Abstract
Background
Cement augmentation of internal fixation of hip fracture has reported to improve fracture stability in osteoporotic hip fractures, reducing the risk of cut-out of the sliding screw through the femoral head. The purpose of present study was to perform a systematic literature review on the effects of augmentation technique in patients with osteoporotic hip fractures.
Material and methods
A comprehensive literature search was systematically performed to evaluate all papers published in English language included in the literature between January 2010 and July 2020, according to the PRISMA 2009 guidelines. In vivo and in vitro studies, case reports, review articles, cadaveric studies, biomechanical studies, histological studies, oncological studies, technical notes, studies dealing with radiological classifications and studies on revision surgery were excluded.
Results
A total of 5 studies involving 301 patients were included. Patients had a mean age of 84.6 years and were followed up for a mean period of 11 months. The proximal femoral fractures were stabilized with implantation of the PFNA or Gamma nail and augmentation was performed with two different cements: polymethylmethacrylate (PMMA) in 4 studies and calcium phosphate (CP) in one study. Overall, 57.5% of patients reached the same or greater preoperative mobility, and postoperative Parker Mobility Score and Harris Hip Score were acceptable. No significantly complications were observed, and no additional surgery related to the implant was required.
Conclusion
The results of this systematic review show that cement augmentation is a safe and effectiveness method of fixation to treat trochanteric fractures.
Keywords: Cement augmentation, Femur fracture, Cut-out risk, Screw mobilization, Osteoporosis
1. Introduction
Trochanteric hip fractures are frequent injuries affecting the elderly,1 and their incidence has substantially increased due to the demographic changes demonstrating progressive ageing.2,3 Often these fractures are the result of a simple fall, or minor trauma,5 with main predisposing factors represented by increased bone fragility related to ageing and osteoporosis.4 The elevated frequency of such fractures produces a high economic impact, with a yearly estimated cost in UK of £ 1130 millions.6 The functional outcomes of these patients are determined by surgical timing, previous health status and associated comorbidities.7 Fixation of trochanteric hip fractures with nail or sliding screw plate represents the gold standard of treatment.8,9 However, in patients with severe osteoporosis and unstable trochanteric fractures, stable and reliable fixation are difficult to achieve,10 and overall rates for mechanical failure have been reported up to 20.5%.11 The most frequent nail-related complications are secondary loss of reduction and implant migration.12 Further, cut-out of the sliding screw through the femoral head represent a complication widely described in the literature,13, 14, 15 with an incidence between 2% and 8%,16,17 resulting one of the main reasons of revision surgery.18 To improve implant anchorage, cement augmentation of the implant has been employed leading to an increase of the load-bearing area of the device, with consequent higher stability and reduction of the risk of implant failure.19, 20, 21 Several biomechanical investigations were performed concerning the use of Polymethyl Methacrylate (PMMA) or calcium phosphate (CP) for the augmentation of intramedullary femoral nail, showing a higher cut-out resistance.22, 23, 24
Primary aim of present paper was to perform a systematic and qualitative review of the current literature to evaluate the effectiveness of cement augmentation of intramedullary devices as an adjunct to internal fixation of trochanteric hip fractures.
2. Material and methods
A systematic review was conducted according to the guidelines presented in the PRISMA Statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).25 Three independent clinical researchers (L.S., S.R. and F.M.) performed an extensive search on PubMed, Cochrane, Medline, Embase and Google Scholar electronic databases for all studies published between January 2010 and July 2020. Only papers published in English language were included. To reduce and minimize the number of missed studies, no filters were applied to the search strategies. The following MeSH entries were used for research articles: augmentation nail cut-out, nail cut-out cement, augmentation cut-out femur, cut-out femur nail, augmentation femoral cut-out, nail cement fracture, nail femoral cut-out, femur nail augmentation, femoral nail augmentation, femur nail failure, femoral nail failure. Animal in vivo and human in vitro studies, case reports, review articles, cadaveric studies, biomechanical studies, histological studies, oncological studies, technical notes, studies dealing with radiological classifications and studies on revision surgery were not included. Only studies evaluating quantifiable functional outcomes with validate scores were included. Papers were initially identified based on the title and abstract. The investigators separately reviewed the abstract of each publication and then performed an accurate reading of all extended papers to minimize bias. Further, researchers checked all the references from the identified articles in order to not miss any relevant study. Moreover, if an agreement of studies inclusion/exclusion was not achieved, the senior author (L.C.) was consulted for the final decision and a consensus was reached through discussion. Relevant data were extracted and recorded by two authors (L.S., S.R.) from each included study according to the following standardized protocol: authors and year of publication, country, study type, patient demographics (age, gender, type of fracture), surgical technique details, implants and cements used for fracture fixation, duration of follow-up and clinical outcomes. In addition, the incidence of intraoperative complications and the need of additional surgery was calculated for individual studies. The extracted data were then cross-checked for accuracy and checked by a third author (F.M.). The flow chart illustrates the number of studies that have been identified, included, and excluded and the reasons for exclusion.26 Two investigators (L.S., S.R.) assessed the methodological quality of the selected studies according to the Modified Coleman Methodology Score (CMS), after agreement between two investigators.27 Meta-analysis and statistical analysis were not feasible due to substantial heterogeneity between studies (different types of implants used in different studies, differences in cement used and differences in patient/fracture related variables), varying methodology and lack of direct comparative results.28 The Newcastle-Ottawa Quality Assessment Scale (NOS) was used to assess the quality of observational studies29 and the study quality assessment was performed by 2 reviewers independently (L.S. and S.R.). The NOS items were based on 3 dimensions: selection of study groups, comparability of the groups, and ascertainment of either the exposure or outcome of interest. We classified quality on the basis of 3 levels (total score was 9): high quality, with scores between 8 and 9; moderate quality, with scores between 5 and 7; and low quality, with scores between 0 and 4. Only articles with high or moderate quality were considered for the study (Table 1).
Table 1.
Studies included in the Review. Abbreviations: PMMA = polymethylmethacrylate; CP = calcium phosphate; PFNA = Proximal Femur Nail Antirotation.
| Authors | Year | Synthesis (nail/cement) | Country | Study type | Modified Coleman methodology score | Newcastle-Ottawa Scale (NOS) |
|---|---|---|---|---|---|---|
| Dall’Oca et al.32 | 2010 | Gamma 3/PMMA (Mendec Spine®) | Italy | Randomized Controlled trial | 54 | 8 |
| Kammerlander et al.20 | 2011 | PFNA/PMMA (Traumacem V + ®) | Multicentric | Prospective study | 49 | 7 |
| Kammerlander et al.19 | 2013 | PFNA/PMMA (Traumacem V + ®) | Multicentric | Prospectivestudy | 50 | 7 |
| Kammerlander et al.30 | 2018 | PFNA/PMMA (Traumacem V + ®) | Multicentric | Randomized Controlled trial | 60 | 8 |
| Kim et al.31 | 2018 | PFNA/CP (Gene X®) | South Korea | Retrospective study | 47 | 6 |
3. Results
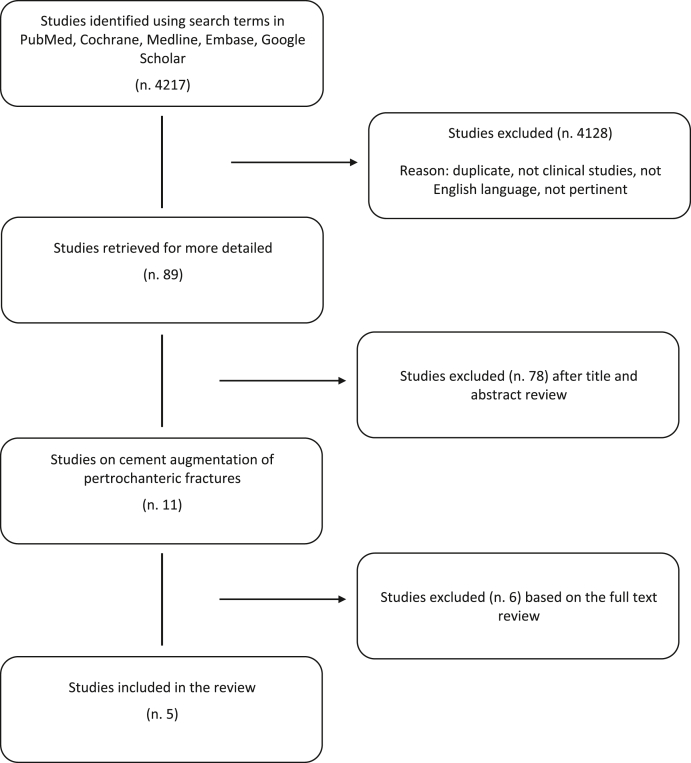
Of 4217 articles, 5 full-text articles were identified for review19,20,30, 31, 32 (Fig. 1). No agreement was reached between two investigators (LS, SR) regarding the inclusion of a study.21 Concerning this study, the senior author (LC) decided to exclude that article because of its close similarity to another study by the same authors.19 The articles included were published between 2010 and 2018. The evaluation of the quality of the included articles revealed that there were 2 prospective trials,19,20 1 retrospective trial31 and 2 randomized controlled trials.30,32 Only patients of the treatment group (cement augmentation) were extrapolated and included in the review. The mean Modified Coleman Methodology Score was 52 (range from 49 to 60) and all the five studies had a NOS>4 demonstrating good methodologic quality (Table 1).
Fig. 1.
Flow diagram that describe the number of studies identified, included, and excluded as well as the reasons for exclusion.
3.1. Demographic data
The pooled number of patients treated with cement augmentation femoral nail for trochanteric fracture fixation included in this review was 301, of whom 71 (23.6%) were male and 230 (76.0%) were female (Table 2). The mean age across all studies was 84.6 ± 1.75 years, (range 67–97 years). The follow-up range across all studies was 4–15.3 months, with a mean of 11 ± 4.2 months. All articles used AO/OTA system (Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association) to include patients in each study: specifically, two studies19,20 treated 31-A1, A2, A3 and three studies30, 31, 32 treated 31-A2, A3 fractures.
Table 2.
Demographic data and treatment information. Abbreviations. N = number; % = percentage.
| Authors | Number of patients | Age (mean) | FemaleN (%) | Male N (%) | Type of Fracture | Cement injected (ml) | Follow-up (months) | IntraoperativeComplications | Complications requiring additional surgery |
|---|---|---|---|---|---|---|---|---|---|
| Dall’Oca et al.32 | 35 | 85.4 | 24 (68.6%) | 11 (31.4%) | AO 31-A2, A3 | 3 | 12 | 1 little amount of cement was extravasated into the hip joint | none |
| Kammerlander et al.20 | 59 | 84.5 | 45 (76.3%) | 14 (24.7%) | AO 31-A1, A2, A3 | 4.2 | 4 | 1 perforation of the k-wire into the hip joint | none |
| Kammerlander et al.19 | 62 | 85.3 | 49 (79.0%) | 13 (21.0%) | AO 31-A1, A2, A3 | 3.8 | 15.3 | 3 open reduction, 2 treated with subtrochanteric cerclage wires | none |
| Kammerlander et al.30 | 105 | 86.1 | 87 (82.8%) | 18 (17.2%) | AO 31-A2, A3 | 3.8 | 12 | 1 cement leakage | none |
| Kim et al.31 | 40 | 81.6 | 25 (62.5%) | 15 (37.5%) | AO 31-A2, A3 | 5 | 12 | 2 superficial wound infection | none |
3.2. Surgical techniques
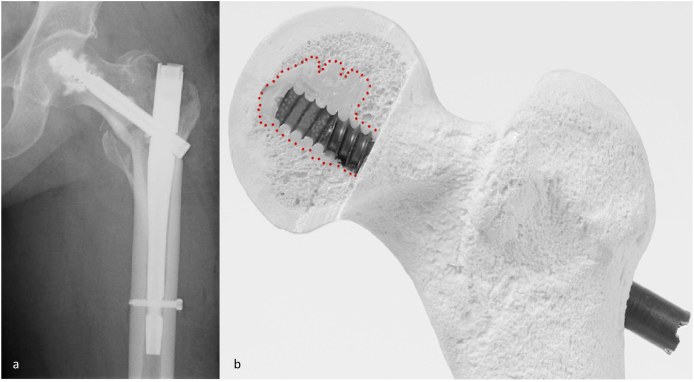
The proximal femoral fractures were reduced and stabilized with Proximal Femur Nail Antirotation (PFNA) (DePuy Synthes, Oberdorf, Switzerland) in 4 studies19,20,30,31 while one study32 Gamma 3 nail (Stryker Trauma GmbH, Schoenkirchen, Germany) using a standard surgical technique. All operations were performed according to standard operating procedures of each femoral nail that provide anatomical reduction of the fracture, guidewire placement and intramedullary nail insertion. After that, the femoral neck screw was inserted in the third inferior portion of the femoral head trough the calcar of the neck. The distal fixation screw was fixed in a static locking mode regardless of the fracture type based on the surgeon’s preference. Where necessary, an open reduction was performed.19 A polymethylmethacrylate (PMMA) was used in 4 studies (Traumacem V + ®19,20,30 or Mendec Spine®32) and was placed through a perforate blade of the PFNA or through the head screw of the Gamma 3 nail implant (Fig. 2). In one study31 the calcium phosphate (CP) Cement (Gene X®) was inserted into the femoral head before the insertion of the neck blade of PFNA nail. In all studies the injection of cement was performed under fluoroscopic control. The mean amount of cement injected was 3.7 ± 0.5 ml in patients treated with PMMA and 5 ml in patients treated with CP. In postoperative time, all patients had a surgeon indication to walk again the day after surgery with rehab of the free weight bearing or as tolerated, according to clinical conditions.
Fig. 2.
A) The radiograph shows fixation with Gamma nail and augmentation with cement in patient with trochanteric fracture. B) Image shows femoral neck screw insertion and the red area shows the cement distribution area.
3.3. Patient reported outcome measures
The main clinical outcomes, focused on the postoperative mobility of patients in relation to their pre-fracture condition (Table 3): the 57.5% of patients reached the same or greater preoperative mobility. The Parker Mobility score,33 evaluated in 3 of 5 studies,19,20,30 was 5.4 ± 1.14 before fracture and 4.8 ± 1.06 at the last follow-up visit. The Harris Hip Score,34 was used to evaluate clinical outcome in 2 of 5 studies,31,32 with a result of 59.9 ± 4.88 before fracture and of 61.6 ± 5.3 at final visit. The visual analog scale (VAS),35 was evaluated in 3 studies19,20,31 showing a disappearance of pain in patients during the follow up. The postoperative range of motion of the hip was not described in these studies.
Table 3.
Post-operative outcomes of studies reviewed. Abbreviations: Pre-op = Pre-operative; Post-op = Post-operative.
| Authors | Post-op weight bearing | Harris Hip Score |
Parker Mobility score |
Patients reached their prefracture mobility (%) | ||
|---|---|---|---|---|---|---|
| Pre-op | Last follow-up | Pre-op | Last follow-up | |||
| Dall’Oca et al.32 | Full (Day 1 post-op | 56.5 | 57.9 | N/A | N/A | N/A |
| Kammerlander et al.20 | N/A | N/A | N/A | 4.5 | 3.8 | 55.3 |
| Kammerlander et al.19 | N/A | N/A | N/A | 5.1 | 4.6 | 59.6 |
| Kammerlander et al.30 | Full as tolerated (Day 1 post-op) | N/A | N/A | 6.7 | 5.9 | N/A |
| Kim et al.31 | Partial the first 2 weeks after surgery and continued for at least 8 weeks | 63.4 (6 months | 65.4 | N/A | N/A | N/A |
3.4. Fixation failures and complications
Two intraoperative complications related to cement augmentation were described, including a little amount of cement extravasated into the hip joint without clinical problems for the patient,32 and cement leakage into the joint30 with exclusion from the study of this patient. A third intra-operative complication reported20 was unrelated with the cement injection. A perforation of the k-wire into the hip joint was observed and, consequently, no cement augmentation was performed in this patient. An open reduction was necessary in three cases,19 whereas in 2 cases a subtrochanteric cerclage wires was used to stabilize the reduction. The procedure was well tolerated with no fixation failure. Any cases of avascular femoral head necrosis were observed. Further, no hypersensitivity or allergy to the cement was noted. Finally, no additional surgery related to the implant was required.
4. Discussion
The results of present review seem to indicate that cement augmentation in the treatment of trochanteric fractures provides good clinical outcome and prevent fixation failure, with 57.5% of patients reaching the same or greater preoperative mobility, and with no additional surgery related to the implant failure.
In elderly patients, trochanteric fractures are often associated with osteoporosis and the correct implant placement is related to fracture reduction and implant fixation.36 The poor bone stock and an inadequate reduction are still the main reasons for failure.37 The shear stress generated on the femoral head with the loading during regular walking can induce varus collapse or the cut-out of the femoral neck screw.38,39 The PFNA possesses a helical blade that give a rotational stability, cut-out resistance and lower reoperation rates for unstable fractures.40 Indeed, as evidenced by the analyzed articles, this surgical procedure was not associated with fixation failure, and cement augmentation of the proximal femur resulted an additional option for failure prevention. The effectiveness of this treatment has been also confirmed by several biomechanical studies that demonstrated the increase of cut-out resistance and rotational stability with PMMA or CP augmentation.22,41,42 In a recent prospective study, Rai et al.43 described a similar method of bone cement augmentation with PMMA in the femoral head, using fixation with dynamic hip screw to prevent cut out, with good outcome results.
The increased mechanical stability with PMMA or CP also contributed to have a shorter period of hospitalization due to a faster mobilization, with earlier return to the daily activities.44 Analyzing the functional outcomes, 57.5% of the patients reached the same or greater preoperative mobility. The mean values of postoperative Harris Hip Score and the slight downward trend of Parker Mobility Score were acceptable and satisfactory in relation with the mean age of 84.6 years of the patients, while, according with the literature,45, 46, 47 comorbidities represented an important factor with negative influence the recovery achieving. Confirming these results, two recent publications,48,49 not included in this systematic review because functional Parker Mobility and Harris Hip scores were not evaluated, demonstrated that cement augmentation with PFNA improved the postoperative functional outcomes, increasing the return to pre-fracture ambulatory level (RPAL) in geriatric patients with a high-surgical-risk.
The authors of the articles analyzed in this review tried to address poor bone quality and comminution with PMMA or CP augmentation, however, many others studies on different augmentation strategies are reported. Pesce et al.50 studied the fixation with nail and cephalic hydroxyapatite coated screws, Gao et al.51 and Kulkarni et al.52 studied the augmentation with a wiring cerclage, and Gadegone et al.53 analyzed the stabilization of lateral trochanteric wall with an additional screw.
Of the 301 patients included in the review, none had complications such as failure of fracture fixation. Regarding the complications related to cement augmentation, a small amount of extravasation in hip joint occurred in 1 patient,32 and cement leakage in another.30 However, no revision surgery was necessary in both cases. As suggested by Von der Linden et al.,22 the injection of small amount of cement does not induce significantly thermal changes, hence this explains the absence of thermal osteonecrosis that might be induced by the exothermic reaction occurring during the cement polymerization.54,55 This could be a disadvantage particularly for PMMA22,55 because CP has a lower polymerization temperature.56
Comparing cement augmentation using PMMA19,20,30,32 or CP,31 no differences in terms of results or complications were found. Confirming these data, Linder et all57 in a review demonstrated that both PMMA and CP cements increase the primary stability of the implant-bone construct in all biochemical and clinical studies. Even though PMMA is widely used more than CP with good results and is considered the gold standard of bone cement, especially in vertebral surgery,58,59 CP also has several studies showing its effectiveness.60 Despite the excellent results found with these types of cements the research is oriented to provide cements offering better injectability, good resistance to disintegration, radiopacity and optimal mechanical stability.61,62
The present review has several limitations due to the low-grade evidence of the studies such as their retrospective design, the shortness of the follow up, and the absence of controls in most reports. In addition, the different outcome measures contributed to increase the possible biases. Therefore, despite the encouraging results, no definitive conclusions can be drawn, and long-term, controlled trials are required to better address the efficacy of cement augmentation for femur fracture repair.
5. Conclusion
The results of this systematic review show that cement augmentations with PMMA or CP are a safe method of fixation to treat trochanteric fractures. Good functional results without any reported cement-associated complications were observed. However, more clinical researches are necessary to determine the extent of their benefit.
Declaration of competing interest
None.
Footnotes
All authors have seen and approved the final manuscript, which we hope will meet with your approval.The manuscript has been reviewed and approved by all co-authors. The authors certify that the paper has not been published (in part or in full) or submitted for publication elsewhere. We certify that each of the authors have made a substantial contribution so as to qualify to the authorship. All authors have disclosed all financial support for this work and other potential conflict of interests.
References
- 1.Baron J.A., Karagas M., Barrett J. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Sandmann G., Biberthaler P. Pertrochanteric femoral fractures in the elderly. Unfallchirurg. 2015;118:447–460. doi: 10.1007/s00113-015-0007-x. [DOI] [PubMed] [Google Scholar]
- 3.Azagra R., Lopez-Exposito F., Martin-Sanchez J.C. Changing trends in the epidemiology of hip fracture in Spain. Osteoporos Int. 2014;25:1267–1274. doi: 10.1007/s00198-013-2586-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nikolaou V.S., Efstathopoulos N., Kontakis G., Kanakaris N.K., Giannoudis P.V. The influence of osteoporosis in femoral fracture healing time. Injury. 2009;40:663–668. doi: 10.1016/j.injury.2008.10.035. [DOI] [PubMed] [Google Scholar]
- 5.Tsuda T. Epidemiology of fragility fractures and fall prevention in the elderly: a systematic review of the literature. Curr Orthop Pract. 2017;28:580–585. doi: 10.1097/BCO.0000000000000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leal J., Gray A.M., Prieto-Alhambra D. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. 2016;27:549–558. doi: 10.1007/s00198-015-3277-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mendelson D.A., Friedman S.M. Principles of comanagement and the geriatric fracture center. Clin Geriatr Med. 2014;30:183–189. doi: 10.1016/j.cger.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Gardner M.J., Lorich D.G., Lane J.M. Osteoporotic femoral neck fractures: management and current controversies. Instr Course Lect. 2004;53:427–439. [PubMed] [Google Scholar]
- 9.Nishiura T., Nozawa M., Morio H. The new technique of precise insertion of lag screw in an operative treatment of trochanteric femoral fractures with a short intramedullary nail. Injury. 2009;40:1077–1083. doi: 10.1016/j.injury.2009.03.049. [DOI] [PubMed] [Google Scholar]
- 10.Kashigar A., Vincent A., Gunton M.J., Backstein D., Safir O., Kuzyk P.R. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Jt J. 2014;96:1029–1034. doi: 10.1302/0301-620X.96B8.33644. [DOI] [PubMed] [Google Scholar]
- 11.Liu W., Zhou D., Liu F., Weaver M.J., Vrahas M.S. Mechanical complications of intertrochanteric hip fractures treated with trochanteric femoral nails. J Trauma Acute Care Surg. 2013;75:304–310. doi: 10.1097/TA.0b013e31829a2c43. [DOI] [PubMed] [Google Scholar]
- 12.Knobe M., Munker R., Sellei R.M. Unstable pertrochanteric femur fractures. Failure rate, lag screw sliding and outcome with extra- and intramedullary devices (PCCP, DHS and PFN) Z für Orthop Unfallchirurgie. 2009;147:306–313. doi: 10.1055/s-0029-1185349. [DOI] [PubMed] [Google Scholar]
- 13.Morvan A., Boddaert J., Cohen-Bittan J., Picard H., Pascal-Mousselard H., Khiami F. Risk factors for cut-out after internal fixation of trochanteric fractures in elderly subjects. Orthop Traumatol Surg Res. 2018;104:1183–1187. doi: 10.1016/j.otsr.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 14.Buyukdogan K., Caglar O., Isik S., Tokgozoglu M., Atilla B. Risk factors for cut-out of double lag screw fixation in proximal femoral fractures. Injury. 2017;48:414–418. doi: 10.1016/j.injury.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Bojan A.J., Beimel C., Taglang G., Collin D., Ekholm C., Jönsson A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Muscoskel Disord. 2013;14:1. doi: 10.1186/1471-2474-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yaozeng X., Dechun G., Huilin Y., Guangming Z., Xianbin W. Comparative study of trochanteric fracture treated with the proximal femoral nail anti-rotation and the third generation of gamma nail. Injury. 2010;41:1234–1238. doi: 10.1016/j.injury.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Ma K.L., Wang X., Luan F.J. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop. Traumatol. Surg. Res. 2014;100:859–866. doi: 10.1016/j.otsr.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 18.Brunner A., Buttler M., Lehmann U. What is the optimal salvage procedure for cut-out after surgical fixation of trochanteric fractures with the PFNA or TFN? A multicentre study. Injury. 2016;47:432–438. doi: 10.1016/j.injury.2015.11.027. [DOI] [PubMed] [Google Scholar]
- 19.Kammerlander C., Doshi H., Gebhard F. Long- term results of the augmented PFNA: a prospective multicenter trial. Arch Orthop Trauma Surg. 2014;134:343–349. doi: 10.1007/s00402-013-1902-7. [DOI] [PubMed] [Google Scholar]
- 20.Kammerlander C., Gebhard F., Meier C. Standardised cement augmentation of the PFNA using a perforated blade: a new technique and preliminary clinical results: a prospective multicentre trial. Injury. 2011;42:1484–1490. doi: 10.1016/j.injury.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Neuerburg C., Mehaffey S., Gosch M., Bocker W., Blauth M., Kammerlander C. Trochanteric fragility fractures: treatment using the cement-augmented proximal femoral nail antirotation. Operat Orthop Traumatol. 2016;28:164–176. doi: 10.1007/s00064-016-0449-5. [DOI] [PubMed] [Google Scholar]
- 22.Von der Linden P., Gisep A., Boner V., Windolf M., Appelt A., Suhm N. Biomechanical evaluation of a new augmentation method for enhanced screw fixation in osteoporotic proximal femoral fractures. J Orthop Res. 2006;24:2230–2237. doi: 10.1002/jor.20299. [DOI] [PubMed] [Google Scholar]
- 23.Erhart S., Schmoelz W., Blauth M., Lenich A. Biomechanical effect of bone cement augmentation on rotational stability and pull-out strength of the proximal femur nail antirotation. Injury. 2011;42:1322–1327. doi: 10.1016/j.injury.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Eriksson F., Mattsson P., Larsson S. The effect of augmentation with resorbable or conventional bone cement on the holding strength for femoral neck fracture devices. J Orthop Trauma. 2002;16:302–310. doi: 10.1097/00005131-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 26.Moher D., Cook D.J., Eastwood S., Olkin I., Rennie D., Stroup D.F. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 27.Coleman B., Khan K., Maffulli N., Cook J.L., Wark J.D. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 28.Higgins J.P., Green S. Wiley Online Library; 2008. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- 29.Wells G.A., Shea B.J., O’Connell D. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. Appl Eng Agric. 2014;18(6):727–734. [Google Scholar]
- 30.Kammerlander C., Hem E.S., Klopfer T. Cement augmentation of the Proximal Femoral Nail Antirotation (PFNA) - a multicentre randomized controlled trial. Injury. 2018;49:1436–1444. doi: 10.1016/j.injury.2018.04.022. [DOI] [PubMed] [Google Scholar]
- 31.Kim S.J., Park H.S., Lee D.W., Lee J.W. Is calcium phosphate augmentation a viable option for osteoporotic hip fractures? Osteoporos Int. 2018;29:2021–2028. doi: 10.1007/s00198-018-4572-z. [DOI] [PubMed] [Google Scholar]
- 32.Dall’Oca C., Maluta T., Moscolo A., Lavini F., Bartolozzi P. Cement augmentation of intertrochanteric fractures stabilised with intramedullary nailing. Injury. 2010 Nov;41:1150–1155. doi: 10.1016/j.injury.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 33.Parker M.J., Palmer C.R. A new mobility score for predicting mortality after hip fracture. J Bone Jt Surg Br. 1993;75:797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 34.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end- result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 35.Jensen M.P., Chen C., Brugger A.M. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4:407–414. doi: 10.1016/s1526-5900(03)00716-8. [DOI] [PubMed] [Google Scholar]
- 36.Baumgaertner M., Curtin S., Lindskog D., Keggi J. The value of the tip-apex distance in predicting failure of fixation of pertrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 37.Lenich A., Vester H., Nerlich M., Mayr E., Stöckle U., Füchtmeier B. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip- blade vs screw. Injury. 2010;41:1292–1296. doi: 10.1016/j.injury.2010.07.499. [DOI] [PubMed] [Google Scholar]
- 38.Pervez H., Parker M.J., Vowler S. Prediction of fixation failure after sliding hip screw fixation. Injury. 2004;35:994–998. doi: 10.1016/j.injury.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 39.Knobe M., Drescher W., Heussen N., Sellei R.M., Pape H.C. Is helical blade nailing superior to locked minimally invasive plating in unstable pertrochanteric fractures? Clin Orthop Relat Res. 2012;470:2302–2312. doi: 10.1007/s11999-012-2268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo Y., Yang H.P., Dou Q.J., He X.B., Yang X.F. Efficacy of femoral nail anti-rotation of helical blade in unstable intertrochanteric fracture. Eur Rev Med Pharmacol Sci. 2017;21:6–11. [PubMed] [Google Scholar]
- 41.Elder S., Frankenburg E., Goulet J., Yetkinler D., Poser R., Goldstein S. Biomechanical evaluation of calcium phosphate cement-augmented fixation of unstable intertrochanteric fractures. J Orthop Trauma. 2000;14:386–393. doi: 10.1097/00005131-200008000-00002. [DOI] [PubMed] [Google Scholar]
- 42.Sermon A., Boner V., Schwieger K. Biomechanical evaluation of bone-cement augmented Proximal Femoral Nail Antirotation blades in a polyurethane foam model with low density. Clin Biomech. 2012;27:71–76. doi: 10.1016/j.clinbiomech.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 43.Rai A.K., Goel R., Bhatia C., Singh S., Thalanki S., Gondane A. Cement augmentation of dynamic hip screw to prevent screw cut out in osteoporotic patients with intertrochanteric fractures: a case series. Hip Pelvis. 2018;30:269–275. doi: 10.5371/hp.2018.30.4.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mattsson P., Alberts A., Dahlberg G., Sohlman M., Hyldahl H.C., Larsson S. Resorbable cement for the augmentation of internally-fixed unstable trochanteric fractures. A prospective, randomised multicentre study. J Bone Joint Surg Br. 2005;87:1203–1209. doi: 10.1302/0301-620X.87B9.15792. [DOI] [PubMed] [Google Scholar]
- 45.Donegan D.J., Gay A.N., Baldwin K., Morales E.E., Esterhai J.L., Mehta S. Use of medical comorbidities to predict complications after hip fracture surgery in the elderly. J Bone Joint Surg Am. 2010;92:807–813. doi: 10.2106/JBJS.I.00571. [DOI] [PubMed] [Google Scholar]
- 46.Roche J.J., Wenn R.T., Sahota O., Moran C.G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roth T., Kammerlander C., Gosch M., Luger T.J., Blauth M. Outcome in geriatric fracture patients and how it can be improved. Osteoporos Int. 2010;21:S615–S619. doi: 10.1007/s00198-010-1401-4. [DOI] [PubMed] [Google Scholar]
- 48.Kulachote N., Sa-ngasoongsong P., Sirisreetreerux N., Chulsomlee K., Thamyongkit S. Predicting factors for return to prefracture ambulatory level in high surgical risk elderly patients sustained intertrochanteric fracture and treated with proximal femoral nail antirotation (PFNA) with and without cement augmentation. Geriatr Orthop Surg Rehabil. 2020;11 doi: 10.1177/2151459320912121. 2151459320912121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yee D.K.H., Lau W., Tiu K.L. Cementation: for better or worse? Interim results of a multi-centre cohort study using a fenestrated spiral blade cephalomedullary device for pertrochanteric fractures in the elderly. Arch Orthop Trauma Surg. 2020:1–8. doi: 10.1007/s00402-020-03449-9. [DOI] [PubMed] [Google Scholar]
- 50.Pesce V., Maccagnano G., Vicenti G. The effect of hydroxyapatite coated screw in the lateral fragility fractures of the femur. A prospective randomized clinical study. J Biol Regul Homeost Agents. 2014;28:125–132. [PubMed] [Google Scholar]
- 51.Gao Y.S., Guo Y.J., Yu X.G., Chen Y., Chen C., Lu N.J. A novel cerclage wiring technique in intertrochanteric femoral fractures treated by intramedullary nails in young adults. BMC Muscoskel Disord. 2018;19:359. doi: 10.1186/s12891-018-2284-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kulkarni S.G., Babhulkar S.S., Kulkarni S.M., Kulkarni G.S., Kulkarni M.S., Patil R. Augmentation of intramedullary nailing in unstable intertrochanteric fractures using cerclage wire and lag screws: a comparative study. Injury. 2017;48:S18–S22. doi: 10.1016/S0020-1383(17)30489-8. [DOI] [PubMed] [Google Scholar]
- 53.Gadegone W.M., Shivashankar B., Lokhande V., Salphale Y. Augmentation of proximal femoral nail in unstable trochanteric fractures. SICOT J. 2017;3:12. doi: 10.1051/sicotj/2016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Heini P.F., Franz T., Fankhauser C., Gasser B., Ganz R. Femoroplasty-augmentation of mechanical properties in the osteoporotic proximal femur: a biomechanical investigation of PMMA reinforcement in cadaver bones. Clin Biomech. 2004;19:506–512. doi: 10.1016/j.clinbiomech.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 55.Li S., Chien S., Branemark P.I. Heat shock-induced necrosis and apoptosis in osteoblasts. J Orthop Res. 1999;17:891–899. doi: 10.1002/jor.1100170614. [DOI] [PubMed] [Google Scholar]
- 56.Larsson S., Bauer T.W. Use of injectable calcium phosphate cement for fracture fixation: a review. Clin Orthop. 2002;395:23–32. doi: 10.1097/00003086-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 57.Lindner T., Kanakaris N.K., Marx B., Cockbain A., Kontakis G., Giannoudis P.V. Fractures of the hip and osteoporosis: the role of bone substitutes. J Bone Joint Surg Br. 2009;91:294–303. doi: 10.1302/0301-620X.91B3.21273. [DOI] [PubMed] [Google Scholar]
- 58.He Z., Zhai Q., Hu M. Bone cements for percutaneous vertebroplasty and balloon kyphoplasty: current status and future developments. J Orthop Translat. 2015;3:1–11. doi: 10.1016/j.jot.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yi S., Rim D.C., Park S.W., Murovic J.A., Lim J., Park J. Biomechanical comparisons of pull out strengths after pedicle screw augmentation with hydroxyapatite, calcium phosphate, or polymethylmethacrylate in the cadaveric spine. World Neurosurg. 2015;83:976–981. doi: 10.1016/j.wneu.2015.01.056. [DOI] [PubMed] [Google Scholar]
- 60.Maestretti G., Sutter P., Monnard E. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J. 2014;23:1354–1360. doi: 10.1007/s00586-014-3206-1. [DOI] [PubMed] [Google Scholar]
- 61.Zhu T., Ren H., Li A. Novel bioactive glass based injectable bone cement with improved osteoinductivity and its in vivo evaluation. Sci Rep. 2017;7:3622. doi: 10.1038/s41598-017-03207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brueckner T., Heilig P., Jordan M.C. Biomechanical evaluation of promising different bone substitutes in a clinically relevant test set-up. Materials. 2019;12 doi: 10.3390/ma12091364. [DOI] [PMC free article] [PubMed] [Google Scholar]