Abstract
The incidence of cervical spine injury in patients with polytrauma is 3.7%. Early identification and management of cervical spine injuries in these patients play a crucial role in preventing secondary cervical spine and cord injuries. C-spine clearance assumes a pivotal role in reducing the morbidity and mortality associated with cervical spine injury. Despite the availability of various validated management algorithms and protocols for C-spine clearance, there are several controversies regarding C-spine clearance, such as the ideal protocol and imaging modality, clearance of obtunded patients and management of patients that lie out of the described protocols and rules. The current article aims to provide a comprehensive review of the relevant literature and address the prevalent controversies.
Keywords: Cervical spine injury, Cervical spine clearance, NEXUS, Canadian C-spine rule, Paediatric C-spine clearance
1. Introduction
The incidence of cervical spine injury in patients with polytrauma is 3.7%, 3% in alert patients and rising to 8% in unconscious or obtunded patients.1 Early identification and management of cervical spine injuries in these patients play a crucial role in preventing secondary cervical spine and cord injuries. Therefore, C-spine clearance assumes a pivotal role in reducing the morbidity and mortality associated with cervical spine injury and improving health-related quality of life (HRQoL) in these patients. Apart from prioritizing treatment protocol, early cervical clearance also prevents excessive duration of cervical spine immobilization as it has been found to have several complications, including early tissue ulceration, increased intracranial pressure through jugular venous compression, mechanical respiratory restriction and harmful unfitted immobilization in ankylosing spondylitis.2, 3, 4, 5 C-spine clearance therefore aims for early identification of C-spine injuries and at the same time reducing unnecessary and prolonged immobilization in trauma patients without C-spine injuries.
Despite the availability of various validated management algorithms and protocols for C-spine clearance, there are several controversies regarding C-spine clearance, such as the ideal protocol and imaging modality, clearance of obtunded patients and management of patients that lie out of the described protocols and rules. The current article aims to provide a comprehensive review of the relevant literature and address the prevalent controversies.
2. Material and methods
An extensive English literature search in various data bases such as PubMed, EMBASE and Cochrane library was carried out with the search terms including ‘cervical spine’, ‘radiology’, ‘injury’, ‘trauma’, ‘cervical spine clearance’, ‘national emergency X-radiography utilization study’ and ‘Canadian c-spine rule’. The yielded citations were examined for relevance and duplication. Unrelated articles and articles in languages other than English language were excluded. After making necessary exclusions, the articles were further analyzed to address the controversies as mentioned above.
3. Primary C-spine evaluation
The initial C-spine evaluation ensues after the primary survey and once the patient is stabilized. The aim of this exercise is to identify the patients at a high risk of significant c-spine injury. All the blunt trauma patients can be divided into four types for the purpose of evaluation6:
-
1.
Asymptomatic – This group comprises of patients with no pain or tenderness and a normal cognitive function. These patients should undergo screening using either NEXUS or Canadian C-spine rule and cleared or examined radiologically accordingly. These algorithms are described in detail in subsequent sections.
-
2.
Temporarily not evaluable – These patients usually present with an impaired cognitive function such as intoxication. Clearance for these patients may be delayed for 12–24 h and may be cleared using the asymptomatic criteria once the cognitive impairment is corrected. However, in a scenario where the delay is not deemed appropriate and immediate clearance is required, the patients may be evaluated as described for obtunded patients.
-
3.
Symptomatic patients – All symptomatic patients are at a high risk for c-spine injury and must be evaluated using an imaging modality. The imaging modalities have been described in detail in subsequent sections of the article.
-
4.
Obtunded patients – Obtunded patients usually present with a GCS of less than 14. The current literature lacks any validated clinical criteria or algorithm for c-spine clearance in these patients. Hence, the clinicians rely on the imaging for clearance.
4. Indications for C-spine imaging in awake and oriented patients
Unrecognized cervical spine injury in a trauma patient can result in catastrophic neurological disability and possible mortality. Therefore, immobilization and subsequent evaluation of cervical spine during clinical and radiological assessment of a trauma patient is of paramount importance. However, liberal and unorganized cervical radiography in trauma patients in an attempt to rule out cervical spine injury results in exuberant expenditure along with excessive radiation exposure. A substantial proportion of expenditure and radiation exposure can be avoided by eliminating even a small number of radiographs in this patient population. Defining indications and protocols for cervical imaging in trauma patients is therefore crucial to avoid missed injuries and unwarranted expenditure at the same time.
Two algorithms or clinical-decision making rules have been defined in the literature for adequate C-spine clearance.7,8 While each has its own set of advantages and drawbacks, none can be considered as superior to the other. The first of these decision-making tools was the National Emergency X-radiography Utilization Study (NEXUS) by Hoffman et al.8 The tool comprises five clinical criteria and all criteria should be fulfilled to rule out a cervical spine injury in patients – no midline tenderness, the absence of a focal neurologic deficit, a normal level of alertness, no evidence of intoxication, and absence of clinically apparent pain that might distract the patient from the pain of a cervical-spine injury. The sensitivity and specificity of the tool was found to be 99% and 12.9% whereas the negative and positive predictive value was found to be 99.8% and 2.7%.8 Despite a low specificity and positive predictive value, the high negative predictive value ensures reliable exclusion of a cervical spine injury. One of the greatest advantages with the NEXUS protocol is its ease of application, which converts to a quick decision making in the emergency room. However, the same criteria in the hands of researchers other than Hoffman et al. were found to have a lower sensitivity of 90.7%.9 Additionally, high subjectivity and lack of clear definitions, such as the last criteria (absence of clinically apparent pain) are other important drawbacks of NEXUS.
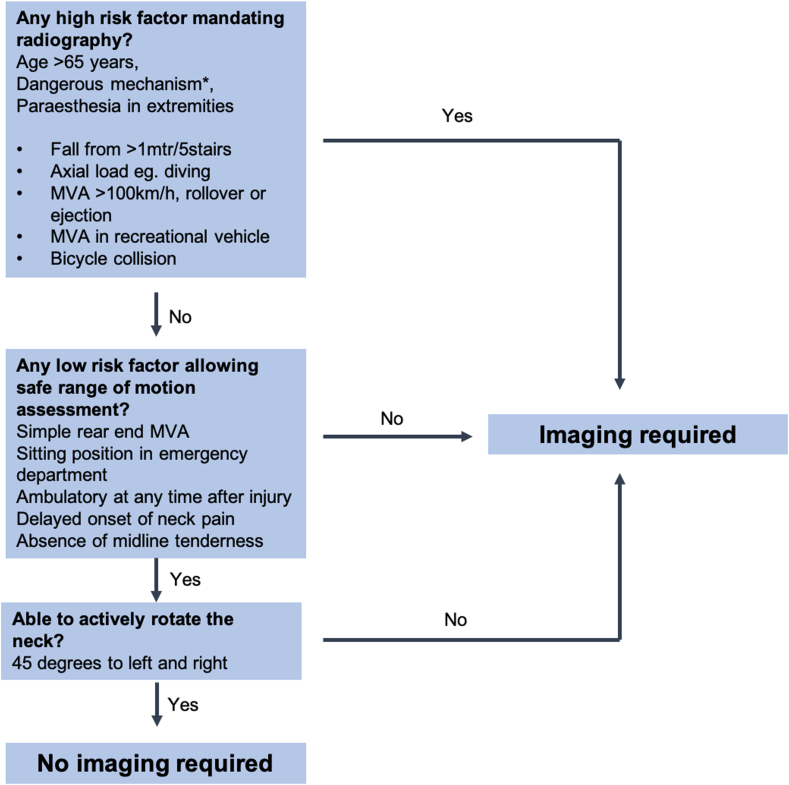
Three years later in 2001, Steill et al. published the Canadian C-spine rule (CCR) (Fig. 1).7 The authors identified high risk and low risk criteria for need of radiography. High risk criteria included age more than 65, dangerous mechanisms of injury such as fall from >1 m/5 stairs, axial load to the head, motor vehicle collision >100 km/h, rollover, or ejection during collision, collision in recreation vehicles or bicycles and paraesthesia in extremities. Presence of any of these high risk criteria warrant a thorough radiological evaluation. Low risk criteria include simple rear-end motor vehicle collision, found to be in the sitting position in the ED, ambulatory status at any time after the injury, delayed onset of neck pain, and absence of midline C-spine tenderness. Presence of any of these low risk criteria allow safe assessment of range of motion examination, which includes a left to right 45-degree rotation examination. A successful exam clears the cervical spine, whereas the absence of low risk criteria or inability to rotate the neck is an indication for radiological evaluation. Although this clinical decision-making rule is more comprehensive and reproducible than NEXUS, the limitations include applicability only to patients above 16 years of age, lack of inclusion of obtunded or unconscious patients and longer time and accurate history needed for clearance.
Fig. 1.
A flow chart depicting the Canadian C-spine rule for cervical spine clearance.
Steill et al. compared CCR and NEXUS in a prospective cohort study comprising 8283 patients in nine Canadian emergency hospitals.9 An important finding in the present study was the reluctance of a number of researchers to evaluate the neck ROM as described in the CCR algorithm in approximately 10% of the patients. The researchers concluded a higher overall sensitivity and specificity for CCR compared to NEXUS. No other study till date provides a direct comparison of NEXUS and CCR in the same study cohort. Michaleff et al. conducted a systematic review and reported a high sensitivity and low specificity for both the algorithms.10 For the Canadian C-spine rule, sensitivity ranged from 0.90 to 1.00 and specificity ranged from 0.01 to 0.77 whereas for NEXUS, sensitivity ranged from 0.83 to 1.00 and specificity ranged from 0.02 to 0.46. Nevertheless, good quality evidence is needed to compare the two and establish the superiority of one diagnostic accuracy test over the other.
5. The ideal radiological modality for C-spine screening
5.1. Plain radiography
Plain radiography has for long been considered the modality of choice for cervical spine screening in trauma patients. Radiographs provide a comprehensive overview of the extent and magnitude of injury and can play an important role in decision making for definitive management.11 Being inexpensive and readily available, radiographs are still considered the screening modality of choice in several developing nations where accessibility to a CT scan is a problem. Nevertheless, given the low sensitivity (40%–60%), plain radiography as an imaging modality for C-spine screening is far from ideal.12, 13, 14
5.2. Computed tomography scan
With the technological advancements and easy accessibility of CT scan imaging, it has become the choice of screening investigation according to several guidelines and society recommendations. Several studies including a few meta-analysis have been published comparing the efficacy of radiographs and CT scans in diagnosing cervical spine injuries (Table 1). All observational studies have reported a higher sensitivity of a helical or MDCT over plain radiography (90%–100%).13, 14, 15, 16, 17 Holmes et al. in a meta-analysis concluded CT outweighs plain radiographs in blunt trauma victims with a high risk of cervical spine injury, whereas plain radiographs are preferred in less injured patients with less significant trauma with lower risk of cervical spine injury.13 Another study found CT scan to be cost-effective compared with radiographs in high risk patients.18 The National Institute for Health and Care Excellence (NICE) guidelines recommend CT and MRI scans as the investigation of choice in adults and children, respectively, who are suspected to have a C-spine injury according to the Canadian C-spine rule.19 Similar to recommendations by Como et al. as a part of the Eastern association of surgery for trauma practice guidelines, the authors also recommend an axial CT from the occiput to T1 with sagittal and coronal reconstruction instead of conventional imaging by means of plain radiographs.20
Table 1.
– Clinical evidence evaluating the efficacy of NEXUS and CCR and guidelines available in literature.
| Author | Study methodology | Level of evidence | Sample size | Sensitivity | Specificity | Missed on X-Rays | Comment/Remarks |
|---|---|---|---|---|---|---|---|
| Mathen 2007 | MCT vs X-Rays | Prospective case series—level 4 | 667 | 100% vs 45% | 99.5% vs 97.4% | 15 of 27 (55.5%) | MCT outperformed plain radiography as a screening modality for the identification of acute c-spine injury in trauma patients |
| Diaz JJ 200515 | HCT vs X-Rays | Prospective case series—level 4 | 1577 | 32% vs 16%a | 299 of 416 (72%) | Helical CT is not only sensitive and specific but also cost-effective tool for screening cervical spine bony injuries. For ligamentous injuries, MRI is superior to CT | |
| Diaz JJ 200314 | CT scan vs X-Rays | Prospective case series—level 4 | 1006 | 97.4% vs 44% | 100% vs 100% | 90 of 172 (52.3%) | CTS outperformed five-view CSX in a group of patients with altered mental status or distracting injuries. |
| Holmes 200512 | CT scan vs X-Rays | Meta-analysis—level 3 | 98% vs 52% | CT significantly outperforms plain radiography as a screening test | |||
| Beckman 2019 | ACR guidelines | Level 5 | CT is the preferred screening modality in blunt trauma patients when indicated with NEXUS or CCR | ||||
| Kortbeek JB 200846 | ATLS guidelines | Level 5 | CT is the preferred screening modality in blunt trauma patients at high and moderate risk of cervical spine fractur | ||||
| Ackland 201216 | RACP guidelines | Level 5 | CT is the preferred imaging. Five-view plain X-ray to be done if CT is unavailable. MRI should be considered in patients with neurologic symptoms or advanced cervical degenerative disease. |
Values only for ligamentous injury.
5.3. Magnetic resonance imaging
MRI is a highly sensitive investigation, especially to identify disco-ligamentous injuries, occult spinal or cord injuries with normal spinal column.21 MRI being an expensive and time intensive investigation with significant false positive results, is not accepted as the investigation of choice for C-spine clearance in routine emergency trauma scenarios. Malhotra et al. in a meta-analysis including 23 studies and 5286 patients reported a negligible number of unstable injuries (16,0.30%) in patients with negative CT scans.22 Another prospective study with over 5200 patients reported 0% missed ligamentous injuries after a negative CT scan.23 Nevertheless, it plays an important role in diagnosing cord injuries in degenerative conditions such as central cord syndrome or SCIWORA injuries in a paediatric age group. Moreover, it is accepted as a screening investigation of choice in paediatric blunt trauma patients with a high index of suspicion for cervical spine injury.
5.4. Dynamic radiographs
Dynamic cervical radiographs were introduced to diagnose instability and ligamentous injury as these dynamic components are inadequately diagnosed in lateral radiographs. However, the sensitivity of these dynamic X-rays is highly dependent on the adequacy of flexion-extension movement. A flexion and extension of 30° from the neutral is considered adequate for diagnosing instability in the cervical spine. Various researchers have documented the adequacy of dynamic X-rays in acute trauma conditions to range from 31% to 70% of the patients.24, 25, 26, 27, 28 The limited mobility of cervical spine, therefore, limits the utility of this modality in an acute trauma scenario. Moreover, several researchers have concluded that dynamic radiographs fail to provide any additional information over static lateral radiographs in acute trauma.20,24,27,28 Therefore, any utility of dynamic radiographs in cervical-spine clearance is questionable.
6. C-spine clearance in obtunded patients
Blunt trauma in an obtunded or intoxicated patient presents a challenging scenario due to the inability to perform a neurological exam, neck range of motion according to CCR or elicit a proper history in many cases. Nevertheless, early diagnosis and prevention of prolonged immobilization is indispensable in these patients for optimum outcome. In the absence of a readily available clinical algorithm for obtunded or intoxicated trauma patients till date, C-spine clearance is usually achieved by cervical spine imaging. However, the imaging modality of choice for the clearance is controversial. Similar to alert patients, radiographs, both static and dynamic have a limited sensitivity in diagnosing cervical spine injuries in obtunded patients. Griffen et al. and Brohi et al. have evaluated the use of plain radiographs in these patients and reported 35% and 45% of missed cervical injuries respectively.29,30
The guidelines with respect to the use of CT scans for cervical spine clearance have also evolved with time. Eastern association of surgery for trauma guidelines of 2009 did not rely on a negative CT scan report alone for C-spine clearance in obtunded patients. However, in light of the recent literature, EAST modified there guidelines in 2015.20,31,32 On the basis of a systematic review, they recommend cervical collar removal after a negative high-quality C-spine CT scan result alone. A systematic review comprising 3443 patients emphasized the use of 64-slice MPR (multiplanar reconstruction) CT or higher quality scan alone to clear a C-spine injury if the images are interpreted by an experienced radiologist and the patient has no obvious neurological symptoms.33 The authors also pointed out a higher prevalence of missed cervical spine injuries (up to 5%) associated with the use of an earlier generation of CT scans without multiplanar reconstruction technology. Badhiwala et al. in a systematic review concluded employing a well-interpreted, high-quality CT scans as safe and effective for C-spine clearance in obtunded patients.34
Use of MRI for C-spine clearance has been evaluated by a few researchers. MRI has been found to be highly sensitive in identifying disco-ligamentous injuries in the cervical spine. Nevertheless, the literature is divided with respect to the indications for MRI for C-spine clearance, especially after a negative CT scan. According to various studies, the prevalence of missed injuries in obtunded patients after a negative CT scan eventually diagnosed with an MR range from 5% to 30%, however the number of injuries requiring stabilization in these patients is less than 1%.35, 36, 37, 38 Moreover, the time and cost-invasiveness of MR imaging may prove to be an important limitation in using this investigation a screening tool in trauma imaging. Longer waiting duration in immobilized spine may also result in several complications and prevent proper medical and nursing care in these patients. Advancements in CT imaging have led to a negative predictive value for all and unstable cervical spine injuries to as high as 98.9% and 100% respectively, which implies that none of the patients rendered negative by CT cervical spine screening would eventually require any intervention.35 The authors recommend the usage of an MDCT interpreted by a trained radiologist for C-spine clearance in obtunded patients.
7. Clearance in patients with pain persisting with negative CT scan
Cases with persistence of pain in trauma patients despite a negative CT present a challenge for the treating physician. Although the scenario is common, but lacks adequate literature to support any recommendations or a validated method of risk-stratification in such patients. A thorough assessment of pain at rest and in motion is warranted in such patients. The authors follow a stratified approach to deal with such scenarios. For mild pain with visual analogue scale of less than three out of 10, the pain can be attributed to positioning or the discomfort of immobilization and c-spine could be cleared without any further intervention. For moderate amount of pain with a VAS of 4–5 out of 10, the pain may be attributed to a minor soft tissue trauma and c-spine may be cleared with a soft collar in place if the patient demonstrates a normal range of motion. In cases with painful or restricted cervical movement or severe pain, MRI is advisable.
8. C-spine clearance in paediatric population
Management of a blunt trauma to a child has its own unique and distinct aspects when compared with adult injuries. The c-spine algorithms used in adults are of questionable importance in paediatric trauma. Subtle signs in this age group such as an unexplained persistent low blood pressure may indicate a significant injury to the cervical cord. Apart from the commonly used c-spine clearance algorithms, Pediatric Emergency Care Applied Research Network (PECARN) retrospectively identified 8 factors highly associated with CSI in children 0–16 years.39 These included altered mental status, focal neurologic deficits, complaints of neck pain, torticollis, substantial injury to the torso, predisposing condition for c-spine injury, high risk MVC and diving.
A few class II multicentric prospective studies have evaluated the use of NEXUS in paediatric population.40,41 Viciello in his study included 3075 patients, all less than 18 years of age reported a 20% reduction in radiography and no missed injuries on evaluating these patients using the NEXUS protocol.40 However, the study included only 88 patients with age less than 2 years and hence, cautious endorsement of application of NEXUS for paediatric age group was done by the authors. Anderson et al. in his study evaluated trauma patients using three view radiographs for screening along with NEXUS criteria. They reported a 60% increase in c-spine clearance in children by non-neurosurgical personnel.41,42 CT scan or MRI were indicated only if radiological abnormality was identified in the screening radiographs. Garton et al. reported no missed injuries in patients above 8 years in contrast to 6% missed injuries in patients less than 8 years of age when evaluated using the NEXUS criteria.43 Ehrlich et al. reported a sensitivity of 43% and 86% for NEXUS and CCR respectively and concluded none of the protocols can be applied to paediatric age group.44
Pieretti-Vanmarcke in a multi-centre review of 12,537 patients with age less than three years concluded four predictors of cervical spine injury in these patients - GCS < 14; GCSeye = 1; motor vehicle crash; age 2–3 years. They reported a 99.93% negative predictive value for c-spine injury if all these criteria were used in combination for screening.45
In summary, based on class II and III evidence, screening imaging is indicated in paediatric patients if any of the five NEXUS criteria is positive or cannot be answered or assessed due to age or head injury. Additionally, children who have experienced trauma that are non-communicative due to age (, 3 years old) and have motor vehicle collision, fall from a height more than 10 feet, or suspected non-accidental trauma as mechanisms, or GCS less than 14 should have screening cervical spine imaging performed.46
9. Conclusion
Proper patient selection for imaging using CCR or NEXUS criteria is a cost effective strategy during C-spine clearance. In a majority of trauma scenarios, good quality axial CT scan, such as a helical or multidetector scan with a sagittal and coronal reconstruction reliably rules out a cervical spine injury in patients. In several trauma centres in developing nations with limited resources or a high patient load, a modified strategy may be adopted using an initial screening with three view radiographs and a comprehensive clinical examination, albeit with limited sensitivity. MRI as a screening investigation may prove to be both a time and cost invasive modality with a high incidence of false positive results. In patients with GCS less than 14, most studies recommend a CT scan for screening with a reasonable sensitivity. However, clearly defined guidelines are lacking. There is a lack of good quality evidence to deal with a patient with persistence of neck pain despite a negative CT scan. Further studies are warranted to formulate guidelines to deal with such a scenario.
Funding source
Nil.
References
- 1.M Ah, H Ch, G W., S Sc. Prevalence of cervical spinal injury in trauma. Neurosurg Focus. 2008 doi: 10.3171/FOC.2008.25.11.E10. [DOI] [PubMed] [Google Scholar]
- 2.Clarke A., James S., Ahuja S. Ankylosing spondylitis: inadvertent application of a rigid collar after cervical fracture, leading to neurological complications and death. Acta Orthop Belg. Jun 2010;76(3):413–415. PMID: 20698467. [PubMed] [Google Scholar]
- 3.Hauswald M., Ong G., Tandberg D., Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med Off J Soc Acad Emerg Med. 1998;5(3):214–219. doi: 10.1111/j.1553-2712.1998.tb02615.x. [DOI] [PubMed] [Google Scholar]
- 4.Walker J. Pressure ulcers in cervical spine immobilisation: a retrospective analysis. J Wound Care. 2012;21(7):323–326. doi: 10.12968/jowc.2012.21.7.323. [DOI] [PubMed] [Google Scholar]
- 5.Sparke A., Voss S., Benger J. The measurement of tissue interface pressures and changes in jugular venous parameters associated with cervical immobilisation devices: a systematic review. Scand J Trauma Resuscitation Emerg Med. 2013;21:81. doi: 10.1186/1757-7241-21-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steven RG, Frank JE, Gordon RB. Rothman-Simeone and Herkowitz’s the Spine. seventh ed. Elsevier
- 7.Stiell I.G., Wells G.A., Vandemheen K.L. The Canadian C-spine rule for radiography in alert and stable trauma patients. J Am Med Assoc. 2001;286(15):1841–1848. doi: 10.1001/jama.286.15.1841. [DOI] [PubMed] [Google Scholar]
- 8.Jr H, Wr M, Ab W, Kh T, Mi Z. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. doi:10.1056/NEJM200007133430203 [DOI] [PubMed]
- 9.Ig S, Cm C, Rd M, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. doi:10.1056/NEJMoa031375 [DOI] [PubMed]
- 10.Michaleff Z.A., Maher C.G., Verhagen A.P., Rebbeck T., Lin C.-W.C. Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: a systematic review. CMAJ Can Med Assoc J. 2012;184(16):E867. doi: 10.1503/cmaj.120675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.B F, R K, J P, L W, J W. Comparison of five-view and three-view cervical spine series in the evaluation of patients with cervical trauma. Ann Emerg Med. doi:10.1016/s0196-0644(89)80203-3 [DOI] [PubMed]
- 12.Mathen R., Inaba K., Munera F. Prospective evaluation of multislice computed tomography versus plain radiographic cervical spine clearance in trauma patients. J Trauma. 2007;62(6):1427–1431. doi: 10.1097/01.ta.0000239813.78603.15. [DOI] [PubMed] [Google Scholar]
- 13.Holmes J.F., Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma. 2005;58(5):902–905. doi: 10.1097/01.ta.0000162138.36519.2a. [DOI] [PubMed] [Google Scholar]
- 14.Sc G, Vh G, Pm R, Cw S. The inefficiency of plain radiography to evaluate the cervical spine after blunt trauma. J Trauma. doi:10.1097/01.ta.0000188632.79060.ba [DOI] [PubMed]
- 15.Diaz J.J., Gillman C., Morris J.A., May A.K., Carrillo Y.M., Guy J. Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma. 2003;55(4):658–663. doi: 10.1097/01.TA.0000088120.99247.4A. discussion 663-664. [DOI] [PubMed] [Google Scholar]
- 16.Diaz J.J., Aulino J.M., Collier B. The early work-up for isolated ligamentous injury of the cervical spine: does computed tomography scan have a role? J Trauma. 2005;59(4):897–903. doi: 10.1097/01.ta.0000188012.84356.dc. ; discussion 903-904. [DOI] [PubMed] [Google Scholar]
- 17.Practitioners trac of G. racgp - cervical spine – assessment following trauma. https://www.racgp.org.au/afp/2012/april/cervical-spine/ Accessed September 15, 2020.
- 18.Cc B, Sd R, Fa M, Ra D. Cervical spine screening with CT in trauma patients: a cost-effectiveness analysis. Radiology. doi:10.1148/radiology.212.1.r99jl08117 [DOI] [PubMed]
- 19.Quality statement 4: assessment for cervical spine injury Trauma Quality standards NICE. https://www.nice.org.uk/guidance/qs166/chapter/Quality-statement-4-Assessment-for-cervical-spine-injury Accessed September 16, 2020.
- 20.Jj C, Jj D, Cm D, et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma. doi:10.1097/TA.0b013e3181ae583b [DOI] [PubMed]
- 21.Mj G, S Y, Jc W. Assessment of cervical ligamentous injury in trauma patients using MRI. J Spinal Disord. doi:10.1097/00002517-200110000-00001 [DOI] [PubMed]
- 22.Malhotra A., Wu X., Kalra V.B. Utility of MRI for cervical spine clearance after blunt traumatic injury: a meta-analysis. Eur Radiol. 2017;27(3):1148–1160. doi: 10.1007/s00330-016-4426-z. [DOI] [PubMed] [Google Scholar]
- 23.Vanguri P., Young A.J., Weber W.F. Computed tomographic scan: it’s not just about the fracture. J Trauma Acute Care Surg. 2014;77(4):604–607. doi: 10.1097/TA.0000000000000407. [DOI] [PubMed] [Google Scholar]
- 24.Insko E.K., Gracias V.H., Gupta R., Goettler C.E., Gaieski D.F., Dalinka M.K. Utility of flexion and extension radiographs of the cervical spine in the acute evaluation of blunt trauma. J Trauma. 2002;53(3):426–429. doi: 10.1097/00005373-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Ryken T.C., Hadley M.N., Walters B.C. Radiographic Assessment: Neurosurgery. 2013;72:54–72. doi: 10.1227/NEU.0b013e318276edee. [DOI] [PubMed] [Google Scholar]
- 26.Brady W.J., Moghtader J., Cutcher D., Exline C., Young J. ED use of flexion-extension cervical spine radiography in the evaluation of blunt trauma. Am J Emerg Med. 1999;17(6):504–508. doi: 10.1016/s0735-6757(99)90185-7. [DOI] [PubMed] [Google Scholar]
- 27.Lewis L.M., Docherty M., Ruoff B.E., Fortney J.P., Keltner R.A., Britton P. Flexion-extension views in the evaluation of cervical-spine injuries. Ann Emerg Med. 1991;20(2):117–121. doi: 10.1016/s0196-0644(05)81205-3. [DOI] [PubMed] [Google Scholar]
- 28.Pollack C.V., Hendey G.W., Martin D.R., Hoffman J.R., Mower W.R., NEXUS Group Use of flexion-extension radiographs of the cervical spine in blunt trauma. Ann Emerg Med. 2001;38(1):8–11. doi: 10.1067/mem.2001.116810. [DOI] [PubMed] [Google Scholar]
- 29.Griffen M.M., Frykberg E.R., Kerwin A.J. Radiographic clearance of blunt cervical spine injury: plain radiograph or computed tomography scan? J Trauma. 2003;55(2):222–226. doi: 10.1097/01.TA.0000083332.93868.E2. discussion 226-227. [DOI] [PubMed] [Google Scholar]
- 30.Brohi K., Healy M., Fotheringham T. Helical computed tomographic scanning for the evaluation of the cervical spine in the unconscious, intubated trauma patient. J Trauma. 2005;58(5):897–901. doi: 10.1097/01.ta.0000171984.25699.35. [DOI] [PubMed] [Google Scholar]
- 31.Walters B.C., Hadley M.N., Hurlbert R.J. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60(CN_suppl_1):82–91. doi: 10.1227/01.neu.0000430319.32247.7f. [DOI] [PubMed] [Google Scholar]
- 32.Patel M.B., Humble S.S., Cullinane D.C. Cervical spine collar clearance in the obtunded adult blunt trauma patient: a systematic review and practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;78(2):430–441. doi: 10.1097/TA.0000000000000503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kanji H.D., Neitzel A., Sekhon M., McCallum J., Griesdale D.E. Sixty-four-slice computed tomographic scanner to clear traumatic cervical spine injury: systematic review of the literature. J Crit Care. 2014;29(2):314. doi: 10.1016/j.jcrc.2013.10.022. e9-13. [DOI] [PubMed] [Google Scholar]
- 34.Badhiwala J.H., Lai C.K., Alhazzani W. Cervical spine clearance in obtunded patients after blunt traumatic injury: a systematic review. Ann Intern Med. 2015;162(6):429–437. doi: 10.7326/M14-2351. [DOI] [PubMed] [Google Scholar]
- 35.Hogan G.J., Mirvis S.E., Shanmuganathan K., Scalea T.M. Exclusion of unstable cervical spine injury in obtunded patients with blunt trauma: is MR imaging needed when multi-detector row CT findings are normal? Radiology. 2005;237(1):106–113. doi: 10.1148/radiol.2371040697. [DOI] [PubMed] [Google Scholar]
- 36.Stassen N.A., Williams V.A., Gestring M.L., Cheng J.D., Bankey P.E. Magnetic resonance imaging in combination with helical computed tomography provides a safe and efficient method of cervical spine clearance in the obtunded trauma patient. J Trauma. 2006;60(1):171–177. doi: 10.1097/01.ta.0000197647.44202.de. [DOI] [PubMed] [Google Scholar]
- 37.Horn E.M., Lekovic G.P., Feiz-Erfan I., Sonntag V.K.H., Theodore N. Cervical magnetic resonance imaging abnormalities not predictive of cervical spine instability in traumatically injured patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves. J Neurosurg Spine. 2004;1(1):39–42. doi: 10.3171/spi.2004.1.1.0039. March 2004. [DOI] [PubMed] [Google Scholar]
- 38.Ghanta M.K., Smith L.M., Polin R.S., Marr A.B., Spires W.V. An analysis of Eastern Association for the Surgery of Trauma practice guidelines for cervical spine evaluation in a series of patients with multiple imaging techniques. Am Surg. 2002;68(6):563–567. discussion 567-568. [PubMed] [Google Scholar]
- 39.Leonard J.C., Kuppermann N., Olsen C. Factors associated with cervical spine injury in children after blunt trauma. Ann Emerg Med. 2011;58(2):145–155. doi: 10.1016/j.annemergmed.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 40.Viccellio P., Simon H., Pressman B.D. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):e20. doi: 10.1542/peds.108.2.e20. e20. [DOI] [PubMed] [Google Scholar]
- 41.Anderson R.C.E., Kan P., Vanaman M. Utility of a cervical spine clearance protocol after trauma in children between 0 and 3 years of age. J Neurosurg Pediatr. 2010;5(3):292–296. doi: 10.3171/2009.10.PEDS09159. [DOI] [PubMed] [Google Scholar]
- 42.Anderson R.C.E., Scaife E.R., Fenton S.J., Kan P., Hansen K.W., Brockmeyer D.L. Cervical spine clearance after trauma in children. J Neurosurg. 2006;105(5 Suppl):361–364. doi: 10.3171/ped.2006.105.5.361. [DOI] [PubMed] [Google Scholar]
- 43.Garton H.J.L., Hammer M.R. Detection of pediatric cervical spine injury. Neurosurgery. 2008;62(3):700–708. doi: 10.1227/01.NEU.0000311348.43207.B7. discussion 700-708. [DOI] [PubMed] [Google Scholar]
- 44.Ehrlich P.F., Wee C., Drongowski R., Rana A.R. Canadian C-spine rule and the national emergency X-radiography utilization low-risk criteria for C-spine radiography in young trauma patients. J Pediatr Surg. 2009;44(5):987–991. doi: 10.1016/j.jpedsurg.2009.01.044. [DOI] [PubMed] [Google Scholar]
- 45.Pieretti-Vanmarcke R., Velmahos G.C., Nance M.L. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the american association for the surgery of trauma. J Trauma. 2009;67(3):543–549. doi: 10.1097/TA.0b013e3181b57aa1. discussion 549-550. [DOI] [PubMed] [Google Scholar]
- 46.Rozzelle C.J., Aarabi B., Dhall S.S. Management of pediatric cervical spine and spinal cord injuries. Neurosurgery. 2013;72(suppl_3):205–226. doi: 10.1227/NEU.0b013e318277096c. [DOI] [PubMed] [Google Scholar]