Abstract
Background
Due to the rare incidence of tibial plateau nonunions, current studies are limited to small sample sizes and patient demographics. The aim of this systematic review is to quantify and report patient and fracture traits, possible risk factors, and treatment outcomes of tibial plateau nonunions.
Methods
PubMed, Clinical Key, and MEDLINE were searched for articles published prior to August 2020 in accordance to the preferred reporting items for systematic reviews and meta-analyses (PRISMA). The authors used varying combinations of the following terms to identify relevant articles: “tibial,” “plateau,” “nonunion,” “non-union.” Studies were assessed for patient demographics, pre-revision nonunion characteristics, treatment, and post-revision outcomes.
Results
Eight studies were included, yielding 31 tibial plateau nonunions (21 males, 10 females). The majority of nonunions were associated with high energy trauma (52.2%) and were Schatzker class VI (54.8%). Schatzker class I and II nonunions were not attributed to neglect, contradicting previous suggestions. Time to union was 4.0 months, the most common treatments being autologous bone grafting (76.7%) and revision plating (63.3%).
Conclusion
This study demonstrates the effectiveness of autologous bone grafts and revision plating for tibial plateau nonunions. Physicians may use these findings to guide decision making in the event of high energy plateau nonunions. Lastly, various limitations exist within the current literature, emphasizing the need for standardized reporting measures.
Keywords: Trauma, Nonunion, Tibial plateau, Fracture, Schatzker
1. Introduction
Tibial plateau fractures represent 1% of all fractures and remain a difficult surgical and clinical problem despite recent surgical advancements. These periarticular fractures occur when axial loading is combined with varus or valgus stress on the knee. Subsequently, a bimodal distribution exists between high-energy accidents in younger adults and low-energy falls in the elderly.
Tibial plateau fractures are challenging injuries associated with significant morbidity and risk for poor outcome. While low-energy falls typically lead to simple fracture patterns, high-energy trauma results in more complex fractures that are associated soft tissue injury, compartment syndrome, neurologic compromise, or infection.1 As a result, complication rates for high-energy tibial plateau fractures treated surgically have been reported up to 30%, with infection and wound complications constituting the majority.1, 2, 3 Malunions or residual deformity make up another significant portion of the complications with rates up to 10%.4,5 The remaining portion of complications is composed of less frequent complications such as nonunion, implant failure, and symptomatic implant.
Tibial plateau nonunions are rare and represent just 1–2% of tibial plateau fracture complications.6 A robust blood supply to the proximal tibia facilitates osteogenic processes and reduce the risk of nonunion. However, high-energy fractures (Schatzker V and VI) are associated with significant vascular compromise and soft tissue injury.1,7 As a result, risk of nonunion is elevated in high energy trauma and has been reported to be as high as 10–20%.1,7 In cases of low-energy trauma, simple fracture patterns may seem amendable to conservative management, but displacement of fracture fragments could lead to nonunion.8
Just as etiology and fracture behavior differ for lateral, medial, and posteromedial tibial plateau fractures, their respective nonunions may also carry their own set of unique characteristics that have not been identified or described.3,9,10 Despite the need to improve our understanding of tibial plateau nonunions, a paucity of research persists. Of the studies that do exist, some do not include important nonunion characteristics and others do not differentiate nonunions from malunions when presenting data.11,12 To our knowledge, no systematic reviews on tibial plateau nonunions exist to date. Accordingly, the authors review the available literature on tibial plateau nonunions to quantify and report patient and fracture traits, possible risk factors, and treatment outcomes.
2. Methods
2.1. Data sources
This systematic review was conducted in accordance to the preferred reporting items for systematic reviews and meta-analyses (PRISMA).13 The authors conducted independent reviews of the literature to identify relevant articles. PubMed, Clinical Key, and MEDLINE were searched using varying combinations of the following terms, with use of Boolean operators, to identify relevant articles: “tibial,” “plateau,” “nonunion,” “non-union.”
2.2. Study selection
Studies were included if they presented characteristics, revision type, and outcomes of tibial plateau nonunions. Studies that did not separate nonunions from malunions, or did not present characteristics, revision type, and outcomes, were excluded. Cadaveric studies, expert opinion studies, and technique articles were excluded.
2.3. Data extraction
Title, author, year, and level of evidence was recorded for each study. Whether or not the study defined a nonunion, and the definition of the nonunion, were recorded. Patient demographics collected included sex, age, time from injury to nonunion, and risk factors predisposing to nonunion. Pre-treatment nonunion variables included Schatzker class, tibial location, type (oligotrophic, atrophic, hypertrophic), pre-treatment range of motion (ROM), symptoms, and initial treatment prior to nonunion. Post-treatment variables included type of revision, complications, time to union, post-treatment ROM, and various scoring system outcome measures. Radiographs included within the text were reviewed to confirm diagnosis.
2.4. Data synthesis
Consensus was reached on articles and data included in this study by the authors (KKO and GL). Statistical analyses were performed using STATA/MP Software 13.0 (StataCorp, College Station, TX) and Microsoft Excel (Redmond, WA: Microsoft Corporation).
3. Results
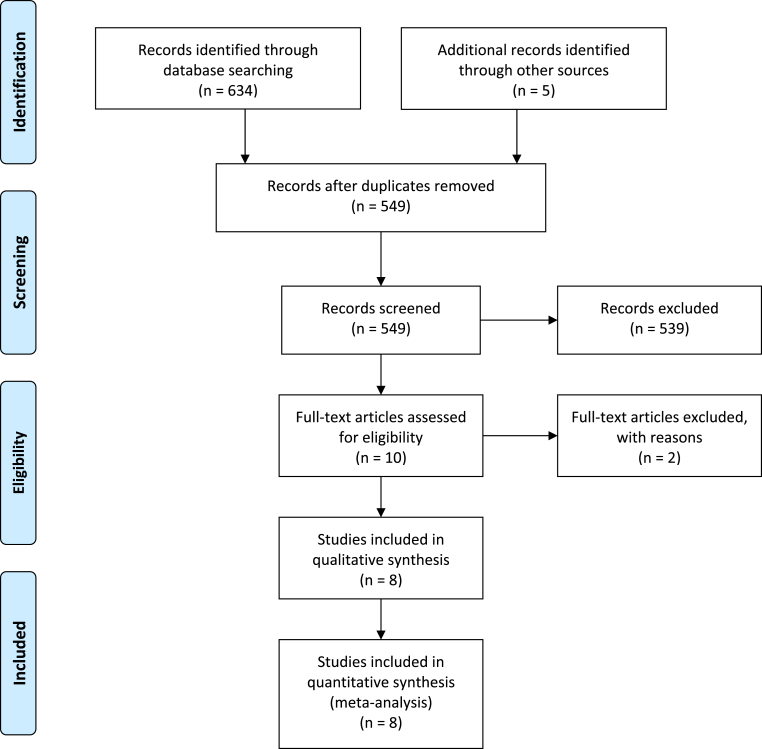
Six hundred forty-four studies were obtained after the initial screen and five studies were identified through other sources (Fig. 1). After removal of duplicates and application of inclusion and exclusion criteria, eight studies were included. Six of these were retrospective cohort studies and two were case reports.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
3.1. Pre-revision characteristics
Within the eight studies, 21 males and 10 females had a 31 tibial plateau nonunions. Average age at the time of presentation was 49.9 years old (Table 1). Average time from injury to revision surgery was 8.7 months.
Table 1.
Patient demographics.
| Patient Demographics | |
|---|---|
| Age | 49.9 years |
| Males | 21 (67.7%) |
| Females | 10 (32.3%) |
The primary risk factor that predisposed to nonunion was high energy trauma (n = 24, 77.4%), followed by polytrauma (n = 6, 19.4%) (Table 2). Thirty out of 31 tibial plateau nonunions were categorized by Schatzker Classification, with one unspecified (Table 3). Nine nonunions were located medially, ten posteromedially, six posterolaterally, and the rest were unspecified. Twelve nonunions were categorized as oligotrophic and one was atrophic. Initial treatments prior to nonunion consisted of periarticular plating (n = 12, 38.7%), unspecified open reduction internal fixation (ORIF) (n = 6, 19.4%), autologous bone grafting (n = 5, 16.1%), conservative treatment (n = 5, 16.1%), external fixator (n = 3, 9.7%), and screws only (n = 2, 6.5%). Four nonunions were classified as “neglected” as they did not receive any form of treatment prior to nonunion.
Table 2.
Pre-revision characteristics.
| Risk Factors | n (%) |
|---|---|
| High Energy Trauma | 24 (77.4) |
| Polytrauma | 6 (19.4) |
| Open Fractures | 3 (9.7) |
| Infection |
2 (6.5) |
|
Location |
n (%) |
| Posteromedial | 10 (40) |
| Medial | 9 (36) |
| Posterolateral |
6 (24) |
|
Type of Nonunion |
n (%) |
| Oligotrophic | 12 (92.3) |
| Atrophic |
1 (7.7) |
|
Initial Treatment |
n (%) |
| Periarticular Plating | 12 (38.7) |
| Unspecified ORIF | 6 (19.4) |
| Bone Graft | 5 (16.1) |
| Conservative | 5 (16.1) |
| External Fixator | 3 (9.7) |
| Screws Only | 2 (6.5) |
Table 3.
Distribution of tibial plateau nonunions by Schatzker Classification.
| Schatzker Classification | |||||
|---|---|---|---|---|---|
| I | II | III | IV | V | VI |
| 1 | 3 | 0 | 6 | 3 | 17 |
At presentation for nonunion, 19 out of 31 knees presented with pain (61.2%), seven with instability (22.6%), four with varus thrust/misalignment (12.9%), three with effusion (9.7%), and three with joint-line tenderness (9.7%). Average pre-operative arc of motion was 8.4–115.4° (Table 4).
Table 4.
Pre and post-revision evaluation.
| Pre-Revision Clinical Evaluation | |
|---|---|
| Flexion | 115.4° |
| Extension | −8.4° |
| Time from Injury to Revision |
8.7 months |
|
Post-Revision Clinical Evaluation | |
| Flexion | 127.9° |
| Extension | −5.8° |
| Time from Revision to Union | 4.0 months |
3.2. Treatment and outcomes
Thirty nonunions were treated operatively. Treatment included autologous bone grafting (n = 23, 76.7%), revision plating (n = 19, 63.3%), lag screws with high tibial osteotomy (n = 3, 10.0%), external fixator (n = 2, 6.7%), conservative treatment (n = 1, 3.3%), intramedullary fixation (n = 1, 3.3%), lag screws only (n = 1, 3.3%), lag screws with intra-articular osteotomy (n = 1, 3.3%), and total knee arthroplasty (n = 1, 3.3%) (Fig. 2, Fig. 3, Fig. 4). Post-revision surgery arc of motion was 5.8–127.9°. Average time to union after revision was 4.0 months. Two patients experienced infection, one of whom had a history of infection. These infections were treated with irrigation and debridement and went on to successful union.
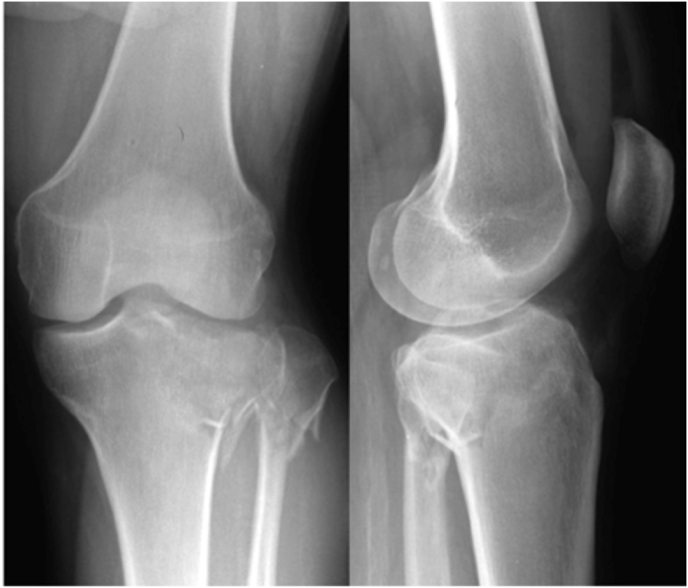
Fig. 2.
AP and lateral radiographs significant for lateral tibial plateau and fibular neck fractures following a motor vehicle accident.
Fig. 3.
AP and lateral radiographs demonstrating nonunion and malreduction of plateau fragment (arrow) at six months following ORIF using arthroscopy-assisted reduction with cannulated screws.
Fig. 4.
Three-year follow-up demonstrating healing of nonunion following revision plating with bone grafts.
One of the 31 knees was treated nonoperatively due to refusal of surgery. This patient was subsequently treated with immobilization in a plaster of Paris (POP) cast. Despite valgus deformity existing three months post-revision, surgery was refused again. The authors state that at four years post-revision, the knee exhibited full ROM with no symptoms, despite tibial malalignment.
4. Discussion
This study presents the first review of the literature analyzing characteristics and outcomes of tibial plateau nonunions. The majority of nonunions in this study were associated with high energy trauma (52.2%) and were Schatzker class VI (54.8%). This is not an unexpected finding, as high-energy Schatzker class VI fractures at the metaphyseal-diaphyseal junction result in compromised blood supply and associated soft tissue injury. Additionally, adjacent structures such as the meniscus and other soft tissues have the potential to displace into the fracture site, preventing adequate bony apposition, resulting in nonunion as evidenced by Toro-Arbelaez et al.14 In a radiographic study of 103 tibial plateau fractures, 91% of patients had a lateral meniscal injury and 44% had a medial meniscal injury.15 In addition, 77% of patients experienced at least one tear or avulsion of the collateral or cruciate ligaments.15 In the presence of high-energy tibial fractures, physicians should be cognizant of fracture patterns contributing towards nonunion.
Although previous research attributed low-energy nonunion to missed diagnosis or benign neglect, our findings seem to indicate otherwise.8 Low-energy Schatzker class I and II constituted 3.2% (1) and 9.7% (3) of nonunions in this study, respectively. Of these four, three were treated with ORIF and one with conservative treatment. The patient who underwent conservative management was the aforementioned Schatzker II that refused surgery. As a result, some low-energy plateau fractures may be at risk for nonunion, regardless of primary treatment.
The various operative methods of treating the 30 out of 31 nonunions all proved to be fairly effective in this study, with an average time to union of 4.0 months. Out of the 30 patients receiving surgery, 76.7% received autologous bone grafting to improve the osteogenic, osteoconductive, and osteoinductive properties of the nonunion.16, 17, 18, 19 The effectiveness of bone grafting in the treatment of tibial nonunions has been reported previously by Braly et al.20 In addition, 63.3% of the 30 patients received revision plating. The decision to combine grafting with revision plating may be attributed to the nature of the nonunions in this study. In cases of oligotrophic nonunions, improving fracture alignment is imperative.21 Although use of autologous bone grafts can be made selectively in cases of oligotrophic nonunion, associated soft tissue injury and compromised blood supply from the high energy trauma may warrant use.21 Additionally, it is possible that a large proportion of the 18 nonunions that were unable to be classified in this study were atrophic, requiring use of bone grafting.21, 22, 23 Subsequently, the authors recommend the use of revision plating systems in conjunction with autologous bone grafting for high energy, atrophic or oligotrophic nonunions.
Importantly, the authors found a low rate of complications following revision of tibial plateau nonunions. The only complications following revision surgery were two instances of infection, one of which was in a patient with a prior history of infection. The infection rate following surgical correction of nonunion in this study was 6.7% (2/30), which is lower than prior reports of 13.6–21.0% following primary treatment of plateau fractures.2,24,25 The higher rate of infection in primary tibial plateau fractures is likely attributed to the difficulty managing the associated soft-tissue injury combined with the invasiveness of ORIF. As a result, ORIF of tibial plateau nonunions can be confidently managed without many of the associated risks inherent to primary plateau fractures.
Although most reports suggest nonunions should be treated operatively, one study achieved full ROM with POP casting in a patient with a Schatzker II nonunion and valgus knee deformity.26 Their patient had failed initial nonoperative management and refused surgery. Despite eventual union and full ROM, malalignment occurred in this patient likely due to lack of initial compressive forces and early weight bearing. Although a limited sample size, this suggests the potential for oligotrophic nonunions without adjacent structural injury as candidates for conservative treatment. If conservative treatment is chosen, establishing tibial alignment and stability are crucial in maximizing chances of eventual union. Poor reduction, wide displacement, or inadequate/uneven compressive forces may result in subsequent nonunion and post-traumatic arthrosis.14,26
In this review, average time from injury to nonunion revision was 8.7 months. This average time to revision may have been lower had patients received sufficient follow-up. Four patients in the review were categorized as having “neglected” nonunion without being evaluated or receiving follow-up prior to diagnosis.8 Previous research suggests tibial nonunion at six months can be predicted three months earlier based on radiographs and clinical history.27 As a result, early identification and revision surgery of fractures at risk for nonunion may prevent unfavorable outcomes.
Both flexion and extension scores improved post-revision from 115.4 and −8.4 to 127.9 and −5.8, respectively. Aggregate data of scoring systems could not be presented in this study due to the large variation between articles. Each of the studies used different clinical scores when assessing outcomes following revision of plateau nonunion. Measures used in these studies included SF36 physical and mental scores, the International Knee Documentation Committee (IKDC) score, Knee Society Rating pain and function subscales, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, Oxford Knee Score (OKS), Knee Function Grading System (Rasmussen), and the International Knee Society (IKS) score. This finding highlights the need for a universally accepted standard to assess outcomes following treatment of nonunion. Similarly, prior research has emphasized the need for consistent reporting following knee arthroplasty after a review identified 86 scoring systems used in 438 different studies.28
This review is not without limitations. First, the majority of the articles presented aggregate data of the cohort, rather than each patient. As a result, the authors could not deduce what treatment or outcomes coincided with particular characteristics of the nonunion. Similarly, aggregate data for revision plating preventing the authors from differentiating between revision plating systems. Second, many studies in the literature reported data on nonunions in combination with malunions. The inability to separate these data prevented the authors from including these studies in the review. Third, our review was limited to studies with a level of evidence of four (retrospective cohort studies and case reports). This is attributed to the low frequency of tibial plateau nonunions and subsequent difficulty in conducting prospective, randomized control trials with meaningful sample sizes. Lastly, the lack of a universally accepted definition of a tibial plateau nonunion was evident in this study. Only four (44.4%) of the studies in this review stated criteria used to classify nonunion.14,29, 30, 31 All four studies defined nonunion as no evidence of fracture healing at six months, with one of these studies noting a nonunion at four months. This differs from that established by the Food and Drug Administration (FDA), which defines a nonunion as “a fracture that is at least 9 months old and has not shown any signs of healing for 3 consecutive months.”32 Lack of a universally accepted definition of “nonunion” results in subjective interpretation and may induce variability between studies.
5. Conclusion
This study demonstrates the effectiveness of operative treatment, particularly autologous bone grafting and revision plating, for tibial plateau nonunions. Physicians may use these findings to guide decision making in the event of high energy plateau nonunions. In addition, the authors found various limitations within the current literature such as highly heterogenous outcome data and different definitions of nonunions, emphasizing the need for standardized reporting measures. Lastly, to overcome the limitation of sample size and statistical power, future research should involve multi-center studies between high-volume institutions.
Declaration of competing interest
None.
References
- 1.Ruffolo M.R., Gettys F.K., Montijo H.E., Seymour R.B., Karunakar M.A. Complications of high-energy bicondylar tibial plateau fractures treated with dual plating through 2 incisions. J Orthop Trauma. 2015;29(2):85–90. doi: 10.1097/BOT.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 2.Khatri K., Sharma V., Goyal D., Farooque K. Complications in the management of closed high-energy proximal tibial plateau fractures. Chin J Traumatol (Zhonghua Chuang Shang Za Zhi) 2016;19(6):342–347. doi: 10.1016/j.cjtee.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van den Berg J., Reul M., Nunes Cardozo M. Functional outcome of intra-articular tibial plateau fractures: the impact of posterior column fractures. Int Orthop. 2017;41(9):1865–1873. doi: 10.1007/s00264-017-3566-3. [DOI] [PubMed] [Google Scholar]
- 4.Manidakis N., Dosani A., Dimitriou R., Stengel D., Matthews S., Giannoudis P. Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. 2010;34(4):565–570. doi: 10.1007/s00264-009-0790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jagdev S.S., Pathak S., Kanani H., Salunke A. Functional outcome and incidence of osteoarthritis in operated tibial plateau fractures. Arch Bone Jt Surg. 2018;6(6):508–516. [PMC free article] [PubMed] [Google Scholar]
- 6.Rademakers M.V., Kerkhoffs G.M.M.J., Sierevelt I.N., Raaymakers E.L.F.B., Marti R.K. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21(1):5–10. doi: 10.1097/BOT.0b013e31802c5b51. [DOI] [PubMed] [Google Scholar]
- 7.Gross J.-B., Gavanier B., Belleville R., Coudane H., Mainard D. Advantages of external hybrid fixators for treating Schatzker V-VI tibial plateau fractures: a retrospective study of 40 cases. Orthop Traumatol Surg Res (OTSR) 2017;103(6):965–970. doi: 10.1016/j.otsr.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 8.Devgan A., Kamboj P., Gupta V., Magu N.-K., Rohilla R. Pseudoarthrosis of medial tibial plateau fracture----role of alignment procedure. Chin J Traumatol (Zhonghua Chuang Shang Za Zhi) 2013;16(2):118–121. [PubMed] [Google Scholar]
- 9.Molenaars R.J., Mellema J.J., Doornberg J.N., Kloen P. Tibial plateau fracture characteristics: computed tomography mapping of lateral, medial, and bicondylar fractures. J Bone Joint Surg Am. 2015;97(18):1512–1520. doi: 10.2106/JBJS.N.00866. [DOI] [PubMed] [Google Scholar]
- 10.Jiwanlal A., Jeray K.J. Outcome of posterior tibial plateau fixation. J Knee Surg. 2016;29(1):34–39. doi: 10.1055/s-0035-1564729. [DOI] [PubMed] [Google Scholar]
- 11.Wang J.-Y., Cheng C.-Y., Chen A.C.-Y., Chan Y.-S. Arthroscopy-assisted corrective osteotomy, reduction, internal fixation and strut allograft augmentation for tibial plateau malunion or nonunion. J Clin Med. 2020;9(4) doi: 10.3390/jcm9040973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu C.-C. Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch Orthop Trauma Surg. 2006;126(2):82–87. doi: 10.1007/s00402-006-0106-9. [DOI] [PubMed] [Google Scholar]
- 13.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toro-Arbelaez J.B., Gardner M.J., Shindle M.K., Cabas J.M., Lorich D.G., Helfet D.L. Open reduction and internal fixation of intraarticular tibial plateau nonunions. Injury. 2007;38(3):378–383. doi: 10.1016/j.injury.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Gardner M.J., Yacoubian S., Geller D. The incidence of soft tissue injury in operative tibial plateau fractures: a magnetic resonance imaging analysis of 103 patients. J Orthop Trauma. 2005;19(2):79–84. doi: 10.1097/00005131-200502000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Hunt K.J., Anderson R.B. Treatment of Jones fracture nonunions and refractures in the elite athlete: outcomes of intramedullary screw fixation with bone grafting. Am J Sports Med. 2011;39(9):1948–1954. doi: 10.1177/0363546511408868. [DOI] [PubMed] [Google Scholar]
- 17.Nauth A., Lane J., Watson J.T., Giannoudis P. Bone graft substitution and augmentation. J Orthop Trauma. 2015;29(Suppl 12):S34–S38. doi: 10.1097/BOT.0000000000000464. [DOI] [PubMed] [Google Scholar]
- 18.Pape H.C., Evans A., Kobbe P. Autologous bone graft: properties and techniques. J Orthop Trauma. 2010;24(Suppl 1):S36–S40. doi: 10.1097/BOT.0b013e3181cec4a1. [DOI] [PubMed] [Google Scholar]
- 19.Khan S.N., Tomin E., Lane J.M. Clinical applications of bone graft substitutes. Orthop Clin N Am. 2000;31(3):389–398. doi: 10.1016/s0030-5898(05)70158-9. [DOI] [PubMed] [Google Scholar]
- 20.Braly H.L., O’Connor D.P., Brinker M.R. Percutaneous autologous bone marrow injection in the treatment of distal meta-diaphyseal tibial nonunions and delayed unions. J Orthop Trauma. 2013;27(9):527–533. doi: 10.1097/BOT.0b013e31828bf077. [DOI] [PubMed] [Google Scholar]
- 21.Marino J.T., Ziran B.H. Use of solid and cancellous autologous bone graft for fractures and nonunions. Orthop Clin N Am. 2010;41(1):15–26. doi: 10.1016/j.ocl.2009.08.003. ; table of contents. [DOI] [PubMed] [Google Scholar]
- 22.Sun L., Li Z., Ma T. Treatment of atrophic nonunion via autogenous ilium grafting assisted by vertical fixation of double plates: a case series of patients. J Int Med Res. 2019;47(5):1998–2010. doi: 10.1177/0300060518814607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jain A., Kumar S., Aggarwal A.N., Jajodia N. Augmentation of bone healing in delayed and atrophic nonunion of fractures of long bones by partially decalcified bone allograft (decal bone) Indian J Orthop. 2015;49(6):637–642. doi: 10.4103/0019-5413.168764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang E.C., Weiner L., Strauss E., Sedlin E., Kelley M., Raphael J. Metaphyseal dissociation fractures of the proximal tibia. An analysis of treatment and complications. Am J Orthop (Belle Mead NJ) 1995;24(9):695–704. [PubMed] [Google Scholar]
- 25.Papagelopoulos P.J., Partsinevelos A.A., Themistocleous G.S., Mavrogenis A.F., Korres D.S., Soucacos P.N. Complications after tibia plateau fracture surgery. Injury. 2006;37(6):475–484. doi: 10.1016/j.injury.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 26.Sen R.-K., Soni A., Saini U.-C., Singh D. Internal fixation and bone grafting for intraarticular nonunion of tibial plateau: a report of four cases. Chin J Traumatol (Zhonghua Chuang Shang Za Zhi) 2011;14(6):371–375. [PubMed] [Google Scholar]
- 27.Yang J.S., Otero J., McAndrew C.M., Ricci W.M., Gardner M.J. Can tibial nonunion be predicted at 3 months after intramedullary nailing? J Orthop Trauma. 2013;27(11):599–603. doi: 10.1097/BOT.0b013e31828f5821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Theodoulou A., Bramwell D.C., Spiteri A.C., Kim S.W., Krishnan J. The use of scoring systems in knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2016;31(10):2364–2370. doi: 10.1016/j.arth.2016.05.055. e8. [DOI] [PubMed] [Google Scholar]
- 29.Kloen P., Buijze G.A., Ring D. Management of forearm nonunions: current concepts. Strat Trauma Limb Reconstr. 2012;7(1):1–11. doi: 10.1007/s11751-011-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matsumura T., Nakashima M., Takahashi T., Takeshita K. Clinical outcomes of open reduction and internal fixation for intra-articular complex tibial plateau non-union with 3-year minimum follow-up. J Orthop Sci Off J Jpn Orthop Assoc. 2020 doi: 10.1016/j.jos.2020.04.003. Published online May 7. [DOI] [PubMed] [Google Scholar]
- 31.Chan D.B., Jeffcoat D.M., Lorich D.G., Helfet D.L. Nonunions around the knee joint. Int Orthop. 2010;34(2):271–281. doi: 10.1007/s00264-009-0924-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cunningham B.P., Brazina S., Morshed S., Miclau T. Fracture healing: a review of clinical, imaging and laboratory diagnostic options. Injury. 2017;48:S69–S75. doi: 10.1016/j.injury.2017.04.020. [DOI] [PubMed] [Google Scholar]