Abstract
Diabetic foot ulcer treatment is a challenge for the healthcare world. Widespread infection and the presence of critical ischemia (especially with end-stage renal disease) can lead to major amputation rather than amenable to conservative treatment. Surgical strategies of the diabetic foot have been changing over the past 10 years and are now focused on reconstructive treatment and limb salvage. These goals were achieved, thanks to an evolution of distal revascularization techniques and a distinct approach, which integrates various methods focused on limb salvage. Podoplastic techniques of the diabetic foot are focused on infection clearance, the surgical treatment of corrective deformities, soft tissue coverage and limb ischemia correction along with the management of diabetes and the comorbidities that compromise tissue repair processes. The reconstructive techniques used in diabetic foot treatment owe their effectiveness in part to the results of technological improvements such as the circular external fixator as a tool for stabilization and surgical site protection. In the last decade, many studies have shown that circular external fixation should be considered as the most useful method to protect the reconstructive surgical site in limb salvage of the diabetic foot. The objective of this review is to highlight the role of surgical offloading using circular external fixation as an adjunct to the podoplastic diabetic foot reconstruction procedures.
Keywords: Diabetic foot surgery, Podoplastic surgery, Limb salvage, Osteomyelitis, Diabetic foot ulcer
1. Introduction
The diabetic foot with its clinical indications (ulcers, soft tissue and bone infections, deformities, and biomechanical factors) associated with or without chronic critical ischemia are a challenge for the healthcare community. Modern diagnostic and therapeutic advances have made it possible to increase limb salvage rates, reserving major amputation to an ever-smaller number of patients.1, 2, 3, 4, 5
The diabetic foot surgeon should integrate and combine their own knowledge as well as the modern orthopedic and plastic surgery techniques. The emerging specialty called orthoplastic (podoplastic) surgery, as described by L. Scott Levin is well suited for diabetic foot cases after sorting through the assessment and management of the vascular situation.6 Peripheral vascular disease reduces and directs the reconstruction options and sometimes limits potential reconstructive alternatives. Even in cases with efficient revascularization, it is necessary to understand which is the best conservative treatment option. Neuropathy affecting diabetic patients involves a reduction in sensitivity or complete numbness which causes - among other things - reduced compliance with offloading indications in the post-operative period.
2. Principles of the podoplastic approach of the diabetic foot
In the past 10 years, there has been a real revolution in diabetic foot surgical procedures in areas of soft tissue reconstruction. This includes lower extremity plastic surgery techniques, fasciocutaneous rotation flaps as well as advancements in muscle flaps are often combined with the treatment of osteomyelitis or deformity correction. The holistic approach to a complete surgical treatment of diabetic foot takes into consideration not only the treatment of bone and soft tissues, but also the offloading of the reconstructed parts.7,8
The main objectives of podoplastic surgery applied to the diabetic foot take into consideration the following:
-
•
Structural bone deformities linked to peripheral neuropathy that create instability and hyper-pressure points that subsequently develop into ulcers. Surgical treatment of bone deformities may be necessary if it is not possible to control the risk of ulcer development with a conservative approach.
-
•
Skin lesions related to underlying bone deformities can progress to deep tissues causing infection resulting in abscess formation, septic arthritis and/or osteomyelitis.
-
•
Bone infection is often associated with deformity and surgical planning can include the simultaneous or staged correction of the deformity, removal of foci of bone infection and simultaneously achieving soft tissue coverage.
The quality of skin around the ulcer and surgical site are of critical importance for predictable healing. It is subjected to various factors such as the arterial and/or venous vascular status, the sensory-motor neuropathy state, as well as the possible presence of edema.
In general, the podoplastic approach for diabetic foot treatment involves a ladder approach beginning with simplest surgical procedures (tendon releases and simple exostectomy) and then moving up to more complex fusions and arthrodesis and microsurgical flap surgery.
2.1. Tenotomy
Digital flexor tenotomy is effective as a decompression treatment of dorsal and acral toe ulcerations. The Achilles tendon delivers a strong deforming thrust in the sagittal plane with a significant increase in plantar pressure on the forefoot and midfoot. This pressure carries a high risk of developing ulcers, especially in Charcot’s osteoarthropathy cases. Furthermore, valgus and varus deformities are the cause of a high ulcer risk in the medial and lateral portions of midfoot amputations, respectively. A release of the tendons responsible for the deformities may mitigate this predicament.9
2.2. Exostectomy
Charcot midfoot plantar bone prominence is a common indication for exostectomy. Resection of plantar bony protrusions of a chronic ulcer lesion helps to reduce a source of extreme pressure. After exostectomy, primary closure of the surgical site should be the surgeon’s key objective. This approach allows for healing time reduction and secondarily, a reduction in healthcare costs. However, if this is not possible, it can be managed as follows. The wound can be left open to heal by secondary intention, particularly if is small and there is any concern on ongoing infection. Larger wound coverage techniques include dermal substitutes or split skin graft, local flaps (advancement or rotation) and local muscle transposition or rotation flaps.
2.3. Bone deformity corrections
In the event of failure or non-applicability of the simplest surgical approaches (i.e., simple exostectomy), one moves up the ladder to more complex procedures such as arthrodesis/fusion both at the midfoot and hindfoot or ankle level. The choice of fixation options (internal or external) is linked to the location of the, the presence or absence of bone infection, the quality of the bone, the associated comorbidities and, ultimately, the surgeon’s experience.
2.4. Advanced wound healing techniques
In case of major soft tissue Defects, adjuvant therapies such as growth factors and negative pressure wound therapy (NPWT) associated with or without antiseptic agents should be considered to accelerate the healing process followed by lesion coverage with skin grafting requires. In recent years it has been proven that a viable neo-dermis can be formed on top of non-suitable tissue, such as bone, by applying a three-dimensional collagen scaffold or similar bioengineered tissue product.10, 11, 12, 13 In this case, it is critical to immobilize the foot and ankle until the reconstruction site is completely healed.
3. Non-surgical offloading to assist with diabetic foot and ankle ulcer healing
One of the most crucial issues in determining the surgical outcome in the diabetic foot is post-operative offloading. Historically, the most common offloading methods for patient weight bearing after diabetic foot reconstructive surgery were a fiberglass total contact cast or surgical shoes, walkers, wheelchair, and/or crutches.14,15 The indications for their use depend on local factors (surgical site location, type of procedure, vascular conditions, and the presence of comorbidities). Total contact casts (TCC) had been considered the gold standard offloading measure following such procedures for decades. However, patients suffering from these conditions are often older and suffer from other comorbidities. This means they often have poor compliance leading to failure of treatment. In addition to this, TCC is contraindicated in neuro-ischemic diabetic foot. Moreover, these patients are often in need of soft tissue reconstruction procedures such as flaps. In these cases, cast usage may result in pressure damage to the healing soft tissues. Furthermore, an incorrect TCC construct does not allow for suitable immobilization and, potentially, can be a source of further injuries and infection.16, 17, 18 Finally, joint instability, infected ulcer lesions, edema, and peripheral vascular disease are also considered contraindication of the use of a cast. The surgeon should create a protective environment around the reconstruction site.19, 20, 21
A complication related to a failure to adequately protect the reconstruction involves not only longer hospitalization time and increased healthcare costs, but also a high risk of amputation.
4. Surgical offloading technique for diabetic foot surgical sites
Historically circular external fixation played a major role in the treatment of open fractures and osteomyelitis. In these clinical applications, this device makes it possible to very frequently obtain a conservative treatment of traumatized osteoarticular structures which in the past required a major amputation. The circular fixator maintains the bone structure alignment through a rigid external frame, although large bone excision procedures are often required for osteomyelitis. Like internal fixation, circular external fixation can achieve optimal stabilization. However, unlike internal fixation, circular external fixation is not contraindicated in the presence of active infection. It has also been shown that the Ilizarov technique (Fig. 1) allows for healing in a shorter time, allowing for earlier weight-bearing. The first application of circular external fixation techniques in the diabetic foot were focused on the treatment of Charcot neuroarthropathy (CN). CN patients have poor bone quality and localized osteoporosis. Poor bone healing response in patients with diabetic neuropathy does not allow for normal bone regeneration and has been shown to have a decreased internal fixation pullout strength21
Fig. 1.
Circular external fixator frame.
4.1. Indications
The indications for the surgical treatment of CN are deformities that cannot be managed with conservative techniques, severe ankle instability, ulcer lesions localized in areas of deformity and hyper-pressure, and infectious progression with involvement of bone structures. Surgical offloading can be considered if the CN deformity has associated infection and soft tissue loss. The objectives of surgical offloading are a reduced hospital stay, reduced antibiotic therapy, and reduced complications (dehiscence) of the surgical site as well as achieving a plantigrade and stable foot. External fixation techniques also make it possible to avoid the complications of strict immobilization, such as heel decubitus and contracture that leads to equinus foot deformity. The general contraindications for the use of external fixation are also valid in surgical offloading. Lack of compliance, blindness or neurological diseases, severe peripheral arterial ischemia, morbid obesity, social or psychiatric problems are absolute contraindications to the use of external fixation.
4.2. Infection surgery
The infection component with or without bone involvement is the first goal of salvage surgery, by performing aggressive surgical debridement, and only subsequently should the correction of the deformities be considered through procedures of increasing difficulty such as decompressive exostectomies, osteotomies and arthrodesis.22, 23, 24, 25, 26, 27, 28, 29, 30
4.3. Stabilization
Once the correction of the deformities has been obtained, temporary stabilization with pins can be achieved. The circular frame is applied in optimal deformity correction and after performing the plastic surgical procedure. Stabilization of the deformity with the fixation is optimal and Latt et al. showed that the stability and compression obtained through circular external fixation is almost double compared to the use of screws.31 Circular external fixators can also achieve multiplanar corrections (distraction, compression, angulation, stabilization and translation).32, 33, 34, 35, 36 The soft tissue reconstruction is also protected by the frame, and this occurs both through joint immobilization (usually the ankle), which prevents tension of the tissues undergoing reconstruction and the use of multi-planar circular fixators that allow complete offloading of the plantar surface and the hindfoot. The first description of the use of circular external fixation techniques as an adjunct offloading device in reconstructive podoplastic surgery dates to 2003.37 In 2007 Bibbo et al. emphasized the efficacy of this method in the offloading of a plantar medial artery (PMA) flap to cover a chronic lesion of the hindfoot after debridement of an osteomyelitis of the heel.38 Subsequently, the use of surgical offloading with a circular external fixator has been suggested in surgical treatment of podoplastic surgery in the plantar site where the protection of the surgical site reduces, if not eliminates the risk of trauma to the soft tissue closure, and therefore, dehiscence. In addition, circular external fixation acts as a deformity correction device by stabilising the decompressive ostectomies, osteotomies, and fusions.39, 40, 41 (Fig. 2) Movement and tissue tension in joints undergoing podoplastic or reconstructive surgery often lead to wound dehiscence or relapse. The option of a circular external fixator allows for on the one hand, immobilization of the surgical site and on the other, an excellent access for post-operative observation and dressing. The protection occurs both through joint immobilization (usually the ankle) which prevents tension of the tissues undergoing reconstruction and the use of multi-planar circular fixators that allow complete offloading of the plantar surface and the hindfoot.
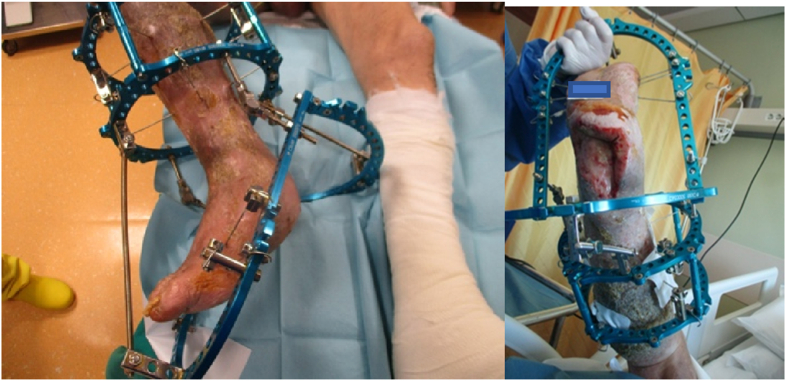
Fig. 2.
Optimal offloading of a surgical site.
4.4. Frame removal
The fixator can be removed as soon as the lesion has healed. Premature loading of the reconstructed site carries a high risk of re-ulceration. In the case of a plantar surgery, it is recommended to keep the frame on for at least 6 weeks.
4.5. Outcomes
Many published works in the last 10 years have shown a significant success rate in the use of circular external fixation for protection post podoplastic surgery in the lower limb.20,32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48 (Fig. 3). Clemens et al. report on the use of a multiplanar circular external fixator in 12 patients with healing/clinical failure after an average period of 285 days of conservative treatment with offloading measures. The overall limb salvage rate was 83% and the mean time to healing was 128 days after the fixator application. The reconstructive procedures performed were: 1 delayed primary closure, 5 split-thickness skin grafts, 4 local or pedicle flaps, and 2 free flaps. During the post-operative follow-up, there were 6 complications (50%) (4 pin site infections) and 2 rescue treatment failures, which required a major amputation (13%).45 Dalla Paola et al. reported, in a prospective study, the results using a circular external fixator (Fig. 4) designed for offloading of hindfoot lesions complicated by osteomyelitis, in a cohort of 18 diabetic patients in their unit. Revascularization procedures were performed where necessary, as well as subtotal calcanectomy, application of dermal substitute and final coverage procedures with autologous split-thickness skin graft. At a mean follow-up of 212 days, full recovery was achieved in 18 patients (100%). The average time between surgery and recovery was 69 days. No major amputation was performed during the follow-up period.20
Fig. 3.
Plantar fascio-cutaneous flap and dermal substitute for donor site coverage.
Fig. 4.
Circular external fixator developed for hindfoot reconstruction.
5. Technical considerations for surgical offloading
The advantages of using circular external fixation for podoplastic surgery of the diabetic foot are: osteo-articular stabilization, the ability to monitor soft tissue condition and the option of performing advanced wound closure techniques. Circular external fixation can be applied in situations where other traditional methods are contraindicated or insufficient, especially when protection of reconstructed soft tissue is required. The construct permits soft tissue management in a strain-protected environment.43,49
5.1. Surgical planning
An offloading circular external fixation is a temporary, non-weightbearing device. Applying a circular external fixator is a skillful surgical procedure that requires a good understanding of lower limb anatomy for the correct positioning of the pins. It is essential not to compromise the skin and the vascularity of the flap. The surgical technique for positioning and assembling the circular external fixator differs depending on the anatomical location of the surgical site, the type of tissue loss and the presence or absence of osteomyelitis. The application of circular external fixation techniques pertaining to podoplastic surgery must consider in the planning phase, the relationship between the K-Wire or pin positioning relative to the site as well as the type of reconstruction. If the positioning of the fixator poses any barrier to free access of the reconstruction site, the circular external fixator must be positioned after surgery.
5.2. Hindfoot correction
Hindfoot lesions associated with osteomyelitis are a difficult and challenging treatment site. As is often the case with pressure lesions, deep tissue involvement is extensive and requires extensive excisions. Offloading of the hindfoot is particularly critical and difficult to achieve with standard unloading techniques and the use of external fixation allows this to be achieved easily.20 Any hindfoot bone involvement makes it necessary to perform a partial or total calcanectomy (Fig. 5). The debridement site can be closed initially, or it can be kept open for secondary closure or for plastic reconstructive procedure. In any case, the positioning of a circular external fixator can achieve the following objectives:
-
•
maintain an equinus ankle position which reduces the tissue tension of the hindfoot
-
•
offloading of the hindfoot permitting protection of the surgical site
-
•
maintain access to the surgical site for reconstructive procedures and local treatment
Fig. 5.
Open partial calcanectomy.
The frame is composed of a foot plate (parallel to the sole of the foot) stabilized by 3 or 4, 1.8 mm K-Wires (on the forefoot and mid-tarsal line) and two-rings for the tibia. The foot plate and tibial rings are connected by 2–4 threaded rods. The equinus position is maintained by inclining the foot plate with a central rotation wire through the ankle axis (tip of medial malleolus to the tip of lateral malleolus). Plantar flexion is gradually reduced over the course of follow-up. The large posterior opening allows for local treatment of the wound site and dressing changes. With this device it is possible to eliminate a postoperative cast and the related potential complications.20 External fixation techniques also make it possible to avoid the complications of strict immobilization, such as heel decubitus and contracture that leads to equinus foot deformity.
5.3. Midfoot correction
For midfoot lesions, the principle of a complete excision of non-viable and infected tissue associated with the debridement of the bone structures involved in the infection progression is always valid. The deformity is treated with a resection of the bony prominences which also corrects the mechanical overload. The treatment of midfoot plantar lesions, involving bone structures relating to Charcot osteoarthropathy, often requires a multistage approach that primarily focuses on the debridement of the soft tissue involved in the infection. The surgical site is kept open and cleansed with NPWT and instillation with antiseptic agents.50,51 Once the infection is controlled, the curative/corrective surgical step associated with a stabilization using a circular external fixator is planned. The stabilization of the foot plate takes place by positioning of 2–3 K-Wires in the forefoot and hindfoot while keeping the midfoot free from metal hardware. Any medial or lateral compression is obtained by placing olive K-Wires.
5.4. Duration of frame stabilization
The treatment time with an external fixator depends on whether the fixation objective is to obtain offloading or if it is used as a fusion/stabilization tool. In the first case, the circular external fixator following a reconstructive procedure can permit a favorable healing environment by reducing pressure on the compartments, offloading the flap, and immobilization of the adjacent joints and the frame removal is usually possible following healing of the surgical site, usually 4–8 weeks. In the case of a Charcot osteoarthropathy fusion complicated by infection and osteomyelitis, the external fixator use varies from 3 to 6 months. A hybrid construct in a triangle or box configuration are useful to obtain total offloading. The rods are placed in a triangular position with the base perpendicular to the axis of the leg.16 (Fig. 6).
Fig. 6.
Box/Hybrid constructs.
5.5. Variations in the frame construct
Circular frames achieve a complete offloading position using a foot plate (one or multiple) and tibial rings. Variations of the construct can be performed for different locations of the ulcer/surgical site (forefoot, midfoot, hindfoot). Skin grafts positioned on the forefoot, midfoot or rearfoot may not take if the graft site is not immobilized. The same outcome can affect local random flaps on the plantar portion of the foot if the active range of motion is not controlled at the metatarsal-phalangeal joints or ankle joint. Immobilization optimizes complex flap viability by minimizing intra-compartment pressure in the reconstructed limb.43,52,53 The circular external fixator cancels direct pressure on the foot compartments and stabilizes the muscle groups adjacent to the flap.
5.6. Complications
Potential complications of external fixation use in diabetic foot patients include hardware infection (soft tissues and/or bone), fractures and deep vein thrombosis. Most complications are minor and related to local skin infection. Optimal pin care and a reduced external fixation frame period could reduce or avoid these complications. A fiberglass cast should be used after the removal of the external fixator for a period of 4–6 weeks to prevent fractures.43,54,55
6. Conclusion
Conservative treatment of the diabetic foot is a challenge for healthcare providers. In the last decade, a surgical school of thought dedicated to the management of neuroischemic pathologies of the diabetic foot has evolved, with the introduction of podoplastic surgery. Podoplastic surgery combines plastic surgical wound closure techniques and circular external fixation techniques. Surgical offloading methods with the placement of circular external fixators have become an integral part of podoplastic surgery. These practices simultaneously permit total offloading of the surgical site, joint immobilization, observation of tissue viability and flaps, and wound care which would all be difficult to achieve using traditional methods.
References
- 1.Dalla Paola L., Faglia E. Treatment of diabetic foot ulcer: an overview. Strategies for clinical approach. Curr Diabetes Rev. 2006 Nov;2(4):431–447. doi: 10.2174/1573399810602040431. [DOI] [PubMed] [Google Scholar]
- 2.Uckay I., Aragon-Sanchez J., Daniel Lew, Lipsky B.A. Diabetic foot infection: what have we learned in the last 30 years? Int J Infect Dis. 2015 Nov;40:81–91. doi: 10.1016/j.ijid.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 3.Senneville E., Robineau O. Treatment options for diabetic foot osteomyelitis. Expet Opin Pharmacother. 2017 Jun;18(8):759–765. doi: 10.1080/14656566.2017.1316375. [DOI] [PubMed] [Google Scholar]
- 4.Blume P., Wu S. Updating the diabetic foot treatment algorithm: recommendations on treatment using advanced medicine and therapies. Wounds. 2018 Feb;30(2):29–35. Epub 2017 Oct 20. [PubMed] [Google Scholar]
- 5.Apelqvist J. Diagnostic and treatment of the diabetic foot. Endocrine. 2012 Jun;41(3):384–397. doi: 10.1007/s12020-012-9619-x. [DOI] [PubMed] [Google Scholar]
- 6.Levin L.S. The reconstructive ladder. An orthoplastic approach. Orthop Clin N Am. 1993 Jul;24(3):393–409. [PubMed] [Google Scholar]
- 7.Pehde C.E., Bennet J., Kingston M. Orthoplastic approach for surgical treatment of diabetic foot ulcer. Clin Podiatr Med Surg. 2020 Apr;37(2):215–230. doi: 10.1016/j.cpm.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Azoury S.C., Stranix J.T., Kovach S.J., Levin L.S. Principles of orthoplastic surgery for lower extremity reconstruction: why is this important? J Reconstr Microsurg. 2021 Jan;37(1):42–50. doi: 10.1055/s-0039-1695753. Epub 2019 Aug 27. PMID: 31454835. [DOI] [PubMed] [Google Scholar]
- 9.Liette M.D., Crisologo P.A., Johnson L.J., Henning J.A., Rodriguez-Collazo E.R., Masadeh S. A surgical approach to location-specific neuropathic foot ulcer. Clin Podiatr Med Surg. 2021 Jan;38(1):31–53. doi: 10.1016/j.cpm.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Alvaro Afonso F.J., Garcia Alvarez Y., Lazaro Martinez J.L., Kakagia D., Papanas N. Advances in dermoepidermal skin substitutes for diabetic foot ulcers. Curr Vasc Pharmacol. 2020;18(2):182–192. doi: 10.2174/1570161117666190408170144. [DOI] [PubMed] [Google Scholar]
- 11.Frykberg R.G., Marston W.A., Cardinal M. The incidence of lower-extremity amputation and bone resection in diabetic foot ulcer patients treated with a human fibroblast-derived dermal substitute. Adv Skin Wound Care. 2015 Jan;28(1):17–20. doi: 10.1097/01.ASW.0000456630.12766.e9. [DOI] [PubMed] [Google Scholar]
- 12.Clerici G., Caminiti M., Curci V., Quarantiello A., Faglia E. The use of a dermal substitute (integra) to preserve maximal foot length in a diabetic foot wound with bone and tendon exposure following urgent surgical debridement for an acute infection. Int J Low Extrem Wounds. 2009 Dec;8(4):209–212. doi: 10.1177/1534734609350553. [DOI] [PubMed] [Google Scholar]
- 13.Dalla Paola L., Cimaglia P., Carone A., Boscarino G., Scavone G. Use of integra dermal regeneration template for limb salvage in diabetic patients with no-option critical limb ischemia. Int J Low Extrem Wounds. 2020 Feb 14 doi: 10.1177/1534734620905741. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.De Oliveira A.L., Moore Z. Treatment of the diabetic foot by offloading: a systematic review. J Wound Care. 2015 Dec;24(12):562–570. doi: 10.12968/jowc.2015.24.12.560. 560. [DOI] [PubMed] [Google Scholar]
- 15.Bus S.A. The role of pressure offloading on diabetic foot ulcer healing and prevention of recurrence. Plast Reconstr Surg. 2016 Sep;138(3 suppl l) doi: 10.1097/PRS.0000000000002686. 179-S-87S) [DOI] [PubMed] [Google Scholar]
- 16.Castro-Aragon O.E., Rapley J.H., Trevino S.G. The use of kickstand modification for the prevention of heel decubitus ulcers in trauma patients with lower extremity external fixation. J Orthop Trauma. 2009;23(29):145–147. doi: 10.1097/BOT.0b013e318196bb6a. [DOI] [PubMed] [Google Scholar]
- 17.Wukich D.K., Motko J. Safety of total contact casting in high-risk patients with neuropathic foot ulcers. Foot Ankle Int. 2004;25(8):556–560. doi: 10.1177/107110070402500808. [DOI] [PubMed] [Google Scholar]
- 18.McHenry T., Simmons S., Alitz C. Forward surgical stabilization of penetrating lower extremity fractures: circular casting versus external fixation. Mil Med. 2001;166(9):791–795. [PubMed] [Google Scholar]
- 19.Buford G.A., Trzeciak M.A. A novel method for lower-extremity immobilization after free-flap reconstruction of posterior heel defects. Plast Reconstr Surg. 2003;111(2):821–824. doi: 10.1097/01.PRS.0000039398.59464.D4. [DOI] [PubMed] [Google Scholar]
- 20.Dalla Paola L., Carone A., Boscarino G., Scavone G., Vasilache L. Combination of open subtotal calcanectomy and stabilization with external fixation as limb salvage procedure in hindfoot infected diabetic foot ulcers. Int J Low Extrem Wounds. 2016 Dec;15(4):332–337. doi: 10.1177/1534734616667865. [DOI] [PubMed] [Google Scholar]
- 21.Grant W.P., Rubin L.G., Pupp G.R. Mechanical testing of seven fixation methods for generation of compression across a midtarsal osteotomy: a comparison of interna and external fixation devices. J Foot Ankle Surg. 2007;46:325–335. doi: 10.1053/j.jfas.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Saltzman C.L. Salvage of diffuse ankle osteomyelitis by single-stage resection and circumferential frame compression arthrodesis. Iowa Orthop J. 2005;25:47–52. [PMC free article] [PubMed] [Google Scholar]
- 23.Frykberg R.G., Sage R.A., Wukich D.K., Pinzur M.S., Schubert J.M. Charcot arthropathy. Foot Ankle Spec. 2012;5:262–271. doi: 10.1177/1938640012451234. [DOI] [PubMed] [Google Scholar]
- 24.Myerson M.S., Henderson M.R., Saxby T., Short K.W. Management of midfoot diabetic neuroarthropathy. Foot Ankle Int. 1994;15:233–241. doi: 10.1177/107110079401500502. [DOI] [PubMed] [Google Scholar]
- 25.Pinzur M.S., Sage R., Stuck R., Kaminsky S., Zmuda A. A treatment algorithm for neuropathic (Charcot) midfoot deformity. Foot Ankle. 1993;14:189–197. doi: 10.1177/107110079301400403. [DOI] [PubMed] [Google Scholar]
- 26.Pinzur M.S. Neutral ring fixation for high-risk non plantigrade Charcot midfoot deformity. Foot Ankle Int. 2007;28:961–966. doi: 10.3113/FAI.2007.0961. [DOI] [PubMed] [Google Scholar]
- 27.Dalla Paola L., Ceccacci T., Ninkovic S., Sorgentone S., Marinescu M.G. Limb salvage in Charcot foot and ankle osteomyelitis: combined use single stage/double stage of arthrodesis and external fixation. Foot Ankle Int. 2009;30:1065–1070. doi: 10.3113/FAI.2009.1065. [DOI] [PubMed] [Google Scholar]
- 28.Pinzur M.S., Gil J., Belmares J. Treatment of osteomyelitis in Charcot foot with single- stage resection of infection, correction of deformity and maintenance with ring fixation. Foot Ankle Int. 2012;33:1069–1074. doi: 10.3113/FAI.2012.1069. [DOI] [PubMed] [Google Scholar]
- 29.Dalla Paola L. Confronting a dramatic situation: the Charcot foot complicated by osteomyelitis. Int J Low Extrem Wounds. 2014 Dec;13(4):247–262. doi: 10.1177/1534734614545875. [DOI] [PubMed] [Google Scholar]
- 30.Frykberg R.G., Wukich D.K., Kavarthapu V., Zgonis T., Dalla Paola L. Surgery for the diabetic foot: a key component of care. Diabetes Metab Res Rev. 2020 Mar;36(suppl 1) doi: 10.1002/dmrr.3251. [DOI] [PubMed] [Google Scholar]
- 31.Latt L.D., Glisson R.R., Adams S.B., Jr. Biomechanical comparison of external fixation and compression screws for transverse tarsal joint arthrodesis. Foot Ankle Int. 2014;35:572–577. doi: 10.1177/1071100715589083. [DOI] [PubMed] [Google Scholar]
- 32.Cooper P.S. Application of external fixators for management of Charcot deformities of the foot and ankle. Semin Vasc Surg. 2002;7:207–254. doi: 10.1053/svas.2003.50007. [DOI] [PubMed] [Google Scholar]
- 33.Jolly G.P., Zgonis T., Polyzois V. External fixation in the management of Charcot neuroarthropathy. Clin Podiatr Med Surg. 2003;20:741–756. doi: 10.1016/S0891-8422(03)00071-5. [DOI] [PubMed] [Google Scholar]
- 34.Baravarian B., Van Gils C.C. Arthrodesis of the Charcot foot and ankle. Clin Podiatr Med Surg. 2004;21(2):271–289. doi: 10.1016/j.cpm.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Farber D.C., Juliano P.J., Cavanagh P.R. Single stage correction with external fixation of the ulcerated foot in individuals with Charcot neuroarthropathy. Foot Ankle Int. 2002;23:130–134. doi: 10.1177/107110070202300209. [DOI] [PubMed] [Google Scholar]
- 36.Roukis T.S., Zgonis T. The management of acute Charcot fracture-dislocation with the Taylor’s spatial external fixation system. Clin Podiatr Med Surg. 2006;23(2):467–483. doi: 10.1016/j.cpm.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 37.Buford G.A., Trzeciak M.A. A novel method for lower-extremity immobilization after free-flap reconstruction of posterior heel defects. Plast Reconstr Surg. 2003;111:821–824. doi: 10.1097/01.PRS.0000039398.59464.D4. [DOI] [PubMed] [Google Scholar]
- 38.Bibbo C., Stough J.D. Reduction calcaneoplasty and local muscle rotation flap as a salvage option for calcaneal osteomyelitis with soft tissue defect. J Foot Ankle Surg. 2012;51(3):375–378. doi: 10.1053/j.jfas.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 39.Oznur A. Management of large soft tissue defects in a diabetic patient. Foot Ankle Int. 2003;24(1):79–82. doi: 10.1177/107110070302400113. [DOI] [PubMed] [Google Scholar]
- 40.Oznur A., Tokgozoglu Closure of central defects of the forefoot with external fixation. J Foot Ankle Surg. 2004;43(1):56–59. doi: 10.1053/j.jfas.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 41.Roukis T.S. Zgonis T Skin grafting techniques for soft-tissue coverage of diabetic foot and ankle wounds. J Wound Care. 2005;14:173–176. doi: 10.12968/jowc.2005.14.4.26763. [DOI] [PubMed] [Google Scholar]
- 42.Armstrong D.G., Nguyen H.C., Lavery L.A. Offloading the diabetic foot wound: a randomized clinical trial. Diabetes Care. 2001;24(6):2153–2154. doi: 10.2337/diacare.24.6.1019. [DOI] [PubMed] [Google Scholar]
- 43.Sagebien C.A., Rodriguez E.D., Turen C.H. The soft tissue frame. Plast Reconstr Surg. 2007;119:2137–2140. doi: 10.1097/01.prs.0000260689.54364.c8. [DOI] [PubMed] [Google Scholar]
- 44.Buford G.A., Trzeciak M.A. A novel method for lower-extremity immobilization after free flap reconstruction of posterior heel defects. Plast Reconstr Surg. 2003;111:821–824. doi: 10.1097/01.PRS.0000039398.59464.D4. [DOI] [PubMed] [Google Scholar]
- 45.Clemens M.W., Parikh P., Hall M.M., Attinger C.E. External Fixator as an adjunct to wound healing. Foot Ankle Clin N Am. 2008;13:145–156. doi: 10.1016/j.fcl.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 46.Ramanujam C., Facarosi Z., Zgonis T. External fixation for surgical offloading of diabetic soft tissue reconstruction. Clin Podiatr Med Surg. 2011;28:211–216. doi: 10.1016/j.cpm.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 47.Lowenberg D.W., Sadeghi C., Brooks D. Use of circular external fixation to maintain foot position during free tissue transfer to the foot and ankle. Microsurgery. 2008;28:623–627. doi: 10.1002/micr.20577. [DOI] [PubMed] [Google Scholar]
- 48.Oznur A., Zgonis T. Closure of major diabetic foot wounds and defects with external fixation. Clin Podiatr Med Surg. 2007;24:519–528. doi: 10.1016/j.cpm.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 49.Klaue K. The role of external fixation in acute foot trauma. Foot Ankle Clin. 2004;9(3):583–594. doi: 10.1016/j.fcl.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 50.Kim P.J., Attinger C.E., Crist B.D. Negative Pressure wound Therapy with Instillation: review of evidence and recommendations. Wounds. 2015 Dec;27(12):S2–S19. [PubMed] [Google Scholar]
- 51.Dalla Paola L. Diabetic foot wounds: the value of negative pressure wound therapy with instillation. Int Wound J. 2013 Dec;10(Suppl 1):25–31. doi: 10.1111/iwj.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jerosch J. Intracompartmental pressure of the anterior tibial compartment as a function of body and joint position. Biomed Tech. 1989;34(9):202–206. doi: 10.1515/bmte.1989.34.9.202. [DOI] [PubMed] [Google Scholar]
- 53.Willy C., Gerngross H., Sterk J. Measurement of intracompartmental pressure with use of a new electronic transducer-tipped catheter system. J Bone Jt Surg Am Vol. 1999;81(29):158–168. doi: 10.2106/00004623-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Rogers L.C., Bevilacqua N.J., Frykberg R.G. Predictors of postoperative complications of Ilizarov external ring fixators in the foot and ankle. J Foot Ankle Surg. 2007;46(5):372–375. doi: 10.1053/j.jfas.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 55.Wukich D.K., Belczyk R.J., Burns P.R. Complications encountered with circular ring fixation in persons with diabetes mellitus. Foot Ankle Int. 2008;29(10):994–1000. doi: 10.3113/FAI.2008.0994. [DOI] [PubMed] [Google Scholar]