Abstract
Hip fractures often occur in elderly people and are a major global health challenge causing many consequences, both in health and socioeconomic costs. This review aimed to identify complications that occur in patients with postoperative hip fracture between 30 days and 60 months after discharge. This review was conducted on articles published from 2005 to 2017 obtained from the EBSCO, PubMed, ProQuest and Google Scholar databases. The literature search followed PRISMA Guidelines. Key search words included the terms: hip fracture, complication, postoperative, community, and nursing. Articles were considered eligible if discussed the complications of hip fracture with surgical treatment, occurring post hospital discharge and the patient was in the community. In this review, 23 articles were included that met the inclusion criteria. There were 16 articles that cohort studies, 3 were retrospective studies, 3 were randomized control trials and 1 article was an observational study. The time of observation varied from 30 days to the longest of 5 years. Quality assessment of the levels of evidence used the Oxford CEBM recommendations. The review results found that postoperative hip fracture patients after discharge still experienced various complications after 30 days and up to 1–3 years post-operation.
Keywords: Hip fracture, Complications, Postoperative, Post-discharge, Literature review
1. Introduction
Hip fracture is a fracture that often occurs in the lower extremities.1 For elderly people, hip fractures cause significant morbidity and mortality and almost 50% of patients cannot fully recover. Many elderly with hip fractures die within 12 months post-operation while a quarter of those who live independently need long-term care.1,2 By 2040, it is estimated that the number of hip fractures will double as the elderly population increases. Various preoperative conditions and complications after surgery contribute to the high morbidity and mortality rates.3
After surgery, many complications can occur when the patient is hospitalized or post hospital discharge. Complications that occur after a patient leaves the hospital often require readmission and can result in death.4 One review reported about several concerns involving postoperative complications that occurred during hospitalization of patients.5 Some systematic reviews have also reported on fractures, examining the post-discharge quality of life and finding patients experienced high morbidity, further fractures, and high mortality rates.6 Another systematic review about preoperative indicators for mortality conducted a meta-analysis of outcomes following hip fracture surgery. There were 13 preoperative characteristics that correlated to postoperative mortality and the results of the meta-analysis indicated four characteristics that were related to mortality risk up to 12 months postoperatively, specifically pre-fracture mobility, age >85 years, abnormal ECG, and cognitive impairment.7
Concerning health-related quality of life, one study showed that most patients recovered within 6 months after the fracture.8 Meanwhile, a specific review of post-operative complications after the patient’s discharge from the hospital has not been completely studied. By knowing the kinds of complications that occur after the patient is in the community, preventive measures can be taken so that their functional outcomes can be increased, mortality and morbidity can be prevented. This literature review aimed to identify postoperative complications of hip fracture in patients after hospital discharge from a variety of available evidence.
2. Methods
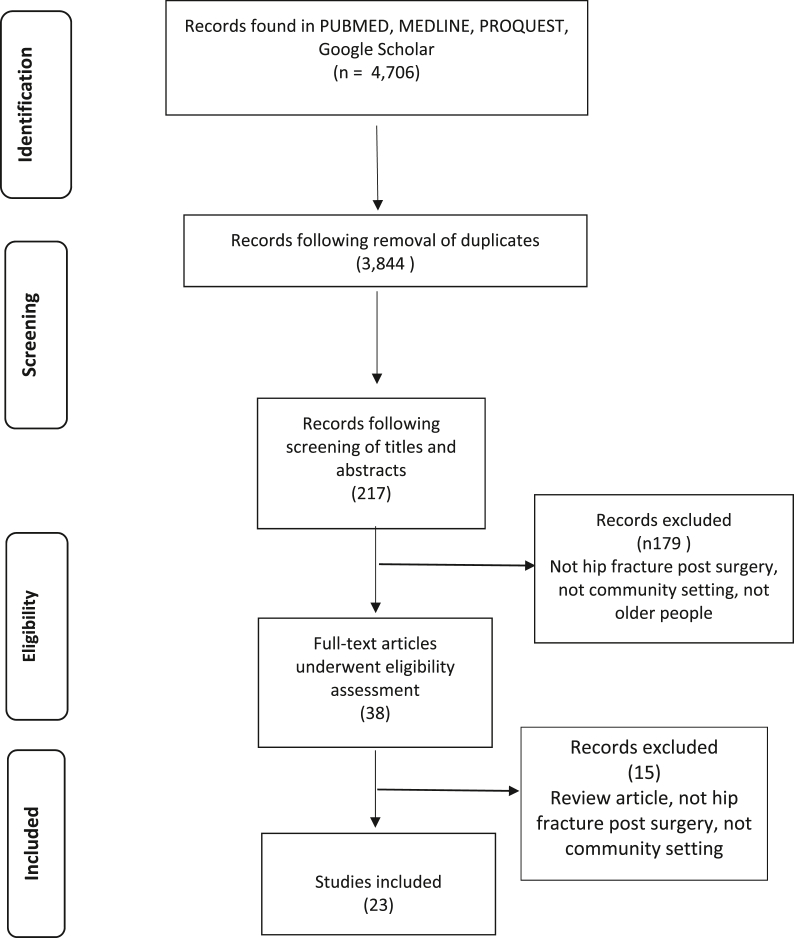
A systematic literature search was conducted in March 2019. Literature reviews were conducted on articles published from 2005 to 2017 obtained from electronic databases: EBSCO, PubMed, ProQuest, and Google Scholar. Literature search used the following search terms: hip fracture, complication, postoperative, community, and nursing, with the limitation of all literature in English. All search results were then exported to Mendeley reference management software. The literature search used the PRISMA guidelines. The search results are presented in Fig. 1.
Fig. 1.
Prisma diagram of search results.
The inclusion criteria of the research article included in this review literature were: a) postoperative hip fracture patients, b) age > 50 years c) measurement of complications made after the patient was in the community d) community settings, and e) articles published in English. All articles in the form of reviews were excluded from this literature review. Search results were sorted after excluding duplicate citations, which was done by reading the title and abstract, then selecting full text article in accordance with eligibility criteria. Articles were considered eligible if they discussed the complications of hip fracture with surgical treatment, which occurred post hospital discharge and the patient returned home to their community. This literature review included all study levels from I to V. Quality assessment of the evidence levels of the studies used the Oxford CEBM recommendations. Data extraction in this review literature contained the list of studies included in the review and complications experienced by hip fracture patients after surgery that have returned home to their community.
3. Results
The main results of the literature search on several electronic databases obtained as many as 4770 studies. After duplicates were removed, the number of studies became 3844. The results of the selection through the title or abstract were 217 studies and after full-text selection according to eligibility criteria, finally there were 23 studies included. Articles included in this literature review consist of 3 articles with 1st level of evidence,10,22,30 13 articles with 2nd level of evidence,8,14, 15, 16,20,21,29,40, 41, 42, 43, 44,49 6 articles with 3rd level of evidence,2,11,26,45, 46, 47 and one article with 4th level of evidence.48
As many as 3 articles used randomized controlled trial study for the research design,10,22,30 and 16 articles were using prospective observational cohort study for the research design,4,8,11,14, 15, 16,20,29,40, 41, 42, 43, 44, 45, 46,49 3 articles were retrospective studies,2,26,47 and one study used observational design.48
Of the 23 studies that were reviewed, there were 13 studies that measured complications after 1 month of discharge, 7 studies that took measurements at 3 months post-discharge, 4 studies that measured at 6 months post-discharge, 15 studies that measured at 1 year post-discharge, 3 studies that measured at 2 years post-discharge, 4 studies that measured at 3 years post-discharge, and 1 study that measured at 5 years post-discharge. Number of studies, types of complications, and time of measurement of complications are shown in Table 1. Complications that appear at each measurement time are presented in Table 2 below.
Table 1.
List number of studies, types of complications and time of measurement of complications.
| Time After Operation | 1 month | 3 months | 6 months | 1 year | 2 years | 3 years | 5 years | |
|---|---|---|---|---|---|---|---|---|
| Complications type/Number of Study | ||||||||
| Mortality | 11 | 5 | 2 | 12 | 2 | 4 | ||
| Pneumonia | 4 | 1 | ||||||
| Chest Infection | 1 | 2 | ||||||
| Respiratory Infection | 1 | 2 | ||||||
| Wound Infection | 1 | 1 | 1 | |||||
| Deep infection | 1 | 3 | 1 | 1 | ||||
| Wound dehiscence | 1 | |||||||
| Urinary Tract Infection | 1 | 4 | 1 | |||||
| Dislocation | 1 | 1 | 6 | 1 | 1 | |||
| Falls | 1 | 4 | 1 | |||||
| Fallen | 1 | 1 | ||||||
| New Fracture | 2 | 1 | ||||||
| New Admission | 1 | 2 | 6 | 1 | ||||
| Deep Venous Thrombosis | 3 | 4 | 1 | |||||
| Pulmonary Embolism | 2 | 5 | 1 | |||||
| Myocardial Infarct | 2 | 1 | 6 | 1 | ||||
| Cardiac Failure | 1 | 1 | 4 | 1 | ||||
| Cardiac Event | 1 | 1 | 2 | |||||
| Anxiety | ||||||||
| Depression | 1 | |||||||
| Decubitus | 3 | 1 | 1 | |||||
| Stroke | 2 | 5 | 1 | |||||
| Gastro intestinal bleed | 1 | 3 | ||||||
| Renal Failure | 1 | |||||||
| Abdominal Pain | 1 | |||||||
| Cancer | 1 | 1 | 2 | |||||
| Gastric ulcer | 1 | 1 | ||||||
| Reoperation | 2 | 2 | 1 | 4 | 2 | 1 | ||
| Atrial Fibrillation | 1 | |||||||
| Avascular necrosis | 1 | |||||||
Table 2.
Post discharge complications in post-operative hip fracture patients.
| No | Time of measurement | Complications |
|---|---|---|
| 1. | 1 month | Mortality, chest infection, wound infection, deep infection, urinary tract infection, deep venous thrombosis, dislocation, falls, pulmonary embolism, new admission, reoperation stroke, gastrointestinal bleed, cancer, myocardial infarct, cardiac failure or event, and depression |
| 2. | 3 months | Mortality, wound infection, dislocation, reoperation, myocardial infarct, and cardiac failure |
| 3. | 6 months | Mortality, new admission, reoperation and cardiac event |
| 4. | 1 year | Mortality, pneumonia, chest infection, respiratory infection, wound infection, deep infection, urinary tract infection, dislocation, falls, new fracture, new admission, decubitus, stroke, gastrointestinal bleed, renal failure, abdominal pain, cancer, gastric ulcer, reoperation, atrial fibrillation, avascular necrosis, deep venous thrombosis, pulmonary embolism, myocardial infarct, and cardiac failure |
| 5. | 2 years | Mortality, deep infection, wound dehiscence, dislocation, decubitus, and reoperation |
| 6. | 3 years | Mortality, pneumonia, respiratory infection, deep infection, urinary tract infection, dislocation, falls, new fracture, new admission, decubitus, stroke, cancer, gastric ulcer, reoperation, deep venous thrombosis, pulmonary embolism, myocardial infarct, cardiac failure and cardiac event |
| 7. | 5 years | No complication occur |
4. Discussion
4.1. Mortality
Mortality is widely used as an outcome parameter in various studies. The results of this review were not different from previous systematic reviews where the mortality rate of patients with hip fractures was very high.6 This is also consistent with the existing literature where patients with hip fracture experienced high mortality.9 High mortality was also correlated to comorbidities suffered by patients at hospital admission, resulting in postoperative complications and increased mortality.4 The mortality rate that occurred after 30 days after surgery ranged from 3.2% to 10.4%. The rate became 4.7%–19% after 3 months, 13%–30.3% after 6 months, 3.3%–46% after 1 year, 26.2% up to 37.2% after 2 years, and 32.3% up to 100% after 3 years.
Another study stated that high mortality other than due to comorbidities was also related to complications that occurred during hospitalization. Cancer, cardiovascular disease, dependence in personal activity of daily living (P-ADL), cardiac failure, dementia, and pulmonary embolism were all independent predictors during hospitalization of mortality.10 Since comorbidities before surgery are very influential, high risk management, such as paying attention to preoperative health status and preventing postoperative complications, is needed to reduce mortality and if complications have occurred, special care and treatment should be given. Several studies of hip fracture patients that included mortality as a long-term outcome parameter indicated that the cause of death was not significantly associated with acute trauma.11, 12, 13 One-year mortality rates were affected by baseline frailty.11
Low mortality in the community was found after the introduction of a new program for hip fracture.14 Comprehensive geriatric assessment contributes to low first year post-operative mortality including daily geriatric medical care with outpatient follow-up. The existence of specific and targeted follow-up related to the assessment of the health of blood vessels and bones might also contribute to reduce 1-year mortality.15
Conversely, one study of mortality found that patient age at the time of injury was the single most significant influence on patient outcome. The results showed that the older patients had higher mortality rate and shorter survival time. The study also found that delay in surgery did not affect the mortality rate.16
4.2. Infection
Complications of infection in postoperative hip fracture patients were mostly related to comorbidities that accompanied patients before surgery.4 Up to 3 months postoperatively, the causes of many readmissions were urinary tract infections (UTI) and pneumonia.2 Complications of postoperative infections were also thought to be related to overlapping surgery.17 The risk of postoperative pneumonia was mostly related to postponement of surgery and old age. It was found to be less in patients with short length of stay (LOS) and early mobilization.2,18,19
At 30 days after surgery, complications of chest infection were 9% (215/2448), while complications of UTI were 4% (98/2448) and wound infection or deep infection were 1.1% and 1% (27/2448), respectively.4 At 1 year after surgery, complications that occurred were deep infection (1.1%–6.7%), wound infection (4%), pneumonia (4.65%–13.3%), surgical infection (4.3%), and UTI (0.9%–34.30%).8,20,21 At 2 years postoperatively, complications of wound dehiscence were as much as 2% and a deep infection was 7%.22 At 3 years postoperatively, UTI was found as much as 52.35%, while respiratory infection was 12.7–34% and deep wound infection was 1.34%.10
4.3. Dislocation
One major complication of total hip arthroplasty (THA) is dislocation, occurring in 2%–20% of patients. The lowest level is THA for patients who do not experience a fracture. The low incidence of complications from dislocation is related to the surgeon’s level of experience, the surgical procedure, and application of cemented stems.23
4.4. New admission
Assessments of quality of care and cost as well as patient outcome often involve frequency of readmission. Shum et al. conducted a study in 2014 found that after the implementation of care pathways was done for one month or 1 year, the level of readmission did not change. However, the level of readmission must be carefully considered in the health care system. Another study stated 1/3 of patients experienced readmission within 6 months after hip fracture surgery.24 Most readmission was caused by non-surgical events, including new falls, systemic infection, and cardiovascular disease. These conditions are in line with previous research conducted by Giusti et al., in 2008, which showed that readmission was mostly caused by infection and cardiac disease.25
4.5. Reoperation
Reoperation in postoperative hip fracture patients can be caused by dislocations that require revision with surgery. Reoperation also occurred due to a deep infection that needed surgery for irrigation.2 Specific reoperation in femoral neck fractures was due to avascular necrosis, nonunion or aseptic loosening in patients with uncemented hemiarthroplasty. In trochanteric fracture patients, the most common reasons for reoperation was nonunion of the fracture, screw penetration, or failure of osteosynthesis.24
4.6. Decubitus
Complications of decubitus in postoperative hip patients are associated with immobility. Special considerations for patients undergoing hip repair include a careful skin examination in the area of stress, especially the heel. Decreased postoperative hip fracture mobility can increase the risk of pressure injury in this area within 24 h.9
4.7. Deep vein thrombosis/pulmonary embolism (DVT/PE)
Patients undergoing hip fracture surgery are at high risk for DVT/PE. Apart from orthopaedic injuries, old age, medical comorbidity, and poor postoperative mobilization contributed to this high risk of thromboembolism.26,27 The incidence of DVT can be reduced by administering prophylaxis. After proximal femoral fracture, fatal pulmonary embolism occurs in less than 10% of patients. The risk of DVT/PE may continue post operatively even after administration of thromboprophylaxis.28
4.8. Anxiety/depression
The results of a study conducted by Ruths in 2017 consistently reported lower anxiety/depression levels 1 year post surgery in cities with majority populations over 80. Lower anxiety/depression levels might indicate that this community provided better living conditions for the elderly in general.29 In other studies, symptoms of depression immediately and 6 weeks after surgery predicted adverse outcomes regardless of patient’s age and functional levels before illness. Symptoms of depression strongly influenced responses to assessment questionnaires such as the Sickness Impact Profile (SIP), which showed that depression worsened the effects of hip fracture on a patient’s life, more than the level of decline in objective function could explain, which was measured by performance-based results.30
4.9. Falls and new fracture
Postoperative hip fracture patients usually have several comorbidities and experience several complications, such as falls, fractures, infections, pressure ulcers, delirium, and cardiovascular events. If they are associated with mortality, the comorbidities and complications were closely related. Usually, if the patient was hospitalized, the complications mentioned above could be prevented properly. Additionally, efforts are needed to prevent any complications that might occur after the patient was discharged from the hospital.10 Falls and new fractures were complications that often occurred after a patient was discharged from the hospital, but precautions can be taken. Falls after hip fracture were also reported in about 20%–50% of patients in 4–6 months after surgery.32 Patients with walking aids who had a history of falling before a hip fracture had three to nine times higher risk fall within six months than those with no previous history.33
4.10. Myocardial infarct, cardiac fail/event
Cardiac failure was a major postoperative complication that caused death within 30 days postoperatively.4,33, 34, 35 Patients with cardiovascular disease commonly experience serious postoperative complications. Preoperative assessment is very important to ascertain the patient’s history of this problem. One study conducted by Berggen et al., in 2016 identified cardiovascular events in almost 50% of deaths that occurred in postoperative patients in the first month after hospital admission. These results match previous studies conducted by36 and.37 Research showed that cardiovascular events are risk factors that might be modified.10,38 Cardiac exacerbation was also a major cause of readmission within 3 months postoperatively.2 Patients with common postoperative complications, especially those with many complications, have a much higher mortality. Accordingly, efforts must be made to prevent these events after hip fracture in order to improve functional outcomes, reduce mortality and morbidity.7,39
5. Conclusions
Postoperative hip fracture patients still experience various complications between 30 and 90 days, and 1–3 years after surgery. Additionally, longitudinal prospective studies can provide confirming evidence of the importance efforts to prevent or minimize the occurrence of post-discharge complications.
Declaration of competing interest
The author (s) declared no conflicts of interest.
Contributor Information
Umi Istianah, Email: umiistianahmadzkur@gmail.com.
Intansari Nurjannah, Email: intansarin@ugm.ac.id.
Rahadyan Magetsari, Email: magetsarir@yahoo.com.
References
- 1.Gupta A. The effectiveness of geriatrician-led comprehensive hip fracture collaborative care in a new acute hip unit based in a general hospital setting in the UK. J R Coll Physicians Edinb. 2014;44(1):20–26. doi: 10.4997/JRCPE.2014.105. [DOI] [PubMed] [Google Scholar]
- 2.Frenkel Rutenberg T., Daglan E., Heller S., Velkes S. A comparison of treatment setting for elderly patients with hip fracture, is the geriatric ward superior to conventional orthopedic hospitalization? Injury. 2017;48(7):1584–1588. doi: 10.1016/j.injury.2017.04.049. [DOI] [PubMed] [Google Scholar]
- 3.Menzies I.B., Mendelson D.A., Kates S.L., Friedman S.M. The impact of comorbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr Orthop Surg Rehabil. 2012;3(3):129–134. doi: 10.1177/2151458512463392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roche J.J.W., Wenn R.T., Sahota O., Moran C.G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ Br Med J. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carpintero P. Complications of hip fractures: a review. World J Orthoped. 2014;5(4):402. doi: 10.5312/wjo.v5.i4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nazrun A.S., Tzar M.N., Mokhtar S.A., Mohamed I.N. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Therapeut Clin Risk Manag. 2014;10:937–948. doi: 10.2147/TCRM.S72456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galli M., Ciriello V., Bocchino L., Gangemi N.M., Peruzzi M., Marzetti E. Clinical and functional outcomes of internal fixation with intertrochanteric antegrade nail in older patients with proximal extracapsular femoral fractures. Eur J Trauma Emerg Surg. 2014;40(4):495–500. doi: 10.1007/s00068-013-0343-x. [DOI] [PubMed] [Google Scholar]
- 8.Hansson S., Rolfson O., Åkesson K., Nemes S., Leonardsson O., Rogmark C. Complications and patient-reported outcome after hip fracture. A consecutive annual cohort study of 664 patients. Injury. 2015;46(11):2206–2211. doi: 10.1016/j.injury.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 9.Ignatavicius D.D., Workman M.L. In: Medical Surgical Nursing, Patients-Centered Collaborative Care. eighth ed. Blair M., Rebar C., Winkelman C., editors. Elsevier; St Louis, Missouri: 2016. [Google Scholar]
- 10.Berggren M., Stenvall M., Englund U., Olofsson B., Gustafson Y. Co-morbidities, complications and causes of death among people with femoral neck fracture - a three-year follow-up study. BMC Geriatr. 2016;16:120. doi: 10.1186/s12877-016-0291-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suhm N., Kaelin R., Studer P. Orthogeriatric care pathway: a prospective survey of impact on length of stay, mortality and institutionalisation. Arch Orthop Trauma Surg. 2014;134(9):1261–1269. doi: 10.1007/s00402-014-2057-x. [DOI] [PubMed] [Google Scholar]
- 12.Tosteson A.N.A., Gottlieb D.J., Radley D.C., Fisher E.S., Melton L.J. Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18(11):1463–1472. doi: 10.1007/s00198-007-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gosch M., Druml T., Nicholas J.A. Fragility non-hip fracture patients are at risk. Arch Orthop Trauma Surg. 2015;135(1):69–77. doi: 10.1007/s00402-014-2115-4. [DOI] [PubMed] [Google Scholar]
- 14.Pedersen S.J., Borgbjerg F.M., Schousboe B. A comprehensive hip fracture program reduces complication rates and mortality. J Am Geriatr Soc. 2008;56(10):1831–1838. doi: 10.1111/j.1532-5415.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- 15.Henderson C.Y., Shanahan E., Butler A. Dedicated orthogeriatric service reduces hip fracture mortality. Ir J Med Sci. 2017;186(1):179–184. doi: 10.1007/s11845-016-1453-3. [DOI] [PubMed] [Google Scholar]
- 16.Muhm M., Arend G., Ruffing T., Winkler H. Mortality and quality of life after proximal femur fracture--effect of time until surgery and reasons for delay. Eur J Trauma Emerg Surg. 2013;39(3):267–275. doi: 10.1007/s00068-013-0267-5. [DOI] [PubMed] [Google Scholar]
- 17.Paterson J.M., Kreder H.J., Pincus D. Association of overlapping surgery with increased risk for complications following hip surgery. JAMA Intern Med. 2017;178(1):75. doi: 10.1001/jamainternmed.2017.6835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klop C., Welsing P.M.J., Cooper C. Mortality in British hip fracture patients, 2000-2010: a population-based retrospective cohort study. Bone. 2014;66:171–177. doi: 10.1016/j.bone.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Jameson S.S., Khan S.K., Baker P. A national analysis of complications following hemiarthroplasty for hip fracture in older patients. QJM. 2012;105(5):455–460. doi: 10.1093/qjmed/hcs004. [DOI] [PubMed] [Google Scholar]
- 20.Ravi B., Pincus D., Wasserstein D. Association of overlapping surgery with increased risk for complications following hip surgery: a population- based, matched cohort study. Jama Intern Med. 2018;178(1):75–83. doi: 10.1001/jamainternmed.2017.6835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roche J.J.W., Wenn R.T., Sahota O., Moran C.G. Effecet of comorbities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529) doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frihagen F., Nordsletten L., Bahr R. An 80 year old woman who fell in her homw. BMJ. 2009;339:b4839. doi: 10.1136/bmj.b4839. [DOI] [PubMed] [Google Scholar]
- 23.Jauregui J., Buttaro M., Musso C., Iserson K.V., Piccaluga F., Monzón D.G. Total hip arthroplasty for hip fractures. Geriatr Orthop Surg Rehabil. 2014;5(1):3–8. doi: 10.1177/2151458514520700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Melander O., Sutton R., Härstedt M., Rogmark C., Fedorowski A. Impact of comorbidity on 6-month hospital readmission and mortality after hip fracture surgery. Injury. 2014;46(4):713–718. doi: 10.1016/j.injury.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 25.Giusti A., Barone B., Razzono M. Predictors of hospital readmission in a cohort of 236 elderly discharged after surgical repaior of hip fracture: one-year follow-up. Ageing Clin Exp Res. 2008;20:253–259. doi: 10.1007/BF03324779. [DOI] [PubMed] [Google Scholar]
- 26.Lüthje P., Helkamaa T., Nurmi-Lüthje I., Kaukonen J.P., Kataja M. An 8-year follow-up study of 221 consecutive hip fracture patients in Finland: analysis of reoperations and their direct medical costs. Scand J Surg. 2014;103(1):46–53. doi: 10.1177/1457496913494726. [DOI] [PubMed] [Google Scholar]
- 27.Anand S., Buch K. Post-discharge symptomatic thromboembotic events in hip fracture patients. Ann R Coll Surg Engl. 2007;89(5):517–520. doi: 10.1308/003588407X202065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gillespie W., Warwick D., Murray D., Gregg P.J. Risks and benefits of prophylaxis against venous thromboembolism in orthopaedic surgery. J Bone Jt Surg [Br] 2000;8282(4):475–479. doi: 10.1302/0301-620x.82b4.10452. [DOI] [PubMed] [Google Scholar]
- 29.Ruths S., Baste V., Bakken M.S., Engesæter L.B., Lie S.A., Haugland S. Municipal resources and patient outcomes through the first year after a hip fracture. BMC Health Serv Res. 2017;17(1):144. doi: 10.1186/s12913-017-2087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Voshaar O.R.C., Banerjee S., Horan M. Fear of falling more important than pain and depression for functional recovery after surgery for hip fracture in older people. Psychol Med. 2006;36(11):1635–1645. doi: 10.1017/S0033291706008270. [DOI] [PubMed] [Google Scholar]
- 32.Kristensen M.T., Foss N.B., Kehlet H. Research report. Phys Ther. 2009;3(4):251–255. [Google Scholar]
- 33.Kenzora J.E., McCarthy R.E., Lowell J.D., Sledge C.B. Hip fracture mortality: relation to age, treatment, preoperative illness, time of surgery, and complications. Clin Orthop Relat Res. 1984;186(186):45–56. [PubMed] [Google Scholar]
- 34.Eiskjaer S., Ostgård S.E. Risk factors influencing mortality after bipolar hemiarthroplasty in the treatment of fracture of the femoral neck. Clin Orthop Relat Res. 1991;270(270):295–300. [PubMed] [Google Scholar]
- 35.Forse L., Søgaard A.J., Meyer H.E., Edna T., Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Screening. 1999:73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 36.Vestergaard P., Rejnmark L., Mosekilde L. Socioeconomic aspects of fractures within universal public healthcare: a nationwide case-control study from Denmark. Scand J Publ Health. 2006;34(4):371–377. doi: 10.1080/14034940500441223. [DOI] [PubMed] [Google Scholar]
- 37.Perez J.V., Warwick D.J., Case C.P., Bannister G.C. Study after proximal femoral. fracture - an autopsy. 1995;26(4):237–240. doi: 10.1016/0020-1383(95)90008-l. [DOI] [PubMed] [Google Scholar]
- 38.Petersen M.B., Jørgensen H.L., Hansen K., Duus B.R. Factors affecting postoperative mortality of patients with displaced femoral neck fracture. Injury. 2006;37(8):705–711. doi: 10.1016/j.injury.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 39.Lawrence V.A., Hilsenbeck S.G., Noveck H., Poses R.M., Carson J.L. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162(18):2053–2057. doi: 10.1001/archinte.162.18.2053. [DOI] [PubMed] [Google Scholar]
- 40.Nielsen K.A., Jensen N.C., Jensen C.M. Quality of care and 30 day mortality among patients with hip fractures: a nationwide cohort study. 2009;9:186. doi: 10.1186/1472-6963-9-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nikkel L.E., Kates S.L., Schreck M. 2015. Length of Hospital Stay after Hip Fracture and Risk of Early Mortality after Discharge in New York State: Retrospective Cohort Study; p. 351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Slor C.J., Witlox J., Jansen R.W.M. Affective functioning after delirium in elderly hip fracture patients. 2013;25(3):445–455. doi: 10.1017/S1041610212001962. [DOI] [PubMed] [Google Scholar]
- 43.Nordström P., Gustafson Y., Michaëlsson K., Nordström A. 2015. Length of Hospital Stay after Hip Fracture and Short Term Risk of Death after Discharge: A Total Cohort Study in Sweden; p. 350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Monzon D.G., Iserson K.V., Jauregui J. Total hip arthroplasty for hip fractures: 5-year follow-up of functional outcomes in the oldest independent old and very old patients. 2015;5(1):3–8. doi: 10.1177/2151458514520700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Härstedt M., Rogmark C., Sutton R., Melander O., Fedorowsk A. Impact of comorbidity on 6-month hospital readmission and mortality after hip fracture surgery. 2014;46(4):713–718. doi: 10.1016/j.injury.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 46.Nuotio M., Tuominen P., Luukkaala T. Association of nutritional status as measured by the Mini-Nutritional Assessment Short Form with changes in mobility, institutionalization and death after hip fracture. 2016;70(3):393–398. doi: 10.1038/ejcn.2015.174. [DOI] [PubMed] [Google Scholar]
- 47.Dwyer J.G., Reynoso J.F., Seevers J.A. Assessing preoperative frailty utilizing validated geriatric mortality calculators and their association with postoperative. Hip Fracture Mortality Risk. 2014;5(3):109–115. doi: 10.1177/2151458514537272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Uriz-Otanoa F., Pla-Vidalb J., Tiberio-Lópezc G., Malafarina . Vol. 89. 2016. Factors associated to institutionalization and mortality over three years; pp. 9–15. (Elderly People with a Hip Fracture—An Observational Study Francisco). [DOI] [PubMed] [Google Scholar]
- 49.Ireland A.W., Kelly P.J., Cumming R.G. Associations between hospital-based rehabilitation for hip fracture and two-year outcomes for mortality and independent living: an australian database study of 1,724 elderly community-dwelling patients. 2016;48(7):625–631. doi: 10.2340/16501977-2108. [DOI] [PubMed] [Google Scholar]