Abstract
Imaging forms a crucial component in reducing mortality of polytraumatized patients by aiding appropriate diagnosis and guiding the emergency and definitive treatment. With the exponential expansion in the radiological armamentarium and introduction of protocols like Extended focused assessment with sonography for trauma (EFAST) and Whole body Computed tomography (WBCT), the role of imaging has considerably increased. Emergency imaging protocols should be done for rapid diagnosis of life-threatening injuries allowing simultaneous evaluation and resuscitation. Subsequent comprehensive imaging is essential to diagnose the often clinically missed injuries to reduce the overall morbidity. Imaging protocols must adapt to the patient’s clinical scenario, which can be dynamically changing. Each trauma team should devise clear guidelines, protocols, and algorithms suitable for their center depending on the local availability of types of equipment and expertise. Radiologists must efficiently communicate and adopt patient-centered approach to ensure early appropriate care to these severely injured patients. Future research should involve multicentre studies to formulate the most appropriate imaging protocol in polytrauma to increase diagnostic accuracy and thereby reduce patient mortality.
Keywords: Polytrauma, Imaging, Emergency, Whole body computed tomography, Focused assessment with sonography for trauma
1. Introduction
Despite recent medical advances, the mortality rate following polytrauma varies between 10% and 20% and can be as high as 63% when associated with brain injuries and up to 35% with pelvic fractures.1 Survival and functional recovery in early phase is dependent on promptness in recognizing and managing the anatomical and physiological alterations, for which radiology plays an important role. Accurate assessment of injury using a time-oriented comprehensive imaging is essential to guide decision-making and orient the clinicians to address injuries with priority. The armamentarium available to the radiologists has expanded considerably, and numerous protocols have been proposed. Each centre must evolve locally tailored trauma protocols, for optimal use of available imaging modalities and establishing consistent reporting procedures. This article outlines the basic imaging principles in polytrauma and briefs the most recent developments in imaging techniques and equipments.
2. Location and infrastructure
Imaging is an essential part of primary survey and hence mobile radiographs, C-arms, and ultrasound, should be available on-site. Computed tomography (CT) scan is an important part of imaging but has a major risk of increased mortality during delays in transfer of patients to radiology department situated far away, earning the CT scan the nick name of the ‘doughnut of death’.2 Moving the CT scanner into the Emergency department (ED) reduces the time between patient arrival to CT imaging by 13% and a 4–7% reduction in mortality.3,4 The Royal College of Radiologists (RCR) recommends all major trauma centers (MTCs) to have 24/7 access to a dedicated CT machine either within or adjacent to the ED with strict SOPs for rapid and safe transfer of patients.5
Currently, there is no available evidence suggesting the use of Magnetic resonance imaging (MRI) in the setting of acute trauma as its role is limited to evaluate spinal cord injuries and pancreatic injuries.5,6
In all major trauma centers interventional radiology (IR) services should be available within 30–60min of demand.5 Delaying IR in hemodynamically unstable patients increases the mortality rate by 47% for every 1 h delay especially in the presence of splenic and pelvic injuries.7
All the imaging modalities should be integrated with Picture archiving and communication system (PACS) to allow images to be transmitted, stored, retrieved, and displayed in different locations of a hospital or health systems without delay. PACS also greatly helps in tele-radiology services if on-site radiologists are not available.2
3. Diagnostic imaging work flow
Advanced Trauma Life Support (ATLS) guidelines recommends a rapid primary clinical survey of the ABCDEs (Airway, Breathing, Circulation, Disability, Exposure) and a trauma series of plain radiographs (lateral c-spine, supine chest radiograph, and pelvis).8 The trauma series radiographs should be followed by a focused assessment with sonography in trauma (FAST). A secondary imaging survey involves a rapid head to toe examination, including CT and angiography. Most commonly followed recommendation of imaging workflow in polytrauma patients depending on hemodynamic stability are in Table 2 and Table 3.5,6,8
Table 2.
Bedside and Whole Body CT Protocols in Stable, Unstable Blunt and penetrating Trauma:6.
| Hemodynamic status of the patient | Beside imaging | WBCT protocol and modifications | Additional comments |
|---|---|---|---|
|
|
|
|
Unstable responding to resuscitation
|
|
|
|
|
Unstable transiently responding to resuscitation In some cases, initially unstable patients will respond to resuscitation only briefly or transiently (transient responders) indicating that more physiologically active injuries are present. |
Imaging protocol same as above. | The key diagnostic information sought in this instance is the presence or absence of:
|
The use of WBCT in transient responders is more controversial, but still valuable and feasible if ongoing physiologic support can be maintained during imaging, and scanning can be completed extremely rapidly in a safe setting in direct proximity to the emergency department. |
| Stable Penetrating trauma | Radiographs are indicated based on severity of injury. | WBCT is not recommended. Focused CT imaging of affected body region is recommended in stable patients with penetrating trauma. Depending on location of injury, intravenous, oral and/or rectal contrast is recommended. |
|
| Unstable penetrating trauma | Chest Radiograph: Assess for pneumothorax E-FAST ultrasound: Assess for hemoperitoneum/hemopericardium/pneumothorax Additional radiographs to identify penetrating objects and their trajectories (head, neck, etc.) |
CT is contraindicated in hemodynamically unstable patients with penetrating trauma. |
Table 3.
Criteria for CT head:6.
| If none of these conditions are met, consider not ordering CT scan of the head |
|---|
|
|
|
|
|
|
|
|
| CT scan of Facial Bones: |
| Head CT can be extended to include all of mandible and skull base in order to obtain CT of both head and facial bones in one acquisition if there is clinical evidence of facial bone injury.Additional axial, coronal and sagittal series using bone algorithm are produced. |
| CTA of Circle of Willis (COW): |
| Clinical setting of headache with intracranial bleed (SAH) and minor trauma raising suspicion of ruptured aneurysm. |
4. Plain radiography
Plain radiographs continue to have major role in primary survey of the polytrauma patients and used extensively to rule out chest, cervical spine and pelvic injuries.
Chest X-ray (CXR) has specificity of 100% in detecting pneumothorax and other chest injuries, with highest sensitivity to detect clavicle fracture.9,10 However 76–80% of pneumothoraces can be occult on supine chest radiography and it can also miss 11% of aortic injuries with low sensitivity for diagnosing pneumomediastinum.10, 11, 12 Hence accurate evaluation in severe blunt thoracic injury warrants CT scan to rule out significant injuries. However, in low impact injury and when CXR is normal, CT thorax is not advised since reported yield of additional significant finding ranges from only 1.4–5.5%.13
Plain X-rays have a similar limitation in cervical spine injuries, wherein pooled injury sensitivity for plain films is 52% in comparison to 98% with CT.14 ATLS, RCR and British Columbia (BC) guidelines suggest CT scan to clear the cervical spine injury whenever an injury is suspected, in a high impact injury and unconscious patient.5,6,8
Pelvic fractures are frequent in high-energy polytrauma. Plain pelvic Xrays are included in ATLS protocol and play important role in hemodynamically unstable patients where further imaging is often not considered. Simple clinical screening tests are adequate to rule out the possibility of pelvic fractures,15 However, when it is suspected in a hemodynamically stable patient, CT scan is considered instead of pelvic radiographs as it adds little value to patient management.16
5. Ultrasound (FAST and EFAST)
Focused assessment with sonography in trauma (FAST) is a rapid assessment tool widely used by radiologists, trauma physicians, surgeons and certain paramedics to detect hemoperitoneum, hemopericardium and hemothorax.
Diagnostic peritoneal lavage (DPL) is replaced by FAST in many centers since FAST is less invasive and is more accurate. Study by Al-Salamah et al. showed the sensitivity for, DPL vs FAST scan to be 98% and 96% and overall accuracy rate of 92% and 95% respectively. DPL has false positive results with retroperitoneal injuries and can miss small bowel injury and pancreatic injury.17
FAST soley depends on detection of hemoperitoneum as an indicator for abdominal injury. However, 34% of the patients with significant intra-abdominal injuries confirmed by CT scan had no hemoperitoneum and 17% of these patients needed surgery or intervention.18 For the detection of solid organ injuries, reported sensitivity varies from 38% to 95.4%. The sensitivity for diagnosis of gastrointestinal injury is only 38.5% but increases to 85.2% when FAST is repeated in 12–24 h.19 In a hemodynamically stable patient with negative FAST, the CT scan is recommended to rule out a major injury or to decide on early discharge of the patient from the ED to the observation ward. (Fig. 1).
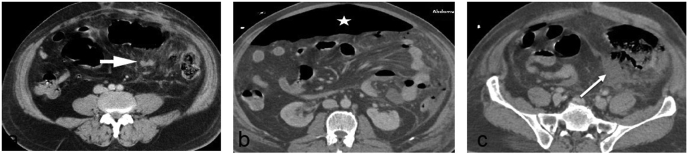
Fig. 1.
Negative clinical examination and FAST in high mechanism injury: 40 year old with major extremity injury following high mechanism blunt trauma was diagnosed fast negative in ED and had no obvious abdominal complaints at presentation. WBCT (Figure a) at the same time showed small mesenteric hematoma (arrow head) in left iliac fossa surrounded by large area of mesenteric fat stranding. FAST was negative since there was no hemoperitoneum as confirmed by WBCT. Initially this was not addressed since patient had no abdominal complaints nor guarding on clinical examination. Two days later patient complained of abdominal pain and developed distension as well as guarding on clinical examination. Repeat CT scan (Figure b, c) shows large pneumoperitoneum (star) and increase in mesenteric collection with air pockets (arrow) suggesting ruptured bowel due to mesenteric injury.
A hemodynamically unstable patient with FAST positive scan goes for laparotomy, bypassing the CT scan to avoid further delay. FAST makes a good triage tool in setting of mass casualty to identify the unstable patients with hemoperitoneum who can directly taken to laparotomy. CT is avoided in hemodynamically unstable patient when hemoperitoneum detected by FAST.
Extended FAST (E-FAST) additionally explores pericardial and pleural spaces. In recent meta-analysis E-FAST showed pooled sensitivities and specificities for the detection of pneumothorax (69% and 99% respectively), pericardial effusion (91% and 94% respectively).20 E-FAST is now an integral part of ATLS protocol in most Level-I trauma care centers.
6. Computer tomography
Having a CT scan in the ED, with adequate staff, and maintaining it 24/7 has a huge financial burden, which will reflect on the final cost incurred.2 However, significant number of occult injuries can often be missed in major trauma which are accurately detected by the CT scan especially in the absence of external injury.20 Major trauma is therefore an indication for CT scan. RCR recommended the criteria of an Injury Severity Score (ISS) > 15 as the definition of major trauma but this has the drawback in being retrospective and often needing a CT for accurate scoring in the absence of external injuries. Using a combination of physiological, anatomical criteria and mechanism of injury to categorize the injury as a major trauma and to indicate the CT scan seems a more reasonable approach. (Table 1).2
Table 1.
Criteria for WBCT in the setting of polytrauma:2.
| Criteria A: High Risk Mechanism of Injurya | Criteria B: Anatomicala | Criteria C: Physiologicala |
|---|---|---|
|
|
|
Any one of the above.
Two known approaches for radiological workup of the polytrauma patients are the standard imaging protocol, where specific body regions are imaged based on clinical judgment and the early WBCT, in which head to proximal femur is scanned in one pass bypassing radiographs and USG. First described in Germany in 1997, WBCT is increasingly employed in the past two decades due to better diagnostic accuracy and reduction in time for acquisition, missed injuries, and mortality rates.22
There is contradictory data regarding the relative value of WBCT and selective CT (SCT) protocols in literature. Proponents of WBCT cite saving of time, as every 3 min delay in definitive treatment of blunt trauma increases mortality by 1%.21 SCT involves scanning specific body regions based on clinical judgement and prior radiographic assessment. Hence if multiple regions are to be scanned, it takes longer duration due to selective planning and scanning, whereas WBCT takes only 12 min due to one pass scanning protocol. WBCT also had fewer missed injuries as it was able to identify 4% injuries not suspected clinically, of which 75% were severe and changed the treatment decisions in 18.9%.23 WBCT is hence advocated in patients with head injuries where a robust clinical examination is not feasible and in hemodynamically stable patients with major trauma. However, the disadvantages of WBCT include increased radiation and higher costs incurred. Effective dose for a single WBCT ranged from 14 to 22.7 mSv (13 mSv more than SCT), pointing to the risk of radiation exposure.24 Certain practices can aid in reducing the radiation dose. Avoidance of WBCT in those who do not reach the clinical threshold for high impact injury, the use of dual-energy CT or multidetector CT scans, a combination of lower dose and special reconstruction methods can allow dose reduction. Additionally, raising patient’s both arms above the level of shoulders in the interval between the head scan and the thorax scan will reduce the effective dose to the body by up to 45%, and a reduction by 19% by raising one arm.25,26
The first randomized trial, REACT 2 (2016), was undertaken in 540 patients documenting injury mechanism, vital parameters and clinical suspicion of potential injuries and found that the in-hospital mortality rates in WBCT and SCT protocols were similar.27 Current evidence suggests reserving WBCT for those with severe trauma (ISS>15),5 where survival advantages overshadow radiation burden and cost. Used judiciously, it also plays a major role in early reassurance for the trauma team, allowing the patient to be discharged from the emergency department and monitored with reassurance.
7. Role of MRI in major trauma patients
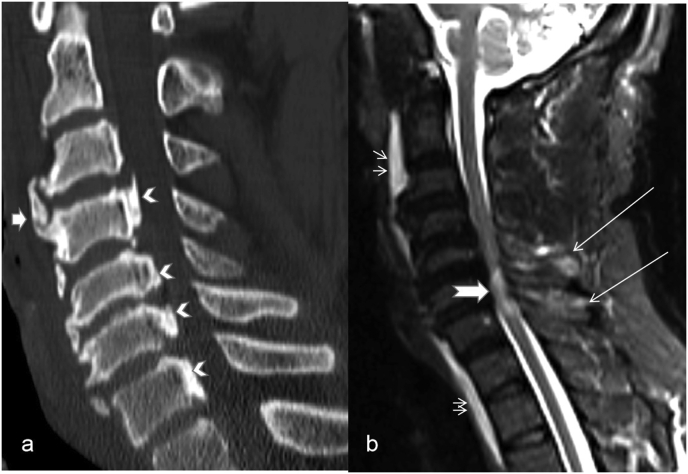
Currently, there is no available evidence suggesting the use of MRI in an emergency setting and it is only used as a second-line problem-solving tool.2 MRI, has special value mainly in suspected spinal cord injuries (Fig. 2) and for the diagnosis of pancreatic duct injuries where Magnetic-resonance cholangiopancreatography (MRCP) has 100% accuracy. It is also a suitable tool for follow up imaging of blunt trauma as there is no radiation hazard, especially in the young and pregnant patients.
Fig. 2.
MRI in spine injury: Patient presented with impaired neurology and suspected cervical level injury. CT scan (Figure a) showed degenerative changes in form of interrupted ossified posterior longitudinal ligament at multiple levels (chevron), marginal bridging osteophytes (arrow head) without any obvious fracture. MRI (Figure b) performed in view of impaired neurology showed multilevel cord contusion (notched arrow) and pre vertebral hematoma (double arrows) and interspinous ligament sprain (long arrows).
8. Vascular assessment
Although the incidence of vascular injuries is less, prompt identification is important to avoid death or amputation. Reported incidence of vascular injury is 5.9% following blunt polytrauma, of which extremity and thoracic injuries are common followed by abdominal injuries with least number affecting head and neck vessels. Majority of on table deaths were due to underlying vascular injuries, of which most common is abdominal vena caval injuries.28
Computed Tomography Angiography (CTA), owing to rapidness, non-invasive nature and high specificity is the popular imaging modality.7 Arterial phase images of WBCT with thin section MPR images are adequate to detect vascular injuries. Angiogram of extremities and head and neck can be covered in same setting when there is clinical suspicion of vascular injury avoiding delay in diagnosing limb saving findings.
Digital Subtraction Angiography (DSA), plays a major role in therapeutic rather than diagnosis. Currently, the accepted indication for DSA is the presence of active extravasation or pseudoaneurysm formation at CT.29
9. Image reporting
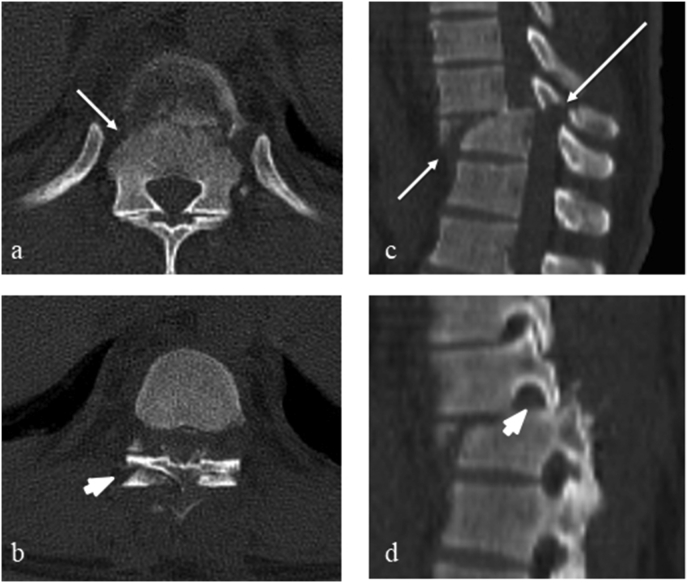
Reporting of WBCT in polytrauma setting is challenging due to pressure of accurate reporting on an emergency basis, repeated interruption from the trauma team and the fatigue of working out-of-hours. Multiplanar reconstruction (MPR) essential to detect spinal, diaphragmatic injuries, and vascular injuries requires additional time for post-processing with an added burden on radiologist for reviewing over >1500 images (Fig. 3).30 There are no studies to quote the exact incidence of reporting errors in the setting of polytrauma imaging although it is estimated that approximately 4% error rate are possible in typical clinical practice.31 Stephen et al., have described various reasons and types of radiological errors, which can be interpretive error, omission errors, errors related to attention and perception, cognitive bias, satisfaction of search.31 They also quoted external factors like lack of clinical history, fatigue related to workload and constant interruption by clinical team can contribute to reporting errors. The Royal College of Radiologists recommends breaking the WBCT report down into two structured parts, a primary and secondary survey, similar to the ATLS phases of resuscitation. The initial survey report is focussed on a few specific high-risk injuries, which are usually immediately apparent on a rapid review of the scan images, e.g., sizeable intracranial hemorrhage, large pneumothoraces. The secondary survey – a definitive consultant report should be provided within an hour, to rule out commonly overlooked “major” injuries (Table 4) (Fig. 4).32 However inspite of guidelines, consultant report within an hour of the CT scan may not be feasible in off working hours even in major trauma centers. Giannakopoulos et al. reported 8% of injuries could be occult even when interpreted by experienced radiologist, suggesting the need for tertiary survey and clinical input in case of discrepancy in radiological report.33
Fig. 3.
Multiplanar reconstruction in trauma patients: WBCT in axial images (a, b) showed thoracic translation injury (arrow) with bilateral facet disruption (arrowhead). Sagittal reconstruction at the same level readily shows the extent of translation (arrow) with fractures (long arrow) and facet disruption (arrowhead).
Table 4.
Commonly overlooked major injuries on initial WBCT reports.2
| Commonly overlooked major injuries on initial WBCT reports. |
|---|
|
|
|
|
|
|
|
|
|
|
Fig. 4.
Importance of secondary survey in emergency trauma reporting. WBCT in high mechanism injury was reported by night on call resident. Right pneumothorax (arrow), hemoperitoneum and features of shock, like collapse IVC (circle) were reported on primary survey. Secondary report by consultant an hour later, showed scapula fracture with large hematoma (thick arrow).
The report should follow a simple, rigid structure to aid the speed of reporting and communication of findings. The most favored reporting classification for abdominal visceral injury is the American Association for the Surgery of Trauma (AAST) Injury scoring scale which is followed in most of the world for reporting and as well as research.34 (Table 5).
Table 5.
Sample of ATLS organ injury scoring - Recent modified liver injury scoring:34.
| Grade I | Grade II | Grade III | Grade IV | Grade V |
|---|---|---|---|---|
|
|
|
|
|
A regular multidisciplinary team (MDT) meeting to discuss the challenging and interesting cases will be beneficial for educative purposes. Trauma MDT may also serve as tertiary survey and enable second opinions in the light of new clinical findings.
10. Special consideration in pediatric and pregnant patients
The concept of ‘one size fits all’ does not hold good for imaging in pediatric trauma patients and needs to be individualized for each child. Children differ in the pattern of injury and its management from adults; injuries regarded as life-threatening in the adult population (for example, liver and spleen trauma) can often be managed conservatively in children.
The emphasis is on careful, competent clinical evaluation and knowledge of injury patterns in children of various ages. Judicious use of plain radiographs and targeted use of CT with discussion with the senior radiologist is critical. Since there is no safe dose limit for radiation exposure in children, decisions regarding anatomical areas to be covered, and the choice of primary imaging between plain radiographs or CT must be made judiciously. Routine use of WBCT as in adults is not recommended for children. When CT is indicated, the ‘as low as reasonably achievable’ (ALARA) concept should be strictly followed using dose reduction software and advanced iterative reconstruction methods, which can reduce the radiation dose up to 40%. Details of imaging protocol for a particular anatomical location is best detailed in RCR guidelines.35
Imaging of pregnant polytrauma patients: Imaging protocols in a pregnancy setting is essentially the same as adult polytrauma. Early involvement of obstetricians to the trauma team is recommended and the WBCT protocol remains unchanged since the mother’s survival outweighs the radiation risk to the fetus. Intravenous contrast medium can be safely used in pregnancy.36
11. Role of interventional radiology (IR) in major trauma
Interventional radiologists play an important role in the management of polytrauma patients by their ability to identify and rapidly intervene in life threatening injuries. Following criteria are a must for effective utilization of IR in trauma setting: (1) a skilled IR who is available for consultation on urgent notice; (2) availability of high-quality digital subtraction angiographic equipment, preferably with digital road mapping and/or fade-fluoroscopic capabilities; (3) availability of skilled nursing and equipment needed for monitoring of critically ill patients; and (4) ability to ready these resources within 30–60 min.7
Solid organ injuries: Hemodynamically unstable patients with solid organ injuries require immediate surgery. Hemodynamically stable patients with solid organ injuries are triaged to non-operative management (NOM) with observation or Transarterial Embolisation (TAE). Currently, the accepted indication for angiography is the presence of active extravasation or pseudoaneurysm formation at CT.29 A prospective multicenter trial using contrast-enhanced helical CT to evaluate stable patients found that 18.4% of patients with visceral injuries had arterial extravasation and will require TAE or surgery.37 Two main objectives of TAE is organ preservation and to control refractory hemodynamic instability, extraparenchymal extravasation. Depending on the objective, choice of site of embolisation and material used is decided by the interventional radiologist.7
11.1. Aortic injuries
The Society for Vascular Surgery (SVS) clinical practice guidelines advocates effective blood pressure control for grade I lesions and urgent Thoracic endovascular aortic repair (TEVAR) for grade II–IV lesions. Both TEVAR and open surgery have similar technical success rates. However, mortality (7.6% vs 15.2%), paraplegia (0% vs 5.6%) and stroke (0.85% vs 5.3%) are significantly lower in the TEVAR group in comparison to surgery. Hence, SVS clinical practice guidelines recommend TEVAR over open repair for all age groups with suitable anatomy.38
Pelvis: Pelvic hemorrhage most commonly arises from fractured bones or disrupted pelvic veins with only 10–20% of severe hemorrhage from arterial injury. Most surgeons prefer immediate TAE in hemodynamically unstable patients and current indications for TAE include active extravasation, arterial branch irregularity or truncation, one or more pseudoaneurysms, and arteriovenous fistula formation. Success rates for TAE range from 85-to 100% with lower mortality rates when TAE was performed earlier than late.7,39
11.2. Extremities
The negative predictive value of a peripheral vascular injury (PVI) in the scenario of normal clinical examination approaches 100% and hence angiography is restricted to patients with hard signs of vascular injury. CTA has a sensitivity of 90–95.1% and a specificity of 98.7–100% for detection of PVI and is increasingly replacing the catheter angiography.
Patients with ischemic type of PVI are treated surgically whereas hemorrhagic type of injuries can be managed surgically or by endovascular approach, which include balloon occlusion, TAE, and insertion of stent-grafts. Balloon occlusion is a temporary method used to control life-threatening hemorrhage in aortic and large proximal arterial injuries where direct application of pressure is not possible. Stent grafts are used to restore vessel patency when operative repair is difficult or there is an immediate need for stopping of hemorrhage. Arterial transections, dissections, and occlusions are increasingly treated by endovascular repair using insertion of stent-graft with lesser morbidity and mortality.7,40
12. Recent concepts and advances in polytrauma imaging
12.1. Damage control radiology
In order to improve clinical outcomes in Polytrauma, “Damage Control Radiology” protocols are being practiced to parallel the Damage Control Resuscitation and Damage Control Surgery measures. The three main goals of such an approach are to identify life-threatening injuries at the earliest, identification of head and spinal injuries and finally streamline the hemodynamically unstable patients for primary intervention in the least possible time.41
12.2. IR in managing unstable patient
Damage control interventional radiology (DCIR) focuses on unstable subjects while conventional interventional radiology focuses mainly on stable patients. Therefore, DCIR aims to restore normal physiology in unstable patients by controlling hemorrhage without definitive repair of the injury.
Matsumoto et al. proposed ‘Prompt and Rapid Endovascular Strategies in Traumatic Occasions” (PRESTO) where trauma patients are managed from arrival to the emergency department until initial completion of hemostasis with endovascular techniques. In this protocol, a femoral arterial sheath will be placed during primary survey providing rapid access route for endovascular balloon occlusion of the aorta. This maintains normal pressure so that patient can be imaged further or transferred to the operating room. CT scan will be performed within 10 min s and analyzed within 3 min s after initial stabilization and shifted directly to IR room for intervention when indicated. As compared to routine protocols, where IR team is activated after the CT scan, in PRESTO IR team is in action as soon the patient enters the ED, saving considerable time.42
In patients with severe injuries, the PRESTO/DCIR algorithm provides a new platform where radiology goes beyond its traditional role as an adjunct to surgery but becomes an equally important alternative or partner to surgery.
12.3. Dual energy CT
Dual energy CT (DECT) uses Xray beams in two different energy spectrum allowing better characterization of tissue composition. A recent study showed that DECT potentially altered management in 9.4% of patients and 14.4% increase in diagnostic confidence in ED imaging. DECT findings also avoided 170 follow up MRI studies, about 25 CT and USG examinations compared to conventional CT imaging and thus reducing considerable costs.43
12.4. Ultrasound applications
The FAST-Doppler protocol evaluates the presence of flow and pattern of a spectral waveform in the dorsalis pedis artery (DPA) and posterior tibial artery (PTA) of the injured limb to rule out vascular injuries without doing a doppler of the whole limb. FAST -D has sensitivity and specificity of 100% similar to standardized Color Duplex Doppler (SD) but fails to differentiate between acute or chronic lesions.44
Contrast-Enhanced Ultrasound (CEUS) has gained recent importance and has been used mainly for following up conservatively managed blunt trauma injuries. Limitations of CEUS include the cost of contrast and difficulty in imaging the deeper structures and urinary tract injuries. Both FAST-D and CEUS are time-consuming, operator dependent and their regular use in polytrauma is not routinely recommended.45
13. Conclusion
Polytrauma is a complex and challenging situation, which requires clinicians, radiologists and other medical personal to work together seamlessly as a team to deliver best results. Appropriate timely imaging and skilled radiologists play a critical role in providing accurate diagnosis. WBCT is the investigation of choice major blunt trauma and has shown better survival in patients than selective CT Imaging. FAST and E-FAST play important role in hemodynamically unstable patients to rule out major thoracic and abdominal injuries. Each institute should formulate appropriate local polytrauma imaging protocols in accordance with national and international guidelines. Multidisciplinary meetings and audits are strongly encouraged in order to achieve this and to improve patient outcomes.
Declaration of competing interest
None of the authors have any conflict of interest to declare.
Abbreviation
- AAST
American association for the surgery of trauma
- ABCDE
Airway, Breathing, Circulation, Disability, Exposure
- ABI
Ankle-brachial index
- ALARA
as low as reasonably achievable
- ATLS
Advance trauma life support
- BC
British Columbia
- CD
Color duplex doppler
- CEUS
Contrast Enhanced Ultrasound
- CT
Computed tomography
- CTA
Computed tomography angiography
- CXR
Chest X-ray
- DCIR
Damage control interventional radiology
- DCT
dual energy computed tomography
- DPA
Dorsalis pedis artery
- DSA
Digital subtraction angiography
- DUS
Doppler ultrasound
- ED
Emergency department
- EFAST
Extended Focused assessment with sonography for trauma
- FAST
Focused assessment with sonography for trauma
- FAST-D
Focused assessment with sonography for trauma-doppler
- IR
Interventional radiology
- ISS
Injury severity score
- IVC
Inferior vena cavae
- MDT
Multidisciplinary trauma
- MDCT
Multidetector computed tomography
- MRI
Magnetic resonance imaging
- MRCP
Magnetic-resonance cholangiopancreatography
- MPR
Multiplanar reconstruction
- NOM
Non-operative management
- PRESTO
Prompt and Rapid Endovascular Strategies in Traumatic Occasions
- PVI
Peripheral vascular injury
- RCT
Randomized control trial
- RRMR
Recorded real mortality rate
- RCR
Royal college of radiologists
- SCT
Selective CT
- SOP
Standard operating procedure
- SVS
Society for Vascular Surgery
- TAE
Transarterial embolisation
- TEVAR
Thoracic endovascular aortic repair
- WBCT
Whole-body CT
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harvey J.J., West/Clinical A.T.H. Radiology. 2013;68:871e886. doi: 10.1016/j.crad.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Hilbert P., Lefering R., Stuttmann R. Trauma care in Germany: major differences in case fatality rates between centers. Dtsch Arztebl Int. 2010;107:463–469. doi: 10.3238/arztebl.2010.0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoeneberg C., Schilling M., Burggraf M. Reduction in mortality in severely injured patients following the introduction of the "Treatment of patients with severe and multiple injuries" guideline of the German society of trauma surgery–a retrospective analysis of a level1trauma center (2010-2012) Injury. 2014;45(3):635–638. doi: 10.1016/j.injury.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 5.RCR . Royal College of Radiologists; London: 2011. Standards of Practice and Guidance for Trauma Radiology in Severely Injured Patients. [Google Scholar]
- 6.BC Imaging Guidelines for Major Trauma. July 2018. [Google Scholar]
- 7.Jennifer E., Gould M.D., Suresh Vedantham M.D. The role of interventional radiology in trauma. Semin Intervent Radiol. 2006;23 doi: 10.1055/s-2006-948766. 270–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ATLS Subcommittee. the ninth ed.American College of Surgeons’ Committee on Trauma International ATLS working group Advanced trauma life support (ATLS®) J Trauma Acute Care Surg. 2013;74:1363–1366. doi: 10.1097/TA.0b013e31828b82f5. [DOI] [PubMed] [Google Scholar]
- 9.Wilkerson R.G., Stone M.B. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010 Jan 17;17(1) doi: 10.1111/j.1553-2712.2009.00628.x. [DOI] [PubMed] [Google Scholar]
- 10.Agladioglu K., Serinken M., Dal O., Beydilli H., Eken C., Karcioglu O. Chest X-rays in detecting injuries caused by blunt trauma. World J Emerg Med. 2016;7(1):55–58. doi: 10.5847/wjem.j.1920-8642.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Exadaktylos A.K., Sclabas G., Schmid S.W., Schaller B., Zimmermann H. Do we really need routine computed tomographic scanning in the primary evaluation of blunt chest trauma in patients with "normal" chest radiograph? J Trauma. 2001 Dec;51(6):1173–1176. doi: 10.1097/00005373-200112000-00025. [DOI] [PubMed] [Google Scholar]
- 12.Brar M.S., Bains I., Brunet G. Occult pneumothoraces truly occult or simply missed: redux. J Trauma. 2010;69:1335e7. doi: 10.1097/TA.0b013e3181f6f525. [DOI] [PubMed] [Google Scholar]
- 13.Kea B., Gamarallage R., Vairamuthu H. What is the clinical significance of chest CT when the chest x-ray result is normal in patients with blunt trauma? Am J Emerg Med. 2013;31(8):1268–1273. doi: 10.1016/j.ajem.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panczykowski D.M., Tomycz N.D., Okonkwo D.O. Comparative effectiveness of using computed tomography alone to exclude cervical spine injuries in obtunded or intubated patients: meta- analysis of 14,327 patients with blunt trauma. J Neurosurg. 2011;115:541–549. doi: 10.3171/2011.4.JNS101672. [DOI] [PubMed] [Google Scholar]
- 15.Den Boer T.A., Geurts M., van Hulsteijn L.T. The value of clinical examination in diagnosing pelvic fractures in blunt trauma patients: a brief review. Eur J Trauma Emerg Surg. 2011;37(4):373–377. doi: 10.1007/s00068-011-0076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soto J.R., Zhou C., Hu D., Arazoza A.C., Dunn E., Sladek P. Skip and save: utility of pelvic x-rays in the initial evaluation of blunt trauma patients. Am J Surg. 2015 Dec;210(6):1076–1079. doi: 10.1016/j.amjsurg.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 17.Al-Salamah S.M., Mirza S.M., Ahmad S.N., Khalid K. Role of ultrasonography, computed tomography and diagnostic peritoneal lavage in abdominal blunt trauma. Saudi Med J. 2002 Nov;23(11):1350–1355. [PubMed] [Google Scholar]
- 18.Shanmuganathan K., Mirvis S.E., Sherbourne C.D., Chiu W.C., Rodriguez A. Hemoperitoneum as the sole indicator of abdom- inal visceral injuries: a potential limitation of screening abdominal US for trauma. Radiology. 1999;212:423–430. doi: 10.1148/radiology.212.2.r99au18423. [DOI] [PubMed] [Google Scholar]
- 19.Mohammadi A., Ghasemi-Rad M. Evaluation of gastrointestinal injury in blunt abdominal trauma “FAST is not reliable”: the role of repeated ultrasonography. World J Emerg Surg. 2012;7(1):2. doi: 10.1186/1749-7922-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stuart Netherton,Velimir Milenkovic,Mark Taylor, Philip J. Davis, Diagnostic accuracy of eFAST in the trauma patient: a systematic review and meta-analysis July 2019Canadian J Emerg Med 21(6):1-12. [DOI] [PubMed]
- 21.Smith C.B., Barrett T.W., Berger C.L. Prediction of blunt traumatic injury in high-acuity patients: bedside examination vs computed tomography. Am J Emerg Med. 2011;29:1e10. doi: 10.1016/j.ajem.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 22.Low R., Duber C., Schweden F. Whole body spiral CT in primary diagnosis of patients with multiple trauma in emergency situations. Röfo. 1997;166:382e8. doi: 10.1055/s-2007-1015446. [DOI] [PubMed] [Google Scholar]
- 23.PtakT RheaJT., NovellineRA Experience with a continuous,single-pass whole-body multidetector CT protocol for trauma: the three-minute multiple trauma CT scan. Emerg Radiol. 2001;8:250–256. [Google Scholar]
- 24.Çorbacıoğlu Şeref Kerem, Gökhan Aksel Whole body computed tomography in multi trauma patients: review of the current literature. Turk J Emerg Med. 3 Oct. 2018;18:4 142–147. doi: 10.1016/j.tjem.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh S., Kalra M.K., Thrall J.H., Mahesh M. Pointers for optimizing radiation dose in pediatric CT protocols. J Am Coll Radiol. 2012;9:77. doi: 10.1016/j.jacr.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Brink M., de Lange F., Oostveen L.J. Arm raising at exposure-controlled multidetector trauma CT of thoracoabdominal region: higher image quality, lower radiation dose. Radiology. 2008;249:661–670. doi: 10.1148/radiol.2492080169. [DOI] [PubMed] [Google Scholar]
- 27.Shannon L., Peachey T., Skipper N. Comparison of clinically suspected injuries with injuries detected at whole-body CT in suspected multi-trauma victims. Clin Radiol. 2015;70:1205–1211. doi: 10.1016/j.crad.2015.06.084. [DOI] [PubMed] [Google Scholar]
- 28.Muckart D., Pillay Bala, Hardcastle Timothy, Skinner David. Vascular injuries following blunt polytrauma. Eur J Trauma Emerg Surg. 2014:315–322. doi: 10.1007/s00068-014-0382-y. [DOI] [PubMed] [Google Scholar]
- 29.Omert L.A., Salyer D., Dunham M., Porter J., Silva A., Protetchb J. Implications of the ‘‘contrast blush’’ finding on computed tomographic scan of the spleen in trauma. J Trauma. 2001;51:272–278. doi: 10.1097/00005373-200108000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Berlin L. Multitasking, interruptions, and errors. AJR Am J Roentgenol. 2012;198:W89. doi: 10.2214/AJR.10.5529. [DOI] [PubMed] [Google Scholar]
- 31.Waite Stephen, Scott Jinel, Gale Brian, Fuchs Travis, Kolla Srinivas, Reede Deborah. Interpretive error in radiology. AJR. 2017;208:739–749. doi: 10.2214/AJR.16.16963. [DOI] [PubMed] [Google Scholar]
- 32.Agostini C., Durieux M., Milot L. Value of double reading of whole body CT in polytrauma patients. J Radiol. 2008;89:325e30. doi: 10.1016/s0221-0363(08)93007-9. [DOI] [PubMed] [Google Scholar]
- 33.Giannakopoulos G.F., Saltzherr T.P., Beenen L.F. Missed injuries during the initial assessment in a cohort of 1124 level-1 trauma patients. Injury. 2011 Sep;43(9):1517–1521. doi: 10.1016/j.injury.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 34.AAST . American Association for the Surgery of Trauma; 2012. Injury Scoring Scale: A Resource for Trauma Care Professionals.www.aast.org Available at: [Google Scholar]
- 35.The Royal College of Radiologists Paediatric Trauma protocols.(Ref No. BFCR (14)8) C The Royal College of Radiologists; August 2014. [Google Scholar]
- 36.Lowdermilk C., Gavant M.L., Qaisi W., West O.C., Goldman S.M. Screening helical CT for evaluation of blunt traumatic injury in the pregnant patient. Radiographics. 1999;19 doi: 10.1148/radiographics.19.suppl_1.g99oc28s243. (Spec No):S243e55. discussion S256e8. [DOI] [PubMed] [Google Scholar]
- 37.Yao D.C., Jeffrey R.B., Mirvis S.E. Using contrast enhanced helical CT to visualize arterial extravasation after blunt abdominal trauma: incidence and organ distribution. AJR Am J Roentgenol. 2002;178:17–20. doi: 10.2214/ajr.178.1.1780017. [DOI] [PubMed] [Google Scholar]
- 38.Akhmerov A., DuBose J., Azizzadeh A. Blunt thoracic aortic injury: current therapies, outcomes, and challenges. Ann Vasc Dis. 2019;12(1):1–5. doi: 10.3400/avd.ra.18-00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Awwad A., Dhillon P.S., Ramjas G., Habib S.B., Al-Obaydi W. Trans-arterial embolisation (TAE) in haemorrhagic pelvic injury: review of management and mid-term outcome of a major trauma centre. CVIR Endovasc. 2018;1(1):32. doi: 10.1186/s42155-018-0031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson C.A. Endovascular management of peripheral vascular trauma. Semin Intervent Radiol. 2010;27(1):38–43. doi: 10.1055/s-0030-1247887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chakraverty S., Zealley I., Kessel D. Damage control radiology in the severely injured patient: what the anaesthetist needs to know. Br J Anaesth. 2014 Aug;113(2):250–257. doi: 10.1093/bja/aeu203. [DOI] [PubMed] [Google Scholar]
- 42.Matsumoto J., Lohman B.D., Morimoto K., Ichinose Y., Hattori T., Taira Y. Damage control interventional radiology (DCIR) in prompt and rapid endovascular strategies in trauma occasions (PRESTO): a new paradigm. Diagn Interv Imaging. 2015;96(7-8):687–691. doi: 10.1016/j.diii.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 43.Aran Shima, Daftari Besheli Laleh, Karcaaltincaba Musturay, Gupta Rajiv, Flores Efren J., Abujudeh Hani H. Applications of dual-energy CT in emergency radiology. Am J Roentgenol. 2014;202(4):W314–W324. doi: 10.2214/AJR.13.11682. [DOI] [PubMed] [Google Scholar]
- 44.Montorfano M.A., Montorfano L.M., Perez Quirante F., Rodríguez F., Vera L., Neri L. The FAST D protocol: a simple method to rule out traumatic vascular injuries of the lower extremities. Crit Ultrasound J. 2017;9(1):8. doi: 10.1186/s13089-017-0063-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miele V., Piccolo C.L., Galluzzo M., Ianniello S., Sessa B., Trinci M. Contrast-enhanced ultrasound (CEUS) in blunt abdominal trauma. Br J Radiol. 2016;89(1061):20150823. doi: 10.1259/bjr.20150823. [DOI] [PMC free article] [PubMed] [Google Scholar]