Abstract
Background
Tourniquet use is ubiquitous in orthopaedic surgery to create a bloodless field and to facilitate safe surgery, however, we know of the potential complications that can occur as a result of prolonged tourniquet time. Experimental and clinical research has helped define the safe time limits but there is not much literature specific to foot and ankle surgery.
Methods
A retrospective review of the postoperative course of patients with prolonged tourniquet time (longer than 180 min) for foot and ankle procedures was done. Data related to the patient factors and the surgical procedure was collected. The length of stay, re-admissions and complications were the important indicators of the individual patient’s recovery.
Results
Twenty patients were identified with longer than 180-min tourniquet times for complex foot and ankle procedures. The average uninterrupted tourniquet time was 191 min. Eight of the twenty procedures were revision surgeries. The average length of stay was 3 days and there were no re-admissions within 30 days. Eight patients (40%) had at least one recorded complication. The complications seen in this group were transient sensory loss, wound issues, superficial infection, ongoing pain and non-union.
Conclusions
This case series has not revealed any major systemic complications resulting from the prolonged tourniquet such as pulmonary embolism or renal dysfunction. Unlike past literature on knee procedures with extended tourniquet times, no major nerve palsies were seen in our patient group. Our understanding of the local and systemic effects of tourniquet is not complete and this study demonstrates that the complications do not necessarily increase in a linear fashion in relation to the tourniquet time.
Keywords: Safe tourniquet time, Foot surgery, Tourniquet complications
1. Introduction
The use of pneumatic tourniquets in orthopaedic surgery has been extensively researched and past studies have directed the established protocols. Current practice is based mainly on animal studies which show adverse biochemical and ultrastructural changes, both systemic and local,1, 2, 3, 4, 5 following prolonged tourniquet time. Majority of the clinical studies have been done for knee procedures6, 7, 8, 9, 10, 11 and evidence for foot and ankle surgery is minimal. Based on current protocol, most foot & ankle surgeons will aim to keep to a tourniquet time of less than 2 h for their procedures and significantly exceeding this time limit is uncommon. The effects of long tourniquet time within this field have therefore been rarely studied and there is a lack of literature on the effects of using tourniquets beyond 3 h. Wakai et al.12 described a number of tourniquet related complications ranging from minor (swelling, delay in recovery of muscle power) to major (rhabdomyolysis, deep vein thrombosis, cerebral infarction). We have retrospectively reviewed our electronic records to see if there was a high incidence of complications in foot and ankle surgery with tourniquet time of 3 h or more.
2. Patients and methods
The hospital trust electronic database holds operative details of all surgical cases. A retrospective review of this database was performed. Procedures for foot and ankle pathology with a thigh tourniquet time exceeding 180 min were identified, with a date restriction between 2011 and 2018. Patient specific details such as age, sex, body mass index (BMI), smoking status and medical co-morbidities were recorded. Procedure specific data including details of surgery, ASA grade, type of anaesthetic, grade of operating surgeon, tourniquet time, length of stay and readmissions within 30 days was also collected. Inpatient records and clinic letters from outpatient appointments were assessed for complications. Reasons for long in-patient stay were investigated by studying the notes made by the medical and nursing staff, physiotherapists and the acute pain team.
3. Results
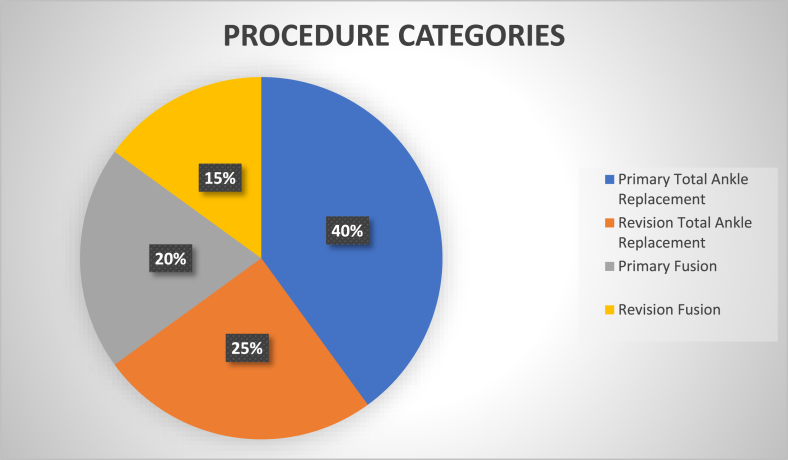
Between 2011 and 2018, 20 patients were identified with thigh tourniquet time of more than 180 min. There were 13 male and 7 female patients. Table 1 gives details of the demographics for the cohort of patients. Fig. 1 illustrates the broad categories of surgeries performed.
Table 1.
Patient characteristics.
| MEAN AGE (years) | 65 (24-84) | |
| SIDE | RIGHT | 8 (40%) |
| LEFT | 12 (60%) | |
| SEX | MALE | 13 (65%) |
| FEMALE | 7 (35%) | |
| ASA | 1 | 4 (20%) |
| 2 | 11 (55%) | |
| 3 | 5 (25%) | |
| MEAN BMI | 29 (19–39.6) | |
Fig. 1.
Procedure categories.
All procedures were complex foot and ankle surgeries and eight of these were revision procedures. The patients received general anaesthesia supplemented by a nerve block. The blocks were popliteal with femoral in two cases and popliteal with saphenous in the rest. A popliteal catheter was left in situ in 15 patients. An elastomeric pump was used to deliver local anaesthetic as continuous infusion through the catheter post-operatively. All blocks were administered with a standard technique using ultrasound and nerve stimulator.
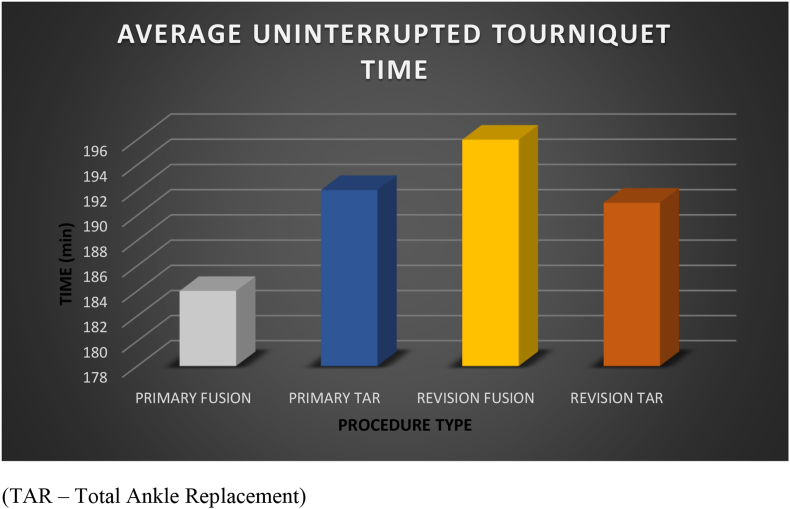
The average uninterrupted tourniquet duration was 191 min. The four cases (revision total ankle replacements) with the longest tourniquet times had an interruption in the period of inflation to allow a reperfusion interval. For these four cases the first tourniquet inflated session lasted between 40 and 53 min and the second session was between 187 and 196 min. Therefore, all 20 patients had an uninterrupted tourniquet time of longer than 180 min. Tourniquet pressure was set at 300 mm Hg for all patients. Fig. 2 reports the average uninterrupted tourniquet times in each surgical category.
Fig. 2.
Average uninterrupted tourniquet time.
Hospital stay ranged from 1 to 7 days. There were four patients with long inpatient stay, two for social reasons and two had pain at the surgical site that was difficult to control. None of the patients had a readmission within 30 days. All patients were reviewed in the outpatient clinic at 2 weeks, 6 weeks and 3 months and then as clinically required.
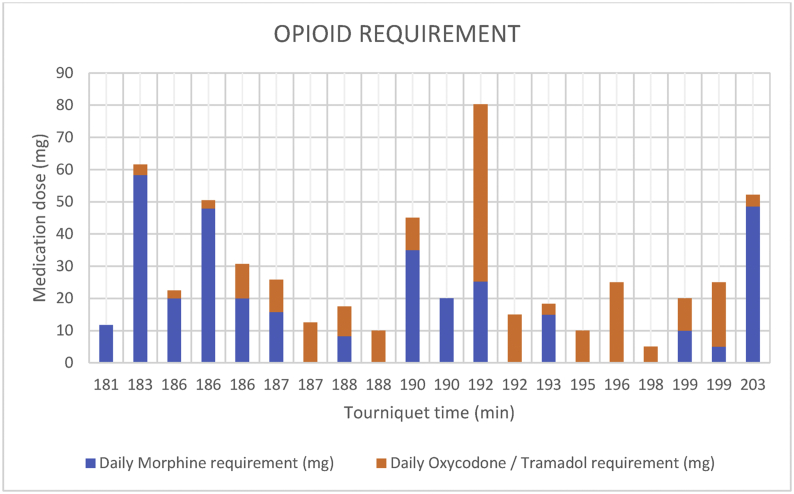
3.1. Opioid requirement
Opioids were commonly administered for post-operative pain relief. Most patients required morphine and oxycodone preparations. One of the patients received Tramadol due to intolerance to morphine and oxycodone. We have looked at the doses required for pain control in the individual patient during their stay in the hospital and calculated the average daily requirement. Fig. 3 is a graphical representation of the average daily opioid doses for individual patients plotted against increasing tourniquet time. As can be seen in the graph, there is no increasing trend of opioid intake with increasing tourniquet time within this group. Table 2 has information on the average daily requirement for morphine and other opioids for each type of surgery as well as the whole group of patients. There was a slightly higher opioid consumption in patients who had a fusion versus a replacement procedure.
Fig. 3.
Average daily opioid requirement.
Table 2.
Average daily opioid intake by procedure type.
| DAILY MORPHINE (mg) | DAILY OXYCODONE/TRAMADOL (mg) | |
|---|---|---|
| ALL PATIENTS | 17 (0–58.3) | 10.9 (0–55) |
| PRIMARY FUSION | 26.4 (11.7–20) | 3.9 (0–10) |
| TOTAL ANKLE REPLACEMENT | 15.8 (0–48) | 7.6 (0–20) |
| REVISION FUSION | 27.9 (0–46) | 7.9 (3.6–10) |
| REVISION TOTAL ANKLE REPLACEMENT | 5.1 (0–25.3) | 23.5 (10–55) |
3.2. Complications
A total of eight patients (40%) had at least one recorded complication. Two patients (10%) had transient loss of sensations in the leg which recovered completely by two weeks. One patient (5%) had blister formation around the wound which settled in two weeks and wound dehiscence which took two months to heal. This patient also had non-union of the extended medial column fusion. One patient had superficial infection which settled with a course of antibiotics. Ongoing pain was experienced by five patients (25%) – two patients (10%) among these had non-union (tibiocalcaneal fusion and extended medial column fusion), one had pain related to a screw in the medial malleolus and the cause of pain couldn’t be determined in the remaining two patients.
None of the patients complained of tourniquet related pain in the thigh. In summary, the five patients with ongoing pain were the only ones suffering persistent problems following surgery. There were no systemic complications such as pulmonary embolism or renal dysfunction due to rhabdomyolysis. Table 3 gives details of the procedures and complications.
Table 3.
Complications by procedure.
| TYPE OF PROCEDURE | PATIENT NUMBER | INDICATION | DETAILS OF SURGERY | COMPLICATIONS |
|---|---|---|---|---|
| PRIMARY FUSION | 1 | Severe cavovarus deformity | Talectomy and tibiocalcaneal fusion with nail | None |
| 2 | Rheumatoid arthritis - Fixed planovalgus deformity and arthritis in the naviculocuneiform and triple joints | Triple fusion and extended medial column fusion | Blisters Wound dehiscence Medial column non-union Ongoing pain |
|
| 3 | Fixed planovalgus deformity | Corrective triple fusion for planovalgus foot correction | Transient numbness below tourniquet level | |
| 4 | Congenital equinovalgus | Corrective triple fusion and tibialis posterior to tibialis anterior transfer | None | |
| PRIMARY TOTAL ANKLE REPLACEMENT | 5 | Ankle osteoarthritis | Total ankle replacement | None |
| 6 | Ankle osteoarthritis | Total ankle replacement | None | |
| 7 | Ankle osteoarthritis with medial malleolar cyst | Total ankle replacement with prophylactic fixation of medial malleolus | Long inpatient stay due to pain control issues Ongoing pain related to medial malleolus screw |
|
| 8 | Ankle osteoarthritis | Total ankle replacement and lateral ligament reconstruction (Brostrom) | None | |
| 9 | Ankle osteoarthritis | Total ankle replacement | Superficial infection controlled with oral antibiotics | |
| 10 | Ankle osteoarthritis with fracture fixation metalwork in-situ | Removal of metalwork and total ankle replacement | None | |
| 11 | Ankle osteoarthritis | Total ankle replacement | None | |
| 12 | Ankle osteoarthritis | Total ankle replacement and lateral ligament reconstruction (Brostrom) and BRT osteotomy | None | |
| REVISION FUSION | 13 | Painful ankle replacement, previous subtalar fusion | Removal of ankle replacement and ankle fusion with fresh frozen femoral head allograft | Transient loss of sensations |
| 14 | Non-union of subtalar and talonavicular fusion. Previous ankle fusion | Revision triple fusion | Long inpatient stay due to pain control issues Ongoing pain in the foot |
|
| 15 | Failed total ankle replacement – aseptic loosening | Removal of total ankle replacement and tibiocalcaneal arthrodesis with fresh frozen femoral head allograft | Infected Non-union of the Tibiocalcaneal fusion Ongoing pain |
|
| REVISION TOTAL ANKLE REPLACEMENT | 16 | Previous ankle fusion in equinus with subtalar and talonavicular degenerative change | Removal of metalwork, revision of ankle fusion to total ankle replacement and debridement of talonavicular joint | None |
| 17 | Failed total ankle replacement – aseptic loosening of talar component | Revision total ankle replacement | None | |
| 18 | Failed total ankle replacement – aseptic loosening of talar component | Revision total ankle replacement | None | |
| 19 | Painful total ankle replacement | Revision total ankle replacement | Ongoing pain | |
| 20 | Painful total ankle replacement | Revision total ankle replacement | None |
4. Discussion
Despite the use of pneumatic tourniquets being commonplace in orthopaedic foot and ankle surgery, our understanding of safe tourniquet times is not complete. Most of the clinical evidence base is centred on knee surgery. Not only is it necessary to look at the existing evidence defining safe time limits, but also to examine outcomes of patients who had prolonged tourniquet times.
Current practices are based on recommendations from a mix of experimental and clinical studies and the larger contribution has been from animal-based studies. Heppenstall et al.,1 using a dog hindleg experiment, found evidence of muscle hypoxia, hypercarbia and acidosis as well as increased levels of CPK and lactic acid with longer tourniquet time.
Patterson and Klenerman2 in a study of ultrastructural changes in Rhesus monkey muscle tissue found increasing damage with higher tourniquet time. However, they found no lasting damage to the muscles distal to and under the tourniquet for up to 3 h. They have suggested that the findings of more profound damage with shorter tourniquet times, by other investigators, might be related to the species of mammal used for the experiments, small animal tissue being more susceptible to ischemic injury.
Ochoa et al.3 studied the effects of tourniquet on nerve ultrastructure in Baboons. The main pathological change was displacement of nodes of Ranvier and more nodes were involved with longer tourniquet time especially under the edge of the tourniquet. But these findings were studied with tourniquet pressures of 500- and 1000-mm Hg which are far higher than pressures used for orthopaedic surgeries.
Rorabeck et al.4 found slowing of sciatic nerve conduction velocity and stated that the conduction always returned to normal if the inflation pressure was less than 500 mm Hg and duration less than 2 h.
Pedowitz5 in a detailed experimental study concluded that the 2- hour threshold might be relevant to clinical scenarios based on the muscle injury patterns noted in a Rabbit model. He used Tc99 and Evans blue uptake as well as histopathological examination of sections to study the muscle damage.
Multiple clinical studies have investigated tourniquet use in knee surgery. Dobner and Nitz6 highlighted EMG changes and impairment of functional capacity which was measured by a single leg vertical jump in patients who had undergone meniscectomy under tourniquet control. The control group with patients who had surgery without tourniquet did not have denervation changes on EMG at 6 weeks post-surgery which was seen in 71% of the tourniquet group.
Clarke et al.7 measured tissue hypoxia using transcutaneous oxygen pressure electrodes. They noted more significant hypoxia of wound flaps with higher tourniquet pressures. They did not find any relation between the duration of tourniquet and tissue hypoxia. Hirota et al.8 found that the number of right atrial emboli (measured using trans-esophageal electrocardiography) correlated with tourniquet time. Kokki et al.9 noted changes in nerve conduction and EMG studies following tourniquet use in ACL reconstruction surgery.
Lin et al.13 outlined decrease in pulmonary function parameters and occurrence of metabolic changes suggestive of lipid peroxidation (plasma malondialdehyde level) and systemic inflammatory response (IL-6 and IL-8 levels) even within safe tourniquet times of sixty to 90 min. This was done on a cohort of patients who had lower limb trauma surgery.
The common theme to all these studies was that long-term clinical problems could not be attributed to the adverse changes.
Olivecrona et al.10 demonstrated high incidence of complications such as superficial infection and cuff pressure injury in knee arthroplasty surgery with tourniquets of longer than 100 min. The odds of suffering a complication were higher in women and if the patient had more medical comorbidities. They noted that there was a 20% increase in the odds of having a complication with every 10-min increase in tourniquet time.
The only study that had patients with longer than 3-h tourniquet times was by Horlocker et al.11 The cohort was of 1166 total knee replacements with average tourniquet time of 145 min. All patients had longer than 2-h tourniquets. There were 30 patients with an uninterrupted 3-h tourniquet time without deflation. 43% of these patients had a major nerve palsy as compared to 7.7% palsies in the whole group. Reperfusion with deflation of tourniquet for longer than 30 min was associated with lower incidence of nerve palsy. 100% of tibial nerve 89% of common peroneal nerve palsies recovered fully.
A systematic review done by Fitzgibbons et al.14 mentions that high quality studies with tourniquet time more than 120 min confirm that short term changes such as muscle atrophy and electrophysiological changes do not result in long term dysfunction. Essentially, there is no strong evidence to stop the individual surgeon from using tourniquets for longer than the standard 2 h if required.
A challenging procedure such as a multi-joint fusion or a revision ankle replacement will have prolonged surgical time. A tourniquet deflation interval can be used in such situations, but the benefits of the reperfusion period are not clear. Mohler et al.15 found no reduction in nerve injury with reperfusion in a rabbit model and Concannon et al.16 suggested possible increase in damage to tissues with reperfusion breaks whereas findings of a study by Sapega et al.17 on canine limbs supports intermittent tourniquet deflation. Horlocker et al. found benefits of tourniquet deflation in reducing the risk of nerve palsy. Due to the conflicting evidence, surgeons must decide on tourniquet deflation weighing the risks of loss of the bloodless field and further prolongation of an already complex surgery versus risks of tourniquet complications.
There is limited literature relating to tourniquet use in foot and ankle surgery and the focus has been on fracture fixation surgery. Konrad et al.18 studied ankle fracture fixation with and without tourniquet and found increased pain and swelling and reduced ankle range of movements in patients who had tourniquet-controlled surgery compared to the control group. However, the maximum time of bloodless field in these studies was 90 min. Kukreja et al.19 found increased opioid use in a group of patients who had foot and ankle surgeries with tourniquet times longer than 90 min compared to those who had less than 90-min tourniquets. Within our group of patients, we did not observe a trend of increasing opioid demand in the post-operative period with increasing tourniquet time. However, the usage of opioids was higher in patients who had a fusion procedure than in those who had an arthroplasty. The significance of these findings is not known because of the lack of a comparative age, ASA and procedure matched cohort of patients with shorter tourniquet times.
The main finding of our case series of 20 patients was that the complication rate is lower than rates in previous studies with comparable tourniquet times. No major nerve palsies occurred in this series compared to the study by Horlocker et al. There were early problems such as transient sensory changes and delayed wound healing, but these resolved completely. Olivecrona et al. reported 21% superficial infections within the group of 268 patients who had longer than 100-min tourniquets. The corresponding number in our series is one (5%) superficial infection. Non-union was a major complication in two patients one of whom had an infected non-union. Both patients had extensive fusions (femoral head allograft used in one) and the risks of non-union were high regardless of tourniquet duration. Non-union rate is reported to be as high as 50% following tibiotalocalacaneal arthrodesis surgeries with bulk femoral graft (Jeng et al.20).
Being aware of the potential for serious tourniquet complications, orthopaedic surgeons do try to keep to the accepted safe tourniquet time but there are factors that can cause them to go beyond this limit. The surgical procedure being complex and intra-operative complications are possible scenarios where this can happen. The risk versus benefit of extending the tourniquet time needs to be considered by the surgeon in each case.
This study has the limitations of being a retrospective case series and statistically valid inferences cannot be made based on the findings, but the low rate of major complications in this group of patients is an important finding. This does underscore our lack of understanding of the safe tourniquet times for foot and ankle surgery. There is a paucity of studies specific to foot and ankle surgery and all findings of knee centric studies probably cannot be extrapolated. That said, we would like to emphasise that the authors do not intend to suggest that breaching the 2-h tourniquet time limit is safe practice. The current recommendations regarding tourniquet use need to be adhered to as far as possible.
Further investigation, possibly with multi-centre studies and combined databases might help shed more light on clinical consequences of prolonged tourniquet use in foot and ankle surgery.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declarations of interest
None.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Contributor Information
Rohit Gangadharan, Email: Rohit.Gangadharan@uhs.nhs.uk.
Charline Roslee, Email: Charline.Roslee@uhd.nhs.uk.
Nichola Kelsall, Email: Nikki.Kelsall@uhd.nhs.uk.
Heath Taylor, Email: Heath.Taylor@uhd.nhs.uk.
References
- 1.Heppenstall R.B., Balderston R., Goodwin C. Pathophysiologic effects distal to a tourniquet in the dog. J Trauma. 1979;19(4):234–238. doi: 10.1097/00005373-197904000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Patterson S., Klenerman L. The effect of pneumatic tourniquets on the ultrastructure of skeletal muscle. J BoneJoint Surg Br. 1979;61(2):178–183. doi: 10.1302/0301-620X.61B2.108286. [DOI] [PubMed] [Google Scholar]
- 3.Ochoa J., Fowler T.J., Gilliatt R.W. Anatomical changes in peripheral nerves compressed by a pneumatic tourniquet. J Anat. 1972;113(pt 3):433–455. [PMC free article] [PubMed] [Google Scholar]
- 4.Rorabeck C.H. Tourniquet-induced nerve ischemia: an experimental investigation. J Trauma. 1980;20(4):280–286. doi: 10.1097/00005373-198004000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Pedowitz R.A. Tourniquet-induced neuromuscular injury: a recent review of rabbit and clinical experiments. Acta Orthop Scand Suppl. 1991;245:1–33. [PubMed] [Google Scholar]
- 6.Dobner J.J., Nitz A.J. Postmeniscectomy tourniquet palsy and functional sequelae. Am J Sports Med. 1982;10(4):211–214. doi: 10.1177/036354658201000404. [DOI] [PubMed] [Google Scholar]
- 7.Clarke M.T., Longstaff L., Edwards D., Rushton N. Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg Br. 2001;83(1):40–44. doi: 10.1302/0301-620x.83b1.10795. [DOI] [PubMed] [Google Scholar]
- 8.Hirota K., Hashimoto H., Kabara S. The relationship between pneumatic tourniquet time and the amount of pulmonary emboli in patients undergoing knee arthroscopic surgeries. Anesth Analg. 2001;93(3):776–780. doi: 10.1097/00000539-200109000-00044. [DOI] [PubMed] [Google Scholar]
- 9.Kokki H., Väätäinen U., Miettinen H., Parviainen A., Könönen M., Partanen J. Tourniquet-induced enmg changes in arthroscopic anterior cruciate ligament reconstruction: a comparison of low and high-pressure tourniquet systems. Ann Chir Gynaecol. 2000;89(4):313–317. [PubMed] [Google Scholar]
- 10.Olivecrona C., Lapidus L.J., Benson L., Blomfeldt R. Tourniquet time affects postoperative complications after knee arthroplasty. Int Orthop. 2013;37:827–832. doi: 10.1007/s00264-013-1826-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horlocker T.T., Hebl J.R., Gali B. Anesthetic, patient, and surgical risk factors for neurologic complications after prolonged total tourniquet time during total knee arthroplasty. Anesth Analg. 2006;102(3):950–955. doi: 10.1213/01.ane.0000194875.05587.7e. [DOI] [PubMed] [Google Scholar]
- 12.Wakai A., Winter D.C., Street J.T., Redmond P.H. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2001;9:345–351. doi: 10.5435/00124635-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Lin L., Wang L., Bai Y. Pulmonary gas exchange impairment following tourniquet deflation: a prospective, single-blind clinical trial. Orthopedics. 2010;33(6):395. doi: 10.3928/01477447-20100429-15. [DOI] [PubMed] [Google Scholar]
- 14.Fitzgibbons P.G., Digiovanni C., Hares S., Akelman E. Safe tourniquet use: a review of the evidence. J Am Acad Orthop Surg. 2012;20:310–319. doi: 10.5435/JAAOS-20-05-310. [DOI] [PubMed] [Google Scholar]
- 15.Mohler L.R., Pedowitz R.A., Myers R.R., Ohara W.M., Lopez M.A., Gershuni D.H. Intermittent reperfusion fails to prevent posttourniquet neurapraxia. J Hand Surg Am. 1999;24(4):687–693. doi: 10.1053/jhsu.1999.0687. [DOI] [PubMed] [Google Scholar]
- 16.Concannon M.J., Kester C.G., Welsh C.F., Puckett C.L. Patterns of free-radical production after tourniquet ischemia: implications for the hand surgeon. Plast Reconstr Surg. 1992;89(5):846–852. doi: 10.1097/00006534-199205000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Sapega A.A., Heppenstall R.B., Chance B., Park Y.S., Sokolow D. Optimizing tourniquet application and release times in extremity surgery: a biochemical and ultrastructural study. J Bone Joint Surg Am. 1985;67(2):303–314. [PubMed] [Google Scholar]
- 18.Konrad G., Markmiller M., Lenich A., Mayr E., Rüter A. Tourniquets may increase postoperative swelling and pain after internal fixation of ankle fractures. Clin Orthop Relat Res. 2005;433:189–194. doi: 10.1097/01.blo.0000151849.37260.0a. [DOI] [PubMed] [Google Scholar]
- 19.Kukreja P., Lehtonen E., Pinto M.C., Patel H.A., McKissack H.M., Shah A. Postoperative tourniquet pain in patients undergoing ffot and ankle surgery. Cureus. 2018 Dec;10(12):e3678. doi: 10.7759/cureus.3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeng C.L., Campbell J.T. Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int. 2013;34(9):1256–1266. doi: 10.1177/1071100713488765. [DOI] [PubMed] [Google Scholar]