Abstract
Purpose
One of the most common adverse events after orthopaedic surgery, with a potential for subsequent serious morbidity and mortality is venous thromboembolism (VTE). Bibliometric analysis has been performed regarding many topics and across orthopaedics. As DVT prophylaxis is a major component of both orthopaedic surgery considerations and research, a bibliometric analysis in this area would prove beneficial in not only in understanding the research done in the field thus far, but would also direct future research efforts.
Methods
The Web of Science (WoS) database from the Institute of Scientific Information (ISI) was used to compile articles for bibliometric analysis using Boolean search: ((Orthopaedic∗ OR Orthopaedic∗) AND (thromboprophylaxis OR Thromboembolism OR Deep vein thrombosis OR thrombus OR embolism OR anticoagulation OR Embolus OR prophylaxis)).
Results
The Top 100 cited articles included in the final list generated a total of 21,099 citations. The highest cited article was Prevention of venous thromboembolism by Geerts et al. published in Chest, which had a total of 2802 on WoS, and a calculated citation density of 215.54 of citations/years since publication. Comparing the overall citation against the year of publication there was a slight positive trend favoring more recent publications (R-value: 0.142; adjusted R-squared: 0.01; p = 0.16). Analysis of an articles Level of Evidence (LOE), 17 were grade with a level of I.
Conclusions
Orthopaedic thromboprophylaxis is an ever-changing field that is at the forefront of orthopaedic literature. The significant trend favoring high quality research within orthopaedic thromboprophylaxis demonstrates the importance of this topic and there was a need for a guide to best understand the evolution of DVT prophylaxis.
Keywords: Venous thromboprophylaxis, Deep vein thrombosis, Pulmonary embolism, Bibliometric analysis, Anticoagulation
1. Introduction
One of the most common adverse events after orthopaedic surgery, with a potential for subsequent serious morbidity and mortality is venous thromboembolism (VTE).1 The incidence of deep venous thrombosis (DVT) has been reported to be as high as 60% in major orthopaedic surgery, with mortality of 6% associated with DVT and 12% with pulmonary embolism (PE).2 The economic cost to the health system has been estimated to be more than twice as high for patients with VTE than without, for various orthopaedic surgery procedures,3, 4, 5 with costs increasing over time.6
There are many different prophylactic anticoagulation regimens available for treatment of VTE.2,7 Similarly, various professional societies and countries have different guidelines for prevention of DVT in orthopaedics.8 The American College of Chest Physicians (ACCP) published guidelines in 2012 for antithrombotic therapy for patients undergoing various orthopaedic procedures.9 A recent comparison of guidelines highlights the ACCP recommendations to still be the most thorough and appropriate.2
Treatment and prevention of VTE in orthopaedic surgery is one of the most heavily studied topics in orthopaedic surgery, and is ever evolving. A search of “orthopaedic/orthopaedic” and “deep vein thrombosis prophylaxis” yields over 40,000 results on Web of Science. Given the volume and complexity of this landscape, it is difficult to thoroughly evaluate and interpret the large body of literature surrounding VTE in orthopaedic surgery. One type of analysis of scientific literature is a bibliometric analysis, which can be useful in stratifying literature based on its impact on a field. It was first defined as a term in 1969, and became a Medical Subject Heading (MeSH) in 1990.10 The use of bibliometric analyses has grown substantially in orthopaedic surgery, especially over the past 20 years.10
A bibliometric analysis provides understanding of how literature regarding a topic changes over time, and allows us to evaluate the most influential articles to inform decision-making. The parameters examined are the number of publications by year, author, country, type of study design, and overall number of citations. Analyzing citation patterns with bibliometrics can reveal how a specific field has been influenced by past publications, the growth patterns of certain publications, which papers have had the greatest impact. A bibliometric analysis can also identify gaps in the publication pool in specific areas. Bibliometric analysis has been performed regarding many topics and across all sub-specialties of orthopaedics and medicine,11, 12, 13, 14 however, to our knowledge there has not yet been an analysis of the body of literature of DVT prophylaxis in orthopaedic surgery. As DVT prophylaxis is a major component of both orthopaedic surgery considerations and research, a bibliometric analysis in this area may prove beneficial in not only in understanding the research done in the field thus far, but may also help direct future research efforts.
The primary aim of this study is to identify the top cited publications and utilize bibliometric analysis to objectively analyze the most influential articles regarding thromboembolism in orthopaedic surgery. This information could aid surgeons, educators and researches in understanding the important historic and current literature regarding DVT in orthopaedic surgery.
2. Methods
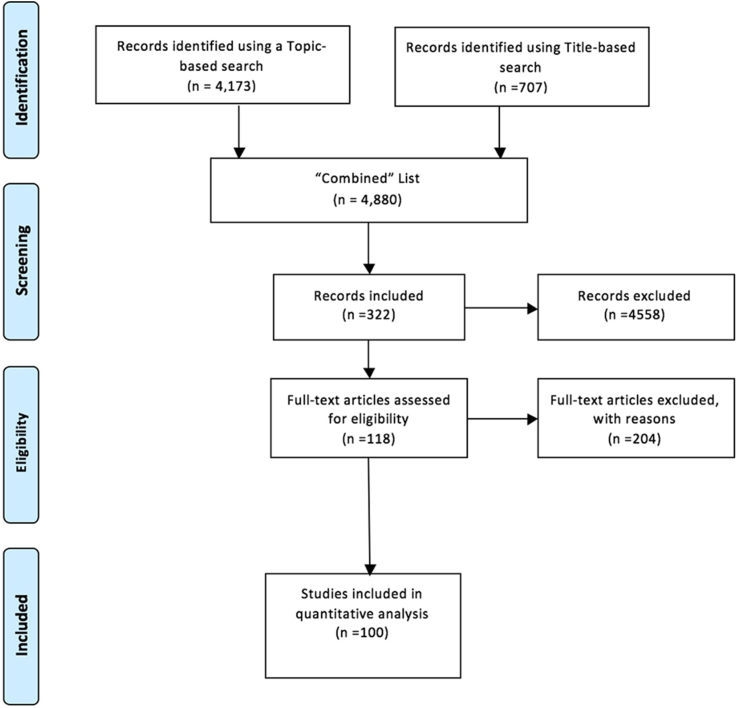
The Web of Science (WoS) database from the Institute of Scientific Information (ISI) was used to compile articles for bibliometric analysis using Boolean search. The Boolean terms which generated the most number of articles for the top 100 list were: ((Orthopaedic∗ OR Orthopaedic∗) AND (thromboprophylaxis OR Thromboembolism OR Deep vein thrombosis OR thrombus OR embolism OR anticoagulation OR Embolus OR prophylaxis)) Initial query was conducted in June 2020 and was reviewed independently by two of the authors (AS and RY). Boolean search terms were conducted using both Topic Search (TS) and Title Search (TI) parameters and results were then aggregated on WoS to create a Combined list. Peer-reviewed research articles, meta-analyses, systematic reviews, case reviews, literature reviews, and panel opinions were included in analysis. Notes, errata, editorial comments, or letters to the editor were excluded. Each abstract of articles on the Combined list was used to screen relevant articles to be included in a Secondary Combined List. Articles of the Secondary List were further screened based on analysis of each full text to determine its relevance to orthopaedic surgery and DVT thromboprophylaxis to create a final list for analysis (Fig. 1).
Fig. 1.
PRISMA-style flow diagram of inclusion and exclusion criterion.
Initial search query was not limited by language, country of publication, institution affiliation, date range, or journal. Articles were then only included if they were peer-reviewed articles, systematic reviews, or editorials. Search results were then sorted by number of citations and the most prolific articles were selected for analysis. There were no additional exclusion criterion.
From the final compiled lists of most cited articles the following data was extracted: date of publication, total citation count, overall citation rate (overall number of citations/years since publication), current citation rate (citations since 2013/years since publication), lead author, country of publication, level of evidence (LOE), topic category. LOE was determined using the Canadian Task Force on Preventative Health’s evidence based medicine guidelines15 and unanimously decided by two authors (AS and LM). Articles were then put in to categories based on clinical focus and are the following; Epidemiologic, Comparison, Aspirin, Asymptomatic DVT, Direct Thrombin Inhibitor, LMWH, Mechanical, Novel Xa Inhibitors, Panel Opinion, Unfractionated Heparin and Warfarin. Comparison classification included all papers which compared two different thromboprophylaxis regiment. Mechanical included all forms of mechanical based thromboprophylaxis, including but not limited to Inferior Vena Cava Filters (IVCs), Sequential Compression Device (SCDs), or Pneumatic Boots.
2.1. Statistics
All analysis was conducted using Microsoft Excel v. 16.16.7 and IBM SPSS v. 26. Shapiro-Wilk test was conducted to test for normality and all normalized data is expressed with medians and standard deviations. Kruskal-Wallis tests were used to assess differences of nonparametric values. One way ANOVA were used to compare normally distributed data, additional post-hoc analysis was conducted to accurately compare significance between groups. Kendall tau tests were used to determine correlations over time. A p value of 0.05 was used to determine significance.
2.2. VOS viewer
Terms were analyzed using Visualization of Similarities (VOS) software version 1.6.15 as it is a recognized and widely used analysis tool especially in bibliometric analyses. Terms with a minimum of 3 connections were used and the top 60% of terms were included in the keyword web.
3. Results
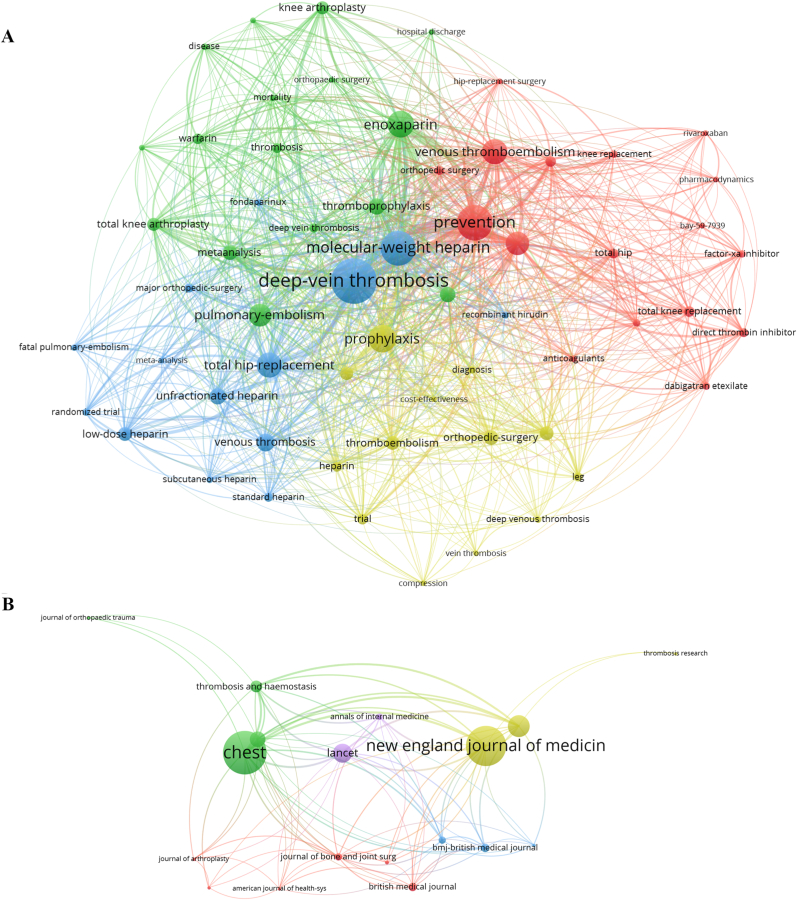
The Top 100 cited articles included in the final overall orthopaedic list generated a total of 21,099 citations (Table 1, Table 2). The most commonly cited keywords of articles included in VOS Viewer analysis include, “deep vein thrombosis”, “low molecular-weight heparin”, and “prevention” (Fig. 2A).
Table 1.
Top 100 most cited articles on venous thromboembolism and thromboprophylaxis across orthopaedic surgery: Articles 1-50.
| No. | Article Title | Authors | Source Title | Publication Date | Total Citations |
|---|---|---|---|---|---|
| 1 | Prevention Of Venous Thromboembolism | Geerts, William H. Et Al. | Chest | Jun 2008 | 2802 |
| 2 | Reduction In Fatal Pulmonary-Embolism And Venous Thrombosis By Perioperative Administration Of Subcutaneous Heparin - Overview Of Results Of Randomized Trials In General, Orthopaedic, And Urologic Surgery | Collins, R Et·Al. | New England Journal Of Medicine | May-88 | 1122 |
| 3 | Rivaroxaban Versus Enoxaparin For Thromboprophylaxis After Knee Arthroplasty | Eriksson, Bengt Et Al. | New England Journal Of Medicine | Jun-08 | 957 |
| 4 | Prevention Of Vte In Orthopaedic Surgery Patients Antithrombotic Therapy And Prevention Of Thrombosis, 9 Th Ed: American College Of Chest Physicians Evidence-Based Clinical Practice Guidelines | Falck-Ytter, Yngve Et Al. | Chest | Feb 2012 | 909 |
| 5 | A Prospective-Study Of Venous Thromboembolism After Major Trauma | Geerts, Wh Et Al. | New England Journal Of Medicine | Dec-94 | 868 |
| 6 | Oral Dabigatran Etexilate Vs. Subcutaneous Enoxaparin For The Prevention Of Venous Thromboembolism After Total Knee Replacement: The Re-Model Randomized Trial | Eriksson, B. I. Et Al. | Journal Of Thrombosis And Haemostasis | Nov 2007 | 712 |
| 7 | Prevention Of Pulmonary Embolism And Deep Vein Thrombosis With Low Dose Aspirin: Pulmonary Embolism Prevention (Pep) Trial | O’Brien, J Et Al. | Lancet | Apr-00 | 690 |
| 8 | Low-Molecular-Weight Heparin Versus Standard Heparin In General And Orthopaedic-Surgery - A Metaanalysis | Nurmohamed, Mt Et Al. | Lancet | Jul-92 | 552 |
| 9 | Fondaparinux Vs Enoxaparin For The Prevention Of Venous Thromboembolism In Major Orthopaedic Surgery - A Meta-Analysis Of 4 Randomized Double-Blind Studies | Turpie, Ag Etal. | Archives Of Internal Medicine | Sep-02 | 546 |
| 10 | A Comparison Of Low-Dose Heparin With Low-Molecular-Weight Heparin As Prophylaxis Against Venous Thromboembolism After Major Trauma | Geerts, Wh Et Al. | New England Journal Of Medicine | Sep-96 | 524 |
| 11 | Low-Molecular-Weight Heparin (Enoxaparin) As Prophylaxis Against Venous Thromboembolism After Total Hip Replacement | Bergqvist, D Et Al. | New England Journal Of Medicine | Sep-96 | 389 |
| 12 | Regular Review - Risk Of And Prophylaxis For Venous Thromboembolism In Hospital Patients | Lowe, Gdo Et Al. | Bmj-British Medical Journal | Sep 5, 1992 | 379 |
| 13 | Extended-Duration Prophylaxis Against Venous Thromboembolism After Total Hip Or Knee Replacement: A Metaanalysis Of The Randomized Trials | Eikelboom, Jw Et Al. | Lancet | Jul-01 | 376 |
| 14 | Low-Molecular-Weight Heparin In Prevention Of Perioperative Thrombosis | Leizorovicz, A Et Al. | Bmj-British Medical Journal | Oct-92 | 330 |
| 15 | A New Oral Direct Thrombin Inhibitor, Dabigatran Etexilate, Compared With Enoxaparin For Prevention Of Thromboembolic Events Following Total Hip Or Knee Replacement: The Bistro Ii Randomized Trial | Eriksson, Bi Et Al. | Journal Of Thrombosis And Haemostasis | Jan 2005 | 314 |
| 16 | Accuracy Of Ultrasound For The Diagnosis Of Deep Venous Thrombosis In Asymptomatic Patients After Orthopaedic-Surgery - A Metaanalysis | Wells, Ps Et Al. | Annals Of Internal Medicine | Jan 1, 1995 | 285 |
| 17 | Incidence Of Venous Thromboembolism Verified By Necropsy Over 30 Years | Lindblad, B Et Al. | British Medical Journal | Mar 23, 1991 | 282 |
| 18 | Duration Of Prophylaxis Against Venous Thromboembolism With Fondaparinux After Hip Fracture Surgery - A Multicenter, Randomized, Placebo-Controlled, Double-Blind Study | Eriksson, Bi Et Al. | Archives Of Internal Medicine | Jun 9, 2003 | 277 |
| 19 | Prolonged Thromboprophylaxis Following Hip Replacement Surgery - Results Of A Double-Blind, Prospective, Randomized, Placebo-Controlled Study With Dalteparin (Fragmin(R)) | Dahl, Oe Et Al. | Thrombosis And Haemostasis | Jan 1997 | 264 |
| 20 | A Meta-Analysis Of Thromboembolic Prophylaxis Following Elective Total Hip Arthroplasty | Freedman, Kb Et Al. | Journal Of Bone And Joint Surgery-American Volume | Jul 2000 | 242 |
| 21 | Differences In Mortality After Fracture Of Hip - The East-Anglian Audit | Todd, Cj Et Al. | British Medical Journal | Apr 8, 1995 | 238 |
| 22 | Bay 59–7939: An Oral, Direct Factor Xa Inhibitor For The Prevention Of Venous Thromboembolism In Patients After Total Knee Replacement. A Phase Ii Dose-Ranging Study | Turpie, Agg Et Al. | Journal Of Thrombosis And Haemostasis | Nov 2005 | 237 |
| 23 | Subcutaneous Low-Molecular-Weight Heparin Compared With Continuous Intravenous Unfractionated Heparin In The Treatment Of Proximal Deep-Vein Thrombosis | Simonneau, G Et Al. | Archives Of Internal Medicine | Jul-93 | 229 |
| 24 | Direct Thrombin Inhibitor Melagatran Followed By Oral Ximelagatran In Comparison With Enoxaparin For Prevention Of Venous Thromboembolism After Total Hip Or Knee Replacement - The Methro Iii Study | Eriksson, Bi Et Al. | Thrombosis And Haemostasis | Feb 2003 | 219 |
| 25 | Prevention Of Deep-Vein Thrombosis After Hip-Replacement - Randomized Comparison Between Unfractionated Heparin And Low-Molecular-Weight Heparin | Leyvraz, Pf Et Al. | British Medical Journal | Sep-91 | 215 |
| 26 | Frequency Of Myocardial Infarction, Pulmonary Embolism, Deep Venous Thrombosis, And Death Following Primary Hip Or Knee Arthroplasty | Mantilla, Cb Et Al. | Anesthesiology | May 2002 | 209 |
| 27 | Death And Thromboembolic Disease After Total Hip-Replacement - A Series Of 1162 Cases With No Routine Chemical Prophylaxis | Warwick, D Et Al. | Journal Of Bone And Joint Surgery-British Volume | Jan 1995 | 207 |
| 28 | Efficacy And Safety Of The Oral Direct Factor Xa Inhibitor Apixaban For Symptomatic Deep Vein Thrombosis. The Botticelli Dvt Dose-Ranging Study | Buller, H. Et Al. | Journal Of Thrombosis And Haemostasis | Aug 2008 | 197 |
| 29 | A Metaanalysis Of Methods To Prevent Venous Thromboembolism Following Total Hip-Replacement | Imperiale, Tf Et Al. | Jama-Journal Of The American Medical Association | Jun 8, 1994 | 197 |
| 30 | Population Pharmacokinetics And Pharmacodynamics Of Rivaroxaban - An Oral, Direct Factor Xa Inhibitor In Patients Undergoing Major Orthopaedic Surgery | Mueck, Wolfgang Et Al. | Clinical Pharmacokinetics | 2008 | 190 |
| 31 | A Cost-Effectiveness Analysis Of Prophylaxis Against Deep-Vein Thrombosis In Major Orthopaedic-Surgery | Oster, G Et Al. | Jama-Journal Of The American Medical Association | Jan 9, 1987 | 181 |
| 32 | Prevention Of Deep-Vein Thrombosis After Total Hip Replacement: Direct Thrombin Inhibition With Recombinant Hirudin, Cgp 39,393 | Eriksson, Bi Et Al. | Lancet | Mar 9, 1996 | 172 |
| 33 | Outcomes For Older Patients With Hip Fractures: The Impact Of Orthopaedic And Geriatric Medicine Cocare | Fisher, Aa Et Al. | Journal Of Orthopaedic Trauma | Mar 2006 | 168 |
| 34 | Insufficient Duration Of Venous Thromboembolism Prophylaxis After Total Hip Or Knee Replacement When Compared With The Time Course Of Thromboembolic Events - Findings From The Global Orthopaedic Registry | Warwick, D. Et Al. | Journal Of Bone And Joint Surgery-British Volume | Jun 2007 | 167 |
| 35 | The Direct Thrombin Inhibitor Melagatran Followed By Oral Ximelagatran Compared With Enoxaparin For The Prevention Of Venous Thromboembolism After Total Hip Or Knee Replacement: The Express Study | Eriksson, Bi Et Al. | Journal Of Thrombosis And Haemostasis | Dec 2003 | 165 |
| 36 | Preoperative Or Postoperative Start Of Prophylaxis For Venous Thromboembolism With Low-Molecular-Weight Heparin In Elective Hip Surgery? | Strebel, N Et Al. | Archives Of Internal Medicine | Jul-02 | 147 |
| 37 | Prophylaxis Of Postoperative Thromboembolism With Low-Molecular-Weight Heparins | Jorgensen, Ln Et Al | British Journal Of Surgery | Jun 1993 | 147 |
| 38 | Prevention Of Venous Thromboembolism In Orthopaedic Patients | Salzman, Ew Et Al. | Journal Of Bone And Joint Surgery-American Volume | 1976 | 144 |
| 39 | Efficacy And Cost Of Low-Molecular-Weight Heparin Compared With Standard Heparin For The Prevention Of Deep-Vein Thrombosis After Total Hip-Arthroplasty | Anderson, Dr Et Al. | Annals Of Internal Medicine | Jan 2008 | 137 |
| 40 | Efficacy And Safety Of Dabigatran Etexilate For The Prevention Of Venous Thromboembolism Following Total Hip Or Knee Arthroplasty A Meta-Analysis | Wolowacz, Sorrel E. Et Al. | Thrombosis And Haemostasis | Dec-93 | 135 |
| 41 | American Association Of Orthopaedic Surgeons And American College Of Chest Physicians Guidelines For Venous Thromboembolism Prevention In Hip And Knee Arthroplasty Differ What Are The Implications For Clinicians And Patients? | Eikelboom, Jw Et Al. | Chest | Feb 2009 | 134 |
| 42 | Oral Rivaroxaban For The Prevention Of Symptomatic Venous Thromboembolism After Elective Hip And Knee Replacement | Eriksson, B. I. Et Al. | Journal Of Bone And Joint Surgery-British Volume | May 2009 | 130 |
| 43 | Comparison Of The Use Of A Foot Pump With The Use Of Low-Molecular-Weight Heparin For The Prevention Of Deep-Vein Thrombosis After Total Hip Replacement - A Prospective, Randomized Trial | Warwick, D Et Al. | Journal Of Bone And Joint Surgery-American Volume | Aug 1998 | 129 |
| 44 | Hospitals’ Compliance With Prophylaxis Guidelines For Venous Thromboeimbolism | Yu, Hsing-Ting Et Al. | American Journal Of Health-System Pharmacy | Jan-07 | 128 |
| 45 | Deep-Vein Thrombosis Rates After Major Orthopaedic Surgery In Asia. An Epidemiological Study Based On Postoperative Screening With Centrally Adjudicated Bilateral Venography | Piovella, F Et Al. | Journal Of Thrombosis And Haemostasis | Dec 2005 | 128 |
| 46 | Incidence Of Venographically Proved Deep Vein Thrombosis After Knee Arthroscopy | Demers, C Et Al. | Archives Of Internal Medicine | Jan-98 | 122 |
| 47 | Coagulation Parameters In Patients Receiving Dabigatran Etexilate Or Rivaroxaban: Two Observational Studies In Patients Undergoing Total Hip Or Total Knee Replacement | Freyburger, G Et Al. | Thrombosis Research | May 2011 | 118 |
| 48 | Prevention Of Venous Thromboembolism - Adherence To The 1995 American College Of Chest Physicians Consensus Guidelines For Surgical Patients | Stratton, Ma Et Al. | Archives Of Internal Medicine | Feb-00 | 118 |
| 49 | Rd Heparin Compared With Warfarin For Prevention Of Venous Thromboembolic Disease Following Total Hip Or Knee Arthroplasty | Friedman, Rj Et Al | Journal Of Bone And Joint Surgery-American Volume | Aug 1994 | 117 |
| 50 | A Dose-Ranging Study Of The Oral Direct Thrombin Inhibitor, Ximelagatran, And Its Subcutaneous Form, Melagatran, Compared With Dalteparin In The Prophylaxis Of Thromboembolism After Hip Or Knee Replacement: Methro I | Eriksson, Bi Et Al. | Thrombosis And Haemostasis | Feb 2002 | 116 |
Table 2.
Top 100 most cited articles on venous thromboembolism and thromboprophylaxis across orthopaedic surgery: Articles 51-100.
| No. | Article Title | Authors | Source Title | Publication Date | Total Citations |
|---|---|---|---|---|---|
| 51 | Dabigatran, Rivaroxaban, Or Apixaban Versus Enoxaparin For Thromboprophylaxis After Total Hip Or Knee Replacement: Systematic Review, Meta-Analysis, And Indirect Treatment Comparisons | Gomez-Outes, A Et Al. | Bmj-British Medical Journal | Jun-12 | 115 |
| 52 | Antithrombotic Therapy Practices In Us Hospitals In An Era Of Practice Guidelines | Tapson, Vf Et Al. | Archives Of Internal Medicine | Jul-05 | 113 |
| 53 | Intermittent Pneumatic Compression And Deep Vein Thrombosis Prevention - A Meta-Analysis In Postoperative Patients | Urbankova, J Et Al | Thrombosis And Haemostasis | Dec 2005 | 108 |
| 54 | Deep Venous Thrombosis After Posterior Spinal Surgery | Oda, T Et Al. | Spine | Nov-00 | 108 |
| 55 | Late Occurring Clinical Deep Vein Thrombosis In Joint-Operated Patients | Dahl, Oe Et Al. | Acta Orthopaedica Scandinavica | Feb 2000 | 108 |
| 56 | Epidemiology Of Venous Thromboembolism In Asian Patients Undergoing Major Orthopaedic Surgery Without Thromboprophylaxis. The Smart Study | Leizorovicz, A Et Al. | Journal Of Thrombosis And Haemostasis | Jan 2005 | 107 |
| 57 | Temporal Trends In Prevention Of Venous Thromboembolism Following Primary Total Hip Or Knee Arthroplasty 1996–2001 - Findings From The Hip And Knee Registry | Anderson, Fa Et Al. | Chest | Dec 2003 | 107 |
| 58 | Effectiveness Of Pneumatic Leg Compression Devices For The Prevention Of Thromboembolic Disease In Orthopaedic Trauma Patients - A Prospective, Randomized Study Of Compression Alone Versus No Prophylaxis | Fisher, Cg Et Al. | Journal Of Orthopaedic Trauma | Feb 1995 | 105 |
| 59 | Subcutaneous Low-Molecular Weight Heparin Or Oral Anticoagulants For The Prevention Of Deep-Vein Thrombosis In Elective Hip And Knee Replacement? | Hamulyak, K Et Al. | Thrombosis And Haemostasis | Dec 1995 | 103 |
| 60 | Efficacy And Safety Of Enoxaparin To Prevent Deep Venous Thrombosis After Hip-Replacement Surgery | Spiro, Te Et Al. | Annals Of Internal Medicine | Jul-94 | 103 |
| 61 | Mortality And Fatal Pulmonary Embolism After Primary Total Hip Replacement - Results From A Regional Hip Register | Fender, D Et Al. | Journal Of Bone And Joint Surgery-British Volume | Nov 1997 | 101 |
| 62 | Aspirin Versus Low-Molecular-Weight Heparin For Extended Venous Thromboembolism Prophylaxis After Total Hip Arthroplasty A Randomized Trial | Anderson, Dr Et Al. | Annals Of Internal Medicine | Jun-13 | 98 |
| 63 | Prevention Of Venous Thromboembolism After Knee Arthroscopy With Low-Molecular Weight Heparin (Reviparin): Results Of A Randomized Controlled Trial | Wirth, T Et Al. | Arthroscopy | Apr 2001 | 96 |
| 64 | Prevention Of Venous Thromboembolism In Orthopaedic Surgery With Vitamin K Antagonists: A Meta-Analysis | Mismetti, P Et Al | Journal Of Thrombosis And Haemostasis | Jul 2004 | 87 |
| 65 | Controversies In Timing Of The First Dose Of Anticoagulant Prophylaxis Against Venous Thromboembolism After Major Orthopaedic Surgery | Raskob, Ge; Hirsh, J | Chest | Dec 2003 | 85 |
| 66 | American Academy Of Orthopaedic Surgeons Clinical Practice Guideline On Prevention Of Symptomatic Pulmonary Embolism In Patients Undergoing Total Hip Or Knee Arthroplasty | Johanson, Na Et Al. | Journal Of Bone And Joint Surgery-American Volume | Jul 2009 | 84 |
| 67 | Identifying Orthopaedic Patients At High Risk For Venous Thromboembolism Despite Thromboprophylaxis | Schiff, Rl Et Al | Chest | Nov 2005 | 77 |
| 68 | Orthopaedic Surgeons And Thromboprophylaxis | Laverick, Md Et Al | British Medical Journal | Sep-91 | 77 |
| 69 | Ultrasound Screening For Asymptomatic Deep Vein Thrombosis After Major Orthopaedic Surgery: The Venus Study | Schellong, Sm Et Al. | Journal Of Thrombosis And Haemostasis | Jul 2007 | 75 |
| 70 | Efficacy And Safety Of Low Molecular Weight Heparin, Unfractionated Heparin And Warfarin For Thrombo-Embolism Prophylaxis In Orthopaedic Surgery: A Meta-Analysis Of Randomized Clinical Trials | Palmer, Aj Et Al. | Haemostasis | Mar–Apr 1997 | 73 |
| 71 | Oral Anticoagulants In Development - Focus On Thromboprophylaxis In Patients Undergoing Orthopaedic Surgery | Eriksson, B Et Al | Drugs | 2006 | 70 |
| 72 | Prevention Of Venous Thromboembolism - A Survey Of Methods Used By Orthopaedic And General Surgeons | Morris, Gk | Lancet | 1980 | 70 |
| 73 | Prophylaxis For Thromboembolic Disease - Recommendations From The American College Of Chest Physicians - Are They Appropriate For Orthopaedic Surgery? | Callaghan, Jj Et Al. | Journal Of Arthroplasty | Apr 2005 | 63 |
| 74 | Rivaroxaban For Thromboprophylaxis After Orthopaedic Surgery: Pooled Analysis Of Two Studies | Fisher, Wd Et Al. | Thrombosis And Haemostasis | Jun 2007 | 59 |
| 75 | Superiority Of Fondaparinux Over Enoxaparin In Preventing Venous Thromboembolism In Major Orthopaedic Surgery Using Different Efficacy End Points | Turpie, Agg Et Al. | Chest | Aug 2004 | 59 |
| 76 | Risks And Benefits Of Prophylaxis Against Venous Thromboembolism In Orthopaedic Surgery | Gillespie, W Et Al. | Journal Of Bone And Joint Surgery-British Volume | May 2000 | 59 |
| 77 | Preadmission Hyperglycemia Is An Independent Risk Factor For In-Hospital Symptomatic Pulmonary Embolism After Major Orthopaedic Surgery | Mraovic, B Et Al. | Journal Of Arthroplasty | Jan 2010 | 51 |
| 78 | The Cost-Effectiveness Of Fondaparinux Compared With Enoxaparin As Prophylaxis Against Thromboembolism Following Major Orthopaedic Surgery | Gordois, A Et Al. | Journal Of Thrombosis And Haemostasis | Oct 2003 | 50 |
| 79 | Efficacy And Safety Of Fondaparinux In Major Orthopaedic Surgery According To The Timing Of Its First Administration | Turpie, A Et Al | Thrombosis And Haemostasis | Aug 2003 | 50 |
| 80 | Cost Of Venous Thromboembolism Following Major Orthopaedic Surgery In Hospitalized Patients | Ollendorf, Da Et Al | American Journal Of Health-System Pharmacy | Sep 15, 2002 | 50 |
| 81 | Venous Thromboembolism Prophylaxis After Major Orthopaedic Surgery: A Pooled Analysis Of Randomized Controlled Trials | Brown, Greg A. | Journal Of Arthroplasty | Sep 2009 | 49 |
| 82 | A Non-Interventional Comparison Of Rivaroxaban With Standard Of Care For Thromboprophylaxis After Major Orthopaedic Surgery In 17,701 Patients With Propensity Score Adjustment | Turpie, Agg Et Al. | Thrombosis And Haemostasis | Jan 2014 | 48 |
| 83 | Flexibility In Administration Of Fondaparinux For Prevention Of Symptomatic Venous Thromboembolism In Orthopaedic Surgery | Colwell, Cw Et Al. | Journal Of Arthroplasty | Jan 2006 | 47 |
| 84 | Economic Consequences Of Venous Thromboembolism Following Major Orthopaedic Surgery | Oster, G Et Al. | Annals Of Pharmacotherapy | Mar 2004 | 45 |
| 85 | Comparing Consensus Guidelines On Thromboprophylaxis In Orthopaedic Surgery | Struijk-Mulder, Mc Et Al. | Journal Of Thrombosis And Haemostasis | Apr 2010 | 44 |
| 86 | Aspirin For The Prophylaxis Of Venous Thromboembolic Events In Orthopaedic Surgery Patients: A Comparison Of The Aaos And Accp Guidelines With Review Of The Evidence | Stewart, Dw Et Al. | Annals Of Pharmacotherapy | Jan 2013 | 43 |
| 87 | Symptomatic Venous Thromboembolism And Mortality In Orthopaedic Surgery - An Observational Study Of 45,968 Consecutive Procedures | Lapidus, Lj Et Al. | Bmc Musculoskeletal Disorders | Jun 4, 2013 | 42 |
| 88 | Venous Thromboembolism Following Major Orthopaedic Surgery: Review Of Epidemiology And Economics | Edelsberg, J Et Al. | American Journal Of Health-System Pharmacy | Nov 1, 2001 | 42 |
| 89 | Measurement Of Dabigatran And Rivaroxaban In Primary Prevention Of Venous Thromboembolism In 106 Patients, Who Have Undergone Major Orthopaedic Surgery: An Observational Study | Samama, Mm Et Al | Journal Of Thrombosis And Thrombolysis | Feb 2013 | 41 |
| 90 | Systematic Review And Meta-Analysis On The Rate Of Postoperative Venous Thromboembolism In Orthopaedic Surgery In Asian Patients Without Thromboprophylaxis | Kanchanabat, B Et Al. | British Journal Of Surgery | Oct 2011 | 41 |
| 91 | Deep Venous Thrombosis After Orthopaedic Surgery In Adult Cancer Patients | Lin, Pp Et Al. | Journal Of Surgical Oncology | May 1998 | 41 |
| 92 | The Safety And Efficacy Of Extended Thromboprophylaxis With Fondaparinux After Major Orthopaedic Surgery Of The Lower Limb With Or Without A Neuraxial Or Deep Peripheral Nerve Catheter: The Expert Study | Singelyn, Fj Et Al. | Anesthesia And Analgesia | Dec 2007 | 40 |
| 93 | Deep Venous Thrombosis Prophylaxis For Total Joint Arthroplasty: American Academy Of Orthopaedic Surgeons Guidelines | Parvizi, J Et Al. | Journal Of Arthroplasty | Oct 2008 | 39 |
| 94 | Orthopaedic Thromboprophylaxis | Warwick, D.; Dahl, O. E.; Fisher, W. D. | Journal Of Bone And Joint Surgery-British Volume | Feb 2008 | 39 |
| 95 | Post Discharge Clinically Overt Venous Thromboembolism In Orthopaedic Surgery Patients With Negative Venography An Overview Analysis | Ricotta, S | Thrombosis And Haemostasis | Dec 1996 | 38 |
| 96 | Impaired Fibrinolysis And Postoperative Thromboembolism In Orthopaedic Patients | Eriksson, Bi | Thrombosis Research | Apr 1991 | 38 |
| 97 | The Risk Of Venous Thromboembolism In The Orthopaedic Patient: Epidemiological And Physiological Data | Paiement, Gd | Orthopaedics | Feb 1997 | 37 |
| 98 | Assessing The Safety Profiles Of New Anticoagulants For Major Orthopaedic Surgery Thromboprophylaxis | Hull, Rd Et Al | Clinical And Applied Thrombosis-Hemostasis | Aug-09 | 36 |
| 99 | Incidence And Risk Factors For Development Of Venous Thromboembolism In Indian Patients Undergoing Major Orthopaedic Surgery: Results Of A Prospective Study | Bagaria, V | Postgraduate Medical Journal | Feb 2006 | 36 |
| 100 | Aspirin Versus Anticoagulation For Prevention Of Venous Thromboembolism Major Lower Extremity Orthopaedic Surgery: A Systematic Review And Meta-Analysis | Drescher, Fs Et Al. | Journal Of Hospital Medicine | Sep 2014 | 35 |
Fig. 2.
Visualization of Similarities (VoS) analysis of Keywords (2A) and Journals relative to number of citations (2B).
The highest cited article was Prevention of venous thromboembolism by Geerts et al.,16 published in Chest, which had a total of 2802 on WoS, and a calculated citation density of 215.54 of citations/years since publication (Fig. 2B). The second highest cited article was Reduction In Fatal Pulmonary-Embolism And Venous Thrombosis By Perioperative Administration Of Subcutaneous Heparin - Overview Of Results Of Randomized Trials In General, Orthopaedic, And Urologic Surgery by Collins et al.17 with a total of 1122 citations and a citation density of 34.0 was published in the New England Journal of Medicine (NEJM) (Fig. 2B).
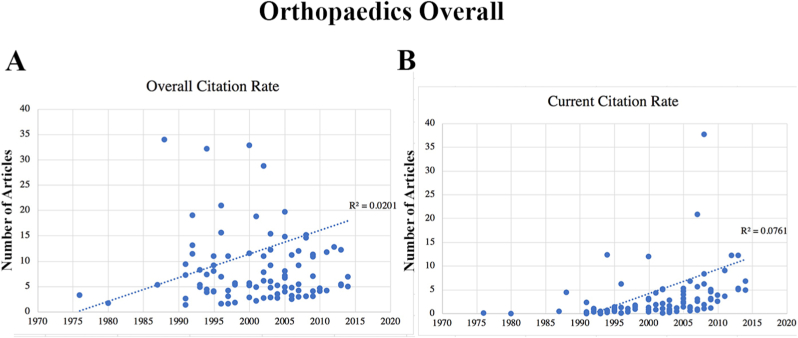
When comparing the overall citation against the year of publication there was a slight positive trend favoring more recent publications (R-value: 0.142; adjusted R-squared: 0.01; p = 0.16). The current citation rate demonstrated a slightly more positive trend in favor of recent articles (R-value: 0.276; adjusted R-squared: 0.07; p = 0.005) (Fig. 3).
Fig. 3.
Linear regression analysis of Overall and Current Citation Rates.
Bengt Eriksson was the most prolific author whose articles made it to the final list accounting for 16% of the top 100 and 3688 citations in total (230.5 citations/article). Alexander Turpie was the second most prolific author included in the final list with a total of 11 publications (11%) with 1626 citations in total (147.82 citations/article).
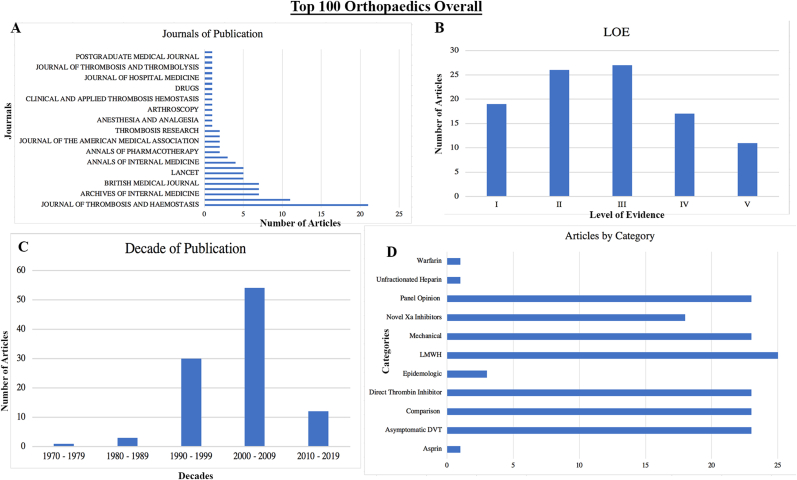
The journal with the most number of publications in the top 100 was The Journal of Thrombosis and Haemostasis (21%) which had an impact factor of 4.662. Followed by the Journal of Bone and Joint Surgery with 11% of publications, and with an impact of 4.31. Lastly, the Archives of Internal Medicine (JAMA) and CHEST each accounting for 7% of the total analyzed articles, with an impact factor of 20.77 and 9.67, respectively (Fig. 4A).
Fig. 4.
Characteristics of the top 100 most cited articles.
The included publications had a date range of 1976–2014, with a majority of publications published in the decade of 2000–2009 (54%) followed by the decade of 1990–1999 (30%). Only 4% of articles included in analysis were published between the years 1976–1989. The most recent decade from 2010 to 2019 only accounted for 14% of articles (Fig. 4C).
Articles included in the final list were assigned a LOE determined by the study design and strength of analysis. Based on the Oxford Centre determination37 of LOE, 11 articles were graded with a level of V, 17 articles were graded with a level of IV, 27 were graded with a level of III, 26 were graded with a level of II, and lastly 17 were grade with a level of I (Fig. 4B). Initial one-way ANOVA determined a statistically significant difference of number citations amongst the 5 LOEs (p = 0.002). Follow-up post-hoc analysis determined there was only a statistically significant difference in number of citations of those articles graded LOE of level I against all other LOE grades (Grade I vs II p = 0.04; Grade I vs III p = 0.008; Grade I vs IV p = 0.2; Grade I vs V p = 0.01).
Final analysis of the Top 100 list focused on the articles’ topic categories. We found that 25% (n = 25) of articles focused on Epidemiology, followed by articles focused on comparing two different thromboprophylaxis regimens (23%; n = 23). Lastly, 18% (n = 18) of articles included in analysis were panel opinions (Fig. 4D).
4. Discussion
Our study’s aggregation and further analysis aims to provide a toolkit for orthopaedic surgeons to navigate the topic of venous thromboembolism, DVT thromboprophylaxis across orthopaedic surgery. This study’s focus on citation number provides an accurate and objective measure of a publication’s impact within the orthopaedic literature. Our study’s use of the VOS Viewer provides a visual mapping of keywords and journals of the most prolific publications on DVTs. This was included in part to provide readers a quick overview of the most relevant topics included in the literature, as well as providing a list of the most influential journals on the topic of DVTs. Studies included in analysis were highly cited for a multitude of factors like clinical significance, study quality, and importance of the work in orthopaedics.
Primary analysis of the top 5 most citied articles highlights many of the most influential trends in orthopaedic thromboprophylaxis. Of the top five, two are the ACCP thromboprophylaxis guidelines with the 8th edition being the most cited,16 and 9th edition as the fourth most cited9; both of which are highly influential and will be discussed in greater detail later in the discussion. One explanation for the number of citations of the ACCP guidelines is the broad, multidisciplinary recommendations brought forth by the ACCP. Interestingly, similar AAOS guidelines tallied a total of 84 citations and was 66th overall on our list.18
The second most cited article in our analysis, Reduction In Fatal Pulmonary-Embolism And Venous Thrombosis By Perioperative Administration Of Subcutaneous Heparin - Overview Of Results Of Randomized Trials In General, Orthopaedic, And Urologic Surgery17 captures some of the earliest high quality findings in orthopaedic thromboprophylaxis. Published in the NEJM in 1988, Rory Collins et al. found inconclusive evidence in a metanalyses of RCT for the use of subcutaneous heparin in orthopaedic surgery. The authors recognized the smaller sample sizes of the orthopaedic RCTs which may have accounted for the non-significance. Some of the earliest articles included in analysis focused on whether surgeons of the 1970’s and 1980’s used any thromboprophylaxis or if there was even a cost-benefit of thromboprophylaxis with subcutaneous unfractionated heparin in the post-operative setting due to production costs of heparin vs cheaper agents like warfarin or mechanical prevention.19, 20, 21, 22
The third most cited article, Rivaroxaban versus enoxaparin for thromboprophylaxis after knee arthroplasty (2008),23 highlights both the role of novel factor Xa inhibitors and the driving force of Arthroplasty in DVT literature. Novel anticoagulants, Factor Xa and direct thrombin inhibitors, have been a source of interest in orthopaedics due to the limited risk profile and ease of dosing. Eriksson BI, Borris LC, Friedman RJ et al. are some of the earliest investigators studying the use of these novel anticoagulants in orthopaedics, and demonstrated that “Rivaroxaban reduced the absolute risk of the composite of deep-vein thrombosis, nonfatal pulmonary embolism, and death from any cause by 9.2%.” Furthermore, investigators found a decrease in risk of major venous thromboembolism by 1.6% against enoxaparin in a RCT of 2459 patients undergoing hip arthroplasty. More recent studies have replicated similar results,24, 25, 26, 27, 28, 29, 30, 31 as a result novel anticoagulants have been recognized as a viable alternative in both the most recent ACCP and AAOS guidelines.9,18
The 5th most cited article in analysis, A Prospective-Study Of Venous Thromboembolism After Major Trauma (1994)32, was a noninterventional study which followed 716 patients in the trauma unit using serial impedance plethysmography and lower-extremity venography. Geerts et al. found that 69% of those with a lower-extremity orthopaedic injury had a radiographically confirmed DVT. Additionally, investigators found a significant increase in risk of DVT after femur or tibia fracture (Odds Ratio: 4.82; 95th CI: 2.79–8.33). This article was a call for a standardization of a safe thromboprophylaxis regiment in orthopaedic trauma.
Further analysis showed an increasing trend in the number of articles published on DVT prophylaxis starting in the early 1990’s and ultimately peaking by 2009, with numbers tapering off in the most recent decade. Prior to any formal guidelines, there was a wide array of DVT prophylactic protocols across hospital networks, using combinations of Warfarin, Aspirin, Unfractionated Heparin, and LMWH. Our analysis captured many of these initial studies and metanalyses highlighting the debate.17,19,33, 34, 35, 36, 37, 38
With the increasing use of LMWH regimens36,37,39 in mid 1990’s these medications became a mainstay in orthopaedics. The Fourth American College of Chest Physicians Conference in 1995 further affirmed the LMWHs of the day, however routine thromboprophylaxis was not still widely practiced. Follow up studies from the late-1990’s showed there was a lack of adherence to any thromboprophylaxis regimen, as the 1995 Grade A recommendations had not been widely accepted.40 One study looking at 1907 patients across 10 sites from January 1st, 1996 to February 28th, 1997 showed only 58.3% of Total Hip Replacement (THR) and 53.3% Hip Fracture Repair (HFR) patients received at least some DVT prophylaxis at discharge.41 By the late-1990’s, LMWHs like dalteparin and enoxaparin42 had become the most commonly used LMWH used in post-operative venous thromboprophylaxis. In the early 2000’s, numerous studies revealed there were fewer incidences of Heparin Induced Thrombocytopenia (HIT) with the use of fondaparinux as compared to other LMWHs.43 Our analysis showed a strong uptick in the number of articles in the early 2000’s focusing on demonstrating superiority of fondaparinux against LMWHs.44, 45, 46, 47, 48, 49, 50
In 2000, the “Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial”51 was published, which is the largest trial on venous thromboprophylaxis randomized control trial (RCT) in Orthopaedics with over 17,000 subjects. This trial revealed a 43% decrease in PE with the use of low-dose aspirin against placebo in hip fracture patients.51 This trial has long since sparked debate within the orthopaedic community and caused disagreements across orthopaedic organizations. In 2007 The American Academy of Orthopaedic Surgeons (AAOS) changed opinion regarding standalone aspirin use and recommended the use of low-dose aspirin for low VTE risk patients undergoing elective TKR or THR procedures if they were at no more increased risk than the surgery itself. This recommendation and its moderate grade was further clarified in a 2011 update,52 stating there were difficulties in the comparability of studies included in analysis and not enough high-quality studies.
In 2008, the 8th edition American College of Chest Physician (ACCP) Guidelines, Prevention of venous thromboembolism, the most cited article of our analysis, maintained a position against the use of aspirin as monotherapy “for any patient group,” continuing the controversy. A later update in the 9th edition by the ACCP in 20129 the fourth most cited article of our analysis, recommended the use of aspirin after elective TKR or THR surgeries, realigning with the prior AAOS recommendation. Numerous other articles in our analysis focused on the variations between the AAOS and ACCP guidelines over the years, highlighting the controversy over aspirin’s efficacy and lower-bleeding potential.8,53, 54, 55 More recent studies have reinvigorated the debate of using aspirin55, 56, 57.
Interestingly, the 8th edition ACCP guidelines remained the most cited, and the new 9th edition, though cited 4th on the list has less than one-third the number of citations (2802 vs 909).9,16 Even on further analysis of the annual citation rate since year of publication, the 8th edition demonstrated a higher annualized rate against the 9th edition (215.5 vs 101). This discrepancy could be due to the fewer number of years since publication of the 9th edition, in turn not allowing the recommendations to gain enough traction, or this could reveal a reluctance to adapt the newer 9th edition guidelines. This is an inherent limitation of bibliometric reviews, as objective analysis of impact of an article necessitates the use of total number of times cited as a measure for impact, naturally articles that are more recently published, might not have had the time to accrue adequate number of citations to be represented highly on the list.
With the advent of the novel Xa inhibitors25,26,29,30,58, 59, 60, 61 and Direct thrombin inhibitors,31,62, 63, 64, 65, 66, 67 there has been increasing focus on these agents in DVT prophylaxis. More recent studies have focused on comparing these two new agents and their efficacy in orthopaedic surgery.24,27,28 Of these new anticoagulants, the ACCP’s most recent 9th edition recommendations recognize dabigatran, and apixaban as viable alternatives to patients who refuse injections (Grade 1B Recommendation).
Lastly, ANOVA analysis of an article’s LOE against its respective number of citations revealed a statistically significant relationship favoring articles with an LOE of I. It is known that a majority of orthopaedic research typically is of lower quality due to limitations in adequately randomizing and the ethical implications of not providing certain treatments for the sake of randomization. This predominance of high-quality research highlights the amount of resources and enduring commitment to enhancing thromboprophylaxis in orthopaedics, which is rarely seen with other topics of research in orthopaedics.
5. Conclusions
Orthopaedic thromboprophylaxis is an ever-changing field that is at the forefront of orthopaedic literature. The significant trend favoring high quality research within orthopaedic thromboprophylaxis demonstrates the importance of this topic. Given the endorsement and subsequent rejection of anticoagulation regimens, there was a need for a guide to best understand the evolution of DVT prophylaxis.
References
- 1.Warren J.A., Sundaram K., Anis H.K. Have venous thromboembolism rates decreased in total hip and knee arthroplasty? J Arthroplasty. 2020;35:259–264. doi: 10.1016/j.arth.2019.08.049. [DOI] [PubMed] [Google Scholar]
- 2.Flevas D.A., Megaloikonomos P.D., Dimopoulos L. Thromboembolism prophylaxis in orthopaedics: an update. EFORT Open Rev. 2018;3:136–148. doi: 10.1302/2058-5241.3.170018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels A.H., Kawaguchi S., Contag A.G. Hospital charges associated with “never events”: comparison of anterior cervical discectomy and fusion, posterior lumbar interbody fusion, and lumbar laminectomy to total joint arthroplasty. J Neurosurg Spine. 2016;25:165–169. doi: 10.3171/2015.11.SPINE15776. [DOI] [PubMed] [Google Scholar]
- 4.Ollendorf D.A., Vera-Llonch M., Oster G. Cost of venous thromboembolism following major orthopedic surgery in hospitalized patients. Am J Health Syst Pharm. 2002;59:1750–1754. doi: 10.1093/ajhp/59.18.1750. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi N.N., Abola M.V., Kim C.Y. The incremental cost of inpatient venous thromboembolism after hip fracture surgery. J Orthop Trauma. 2020;34:169–173. doi: 10.1097/BOT.0000000000001675. [DOI] [PubMed] [Google Scholar]
- 6.Shahi A., Chen A.F., Tan T.L. The incidence and economic burden of in-hospital venous thromboembolism in the United States. J Arthroplasty. 2017;32:1063–1066. doi: 10.1016/j.arth.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Landy D.C., Bradley A.T., King C.A., Puri L. Stratifying venous thromboembolism risk in arthroplasty: do high-risk patients exist? J Arthroplasty. 2020;35:1390–1396. doi: 10.1016/j.arth.2020.01.013. [DOI] [PubMed] [Google Scholar]
- 8.Struijk-Mulder M.C., Ettema H.B., Verheyen C.C., Büller H.R. Comparing consensus guidelines on thromboprophylaxis in orthopedic surgery. J Thromb Haemostasis. 2010;8:678–683. doi: 10.1111/j.1538-7836.2009.03728.x. [DOI] [PubMed] [Google Scholar]
- 9.Falck-Ytter Y., Francis C.W., Johanson N.A. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e278S–e325S. doi: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson D.F., Walker C.K. A descriptive and historical review of bibliometrics with applications to medical sciences. Pharmacotherapy. 2015;35:551–559. doi: 10.1002/phar.1586. [DOI] [PubMed] [Google Scholar]
- 11.Ahmad S.S., Albers C.E., Büchler L. The hundred most cited publications in orthopaedic hip research - a bibliometric analysis. Hip Int. 2016;26:199–208. doi: 10.5301/hipint.5000322. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad S.S., Evangelopoulos D.S., Abbasian M. The hundred most-cited publications in orthopaedic knee research. J Bone Joint Surg Am. 2014;96 doi: 10.2106/JBJS.N.00029. [DOI] [PubMed] [Google Scholar]
- 13.Hohmann E., Glatt V., Tetsworth K. Orthopaedic academic activity in the United States: bibliometric analysis of publications by city and state. Journal of the American academy of orthopaedic surgeons. Global research & reviews. 2018;2(7):e027. doi: 10.5435/JAAOSGlobal-D-18-00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang Y., Hu R., Zhu G. Top 100 cited articles on infection in orthopaedics: a bibliometric analysis. Medicine (Baltim) 2019;98 doi: 10.1097/MD.0000000000014067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Interval C. 2009. Oxford Centre for Evidence-Based Medicine: Levels of Evidence. [Google Scholar]
- 16.Geerts W.H., Bergqvist D., Pineo G.F. Prevention of venous thromboembolism: American College of chest Physicians evidence-based clinical practice guidelines. Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. 8th Edition. [DOI] [PubMed] [Google Scholar]
- 17.Collins R., Scrimgeour A., Yusuf S., Peto R. Reduction in fatal pulmonary embolism and venous thrombosis by perioperative administration of subcutaneous heparin. Overview of results of randomized trials in general, orthopedic, and urologic surgery. N Engl J Med. 1988;318:1162–1173. doi: 10.1056/NEJM198805053181805. [DOI] [PubMed] [Google Scholar]
- 18.Johanson N.A., Lachiewicz P.F., Lieberman J.R. American academy of orthopaedic surgeons clinical practice guideline on. Prevention of symptomatic pulmonary embolism in patients undergoing total hip or knee arthroplasty. J Bone Joint Surg Am. 2009;91:1756–1757. doi: 10.2106/JBJS.I.00511. [DOI] [PubMed] [Google Scholar]
- 19.Anderson D.R., O’Brien B.J., Levine M.N. Efficacy and cost of low-molecular-weight heparin compared with standard heparin for the prevention of deep vein thrombosis after total hip arthroplasty. Ann Intern Med. 1993;119:1105–1112. doi: 10.7326/0003-4819-119-11-199312010-00008. [DOI] [PubMed] [Google Scholar]
- 20.Morris G.K. Prevention of venous thromboembolism. A survey of methods used by orthopaedic and general surgeons. Lancet. 1980;2:572–574. doi: 10.1016/s0140-6736(80)92002-4. [DOI] [PubMed] [Google Scholar]
- 21.Oster G., Tuden R.L., Colditz G.A. A cost-effectiveness analysis of prophylaxis against deep-vein thrombosis in major orthopedic surgery. J Am Med Assoc. 1987;257:203–208. [PubMed] [Google Scholar]
- 22.Salzman E.W., Harris W.H. Prevention of venous thromboembolism in orthopaedic patients. J Bone Joint Surg Am. 1976;58:903–913. [PubMed] [Google Scholar]
- 23.Eriksson B.I., Borris L.C., Friedman R.J. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358:2765–2775. doi: 10.1056/NEJMoa0800374. [DOI] [PubMed] [Google Scholar]
- 24.Edelsberg J., Ollendorf D., Oster G. Venous thromboembolism following major orthopedic surgery: review of epidemiology and economics. Am J Health Syst Pharm. 2001;58(Suppl 2):S4–S13. doi: 10.1093/ajhp/58.suppl_2.S4. [DOI] [PubMed] [Google Scholar]
- 25.Eriksson B.I., Kakkar A.K., Turpie A.G.G. Oral rivaroxaban for the prevention of symptomatic venous thromboembolism after elective hip and knee replacement. J Bone Joint Surg Br. 2009;91:636–644. doi: 10.1302/0301-620X.91B5.21691. [DOI] [PubMed] [Google Scholar]
- 26.Fisher W.D., Eriksson B.I., Bauer K.A. Rivaroxaban for thromboprophylaxis after orthopaedic surgery: pooled analysis of two studies. Thromb Haemostasis. 2007;97:931–937. [PubMed] [Google Scholar]
- 27.Freyburger G., Macouillard G., Labrouche S., Sztark F. Coagulation parameters in patients receiving dabigatran etexilate or rivaroxaban: two observational studies in patients undergoing total hip or total knee replacement. Thromb Res. 2011;127:457–465. doi: 10.1016/j.thromres.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 28.Gómez-Outes A., Terleira-Fernández A.I., Suárez-Gea M.L., Vargas-Castrillón E. Dabigatran, rivaroxaban, or apixaban versus enoxaparin for thromboprophylaxis after total hip or knee replacement: systematic review, meta-analysis, and indirect treatment comparisons. BMJ. 2012;344 doi: 10.1136/bmj.e3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hull R.D., Yusen R.D., Bergqvist D. State-of-the-art review: assessing the safety profiles of new anticoagulants for major orthopedic surgery thromboprophylaxis. Clin Appl Thromb Hemost. 2009;15:377–388. doi: 10.1177/1076029609338712. [DOI] [PubMed] [Google Scholar]
- 30.Turpie A.G.G., Haas S., Kreutz R. A non-interventional comparison of rivaroxaban with standard of care for thromboprophylaxis after major orthopaedic surgery in 17,701 patients with propensity score adjustment. Thromb Haemostasis. 2014;111:94–102. doi: 10.1160/TH13-08-0666. [DOI] [PubMed] [Google Scholar]
- 31.Wolowacz S.E., Roskell N.S., Plumb J.M. Efficacy and safety of dabigatran etexilate for the prevention of venous thromboembolism following total hip or knee arthroplasty. A meta-analysis. Thromb Haemostasis. 2009;101:77–85. [PubMed] [Google Scholar]
- 32.Geerts W.H., Code K.I., Jay R.M. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331:1601–1606. doi: 10.1056/NEJM199412153312401. [DOI] [PubMed] [Google Scholar]
- 33.Friedman R. RD heparin compared with warfarin for prevention OF venous thromboembolic disease following total HIP or knee arthroplasty. Journal of Bone and Joint Surgery - American. 1994;76A:1174–1185. doi: 10.2106/00004623-199408000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Imperiale T.F., Speroff T. A meta-analysis of methods to prevent venous thromboembolism following total hip replacement. J Am Med Assoc. 1994;271:1780–1785. [PubMed] [Google Scholar]
- 35.Jørgensen L.N., Wille-Jørgensen P., Hauch O. Prophylaxis of postoperative thromboembolism with low molecular weight heparins. Br J Surg. 1993;80:689–704. doi: 10.1002/bjs.1800800607. [DOI] [PubMed] [Google Scholar]
- 36.Leizorovicz A., Haugh M.C., Chapuis F.R. Low molecular weight heparin in prevention of perioperative thrombosis. BMJ. 1992;305:913–920. doi: 10.1136/bmj.305.6859.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nurmohamed M.T., Rosendaal F.R., Büller H.R. Low-molecular-weight heparin versus standard heparin in general and orthopaedic surgery: a meta-analysis. Lancet. 1992;340:152–156. doi: 10.1016/0140-6736(92)93223-a. [DOI] [PubMed] [Google Scholar]
- 38.Simonneau G., Charbonnier B., Decousus H. Subcutaneous low-molecular-weight heparin compared with continuous intravenous unfractionated heparin in the treatment of proximal deep vein thrombosis. Arch Intern Med. 1993;153:1541–1546. [PubMed] [Google Scholar]
- 39.Leyvraz P.F., Bachmann F., Hoek J. Prevention of deep vein thrombosis after hip replacement: randomised comparison between unfractionated heparin and low molecular weight heparin. BMJ. 1991;303:543–548. doi: 10.1136/bmj.303.6802.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stratton M.A., Anderson F.A., Bussey H.I. Prevention of venous thromboembolism: adherence to the 1995 American College of Chest Physicians consensus guidelines for surgical patients. Arch Intern Med. 2000;160:334–340. doi: 10.1001/archinte.160.3.334. [DOI] [PubMed] [Google Scholar]
- 41.Dahl O.E., Andreassen G., Aspelin T. Prolonged thromboprophylaxis following hip replacement surgery—results of a double-blind, prospective, randomised, placebo-controlled study with dalteparin (Fragmin) Thromb Haemostasis. 1997;77:26–31. [PubMed] [Google Scholar]
- 42.Bergqvist D., Benoni G., Björgell O. Low-molecular-weight heparin (enoxaparin) as prophylaxis against venous thromboembolism after total hip replacement. N Engl J Med. 1996;335:696–700. doi: 10.1056/NEJM199609053351002. [DOI] [PubMed] [Google Scholar]
- 43.Warkentin T.E., Cook R.J., Marder V.J. Anti-platelet factor 4/heparin antibodies in orthopedic surgery patients receiving antithrombotic prophylaxis with fondaparinux or enoxaparin. Blood. 2005;106:3791–3796. doi: 10.1182/blood-2005-05-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Colwell CW, Kwong LM, Turpie AGG, Davidson BL (2006) Flexibility in administration of fondaparinux for prevention of symptomatic venous thromboembolism in orthopaedic surgery. J Arthroplasty 21:36–45. 10.1016/j.arth.2005.05.023. [DOI] [PubMed]
- 45.Eriksson BI, Lassen MR, PENTasaccharide in HIp-FRActure Surgery Plus Investigators (2003) Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery: a multicenter, randomized, placebo-controlled, double-blind study. Arch Intern Med 163:1337–1342. 10.1001/archinte.163.11.1337. [DOI] [PubMed]
- 46.Gordois A., Posnett J., Borris L. The cost-effectiveness of fondaparinux compared with enoxaparin as prophylaxis against thromboembolism following major orthopedic surgery. J Thromb Haemostasis. 2003;1:2167–2174. doi: 10.1046/j.1538-7836.2003.00396.x. [DOI] [PubMed] [Google Scholar]
- 47.Singelyn F.J., Verheyen C.C.P.M., Piovella F. The safety and efficacy of extended thromboprophylaxis with fondaparinux after major orthopedic surgery of the lower limb with or without a neuraxial or deep peripheral nerve catheter: the EXPERT Study. Anesth Analg. 2007;105:1540–1547. doi: 10.1213/01.ane.0000287677.95626.60. table of contents. [DOI] [PubMed] [Google Scholar]
- 48.Turpie A., Bauer K., Eriksson B. Efficacy and safety of fondaparinux in major orthopedic surgery according to the timing of its first administration. Thromb Haemostasis. 2003;90:364–366. [PubMed] [Google Scholar]
- 49.Turpie A.G.G., Bauer K.A., Eriksson B.I., Lassen M.R. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162:1833–1840. doi: 10.1001/archinte.162.16.1833. [DOI] [PubMed] [Google Scholar]
- 50.Turpie A.G.G., Bauer K.A., Eriksson B.I., Lassen M.R. Superiority of fondaparinux over enoxaparin in preventing venous thromboembolism in major orthopedic surgery using different efficacy end points. Chest. 2004;126:501–508. doi: 10.1378/chest.126.2.501. [DOI] [PubMed] [Google Scholar]
- 51.Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295–1302. [PubMed] [Google Scholar]
- 52.Mont M.A., Jacobs J.J., Boggio L.N. Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg. 2011;19:768–776. doi: 10.5435/00124635-201112000-00007. [DOI] [PubMed] [Google Scholar]
- 53.Eikelboom J.W., Karthikeyan G., Fagel N., Hirsh J. American Association of Orthopedic Surgeons and American College of Chest Physicians guidelines for venous thromboembolism prevention in hip and knee arthroplasty differ: what are the implications for clinicians and patients? Chest. 2009;135:513–520. doi: 10.1378/chest.08-2655. [DOI] [PubMed] [Google Scholar]
- 54.Raskob G.E., Hirsh J. Controversies in timing of the first dose of anticoagulant prophylaxis against venous thromboembolism after major orthopedic surgery. Chest. 2003;124:379S–385S. doi: 10.1378/chest.124.6_suppl.379s. [DOI] [PubMed] [Google Scholar]
- 55.Stewart D.W., Freshour J.E. Aspirin for the prophylaxis of venous thromboembolic events in orthopedic surgery patients: a comparison of the AAOS and ACCP guidelines with review of the evidence. Ann Pharmacother. 2013;47:63–74. doi: 10.1345/aph.1R331. [DOI] [PubMed] [Google Scholar]
- 56.Anderson D.R., Dunbar M.J., Bohm E.R. Aspirin versus low-molecular-weight heparin for extended venous thromboembolism prophylaxis after total hip arthroplasty: a randomized trial. Ann Intern Med. 2013;158:800–806. doi: 10.7326/0003-4819-158-11-201306040-00004. [DOI] [PubMed] [Google Scholar]
- 57.Drescher F.S., Sirovich B.E., Lee A. Aspirin versus anticoagulation for prevention of venous thromboembolism major lower extremity orthopedic surgery: a systematic review and meta-analysis. J Hosp Med. 2014;9:579–585. doi: 10.1002/jhm.2224. [DOI] [PubMed] [Google Scholar]
- 58.Investigators Botticelli, Committe Writing, Buller H. Efficacy and safety of the oral direct factor Xa inhibitor apixaban for symptomatic deep vein thrombosis. The Botticelli DVT dose-ranging study. J Thromb Haemostasis. 2008;6:1313–1318. doi: 10.1111/j.1538-7836.2008.03054.x. [DOI] [PubMed] [Google Scholar]
- 59.Eriksson B.I., Dahl O.E., Rosencher N. Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE-MODEL randomized trial. J Thromb Haemostasis. 2007;5:2178–2185. doi: 10.1111/j.1538-7836.2007.02748.x. [DOI] [PubMed] [Google Scholar]
- 60.Mueck W., Eriksson B.I., Bauer K.A. Population pharmacokinetics and pharmacodynamics of rivaroxaban—an oral, direct factor Xa inhibitor—in patients undergoing major orthopaedic surgery. Clin Pharmacokinet. 2008;47:203–216. doi: 10.2165/00003088-200847030-00006. [DOI] [PubMed] [Google Scholar]
- 61.Turpie A.G.G., Fisher W.D., Bauer K.A. Bay 59-7939: an oral, direct factor Xa inhibitor for the prevention of venous thromboembolism in patients after total knee replacement. A phase II dose-ranging study. J Thromb Haemostasis. 2005;3:2479–2486. doi: 10.1111/j.1538-7836.2005.01602.x. [DOI] [PubMed] [Google Scholar]
- 62.Eriksson B.I., Agnelli G., Cohen A.T. The direct thrombin inhibitor melagatran followed by oral ximelagatran compared with enoxaparin for the prevention of venous thromboembolism after total hip or knee replacement: the EXPRESS study. J Thromb Haemostasis. 2003;1:2490–2496. doi: 10.1111/j.1538-7836.2003.00494.x. [DOI] [PubMed] [Google Scholar]
- 63.Eriksson B.I., Agnelli G., Cohen A.T. Direct thrombin inhibitor melagatran followed by oral ximelagatran in comparison with enoxaparin for prevention of venous thromboembolism after total hip or knee replacement. Thromb Haemostasis. 2003;89:288–296. [PubMed] [Google Scholar]
- 64.Eriksson B.I., Arfwidsson A.-C., Frison L. A dose-ranging study of the oral direct thrombin inhibitor, ximelagatran, and its subcutaneous form, melagatran, compared with dalteparin in the prophylaxis of thromboembolism after hip or knee replacement: METHRO I. MElagatran for THRombin inhibition in Orthopaedic surgery. Thromb Haemostasis. 2002;87:231–237. [PubMed] [Google Scholar]
- 65.Eriksson B.I., Dahl O.E., Büller H.R. A new oral direct thrombin inhibitor, dabigatran etexilate, compared with enoxaparin for prevention of thromboembolic events following total hip or knee replacement: the BISTRO II randomized trial. J Thromb Haemostasis. 2005;3:103–111. doi: 10.1111/j.1538-7836.2004.01100.x. [DOI] [PubMed] [Google Scholar]
- 66.Eriksson B.I., Ekman S., Kalebo P. Prevention of deep-vein thrombosis after total hip replacement: direct thrombin inhibition with recombinant hirudin, CGP 39393. Lancet. 1996;347:635–639. doi: 10.1016/s0140-6736(96)91200-3. [DOI] [PubMed] [Google Scholar]
- 67.Eriksson B.I., Quinlan D.J. Oral anticoagulants in development: focus on thromboprophylaxis in patients undergoing orthopaedic surgery. Drugs. 2006;66:1411–1429. doi: 10.2165/00003495-200666110-00001. [DOI] [PubMed] [Google Scholar]