Significance Statement
Percutaneous coronary intervention is linked with greater risk of AKI incidence; however, differences in this link by race remain less clear. This study quantified the association of race (White, Black, or other) with odds for AKI incidence within 7 days after percutaneous coronary intervention. After adjustment for demographics, comorbidities, medications, and procedural characteristics, the study found that, compared with Whites, odds for AKI incidence were substantially greater among Black but not other patients. Racial difference in odds for AKI incidence after percutaneous coronary intervention did not differ by baseline kidney function. These findings highlight the need to investigate factors that predispose Black individuals to greater risk for AKI after percutaneous coronary intervention.
Keywords: acute kidney injury, African Americans, racial disparities, percutaneous coronary intervention
Abstract
Background
Undergoing percutaneous coronary intervention (PCI) is a risk factor for AKI development, but few studies have quantified racial differences in AKI incidence after this procedure.
Methods
We examined the association of self-reported race (Black, White, or other) and baseline eGFR with AKI incidence among patients who underwent PCI at Duke University Medical Center between January 1, 2003, and December 31, 2013. We defined AKI as a 0.3 mg/dl absolute increase in serum creatinine within 48 hours, or ≥1.5-fold relative elevation within 7 days post-PCI from the reference value ascertained within 30 days before PCI.
Results
Of 9422 patients in the analytic cohort (median age 63 years; 33% female; 75% White, 20% Black, 5% other race), 9% developed AKI overall (14% of Black, 8% of White, 10% of others). After adjustment for demographics, socioeconomic status, comorbidities, predisposing medications, PCI indication, periprocedural AKI prophylaxis, and PCI procedural characteristics, Black race was associated with increased odds for incident AKI compared with White race (odds ratio [OR], 1.79; 95% confidence interval [95% CI], 1.48 to 2.15). Compared with Whites, odds for incident AKI were not significantly higher in other patients (OR, 1.30; 95% CI, 0.93 to 1.83). Low baseline eGFR was associated with graded, higher odds of AKI incidence (P value for trend <0.001); however, there was no interaction between race and baseline eGFR on odds for incident AKI (P value for interaction = 0.75).
Conclusions
Black patients had greater odds of developing AKI after PCI compared with White patients. Future investigations should identify factors, including multiple domains of social determinants, that predispose Black individuals to disparate AKI risk after PCI.
AKI, or the sudden loss of kidney function, carries a threat of adverse outcomes that can persist over a life course. These include higher long-term risk for mortality, incidence of cardiovascular disease, persistent loss of kidney function, progression of kidney dysfunction to ESKD, and development of recurrent AKI.1,2 Rates of AKI are increasing, the reasons for which are multifactorial and related to an aging population and improved detection through the emergence of electronic health record data.1,3 However, with the emergence of better AKI detection, inequities in the frequency of AKI among racial and ethnic minorities compared with Whites are becoming increasingly apparent. This racial difference in AKI occurrence is evident in the general population,4 and among high-risk subgroups such as hospitalized patients with diabetes,5 stroke,6 or liver disease.7
Percutaneous coronary intervention (PCI) is an additional risk factor for AKI,8 and development of AKI after PCI portends risk for long-term unfavorable health consequences.9,10 Recent literature suggest racial susceptibility in risk for AKI after PCI exists, with a disproportionate risk in Black compared with White patients.11 However, the magnitude of this racial inequity and the underlying causes of the excess AKI risk in Black patients remain less clear. Specifically, few studies have investigated the predisposing role of comorbidities (e.g., diabetes and cardiovascular disease), standard periprocedural care related to AKI risks (e.g., contrast volume), and socioeconomic stressors on racial disparities in AKI incidence post-PCI.
We aimed to quantify the independent association of race with AKI incidence after PCI using detailed clinical data available in the Duke Databank for Cardiovascular Disease. This unique data resource allowed for the comprehensive assessment of relevant individual and procedural characteristics, including demographics, socioeconomic status, comorbidities, pre-PCI medication use, indication for PCI, periprocedural AKI prophylaxis, and PCI procedural characteristics.
Methods
Study Design and Population
The Duke Databank for Cardiovascular Disease is a clinical care database comprising all patients who underwent cardiac catherization and cardiac surgery at Duke University Medical Center in Durham, North Carolina. Data collection began in 1974 and completed in 2014. A detailed description of the databank, including its data acquisition process, is available elsewhere.12 Briefly, the Duke Databank for Cardiovascular Disease prospectively documented clinical and laboratory data related to clinical care for all eligible cardiac procedural patient encounters using standardized case report forms. At enrollment, house staff completed intake forms for patients to capture baseline data, which were validated by cardiology providers.
For this study, we included patients who underwent PCI between January 1, 2003 and December 31, 2013, and had data for the assessment of race and AKI incidence post-PCI. This time period was chosen as it includes the most recent data available in the Duke Databank for Cardiovascular Disease that would allow at least 1-year follow-up for outcomes after PCI. We excluded patients who were below 18 years of age or were on chronic dialysis at the time of PCI. We further restricted analysis to the first PCI procedure within the study period for patients with multiple eligible PCI procedures. The study was reviewed by the Duke Institutional Review Board (Pro00080787).
Primary Exposure: Self-Reported Race
Available race categories in the Duke Databank for Cardiovascular Disease include Black, White, Native American, or “other” based on patients’ self-report. Of note, ethnicity was not captured in this database. Due to a small number of patients who reported race as Native American (n=270, 3%) and “other” categories (n=214, 2%), these groups were combined to comprise the “other” category in our analysis. Therefore, our final race categories were Black, White, and other.
Definition of AKI
The primary outcome for this study was AKI incidence, defined based on the Kidney Disease Improving Global Outcomes (KDIGO) criteria as a 1.5-fold or greater relative elevation in serum creatinine from the reference value to the highest value within 7 days after the date and time of PCI, or a 0.3 mg/dl absolute increase in serum creatinine from the reference value within 48 hours after the date and time of PCI.13 The reference value was the average of all serum creatinine measurements obtained in an outpatient or inpatient setting within 30 days before PCI; the median number of serum creatinine measurements available per patient was two (interquartile range (IQR), 1–3), and it was similar by race (Supplemental Table 1). We considered the date of PCI as time zero for the 7-day window for ascertainment of peak elevation in serum creatinine post-PCI.
We assessed additional AKI classifications per the KDIGO clinical guidelines13 as secondary endpoints, including AKI severity, AKI requiring dialysis, and contrast-induced nephropathy. We used KDIGO guidelines to quantify AKI severity into stages 1–3 based on the degree of elevation in serum creatinine from the reference to the highest value within 14 days post-PCI. Stage 1: 1.5–1.9-fold or 0.3–3.9 mg/dl absolute increase; stage 2: 2–2.9-fold; and stage 3: ≥ three-fold, or ≥4 mg/dl absolute increase or initiation of dialysis.13 We defined AKI requiring dialysis using inpatient dialysis procedure codes as receipt versus no receipt of dialysis within 14 days of PCI in a patient with AKI. We defined contrast-induced nephropathy as ≥0.5 mg/dl absolute elevation in serum creatinine from the reference value within 7 days after PCI.13
Assessment of Covariates
We included demographics, comorbidities, medication use, indication for PCI, periprocedural AKI prophylaxis and PCI procedural characteristics, and socioeconomic variables in our models as adjustment covariates for the association between race and AKI incidence. These individual and procedural data were prospectively captured using the intake forms that were completed for each patient encounter by the clinical care team at the initial workup and subsequent course of cardiovascular care, including catheterization.12 Demographics included sex, male versus female, and age, continuous in years. Comorbidities included tobacco use; body mass index, continuous in kg/m2; pre-existing cardiovascular disease (history of acute coronary syndrome, angina, congestive heart failure, myocardial infarction [MI], cerebrovascular disease, peripheral vascular disease, carotid bruits, prior PCI), hyperlipidemia, diabetes, and diabetes with end-organ damage based on presence of nephropathy, retinopathy, neuropathy, gastroparesis, or peripheral vascular disease. Glycated hemoglobin A1c was unavailable for the majority of patients (n=5982; 63%) and was not included. Medication use included renin-angiotensin-aldosterone system (RAAS) inhibitors, nonsteroidal anti-inflammatory drugs, and diuretics within 30 days before PCI. Indication for PCI included possible categories of acute coronary status: no acute coronary syndrome, ST-elevation MI, non-ST–elevation MI, MI unspecified, or unstable angina. Periprocedural AKI prophylaxis included periprocedural intravascular fluid administration and use of N-acetylcysteine within 24 hours of PCI. Although N-acetylcysteine is no longer recommended for AKI prophylaxis due to lack of effect,14 its use during the timeframe of this study serves as a proxy for recognition of elevated AKI risk and was thus included. Procedural characteristics included year of PCI; setting of PCI: elective versus nonelective (urgent or emergent); number of stents placed; contrast volume; and systolic and diastolic BP, continuous in mm Hg.
Socioeconomic variables included as adjustment covariates were marital status and median household income. Marital status was assessed using the clinic intake forms and was categorized into married or life partner versus other (single, separated, divorced, widowed, or unknown) as adjustment for social support. Median household income was defined at the US Census Block Group (neighborhood) level and ascertained through linkage of the Duke Databank of Cardiovascular Disease to the American Community Survey 2007–2011. Detailed methodology for ascertainment of neighborhood-level median household income is described elsewhere.15 We modeled median household income as a continuous variable in the analysis.
Baseline eGFR was calculated from serum creatinine data using the Chronic Kidney Disease Epidemiology Collaboration equation. We a priori sought to utilize outpatient serum creatinine data obtained between 6 months and up to 30 days before PCI to calculate eGFR as the primary approach. However, this approach was feasible in only 1957 (21%) patients due to creatinine unavailability; therefore, we used the reference serum creatinine value described above under the AKI definition to calculate baseline eGFR in the analysis.
Statistical Analyses
Patient characteristics at the time of PCI are described by race using counts and proportions for categorical variables and medians with IQR for continuous variables; differences in patient characteristics, including incidence and severity of AKI, by race were compared using chi-squared tests for discrete variables and Kruskal-Wallis tests for continuous variables. We employed logistic regression models, adjusted for potential confounders, to estimate associations of race and baseline eGFR with odds of incident AKI in the primary analysis. Missing data were imputed using multiple imputation for the following variables: median household income (15% missing), diastolic BP (7%), and systolic BP (6%). All other variables with 5% or lower rate of missingness were imputed using median imputation. We tested model assumptions, and although we had a priori sought to implement spline transformations to model nonlinear associations on the log-odds scale for continuous covariates, this was unnecessary as the linearity assumption was not violated. For illustrative purposes, we obtained final model results with baseline eGFR categorized as ≥90, 60 to <90, 30 to <60, 15 to <30, and <15 ml/min per 1.73 m2.
In a sensitivity analysis, we added an interaction term between race and baseline eGFR to the above primary models to assess interactions between these two risk factors on AKI incidence. Additionally, we used a complete-case analysis that did not feature imputation for missing data to determine if our findings were robust to missingness. All hypothesis tests were two sided at the 5% significance level. We used SAS software, Version 9.4 (SAS Institute, Cary, NC) for all analyses.
Results
Baseline Characteristics of Patients
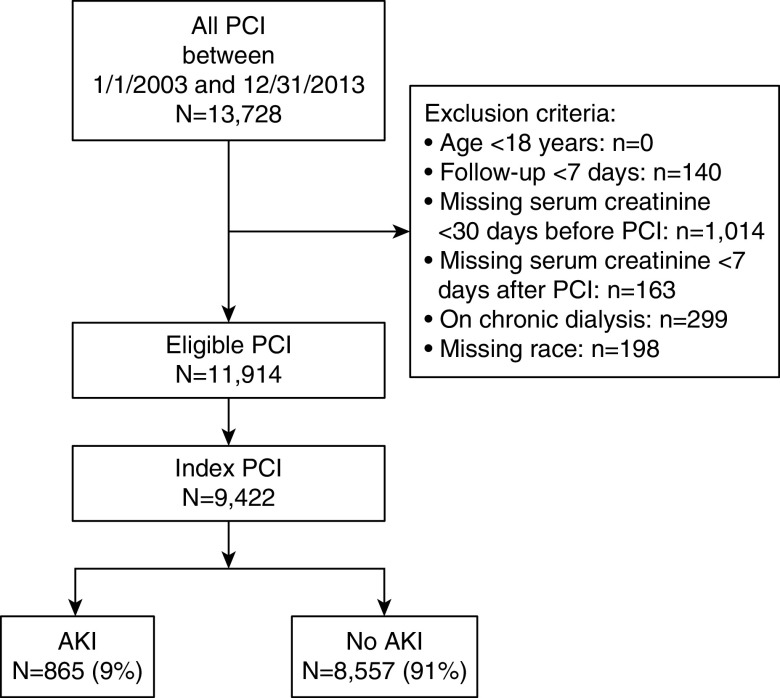
Of 13,728 PCI procedures between January 1, 2003 and December 31, 2013, 9422 unique patient encounters met the inclusion criteria (Figure 1). Of the 9422 included patients, 75% were White, 20% Black, and 5% other; the median age was 63 years (IQR, 54–72), and 45% had a history of tobacco use. Median age was 64 years among White patients; 60 years among Black patients; and 60 years among other patients. Only 30% of White patients versus 44% of Black patients were women (Table 1).
Figure 1.
Flow chart describing derivation of analytic cohort based on inclusion criteria and availability of required data.
Table 1.
Baseline characteristics of patients stratified by race
| Covariates | Overall, n=9422 | Race | |||
|---|---|---|---|---|---|
| White, n=7084 | Black, n=1854 | Other, n=484 | P Value | ||
| Demographics and socioeconomic variables | |||||
| Sex: women, n/N (%) | 3097/9422 (33) | 2127/7084 (30) | 820/1854 (44) | 150/484 (31) | <0.001 |
| Age, yr, N, median, (Q1, Q3) | 9422, 63 (54, 72) | 7084, 64 (55, 73) | 1854, 60 (51, 69) | 484, 60 (52, 68) | <0.001 |
| Marital status, n/N (%) | <0.001 | ||||
| Married or life-partner | 6355/9377 (68) | 5013/7051 (71) | 1015/1848 (55) | 327/478 (68) | |
| Othera | 3022/9377 (32) | 2038/7051 (29) | 833/1848 (45) | 151/478 (32) | |
| Median household income scaled in US$1000, N, median, (Q1, Q3) | 8048, 45 (33, 61) | 6123, 46 (36, 63) | 1528, 37 (26, 48) | 397, 37 (27, 58) | <0.001 |
| Comorbidities | |||||
| Tobacco use, n/N (%) | 4244/9422 (45) | 3247/7084 (46) | 782/1854 (42) | 215/484 (44) | 0.02 |
| BMI, kg/m2, N, median, (Q1, Q3) | 9384, 29 (25, 33) | 7059, 29 (25, 32) | 1842, 29 (26, 34) | 483, 28 (25, 32) | <0.001 |
| Pre-existing CVD, n/N (%) | |||||
| Congestive heart failure | 1592/9316 (17) | 1201/7006 (17) | 318/1835 (17) | 73/475 (15) | 0.58 |
| Cerebrovascular disease | 802/9422 (9) | 614/7084 (9) | 146/1854 (8) | 42/484 (9) | 0.55 |
| Myocardial infarction | 4631/9422 (49) | 3376/7084 (48) | 990/1854 (53) | 265/484 (55) | <0.001 |
| PVD | 756/9422 (8) | 586/7084 (8) | 131/1854 (7) | 39/484 (8) | 0.24 |
| Hyperlipidemia, n/N (%) | 5866/9422 (62) | 4542/7084 (64) | 1040/1854 (56) | 284/484 (59) | <0.001 |
| Diabetes, n/N (%) | 2804/9422 (30) | 1921/7084 (28) | 715/1854 (39) | 168/484 (35) | <0.001 |
| Diabetes with end organ damage, n/N (%) | 159/9422 (1.7) | 111/7084 (1.6) | 40/1854 (2.2) | 8/484 (1.7) | 0.21 |
| HBA1c, %, N, median, (Q1, Q3) | 3440, 6.3 (5.8, 7.4) | 2441, 6.2 (5.7, 7.2) | 810, 6.5 (5.9, 8.1) | 189, 6.3 (5.8, 7.6) | <0.001 |
| Baseline eGFR, ml/min per 1.73 m2, N, median, (Q1, Q3) | 9422, 74 (57, 89) | 7084, 73 (56, 88) | 1854, 78 (58, 97) | 484, 78 (60, 93) | <0.001 |
| Medication use, n/N (%) | |||||
| RAAS inhibitors | 4352/9422 (46) | 3193/7084 (45) | 929/1854 (50) | 230/484 (48) | <0.001 |
| Diuretics | 1976/9422 (21) | 1428/7084 (20) | 470/1854 (25) | 78/484 (16) | <0.001 |
| NSAIDs | 4920/9422 (52) | 3625/7084 (51) | 1040/1854 (56) | 255/484 (53) | <0.001 |
| Indication for PCI, n/N (%) | |||||
| Acute coronary status | 6328/9422 (67) | 4632/7084 (65) | 1343/1854 (72) | 353/484 (73) | <0.001 |
| STEMI | 1987/9422 (21) | 1403/7084 (20) | 473/1854 (26) | 111/484 (23) | |
| Non-STEMI | 1682/9422 (18) | 1174/7084 (17) | 394/1854 (21) | 114/484 (24) | |
| MI unspecified | 18/9422 (0.2) | 15/7084 (0.2) | 1/1854 (0.2) | 2/484 (0.4) | |
| Unstable angina | 2641/9422 (28) | 2040/7084 (29) | 475/1854 (26) | 126/484 (26) | |
| Peri-procedural AKI prophylaxis, n/N (%) | |||||
| IV fluid administration | 9047/9422 (96) | 6805/7084 (96) | 1780/1854 (96) | 462/484 (96) | 0.15 |
| N-Acetylcysteine use | 153/9422 (2) | 117/7084 (2) | 30/1854 (2) | 6/484 (1) | 0.63 |
| PCI procedural characteristics | |||||
| yr of index PCI, n/N (%) | 0.003 | ||||
| 2003–2005 | 4022/9422 (43) | 3043/7084 (43) | 746/1854 (40) | 233/484 (48) | |
| 2006–2008 | 2515/9422 (27) | 1864/7084 (26) | 510/1854 (28) | 141/484 (29) | |
| 2009–2011 | 1735/9422 (18) | 1308/7084 (19) | 360/1854 (19) | 67/484 (14) | |
| 2012–2013 | 1150/9422 (12) | 869/7084 (12) | 238/1854 (13) | 43/484 (9) | |
| PCI setting: nonelective | 3027/9422 (32) | 2179/7084 (31) | 682/1854 (37) | 166/484 (34) | <0.001 |
| Contrast volume, ml, N, median, (Q1,Q3) | 9353, 250 (190, 335) | 7030, 250 (190, 335) | 1843, 240 (180, 325) | 480, 250 (190, 325) | 0.005 |
| No. of stents placed, n/N (%) | 0.07 | ||||
| 0 | 326/9378 (4) | 243/7043 (4) | 68/1852 (4) | 15/483 (3) | |
| 1 | 5509/9378 (59) | 4077/7043 (58) | 1149/1852 (62) | 283/483 (59) | |
| 2 | 2285/9378 (24) | 1755/7043 (25) | 410/1852 (22) | 120/483 (25) | |
| 3 | 842/9378 (9) | 638/7043 (9) | 153/1852 (8) | 51/483 (11) | |
| 4 | 305/9378 (3) | 244/7043 (4) | 50/1852 (3) | 11/483 (2) | |
| 5–8 | 111/9378 (1) | 86/7043 (1) | 22/1852 (1) | 3/483 (1) | |
| Systolic BP, mm Hg, N, median, (Q1, Q3) | 8874, 141 (127, 160) | 6670, 140 (126, 158) | 1754, 146 (131, 166) | 450, 141 (126, 159) | <0.001 |
| Diastolic BP, mm Hg, N, median, (Q1, Q3) | 8775, 81 (72, 90) | 6598, 80 (72, 89) | 1730, 85 (76, 95) | 447, 82 (74, 91) | <0.001 |
BMI, body mass index; CVD, cardiovascular disease; PVD, peripheral vascular disease; STEMI, ST-elevation myocardial infarction; NSAIDs, nonsteroidal anti-inflammatory drugs; IV, intravenous.
Other includes single, separated, divorced, widowed, or unknown.
Neighborhood-level median household income was lower among Black ($36,761 [IQR, 26,333–48,268]) compared with White patients ($46,319 [IQR, 35,673–63,329]). Black patients were also less likely to report being married or having a life partner (55%) compared with White (71%) or other patients (68%) (Table 1).
Diabetes and hypertension were more prevalent among Black than White and other patients (diabetes: 39%, 28%, and 35%; hypertension: 76%, 69%, 70%, among Black, White, and others, respectively). Baseline eGFR was higher among Black patients and other patients than White patients (median eGFR: 78, 72, and 79 ml/min per 1.73 m2 among Black, White, and others, respectively). Use of RAAS inhibitors was 50% among Black patients, 45% among Whites, and 48% among Other patients (Table 1).
At presentation for PCI, 72% (n=1343) of Black patients had acute coronary syndrome compared with 65% (n=4632) of White patients, and 73% (n=353) of other patients. Administration of intravenous fluids and N-acetylcysteine, and number of stents placed were similar by race. However, Black patients had higher systolic and diastolic BP at the time of PCI versus their nonBlack counterparts (median systolic BP: 146, 140, and 141 mm Hg, and median diastolic BP: 85, 80, and 80 mm Hg in Black, White, and other patients, respectively). Black patients (37%) were also more likely to undergo nonelective PCI compared with White (31%) or other patients (34%) (Table 1).
Incidence of AKI by Race and Baseline eGFR
Overall, 9% (n=865) of patients developed AKI within 7 days after PCI. Of these, 77% (n=662) had AKI stage 1, 11% (n=96) had AKI stage 2, and 12% (n=107) had AKI stage 3. Only 8% (n=66) of the 865 patients who developed AKI required dialysis within 14 days after PCI. Incidence of contrast-induced nephropathy within 7 days after PCI was 6% (531 of 9422) overall (Table 2).
Table 2.
AKI incidence after PCI by race and baseline eGFR
| AKI Outcomes, n/N (%) | Overall, n=9422 | Race | |||
|---|---|---|---|---|---|
| White, n=7084 | Black, n=1854 | Other, n=484 | P Value | ||
| AKI incidence | 865/9422 (9) | 561/7084 (8) | 258/1854 (14) | 46/484 (10) | <0.001 |
| By baseline eGFR, ml/min per 1.73 m2 | NA | ||||
| ≥90 | 127/2227 (6) | 67/1471 (5) | 52/611 (9) | 8/145 (6) | |
| 60 to <90 | 237/4439 (5) | 158/3472 (5) | 66/750 (9) | 13/217 (6) | |
| 30 to <60 | 358/2396 (15) | 261/1909 (14) | 79/384 (21) | 18/103 (18) | |
| 15 to <30 | 83/248 (34) | 49/180 (27) | 31/56 (55) | 3/12 (25) | |
| <15 | 60/112 (54) | 26/52 (50) | 20/53 (57) | 4/7 (57) | |
| Incidence of other AKI classifications | |||||
| AKI severitya | 0.17 | ||||
| Stage 1 | 662/865 (77) | 441/561 (79) | 188/258 (73) | 33/46 (72) | |
| Stage 2 | 96/865 (11) | 62/561 (11) | 28/258 (11) | 6/46 (13) | |
| Stage 3 | 107/865 (12) | 58/561 (10) | 42/258 (16) | 7/46 (15) | |
| AKI requiring dialysis | 66/865 (8) | 34/561 (6) | 27/258 (11) | 5/46 (11) | 0.05 |
| Contrast-induced nephropathy | 531/9422 (6) | 344/7084 (5) | 160/1854 (9) | 27/484 (6) | <0.001 |
NA means the P value for interaction between race and baseline eGFR on AKI incidence is reported in Table 3.
AKI definitions are based on the KDIGO criteria as follows:
⋅ AKI: a 1.5-fold or greater relative elevation in serum creatinine from a reference value to the highest value within 7 d after PCI. The reference value was the average of all serum creatinine measurements obtained in an outpatient or inpatient setting within 30 d before PCI; and the date of PCI was time zero for the 7-d window.
⋅ AKI severity: stages 1–3 based on the degree of elevation in serum creatinine to the highest value within 14 d post-PCI. Stage 1: 1.5–1.9-fold or 0.3–3.9 mg/dl absolute increase; stage 2: 2–2.9-fold; and stage 3: ≥ three-fold or ≥4 mg/dl absolute increase or initiation of dialysis.
⋅ AKI requiring dialysis: based on dialysis procedure codes obtained from inpatient settings, and defined as receipt versus no receipt of dialysis in a patient with AKI.
⋅ Contrast-induced nephropathy: ≥0.5 mg/dl absolute elevation in serum creatinine from the reference value within 7 d after PCI.
Denominator for AKI severity is number of incident AKI (n=865 overall).
AKI incidence was higher among Black (14%, n=258) than White (8%, n=561) or other patients (10%, n=46); P<0.001. Compared with Whites, Black patients with AKI had greater, albeit NS, incidence of AKI stage 3 (16% Black; 10% White), and AKI requiring dialysis (11% Black; 6% White). Incidence of contrast-induced nephropathy was 9% (n=160) among Black patients, 5% (n=344) among White patients, and 6% (n=27) among other patients; P<0.001 (Table 2).
AKI incidence was higher at lower baseline eGFR categories. Compared with patients with eGFR ≥90 ml/min per 1.73 m2 (6%, n=127), AKI incidence was 5% (n=239) among those with eGFR 60 to 90; 15% (n=358) in the eGFR 30 to 60 subgroup; 35% (n=84) among those with eGFR 15 to <30; and 55% (n=57) among those with eGFR <15 ml/min per 1.73 m2 (P value for trend <0.001) (Table 2).
Associations of Race and Baseline eGFR with AKI Incidence
After adjustment for demographics, socioeconomic status, comorbidities, medications, PCI indication, periprocedural AKI prophylaxis, and PCI procedural characteristics, Black patients had greater odds of AKI incidence compared with White patients: odds ratio (OR) 1.79; 95% confidence interval (95% CI), 1.48 to 2.15. Odds of AKI incidence in other patients was higher, but NS, compared with that in White patients: OR, 1.30; 95% CI, 0.93 to 1.83 (Table 3).
Table 3.
Association of race and baseline eGFR with odds of incident AKI post-PCI
| Variables | Incident AKI | ||
|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | P Value | |
| No. of events/no. of patients | 865/9422 | ||
| Race | <0.001 | ||
| White | Reference | Reference | |
| Black | 1.79 | 1.48 to 2.15 | |
| Other | 1.30 | 0.93 to 1.83 | |
| Baseline eGFR, ml/min per 1.73 m2 | <0.001 | ||
| ≥90 | Reference | Reference | |
| 60 to <90 | 0.90 | 0.71 to 1.14 | |
| 30 to <60 | 2.29 | 1.77 to 2.97 | |
| 15 to <30 | 5.77 | 3.96 to 8.41 | |
| <15 | 15.71 | 9.97 to 24.77 | |
| Interaction of race and baseline eGFR | NA | NA | 0.75 |
AKI is defined as a 1.5-fold or greater relative elevation in serum creatinine from a reference value to the highest value within 7 d after PCI or a 0.3 mg/dl absolute increase in serum creatinine from the reference value within 48 h after the date and time of PCI.
Baseline eGFR, calculated from serum creatinine using the Chronic Kidney Disease Epidemiology Collaboration equation.
Additional model covariates include demographics: yr of index PCI; sex (male versus female); age; tobacco use. PCI procedural characteristics: PCI setting (elective versus nonelective); number of stents placed; contrast volume; systolic and diastolic BP, mm Hg. Medication use: RAAS inhibitors, diuretics, and nonsteroidal anti-inflammatory drugs. Periprocedural AKI prophylaxis: administration of intravascular fluid and N-acetylcysteine. Comorbidities: body mass index, kg/m2; acute coronary status pre-CATH (ST-elevation myocardial infarction (STEMI), non-STEMI, MI unspecified, unstable angina); pre-existing cardiovascular disease (prior MI, prior PCI, prior coronary artery bypass grafting, history of angina, congestive heart failure, cerebrovascular disease, peripheral vascular disease, carotid bruits); history of hyperlipidemia; diabetes and diabetes with end organ damage. Socioeconomic status: marital status (married or life partner versus other); median household income.
OR, 95% CIs, and P values for race and baseline eGFR are from a main effects model. The interaction P value is from a model incorporating a crossproduct of AKI with baseline eGFR.
Low baseline eGFR was significantly associated with graded, higher odds of AKI incidence (P value for trend <0.001). Compared with eGFR ≥90 ml/min per 1.73 m2, OR for AKI incidence was 0.90 (95% CI, 0.71 to 1.14) in eGFR 60 to <90 subgroup; 2.29 (95% CI, 1.77 to 2.97) in eGFR 30 to <60; 5.77 (95% CI, 3.96 to 8.41) in eGFR 15 to <30; and 15.71 (95% CI, 9.97 to 24.77) in the eGFR <15 ml/min per 1.73 m2 subgroup (Table 3).
Sensitivity Analysis
There was no interaction between race and baseline eGFR on odds for incident AKI (P value for interaction = 0.75) (Table 3). Results remained generally unchanged in a complete-case analysis that did not feature correction for missing data (Supplemental Table 2).
Discussion
In this large cohort of patients who underwent PCI at a single institution between 2003 and 2013, the odds of AKI incidence after the procedure were about 80% greater in Black compared with White individuals. Low baseline eGFR was also associated with graded, higher odds for AKI incidence postprocedure. These associations persisted after adjustment for demographics, comorbidities (e.g., diabetes and cardiovascular disease), medication use (RAAS inhibitors, diuretics, and nonsteroidal anti-inflammatory drugs), indication for the procedure, periprocedural AKI prophylaxis (e.g., administration of intravenous fluids and N-acetylcysteine), procedural characteristics (e.g., elective versus nonelective PCI, number of stents placed, contrast volume, and BP), and socioeconomic variables. There was no interaction between race and baseline eGFR on odds for AKI incidence. These data support the need for interventions to mitigate racial susceptibility to AKI incidence among high-risk patients undergoing PCI.
PCI is an established risk for AKI development. AKI incidence after PCI in the general population is estimated at approximately 7%,8,9,11,16 but reports range from 3% to 20%. Key risk factors for AKI development post-PCI include pre-existing comorbidities (e.g., kidney dysfunction, diabetes, and cardiovascular disease) and periprocedural contrast exposure and volume depletion. Given the frequency of this adverse event, prevention of postprocedural AKI has become the focus of many recent and ongoing initiatives. These include risk stratification for AKI using clinical prediction tools–18; minimizing contrast exposure19; volume expansion19; optimizing arterial access site20; administration of N-acetylcysteine21; and institution of a care bundle that addresses multiple AKI risk factors.22,23 Despite overall reductions in AKI incidence post-PCI consequent to these measures focused on known risk factors,19 emerging work is suggestive of racial differences in susceptibility to post-PCI AKI.
One prior study by Kobayashi et al.11 quantified differences in AKI incidence between Black and White patients who underwent PCI at 62 US Veterans Affairs hospitals. The authors found a 22% higher odds for AKI 30 days post-PCI in Black relative to White patients. Although the authors adjusted analysis for demographics, income, comorbidities, PCI setting, indication, and number of stents placed, they did not account for critical periprocedural AKI prophylaxis and some PCI procedural characteristics that potentially confound this estimation. After adjustment for numerous PCI characteristics, our study found an 80% excess odds of AKI post-PCI in Black versus White patients. Thus, to our knowledge, our estimation is one of the first robust quantification of racial differences in AKI incidence after PCI and, importantly, suggests a larger magnitude of difference than previously reported.
Predisposing factors that underlie the excess risk for AKI development in Black patients remain elusive, and require multisectoral investigation. Comorbidities such as pre-existing cardiovascular disease, diabetes, and baseline eGFR appear to play a limited role, despite their established role as AKI risk factors in the general population.4 Additionally, high-risk APOL1 variants that confer disproportionate CKD risk in Black individuals seem unrelated to AKI risk.4 Likewise, our data demonstrated limited evidence in support of a role for proven AKI prophylactic measures and medication use: racial distribution of these factors were generally proportionate in our cohort. Thus, differences in AKI risk by race may not be solely due to traditionally recognized risk factors.
It is noteworthy that adjustment for income did not attenuate the differential AKI risk between Black and White patients in our study cohort. One prior study using the community-based Atheroslerosis Risk in Communities study found attenuation of the link between race and hospitalized AKI after adjustment for income and insurance status.4 Although we used neighborhood-level income, our findings are aligned with those of Kobayashi et al.,11 which do not support patient-level income as an independent risk factor for post-PCI AKI. This is significant given income was lower among Black compared with nonBlack patients in both PCI studies. Additional socioeconomic factors such as educational attainment have been linked with unfavorable cardiovascular outcomes after PCI,24,25 but are yet to be related to post-PCI AKI development.26 It may be that evaluation of socioeconomic influence on health requires a more robust assessment of such influences, and that it is unlikely single measures can fully capture the spectrum of influence of social and environmental determinants of health. For instance, in a recent study, we noted cumulative lifetime socioeconomic status predicted adulthood kidney health better than its constituent socioeconomic measures among Black Americans in the Jackson Heart Study.27 Furthermore, utilization of routine medical care, which is important for promotion of kidney health, is related to multiple factors unrelated to socioeconomic status, including medical mistrust,28,29 and is especially low among Black Americans with kidney disease.30 Therefore, routine integration of multidimensional measures of social determinants into health systems might strengthen our understanding of racial susceptibility to AKI.
Our study had limitations worthy of mention. The data represent observations from a single academic medical center in the Southeastern United States, and may not be generalizable elsewhere. There is also substantial variability in the definition of AKI in the literature, particularly with regard to the choice of the reference serum creatinine value. For the purposes of our study, we used any serum creatinine value regardless of location obtained within 30 days before PCI as our reference value. This approach, which includes inpatient values, may underestimate AKI incidence as serum creatinine is often elevated during hospitalization31; however, it is unlikely this would bias estimation of racial differences in AKI risk. Further, in our study, only 21% of patients had data available to obtain baseline eGFR using outpatient serum creatinine between 30 days and 6 months before PCI, which was the a priori approach. Our subsequent utilization of serum creatinine obtained within 30 days before PCI for GFR estimation in the analysis may not accurately reflect baseline kidney function given the proximity of this measure to a medical intervention. Additionally, given the heterogeneity of AKI, it is possible AKI cases observed in our data were not solely attributable to PCI. Residual confounding may also exist as we were unable to adjust for additional socioeconomic variables, such as educational attainment and insurance status due to missing data. Furthermore, racial inequities permeate multiple domains of social determinants that may not be captured by traditional measures, but which disproportionately predispose Blacks to unfavorable health. For example, the weathering hypothesis32,33 suggests that repeated exposure to stressors, such as structural racism, throughout one’s life course contributes to observed racial differences in adverse health outcomes through maladaptive biologic responses, such as allostatic load.27 Despite these limitations, our study had several strengths. We leveraged a robust clinical database with detailed clinical variables obtained from case report forms that were prospectively completed by physicians during clinical care and, as such, is not subject to limitations of retrospective designs, such as recall bias. Availability of detailed clinical variables permitted comprehensive adjustments for clinical factors that may confound associations of race with AKI risk after PCI. Our analysis also included adjustments for the year of PCI during a period spanning over a decade, which accounted for the potential effect of temporal changes in PCI practices on racial differences in AKI risk.
In conclusion, after adjustment for PCI-related characteristics, Black patients had substantially greater odds of AKI development compared with their White counterparts. Future work will need to identify predisposing factors that underlie this relation, including the role of multidimensional measures of social determinants (e.g., access to and quality of routine care, neighborhood deprivation, etc.), to inform targeted interventions to mitigate racial susceptibility to AKI incidence post-PCI.
Disclosures
C.J. Diamantidis reports consultancy with United Health Group. J.J. Scialla reports consultancy agreements with Tricida; receiving research funding from AstraZeneca, GlaxoSmithKline, Sanofi, Modest for Clinical Event Committee Activities; and receiving honoraria from Tricida. K.L. Thomas reports receiving honoraria from Pfizer and being a scientific advisor or member of Circulation. P.H. Pun reports consultancy agreements with Fresenius Medical Care, Janssen; receiving research funding from Medtronic, Hope Pharmaceuticals; receiving honoraria from Relypsa; and being a scientific advisor or member of AstraZeneca. All remaining authors have nothing to disclose.
Funding
This work was supported by Research, Education, and Training Subcore Research Voucher from the Duke Center for Research to Advance Health Equity (Duke REACH Equity). The Research, Education, and Training award is supported by the Duke University Chancellor for Health Affairs and the Duke University School of Medicine.
Supplementary Material
Acknowledgments
Dr. Clarissa J. Diamantidis, Dr. Joseph Lunyera, Dr. Julia J. Scialla, Dr. Kevin L. Thomas, Dr. Monique A. Starks, and Dr. Patrick H. Pun conceptualized the study. Dr. Karen Chiswell and Mr. Robert M. Clare analyzed the data. All authors reviewed the data output, contributed to manuscript development and finalization, and approved the final version of the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2020040502/-/DCSupplemental.
Supplemental Table 1. Availability of creatinine measurements within 30 days before percutaneous coronary intervention (PCI) for ascertainment of the reference creatinine value.
Supplemental Table 2. Association of race and baseline eGFR with odds of incident AKI after PCI in a complete-case analysis without multiple imputation for missing data.
References
- 1.Rewa O, Bagshaw SM: Acute kidney injury-epidemiology, outcomes and economics. Nat Rev Nephrol 10: 193–207, 2014 [DOI] [PubMed] [Google Scholar]
- 2.Parr SK, Siew ED: Delayed consequences of acute kidney injury. Adv Chronic Kidney Dis 23: 186–194, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoste EA, Schurgers M: Epidemiology of acute kidney injury: How big is the problem? Crit Care Med 36[Suppl]: S146–S151, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Grams ME, Matsushita K, Sang Y, Estrella MM, Foster MC, Tin A, et al.: Explaining the racial difference in AKI incidence. J Am Soc Nephrol 25: 1834–1841, 2014. 24722442 [Google Scholar]
- 5.Mathioudakis NN, Giles M, Yeh HC, Haywood C Jr., Greer RC, Golden SH: Racial differences in acute kidney injury of hospitalized adults with diabetes. J Diabetes Complications 30: 1129–1136, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nadkarni GN, Patel AA, Konstantinidis I, Mahajan A, Agarwal SK, Kamat S, et al.: Dialysis requiring acute kidney injury in acute cerebrovascular accident hospitalizations. Stroke 46: 3226–3231, 2015 [DOI] [PubMed] [Google Scholar]
- 7.Nadkarni GN, Simoes PK, Patel A, Patel S, Yacoub R, Konstantinidis I, et al.: National trends of acute kidney injury requiring dialysis in decompensated cirrhosis hospitalizations in the United States. Hepatol Int 10: 525–531, 2016 [DOI] [PubMed] [Google Scholar]
- 8.Tsai TT, Patel UD, Chang TI, Kennedy KF, Masoudi FA, Matheny ME, et al.: Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: Insights from the NCDR Cath-PCI registry. JACC Cardiovasc Interv 7: 1–9, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James MT, Ghali WA, Knudtson ML, Ravani P, Tonelli M, Faris P, et al.; Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) Investigators: Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation 123: 409–416, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Hsu CY, Chinchilli VM, Coca S, Devarajan P, Ghahramani N, Go AS, et al.; ASSESS-AKI Investigators: Post-acute kidney injury proteinuria and subsequent kidney disease progression: The Assessment, Serial Evaluation, and Subsequent Sequelae in Acute Kidney Injury (ASSESS-AKI) study. JAMA Intern Med 180: 402–410, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kobayashi T, Glorioso TJ, Armstrong EJ, Maddox TM, Plomondon ME, Grunwald GK, et al.: Comparative outcomes after percutaneous coronary intervention among Black and white patients treated at US veterans affairs hospitals. JAMA Cardiol 2: 967–975, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosati RA, McNeer JF, Starmer CF, Mittler BS, Morris JJ Jr., Wallace AG: A new information system for medical practice. Arch Intern Med 135: 1017–1024, 1975 [PubMed] [Google Scholar]
- 13.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group: KDIGO Clinical Practice Guideline for Acute Kidney Injury. Available at: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-AKI-Guideline-English.pdf. Accessed December 4, 2020
- 14.Mei M, Zhao HW, Pan QG, Pu YM, Tang MZ, Shen BB: Efficacy of N-acetylcysteine in preventing acute kidney injury after cardiac surgery: A meta-analysis study. J Invest Surg 31: 14–23, 2018 [DOI] [PubMed] [Google Scholar]
- 15.Anderson ML, Pruitt S; Rethinking Clinical Trials: Resource chapters: Linking demographic and socioeconomic data to the electronic health record, 2019. In: Rethinking Clinical Trials: A Living Textbook of Pragmatic Clinical Trials. Bethesda, MD, NIH Health Care Systems Research Collaboratory. Available at: https://rethinkingclinicaltrials.org/resources/linking-electronic-health-record-data-to-socioeconomic-status-methods-and-documentation/. Accessed December 4, 2020
- 16.Brown JR, MacKenzie TA, Maddox TM, Fly J, Tsai TT, Plomondon ME, et al.: Acute kidney injury risk prediction in patients undergoing coronary angiography in a national veterans health administration cohort with external validation. J Am Heart Assoc 4: e002136, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai TT, Patel UD, Chang TI, Kennedy KF, Masoudi FA, Matheny ME, et al.: Validated contemporary risk model of acute kidney injury in patients undergoing percutaneous coronary interventions: Insights from the National Cardiovascular Data Registry Cath-PCI Registry. J Am Heart Assoc 3: e001380, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fan PC, Chen TH, Lee CC, Tsai TY, Chen YC, Chang CH: ADVANCIS score predicts acute kidney injury after percutaneous coronary intervention for acute coronary syndrome. Int J Med Sci 15: 528–535, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brar SS, Aharonian V, Mansukhani P, Moore N, Shen AY, Jorgensen M, et al.: Haemodynamic-guided fluid administration for the prevention of contrast-induced acute kidney injury: The POSEIDON randomised controlled trial. Lancet 383: 1814–1823, 2014 [DOI] [PubMed] [Google Scholar]
- 20.Andò G, Gragnano F, Calabrò P, Valgimigli M: Radial vs femoral access for the prevention of acute kidney injury (AKI) after coronary angiography or intervention: A systematic review and meta-analysis. Catheter Cardiovasc Interv 92: E518–E526, 2018. 10.1002/ccd.27903 [DOI] [PubMed] [Google Scholar]
- 21.Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS, et al.; PRESERVE Trial Group: Outcomes after angiography with sodium bicarbonate and acetylcysteine. N Engl J Med 378: 603–614, 2018 [DOI] [PubMed] [Google Scholar]
- 22.Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, et al.: Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: The PrevAKI randomized controlled trial [published correction appears in Intensive Care Med 43: 1749, 2017 10.1007/s00134-017-4735-y]. Intensive Care Med 43: 1551–1561, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kashani K, Rosner MH, Haase M, Lewington AJP, O’Donoghue DJ, Wilson FP, et al.: Quality improvement goals for acute kidney injury. Clin J Am Soc Nephrol 14: 941–953, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai A, Dillon C, Hillegass WB, Beasley M, Brott BC, Bittner VA, et al.: Risk of major adverse cardiovascular events and major hemorrhage among white and Black patients undergoing percutaneous coronary intervention. J Am Heart Assoc 8: e012874, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Batchelor W, Kandzari DE, Davis S, Tami L, Wang JC, Othman I, et al.: Outcomes in women and minorities compared with white men 1 year after everolimus-eluting stent implantation: Insights and results from the PLATINUM diversity and PROMUS element plus post-approval study pooled analysis. JAMA Cardiol 2: 1303–1313, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mensah GA: Black-white disparities: More than just race. J Am Heart Assoc 8: e014272, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lunyera J, Stanifer JW, Davenport CA, Mohottige D, Bhavsar NA, Scialla JJ, et al.: Life course socioeconomic status, allostatic load, and kidney health in Black Americans. Clin J Am Soc Nephrol 15: 341–348, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agrawal V, Jaar BG, Frisby XY, Chen SC, Qiu Y, Li S, et al.; KEEP Investigators: Access to health care among adults evaluated for CKD: Findings from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 59[Suppl 2]: S5–S15, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans K, Coresh J, Bash LD, Gary-Webb T, Köttgen A, Carson K, et al.: Race differences in access to health care and disparities in incident chronic kidney disease in the US. Nephrol Dial Transplant 26: 899–908, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diamantidis CJ, Davenport CA, Lunyera J, Bhavsar N, Scialla J, Hall R, et al.: Low use of routine medical care among African Americans with high CKD risk: The Jackson Heart Study. BMC Nephrol 20: 11, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siew ED, Matheny ME: Choice of reference serum creatinine in defining acute kidney injury. Nephron 131: 107–112, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Geronimus AT, Hicken M, Keene D, Bound J: “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health 96: 826–833, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lunyera J, Davenport CA, Bhavsar NA, Sims M, Scialla J, Pendergast J, et al.: Nondepressive psychosocial factors and CKD outcomes in Black Americans. Clin J Am Soc Nephrol 13: 213–222, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.