Abstract
Objective
High tibial osteotomy (HTO) is an established procedure to treat medial compartmental osteoarthritis (OA) knee associated with varus deformity. It is well documented that precise correction of deformity and maintenance of correction achieved is important to ensure long term good results. This study was undertaken to record changes in radiological parameters and its effect on the functional outcomes in first two years following HTO done for varus degenerative OA kneeby hemicallotasis technique using HTO fixator.
Methods
31 patients meeting our inclusion-exclusion criteria who underwent HTO by hemicallotasis method using self-adjusting unilateral HTO fixator were included in the study. Their femoro tibial angle (FTA), mechanical axis %, Insall- Salvati ratio, proximal tibial antero-posterior slope and knee injury and osteoarthritis outcome Score (KOOS) were recorded preoperatively, postoperatively at the time of removal of fixator, at 1 year and at 2 years.
Results
The FTA and mechanical axis significantly improved from a mean of 183.12⁰ and −3.26% respectively preoperatively to 173.38⁰ and 61.81% at the time of removal of fixator but subsequently showed significant deterioration to 176.06⁰ and 57.96% at 1 year and further insignificant deterioration to 176.16⁰ and 57.74 at 2 years. The KOOS improved from mean 56.61 preoperatively to 70.48 at the time of fixator removal and further improved significantly to 85.68 at 1 year but significantly deteriorated to 84.54 at 2 years. The Insall-Salvati ratio, tibial slope showed no significant change throughout the study. Conclusion: Though desired alignment can be achieved by using the fixator, we found a significant deterioration in achieved radiological parameters after removal of fixator adversely affecting the functional outcome which is a matter of concern.
Keywords: Hemicallotasis (HC), Medial opening wedge high tibial osteotomy (MOWHTO), Femoro tibial angle (FTA), Mechanical axis, KOOS, Medial compartment OA Knee, Varus knee
1. Introduction
Osteoarthritis (OA) is the most common form of chronic arthritis world over and is a known cause of pain and disability. In a community based cross-sectional study of individuals aged 40 and more in a population similar to ours, Pal et al. found the overall prevalence of knee OA to be 28.7%.1 They found a prevalence of 19.2% in individuals less than 50 years of age and this burden continues to increase significantly. Increasing number of patients with disabling knee pain are presenting for treatment in the 4th, 5th and 6th decades itself.
When OA occurs in an active patient, it is generally progressive. Limb alignment has been noted to be a major contributor to persistent mechanical loading of a deranged compartment and is responsible for relentless progression of the disease.2 Varus deformity is the most common and earliest deformity encountered in OA of the knee, responsible for accelerating the degenerative changes of the knee. Joint preserving surgical options available for treatment of this condition include arthroscopic debridement and lavage, bone stimulation procedures such as drilling, micro-fracturing, or abrasion chondroplasty, cartilage restoration via autologous chondrocyte transplantation or autologous osteochondral transplantation and corrective valgus high tibial osteotomy (HTO).3 Joint replacement procedures like the unicompartmental arthroplasty, and total knee arthroplasty are the other available established procedures but there are concerns about the longevity of implants due to accelerated wear and early loosening, especially in younger patients.5
HTO restores the mechanical axis and brings symptomatic relief in patients with medial compartment OA with varus knees. The goal is to unload the degenerated medial compartment by shifting the weight-bearing forces to the healthier lateral compartment which is known to improve the biological quality of damaged articular cartilage and maintain the articular cartilage in the less degenerated compartment.6,7
The survival of HTO has been reported to be approximately 80–90% at 5 years and 70–80% at 10 years.4 These patients may eventually require arthroplasty. This delay in joint replacement is desirable in active individuals who might be interested in an unimpeded lifestyle. HTO can be performed by various methods like lateral closing wedge HTO, dome or barrel vault HTO and medial opening wedge HTO (MOWHTO). The lateral closing wedge osteotomy is associated with high rate of complications such as patella baja, tibial slope inversion and lateralization of proximal tibial epiphysis8 peroneal nerve palsy, over or under correction, compartment syndrome, infection and intra-articular fracture9,10 Dome osteotomy also had many reported complications reported like peroneal nerve injury during fibular osteotomy or during the placement of the steinmann pins, anterior compartment syndrome and decrease in posterior tibial slope etc.11 Due to these problems, the MOWHTO started gaining popularity over the other methods12 but it requires maintenance of correction till healing occurs as the bone surfaces are not in contact. This can be achieved using long leg cast/staples/various plate-and-screw fixation with or without autogenous or allogeneic bone graft or graft substitutes and a gradual distraction by hemicallotasis (HC) technique using monolateral dynamic external fixator or ilizarov fixator.13, 14, 15
The advantages of MOWHTO over the lateral closing wedge or dome osteotomy are the protection of bone stock, minimal soft tissue stripping during surgery, maintenance of limb length, negligible chances of neurovascular complications and rectification of the deformity and accurate restoration of mechanical and anatomical axis without introducing iatrogenic translation as the correction is at or very close to the centre of rotation of angulation (CORA) in the proximal tibial metaphysis. The disadvantages include the need for bone graft, and the risk of delayed union or nonunion.13 There are also concerns of changing the posterior tibial slope and patellar height, and thus the patellofemoral compartment pressure, that often occur when too much correction is done.16,17
Few studies have mentioned the concerns about the loss of correction over a period of time after removal of fixator18 and eventual deterioration of knee function19 however the chronology and magnitude of the same has not been recorded to our knowledge. To investigate this possibility, a prospective study was undertaken aimed to record the change in radiological and functional outcomes with time over the first two years after achieving desired correction while treating varus degenerative OA of knee by HC Technique using self-adjusting HTO fixator.
2. Methods
This was a prospective study carried out on patients who underwent HTO by hemicallotasis technique at our institute between May 01, 2016 to Dec 31, 2017.
2.1. Pre-operative management
All patients who failed to show clinical improvement after a trial of conservative management (oral analgesics, physical therapy, life style modifications, offloading knee braces etc.) for at least 6 months were enrolled in the study.
We had a total of 43 patients satisfying our inclusion criteria visiting our OPD during the study period after completion of at least 6 months of conservative management. 10 were excluded initially (4 had chronic ligamentous insufficiency, 3 had previous tibial shaft/plateau fractures, 2 had tricompartmental involvement radiologically and one had BMI>35) and 2 more patients were excluded after a finding of extensive lateral and patellofemoral compartment involvement during mandatory diagnostic arthroscopy performed prior to start of HTO. Finally 31 patients who underwent HTO by hemicallotasis were included in our study.
Our inclusion-exclusion criteria is presented in Table 1.
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria |
|
| Exclusion Criteria |
|
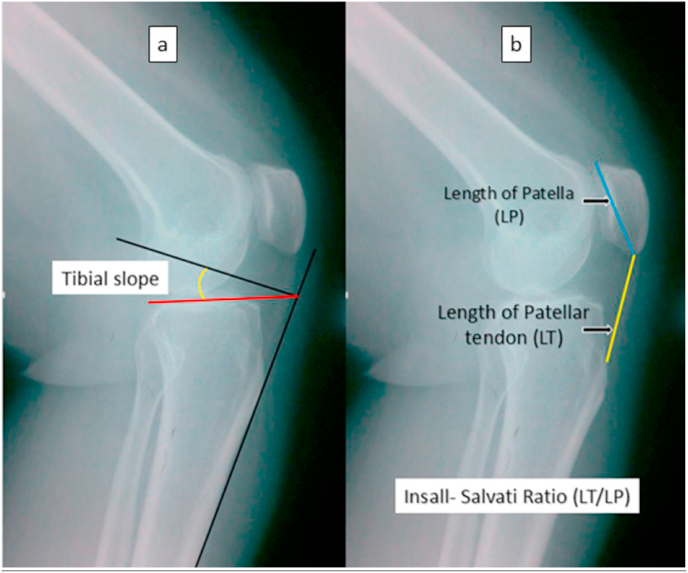
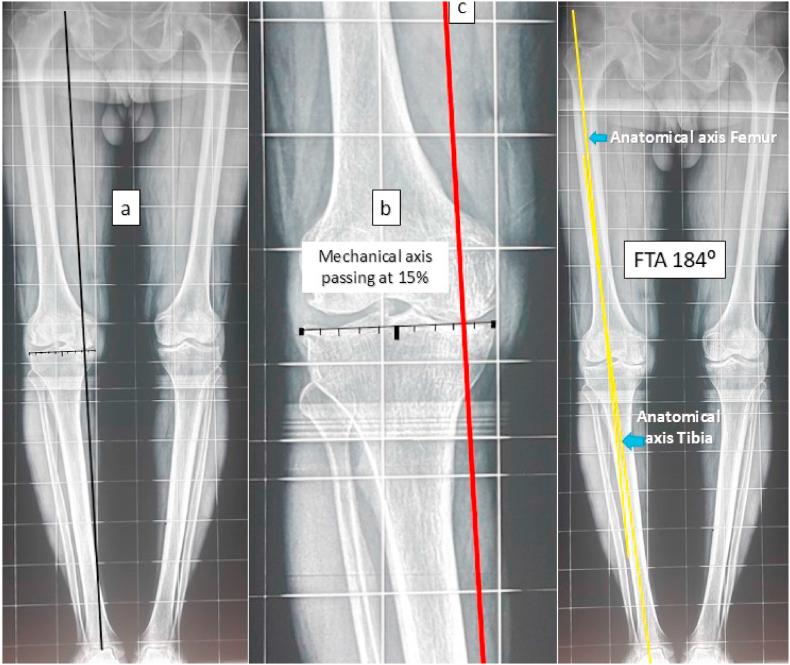
Informed written consent was taken from all patients willing to undergo the procedure. All the patients were evaluated preoperatively by KOOS score. The radiographic assessment was done using a weight bearing antero-posterior and lateral radiograph which was used to calculate the posterior tibial slope (by Moore and Harvey technique)20 and the patellar height (assessed using the Insall-Salvati ratio (Fig. 1).21 A weight bearing scannogram was used to assess the femoro tibial angle (FTA). An angle of 180⁰ was considered neutral coronal plane alignment of knee, values > 180⁰ were considered varus alignment and <180⁰ considered valgus alignment. The target range of FTA after correction was set at 173–177⁰ (3–7⁰ valgus), correction < 173⁰ was defined as over correction and >177⁰ as under correction. The mechanical axis as described by Moreland, Bassett and Hanker (Fig. 2)22 was also drawn on the scannogram. The point where this line crossed the tibial plateau was recorded and depicted as a percentage of the total breadth of the tibial articular surface, with the medial edge as 0% and the lateral edge as 100%. The target after correction was the mechanical axis passing at 62–63% (base of lateral tibial spine) as described by Fugisawa et al.23 All the radiographic calculations were done by two senior radiologists of our institution twice at two weeks interval and the mean was accepted as the final value. All the functional assessments were done by the two experienced physiotherapist blinded to the study and the mean value was accepted as final.
Fig. 1.
Pre-operative radiological measurements.a-Tibial slope calculation; b-Insall-Salvati ratio calculation.
Fig. 2.
Pre-operative radiological measurements.a-Mechanical Axis (A line from centre of femoral head to centre of ankle); b-Mechanical axis percentage calculation in relation to proximal tibial articular surface scale of 100; c-Calculation of femoro tibial angle (FTA) from anatomical axes of femur and tibia.
2.2. Operative procedure
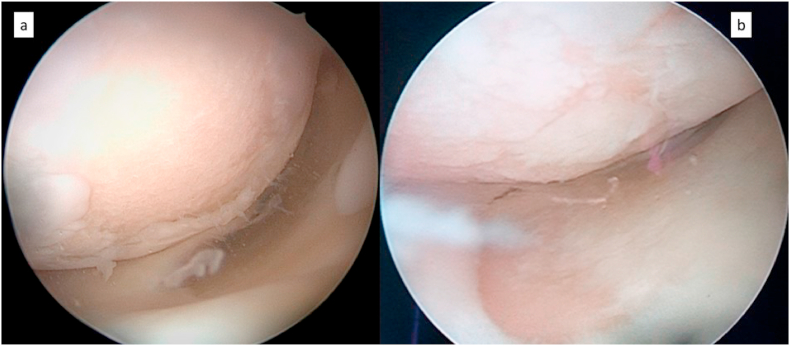
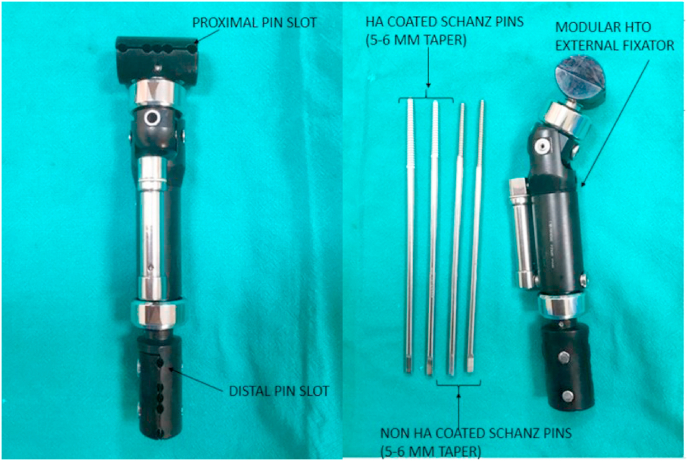
All surgeries were performed under spinal anaesthesia by the two senior surgeons. Tourniquet was used in all cases. A diagnostic arthroscopy was performed in all patients to ascertain and document the extent of the joint involvement (Fig. 3). Intra-articular procedures such as meniscal balancing, removal of osteophytes in the roof of the notch, removal of loose bodies and debridement of unstable cartilage were done as needed. A self-adjusting HTO fixator (SH Pitkar Orthotools Pvt Ltd.) (Fig. 4) was applied to the tibia with two 5–6 mm tapered HA coated Schanz screws in proximal fragment (2–3 cm distal and parallel to the medial joint line) and two 5–6 mm tapered schanz pins in the shaft distal to osteotomy. Under c-arm guidance, a minimally invasive medially based (approximately 8–10 cm distal to medial joint line), uniplanar, oblique (directed towards the proximal tibiofibular joint), proximal tibial osteotomy was performed with a thin 1 cm wide osteotome thorough a small 2 cm longitudinal incision over the posteromedial border of proximal tibial metaphysis. The osteotomy was fashioned in such a way that the tibial tuberosity was with the proximal fragment (to avoid patella baja) and the care was taken not to breach the lateral cortex of the tibial metaphysis (Fig. 5). During the surgery, markers (ECG electrodes) were placed over the centre of femoral head and one over centre of ankle joint under c-arm guidance. After completion of osteotomy and fixator application, acute distraction was carried out intraoperatively. A cautery lead (radiolucent) was held taught in a straight line joining the centre of femoral head to the centre of ankle joint. The point where this wire intersected the tibia was noted on the c-arm image of knee and distraction fine-tuned till it intersected at the desired point. The amount of distraction required to achieve this was recorded as a guide to the end point of the distraction process.
Fig. 3.
Arthroscopy evaluation findings prior to HTO.a-Extensive loss of femoral articular cartilage in medial compartment; b-patchy chondral changes in femoral and tibial articular cartilage with intact medial meniscus.
Fig. 4.
Modular dynamic HTO fixator and Schanz screws used.
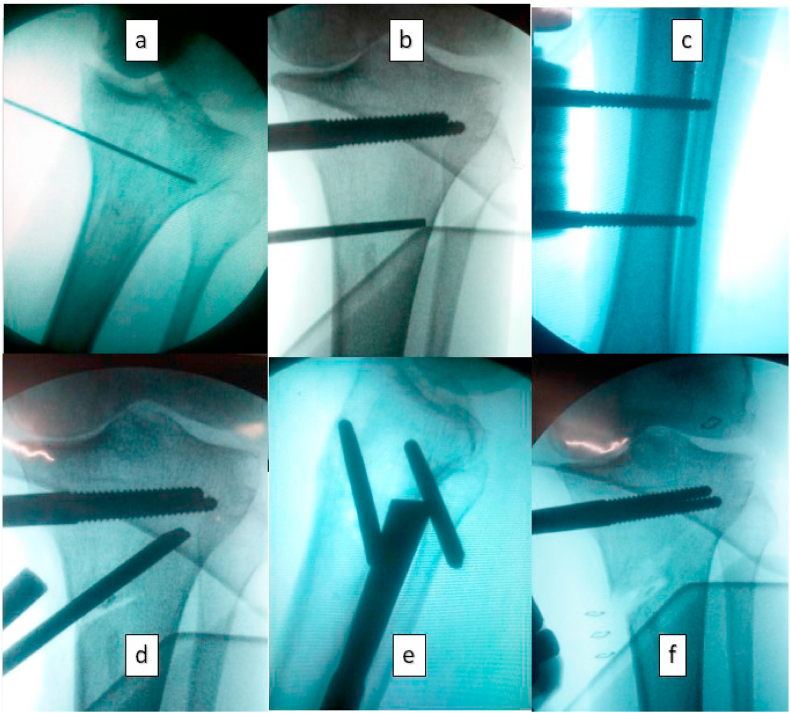
Fig. 5.
Operative Steps of HTO with self-adjusting HTO fixator application.a-Insertion of guide wires parallel to the joint line; b & c-Insertion of proximal and distal tapered schanz pins; d&e- completion of osteotomy stopping short of lateral cortex; f- Intraoperative distraction of osteotomy to the desired level.
2.3. Post-operative period
Post-operative antibiotics were given for 24 h. Post-op analgesia was tailored as per patient’s needs. Early active and passive range of movement exercises of the knee were started on the evening of surgery. Pin tract care was done daily and explained to the patient. Patient started on assisted ambulation with partial weight bearing allowed as per tolerance with help of crutches on the first post-operative day and discharged home. After a latent period of 07 days, distraction of the fixator was started at the rate of 01 mm per day in four equal increments. The patient was instructed about the number of days the distraction was to be continued till the target was achieved based on the amount of distraction noted during the surgery. Radiological assessment for quality of regenerate was done 2 weekly starting one month after completion of distraction till the removal of fixator. The fixator was maintained till consolidation of the callus seen radiographically (usually between 2 and 3 times the duration of the distraction period). The consolidation was assessed based on the opacity of the regenerate compared to the opacity of the surrounding normal bone. All this while the patient was kept partial weight bearing but allowed full ROM of knee. After satisfactory regenerate was seen radiologically, dynamisation of the fixator was done by removing the compression-distraction unit from the distractor for last two weeks prior to removal of fixator and patient was asked to bear maximum weight possible on operated leg. The ability of patient to bear full weight with no pain/tenderness in the osteotomy site was taken as satisfactory clinical consolidation of the regenerate. At the end, the fixator was removed in OPD. The functional scores were recorded on (a) removal of fixator, (b) at 1 year and (c) at 2 years. The radiological measurements on the scannograms were recorded during follow-up period (a) after the distraction was completed (b)at 1 year and (c) at 2 years.
3. Statistical analysis
The collected data was entered in Microsoft excel sheet. SPSS 22.0 (SPSS Inc., Chicago, IL) software was used for carrying out the statistical analysis. Descriptive data has been presented as mean, range and SD. The categorical data has been presented as actual value and percentage. The paired sample t-test was used to determine the significance of change of mean FTA, Mechanical Axis (%), Insall-Salvati Ratio, Tibial Slope, KOOS at pre-operative period, during removal of fixator (after achieving correction), 1 yearand 2 years follow-up. The correlation between the correction achieved and the functional score was done by the Pearson’s correlation coefficient. p-value of 0.05 was considered to be statistically significant for all the statistical tests.
4. Results
The demographic and pre-operative data of our study subjects is as per Table 2.
Table 2.
Demographic and preoperative variables.
| Total Number (n) | 31 |
|---|---|
| Age | Mean: 49.3 years Range: 39–67 years Standard Deviation: 6.74 |
| Sex | Female: 17 (54.84%) Male: 14 (45.16%) |
| Side | Right: 11 (35.48%) Left: 20 (64.52%) |
| BMI | Mean: 27 Range: 21-32 Standard Deviation: 3.07 |
| KL grade | Grade 1: 11 (35.48%) Grade 2: 20 (64.52%) |
| Pre op FTA | Mean: 183.12⁰ Range: 179-198 Standard Deviation: 3.49 |
| Pre Op Mechanical axis | Mean: −3.26 Range: −20 to 10 SD:7.86 |
| Pre op KOOS Score | Mean: 56.61 Range: 51 to 60 SD: 2.55 |
The arthroscopy findings and the arthroscopic procedures done in our study are tabulated in Table 3.
Table 3.
Arthroscopic findings and appropriate procedure done.
| Arthroscopy findings | Number (n) | Procedure |
|---|---|---|
| 1. Degenerative tears of medial meniscus | 17 | Balancing of the medial meniscus. |
| 2. Mild degenerative fraying of lateral meniscus | 04 | Balancing of lateral meniscus. |
| 3. Loose bodies | 04 | Removal of loose bodies. |
| 4. Chondral damage medial compartment- varying grades as per International Cartilage Research Society (ICRS) | 28 | Mostly left alone. Debridement of unstable cartilage flap. Microfracturing in cases of complete loss of cartilage upto a size of 3 square Cm. |
| 5. Osteophytes in the notch, spiking of tibial spine | 12 | Removal of osteophytes from roof of intercondylar notch and flattening of the pointed tibial spine. |
| 6. Extensive Lateral/patellofemoral compartment involvement (Chondral damage/loss of cartilage) or extensive lateral meniscal tear/degeneration. | 02 | HTO abandoned. |
The commonest arthroscopy finding (in 28 patients) was chondral changes in the medial tibial and femoral condyles of varying grades as per International Cartilage Research Society (ICRS). Mostly they were left alone. Only when unstable cartilage flap was seen, it was debrided.Microfracturing was done in cases of complete loss of cartilage. Minor degenerative tears of medial meniscus were seen in 17 cases and of lateral meniscus in 04 cases. Balancing of the menisci was done in these cases. In 12 cases, osteophytes in the intercondylar notch or excessive spiking of the tibial spine impinging in the intercondylar notch were seen wherein removal of osteophytes from roof of intercondylar notch and flattening of the pointed tibial spine with arthroscopic burr was done. In 04 cases loose bodies were found which were removed.
The total duration (in days) of distraction for achieving the desired alignment varied depending on the amount of correction required. The mean duration of distraction was 28 days (Range 18–45 days, SD 9.12). The mean time from surgery to removal of the fixator was 97 days (Range 75–128 days, SD 15.61).
Pin tract infection was the commonest post-operative complication recorded in 18 of total 60 Schanz screws used (30%). 11 of these healed by pin tract care alone, 05 required additional oral antibiotics for a week and 02 had loosening of the pins. There were 2 cases of delayed consolidation of the regenerate in which the fixator was retained for a prolonged period of more than 3 times the duration of distraction. The complications of the procedure were recorded as per Table 4.
Table 4.
Complications.
| Sr. No. | Complication | Count |
|---|---|---|
| 1 | Pin Tract Infection (superficial) | 18 of 60 Schanz Screws (30%) 11 healed by pintract care alone. 05 required additional oral antibiotics (05 Days) 02 had loosening |
| 2 | Non-Union | Nil |
| 3 | Delayed Union | 02 (6.45%) |
| 4 | Compartment Syndrome | Nil |
| 5 | Deep Vein Thrombosis | Nil |
| 6 | Osteomyelitis | Nil |
| 7 | Loss of Correction (<5°) | 09 (29.03%) |
| 8 | Loss of correction (>5⁰) | 05 (16.12%) |
| 9 | Loss of ROM | Nil |
| 10 | Septic Arthritis | Nil |
| 11 | Lateral cortex fracture | Nil |
| 12 | Tibial Plateau fracture | Nil |
| 13 | Failure | Nil |
| 14 | Ring sequestrum | Nil |
| 15 | Neurovascular compromise | Nil |
The mean values of FTA, mechanical axis, Insall-Salvati Ratio, tibial slope, KOOS score at various time points are presented in Table 5.
Table 5.
The mean values of FTA, mechanical axis, Insall-Salvati Ratio, tibial slope, KOOS score at various time points.
| Variables | Pre-operative value/score (a) | Value/score at the time of removal of fixator (b) | Mean Difference of value/score at removal of fixator compared to at Pre Op score (c) = (b-a) | p value for (c) | Value/score at 1 year Post-removal of fixator (d) | Mean Difference of value/score at 1 year compared to score after removal of fixator (e)=(d-b) | p value for (e) | Value/score at 2 years Post-removal of fixator (f) | Difference of Value/score at 2 years compared to at 12 months (g)=(f-d) | p value for (g) | Overall difference between the start and end of the study (h) =(f-a) | p value for (h) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FTA (Average) | 183.12⁰ | 173.38⁰ | −9.74⁰ | 0.00001 | 176.06⁰ | 2.68⁰ | 0.00001 | 176.16⁰ | 0.10⁰ | .0839 | −6.96⁰ | 0.00001 |
| Mechanical Axis (%) (Average) | −3.26 | 61.81 | 65.06 | 0.00001 | 57.96 | −3.85 | 0.0001 | 57.74 | −0.22 | .0505 | 61.0 | 0.00001 |
| Insall-Salvati Ratio (Average) | 1.04 | 1.03 | 0.01 | 0.3183 | 1.03 | 0 | 1 | 1.03 | 0 | 1 | −0.01 | 0.3183 |
| Tibial Slope (Average) | 11.33 | 11.33 | 0 | 1 | 11.33 | 0 | 1 | 11.33 | 0 | 1 | 0 | 1 |
| KOOS Score (Average) | 56.61 | 70.48 | 13.87 | 0.00001 | 85.68 | 15.20 | 0.00001 | 84.54 | −1.14 | .0014 | 27.93 | 0.00001 |
The mean preoperative FTA improved from a mean 3.12⁰ of Varus (mean 183.12⁰; range 179–198⁰) preoperatively to 6.62⁰ valgus (173.38⁰; range 170 to 178⁰) at the time of removal of fixator (a change of mean 9.74⁰). Over the first 1 year we observed a mean deterioration of 2.68⁰ of the initially achieved correction (change of mean FTA to 176.06⁰) which was a significant loss of correction. There was further insignificant loss of correction of a mean 0.10⁰ over next 1 year and the final mean FTA at 2 years was valgus of 3.84⁰ (range 173⁰ to 180⁰ of FTA). The mean overall change in FTA at 2 years compared to the pre-operative value was 6.96⁰. We observed that we could achieve the target correction at the time of fixator removal in 26 out of 31 cases (83.9%), 4 (12.9%) had over correction and 01 (3.2%) had under correction. 14 patients (45.16%) had loss of correction over first 1 year with 09 having a loss of <5⁰ and 05 having a loss of >5⁰. This resulted in only 16 (51.6%) retaining the target correction and 15 (48.38%) having an under correction. There was no further significant change in FTA in next 1 year till the end of the study.
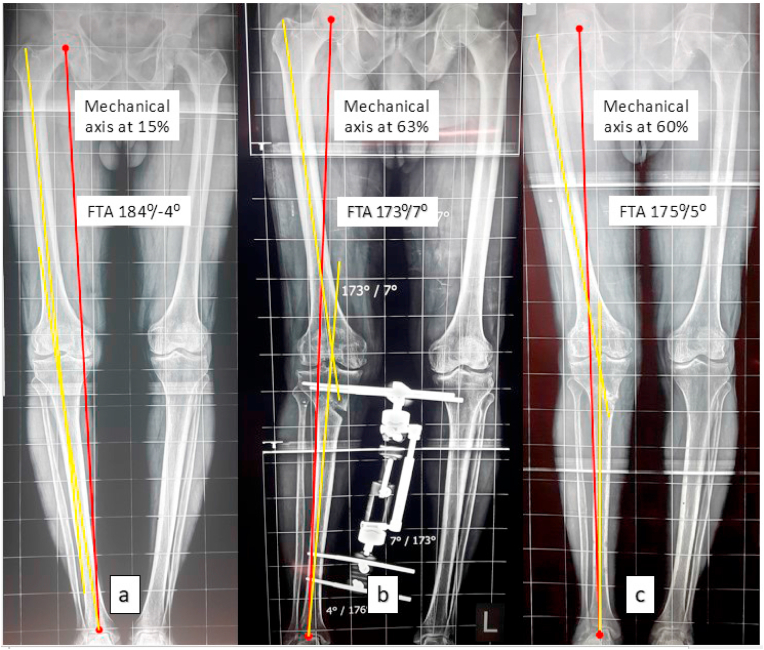
The mean preoperative mechanical axis was at −3.26% (range 10% to −20%) This improved to 61.81% following completion of correction which was statistically significant. There was significant progressive deterioration (commensurate with change of FTA) of the axis to 57.96% at 1 year. There was a further insignificant deterioration over the next 1 year till the completion of study and the final mechanical axis was at 57.74% (range 48–63%). Fig. 6 shows serial scannograms showing changes in limb alignment measured in one of our cases during and after completion of treatment.
Fig. 6.
Changes in limb alignment. a- Pre-operative Femoro tibial angle (FTA) 184⁰ and mechanical axis passing at 15% tibial width; b- An FTA of 173⁰ and mechanical axis passing through 63% of tibial articular surface width after correction of deformity.; c- Change of FTA to 175⁰ and mechanical axis to 60% at the end of one year.
There was no significant change noticed in the patellar height or the tibial slope at various time points during the study.
The mean pre-op KOOS was 56.61 which improved to 70.48 at the time of removal of fixator and this was statistically significant. At 12 months following removal of fixator, mean KOOS was 85.68 which was a significant improvement. Subsequently there was a significant reduction of this score over next one year to 84.54 at 2 years. Despite this reduction, there was a significant overall improvement in KOOS at the end of the study compared to the pre-operative score by 29.16 points.
5. Discussion
High tibial osteotomy (HTO) is an acknowledged procedure to treat medial compartment osteoarthritis. It is generally performed for patients younger than 60 years12,23,24 however Coventry suggested that the age of the patient is irrelevant for surgery and there are studies wherein HTO was done in patients up to 72 years19 with good outcome. The mean age of the study population in our study was 49.3 years with minimum age of 39 and maximum age of 67 years. We feel that osteotomy should not be denied to patients based upon only the chronological age if he/she is in good health and if other inclusion and exclusion criteria as noted earlier are met.
It is generally agreed in the contemporary literature that a low degree of arthrosis is linked to better outcomes of HTO and that tricompartmental OA is a contraindication to osteotomy.25,26 HTO by hemicallotasis technique may be used in patients with KL grade 3 and 4 OA also but due to increased chances of involvement of the lateral and patellofemoral compartment in the degenerative process with increase in KL grade, the results of HTO may not be satisfactory. Hence we limited ourselves to cases up to KL grade 2 only.
A few Studies have shown that a HTO in patients with BMI less than 30 generally have better outcome.27,28 There is no prescribed upper limit for this technique however it is our belief that patients with BMI >35 should not be offered HTO by any technique. In fact, a recent editorial commentary by Arne Ekeland, Tor Kjetil Nerhus seems to strengthen our belief in this regard.26 None of the patients in our study had a BMI >35.
All the patients underwent diagnostic arthroscopy to ascertain the intactness of the lateral compartment (as the new mechanical axis is supposed to pass through the lateral compartment). The role of arthroscopy prior to HTO is debatable. There are studies giving due importance to arthroscopy to accurately document the joint pathology, address unstable cartilage and meniscal lesions and loose bodies29,30 prior to HTO. We also believe that arthroscopy was beneficial as it improved the immediate functional outcome as a result of joint lavage, minimal debridement and removal of loose bodies.
While using dynamic fixator for HTO it is important not to violate the lateral cortical hinge while performing osteotomy. There were no cases of lateral cortical breach in our series as we were careful about stopping at least 05 mm short of lateral cortex. The bail out option for a lateral cortex fracture if it happens per-op can be (a) If the fracture of lateral cortex is complete with displacement of proximal and distal fragments, it requires conversion of dynamic fixator to a fixed angle locked HTO plate like Tomofix/Puddu plate with or without bone grafting. (b) If there is no displacement, plating the lateral cortex with 3.5 mm 1/3 tubular plate in addition to the HTO fixator application may be adequate however starting of distraction needs to be delayed to around 2 weeks.
Variable rates of pin tract infections with hemicallotasis, ranging from 8% to 60% have been reported.12,30,31 Superficial infection can be managed with proper pin site care with or without antibiotics. A deep infection without loosening of pins is a tricky situation and will require injectable antibiotics along with thorough pin site irrigation. With use of HA coated pins the chances of loosening are minimised. The bail out option if loosening still happens are (a) The tapered schanz screws may be tightened further and that improves the hold and may be sufficient as in our case. (b) Removal of loose pins and insertion of fresh pins in the alternate slots available in the fixator. The fixator offers 5 slots for pin insertion as shown in Fig. 3 and only two slots are used initially (Generally 1st and 4th). 18 (30%) pins in 14 patients (45.16%) were infected at some point of time during our study and were the major cause of discomfort for the patients. Most (15/18) of these were the proximal pins. 11 required only pin tract care by the patients themselves, only 05 required additional oral antibiotics. In 02 patients there was pin tract infection associated with loosening of one of the proximal two pins. This was controlled IV antibiotics and tightening the pin a few more turns as we had used the tapered pins. None of the patients required premature pin replacement. We did not have any case of deep infection or osteomyelitis. 14 patients were not too comfortable with the fixator especially considering the care it required however, they were happy with the improved functionality and an implant-less end result after removal of fixator.
Distraction was carried out at the rate of 01 mm per day divided into 04 intervals. The callus formed at the end of maintenance phase was of good density. The frequency of distraction is shown to affect the density of the regenerate formed.The greater the frequency better the density of the regenerate.32 The amount of distraction at the unilateral fixator does not translate into actual distraction at the osteotomy site as it depends on the distance of the distractor as well as the hinge (lateral tibial cortex) from the osteotomy which is variable and therefore cannot be calculated preoperatively accurately and hence was done intraoperatively under image guidance and noted. We found this to correlate well with the accuracy of final correction achieved in our study as seen by the fact that about 84% achieved desired correction with only about 13% over correction and about 3% under corrections during the time of fixator removal. The patients could be accurately instructed the number of days they were required to continue the distraction. This is a very important technical point and can be easily followed by anyone desirous of using similar fixator for HTO.
Restoration of 3–5° of physiological valgus is considered optimal correction.23,33 Varus under-correction may lead to recurrence of deformity12,34 and valgus over-correction also results in rapid deterioration of lateral compartment.12,35 The results of HTO are known to worsen with time, but more so in knees that remain under or over-corrected.6,36 In the present study the desired correction could be achieved with the fixator in 83.9%, with 12.9% over-corrections (FTA< 173⁰) and 3.2% under-correction (FTA>177⁰) but by the end of the study this changed to only 16 (51.61%) retaining the desired correction and 15 (48.38%) under-corrections. There was no further significant change in the axis in the subsequent year till the end of the study. Other studies on HTO by hemicallotasis using unilateral fixator have mentioned maintenance of the achieved correction19,37 but our results are at a variance from these studies especially in the first year after removal of fixator. The possible reason for decline in radiological parameters is a gradual compression of the regenerate with continued weight bearing leading to reappearance of relative varus once the protection to collapse afforded by the fixator is removed. We believe that though radiologically adequate consolidation is seen and patient is able to bear full weight before the removal of fixator, the consolidation continues well beyond this point and is complete only after a few more months at least but patient may not tolerate the fixator for that long. We believe that this gradual collapse is unlikely to happen with locked plates like Tomofix/Puddu plate since they continue to provide protection to the regenerate.
On closer evaluation of components of pre op KOOS for assessing the activity level within our cohort of population, the mean activities of daily living component score was 62.67% (Range 57–66%, SD 2.81) and the sports and recreational activities component score was 42.43% (Range 38 to 49, SD - 2.35). A narrow standard deviation in both these components shows that these scores in all the subjects within the cohort was closer to the mean indicating that the activity levels were not grossly different and comparable. Though there was significant improvement in the KOOS at the end of study compared to the pre-operative level but on analysis of its progressive change, we found that the it improved significantly by the time correction was achieved and fixator removed compared to pre op, continued to significantly improve at the 1 year follow-up but in the following 1 year, there was a significant reduction. Since the functional scores generally depend on the accuracy of the radiological correction, probably a change in these scores was seen with change in radiological parameters as noted earlier. Additionally with progressing age, the functional scores are likely to reduce naturally. The relationship between the correction achieved and the functional outcome is confirmed by the negative correlation between FTA and KOOS (Pearson’s correlation coefficient r = −.8113 which was highly significant p < 0.00001) and the positive correlation between the final mechanical axis and KOOS score (Pearson’s correlation coefficient r = 0.607 which also was highly significant p = 0.000289).
Our study correlates well with the studies16,19,37 wherein no significant changes were found in either the tibial slope or the Insall-Salvati ratio following HTO by HC. We feel that the ability to maintain sagittal alignment which is difficult to control by stapling or various forms of plating38,39 is an advantage of hemicallotasis.
The strengths of the study are that this was a prospective study with a very exhaustive and tight inclusion-exclusion criteria. The limitations of this study are that we have a relatively small sample size and the follow up period was short.
6. Conclusion
In a relatively young individual wishing to pursue an active lifestyle, MOWHTO using self-adjusting unilateral HTO fixator with its benefits of early weight bearing, precise correction, no significant alteration of patellofemoral joint dynamics, no loss of limb length, and minimal chances of delayed union or non-union, is a good option. Though it is possible to achieve the target correction by this method without a retained implant, a large number of patients are not comfortable with the fixator and the significant loss of correction after removal of fixator within the first 1 year is a worrying observation as maintenance of correction is the most important factor to ensure good outcome in the long term.
Ethics
Approval of the institutional ethics committee was obtained for the study.
Consent
Informed consent was obtained from all patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
References
- 1.Pal C.P., Singh P., Chaturvedi S., Pruthi K.K., Vij A. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop. 2016 Sep;50(5):518–522. doi: 10.4103/0019-5413.189608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cerejo R., Dunlop D.D., Cahue S., Channin D., Song J., Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–2636. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 3.Michael J.W., Schlüter-Brust K.U., Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee [published correction appears in Dtsch Arztebl Int. 2010 Apr; 107(16):294] Dtsch Arztebl Int. 2010;107(9):152–162. doi: 10.3238/arztebl.2010.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang W., Bennett C.H. High tibial osteotomy and related surgeries. Curr Opin Orthop: April. 2005;16 – Issue 2:77–81. [Google Scholar]
- 5.Sutton Paul M., Holloway Edward S. The young osteoarthritic knee: dilemmas in management. BMC Med. 2013;14 doi: 10.1186/1741-7015-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coventry M.B., Ilstrup D.M., Wallrichs S.L. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am. 1993 Feb;75(2):196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Spahn G., M Klinger H., Harth P., O Hofmann G. Cartilage regeneration after high tibial osteotomy. Results of an arthroscopic study. Z für Orthop Unfallchirurgie. 2012;150:272–279. doi: 10.1055/s-0031-1298388. [DOI] [PubMed] [Google Scholar]
- 8.Aglietti P., Buzzi R., Vena L.M., Baldini A., Mondaini A. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg. 2003;16:21–26. [PubMed] [Google Scholar]
- 9.Coventry M.B. Upper tibial osteotomy for gonarthrosis: the evolution of the operation in the last 18 years and long term results. Orthop Clin N Am. 1979;10:191–210. [PubMed] [Google Scholar]
- 10.Murphy S.B. Tibial osteotomy for genu varum: indications, preoperative planning, and technique. Orthop Clin N Am. 1994;25:477–482. [PubMed] [Google Scholar]
- 11.Cullu E., Aydogdu S., Alparslan B. Tibial slope changes following dome-type high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2005;13:38Y43. doi: 10.1007/s00167-004-0501-0. [DOI] [PubMed] [Google Scholar]
- 12.Hernigou Ph, Medevielle D., Debeyre J. Proximal tibial osteotomy for osteoarthritis with varus deformity: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332Y354. [PubMed] [Google Scholar]
- 13.Brinkman J.-M., Lobenhoffer P., Agneskirchner J.D., Staubli A.E., Wymenga A.B., van Heerwaarden R.J. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008 Dec;90(12):1548–1557. doi: 10.1302/0301-620X.90B12.21198. [DOI] [PubMed] [Google Scholar]
- 14.Adili A., Bhandari M., Giffin R., Whately C., Kwok D.C. Valgus high tibial osteotomy: comparison between an Ilizarov and a Coventry wedge technique for the treatment of medial compartment osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2002;10:169–176. doi: 10.1007/s00167-001-0250-2. [DOI] [PubMed] [Google Scholar]
- 15.Sen C., Kocaoglu M., Eralp L. The advantages of circular external fixation used in high tibial osteotomy (average 6 years follow-up) Knee Surg Sports Traumatol Arthrosc. 2003;11:139–144. doi: 10.1007/s00167-003-0344-0. [DOI] [PubMed] [Google Scholar]
- 16.Brouwer R.W. Patellar height and the inclination of the tibial plateau after high tibial osteotomy: the open versus the closed-wedge technique. J Bone Jt Surg - Br. 2005;87–B(9):1227–1232. doi: 10.1302/0301-620X.87B9.15972. [DOI] [PubMed] [Google Scholar]
- 17.Ducat A., Sariali E., Lebel B. Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res. 2012;98(1):68–74. doi: 10.1016/j.otsr.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 18.Lee D.C., Byun S.J. High tibial osteotomy. Knee Surgery & Related Research. 2012;24(2):61–69. doi: 10.5792/ksrr.2012.24.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bachhal V., Sankhala S.S., Jindal N., Dhillon M.S. High tibial osteotomy with a dynamic axial fixator: precision IN achieving alignment. Bone Joint J [Internet] 2011;93–B(7):897–903. doi: 10.1302/0301-620X.93B7.26124. [DOI] [PubMed] [Google Scholar]
- 20.Moore T.M., Harvey J.P., Jr. Roentgenographic measurement of tibial-plateau depression due to fracture. J Bone Jt Surg Am. 1974;56-A:155–160. [PubMed] [Google Scholar]
- 21.Insall J., Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 22.Moreland J.R., Bassett L.R., Hanker G.J. Radiographic analysis of the axial alignment of the lower extremity. J Bone Jt Surg Am. 1987;69-A:745–749. [PubMed] [Google Scholar]
- 23.Fujisawa Y., Masuhara K., Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am. 1979;10(3):585–608. [PubMed] [Google Scholar]
- 24.Gerdhem P., Abdon P., Odenbring S. Hemicallotasis for medial gonarthrosis: a short-term follow-up of 21 patients. Arch Orthop Trauma Surg. 2002;122:134–138. doi: 10.1007/s004020100323. [DOI] [PubMed] [Google Scholar]
- 25.Bonasia D.E., Dettoni F., Sito G. Rossi R Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med. 2014 Mar;42(3):690–698. doi: 10.1177/0363546513516577. [DOI] [PubMed] [Google Scholar]
- 26.Ekeland Arne, Nerhus Tor Kjetil. Editorial Commentary: High tibial osteotomy for varus knees with medial osteoarthritis may prevent total knee arthroplasty. Arthrosc J Arthrosc Relat Surg. 2020;36(No 2):544–545. doi: 10.1016/j.arthro.2019.10.039. [DOI] [PubMed] [Google Scholar]
- 27.Flecher X., Parratte S., Aubaniac J.M. Argenson JN A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res. 2006 Nov;452:91–96. doi: 10.1097/01.blo.0000229362.12244.f6. [DOI] [PubMed] [Google Scholar]
- 28.Howells N.R., Salmon L., Waller A., Scanelli J. Pinczewski LA the outcome at ten years of lateral closing-wedge high tibial osteotomy: determinants of survival and functional outcome. Bone Joint Lett J. 2014 Nov;96-B(11):1491–1497. doi: 10.1302/0301-620X.96B11.33617. [DOI] [PubMed] [Google Scholar]
- 29.Noyes Frank R., Mayfield William, Barber-Westin Opening wedge high tibial osteotomy: an operative technique and rehabilitation program to decrease complications and promote early union and function. Am J Sports Med. 2006;34(Issue 8):1262–1273. doi: 10.1177/0363546505286144. [DOI] [PubMed] [Google Scholar]
- 30.Niemeyer P., Schmal H., Hauschild O. Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. YJARS [Internet] 2010;26(12):1607–1616. doi: 10.1016/j.arthro.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 31.Ohsawa S., Hukuda K., Inamori Y., Yasui N. High tibial osteotomy for osteoarthritis of the knee with varus deformity utilizing the hemicallotasis method. Arch Orthop Trauma Surg. 2006;126:588–593. doi: 10.1007/s00402-006-0130-9. [DOI] [PubMed] [Google Scholar]
- 32.Mizuta H., Nakamura E., Kudo S., Maeda T., Takagi K. Greater frequency of distraction accelerates bone formation in open-wedge proximal tibial osteotomy with hemicallotasis. Acta Orthop Scand. 2004;75(5):588–593. doi: 10.1080/00016470410001475. [DOI] [PubMed] [Google Scholar]
- 33.Lee M.D., Seong Joon Byun M.D. High Tibial Osteotomy Knee Surg Relat Res. 2012 Jun;24(2):61–69. doi: 10.5792/ksrr.2012.24.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee D.C., Byun S.J. High tibial osteotomy. Knee Surg Relat Res. 2012;24(2):61–69. doi: 10.5792/ksrr.2012.24.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwon S.K., Moon H.K., Choi C.J. Accelerated degeneration of the discoid lateral meniscus after medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015;23:97–103. doi: 10.1007/s00167-012-2289-7. [DOI] [PubMed] [Google Scholar]
- 36.Insall J., Shoji H., Mayer V. High tibial osteotomy: a five-year evaluation. J Bone Jt Surg Am. 1974;56-A:1397–1405. [PubMed] [Google Scholar]
- 37.Nakamura E., Okamoto N., Nishioka H., Karasugi T., Hirose J., Mizuta H. The long-term outcome of open-wedge osteotomy of the proximal tibia with hemicallotasis. Bone Jt J. 2014;96 B(4):467–472. doi: 10.1302/0301-620X.96B4.31345. [DOI] [PubMed] [Google Scholar]
- 38.Giffin J.R., Vogrin T.M., Zantop T., Woo S.L., Harner C.D. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 39.El-Azab H., Glabgly P., Paul J., Imhoff A.B., Hinterwimmer S. Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med. 2010 Feb;38(2):323–329. doi: 10.1177/0363546509348050. [DOI] [PubMed] [Google Scholar]