Abstract
Objectives
The incidence of hip fractures continues to rise dramatically, but few studies have examined these injuries in the population of individuals over 90 years of age, which is one of the fastest growing populations. We present the largest such study specifically examining hip fractures in the super-elderly.
Methods
A review of 216 hip fracture patients over 90 years of age were examined for immediate postoperative complications and in-house, 30-day, and 1-year mortality.
Results
Overall 1-year mortality was 38.1%. Statistically-significant risk factors for 1-year mortality included oncologic fracture, dementia, and CHF. Fracture classification and hospital length of stay were associated with perioperative complications including anemia and pneumonia.
Conclusion
The nonagenarian hip fracture is associated with a higher 1-year mortality than prior reported rates of mortality for elderly hip fractures. Factors previously reported to influence the risk of 1-year mortality in hip fractures are not observed in the super-elderly.
Keywords: Nonagenarian, Elderly, Hip fracture, Mortality
1. Introduction
Hip fractures in the elderly can be a devastating event. The number of hip fractures in North America has been estimated to be over 320,000 per year and 1,600,000 worldwide per year.1, 2, 3 These numbers are expected to rise sharply as the number of elderly individuals will increase in the coming years. Estimates have projected the total number of hip fractures worldwide at 2.6 million in 2025 and 4.5 million by 2050.4 The morbidity and mortality that result from these fractures are profound and well-documented. The one-year mortality rate after hip fractures in the elderly has been widely studied, and a recent systematic review of the literature describes an overall one-year mortality rate of 21% for all hip fractures sustained after the year 2000.5 By 2040 the estimated premature loss of years of life is expected to be 1.1 million at an overall cost of $47 billion in the United States alone.6
Given the substantial impact to the patient and families as well as the overall burden to the health care industry, many studies have focused on identifying hip fracture patients who are at the highest risk for morbidity and mortality. Age greater than 85 years at the time of fracture has been suggested in several studies as correlative for increased risk of 1-year mortality.7 A study in 2009 reported that patients over the age of 90 accounted for 19% of reported hip fractures, despite representing 0.58% of the wider population.8 Currently, the “oldest-old” population of individuals over 90 is one of the fastest growing age groups in the United States, which has tripled over the past 30 years and is expected to continue to grow rapidly. This portends a dramatic rise in the number of super-elderly hip fractures that the orthopaedic profession will encounter in the coming years. Previous analyses of hip fractures in the 90-plus age group estimate the one-year mortality to be between 9 and 36%, with perioperative complication rates as high as 52%. However, very few studies have specifically examined large numbers of hip fractures in the nonagenarian population.9, 10, 11, 12
The purpose of our study is to examine the morbidity and mortality associated with hip fractures sustained by patients 90 years of age and older at our institution. We aim to examine risk factors that can be identified preoperatively, and treatment-related risks that can potentially be controlled so as to provide prognostic and therapeutic value to patients and their families for these extremely serious injuries.
1.1. Methods
A retrospective review of medical records and public mortality records was performed for patients admitted to our institution between January 1st 2010 and December 31st 2017 with a diagnosis of femoral neck, intertrochanteric, peritrochanteric, or subtrochanteric fracture of the proximal femur. Inclusion criteria were age 90 years or greater. Exclusion criteria were patients with incomplete medical records.
Data collected included demographic data such as age, gender, and residence in an assisted living facility. Medical comorbidities including dementia, chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), congestive heart failure (CHF), atrial fibrillation (AF), and chronic kidney disease (CKD) were documented. Each fracture was classified according to the AO foundation classification system by two board-certified orthopaedic faculty (including senior author and an independent reviewer). Associated pathologic lesions and polytrauma were also recorded. Surgical data including type of procedure and time to surgery were noted. Outcomes recorded were post-operative complications which included arrhythmia, acute kidney insufficiency (AKI), pneumonia, myocardial infarction (MI), and anemia requiring blood transfusion. Mortality outcomes while inpatient, within 30 days, and within 1 postoperative year were documented.
A series of Fischer exact tests were performed to compare mortality rates between isolated hip fractures, pathologic hip fractures, and geriatric polytrauma. Binary logistic regression models were used to evaluate risk factors for mortality during inpatient stay, 30 day, and 1-year intervals. A binary logistic regression model was then constructed for the predictive value of age, gender, American Society of Anesthesiologists (ASA) score, residence in an assisted living facility, fracture type, treatment type, hospital length of stay (LOS), and time to surgery on the development of postoperative complications.
IRB approval was obtained prior to this study.
2. Results
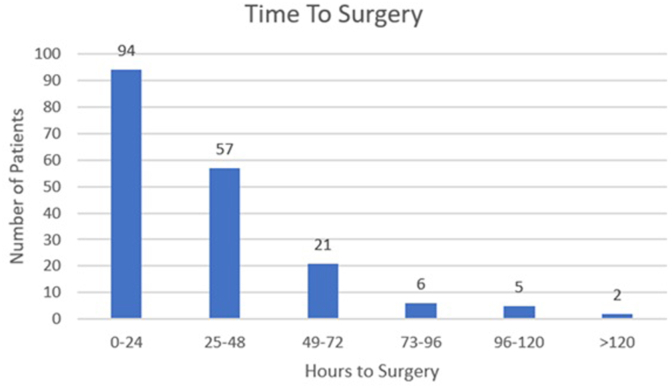
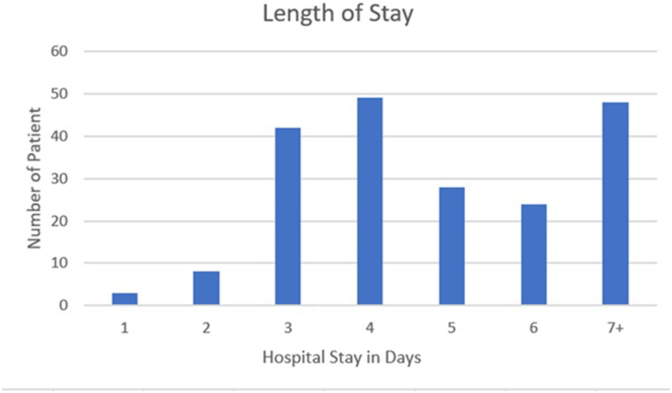
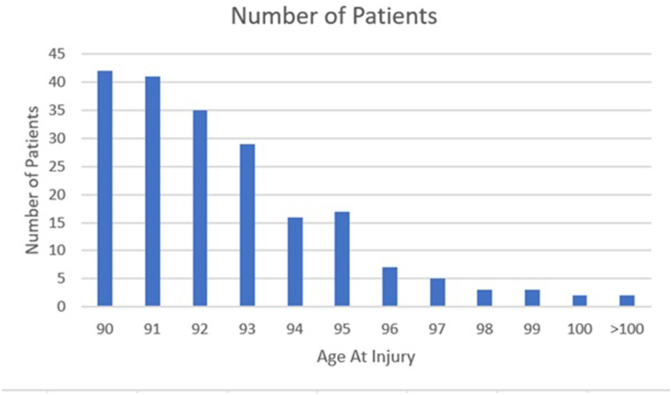
A total of 215 patients were identified. After 13 patients were excluded for inadequate/incomplete records, 202 patients were reviewed. Fractures were isolated in 193 patients, associated with geriatric polytrauma in 6 patients, and oncologic in origin in 3 patients. There were 148 female patients and 54 male patients (74.4% vs. 25.6%). Mean age was 92.6 ± 2.5 years (range 90–103). Mean time to surgery was 33.2 ± 24.7 h (range: 3–132) and mean hospital stay was 5.4 ± 3.2 days (range: 1–31) (Fig. 1, Fig. 2, Fig. 3). Intertrochanteric and peritrochanteric fractures accounted for 144 patients, and femoral neck fractures an additional 58 patients (71.3% vs. 28.7%). The two most prevalent fracture classifications were 31B2.1 and 31A2.2 at 41 (20.2%) and 40 (19.8%) respectively. The complete breakdown of fracture type by OTA classification is included in Table 1.
Fig. 1.
Time to surgery.
Fig. 2.
Hospital length of stay.
Fig. 3.
Patient age at time of injury.
Table 1.
OTA fracture classification of nonagenarian hip fractures.
| FRACTURE PATTERN | OTA CLASSIFICATION | NUMBER OF FRACTURES (n = 202) |
|---|---|---|
| 2-Part Intertrochanteric Fracture | 31A1.2 | 37 (18.3%) |
| Intertrochanteric Fracture with Lesser Trochanter Fracture | 31A1.3 | 33 (16.3%) |
| Peritrochanteric Fracture with Greater and Lesser Trochanter Fracture, 1 Intermediate Fragment | 31A2.2 | 40 (19.8%) |
| Peritrochanteric Fracture with Greater and Lesser Trochanter Fracture, Multiple Intermediate Fragments | 31A2.3 | 27 (13.4%) |
| Simple Reverse Obliquity Fracture | 31A3.1 | 1 (0.5%) |
| Transverse Intertrochanteric Fracture | 31A3.2 | 2 (0.9%) |
| Multifragmentary Reverse Obliquity Fracture | 31A3.3 | 4 (2.0%) |
| Valgus-Impacted Femoral Neck Fracture | 31B1.1 | 8 (4.0%) |
| Nondisplaced Transcervical Femoral Neck Fracture | 31B2.1 | 7 (3.5%) |
| Displaced Transcervical Femoral Neck Fracture | 31B2.1 | 41 (20.3%) |
| Basicervical Femoral Neck Fracture | 31B3 | 2 (0.9%) |
Overall 1-year mortality rate was 38.1% (77/202). In house and 30-day mortality were 3.9% (8/202) and 12.4% (25/202) respectively. We report an overall complication rate of 44.1% (89/202) with anemia requiring transfusion being the most common at 33.2% (66/202) followed by AKI and arrythmia at 5.9% and 5% respectively (Table 2).
Table 2.
Incidence of morbidity and mortality in nonagenarian hip fractures.
| Complication | Incidence | |
|---|---|---|
| Morbidity | Anemia Requiring Transfusion (n = 67) | 33.2% |
| AKI (n = 12) | 5.9% | |
| Arrhythmia (n = 10) | 5.0% | |
| Pneumonia (n = 9) | 4.5% | |
| MI (n = 5) | 2.5% | |
| Overall (n=89) | 44.1% | |
| Mortality | Inpatient Mortality (n = 8) | 4% |
| Discharge to 30-Day (n = 17) | 8.4% | |
| 30-Day to 1-Year (n = 52) | 25.7% | |
| Overall 1-Year (n=77) | 38.1% |
We did not identify statistically significant differences in mortality or complication rates when comparing isolated hip fractures and geriatric polytrauma. When isolated hip fractures and oncogenic pathologic fractures, we did observe a difference in mortality at the 30-day interval and at the 1-year interval (Table 3). There was no difference in perioperative complications between oncologic, polytrauma, and isolated hip fracture groups, but the limited numbers of patients in these series are low and preclude statistical comparison.
Table 3.
Fisher exact test summary for isolated versus geriatric polytrauma and pathologic fractures.
| Isolated Hip Fracture vs: | Geriatric Polytrauma | Pathologic Fracture |
|---|---|---|
| Inpatient Mortality | p > 0.999 | p > 0.999 |
| 30-Day Mortality | P = 0.075 | p=0.018 ∗ |
| 1-Year Mortality | P = 0.67 | p=0.052 |
| Anemia | p > 0.999 | P = 0.552 |
| AKI | p > 0.999 | P = 0.173 |
| Arrhythmia | p > 0.999 | p > 0.999 |
| Pneumonia | p > 0.999 | p > 0.999 |
| MI | p > 0.999 | p > 0.999 |
∗statistically significant.
None of the examined variables demonstrated predictive ability for mortality for inpatient and 30-day mortality. Residence in an assisted living facility (p = 0.032) and increased hospital length of stay (p = 0.032) demonstrated predictability with respect to 1-year mortality. Patients in an assisted living facility were nearly 2.5 times more likely to suffer mortality within one year (95% CI: 1.1, 5.6). Each day of increase in hospital length of stay increased risk of 1-year mortality by 1.2 times (95% CI: 1.0, 1.4). We further observed patients treated with a short nail were 1/5th as likely to suffer mortality at one year (p = 0.014, 95% CI: 0.07, .074) (Table 4).
Table 4.
Summary of logistic regression analysis for 1-year mortality.
| Variable (n) | Odds Ratio | 95% Confidence Interval | p value |
|---|---|---|---|
| Age | .977 | 0.943–1.013 | 0.207 |
| Gender | 1.574 | 0.606–4.085 | 0.352 |
| ASA | 0.756 | 0.312–1.830 | 0.535 |
| Assisted Living (95) | 2.465 | 1.078–5.635 | 0.032 ∗ |
| AO Fx type | 2.945 | 0.479–18.094 | 0.244 |
| Type of Surgery | 0.939 | 0.131–6.727 | 0.950 |
| Short Nail (35) | 0.221 | 0.066–0.742 | 0.014 ∗ |
| Long Nail16 | 0.265 | 0.052–1.350 | 0.110 |
| Hospital LOS | 1.182 | 1.014–1.378 | 0.032 ∗ |
| Time to Surgery | 0.996 | 0.977–1.014 | 0.646 |
| COPD18 | 1.231 | 0.342–4.429 | 0.750 |
| Dementia (73) | 1.354 | 0.568–3.223 | 0.494 |
| CAD (55) | 1.198 | 0.470–3.055 | 0.705 |
| CHF (30) | 0.575 | 0.166–1.987 | 0.382 |
| AF (46) | 0.544 | 0.185–1.598 | 0.268 |
| CKD (37) | 1.017 | 0.387–2.671 | 0.973 |
∗statistically significant.
None of the variables analyzed demonstrated predictive ability for the development of postoperative arrhythmia or AKI. Intertrochanteric fractures were predictive for postoperative anemia requiring transfusion (p = 0.023). Patients with intertrochanteric fractures were 9x more likely to require blood transfusion than patients with femoral neck fractures (95% CI: 1.4, 61.1). Hospital length of stay was found to be a predictor of myocardial infarction (p = 0.045); with each day of increase in hospital LOS patients associated with a 2-fold increase in risk of MI (95% CI: 1.0, 4.1). Significant risk factors for the development of perioperative pneumonia included femoral neck fractures (p = 0.024), treatment with a long nail (p = 0.037), and increased hospital length of stay (p = 0.01). For every 1-day increase in length of stay, patients were 1.8 times as likely to develop pneumonia (95% CI: 1.2, 2.9). These results are summarized in Table 5.
Table 5.
Summary of logistic regression analysis for perioperative morbidity.
| Variable | Anemia | AKI | Arrhythmia | Pneumonia | MI |
|---|---|---|---|---|---|
| Age | p = 0.568 | P = 0.214 | P = 0.757 | p = 0.697 | p = 0.459 |
| Gender | p = 0.476 | P = 0.195 | P = 0.069 | p = 0.167 | p = 0.572 |
| ASA | p = 0.301 | P = 0.104 | P = 0.631 | p = 0.304 | p = 0.994 |
| Assisted Living | P = 0.825 | P = 0.870 | P = 0.391 | p = 0.619 | p = 0.544 |
| Fx type | P = 0.023 ∗ (IT) | P = 0.724 | P = 0.996 | p = 0.024 ∗(Fem Neck) | p = 0.998 |
| Type of Surgery | p = 0.241 | P = 0.314 | P = 0.360 | p = 0.999 | p = 0.120 |
| Short Nail | P = 0.165 | P = 0.993 | P = 0.996 | p = 0.088 | p = 0.996 |
| Long Nail | P = 0.242 | P = 0.226 | P = 0.996 | p = 0.037 ∗ | p = 0.959 |
| Hospital LOS | P = 0.373 | P = 0.278 | P = 0.208 | p = 0.010 ∗ | p = 0.045 ∗ |
| Time to Surgery | P = 0.432 | P = 0.271 | P = 0.476 | p = 0.304 | p = 0.488 |
| COPD | P = 0.883 | P = 0.357 | P = 0.936 | p = 0.290 | p = 0.998 |
| Dementia | P = 0.438 | P = 0.914 | P = 0.470 | p = 0.060 | p = 0.509 |
| CAD | P = 0.062 | P = 0.305 | P = 0.359 | p = 0.439 | p = 0.295 |
| CHF | P = 0.455 | P = 0.959 | P = 0.631 | p = 0.833 | p = 0.996 |
| AF | P = 0.062 | P = 0.513 | P = 0.790 | p = 0.070 | p = 0.613 |
| CKD | P = 0.140 | P = 0.225 | P = 0.077 | p = 0.113 | p = 0.185 |
∗statistically significant.
3. Discussion
We observed an overall 1-year mortality of 38.1% for nonagenarian hip fracture patients in our study. This is toward the upper limits of prior reporting for nonagenarian hip fractures (9–46%), and higher than the reported risk for elderly hip fractures overall.9, 10, 11, 12,19,21,22 We found comparable rates of in-house mortality (4.5%) and 30-day mortality (12.4%) compared to prior investigations (2–10.3%, and 3.7–18.7% respectively).9, 10, 11,20,22,23 This confirms that age over 90 years is a predictive risk factor for mortality after hip fracture.
Other risk factors for mortality after hip fracture are inconsistently reported in prior studies. ASA score, dementia, and extracapsular fracture locations have been the most frequently reported in prior studies, but none of these factors achieved statistical significance in our series.9, 10, 13, 14, 15, 17, 18, 20 Additional variables examined in our study included age, gender, COPD, CAD, atrial fibrillation, CKD, CHF, and surgical procedure, none of which demonstrated significance. Our validated risk factors for 1-year mortality included pathologic hip fractures, residence in an assisted living facility, and increasing length of hospital stay. These results suggest that for patients over the age of 90, the injury itself is the greatest threat to life, and that specific demographics, fracture types, surgical procedures, and comorbidities that are observed to affect outcomes in younger patients are less impactful within this cohort.15, 16 One potential limitation to this approach is our examination of individual comorbidities, which is rarely a comprehensive evaluation of the myriad comorbid conditions with which a nonagenarian potentially presents. As such, the complexity of care in the super elderly population may render analysis by discrete variables inherently unreliable. Future investigations in the super elderly are likely to benefit from prospective analysis of more comprehensive comorbidity indices such as the Acute Physiology and Chronic Health Evaluation (APACHE), Deyo-Charlson Comorbidity Index (DCCI) or Elixhauser-van Walraven Comorbiditiy Index (EVCI) scores.10 Correlating outcomes to a scale of values that summarize the overall health status of elderly patients may provide greater prognostic information at the time of initial presentation.
In examining fracture patterns in the nonagenarian population, we observed a preponderance of displaced and multi-fragmentary fracture patterns compared to simple and stable fracture patterns. Without historical data for comparison, we cannot comment on this finding definitively, but we suspect that higher severity fracture patterns predominate in the super-elderly population.
We demonstrated a decrease in 1-year mortality risk comparing short cephalomedullary nails to long nails. This is a curious finding for which we cannot provide a definitive explanation. We theorize that shorter devices may be selected preferentially for less severe fracture patterns, may have shorter operative times, or may be associated with less pressurization of the femoral canal and less marrow embolization compared to longer reamed nails. None of these hypotheses are validated in our analysis of related variables, except an elevated risk of postoperative pneumonia observed with longer nails.
The nonagenarian hip fracture population is at notable risk for perioperative morbidity. We observed an overall perioperative complication rate of 44.1%, with anemia requiring transfusion the most common postoperative complication (33.2%). Compared to femoral neck fractures, intertrochanteric fractures were associated with an elevated risk of postoperative pneumonia, and a 9x higher risk of anemia requiring blood transfusion. Hospital length of stay was also associated with postoperative morbidity; the risk of myocardial infarction is increased 2-fold, and the risk of hospital-acquired pneumonia increased 1.8x for every 1-day increase in hospital stay.
Limitations of our study include its retrospective design, analysis of discrete rather than continuous variables, and inability to correlate morbidity and mortality with long-term functional outcomes. Future investigations should include prospective, standardized data collection, documentation of pre-injury functional status, and diligent postoperative medical and functional assessments for a minimum of 1 year after injury.
4. Conclusion
To our knowledge, this study is the largest investigation of nonagenarian hip fractures reported. We observed an overall mortality rate of 38.1% at one year. This is higher than the 1-year mortality rate of 20–30% observed for all elderly hip fractures. The elevated risk of morbidity and mortality after hip fracture in the nonagenarian population should be recognized by the provider and communicated with the patient, family, and geriatric care team. Residence in an assisted living facility, longer hospital stays, and pathologic fractures are associated with elevated risks of mortality. Many other factors previously reported to influence the risk of 1-year mortality in hip fractures are not observed in the super-elderly, which may be reflective of the cumulative medical and physical frailty in this rapidly-growing population segment. Our observed medical complication rate of 44% further demands that this patient population receive diligent peri-operative management.
Level of evidence
Level III.
Funding
No external funding was used for this research and the above authors have no legal or financial disclosures.
Ethical review committee statement
Studies have been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki.
All studies have been carried out in accordance with relevant regulations of the US Health.
Insurance Portability and Accountability Act (HIPAA). Details that might disclose the identity of the subjects under study have been omitted.
Declaration of competing interest
None.
Contributor Information
Dane Bolton, Email: dbolton@wellspan.org.
Matthew T. Wallace, Email: matthew.t.wallace@medstar.net.
References
- 1.Cooper C., Campion G., Melton L.J. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(96):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 2.Schemitsch E., Bhandari M. Femoral neck fractures: controversies and evidence. J Orthop Trauma. 2009;23(6):385. doi: 10.1097/BOT.0b013e3181acc51f. [DOI] [PubMed] [Google Scholar]
- 3.Johnell O., Kanis J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 4.Chang K., Center J. Incidence of Hip and other osteoporotic fractures in elderly men and women: dubbo osteoporosis epidemiology study. J Bone Miner Res. 2004;19(4):532–536. doi: 10.1359/JBMR.040109. [DOI] [PubMed] [Google Scholar]
- 5.Mundi S., Pindiprolu B. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop. 2014;85(1):54–59. doi: 10.3109/17453674.2013.878831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braithwaite R., Col N., Wong J. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51:364–370. doi: 10.1046/j.1532-5415.2003.51110.x. [DOI] [PubMed] [Google Scholar]
- 7.Smith T., Pelpola K. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age and Aging. 2014;43(4):464–471. doi: 10.1093/ageing/afu065. [DOI] [PubMed] [Google Scholar]
- 8.Court-Brown C.M., Clement N. Four score and ten an analysis of the epidemiology of fractures in the very elderly. Injury Int J. Care Injured. 2009;40:1111–1114. doi: 10.1016/j.injury.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Ovidiu A., Stefan G. Survival of nonagenarian patients with hip fractures: a cohort study. Acta Ortopédica Bras. 2017;25(4):132–136. doi: 10.1590/1413-785220172504167561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fansa A., Huff S., Ebraheim N. Prediction of mortality in nonagenarians following the surgical repair of hip fractures. Clin Orthop Surg. 2016;8:140–145. doi: 10.4055/cios.2016.8.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang B., Lee Y. Mortality after hip fractures in nonagenarians. J Bone Metab. 2012;19(2):83–86. doi: 10.11005/jbm.2012.19.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ooi L.H., Wong T.H., Wong H.P. Hip fractures in nonagenarians-a study on operative and non-operative management. Injury, Int. J. Care Injured. 2005;36:142–147. doi: 10.1016/j.injury.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 13.Jiang H., Majumdar S. Development and initial validation of a risk score for predicting in hospital and 1 year mortality in patients with hip fractures. J Bone Miner Res. 2009;20(3):494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 14.Rogers F., Shackford S. Early fixation reduces morbidity and mortality in elderly patients with hip fractures from low impact falls. J of Trauma and Acute care surgery. 1995;39(2):261–265. doi: 10.1097/00005373-199508000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Lefaivre K.A., Macadam S.A. Length of stay, mortality, morbidity and delay to surgery in hip fractures. JBJS. 2009;91-B(7):922–927. doi: 10.1302/0301-620X.91B7.22446. [DOI] [PubMed] [Google Scholar]
- 16.Gdalevich M., Cohen D. Morbidity and mortality after hip fracture: the impact of operative delay. Archives of Orthop and Trauma surgery. 2004;124(5):334–340. doi: 10.1007/s00402-004-0662-9. [DOI] [PubMed] [Google Scholar]
- 17.Hu F., Jiang C. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury, Int. J. Care Injured. 2012;43:676–685. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 18.Kadowaki M., Kono M. Mortality in patients with hip fracture aged over 90 years: a report from a progressively aging island. Arch Gerontol Geriatr. 2012;54(2):113–117. doi: 10.1016/j.archger.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Kerkhove M.P., Anthenunis P.S. Hip fractures in nonagenarians: perioperative mortality and survival. Injury, Int J. Care Injured. 2008;39:244–248. doi: 10.1016/j.injury.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Jennings A.G., de Boer P. Should we operate on nonagenarians with hip fractures? Injury Int. j Care Injured. 1999;30:169–172. doi: 10.1016/s0020-1383(98)00249-6. [DOI] [PubMed] [Google Scholar]
- 21.Tay Y., Hong C. Functional outcome and mortality in nonagenarians following hip fracture surgery. Archives of orthop and trauma surgery. 2014;134(6):765–772. doi: 10.1007/s00402-014-1982-z. [DOI] [PubMed] [Google Scholar]
- 22.Miller A., Bercik M. Nonagenarian hip fracture: treatment and complications. J Trauma. 2012;72(5):1411–1415. doi: 10.1097/TA.0b013e318246f3f8. [DOI] [PubMed] [Google Scholar]
- 23.Graver A., Merwin S. Comorbid profile rather than age determines hip fracture mortality in a nonagenarian population. HSS J. 2015;11:223–235. doi: 10.1007/s11420-015-9435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]