Abstract
Iatrogenic nerve injuries can cause patients and surgeons a great deal of distress and anxiety. To help prevent such injuries, surgeons should remain mindful for potential distortion of anatomy due to scarring and adhesions. Peripheral nerves are vulnerable to thermal injury, as well as mechanical injury by laceration and traction.
Revision arthroplasty may involve removal of the implant and cement mantle. During this removal process, breaches in cortical bone can occur, with resultant cement extrusion within the soft tissues. Screw holes left vacant following screw removal may also allow for cement leakage. Thermal energy is released during the exothermic polymerisation process of cement curing. As a result, this thermal energy can also lead to injury to neural tissue.
In this article, we present three cases of radial nerve palsy associated with cement extrusion during revision arthroplasty, in order to highlight pitfalls and learning points in the management. In addition, we propose strategies to avoid such injuries. Surgeons are reminded to be vigilant for cortical breaches intraoperatively, and if recognised, steps should be taken to minimise the risk of nerve injury.
Keywords: Cement extrusion, Radial nerve palsy, Revision arthroplasty, Cortical breach
Introduction
Iatrogenic nerve injuries can cause patients and surgeons great anxiety. There is increased risk during revision surgery.1 Surgeons should remain mindful for potential anatomical distortion due to scarring and adhesions. Nerves are vulnerable to mechanical injury by laceration or traction, and thermal insult.
Revision arthroplasty may involve removal of the implants and cement. During removal, breaches within cortical bone can occur, with resultant cement extrusion within the soft tissues. Vacant screw-holes following screw removal also allow for cement leakage. Thermal energy is released during the exothermic polymerisation process of cement curing, leading to injury to neural tissue, in addition to bone necrosis, chondrocyte and skin damage.2
Three cases of radial nerve palsy associated with cement extrusion during revision arthroplasty are presented to highlight learning points in the management. Strategies to avoid such injuries are also proposed.
Case 1
An 80-year-old patient underwent revision of a loose humeral component 13-years following elbow arthroplasty. A posterior cortical window was created to aid cement removal. During humeral preparation, the cortex was breached with the trial implant. The window and penetration site were protected with a shield manufactured from a syringe, and the radial nerve was exposed prior to cementing. Implants were then cemented using image-guidance. Postoperatively, the patient developed a wrist drop. Sensibility in the first dorsal web space was preserved. Plain radiographs (Fig. 1) revealed cement extrusion.
Fig. 1.
AP and lateral radiographs of the elbow revealing cement extrusion proximally.
Initially the wrist drop was managed expectantly. However, there was no recovery; neurophysiology at three months confirmed a dense radial nerve palsy. The patient was referred to the nerve service, with exploration revealing significant adherence/scarring as the nerve coursed around the spiral groove. Following neurolysis, it was evident that there was complete disruption of the radial nerve (Fig. 2A, Fig. 2B). The resultant defect post-debridement was over 10cm. In view of the patient’s age and extensive nerve defect, nerve grafting was not attempted. Tendon transfer was performed at a later date.
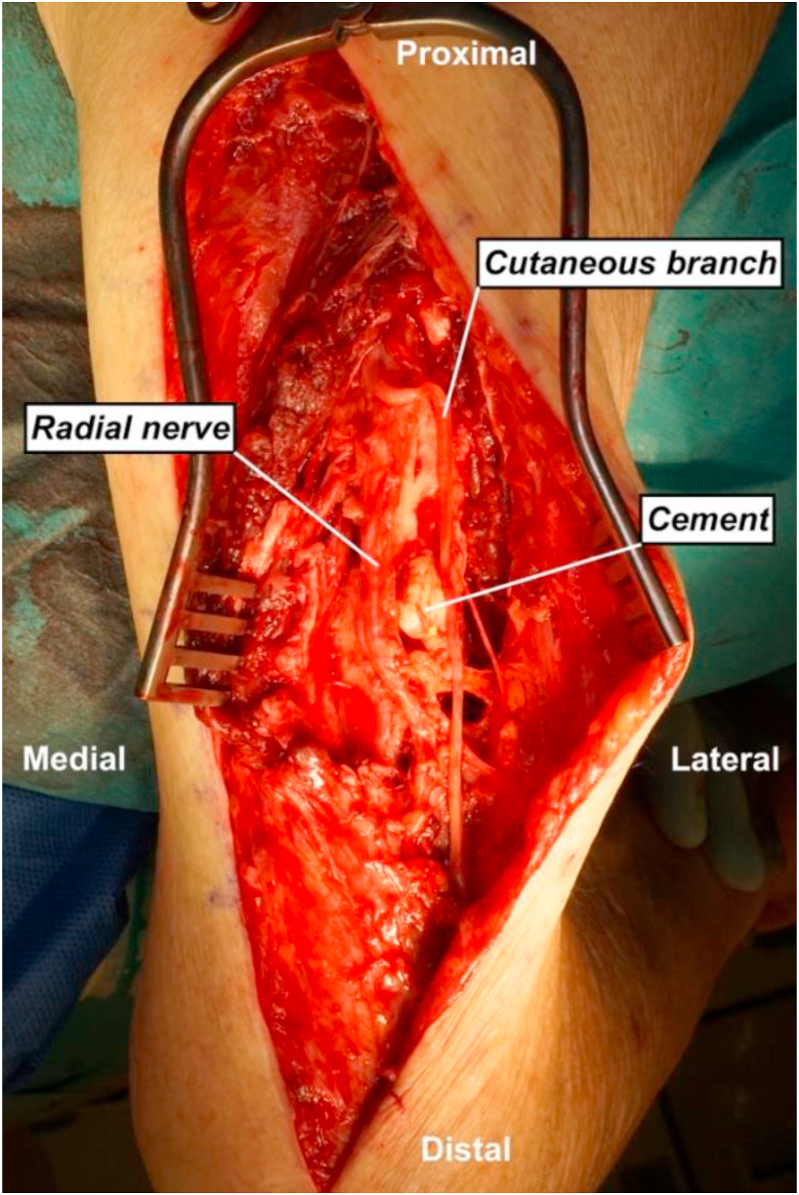
Fig. 2A.
Intraoperative image showing the posterior approach to the radial nerve. The radial nerve was encased within cement and was traced to a neuroma at the intermuscular septum.
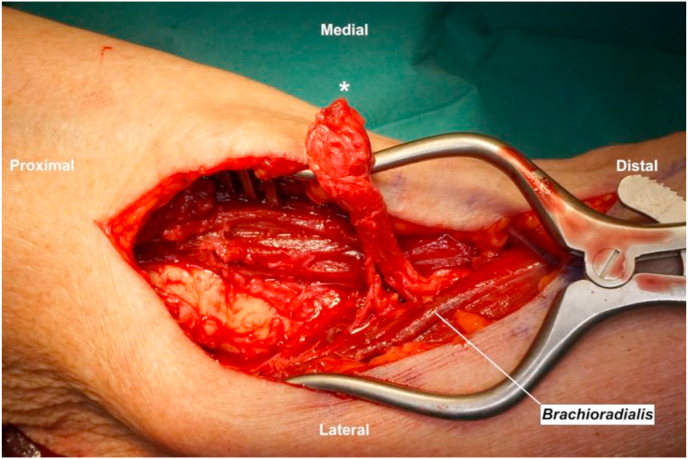
Fig. 2B.
Intraoperative image showing the anterior approach to the radial nerve. The distal nerve stump is marked with an asterisk.
Case 2
A 60-year-old patient with rheumatoid arthritis underwent revision of a humeral component 6 years following elbow arthroplasty. The patient underwent cement and implant removal with cannulated intramedullary reaming, before the new component was cemented, with no documented cortical breaches. Postoperatively, the patient developed a wrist drop. Plain radiographs revealed cement extrusion (Fig. 3). Neurophysiology at three months revealed axonal injury to the radial nerve.
Fig. 3.
AP and lateral radiographs of the elbow revealing cement extrusion.
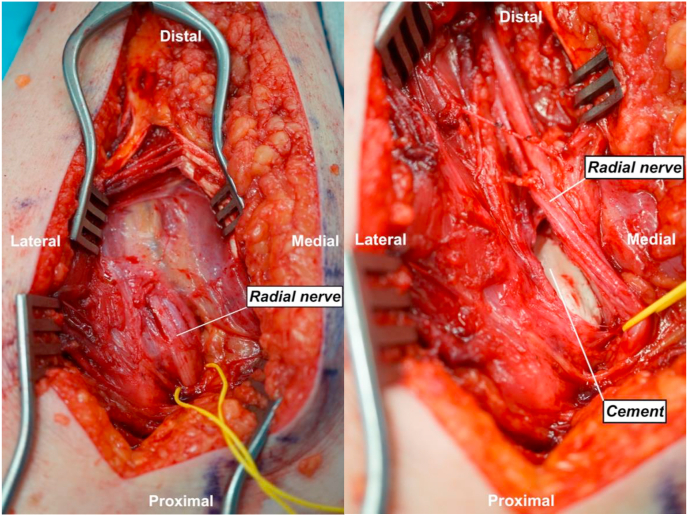
The patient was referred to the nerve service, with exploration revealing the nerve to be in continuity. Beneath the nerve, a pseudocapsule had formed around the cement, which itself was smooth. External neurolysis was performed (Fig. 4), epineural vessels were then visible. Fascial tissue was repaired over the cement to serve as interposition between cement and nerve. By eight months, the patient had fully recovered wrist and digital extension.
Fig. 4.
Intraoperative images showing the posterior approach to the radial nerve. The nerve has been exposed but not formally neurolysed. Following neurolysis, note the impression left on the cement by the radial nerve, which was in continuity.
Case 3
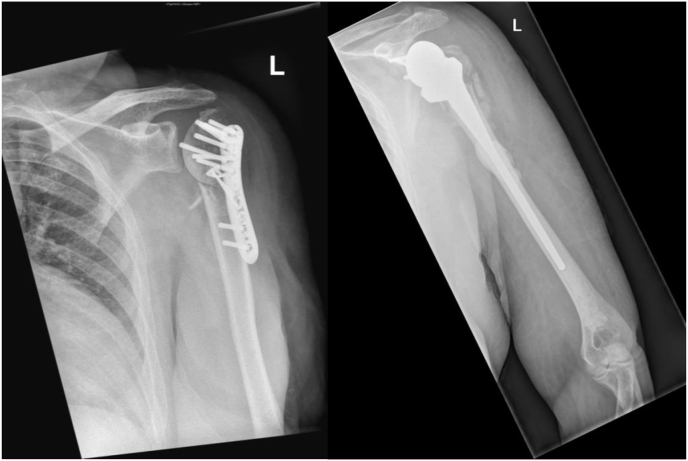
A 65-year-old patient underwent single-stage revision of failed proximal humerus fixation to reverse shoulder arthroplasty (Fig. 5). Post-operatively, the patient developed a wrist drop. Plain radiographs revealed cement extrusion.
Fig. 5.
Varus collapse following fixation, leading to revision to a long-stemmed reverse shoulder arthroplasty.
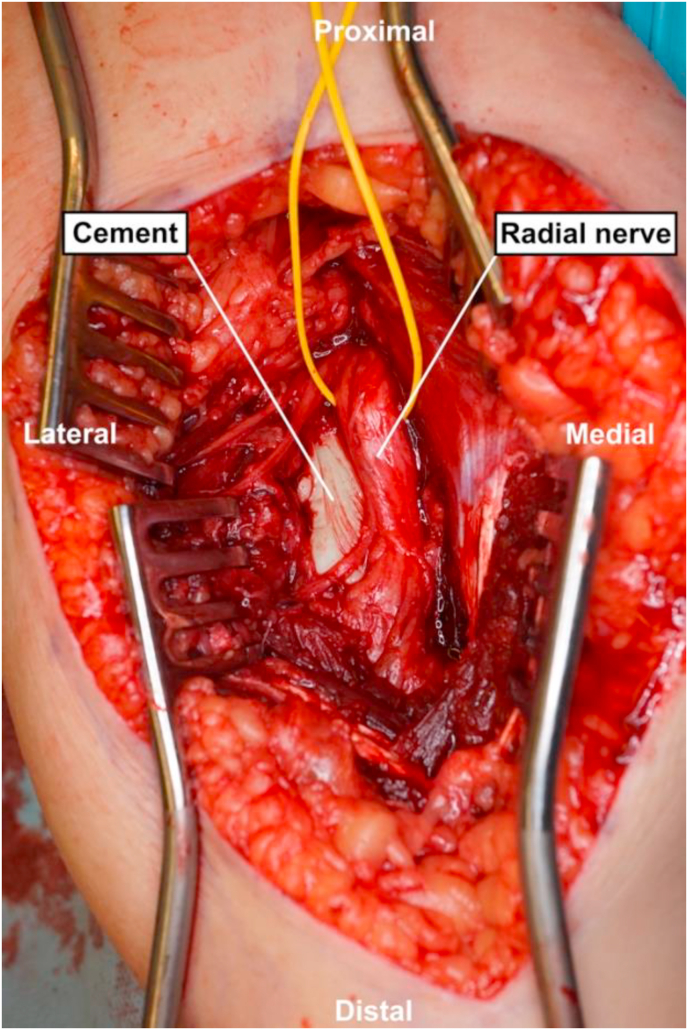
Neurophysiology at two months revealed a severe radial nerve lesion. The patient was referred to the nerve service. Exploration at 4 months revealed the nerve to be in continuity, albeit tethered to and overlying a large area of cement. Following neurolysis, the segment of radial nerve was noted to be soft, thus nerve grafting was not performed (Fig. 6). The pseudocapsule over the cement was repaired to serve as interposition. There had been recovery of wrist extension at five months.
Fig. 6.
Intraoperative image showing the posterior approach to the radial nerve. There was a pseudocapsule covering the cement and the nerve remained in continuity.
Discussion
Removing implants and cement during revision arthroplasty can be challenging. Perforation of cortical bone may occur unbeknownst to the surgeon. Drills may veer from their intended target and cause breaches. This leaves a tract for cement extrusion, potentially causing thermal damage to adjacent neural structures. A technical tip to avoid inadvertent penetration is to use a syringe as a centralising device during reaming of the cement mantle.3 Cortical perforation can also occur during stem insertion4 (case 1). Surgeons should be mindful of this in those with poor bone quality. Stems can also be pushed off-course by remnants of cement within the canal.
Vacant screw-holes following plate removal are also a source of cement leakage. Strategies to prevent this include occlusion with finger-tips while cementing, plugging the holes with bone-chips, or inserting short-threaded unicortical screws. Where a two-stage procedure is planned, screw-holes can fill-in naturally. Humeral component cementation therefore demands awareness, especially in cases where empty screw-holes may be present. If such breaches knowingly occur, we recommend the nerve at risk is formally exposed and protected throughout the remainder of the procedure.
The British Orthopaedic Association (BOA) guideline on the management of nerve injuries highlighted that ‘it must be accepted that nerve injury during operation may occur in spite of due care. Early recognition and prompt remedial action after the event are the keys to a good outcome’.5 Requesting neurophysiology must not delay referral or treatment.6 The presence of cement extrusion in the vicinity of a nerve with a dense palsy should prompt serious consideration for urgent exploration. Cement curing temperature has been known to rise up to 100° Celsius in vitro,7 which is some way above the protein denaturation point. Thus, one may argue that permanent nerve damage could take place within minutes of cement extrusion hence disputing the value of delayed nerve exploration. However, the presence of fluid/soft tissue between cement and nerve could potentially buffer heat conduction, which may explain the subsequent recovery seen in cases 2 and 3.
Surgical exploration permits the nature and extent of nerve injury to be ascertained. Some may have reservations regarding exploration of nerve palsies following arthroplasty due to concern for secondary infection. However, even in cases where nerves are in continuity, it has been shown that neurolysis may improve neuropathic pain,8 by removing scar tissue or tight fascia that may be impeding neural recovery.
In conclusion, the reported cases highlight an infrequent cause of radial nerve palsy due to cement extrusion during revision upper limb arthroplasty. Surgeons should remain vigilant for cortical breaches intraoperatively, and if recognised, steps should be taken to minimise the risk of nerve injury.
Conflicting interests
The authors declare that there is no conflict of interest.
Funding
No grants were received from any funding agency in the public, commercial, or not-for-profit sectors.
Informed consent
Written informed consent was obtained from the patients for their anonymised information to be published in this article.
Ethical approval
Not applicable.
Guarantor
Not applicable.
Contributorship
AA drafted the article; CYN reviewed and edited the article. Both authors approved the final version to be published.
Acknowledgements
None.
References
- 1.Hasija R., Kelly J.J., Shah N.V. Nerve injuries associated with total hip arthroplasty. J Clin Orthop Trauma. 2018;9(1):81–86. doi: 10.1016/j.jcot.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy T.A., Mathews J.A., Whitehouse M.R., Baker R.P. Investigation of thermally induced damage to surrounding nerve tissue when using curettage and cementation of long bone tumours, modelled in cadaveric porcine femurs. Arch Orthop Trauma Surg. 2019;139(8):1033–1038. doi: 10.1007/s00402-019-03129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phadnis J., Hearnden A. An adjunct to safe cement removal in revision shoulder arthroplasty. Ann R Coll Surg Engl. 2014;96(3):248–249. doi: 10.1308/rcsann.2014.96.3.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Owens C.J., Sperling J.W., Cofield R.H. Utility and complications of long-stem humeral components in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(7):e7–12. doi: 10.1016/j.jse.2012.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Birch R., Biant L. British Orthopaedic Association; 2011. The Management of Nerve Injuries: A Guide to Good Practice. [Google Scholar]
- 6.British Orthopaedic Association . 2012. BOAST - Peripheral Nerve Injury. [Google Scholar]
- 7.Koh B.T.H., Tan J.H., Ramruttun A.K., Wang W. Effect of storage temperature and equilibration time on polymethyl methacrylate (PMMA) bone cement polymerization in joint replacement surgery. J Orthop Surg Res. 2015;10(1):178. doi: 10.1186/s13018-015-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kyriacou S., Pastides P.S., Singh V.K., Jeyaseelan L., Sinisi M., Fox M. Exploration and neurolysis for the treatment of neuropathic pain in patients with a sciatic nerve palsy after total hip replacement. J Bone Jt Surg. 2013;95-B(1):20–22. doi: 10.1302/0301-620x.95b1.29740. [DOI] [PubMed] [Google Scholar]