae.15146. [DOI] [PubMed] [Google Scholar]
- 6.Huerta A., Rincón G., Peidro L., Combalia A., Sastre S. Controversies in the surgical management of shoulder instability: open vs arthroscopic procedures. Open Orthop J. 2017;11:875–881. doi: 10.1177/0363546516658037. 10.2174/1874325001711010875 44(12):3198-3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussain N., Goldar G., Ragina N., Banfield L., Laffey J.G., Abdallah F.W. Suprascapular and interscalene nerve block for shoulder surgery: a systematic review and meta-analysis. Month Anesthesiol. 2017;127(6):998–1013. doi: 10.1097/ALN.0000000000001894. [DOI] [PubMed] [Google Scholar]
- 8.Mason S.E., Noel-Storr A., Ritchie C.W. The impact of general and regional anesthesia on the incidence of post-operative cognitive dysfunction and post-operative delirium: a systematic review with meta-analysis. J Alzheim Dis. 2010;22(Suppl 3):67–79. doi: 10.3233/JAD-2010-101086. [DOI] [PubMed] [Google Scholar]
- 9.Saied N.N., Helwani M.A., Weavind L.M., Shi Y., Shotwell M.S., Pandharipande P.P. Effect of anaesthesia type on postoperative mortality and morbidities: a matched analysis of the NSQIP database. Br J Anaesth. 2017:105–111. doi: 10.1093/bja/aew383. [DOI] [PubMed] [Google Scholar]