Abstract
Background
Correct management of Hoffa fractures is a challenge in the clinical context. Open reduction along with internal fixation should be the therapy of choice. Mechanical trials with the main internal fixation systems conducted by individualized finite element (FEM) models, to date, have been neglected. The aim of this study was to biomechanically analyze four fixation methods for the treatment of Type II Hoffa fracture (OTA Classification: 33B3.2∗ lateral) using FEM.
Methods
Four internal fixators were developed to treat Type II Hoffa fracture using finite elements: 4.5 mm cortical screws and 7 mm cannulated screw in anterior-to-posterior and posterior-to-anterior directions (4.5AP, 4.5 PA, 7AP and 7 PA). Under the same conditions, fractural deviation in the vertical, maximum and minimum principal and Von Mises directions in the syntheses used were evaluated.
Results
The vertical displacements evaluated were 0.7 mm, 0.5 mm, 0.8 mm and 0.3 mm; the values of maximum were 6.14 Mpa, 6.15 hPa, 6.0 Mpa and 6.2 Mpa, the values obtained from minimum data were 6.26 Mpa, −6.45 Mpa, −7.3 MPa and −6.8 Mpa and the maximum values of Von Mises peak stress were 185.0 Mpa, 194.1 Mpa, 143.6 Mpa and 741.4 Mpa, for the fixation models 4.5AP, 4.5 PA, 7AP and 7 PA, respectively.
Conclusion
The 7 mm-cannulated screw fixation system yielded the best mechanical results evaluated by FEM in the treatment of Type II Hoffa fracture, causing a decrease in vertical displacement when used in retrograde and in Von Mises peak stress in anterograde.
Keywords: Screw, Hoffa fracture, Internal fixation, Finite element analysis, Biomechanics
1. Introduction
Coronal fractures of femoral condyles, extremely rare and little explored scientifically, were initially described in 1869 1,2 and publicized as Hoffa fractures3 since 1904. Injuries are more frequent in the posterior region of the lateral femoral condyle, representing up to 13% of the total distal fractures of the femur.1,4 The specific injury mechanism remains uncertain, however, they are usually linked to high-energy trauma, causing shear stresses between the femoral condyle and the tibial plateau.1,5 According to Letenneur et al6 fractures are classified into 3 types, based on the fracture line and relationships to ligaments and soft tissues. Type II fractures (horizontal to the base of the posterior condyle), are usually more complex and with worse prognosis, having a higher probability of non-union due to lack of intrinsic stability and decrease in blood supply.6,7
Conservative treatment is associated with less favorable outcome resulting into high incidence of non-union and poor functional results.1,4 Therefore, a surgical approach becomes necessary.8,9 The primary goals of treatment consist in the effectiveness of anatomical reduction of the joint surface, stable fixation methods and early mobilization.9, 10, 11 Fracture line characteristics, severity and associated injuries are crucial aspects when designing the surgical plan.1
Despite the various fixation techniques, the scientific literature does not show a consensus on the best method, number, size and configuration of the screws.1,4,9,12,13 The principle of treatment, since it is a strictly joint fracture, must be based on absolute stability with the use of interfragmentary compression.1,4 The discussion inherent to the degree of stability produced by the methods using screws inserted in the anterior-to-posterior or posterior-to-anterior direction still remains inconclusive.1,13 Biomechanical analysis of treatment methods for Hoffa fractures is scarce, and, to the best of our knowledge, mechanical trials conducted by finite element models (FEM) until now, are unknown.
The aim of this study was to compare the biomechanical capacity of four fixation methods (4.5 mm cortical screws and 7 mm cannulated screws in anterior-to-posterior and posterior-to-anterior directions), using the absolute stability principle, for the treatment of type II Hoffa fracture (OTA Classification: 33B3.2∗ lateral)7 using FEM, to describe the fracture deviation, maximum and minimum principal and Von Mises stress in the syntheses used.
2. Methodology
2.1. Dimensional characteristics and screw insertion technique
The screws used were formatted with the dimensional similarities evaluated in the De Puy Synthes® brand standards. Screw models: 4.5 mm cortical and 7.0 mm cannulated (with 32 mm long thread) screws. The technique employed observed the use of holes that would allow interfragmentary compression (smooth hole), always located in the fractured segment where the screw heads would be placed, as described by the AO (Arbeitsgemeinschaft für Osteosynthesefragen) technique when using the 4.5 screw, whereas the 7.0 mm screw was only drilled through the pilot hole, whose diameter was large enough to fit the screw core.
2.2. Finite element analysis (FEM)
After formatting the syntheses, the 4.5 mm cortical screw was inserted in the anterior-to-posterior direction (4.5 AP) and in the posterior-to-anterior direction (4.5 PA). The same was done with 7 mm cannulated screw (7 AP and 7 PA), respectively.
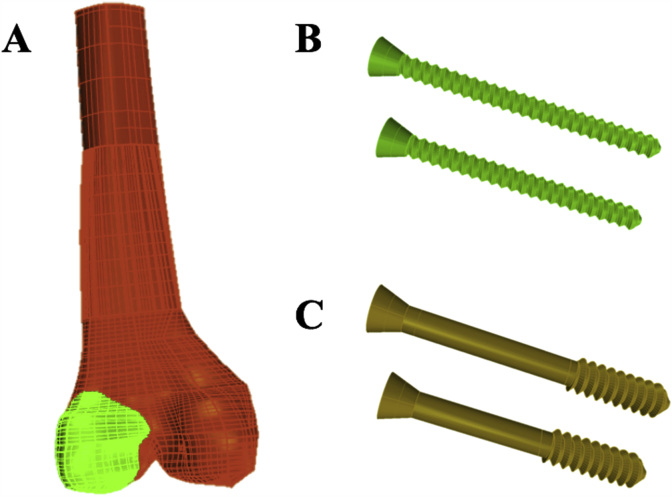
In order to compose the biocad, the distal femur of a bone model (medium size) of left femurs, fourth generation model 3403-106, from Sawbones ™ (Pacific Laboratories Inc., Vashon, WA, model 3403) was used. This was scanned to obtain images in DICOM (Digital Imaging and Communications in Medicine). The tomography used was Emotion (16 channels, Siemens ™, Munich, Germany) with resolution of (512 x 512) and distance between sections of 1.0 mm. With the DICOM images, using the InVesalius ™ program, three-dimensional (3D) reconstruction of the anatomical structure took place (Fig. 1). These 3D models were exported to the Rhinoceros ™ 6 program (Robert McNeel & Associates, United States) in order to design and reproduce the fracture fragment in the lateral condyle, with angular dimensions and positions of the fracture line, in order to obtain a fracture axial Hoffa type II (OTA Classification: 33B3.2 ∗ lateral).
Fig. 1.
(A) Construction of Type II Hoffa fracture Model (OTA Classification: 33B3.2∗ lateral),7 (B) 4.5 mm cortical screw and (C) 7 mm cannulated screw.
The study by MEF was carried out in the SimLab ™ program (HyperWorks, United States) using the Optistruct solver. The element used in the composite was the tetrahedral, executed after the implementation of the properties, distinctly for each element that comprised the models, being: the elasticity module and Poisson’s ratio (Table 1).
Table 1.
Properties of materials. Cortical bone; Trabecular bone and Syntheses.
| Material | Properties of materials |
|
|---|---|---|
| Elastic Modulus (Mpa) | Poisson’s ratio (v) | |
| Cortical bone | 17 | 0.26 |
| Trabecular bone | 1.7 | 0.26 |
| Steel syntheses | 193 | 0.33 |
The tests were carried out by applying a load in the direction of the Z axis in the value of 6000 N, on the long axis of the femur, positioned with an inclination angle in flexion of the femur of 20° and neutral in the axial direction. On the X and Y axes no load was applied. The mobility restrictions of the composite were determined, as fixed, on the X,Y and, Z axes. This restriction, which ensured the alignment and stability of the system.
The vertical displacement in mm of the fractured fragment (femoral condyle), the Maximum Principal (traction) and Minimum Principal (compression) variables for bone composites were analyzed by the MEF. For the synthesis materials, the Von Mises Equivalent stress was analyzed.
3. Results
3.1. Description of vertical displacements of the fracture with the different fixation models
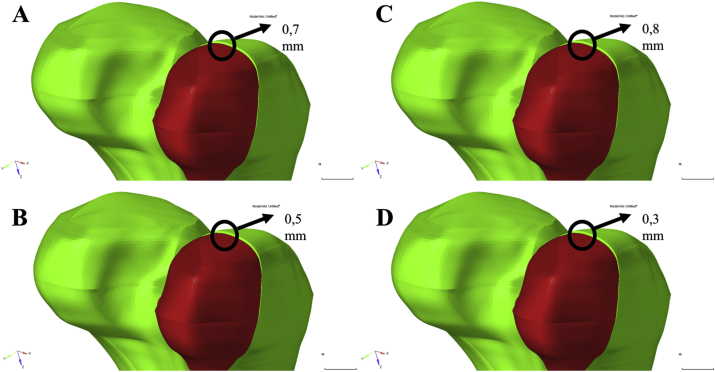
The vertical displacements evaluated were 0.7 mm, 0.5 mm, 0.8 mm and 0.3 mm for the fixation models 4.5AP, 4.5 PA, 7AP, 7 PA, respectively (Fig. 2).
Fig. 2.
Vertical dislocations of the fracture with the different fixation models. (A) 4.5 mm anterior-to-posterior cortical screw (4.5 AP), (B) 4.5 mm posterior-to-anterior cortical screw (4.5 PA), (C) 7 mm anterior-to-posterior cannulated screw (7AP) and (D) 7 mm posterior-to-anterior cannulated screw (7 PA). The results were 0.7 mm, 0.5 mm, 0.8 mm and 0.3 mm, respectively.
It was thus demonstrated that the use of the 7 mm screw in a retrograde mode (7 PA) reduced the vertical displacement by about 62.5%, when compared to the 7 mm screw anterograde method (7AP).
The results were similar for the 4.5 mm screws, where a decrease of 29% was obtained with the use of the retrograde route (4.5 PA) when compared to the anterograde route (4.5AP).
In the comparison between the two screws used in retrograde mode, a 40% decrease in 7 PA was observed when compared to 4.5 PA.
3.2. Maximum (traction) and minimum (compression) principals distribution on fractures with the different fixation models
Maximum principal values, obtained adjacent to the fracture, were 6.14 Mpa, 6.15 Mpa, 6.0 Mpa and 6.2 Mpa, for fixation models 4.5AP, 4.5 PA, 7AP, 7 PA, respectively.
The values from minimum principal data obtained adjacent to the fracture were −6.26 Mpa, −6.45 Mpa, −7.3 Mpa and −6.8 Mpa for fixation models 4.5AP, 4.5 PA, 7AP, 7 PA, respectively.
It can be noted that the values for the maximum principal were quite homogeneous among the 4 methods of fixation tested.
For the minimum values, the 7 mm posterior-to-anterior screw (7 PA) showed a decrease of 7%, when compared to the 7 mm posterior-to-anterior screw (7AP). The minimum values obtained with the anterograde and retrograde techniques using the 4.5 mm screw were homogeneous.
In the comparison between the 4.5 mm and 7 mm screws (anterograde and retrograde), we observed a decrease in the minimum distribution of about 10% in the 4.5 AP and 4.5 PA.
3.3. Von Mises peak stress distribution in the different fixation models
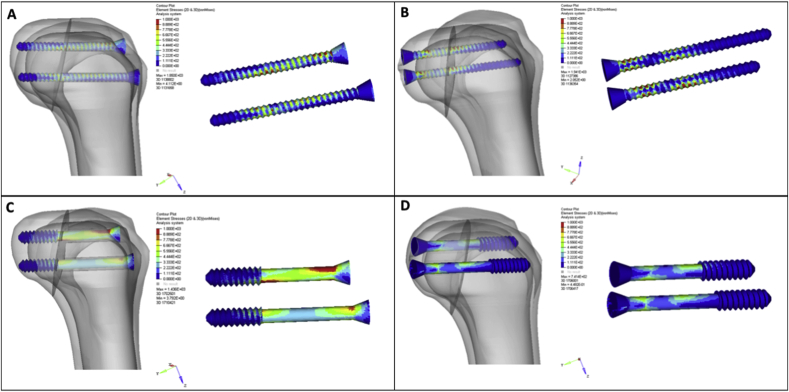
The maximum Von Mises peak stress values were 185.0 Mpa, 194.1 Mpa, 143.6 MPa and 741.4 Mpa, for the fixation models 4.5AP, 4.5 PA, 7AP and 7 PA, respectively (Fig. 3).
Fig. 3.
Peak Von Misses of the different fixation models. (A) 4.5 mm anterior-to-posterior cortical screw (4.5 AP), (B) 4.5 mm posterior-to-anterior cortical screw (4.5 PA), (C) 7 mm anterior-to-posterior cannulated screw (7AP) and (D) 7 mm posterior-to-anterior cannulated screw (7 PA). The results were 185.0Mpa, 194.1Mpa, 143.6 MPa e 741.4Mpa, respectively.
The 7 mm retrograde screw (7 PA) showed a remarkable increase in Von Mises peak stress (≅80%) when compared to the anterograde technique with the 7 mm screw (7AP). The values obtained with the anterograde and retrograde techniques using the 4.5 mm screw were homogeneous.
4. Discussion
The correct diagnosis and management of Hoffa fractures is a challenge within the clinical context.1,2,5 Open reduction, together with stable internal fixation should be the therapy of choice, since fixation stability is a primary factor for healing.9 Cannulated or spongy screws of different dimensions, used in the anterior-to-posterior or posterior-to-anterior direction are the main means of stabilization, yielding different clinical results.4,9,12, 13, 14, 15
In light of this, the present biomechanically study analyzed 4.5 mm cortical and 7 mm cannulated screws in both anterior-to-posterior and posterior-to-anterior directions for Hoffa fracture fixation by FEM. Our results showed that the use of the 7 mm screw through the posterior-to-anterior (7 PA), provided a better result in the reduction of vertical displacement, producing greater fracture stability. The maximum distribution results were homogeneous among the four scenarios tested, but the minimum distribution was better with a 4.5 mm screw, whereas the best effect was achieved in the anterior-to-posterior technique (4.5AP). Finally, the anterior-to-posterior direction with 7 mm screw (7AP) provided the greatest decrease in Von Mises peak stress when compared to the different models tested.
The easiest technique and preferably employed in the treatment of Type II Hoffa fracture is the use of anterior-to-posterior directed screws, due to their ease of access and execution.14 However, by observing the comparative result of the vertical displacement, a better result was achieved with the screw being used in the posterior-to-anterior direction. This finding, although it may be a contributing discovery, requires clinical trials (higher levels of evidence), producing a comparison between the techniques for clinical conclusions. It is worth noting that the difficulty of using the posterior-to-anterior technique should not constitute a problem for obtaining syntheses with better results, since in-depth training by surgeons will provide the confidence required for executing the technique.
Despite the scientific scarcity, previous studies have shown positive biomechanical effects (greater stability) with the application of screws posteriorly, preventing possible migrations linked to shearing stress during knee movements.12,15 Jarit et al.12 published the first cadaveric study (experimental mechanical trials), involving the comparison of insertion techniques of anterior-to-posterior and posterior-to-anterior screws. The authors showed that posterior-to-anterior fixation was significantly more stable, causing smaller vertical displacements, an aspect also observed in the present study with FEM. However, the posterior-to-anterior surgical approach is more difficult, it can put neurovascular structures at risk and increase the chances of damaging articular cartilage.12 Similarly, in the first prospective study published on the subject, Gavaskar et al.15 treated 18 patients using anterograde or retrograde 3.5 mm and 4 mm screws. The researchers evidenced only one complication, among all the cases evaluated, occurring with the use of the anterior-to-posterior route. In addition, all type II Hoffa fractures were treated with retrograde screws, since, according to the authors, the choice of anterior-to-posterior strategy would not provide the necessary stability for this complex fracture type.
Our results also show mechanical variables favorable to the anterograde route, especially in the significant decrease of Von Mises peak stress. Recently, Singh et al.13 demonstrated that surgery performed with two 6.5 mm cannulated spongy screws in the anterior-to-posterior approach provided good stability and positive functional results after 28 months. With a retrospective evaluation, Trikha et al.5 analyzed 32 patients treated with 4.5 mm and 6 mm anterograde screws and exposed to aggressive physiotherapy in the postoperative period. The positive clinical subjective results, evaluated by scales of reported and functional capacity, demonstrate that the anterior-to-posterior direction is a scientifically proven choice.
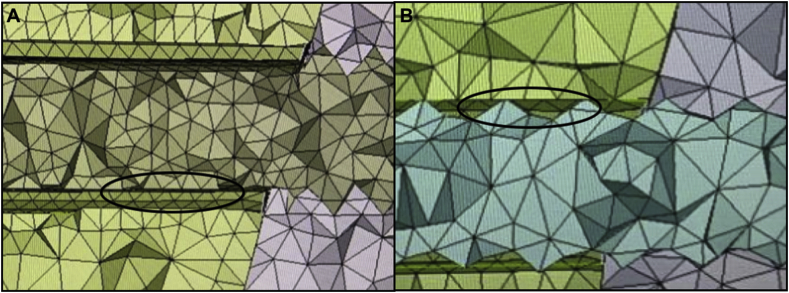
Finally, when comparing the mechanical results obtained between the two dimensions of tested screws, it is evident that the 7 mm screw produced greater stability (vertical displacement decrease) and decreased the Von Mises peak stress, when compared to the 4.5 mm screw. In an experimental study in cadaveric model, Becker et al.16 found similar results. The researchers compared rigidity and total load to failure among 3.5 mm, 4.5 mm and 6.5 mm screws. The authors showed that the results were homogeneous in relation to rigidity, but the 6.5 mm screw demonstrated greater ability to sustain higher loads when compared to the others, providing greater stability. One of the indirect objectives of this study was to qualitatively analyze the intimate relationship between the synthesis material and the bone structure, using the interfragmentary compression technique. The intimate contact of the 7 mm cannulated screw, due to the absence of the need for a smooth tunnel in its technique (different from the 4.5 mm screw), seems to be a possible explanation for its better biomechanical results. Future work needs to improve the methodology for more accurate assessment and determination of this clinical hypothesis (Fig. 4).
Fig. 4.
Qualitative analysis of the relationship between the synthesis material and the bone structure. (A) intimate/grasped relationship between the 7 mm screw and the bone structure. (B) need for a smooth tunnel in the interfragmentary compression technique with the 4.5 mm cortical screw does not allow the same degree of relationship, observed in the 7 mm screw, between the synthesis and the bone structure.
In methodological terms, the great novelty of the present study was the use of FEM in order to compare different fixation methods, analyzing complex biomechanical variables, such as Von Mises peak stress and compression and traction distribution on fractures. Without the use of FEM, such assessments would not be possible. This is the first study to use this effective methodology for biomechanical analysis17,18 in Type II Hoffa fractures. It is important to mention that the lack of the effects of muscles and ligaments on fracture stability and bone quality is a limitation that must be taken into consideration.
5. Conclusion
The 7 mm cannulated screw fixation system has demonstrated the best mechanical results evaluated by FEM in the treatment of Type II Hoffa fracture, producing a decrease in vertical displacement when used retrogradely and in Von Mises peak stress when anterograde.
Ethics approval
This article does not contain any studies with human or animal participants performed by any of the authors.
Data and material availability
Data and materials were accessible in the case system at our department.
Funding
There is no funding to this study.
Declaration of competing interest
All authors declare that they have no conflicts of interest concerning this study.
References
- 1.Zhou Y., Pan Y., Wang Q., Hou Z., Chen W. Hoffa fracture of the femoral condyle: injury mechanism, classification, diagnosis, and treatment. Medicine (Baltim) 2019;98(8) doi: 10.1097/MD.0000000000014633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu Y., Li H., Yang H., Pan Z. A comparison of the clinical effect of two fixation methods on Hoffa fractures. SpringerPlus. 2016;5 doi: 10.1186/s40064-016-2861-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lehrbuch der A.H. Ferdinand Enke- Verlag; Stuttgart: 1904. Frankturen und Luxationen; pp. 451–453. [Google Scholar]
- 4.Patel P.B., Tejwani N.C. The Hoffa fracture: coronal fracture of the femoral condyle a review of literature. J Orthop. 2018;15:726–731. doi: 10.1016/j.jor.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trikha V., Das S., Gaba S., Agrawal P. Analysis of functional outcome of Hoffa fractures: a retrospective review of 32 patients. J Orthop Surg (Hong Kong) 2017;25(2) doi: 10.1177/2309499017718928. 2309499017718928. [DOI] [PubMed] [Google Scholar]
- 6.Letenneur J., Labour P.E., Rogez J.M., Lignon J., Bainvel J.V. [Hoffa’s fractures. Report of 20 cases (author’s transl)] Ann Chir. 1978;32(3-4):213–219. [PubMed] [Google Scholar]
- 7.Meinberg E.G.A.J., Roberts C.S. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32 doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 8.Lu∗ B., Zhao∗ S., Luo Z., Lin Z., Zhu Y. Compression screws and buttress plate versus compression screws only for Hoffa fracture in Chinese patients: a comparative study. J Int Med Res. 2019;47:142–151. doi: 10.1177/0300060518798224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahu R.L., Gupta P. Operative management of Hoffa fracture of the femoral condyle. Acta Med Iran. 2014;52(6):443–447. [PubMed] [Google Scholar]
- 10.Giotikas D., Nabergoj M., Krkovic M. Surgical management of complex intra-articular distal femoral and bicondylar Hoffa fracture. Ann R Coll Surg Engl. 2016;98:e168–170. doi: 10.1308/rcsann.2016.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao M., Tao J., Zhou Z., Liu Q., Du L., Shi J. Surgical treatment and rehabilitation of medial Hoffa fracture fixed by locking plate and additional screws: a retrospective cohort study. Int J Surg. 2015;19:95–102. doi: 10.1016/j.ijsu.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 12.Jarit G.J., Kummer F.J., Gibber M.J., Egol K.A. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B) J Orthop Trauma. 2006;20(4):273–276. doi: 10.1097/00005131-200604000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Singh R., Mahendra M. Functional outcome of isolated Hoffa fractures treated with cannulated cancellous screw. Malays Orthop J. 2017;11(2):20–24. doi: 10.5704/MOJ.1707.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arastu M.H., Kokke M.C., Duffy P.J., Korley R.E., Buckley R.E. Coronal plane partial articular fractures of the distal femoral condyle: current concepts in management. Bone Joint J. 2013;95-b(9):1165–1171. doi: 10.1302/0301-620X.95B9.30656. [DOI] [PubMed] [Google Scholar]
- 15.Gavaskar A.S., Tummala N.C., Krishnamurthy M. Operative management of Hoffa fractures--a prospective review of 18 patients. Injury. 2011;42(12):1495–1498. doi: 10.1016/j.injury.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Becker P.L.S.P., Goulet R. Proceedings of the 67th Annual Meeting of the American Academy of Orthopaedic Surgeons. 2000. Comparative analysis for the fixation of coronal distal intraarticu1ar femur fractures; pp. 15–19. [Google Scholar]
- 17.Noda M., Saegusa Y., Takahashi M., Tezuka D., Adachi K., Naoi K. Biomechanical study using the finite element method of internal fixation in pauwels type III vertical femoral neck fractures. Arch Trauma Res. 2015;4(3) doi: 10.5812/atr.23167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samsami S., Saberi S., Sadighi S., Rouhi G. Comparison of three fixation methods for femoral neck fracture in young adults: experimental and numerical investigations. J Med Biol Eng. 2015;35(5):566–579. doi: 10.1007/s40846-015-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]