Abstract
Objective
To evaluate biomechanical behavior of different internal fixation methods for the treatment of Pauwels Type III femoral neck fractures.
Methods
Three internal fixators were developed to treat Pauwels Type III femoral neck fracture using finite elements: dynamic hip screw (DHS); DHS combined with anti-rotation screw; three cannulated screws in an inverted triangular configuration (ASNIS). Under the same conditions, vertical fracture displacement, and maximum and minimum principal, and Von Mises stresses were evaluated.
Results
The vertical displacements evaluated were: 5.43 mm, 5.33 mm and 6.22 mm, rotational displacements values were 1.1 mm, 0.4 mm and 1.3 mm; maximum principle stress values obtained for the upper region of the femoral neck were 3.26 hPa, 2.77 hPa, and 4.5 hPa, minimum principal stress values obtained for the inferior region of the femoral neck were −1.97 hPa, −1.8 hPa and t −3.15 hPa; Von Mises peak stress values were 340.0 MPa, 315.5 MPa and 326.1 Mpa, for DHS, DHS with anti-rotation device, and ASNIS, respectively. Conclusion: The DHS combined with anti-rotation screw yielded better results in terms of rotational and vertical displacements, traction and compression distributions on fractures, and Von Mises stress, demonstrating mechanical superiority for Pauwels Type III fracture.
Keywords: Femoral neck fracture, Internal fixation, Finite element analysis, Biomechanics
1. Introduction
More than 2 million cases of hip fractures are reported annually.1 Estimates point to around 30% increase by 2025.2 Of this total, 50% are femoral neck fractures, which have the highest morbidity and lethality rates.3 With high prevalence in young adults, they are usually the result of high-energy traumas.4 The treatment of choice, in this age group, is focused on anatomical reduction and internal fixation, with preservation of the blood supply of the femoral head.5 Fracture displacement degree and the quality of the reduction are determining factors in the progression to osteonecrosis in patients aged fifteen to fifty years.6 Based on the degree of verticality, Pauwels classified the fractures into 3 categories.7 Pauwels Type III fractures (equal to or greater than 50°) are subjected to greater shearing forces, causing great challenges to fixation and postoperative8 wound healing, resulting in a greater degree of fracture instability.
Epidemiological studies show that up to 59% of these evolve with non-union of fractures, and the incidence of femoral head necrosis ranged from 11% to 86%.7 An important meta-analysis showed implant failures in about 10% of cases in young patients.9 The difficulty of reducing the fracture and positioning the screws correctly make surgery a challenge even for experienced surgeons.10,11 The repair must withstand shearing forces inherent in the vertical fracture line to the greatest extent possible.10 Thus, the search for effective internal fixations has become the focus of scientific research over the years.
Widely used at the clinical level, the dynamic hip screw (DHS), added or not to the anti-rotation screw, and three cannulated screws in an inverted triangular configuration (ASNIS) are the main osteosynthesis techniques of choice.8,11, 12, 13, 14, 15 A recent systematic review studied the biomechanical capacity of several internal fixators (DHS, locking plate, proximal femoral rod and multiple cannulated screws), demonstrating that, to date, there is no conclusion on the best method to be used, with advantages and disadvantages for all osteosyntheses. DHS systems, with or without anti-rotation screw, show better results in biomechanical trials, with greater gains in stability, but require a larger incision, generating large dissection of soft tissues.14,16,17
Therefore, despite the importance of the subject, the literature is still controversial as regards the best type of synthesis. In addition, to the best of our knowledge, the use of evaluation techniques such as the finite element method14 (FEM), already proven effective for this purpose, are so far quite scarce. FEM is a widely used, reliable and practical method for analyzing mechanical structures in engineering, being adopted by researchers from other areas (such as orthopedics and traumatology), making it an important and powerful tool for biomechanical tests on osteosynthesis, offering information detailed without the need for destructible physical mechanical tests.18,19 For that reason, the objective of this study was to use FEM to determine the biomechanical stability of three forms of fixation of Pauwels Type III femoral neck fractures (DHS, DHS with anti-rotation device and ASNIS), describing the fracture deviation in the vertical and rotational directions, maximum and minimum principal, and Von Mises in the syntheses used.
2. Materials and methods
2.1. Finite element analysis
To compare the mechanical behavior of the fixation methods, their FEM models were created.
In the FEM study, the materials used are divided into ductile and non-ductile, according to their characteristics. Metallic materials, such as syntheses, belong to the ductile group and their stress is measured by the von Mises equivalent stress test. However, von Mises stress does not apply for bone analysis, since these belong to the non-ductile materials group, and the use of maximum and minimum principal stresses is appropriate for its evaluation.
2.2. Biocad preparation
The preparation of the three-dimensional (3D) virtual models of each system (bone and synthesis) was performed using the Rhinoceros™ 6 software (Robert McNeel & Associates, United States) and the FEM analysis was performed in the SimLab™ software (HyperWorks, United States) using the Optistruct solver, running on a computer powered by Intel Xeon CPU E−3-1240 V3 3.40 GHz, with 32 GB RAM and 64-bit Windows 7 operating system.
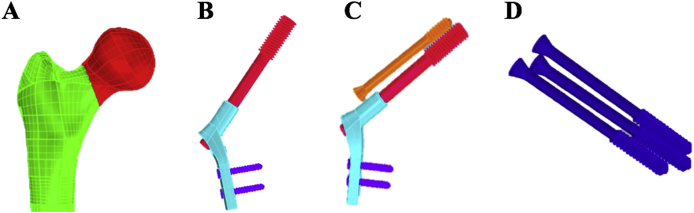
Tomographic images of the bone were obtained from the synthetic bone models and titanium syntheses, and archived in the communication protocol that includes DICOM (Digital Imaging and Communications in Medicine) files. The tomograph used was the Emotion (16 channels, Siemens™, Munich, Germany) at a 512 x 512 resolution and cuts 1.0 mm apart. The (DICOM) file was imported into the InVesalius™ software for three-dimensional reconstruction of the anatomical structure. Based on a set of two-dimensional images obtained through computerized tomography equipment, the program allows the generation of three-dimensional virtual models of the regions of interest of the system imported into it (Fig. 1). After three-dimensional reconstruction of DICOM images, the program allows the generation of 3D files in STereo Lithography (STL) format, although sometimes it is also referred to as "Standard Triangle Language" (STL).
Fig. 1.
Construction of Pauwels type III femoral neck fracture model (A), internal sliding hip fixation (DHS) (B), combined with the anti-rotation screw (C) and three cannulated screws in an inverted triangular configuration (ASNIS) (D).
2.3. Converting files
All the slices were imported into the InVesalius™ program to obtain the STL file with the images that would be used in the process of obtaining the 3D solid, thus providing the multiplanar generation option, which shows the view of sagittal, coronal, and axial images and the volume. From the volume, the 3D surface is created and you have the option of selecting the regions of interest using masks and/or filters, which hides or displays the file according to the algorithm in question, thereby generating the 3D surface.
2.4. Simulation
FEM was used for the stability simulations of the different assemblies. First, the files were imported into the Simlab™ program, with an identification of each part of the digital models. After checking the meshes of each part, care should be taken to always maintain the size of the element, so that there are no problems of contacts between the different parts of the image in the simulations. The element adopted for mesh formation is tetrahedral. The amount of nodes was also defined.
2.4.1. Properties of materials
To perform the simulations it was necessary to know and define the properties of the materials of each part of the digital models, namely: cortical bone, trabecular bone and titanium alloy. The properties of the materials used for the simulations are: Elastic Modulus and Poisson’s ratio (Table 1).
Table 1.
Properties of materials (cortical bone, trabecular bone and syntheses).
| Material | Properties of materials |
|
|---|---|---|
| Elastic Modulus (Mpa) | Poisson’s ratio (v) | |
| Cortical bone | 17 | 0.26 |
| Trabecular bone | 1.7 | 0.26 |
| Syntheses | 193 | 0.33 |
2.4.2. Boundary conditions
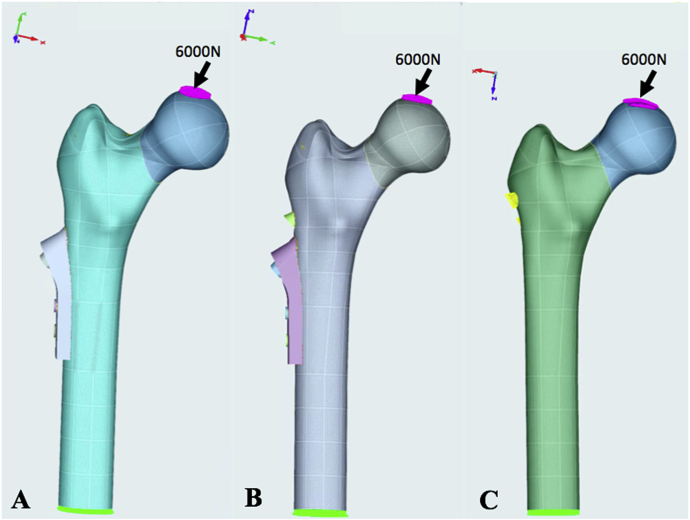
To define boundary conditions, regions were selected for applying the load, initially 2040 N along the Z-axis and −5040 along the Y-axis, this force being a vector decomposition of 6000 N with the virtual bone model at an angle of 20° of adduction. No load was applied to the X-axis. Subsequently, regions of movement restriction (fixed) were established, marked in all directions of X, Y and Z axes of both displacements and rotation. These restrictions are to ensure that the system has a perfect alignment without displacement and/or rotation (Fig. 2).
Fig. 2.
Load application regions and internal fixations evaluated. A- Dynamic Hip Screw Internal Fixation (DHS). B- DHS combined with the anti-rotation screw. C- Three cannulated screws in an inverted triangular configuration (ASNIS).
After checking the meshes of each part, care should be taken to always maintain the size of the element, so that there are no problems of contacts between the different parts (femoral syntheses) in the simulations. The element adopted for mesh formation was tetrahedral.
2.5. Evaluation criteria
The analysis using finite element method evaluated the displacement of the models and the rotation of the fractured fragment (femoral neck). For the analysis of stresses in non-ductile materials, i.e. bone and fracture, we used the maximum principal (traction) and minimum principal (compression) variables. For ductile and metallic materials, the stress analyzed was Von Mises equivalent stress. The vertical and rotational displacements of the fracture were also evaluated.
3. Results
3.1. Description of fracture vertical and rotational displacements with the different fixation models
The vertical displacements evaluated were 5.43 mm, 5.33 mm and 6.22 mm for the fixation models using DHS, DHS with anti-rotation screw and ASNIS, respectively. The rotational displacements evaluated were 1.1 mm, 0.4 mm and 1.3 mm, for the fixation models with DHS, DHS with anti-rotation screw and ASNIS, respectively.
It was demonstrated that the use of the DHS device associated with the anti-rotation screw reduced the vertical displacement by about 15% when compared to the ASNIS device, and the rotational displacement by more than 50% when compared to DHS and ASNIS in the Pauwels Type III femoral neck fracture.
3.2. Maximum (traction) and minimum (compression) principals distribution on fractures with the different fixation models
The maximum values for the upper region of the femoral neck adjacent to the fracture were 3.26 hPa, 2.77 hPa and 4.5 hPa for fixation models with DHS, DHS with anti-rotation device and ASNIS, respectively. The values obtained for minimum stress in the lower region of the femoral neck adjacent to the fracture were −1.97 hPa, −1.8 hPa and −3.15 hPa for fixation models with DHS, DHS with anti-rotation device and ASNIS, respectively.
It is possible to show that the DHS device associated with the anti-rotation screw yielded better results in traction and compression distribution on fractures, with a reduction of approximately 15% and 38% in traction and attenuation of approximately 9% and 43% in compression, when compared to the isolated DHS device and ASNIS, respectively.
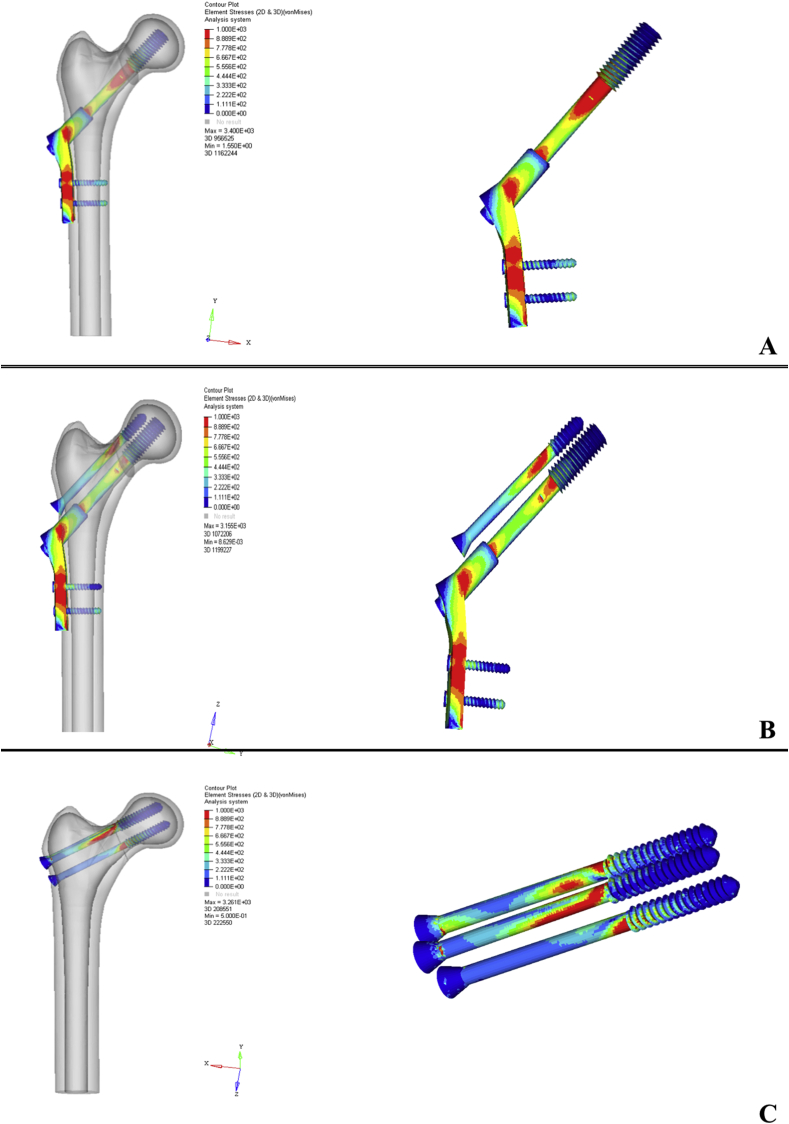
3.3. Von Mises peak stress distribution in the different fixation models
The maximum Von Mises peak stress values were 340.0 MPa, 315.5 MPa and 326.1 Mpa for fixation models with DHS, DHS with anti-rotation device and ASNIS, respectively. The reduction observed in DHS with an anti-rotation device was achieved by distributing the load on the anti-rotation screw, which indicates that it is an important factor in the distribution of the force applied to this type of fracture. In addition, the area of the highest stress on all synthesis was on the fracture line. This site represents a greater concern in the fracture of the synthesis (Fig. 3).
Fig. 3.
Von Mises peak stress distribution of the different internal fixation models: the maximum Von Mises stress of the 3 internal fixation models (A- Dynamic Hip Screw Internal Fixation (DHS). B- DHS combined with the anti-rotation screw. C- Three cannulated screws in an inverted triangular configuration (ASNIS) were 340.0 MPa, 315.5 MPa and 326.1 MPa.
4. Discussion
Femoral neck fractures have a high incidence of complications, with only 40–60% of patients regaining their pre-fracture mobility level. With an increased shearing force and a high incidence of varus displacement of the proximal fragment, Pauwels Type III fractures are the most complex. The surgical process must be very well planned, since fixation failures in young adults are associated with high morbidity, making it very difficult to solve.11 Duckworth et al.20 evidenced in their retrospective study with 122 patients, that 32% (39) evolved with non-union of the fractured focus and 11.4% (14) developed femoral head necrosis.
Based on these premises and the controversy still existing as to the ideal method of fixation for vertical fractures of the femoral neck, the need for studies with advanced technologies, focused on biomechanical analysis of internal fixations is imminent. Our study analyzed, through a computational model, the mechanical stability of DHS, DHS with anti-rotation screw and ASNIS fixators in Pauwels Type III femoral neck fractures. The results of this study show that the fixation technique with DHS combined with the anti-rotation screw, provided lower rotational and vertical displacements, traction and compression distributions on fractures and Von Mises peak stress, when compared to methods with isolated DHS and ASNIS.
The biomechanical behavior of Pauwels type III fractures should be taken into consideration when performing the internal fixation, as this repair must resist the shearing force inherent to the vertical fracture line to the greatest extent possible. Evidence in favor of the use of an anti-rotation screw combined with DHS device, with observed reduction of fracture displacement, increased stability and load ratio to failure, gained traction in the years 2000.16,21 Stoffel Samsami et al.,16, biomechanically compared DHS devices combined with the anti-rotation screw with three parallel cannulated screws, in 20 cadaveric femoral samples with an unstable fracture of the femoral neck at 70°. The results have shown significantly higher overall stability in the DHS device plus anti-rotation screw, with superior results in variables tested through mechanical tests, such as cycles to failure, femoral neck, and femoral leg shortening. Using experimental and computational analysis, Samsami et al.14 compared three fixation methods for femoral head fractures in young adults (DHS with anti-rotation screw, cannulated screws and proximal femoral locking plate) and obtained similar results to our study. The authors showed that the DHS combined with the anti-rotation screw offered the greatest resistance against shearing and rotation forces of the femoral head, keeping the proximal and distal segment closer together and firm during the healing process. Therefore, the authors conclude that the DHS device, combined with the anti-rotation screw, can provide greater stability and more positively influence fracture consolidation when compared to the other methodologies studied. In addition, the results observed through finite element analysis were similar to those of the experimental evaluation, showing that the computational models have great potential to predict the mechanical performance of bone implants.
Biomechanical results unfavorable to the treatment with cannulated screws in triangular configuration, as demonstrated in our study, have been previously evidenced. Liporaci et al.22 evaluated 76 patients with Pauwels Type III femoral neck fracture over 12 years. The researchers found that 32% of the individuals treated with cannulated screws had post-surgical complications such as osteonecrosis and non-union of the fracture, while the rate was minimized (14%) when the synthesis of choice was DHS.
Studies with the use of FEM for biomechanical evaluation of fractures and syntheses are a minority in the literature, albeit proven effective. Noda et al.13 demonstrated that FEM models provide a means to solve clinical problems, predicting the distribution of stresses in the structures of interest. The authors found that Pauwels Type III fractures have a high risk of displacement with the use of ASNIS-like synthesis. The main explanations relate to the lack of pressure perpendicular to the fracture line and presence of pressure at the parallel level, exerting a pulling force on the screw and predisposing the generation of a slip between the ends, allowing recurrent complications, such as the non-union of the fracture and varus deformity of the hip.23 These findings are reinforced by previous studies, where the use of three cannulated screws in an inverted triangular configuration did not generate the necessary mechanical stability to treat femoral neck fractures, showing a significantly lower capacity to withstand maximum loads than an L-shaped fixation set with three screws.15
Compared to the classical configuration of DHS and ASNIS, the DHS with anti-rotation screw, in the present study, was also superior in terms of the biomechanical variables evaluated. The novelty of this study is that FEM was used to compare various fixation methods, evaluating parameters too complex to be measured experimentally such as compression and traction distribution on fractures and Von Mises peak stress in the different fixation models. In terms of limitations, it is important to note that the effects of surrounding muscles and ligaments on fracture stability have not been taken into account. Besides that, we did not investigate important individual differences such as ethnicity, age and gender or possible effects of previous hip disorders, which could modify our findings.
5. Conclusion
The present FEM analysis showed that the DHS combined with anti-rotation screw yielded better results in terms of rotational and vertical displacements, traction and compression distributions on fractures, and Von Mises stress, demonstrating mechanical superiority when compared to the classical configuration of DHS and ASNIS for treatment of Pauwels Type III fracture.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- 1.Rapp K., Büchele G., Dreinhöfer K., Bücking B., Becker C., Benzinger P. Epidemiology of hip fractures: systematic literature review of German data and an overview of the international literature. Z Gerontol Geriatr. 2019;52:10–16. doi: 10.1007/s00391-018-1382-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gullberg B., Johnell O., Kanis J.A. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 3.Augat P., Bliven E., Hackl S. Biomechanics of femoral neck fractures and implications for fixation. J Orthop Trauma. 2019;33(Suppl 1):S27–s32. doi: 10.1097/BOT.0000000000001365. [DOI] [PubMed] [Google Scholar]
- 4.Shen M., Wang C., Chen H., Rui Y., Zhao S. An update on the Pauwels classification. J Orthop Surg Res. 2016;11 doi: 10.1186/s13018-016-0498-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parker M.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2009;91:490–491. United States. [PubMed] [Google Scholar]
- 6.Haidukewych G.J., Rothwell W.S., Jacofsky D.J., Torchia M.E., Berry D.J. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004;86(8):1711–1716. doi: 10.2106/00004623-200408000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Bartonicek J. Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma. 2001;15(5):358–360. doi: 10.1097/00005131-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Cha Y.H., Yoo J.I., Hwang S.Y. Biomechanical evaluation of internal fixation of Pauwels type III femoral neck fractures: a systematic review of various fixation methods. Clin Orthop Surg. 2019;11(1):1–14. doi: 10.4055/cios.2019.11.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slobogean G.P., Sprague S.A., Scott T., Bhandari M. Complications following young femoral neck fractures. Injury. 2015;46(3):484–491. doi: 10.1016/j.injury.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Panteli M., Rodham P., Giannoudis P.V. Biomechanical rationale for implant choices in femoral neck fracture fixation in the non-elderly. Injury. 2015;46(3):445–452. doi: 10.1016/j.injury.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 11.Giordano V., Alves D.D., Paes R.P. The role of the medial plate for Pauwels type III femoral neck fracture: a comparative mechanical study using two fixations with cannulated screws. J Exp Orthop. 2019;6(1):1–9. doi: 10.1186/s40634-019-0187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye Y., Hao J., Mauffrey C., Hammerberg E.M., Stahel P.F., Hak D.J. Optimizing stability in femoral neck fracture fixation. Orthopedics. 2015;38(10):625–630. doi: 10.3928/01477447-20151002-05. [DOI] [PubMed] [Google Scholar]
- 13.Noda M., Saegusa Y., Takahashi M., Tezuka D., Adachi K., Naoi K. Biomechanical study using the finite element method of internal fixation in Pauwels type III vertical femoral neck fractures. Arch Trauma Res. 2015;4(3) doi: 10.5812/atr.23167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Samsami S., Saberi S., Sadighi S., Rouhi G. Comparison of three fixation methods for femoral neck fracture in young adults: experimental and numerical investigations. J Med Biol Eng. 2015;35(5):566–579. doi: 10.1007/s40846-015-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giordano V., Paes R.P., Alves D.D. Stability of L-shaped and inverted triangle fixation assemblies in treating Pauwels type II femoral neck fracture: a comparative mechanical study. Eur J Orthop Surg Traumatol. 2018;28(7):1359–1367. doi: 10.1007/s00590-018-2207-x. [DOI] [PubMed] [Google Scholar]
- 16.Stoffel K., Zderic I., Gras F. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131–137. doi: 10.1097/BOT.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 17.Freitas A., Torres G.M., Souza A.C., Maciel R.A., Souto D.R., Ferreira G.N. Analysis on the mechanical resistance of fixation of femoral neck fractures in synthetic bone, using the dynamic hip system and an anti-rotation screw. Rev Bras Ortop. 2014;49(6):586–592. doi: 10.1016/j.rboe.2014.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.JH K., JM M., HB S., CD M. Automated three-dimensional finite element modelling of bone: a new method. J Biomed Eng. 1990;12(5) doi: 10.1016/0141-5425(90)90022-f. [DOI] [PubMed] [Google Scholar]
- 19.Wieding J., Souffrant R., Fritsche A., Mittelmeier W., Bader R. Finite element analysis of osteosynthesis screw fixation in the bone stock: an appropriate method for automatic screw modelling. PLoS One. 2012;7(3):e33776. doi: 10.1371/journal.pone.0033776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duckworth A.D., Bennet S.J., Aderinto J., Keating J.F. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. 2011;93(6):811–816. doi: 10.1302/0301-620X.93B6.26432. [DOI] [PubMed] [Google Scholar]
- 21.Bonnaire F.A., Weber A.T. Analysis of fracture gap changes, dynamic and static stability of different osteosynthetic procedures in the femoral neck. Injury. 2002;33(Suppl 3):C24–C32. doi: 10.1016/s0020-1383(02)00328-5. [DOI] [PubMed] [Google Scholar]
- 22.Liporace F., Gaines R., Collinge C., Haidukewych G.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90(8):1654–1659. doi: 10.2106/JBJS.G.01353. [DOI] [PubMed] [Google Scholar]
- 23.Wang G., Tang Y., Wu X., Yang H. Finite element analysis of a new plate for Pauwels type III femoral neck fractures. J Int Med Res. 2020;48(2) doi: 10.1177/0300060520903669. 300060520903669. [DOI] [PMC free article] [PubMed] [Google Scholar]