Abstract
Background
Trigger finger or stenosing tenosynovitis is a disproportion between the volume of the tendon sheath and its contents. This disproportion prevents gliding of the tendon as it moves freely through the annular pulley. The technique of percutaneous release of the annular pulley for trigger finger has been described well in the literature, which has undergone several modifications, like use of hypodermic needle, tenotome or specially designed knives.
Method
We performed percutaneous trigger finger release using a 20-gauge hypodermic needle to know the outcome and efficacy of the technique post release. A Prospective cohort study was conducted in 80 consecutive trigger fingers of 67 patients who were treated by percutaneous release using 20-gauge hypodermic needle. Quinell’s grading system was used to quantify severity of triggering and pain was assessed using visual analogue scale (VAS) before and after the procedure. Patients were evaluated based on these two parameters at timely interval and final outcome was assessed at the end of one year.
Results
Out of 80 digits treated, most of the subjects were in the age group 40–50 years (39.07%). Most common grade of trigger finger observed was Grade 3 (60%) followed by Grade 4 (30%) with VAS score of 8 (46%) followed by VAS score of 7 (24%) before release. At a year follow-up 95% of patients improved to grade 0 and mean VAS score was 0.44. Three patients developed scar tenderness, which gradually subsided by analgesics and physiotherapy with no other major complications.
Conclusion
Our technique of percutaneous release of trigger digit with 20 G needle is effective and can be performed safely with ease. It is cost efficient and has a short learning curve with great acceptance being an outpatient procedure.
1. Introduction
Trigger finger, or stenosing tenosynovitis first described by Alphonse Nota in 1850 is a common cause of hand pain, discomfort, and disability.1 Patient usually presents with painful “triggering” or “snapping” which is severe in morning but can occur throughout the day. It frequently affects adults aged 40–60 years with repetitive gripping and grasping activity. It is more common among females.2,3 The basic pathogenesis of trigger finger is the incompatibility between the tendon and its sheath that interferes with the normal gliding of tendon within its sheath. Normal gliding motion of a flexor tendon is dependent on a “critical tendon sheath calibre tolerance,” which allows the passage of the flexor tendons through the annular pulleys.4,5 Inflammation causes fibrocartilage metaplasia results in thickening of the annular pulley (most commonly A1 pulley).6 Forceful flexion or gripping causes bunching of the flexor tendon making them stuck proximal to the thickened annular pulleys. Freiberg et al.7 classified tendon sheath pathology based on palpation of the pulley into nodular and diffuse. If the swelling is contained and there is a definite palpable nodule, which moves back and forth under the examiner’s finger as the digit triggers, the pathology is nodular. If the swelling ill defined, it is classified as diffuse.
Annular pulleys are thickening of the tendon sheath in five areas along the flexor tendons of the 2nd to 5th finger and numbered as A1 to A5, while thumb has only two annular pulleys (A1 and A2). The tendon sheath is made up of two components - membranous synovial portion and retinacular pulley portion.8 The membranous synovial portion of the sheath is composed of a visceral or epitenon layer intimate with the tendon and a parietal or outer layer that maintains the synovial pouch. The retinacular pulley is a series of transverse, annular and cruciform fibrous tissue bands that overlie the synovial portion of the sheath.8 Doyle and Blythe et al.9 demonstrated that the flexor sheath in the finger is a double-walled, hollow, synovial-lined, connective tissue cylinder that is held in place by four annular and three cruciform pulleys that vary in length, width and thickness. The A1 pulley is most commonly involved in trigger finger and acts as the most palmar restraint to the finger flexors in the region of the metacarpo-phalangeal (MCP) joint.10 Anatomically, A1 pulley is contiguous with the retinacular restraints of the MCP joint assemblage including palmar plate. The A1 pulley gains two thirds of its origin from the palmar plate of the (MCP) joint and may at times be hypertrophied to two or three times its normal size.10,11
The exact pathobiology of trigger finger is unknown, and most of the cases are idiopathic in nature, yet it can be associated with a number of conditions, including direct tendon trauma, diabetes mellitus, carpal tunnel syndrome, De quervain’s tenosynovitis, Rheumatoid arthritis, Hypothyroidism, Mucopolysaccharidosis, amyloidosis, gout, hypertension, various tumours and neoplasms. Several forms of conservative treatment is recommended, including splint immobilization, non-steroidal anti-inflammatory medication, steroid injection with good results in single digit involvement and in early cases. Surgical release of A1 pulley is usually indicated when conservative treatment fails.
Both open and percutaneous release of trigger finger have been described in the literature. Lorthioir in 1958 first described a technique of percutaneous release using a fine tenotome.12 Percutaneous release using a needle was introduced by Eastwood in 1992 with a high success rate.13 Quinell’s grading (Table 1) is the most commonly followed classification for grading trigger digits and it has been graded from 0 to 4 based on the severity of triggering.
Table 1.
Quinell’s grading.
| Grade | Clinical Findings |
|---|---|
| Grade 0 | Normal movements, no Pain |
| Grade 1 | Uneven Movements. |
| Grade 2 | Actively correctable |
| Grade 3 | Passively correctable |
| Grade 4 | Fixed deformity |
2. Method
A Prospective cohort study was done on patients who had idiopathic triggering due to pathology in the A1 pulley. Patients who had triggering due to lesion in other pulleys were excluded. All those patients who did not respond to conservative treatment, given for a period of minimum 3 months were included. All those patients with known history of hypothyroidism, rheumatoid arthritis with secondary triggering were excluded. Details of the procedure including the expected complications were explained to every patient and proper informed consent was taken. Patients triggering severity was assessed using Quinell’s grading and pain was assessed using VAS score pre operatively. All the preoperative assessment and scoring was done by same senior resident. Post operatively to prevent bias a different senior resident was asked to assess the patient’s grade of triggering and VAS score. These patients were followed up for a minimum period of 1 year at timely intervals.
All percutaneous releases were done as an outpatient procedure. Same senior resident who did the pre-operative assessment performed all the percutaneous release. A1 pulley was located by both palpation and predefined surface markings. The surface landmarks corresponding to proximal edge of A1 pulley are the metacarpophalangeal crease of the thumb, the proximal palmar crease of the index finger, halfway between the proximal and distal palmar creases of middle finger and the distal palmar creases of the ring and little finger. The procedure was done in a outpatient procedure room using a strict aseptic technique. 2 ml of 2% plain lignocaine is injected locally around the nodule. Few minutes after injecting local anaesthesia, once pain subsided the finger is held firmly and hyper-extended at the metacarpophalangeal joint for palpation of the pulley. Hyperextension is essential, as it causes the flexor tendon sheath to lie directly under skin and allows the digital neurovascular bundles to displace to either side. A 20 G hypodermic needle is inserted into the flexor tendon sheath or nodule proximally, with bevel of the needle oriented along the line of the finger (Fig. 1). Position of the needle in the tendon sheath is confirmed by actively flexing the digit and observing the motion of the needle. The needle is then withdrawn slightly until it ceases to move with flexion of the fingertip. The A1 pulley is cut by moving bevel of the needle longitudinally from proximal to distal. The surgeon feels a grating sensation as the needle tip cut through the transverse fibres of the A1 pulley. Loss of grating sensation indicates adequacy of the release, and the patient is asked to actively flex and extend the finger to verify the success of the procedure. Adequate release of the pulley is shown by disappearance of the triggering on active movement of the digit. If a patient demonstrated continued triggering the needle is reinserted more distally and additional release is performed. A small adhesive strip bandage was placed on the puncture wound (Fig. 2). Patient were asked to return to their activity once the VAS score was less than three. Physiotherapy and rehabilitation started once pain subsided in the form of active finger movement and stretching and were given for minimum period of 2–3 weeks.
Fig. 1.
Clinical picture showing release of A1 pulley with 20 gauge needle by hyper extending the metacarpo-phalangeal joint.
Fig. 2.
Clinical picture after the release with small adhesive dressing.
3. Results
67 patients who had idiopathic triggering were included in the study. 41 were females and 26 were males. Of the 67 patients, 13 had triggering in more than one finger (2 fingers – 10 patients, 3 fingers- 3 patients), 54 had triggering in a single finger, making a total of 83 trigger fingers. 64 patients were followed up at timely intervals for one year after the index procedure, three patients (all single digit trigger finger) were lost to follow-up making a total of 80 fingers who had a minimum follow-up of one year.
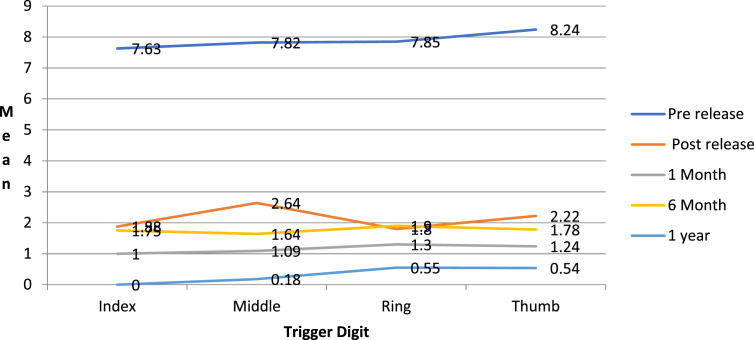
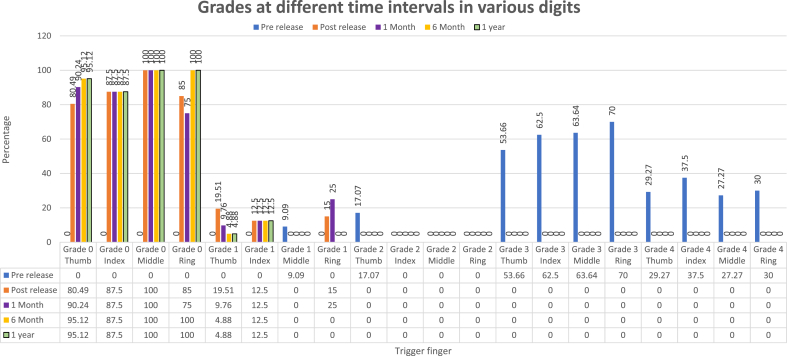
Basic demographic details (Table 2). Patient’s preoperative and post-operative Quinells score at different time intervals (Table 3), Preoperative and post-operative VAS score on different time interval (Table 4) are shown in the respective table. Majority of the subjects (39.07%) were in the age group 40–50 years. The most common digit involved (Table 5) is thumb (51.25%) followed by ring finger (25.0%). Most of the patients preoperatively (60%) belonged to quinells grade 3 followed by grade 4 (30%). Immediate post release most of the patients (85%) had quinells grade 0. Follow up at one year showed (95%) to have quinells grade 0. The preoperative mean VAS score was 8.03, which improved to a mean VAS of 0.44 at one year follow-up. Three patients had scar tenderness which improved gradually with physiotherapy and NSAIDs, there was no major complications like digital nerve injury, bowstringing and infection etc.
Table 2.
Distribution of the study subjects based on the age group.
| Age group | Number | Percentage % | ||
|---|---|---|---|---|
| 30 to 40 | 3 | 4.69 | Mean | 53.12 |
| 40 to 50 | 25 | 39.07 | SD | 9.93 |
| 50 to 60 | 14 | 21.86 | Range | 31 to 77 |
| 60 to 70 | 19 | 29.69 | ||
| 70 to 80 | 3 | 4.69 |
Table 3.
Quinell’s grading at different time intervals.
| Grades | Pre release |
Post release |
1 month |
6 month |
1 year |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Nor | % | Nor | % | Nor | % | Nor | % | Nor | % | |
| Grade 0 | 0 | 0 | 68 | 85.00 | 70 | 87.50 | 77 | 96.25 | 76 | 95.00 |
| Grade 1 | 1 | 1.25 | 12 | 15.00 | 10 | 12.50 | 3 | 3.75 | 4 | 5.00 |
| Grade 2 | 7 | 8.75 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Grade 3 | 48 | 60.00 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Grade 4 | 24 | 30.00 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Table 4.
VAS score at different time intervals.
| VAS | Pre release |
Post release |
1 month |
6 month |
1 year |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 8.03 | 0.97 | 2.14 | 1.46 | 1.21 | 1.48 | 1.79 | 0.65 | 0.44 | 0.95 | |
Table 5.
Distribution based on the digits.
| Trigger digit | Frequency | Percentage |
|---|---|---|
| Index | 8 | 10.00 |
| Middle | 11 | 13.75 |
| Ring | 20 | 25.00 |
| Thumb | 41 | 51.25 |
| Total | 80 | 100.00 |
4. Discussion
The entity trigger finger was first described by Notta in 1850.1 The treatment option includes physiotherapy, splinting, corticosteroid injection, failure of which, open or percutaneous release of the A1 pulley is recommended. Both procedures are done on outpatient basis, some prefer local anaesthesia for better patient compliance and provides immediate relief of pain due to triggering during release, while some believe local anaesthesia distorts local anatomy and prefers biers block. Release of A1 pulley increases work of flexion by 10%, but it appears to be clinically irrelevant. Releasing the A2 pulley increases work of flexion by 22% and releasing both A1 and A2 pulley increases flexion work by 62%. Though there is an increase in work of flexion on releasing the annular pulley, Near-normal hand function is possible with intact A-2 and A-4 pulleys.20
Both open and percutaneous release can be done with minimal complications, but catastrophic complication like bowing of flexor tendon, digital nerve injury, incomplete release and flexor tendon injury can also occur. A2 pulley is prone for injury in both percutaneous and open procedure due to its close relation with A1 pulley as described by Doyle and Blythe in their anatomical study, where they found a 50% chance in continuity between the A-1 and A-2 pulleys and the separation between the two pulleys is generally 0.4–4.1 mm.8,9 Carrozella et al.14 cadaveric study showed radial digital nerve of the thumb to be only 2.19 mm below the dermis and 1.15 mm anterior to the radial sesamoid bone, which act as a cutting board for transacting the nerve.
Pope and Wolfe15 performed percutaneous release in 13 trigger fingers using a 19-gauge needle and then opened the wound to see for the adequacy of the release. They found, complete release only in 8 patients; while the rest had distal 10%–15% of the pulley intact even though all patients were free of triggering postop. They hypothesized that triggering resolves even if the distal edge of the A-1 pulley is not released.
Bain et al.16 in their cadaveric studies, demonstrated damage to the flexor tendons following percutaneous release, but all those were small longitudinal tears. These generally do not cause any problem in outcome but can cause painful tenosynovitis without triggering. The use of a corticosteroid along with local anaesthetic may prevent the post-procedure tenosynovitis.17 Steroids are known to possess anti-inflammatory action; our study did not include injection of local steroid post release, as we purely wanted to assess the results of the technique of percutaneous release.
Percutaneous release has various advantage over open release as shown by a Gilberts et al.18 in their prospective study of 100 patients comparing the 2 techniques. They showed 100% relief of symptoms in patients who had undergone percutaneous release and 98% with open release. They reported 1 treatment failure as a result of excessive scar formation, causing recurrent triggering that required another procedure. They further favoured percutaneous technique as they have of shorter procedure time (7 vs 11 min), shorter duration of postoperative pain (3.1 vs 5.7 days), quicker recovery of full hand function (7 vs 18 days after the procedure), and faster return to work (3.9 vs 7.5 days).
The technique of percutaneous trigger finger release has gained popularity recently and a number of studies have evaluated the safety and efficacy of percutaneous release. Several instruments have been advocated for this procedure, which includes hypodermic needle of different sizes, tenotome or specially designed knives. We used a 20G hypodermic needle in our study, which has been never described previously. Lorthioir used a fine tenotome to perform percutaneous release and reported no complications in 52 patients.12 Eastwood et al.13 used a 21-gauge hypodermic needle on 35 trigger digits and post operatively 94% had relief of symptoms without any complications. Although Eastwood et al.13 released 3 thumbs in their study they noted that the obliquity and volar position of the neurovascular bundles in the thumb required particular caution. We had 41 trigger thumbs, at 1-year follow-up the mean VAS score was 0.54 and 95.12% had Quinells grade 0.
Ha CW et al.3 had 185 percutaneous trigger fingers release using specially designed HAKI knife and had 12 (6.48%) digits with persistent triggering. Pandey BK et al.2 had done percutaneous release of 58 fingers with 18 G needle and had 2 digits with persistence of triggering. Our series has no persistence of triggering. Patients satisfaction in both the series (Pandey BK et al.2 and HA CW et al.3) were 93% and 97% respectively. Our series at the end of one year had a mean VAS score of 0.44, and 95.0% had Quinells grade 0, while preoperatively the mean VAS score was 8.16 and (Chart 1) 60% had Quinells grade 3 and 30% had grade 4 (Chart 2). Though three patients developed scar tenderness, the symptoms were completely relieved with physiotherapy and NSAID’s. Our study had no recurrence as adequacy of the release was confirmed during the procedure and if required re-release was performed at the same time. A comparison of the various methods of trigger finger is shown in Table 6.
Chart 1.
VAS score over different time interval.
Chart 2.
Grade of triggering over different time interval.
Table 6.
Comparison of outcome in percutaneous release of trigger finger.
| SI no. | Study | Sample size | Methodology | Mean Follow up | Results | Complications |
|---|---|---|---|---|---|---|
| 1 | Ha J, Park MJ, Ha CW et al.3 (2001) |
151 patients with 185 digits | Specially designed HAKI knife | 12.2 months | Satisfactory results with complete relief in 93% of the digits | 12 digits with persistent triggering |
| 2 | Pandey BK, Sharma S et al.2 (Jan 2010) |
58 trigger digits in 51 patients | 18 G needle | 12 months | Satisfactory results in 97% patients. | 2 digits with persistent triggering, later performed open release |
| 3 | Vedat Uruc et al.19 (2011) |
50 trigger digits in 50 patients | 19 G microvitreo retinal blade | 6.4 months | Satisfactory results in 90% patients | Residual deformity in 3 fingers, open release performed later on. |
| 4 | Ramy Ahmed Diab et al. (2014) | 43 trigger digits | 18 G needle | 12 months | Satisfactory results in 93% patients | Superficial flexor tendon laceration in 6 fingers |
| 5 | Current study | 80 trigger digits in 74 patients | 20 G needle | 12 months | Satisfactory results in 95% patients | Scar tenderness in two patients. No residual triggering. |
Our procedure of percutaneously releasing trigger finger using a 20G hypodermic needle is a simple outpatient procedure with easy learning curve. It has a high success rate with very few complication and negligible recurrence. The drawbacks of the study includes that no control group was there for comparison, only patients with A1 pulley trigger were included, even after release patients were given physiotherapy for 2–3 weeks which must have caused a bias.
Informed consent
A detailed informed consent has been given by all the patients to publish this data and relevant details. The patient understand that his name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed. Informed consent was obtained for experimentation with human subjects.
Declaration of competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. The authors declare that they have no competing interests.
Acknowledgement
The authors would like to express gratitude toward the patients and their families for allowing us to use the information for medical documentation and research purpose that led to the present article.
Contributor Information
Atul Panghate, Email: atulpanghate@gmail.com.
Sameer Panchal, Email: panchalsameer1992@gmail.com.
Akil Prabhakar, Email: akil.prabhakar@gmail.com.
Abhinav Jogani, Email: drabhinavdjogani@gmail.com.
References
- 1.Philip J., Clapham B.S., Chung Kevin C., Md M.S. A historical perspective of the notta’s node in trigger fingers. J Hand Surg Am. 2009 Oct 34;(8):1518–1522. doi: 10.1016/j.jhsa.2009.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pandey B.K., Sharma S., Manandhar R.R., Pradhan R.L., Lakhey S., Rijal K.P. Percutaneous trigger finger release. Nepal Orthop Assoc J. Jan 2010;1 Number one. [Google Scholar]
- 3.Ha K.I., Park M.J. Percutaneous Release of Trigger Digits. 83-B. Jan 2001. C.W. Ha from sungkyunkwan university school of medicine. No.1. [DOI] [PubMed] [Google Scholar]
- 4.Mark Ryzewicz , MD , Jennifer Moriatis Wolf , MD Department of Orthopedics , University of Colorado Health Sciences Center, Denver , CO. Trigger Digits : Principles , Management , and Complications. [DOI] [PubMed]
- 5.Steven P., Sampson, MD, Marie A, et al. Pathobiology of the Human A 1 Pulley in Trigger Finger
- 6.Littler J.W. Stenosing digital tendovaginitis. In: Converse J.M., Littler J.W., editors. Reconstructive Plastic Surgery. vol. 6. WB Saunders; New York: 1977. pp. 3440–3443. (The Hand and Upper Extremity). [Google Scholar]
- 7.Freiberg A., Mulholland R.S., Levine R. Non-operative treatment of trigger fingers and thumbs. J Hand Surg [Am] 1989;14:553–558. doi: 10.1016/s0363-5023(89)80024-3. [DOI] [PubMed] [Google Scholar]
- 8.Doyle J.R., Blythe W.F. Anatomy of the flexor tendon sheath and pulleys of the thumb. J Hand Surg. 1977;2:149–151. doi: 10.1016/s0363-5023(77)80101-9. [DOI] [PubMed] [Google Scholar]
- 9.Doyle J.R., Blythe W.F. AAOS Symposium on Tendon Surgery in Hand. the CV Mosby Company; St. Louis: 1975. The finger flexor tendon sheath and pulleys: anatomy and reconstruction; p. 81. [Google Scholar]
- 10.Saldana M.J. Trigger digits: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:246–252. doi: 10.5435/00124635-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Wilhelmi B.J., Mowlavi A., Neumeister M.W., Bueno R., Lee W.P. Safe treatment of trigger finger with longitudinal and transverse landmarks: an anatomic study of the border fingers for percutaneous release. Plast Reconstr Surg. 2003;112:993–999. doi: 10.1097/01.PRS.0000076225.79854.F7. [DOI] [PubMed] [Google Scholar]
- 12.Lorthioir J. Surgical treatment of trigger finger by a subcutaneous method. J Bone Joint Surg [Am] 1959;40-A:793–795. [PubMed] [Google Scholar]
- 13.Eastwood D.M., Gupta K.J., Johnson D.P. Percutaneous release of the trigger finger: an office procedure. J Hand Surg [Am] 1992;17:114–117. doi: 10.1016/0363-5023(92)90125-9. [DOI] [PubMed] [Google Scholar]
- 14.Griggs S.M., Weiss A.P.C., Lane L.B., Schwenker C., Akeiman E., Sacher K. Treatment of trigger finger in patients with diabetes mellitus. J Hand Surg. 1995;20:787–789. doi: 10.1016/S0363-5023(05)80432-0. [DOI] [PubMed] [Google Scholar]
- 15.Cebesoy O., Karakurum G., Kose K.C., Baltaci E.T., Isik M. Percutaneous release of the trigger thumb. Int Orthop. 2007;31 doi: 10.1007/s00264-006-0180-1. 345-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bain G.I., Turnbull J., Charles M.N., Roth J.H., Richards R.S. Percutaneous A1 pulley release: a cadaveric study. J Hand Surg [Am] 1995;20:781–784. doi: 10.1016/S0363-5023(05)80430-7. [DOI] [PubMed] [Google Scholar]
- 17.Maneerit J., Sriworakun C., Budhraja N., Nagavajara P. Trigger thumb: results of prospective randomised study of percutaneous release with steroid injection versus steroid injection alone. J Hand Surg (Br Eur vol) 2003;28(6):586–589. doi: 10.1016/s0266-7681(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 18.Gilberts E.C., Beekman W.H., Stevens H.J., Wereldsma J.C. Prospective randomized trial of open versus percutaneous release for trigger digits. J Hand Surg. 2001;26A:497–500. doi: 10.1053/jhsu.2001.24967. [DOI] [PubMed] [Google Scholar]
- 19.Vedat Uruc, Abdullah Kursat Cingu, Emrah Sayit, Fatih Kucukdurmaz, Mahmut Nedim Aytekin, Department of Orthopaedics and Traumatology, Turkey. Percutaneous Trigger Finger Release with Microvitreoretinal 19 Gauge Ophthalmologic Knife
- 20.Peterson William W., Manske Paul R., Bollinger Bruce A., Lesker Peggy A., McCarthy John A. Effect of pulley excision on flexor tendon biomechanics. J Orthop Res. 1986;4(No.1) doi: 10.1002/jor.1100040112. [DOI] [PubMed] [Google Scholar]