Abstract
Introduction
Improper cup positioning and leg length discrepancy (LLD) are two of the most common errors following total hip arthroplasty (THA) and are associated with potentially significant consequences. Obesity is associated with increased risk of mechanical complications, including dislocations, which may be secondary to cup malposition and failure to restore leg length and offset. 3D Optical Camera computerassisted navigation (CAN) system may reduce the risk of component malposition and LLD with real time intraoperative feedback. The aim of this study was to investigate whether the use of CAN influences acetabular component placement (CP) accuracy and leg length restoration in obese (body mass index(BMI)≥35kg/m 2 ) patients undergoing primary THA.
Methods
A multi-center retrospective review was conducted identifying consecutive THA cases with BMI > 35kg/m 2 using CAN (Intellijoint Hip, Waterloo, CA) from 2015-2019. These patients were then matched with patients undergoing conventional THA (control) at a 1:1 ratio according to BMI, American Society of Anesthesiologists score, and gender. TraumaCad™ software (Brainlab, Chicago, IL) was used to measure cup anteversion, inclination, and change (Δ) in LLD between pre- and postoperative radiographic images. The safety target zones used as reference for precision analysis of CP were 15°-30° for anteversion and 30°-50° for inclination.
Results
176 patients were included: 88 CAN and 88 control cases. CAN cases were found to have a lower ΔLLD than controls (3.53±2.12mm vs. 5.00±4.05mm; p=0.003). Additionally, more CAN cases fell within the target safe zone than controls (83% vs.60%, p=0.00083).
Conclusion
Our findings suggest that the use of a CAN system may be more precise in component placement, and useful in facilitating the successful restoration of preoperative leg length following THA than conventional methodology.
1. Introduction
Total hip arthroplasty (THA) is a highly successful treatment for hip osteoarthritis (OA). While generally associated with positive results, errors in cup positioning (CP), defined as anteversion and inclination, and failure to restore equal leg lengths (LL) can lead to potentially significant consequences, such as post-operative complaints of low back pain, neurological deficits, and overall patient dissatisfaction.1 Furthermore, acetabular component malpositioning increases the risk of dislocation and the likelihood of early revision surgery.1, 2, 3, 4, 5
An important factor linked to adverse outcomes and acetabular component malpositioning is obesity, which has been associated with increased overall complication rate, increased dislocation rate, and inferior functional outcome after primary THA compared to non-obese counterparts.6 Callanan et al. found a 1.3-fold increased risk for cup malpositioning in patients with a body mass index (BMI) > 30 kg/m2 compared to patients in the lower BMI groups.7 Elson et al. demonstrated a similar impact on CP in morbidly obese patients (BMI > 35 kg/m2) showing a significant trend towards decreased anteversion and greater abduction angles in the morbidly obese cohort compared to patients with BMI < 25 kg/m28
Conventional methods for LL and CP are susceptible to limited visibility of anatomic landmarks, intraoperative movement, and mainly rely on surgeon experience, and for this reason have variable accuracy. In order to address these limitations, enabling technologies have evolved with the goal of increasing accurate CP and reducing outliers. Numerous studies have shown the efficacy of imageless computer-assisted navigation (CAN) in increasing the accuracy of CP, without significantly increasing surgical time.9, 10, 11, 12 However, imageless CAN for THA has been found to be less accurate in obese patients, likely due to difficulty in accurate registration of the software with increased adiposity over bony surfaces.13,14
One surgical navigation tool currently available is the CAN HIP (Intellijoint Surgical, Inc, Waterloo, ON, Canada). This is a guidance tool which provides real-time data on LL/CP to the surgeon and allows for immediate feedback on component positioning and leg length. Cadaveric studies with CAN showed that the device was accurate when evaluated with CT scans pre- and post-op, with cup position within one degree for anteversion and inclination and a mean difference for LL of 0.27 mm.15 CAN use in THA patients has also been found to be accurate when compared to conventional guides in terms of anteversion, inclination and LLD.16, 17, 18, 19, 20 However, no study to date, has investigated the validity of this navigation system for patients with a higher BMI.
Given the high volume of THA performed yearly, the increasing revision burden, and the rising rate of obesity, it is imperative precautions are taken to minimize the risk of component malpositioning, especially in this higher-risk populations. The purpose of this study is to evaluate the efficacy of using CAN on the acetabular component positioning and residual LLD in patients with a BMI ≥ 35 kg/m2. We hypothesize that the use of this imageless navigation tool would increase the accuracy of CP and decrease the LLD in primary THA when compared to non-navigated THA.
2. Methods
2.1. Study design and patient population
A multi-center retrospective review at two high-volume, urban, academic institutions was performed identifying consecutive patients with a BMI above or equal to 35 kg/m2 who underwent an elective primary THA, through the mini-posterior approach, using a navigation system from January 2015 to June 2019. Patients qualified for eligibility if they were greater than or equal to 18-years-old, had a BMI greater than or equal to 35, were undergoing an elective primary THA due to primary OA, and had pre- and post-op X-rays available. Patients were excluded if they were less than 18-years-old, had a BMI less than 35, if pre-op or post-op X-rays were not available, or if they presented for THA due to any cause other than primary OA such as developmental dysplasia of the hip, traumatic causes, or rheumatoid arthritis. Patients in the experimental group were excluded if the CAN system was removed for any reason during the operation or if there was any instability in the pelvic CAN platform such that accurate measurements were not obtainable. In an attempt to control for the amount of preoperative acetabular defects and damage that may impact final cup placement of our cases, we have only included primary THA patients and excluded all revisions and conversion cases. As such, all of our cases received primary acetabular cup implants since none had any significant acetabular defects (Paprosky classification type 1).
The variables that were collected in the study were: cup anteversion, cup inclination, LLD between pre- and post-operative radiographic (AP pelvis) x-rays two to six weeks post-surgery, and baseline patient characteristics such as age, BMI, sex, and American Society of Anesthesiologists (ASA) score. Each of the experimental cases were then matched with control cases using non-navigation assisted approach at a 1:1 ratio according to patient demographics, specifically age, BMI, ASA, and sex. The primary outcome of the study was to compare CP based on cup anteversion and inclination between CAN cases and conventional THA. LLD was also compared between pre and post-op X-rays. All de-identified data was collected using Microsoft Excel software.
2.2. Analysis plan
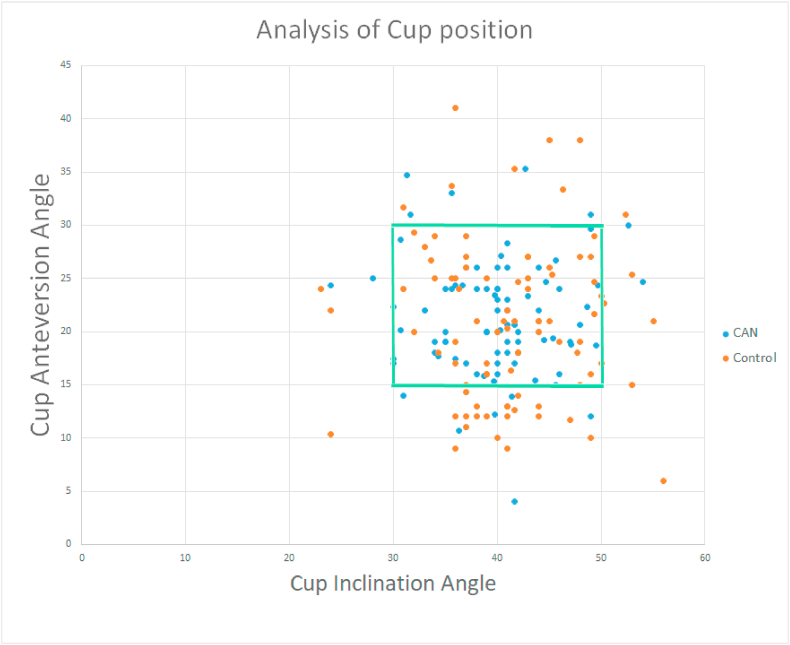
TraumaCad™ software (Brainlab, Chicago, IL) was used to measure cup anteversion, inclination, and LLD. Each of these measurements were taken by three raters independently and averaged. The average cup measurements and LLD were then used in our final analysis. Cup position accuracy was determined according to surgeon preference safe zone with an anteversion angle between 15° and 30° and an inclination angle between 30° and 50° (Fig. 1).
Fig. 1.
Analysis of CP in reference to surgeon safety zone.
2.3. Statistical analysis
Independent sample, two-sided t-tests were used to determine any significant differences between continuous variables, including age, BMI, ASA, and cup measurements (anteversion, inclination, and LLD). Chi-squared tests were used to detect any differences among categorical variables such as demographic data, and cup position analysis. Lastly, an intraclass correlation coefficient (ICC) was used to compare cup anteversion, inclination, and LLD among raters. All statistical analyses and calculations were performed using SPSS v25 (IBM Corporation, Armonk, New York). A p-value of less than 0.05 was used to determine the statistical significance of a finding. An ICC of more than 0.75 was deemed good to excellent.21
3. Results
A total of 176 eligible patients were identified in this study. 88 THA patients were identified using the CAN system while 88 THA patients were identified without navigation assistance for the control group. The CAN cohort was comprised of 40.91% females and 59.09% males with an average age of 56.6 (±11.3) years, average BMI of 39.47 (±4.21) kg/m2, and ASA of 2.52 (±0.57. The control group also consisted of 42.05% females and 57.59% males with an average age of 58.51 (±10.5) years, average BMI of 38.50 (±3.24) kg/m2, and ASA of 2.55 (±0.53). There was no statistically significant difference in any of the baseline patient characteristics found between CAN and control cases (Table 1).
Table 1.
Patient Characteristics and Surgeon, represented as means (±SD) or counts (%).
| Variables | CAN (n = 88) | Control (n = 88) | p-value∗ |
|---|---|---|---|
| Age (years) | 56.6 (±11.3) | 58.41 (±10.5) | 0.43 |
| BMI (kg/m2) | 39.47 (±4.21) | 38.50 (±3.24) | 0.09 |
| ASA | 2.52 (±0.57) | 2.55 (±0.53) | 0.79 |
| Gender | 0.88 | ||
| Male | 52 (59.09%) | 51 (57.95%) | |
| Female | 36 (40.91%) | 37 (42.05%) |
∗p-values derived from two tail t-test or chi-squared for categorical values.
When comparing cup measurements in patients with BMI ≥35 kg/m2 between CAN and control groups, our results show that pre-op and post-op ΔLLD was significantly more accurate in the navigated group compared to non-navigated. The residual post-operative LLD was 1.5 mm more accurate in CAN cases (3.53 mm ± 2.12 vs 5.00 mm ± 4.05, p = 0.003) compared to non-navigated cases. When using the surgeon preference safe zone as a reference for precision analysis of CP, there was a significant difference in improved safe zone placement for the navigated group. CAN cases fell within the safe zone in 83% of cases versus 60% of control cases (p < 0.01), see Table 3 and Fig. 1. There was no statistically significant difference in mean cup anteversion (21.27° ± 5.27 vs 20.81° ± 7.38, p = 0.64) or mean inclination (39.96° ± 5.69 vs 41.2° ± 6.66, p = 0.19) in CAN vs. control (Table 2).
Table 3.
Precision analysis of CP in surgeon safety zone.
| Precision analysis of Cup Position: Computer Navigation vs Conventional | |||
|---|---|---|---|
| Computer Navigation | Control | p-value | |
| n = 88 | n = 88 | ||
| Within Surgeon Preference zone | 0.00088 | ||
| Yes (%) | 73 (83%) | 53 (60%) | |
| No (%) | 15 (17%) | 35 (40%) | |
Table 2.
Bivariate comparison between cup anteversion, inclination, and LLD between CAN and controls (i.e. surgical experience), represented as means (±SD).
| Variables | CAN (n = 88) | Control (n = 88) | p-value∗ |
|---|---|---|---|
| Cup anteversion | 21.27° (±5.27) | 20.81° (±7.38) | 0.64 |
| Cup inclination | 39.96° (±5.69) | 41.2° (±6.66) | 0.19 |
| Leg length difference (LLD) between pre-op and post-op THA | 3.53 mm (±2.12) | 5.00 mm (±4.05) | 0.003 |
4. Discussion
Primary THA for the management of moderate-to-severe hip OA is a common and very successful procedure resulting in significant pain relief and functional improvement for the majority of patients.1, 2, 3, 4, 5 Obesity is associated with increased rate of medical and mechanical complications, including dislocations, which may be secondary to cup malposition and failure to restore leg length, with potentially serious complications.6, 7, 8 Although THA is generally associated with excellent clinical outcomes, a non-insignificant percentage of patients who undergo traditional THA may report some degree of symptom, including low back pain from persistent LLD, or experience a more significant complication such as hip dislocation which may become recurrent and lead to revision surgery.22 Conventional methods of restoring leg length and offset rely on preoperative templating and intraoperative landmarks but are susceptible to patient position changes or limited intra-operative visualization. For this reason, obesity has been associated with increased risk of LL/CP. CAN systems have been incorporated into THA for the past 2 decades but there is little literature on the impact of computer navigation on obese patients. As registration methods are different between different CAN systems, the impact of BMI may be variable. A novel imageless CAN system which a pelvic platform and 3D optical camera (CAN HIP) may improve acetabular component placement and minimize post-operative LLD with real-time data intraoperatively. However, the CAN system reported in our study has not been evaluated in patients with BMI above or equal to 35 kg/m2. The purpose of this study was to evaluate the use of CAN in patients with BMI greater than or equal to 35 kg/m2 and its effect on CP and LLD compared to a matched group of patients undergoing THA with conventional techniques.
Our study found no significant difference in CP for mean anteversion (21.27° ± 5.27 in CAN cases vs 20.81° ± 7.38 in control, p = 0.64) and mean inclination (39.96° ± 5.69 vs 41.2° ± 6.66, p = 0.19) between CAN and control cases. This finding is supported by other studies found in the literature. Moskal et al. conducted a study comparing CP in CAN cases and controls and found no significant difference between cohorts in regards to cup anteversion (20.11° vs 20.24°, p = 0.9672) and inclination (42.65° vs 43.57°, p = 0.5686).23 On the other hand, Sendtner et al. conducted a study to compare CP between cases using minimally-invasive computer-assisted navigation and traditional cases and found statistical difference in regards to inclination (42.3° vs 37.9°, p = 0.002) but not for anteversion (24.5° vs 23.8°, p = 0.739) in CAN compared to conventional method.24
Our study also looked at pre- and post-op ΔLLD and found an accuracy difference of about 1.5 mm between CAN and traditional cases (LLD was 3.53 mm in CAN THA vs 5.00 mm in traditional THA, p = 0.003) but difference was not statistically significant, p = 0.003. However, there is some disagreement about pre- and post-op ΔLLD in which some studies found a difference in LLD while others did not.22,25,26 Manzotti et al. conducted a study comparing CAN to non-navigational methods showing a significant difference in LLD favoring CAN cases at about the same difference of 2 mm (5.06 mm vs 7.64 mm, p = 0.0043).25 Ellapparadja et al. found similar results supporting CAN cases as well, but at a greater difference of 4 mm (3 mm vs 6.9 mm, p = 0.001).26 On the other hand, Paprosky et al. conducted a study that compared CAN vs non-CAN use in THA cases and found LLD favoring traditional cases, although not statistically significant (2.0 mm vs 1.2 mm, p = 0.66).22 While there is disagreement about LLD in the literature, the results of our study suggest that CAN use may help to facilitate the successful restoration of pre-op leg length following THA. While this difference is unlikely to be clinically significant, we found that patients in the control group were more likely to have a LLD >5 mm, suggesting that these results may have greater clinical impact.26,27
In addition to studying the differences between CP and LLD in CAN vs control cases, our study also looked at the precision analysis of CP in reference to the surgeon safety target zone (15°–30° for anteversion and 30°–50° for inclination). Our results found that a higher proportion of CAN cases fell within the safe zone compared to conventional cases (83% vs 60%, p < 0.01). These findings are consistent with those found in the literature which favors CAN cases. Suksathien et al. found significant differences in the percentage of anteversion within the safe zone using imageless navigation compared to freehand technique in patients with an average BMI of 22 kg/m2 (100% vs 51.6%, p < 0.001).28
4.1. Limitations
There are several limitations to our study. The retrospective design exposes our study to selection bias, which may limit the demographic variability and diversity of the cases we selected. To counter this issue, we matched our cases by age, BMI, gender, and ASA at a 1:1 ratio and our analysis showed no significant differences in patient characteristics in either cohort. Moreover, this limits our ability to select and control for surgeon, which may affect the results of the traditional cases that rely on surgeon experience. Most importantly, the observational nature of our study may limit the interpretation of our results on CP and LLD due to the limited accuracy of x-ray imaging and errors that can be made with subjective measurements.29,30 Despite these limitations, post THA measurements using plain radiographs have been shown to be reliable and reproducible.31 Kjellberg et al. reported excellent inter-observer reliability (mean ICC of 0.83) and intra-observer reproducibility for LLD measurement on plain radiographs (ICC of 0.90 and 0.88).31 To that effect, our results have also shown great inter-observer reliability using a similar methodology for pre and post-op THA radiographs as evident by our ICC for each of our measurements (ICC of 0.99 for both anteversion and inclination in CAN cases and controls, ICC of 0.799 and 0.801 for LLD in CAN cases and controls, respectively). Other limitations include possible differences of intra-operative use of the navigation system among operating surgeons. While we consider the inclusion of data from multiple centers to be a strength of our study, we acknowledge that this may also introduce other biasness that we may not have accounted for as a result of the differences between institutions. These biases may include differences in operating facilities and surgical expertise, especially in regards to training and surgical skill. Although these limitations exist, our study suggest that the use of a CAN system may be more precise in component placement, and useful in facilitating the successful restoration of pre-operative leg length following THA than conventional methodology.
5. Conclusion
The use of computer-assisted navigation program for CP and LLD in obese patients (BMI greater than or equal to 35 kg/m2) undergoing primary THA improved post-op LLD accuracy 1.5 mm, suggesting that CAN use may help to facilitate the successful restoration of pre-op leg length following THA. While this difference is unlikely to be clinically significant, patients in our control group were more likely to have a LLD >5 mm which has been shown to have clinical consequences. Our findings also suggest that the use of a CAN system is more precise in surgeon “safe zone” component placement following THA compared to conventional methodology in patients with BMI ≥ 35 kg/m2.
Contributor Information
Mohamad Sharan, Email: dr.msharan@yahoo.com.
Ran Schwarzkopf, Email: ran.schwarzkopf@nyulangone.org.
References
- 1.Malik A., Maheshwari A., Dorr L.D. Impingement with total hip replacement. J Bone Jt Surg. 2007;89(8):1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 2.Oki H., Ando M., Omori H. Relation between vertical orientation and stability of acetabular component in the dysplastic hip simulated by nonlinear three-dimensional finite element method. Artif Organs. 2004;28(11):1050–1054. doi: 10.1111/j.1525-1594.2004.00017.x. [DOI] [PubMed] [Google Scholar]
- 3.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 4.Masaoka T., Yamamoto K., Shishido T. Study of hip joint dislocation after total hip arthroplasty. Int Orthop. 2006;30(1):26–30. doi: 10.1007/s00264-005-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nishii T., Sugano N., Miki H., Koyama T., Takao M., Yoshikawa H. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty. 2004;19(2):162–166. doi: 10.1016/j.arth.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Liu W., Wahafu T., Cheng M., Cheng T., Zhang Y., Zhang X. The influence of obesity on primary total hip arthroplasty outcomes: a meta-analysis of prospective cohort studies. Orthop Traumatol Surg Res. 2015 doi: 10.1016/j.otsr.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Callanan M.C., Jarrett B., Bragdon C.R. The john charnley award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469(2):319–329. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elson L.C., Barr C.J., Chandran S.E., Hansen V.J., Malchau H., Kwon Y.M. Are morbidly obese patients undergoing total hip arthroplasty at an increased risk for component malpositioning? J Arthroplasty. 2013;28(8 SUPPL):41–44. doi: 10.1016/j.arth.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 9.Lass R., Kubista B., Olischar B., Frantal S., Windhager R., Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29(4):786–791. doi: 10.1016/j.arth.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 10.Biedermann R. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty [9] J Bone Jt Surg Ser A. 2007;89(8):1869. doi: 10.2106/00004623-200708000-00035. [DOI] [PubMed] [Google Scholar]
- 11.Moskal J.T., Capps S.G. Acetabular component positioning in total hip arthroplasty: an evidence-based analysis. J Arthroplasty. 2011;26(8):1432–1437. doi: 10.1016/j.arth.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Christ A., Ponzio D., Pitta M., Carroll K., Muir J.M., Sculco P.K. Minimal increase in total hip arthroplasty surgical procedural time with the use of a novel surgical navigation tool. Open Orthop J. 2018;12(1):389–395. doi: 10.2174/1874325001812010389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsukada S., Wakui M. Decreased accuracy of acetabular cup placement for imageless navigation in obese patients. J Orthop Sci. 2010;15(6):758–763. doi: 10.1007/s00776-010-1546-1. [DOI] [PubMed] [Google Scholar]
- 14.Buller L.T., McLawhorn A.S., Romero J.A., Sculco P.K., Mayman D.J. Accuracy and precision of acetabular component placement with imageless navigation in obese patients. J Arthroplasty. 2019 doi: 10.1016/j.arth.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Vigdorchik J.M., Cross M.B., Bogner E.A., Miller T.T., Muir J.M., Schwarzkopf R. A cadaver study to evaluate the accuracy of a New 3D mini-optical navigation tool for total hip arthroplasty. Surg Technol Int. 2017;30:447–454. [PubMed] [Google Scholar]
- 16.Muir J.M., Vincent J., Schipper J., Govindarajan M., Paprosky W.G. Evaluation of tilt-correction of anteversion on anteroposterior pelvic radiographs in total hip arthroplasty. Cureus. 2018;10(5) doi: 10.7759/cureus.2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grosso P., Snider M., Muir J.M. A smart tool for intraoperative leg length targeting in total hip arthroplasty: a retrospective cohort study. Open Orthop J. 2016;10(1):490–499. doi: 10.2174/1874325001610010490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pitta M., Ponzio D., Mayman D., Jerabek S., Sculco P. AAOS Annual Meeting Las Vegas. 2019. Validation of a novel optical surgical navigation system for total hip arthroplasty. NV. [Google Scholar]
- 19.Pitta M., Ponzio D., Mayman D., Jerabek S., Sculco P. 13th Congress of European Hip Society. 2018. Validating the accuracy of a novel computer-assited system using two-dimensional and three-dimensional radiographic analysis. The Hague, Netherlands. [Google Scholar]
- 20.Wolfstadt J., Amenabar T., Safir O., Backstein D., Gros A., Kuzyk P. The Combined Meeting of American Orthopedic Association and the Canadian Association. 2014. An intelligent instrument for improved leg length and hip offset accuracy in total hip arthroplasty. Montreal, Quebec. [Google Scholar]
- 21.Cicchetti D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. doi: 10.1037/1040-3590.6.4.284. [DOI] [Google Scholar]
- 22.Paprosky W.G., Muir J.M. Intellijoint HIP®: a 3D mini-optical navigation tool for improving intraoperative accuracy during total hip arthroplasty. Med Devices (Auckl) 2016;9:401–408. doi: 10.2147/MDER.S119161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moskal J.T., Capps S.G. Acetabular component positioning in total hip arthroplasty: an evidence-based analysis. J Arthroplasty. 2011;26(8):1432–1437. doi: 10.1016/j.arth.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Sendtner E., Schuster T., Wörner M., Kalteis T., Grifka J., Renkawitz T. Accuracy of acetabular cup placement in computer-assisted, minimally-invasive THR in a lateral decubitus position. Int Orthop. 2011 doi: 10.1007/s00264-010-1042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manzotti A., Cerveri P., De Momi E., Pullen C., Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop. 2011;35(1):19–24. doi: 10.1007/s00264-009-0903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellapparadja P., Mahajan V., Atiya S., Sankar B., Deep K. Leg length discrepancy in computer navigated total hip arthroplasty - how accurate are we? HIP Int. 2016;26(5):438–443. doi: 10.5301/hipint.5000368. [DOI] [PubMed] [Google Scholar]
- 27.Sykes A., Hill J., Orr J. Patients’ perception of leg length discrepancy post total hip arthroplasty. HIP Int. 2015;25(5):452–456. doi: 10.5301/hipint.5000276. [DOI] [PubMed] [Google Scholar]
- 28.Suksathien Y., Suksathien R., Chaiwirattana P. Acetabular cup placement in navigated and non-navigated total hip arthroplasty (THA): results of two consecutive series using a cementless short stem. J Med Assoc Thail. 2014;97(6) [PubMed] [Google Scholar]
- 29.Sabharwal S., Kumar A. vol. 466. Springer; New York: 2008. Methods for assessing leg length discrepancy; pp. 2910–2922. (Clinical Orthopaedics and Related Research). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sabharwal S., Zhao C., McKeon J.J., McClemens E., Edgar M., Behrens F. Computed radiographic measurement of limb-length discrepancy: full-length standing anteroposterior radiograph compared with scanogram. J Bone Jt Surg Ser A. 2006;88(10):2243–2251. doi: 10.2106/JBJS.E.01179. [DOI] [PubMed] [Google Scholar]
- 31.Kjellberg M., Al-Amiry B., Englund E., Sjödén G.O., Sayed-Noor A.S. Measurement of leg length discrepancy after total hip arthroplasty. The reliability of a plain radiographic method compared to CT-scanogram. Skeletal Radiol. 2012;41(2):187–191. doi: 10.1007/s00256-011-1166-7. [DOI] [PubMed] [Google Scholar]