Abstract
Objectives
To analyze the effect of indigenous bicentric bipolar prosthesis on horizontal and vertical offsets in fracture neck of femur when compared to contralateral normal hip and to evaluate functional outcomes. We hypothesized that our non-modular bipolar device restores satisfactory offsets in such patients.
Methods
All active elderly patients with displaced fracture NOF having contralateral normal hip were included. We used an indigenous bicentric bipolar hip-prosthesis, which is a non-modular single-piece device in all cases by lateral Hardinge approach. Postoperative radiograph AP view was taken in 15° internal rotation to decrease the effect of limb rotation on offset. CT scan was also used to evaluate offsets using ADW4.6 ADVANCED GE optima 128 slice software system. Subjects were followed for a minimum of 12 months postoperatively and functional outcome of effect of offsets change were evaluated by modified Harris Hip Score.
Results
There is minimal difference in horizontal and vertical offset after bicentric bipolar hemi-replacement which is statistically insignificant supporting our hypothesis. The clinical outcomes were good to fair according to modified Harris Hip Score. The mean value of horizontal offset after our bipolar hemireplacement was 42.4 ± 2.04 mm and of normal hip was 41.8 ± 1.81 mm and P-value=0.08 in plain radiographs and value of horizontal offset in CT scan was 40.73 ± 0.27on bipolar side and 41.19 ± 0.77 on normal side. Vertical offset after bicentric bipolar was 32.67 ± 2.85 mm and vertical offset of normal hip was 32.53 ± 2.73 mm. Mean 9.77 ± 1.09 mm of calcar was preserved. Modified Harris Hip Score at 6 and 12 months postoperatively was 75.78 ± 4.16 and 79.53 ± 3.95 respectively. There was no incidence of hip dislocation.
Conclusion
Our study data clearly demonstrates that vertical and horizontal offsets are effectively maintained by the indigenous bicentric hip device. There was insignificant change in offsets as compared to contralateral normal side due to its design modifications. Indigenous bicentric non-modular bipolar device offers an excellent option for femur neck fractures in elderly patients in resource constrained situations. It allows rapid rehabilitation due to reduced surgical time, minimal blood loss and early return to function and activities of daily living.
Keywords: Fracture, Femur, Neck, Hemiarthroplasty, Bipolar, Bicentric, Offset
1. Introduction
In elderly population, hip fractures are very common and the trend is increasing. Annual incidence approximates 600,000 such cases in India.1 By 2050 nearly half of all expected hip fractures may occur in Asia.2
There are many reports of total hip replacement (THR) being better in elderly femoral neck fractures especially from the west.3 The circumstances in developing countries are different. Here, due to cost-benefit factors, socioeconomic status and life expectancy bipolar hemireplacement is still the treatment of choice for femoral neck fractures in active elderly.
The conventional femoral stems do not provide options for variable offset, unlike modular stem. Restoration of horizontal and vertical offset is not always possible with bipolar.4 Initially bipolar devices were designed to provide treatment for few years in patients with short life expectancy. Increased life expectancy necessitated restoration of the hip anatomy and offsets even after bipolar hemireplacement where THR is not suitable due to high cost and associated morbidities. Previous studies have reported inconsistent results regarding the importance of offset modifications.5
Femoral offsets affect muscle strength, the abductor lever arm, the joint-stability and the joint-reaction force in THR patients.6 The clinical outcomes and quality of life after bipolar hemiarthroplasty can be influenced by change of horizontal offset.7 The literature is varied regarding this subject due to difficulties in evaluating horizontal offset. Vertical offset is easy to evaluate after hemi-replacement in plain radiographs because it has very less dependence on the rotation of the affected limb. However, measurement of horizontal offset is influenced by the technique of the implant insertion, design of fixed offset bipolar, version of bipolar stem and the rotation of the lower extremity. The limitations and errors in horizontal offset have been described in some studies.8
We tried to evaluate horizontal and vertical offset after indigenous bicentric bipolar hip hemireplacement (our institutional bipolar device) in subjects with displaced neck femur fracture and assess the effect of change in femoral offset over the post-operative functional outcome.
2. Material and methods
The study was conducted in the Department of Orthopedics of a tertiary level university teaching hospital after ethics committee clearances vide letter no. 2017–18/EC/495. This prospective study was carried out from June 2017 to July 2019 on patients admitted in the orthopedics department of the hospital. A total of forty patients were studied. Written and informed consent for participation was obtained. Patients aged 55–80 years with displaced femoral neck fracture willing for follow up as required were included.
Fractures older than 4 weeks, associated uncontrolled comorbidities, pre-existing acetabular disease on same side, associated fracture in lower limb, rheumatoid arthritis, ankylosing spondylitis, contralateral hip pathology and any previous operative procedure in contralateral hip were excluded. All cases were operated with our bicentric bipolar hip device. A brief description of the bicentric bipolar device is presented.
Bicentric bipolar device9: The cup here is bicentric, i.e. the axis of metal cup and polyethylene cup is different which moves laterally on weight bearing preventing impingement of head/neck on cup edge. This anti-varus mechanism is the fundamental concept in bicentric bipolar.
The sizes range from 37 to 54 mm. The neck shaft angle is 128°. The offsets vary with different implant sizes ranging from 40 to 45 mm. The proximal stem-collar angle has been modified so as to preserve calcar by 8–10 mm after prosthesis insertion which is very low in conventional bipolar. This prevents sinking in cases where prosthesis is inserted without cement. The margin of polyethylene liner is beveled along with trapezoidal Charnley type neck improving the range of motion and reducing wear and tear.
The inner metal head size is 22 mm allowing for larger thickness polyethylene liner, thus improving survivorship. Outer head sizes are available from 37 to 55 mm with 1 mm increment allowing better fit. Both cemented and uncemented stem designs are available. All these factors combined provide for improved movement at inner bearing, prosthesis durability and better hip range of motion permitting sitting and squatting as per socio-cultural needs of our population.
Surgical tactic: Routine surgical case preparation was done. Appropriate radiographs were obtained. Preoperative manual templating was done from the normal side. We obtain digital radiographs with measuring scale marked on the radiographs. All cases were operated using lateral Hardinge approach in lateral patient position under spinal/epidural anesthesia as considered appropriate by the anesthetic team. All the surgeries were performed/assisted by the first author. Intra-operatively lesser trochanter was taken as the reference guide for the insertion of the prosthesis. Head sizing was done taking one size larger than the measured size. Calcar (8–10 mm) was preserved in an attempt to equalize the limb length (vertical offset). The femoral canal was prepared in line with lateral femoral cortex to avoid stem varus or valgus. When the fracture pattern was close to lesser trochanter such that 10 mm neck preservation was not possible, then cemented stem was used. The greater trochanter level was equalized with center of head in such cases. This way offset was managed in different fracture patterns.
The posterior border of the neck of the implant was aligned along the plane of anterior lesser trochanter to balance the effect of the rotation of the stem on the horizontal offset. Standard bipolar hemiarthroplasty procedure was carried out. Cementing was decided depending on femoral canal type as described by Dorr et al.10
Post-operatively, abduction pillow was placed. Ankle pumps and static quadriceps exercises were started immediately. We do not use any chemo-thromboprophylaxis. Drain was removed on day two after surgery. Patient was allowed to stand and walk with partial weight-bearing using walker as tolerated.
Post operative radiographs were obtained in a standard fashion with pelvis squared and lower limbs in 15° internal rotation. Internal rotation of lower limb was assessed with goniometer taking second toe as axis of foot in an attempt to decrease effect of rotation of lower limb on offset measurement.
CT scan was also used post-operatively to calculate offset more precisely using ADW4.6 ADVANCED GE optima 128 slice software system. Modified Harris hip score was evaluated at 3, 6 and 12 months after surgery to assess the functional outcome.
3. Results
A total of 40 patients were considered during the study period. Two patients demised in early follow up period due to causes unrelated to surgery. Eight patients were lost to follow up. Finally thirty cases were included in the analysis of which 11 were males and 19 females. Mean age was 69.9 ± 6.5 yrs (range 59–89yrs). Fractures were more common in seventh decade. This is possible due to increased mobility of these age group patients in spite of osteoporosis.
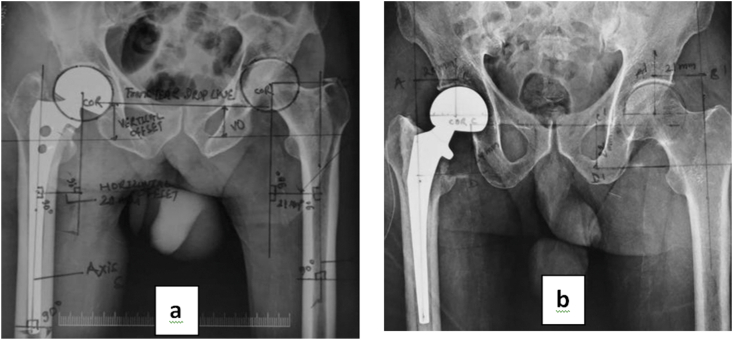
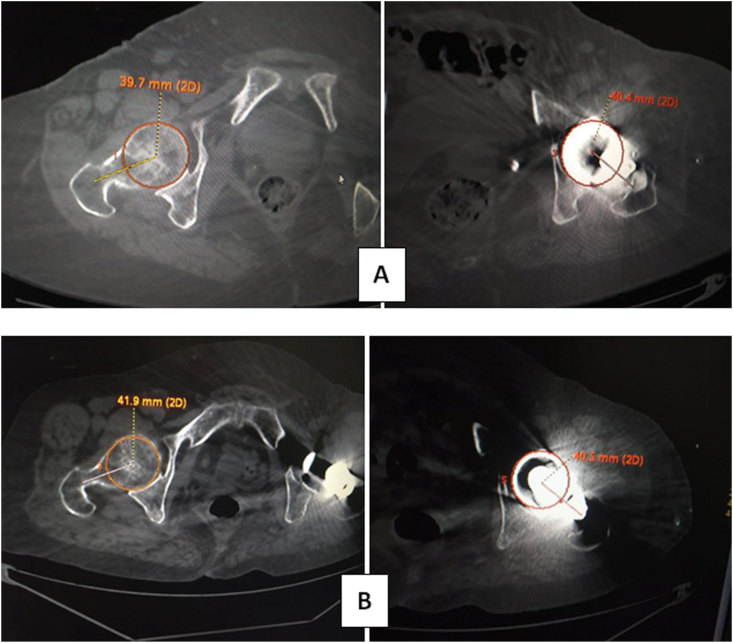
Mean follow up was 12.8 months. Average duration of surgery was 60 min. Average blood in surgery was 150 ml. In 46.7% patient calcar preservation was 10 mm. In fact in 80.1% cases calcar conserved was 10 ± 1 mm. Comparison of various parameters on operated (indigenous bipolar in situ side) and non-operated side is depicted in Table 1. Both the types of stem designs-cemented and uncemented are represented in Fig. 1. CT scan measurement of offset is shown in Fig. 2.
Table 1.
Comparison of horizontal offset of BHU bipolar hip to contralateral normal side.
| Parameter | Mean | P-value | |
|---|---|---|---|
| Horizontal offset (X-ray) | Bipolar | 42.40 ± 2.044 | 0.080 |
| Normal | 41.80 ± 1.814 | ||
| Horizontal offset (CT scan) | Bipolar | 40.733 ± 0.272 | >0.05 |
| Normal | 41.19 ± 0.77 | ||
| Vertical offset (X-ray) | Bipolar | 32.67 ± 2.845 | >0.05 |
| Normal | 32.53 ± 2.726 | ||
| Calcar preserved (above apex of lesser trochanter) | Range (8–12 mm) | 9.87 ± 1.074 | >0.05 |
| Modified Harris Hip Score | 6 month | 77.53 ± 4.614 | 0.001 |
| 12 month | 84.87 ± 3.946 | ||
Fig. 1.
Post-operative AP radiograph of pelvis in 15° internal rotation of lower limbs: (a) uncemented stem and (b) cemented stem designs of the bicentric bipolar hip device.
Fig. 2.
a & b. Case examples comparing horizontal offset in postoperative CT scan on bipolar in situ side and contralateral normal hip. Metallic artifact can make offset measurement on implant side difficult. The head and its center are marked by the software. The lateral point is marked by extrapolation from the center of the medullary canal. This is independent of rotation of limb (in radiographs it is rotation dependant).
4. Discussion
The incidence of hip fracture increases with age and is two to three times higher in women than in men.1,2 With increasing age the failure rate of osteosynthesis may reach 35%.11 Due to increased nonunion and avascular necrosis in such fractures replacement procedures like THR or hemiarthroplasty were being preferred when treating older patients.12
Our indigenous bicentric bipolar device has shown good clinical results in non-traumatic hip disorders also with motion preservation at inner bearing even at ten years.13 In the current study we analyzed fracture neck femur in active elderly patients treated with indigenous bipolar device as in developing countries hemiarthroplasty is still treatment of choice due to economic reasons.
Out of 40 patients considered, 30 patients were finally eligible for analysis of which 19 were females (63.3%) and 11 were males (36.7%) with average age 69.9 ± 6.5 yrs (range 59–89yrs). This shows the neck femur fracture is more common in 6th and 7th decade of life with relatively high incidence in females as supported by other studies.
Cementing was done in 16 (53.3%) cases and 14 (46.7%) cases were uncemented. There was one periprosthetic fracture after a month in one patient which was managed by plating alone as the prosthesis was found to be stable.
Analysis of the femoral offset is quite interesting and recent in the literature.14,15 Many studies have shown that increasing femoral offset improves hip abductor strength, reduces limping and the need of crutches. Offset restoration seems to decrease dislocation rate, cup strain and polyethylene wear and increases hip range of motion.16,17 Reduced femoral offset on the other hand leads to lower performance on functional tests.18,19
In our study, horizontal offset on bipolar side was 42.4 ± 2.1 mm and normal side was 41.8 ± 0.6 mm which was statistically insignificant, p-value 0.08. This supports the hypothesis that our indigenous non-modular single piece bipolar restores the anatomy.
Similarly the mean value of vertical offset on our bipolar side was 32.7 ± 2.8 mm as compared to 32.5 ± 2.7 mm on the normal hip.
Modified Harris Hip Score at 6 and 12 months postoperatively was 75.78 ± 4.16 (range 68–84) and 79.53 ± 3.95 (range 79–87) respectively which was assessed to be good to fair.
The range of calcar preservation was 8–12 mm above the apex of lesser trochanter. The mean value was 9.87 ± 1.1 mm. This suggests that 8–12 mm of calcar preservation gives near accurate vertical offset correction.
Considering the study limitations, larger sample size and longer follow-up will give more precise insight over long term. Future directions may include comparing this indigenous bicentric bipolar device with modular bipolar as control group.
5. Conclusion
The current study demonstrated that the vertical and horizontal offsets and hence limb length are effectively maintained by our indigenous bicentric non-modular bipolar hip device. There was statistically insignificant change in offsets as compared to contralateral normal side due to its design modifications and calcar preservation. This indigenous bipolar device offers an excellent option for femur neck fractures in elderly patients in resource constrained situations. It allows rapid rehabilitation due to relatively less surgical time and minimal blood loss comparing standard total hip replacement. It is technically less demanding than THR and modular bipolar procedure and also leads to early return to function and activities of daily living especially in those with comorbidities.
Authorship declaration
All authors listed meet the authorship criteria as per ICMJE guidelines and all authors are in agreement with the manuscript. The authors have no financial disclosures to make.
Declaration of competing interest
There are no conflicts of interest associated with this work.
References
- 1.Dhanwal D.K., Dennison E.M., Harvey N.C., Cooper C. Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop. 2011;45(1):15–22. doi: 10.4103/0019-5413.73656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnell O., Kanis J.A. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- 3.Sassoon A., D’Apuzzo M., Sems S., Cass J., Mabry T. Total hip arthroplasty for femoral neck fracture: comparing in-hospital mortality, complications, and disposition to an elective patient population. J Arthroplasty. 2013;28(9):1659–1662. doi: 10.1016/j.arth.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 4.Cho M.R. Lee HS Early results after the treatment with total hip arthroplasty with larger diameter femoral head versus bipolar arthroplasty in patients with femoral neck fractures. J Korean Hip Soc. 2007;19(4):463–467. [Google Scholar]
- 5.Lecerf G., Fessy M.H., Philippot R. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009;95(3):210–219. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Bjordal F., Bjorgul K. The role of femoral offset and abductor lever arm in total hip arthroplasty. J Orthop Traumatol. 2015;16(4):325–330. doi: 10.1007/s10195-015-0358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sariali E., Klouche S., Mouttet A., Pascal-Moussellard H. The effect of femoral offset modification on gait after total hip arthroplasty. Acta Orthop. 2014;85(2):123–127. doi: 10.3109/17453674.2014.889980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Merle C., Waldstein W., Pegg E. Femoral offset is underestimated on anteroposterior radiographs of the pelvis but accurately assessed on anteroposterior radiographs of the hip. J Bone Joint Surg Br. 2012;94(4):477–482. doi: 10.1302/0301-620X.94B4.28067. [DOI] [PubMed] [Google Scholar]
- 9.Rai A.K., Agarwal R., Singh S., Ratan R. The BHU bicentric bipolar prosthesis in fracture neck femur in active elderly. J Trauma Manag Outcome. 2008;25(2):1–7. doi: 10.1186/1752-2897-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dorr L.D., Faugere M.C., Mackel A.M., Gruen T.A., Bognar B., Malluche H.H. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14(3):231–242. doi: 10.1016/8756-3282(93)90146-2. [DOI] [PubMed] [Google Scholar]
- 11.Johansson T., Jacobsson S.A., Ivarsson I., Knutsson A. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fracture in 100 hips. Acta Orthop Scand. 2000;71:597–602. doi: 10.1080/000164700317362235. [DOI] [PubMed] [Google Scholar]
- 12.D’Arcy J., Devas M. Treatment of fractures of the femoral neck by replacement with the Thompson prosthesis. J Bone Joint Surg Br. 1976;58:279–286. doi: 10.1302/0301-620X.58B3.182698. [DOI] [PubMed] [Google Scholar]
- 13.Jha S.C., Rai A.K., Shakya P. 2017. Bicentric Bipolar Prosthesis in Non-traumatic Hip Pathologies: Maximum 10 Years Follow up. [Google Scholar]
- 14.Miyamoto R.G., Kaplan K.M., Levine B.R., Egol K.A., Zuckerman J.D. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16:596–607. doi: 10.5435/00124635-200810000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Devane P., Home G., Winemaker M. The effect of restoring femoral offset during THR on 3D volumetric wear. J Bone Joint Surg. 1997;79:385. [Google Scholar]
- 16.Yamaguchi T., Naito M., Asayama I. Total hip arthroplasty: the relationship between posterolateral reconstruction, abductor muscle strength, and femoral offset. J Orthop Surg. 2004;12:164–167. doi: 10.1177/230949900401200205. [DOI] [PubMed] [Google Scholar]
- 17.Bachour F., Marchetti E., Bocquet D. Radiographic preoperative templating of extra-offset cemented THA implants: how reliable is it and how does it affect survival? Orthop Traumatol Surg Res. 2010;96:760–768. doi: 10.1016/j.otsr.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Charles M.N., Bourne R.B., Davey J.R. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131–141. [PubMed] [Google Scholar]
- 19.Ebied A., Hoad-Reddick D.A., Raut V. Medium-term results of the Charnley low-offset femoral stem. J Bone Joint Surg Br. 2005;87:916–920. doi: 10.1302/0301-620X.87B7.15415. [DOI] [PubMed] [Google Scholar]