Abstract
Injury-related morbidity and mortality have been one of the most common causes of loss in productivity across all geographic distributions. It remains to be a global concern despite a continual improvement in regional and national safety policies. The establishment of trauma care systems and advancements in diagnostics and management have improved the overall survival of severely injured. A better understanding of the physiopathological and immunological responses to injury led to a significant shift in trauma care from “Early Total Care” to “Damage Control Orthopedics.” While most of these algorithms were tailored to the philosophy of “life before limb,” the impact of improper fracture management on disability and societal loss is increasingly being recognized. Recently, “Early Appropriate Care” of extremities has gained importance; however, its implementation is influenced by regional health care policies, available resources, and expertise and varies between low and high-income countries. A review of the literature was performed using PubMed, Embase, Web of Science, and Scopus databases on articles published from 1990 to 2020 using the Mesh terms “Polytrauma,” “Multiple Trauma,” and “Fractures.” This review aims to consolidate on guidelines and available evidence in the management of extremity injuries in a polytraumatized patient to achieve better clinical outcomes of these severely injured.
Keywords: Polytrauma, Damage control, Resuscitation, Fracture fixation, Traumatic brain injury, Chest injury
1. Introduction
Polytrauma is a leading cause of death in young individuals aged less than 40, and the management of these patients continues to be a significant challenge.1 The prevalence of extremity injuries in a polytraumatized patient is as high as 60%.2 Management of these patients begins at the trauma site and should always follow a continuum of care through the prehospital phase, emergency care, and primary operative management. Care of a Polytrauma patient with extremity injuries should be in line with the Advanced Trauma Life Support (ATLS) protocol and should include all the ABCDEs of the primary survey. Considerable evidence and consensus have been achieved on resuscitation of these critically injured. However, the appropriate method and time of fracture stabilization in Polytrauma patients has been long debated and has witnessed a constant change. This is mainly because of the developments achieved in the understanding of the systemic inflammatory response to trauma and advancements in diagnostics and the discovery of biomarkers to assess the severity of the traumatic insult and its physiological recovery.
Besides, the decision on the choice of management is determined by several factors, including soft tissue loss, neurovascular damage, hemodynamic stability, severity and location of extremity injury, and the physiological reserve of each patient. Also, the coordination and technical competence of the multidisciplinary trauma team is of paramount importance in making timely decisions in managing these patients. Delayed definitive management of extremity injuries leads to increased complications such as infection, nonunion, or even failure in limb salvage. On the other hand, early radical surgery can result in higher mortality, and therefore striking the right balance between the two is essential to achieve the benefits of early mobilization. This review article highlights the current updates in the diagnosis and management of extremity injuries in a polytraumatized patient.
2. Epidemiology of extremity injuries
The cause of Polytrauma injuries may vary from low energy falls in the elderly to high energy trauma in young.3 While Road traffic accidents and falls from height are the leading causes, natural calamity related polytrauma and ballistic injuries are not uncommon.4,5 In a retrospective analysis of 24,885 multiple trauma patients, Banerjee et al. reported a prevalence of upper extremity injuries in 21.8% compared to 19% of lower extremity injuries and 17.7% who had both upper and lower extremity injuries. Amongst the upper extremity injuries, the Clavicle (10.4%) was the most commonly affected bone followed by Radius (9.9%) and Humerus (7.4%). Amongst lower extremity injuries, the Femur (16.5%) was the most common bone, followed by Tibia (12.6%) and Foot/Ankle (5.8%).2
Despite a well documented high prevalence of extremity fractures in Polytrauma, missed injuries in these critically injured patients vary from 45% to 81% and are primarily musculoskeletal.6 Unfortunately, up to 20% of these missed orthopedic injuries required surgical fixation. With the implementation of ATLS guidelines, the rate of these missed injuries has come down significantly. Pape et al. observed a decreasing trend of missed pelvic and hip fractures in his review of polytrauma patients across three decades following routine usage of anteroposterior pelvic radiograph.7 Risk factors for missing injuries include a higher Injury Severity Score >15, altered mental status, a Glasgow Coma Scale (GCS) score <8, a stay in the intensive care unit, and need for emergency surgery.7 A high index of suspicion is required to diagnose all injuries efficiently, and the importance of a carefully performed tertiary survey cannot be overemphasized.
3. Diagnostic protocol and imaging techniques in extremity injuries
Diagnostic evaluation and management of Polytrauma must go hand in hand, and errors in sequential management have been reported to increase mortality rates in Polytrauma. Gruen et al. reported an error-related mortality of 2.4% in trauma, which mainly included failure to secure or protect an airway and delayed control of hemorrhage.8 Investigation in Polytrauma following a primary and secondary survey consists of a chest and pelvis plain radiograph and possibly a CT at the discretion of the trauma team considering the hemodynamic status of the patient. Following the pioneering work of Enderson et al. tertiary survey within 24 h of injury by a physician who is not involved in the initial evaluation has become a part of Polytrauma management.9 The tertiary survey typically includes a complete physical examination, a review of all prior imaging, and blood reports followed by further imaging. Hand and foot injuries are the most common to be missed despite a careful tertiary survey.
A discussion on other imaging modalities such as Focused Assessment with Sonography for Trauma (FAST), CT (whole-body versus selective), and Angiogram is beyond the scope of this review article. However, it is worth mentioning that vascular injuries may go undiagnosed, especially in a hemodynamically unstable patient. While angiography is the gold standard diagnostic tool, an ankle-brachial pressure index (ABPI) < 1 is a non-invasive tool indicative of peripheral vascular injury. However, in patients with extremity injuries and hemodynamic instability, its sensitivity is questionable.10 Recently, Montorfano et al. proposed a FAST D protocol, where the presence of flow and the aspects of the Doppler waveform of the dorsalis pedis artery (DPA) and posterior tibial artery (PTA) of the injured lower limb (2PFD) were assessed and found to have a sensitivity and specificity of 100% when compared to standardized Color Duplex Doppler (SD) evaluation.11 However, the overall high accuracy of 98% for Doppler Ultrasound (DUS) is overshadowed by the time and expertise required in diagnosing vascular lesions.12
Stevens et al. recommended an orthopedician to do a standardized tertiary evaluation starting from upper to lower extremity.6 It involves a systematic assessment of osseous, musculotendinous, and ligamentous injuries, followed by a neurovascular examination, and finally, the inspection of the pelvis and spine to reduce the chance of missed injuries, which seems practical and can be performed easily.
Our practice is to use a FAST scan for an initial assessment in all polytrauma patients followed by a whole-body CT scan in patients with positive or inconclusive findings. Our protocol is that an unstable patient always goes to Operation theatre and not to the CT scan. Apart from a tertiary survey by an orthopedic surgeon, a standardized survey by a team of the intensivist, anesthesiologist, neurosurgeon, orthopedic and plastic surgeon is a part of our routine and this has led to a decline in the incidence of missed injuries and helped in making appropriate decisions.
The development of standard imaging and diagnostic protocols with the efficient and safe use of available technology including whole-body CT is needed. Such protocols should incorporate the variations encountered in different population groups and geographical areas.
4. Hemorrhagic shock and resuscitation
The pathophysiology of hemorrhagic shock, which contributes up to 50% of all mortalities in trauma, has only been recently understood.13 At the cellular level, hemorrhagic shock leads to insufficient oxygen delivery to meet the tissue demand resulting in a transition from aerobic to anaerobic metabolism. The resultant accumulation of lactic acid, oxygen radicals, and release of damage-associated molecular patterns (DAMP) set up a systemic inflammatory response. Hypovolemia and vasoconstriction cause hypoperfusion, resulting in end-organ damage and multiple organ dysfunction syndromes (MODS) in those who survive the initial vascular insult. Adaptive changes include the formation of hemostatic plugs through the activation of platelets and the coagulation cascade. The initial concept of aggressive fluid administration to normalize blood pressure has been detrimental due to the dislodgement of these clots, which is familiarly known as the “pop the clot” phenomenon.14
Military physicians developed Damage Control Resuscitation (DCR) measures after witnessing the benefits of whole-blood based transfusion. They noted a significant reduction in dilutional coagulopathy by replacing crystalloids, with whole blood. The primary aim of preventing or reversing coagulopathy through the DCR approach includes permissive hypotension, lesser usage of crystalloids, and liberal usage of plasma and platelets.15 The goal of permissive hypotension is to maintain systolic blood pressure (SBP) of 80–90 mmHg to ensure end-organ perfusion until major bleeding is brought under control in the initial phase following trauma.16 However, the ill-effects of decreasing the intracerebral perfusion pressure in severe traumatic brain injury (TBI), has been well documented. In patients with severe TBI (GCS ≤8), maintenance of a mean arterial pressure ≥80 mm Hg is recommended, which approximately equates to the restoration of a palpable radial pulse.17
The conventional DCR strategy of rapidly transfusing 1–2L of crystalloids followed by RBC transfusion has been renewed to a 1:1:1 policy of transfusing plasma, platelets, and RBCs. In the Pragmatic Randomized Optimal Platelet and Plasma Ratios (PROPPR) trial, improved survival at 3 h post-admission and a reduction in mortality caused by exsanguination in the first 24 h was observed in the 1:1:1 group compared to the 1:1:218. Improvement in survival rates and rapid hemorrhagic control has been achieved by the early administration of a balanced ratio of FFP, PLTs, and RBCs in multiple studies.19,20 A meta-analysis assessed three prospective studies and seven retrospective observational studies that compared different fluid administration strategies in trauma patients. The quantitative synthesis indicated that initial liberal fluid resuscitation strategies might be associated with higher mortality when compared to restricted fluid strategies, both in RCTs and observational studies in trauma patients. However, the authors cautioned that the available studies are subject to a high risk of selection bias and clinical heterogeneity21,22.
Our practice is blood-based resuscitation as described by the PROPPR trial and maintenance of a mean arterial pressure ≥80 mm Hg. This strategy has led to improved survival and better outcomes in our patients.
Future research should concentrate on methods for quantifying the amount of blood loss, especially in blunt trauma. Also, appropriate interventions, devices, and biomarkers for assessing tissue perfusion and ischemic risk should be developed.23 Similarly, large scale validation of resuscitation strategies is needed across different population groups to improve the existing protocols.
5. Endpoints of resuscitation, and predictive models of complications in polytrauma patients
Various laboratory markers have been used heterogeneously to assess the severity and recovery of the traumatic insult. They can broadly be classified into markers of tissue hypoxia, and trauma-related coagulopathy. The serum lactate level is an indicator of anaerobic metabolism and is the most widely used parameter to monitor tissue hypoxia. While reduced lactate levels and good lactate clearance represents the restoration of peripheral blood flow, lactate metabolism can also be influenced by alcohol consumption, chronic renal failure, metabolic diseases, medication, sepsis, seizures, CO-poisoning, strenuous exercise, and respiratory or hepatic failure. Calculation of Base deficit is yet another measure of acidosis and has been used to quantify the severity of hemorrhagic shock. A Base deficit of (6–10 mmol/L) is considered as moderate shock beyond which the risk of coagulopathy increases tremendously.24 Biomarkers for trauma-related coagulopathy include fibrinogen level, D dimer level, platelet count, Prothrombin time, and activated partial thromboplastin time. Real-time monitoring of coagulopathy using critical administration threshold (CAT), the assessment of blood consumption (ABC) score, and other dynamic platelet function tests (diamond of death) such as thrombelastography (TEG) and ROTEM (Rotational Thromboelastometry) are now available in advanced trauma centers.25
These parameters have also been used to predict outcomes of initial resuscitative measures and therefore used for timing the definitive surgical interventions. Vallier et al., in the “Early Appropriate Care” (EAC) protocol, recommend definitive fracture fixation within 36 h on achieving the following parameters of lactate <4.0 mmol/L, pH ≥ 7.25, or base excess (BE) ≥−5.5 mmol/L.26 Halvachizadeh et al. compared various scaling systems that used different combinations of parameters to assess physiological states of coagulopathy, acidosis, and soft tissue injuries. The polytrauma grading score (PTGS; shock, coagulation, and ISS), was found to be superior to the clinical grading scale (CGS; acidosis, shock, coagulation, and soft tissue injuries), and the modified clinical grading scale (mCGS) in predicting late complications, sepsis, and/or pneumonia. On the other hand, the early appropriate care protocol (EAC; acid-base changes) was a good predictor of hemorrhage-induced early mortality but not for late complications. Authors have mentioned that the prediction of complications is more precise after using values that cover different physiological systems (coagulation, hemorrhage, acid-base changes, and soft tissue damage) when compared with using values of only one physiological system (e.g., acidosis)27.
In our practice, we use a combination of hemodynamic stability, acid-base markers (serum lactate and base deficit) along with other physiological markers (PT, INR, platelet count, fibrinogen) for assessing the adequacy of resuscitation. Patients who show adequate response to resuscitation with improvement. in clinical parameters and with moderate severity of the injury as determined by ISS score are taken up for definitive fixation. Patients who are poor responders and borderline patients with severe systemic injuries and patients in extremis are managed according to principles of damage control orthopedics.
Future recommendations include validation of recent technological advancements like dynamic platelet function tests on outcomes in polytrauma patients. Various predictive models should be validated in different populations for large scale applications in routine clinical care. The advent of Artificial Intelligence and patient-specific genomics present exciting opportunities for developing new markers for assessing the adequacy of resuscitation and development of patient-specific management protocols based on individual differences in response to injury.28
6. Traumatic brain injury (TBI) and extremity injury management
In patients with coexisting extra-cranial injuries and TBI, the disruption of the blood-brain barrier potentiates the entry of pro-inflammatory cytokines, and therefore, the brain is more susceptible to secondary insults, like ischemia, hypotension, sepsis, seizures, or surgical interventions.29 The high incidence of neurological deterioration (48%) and coagulopathy (55%) and chances of hypotension following orthopedic intervention which might further worsen cerebral edema warrants a severe debate between “Early Total Care” and “Damage Control Orthopaedics.30 The risk of secondary brain damage due to intraoperative blood loss, inflammatory responses, hypotension, hypoxia, and coagulopathy outweighs the advantages of early fixation for extremity fractures (prevention of soft tissue damage, callus formation, joint stiffness, and fat and pulmonary embolism) in TBI.31 Townsend et al. reported an 8-fold increase in the risk of intraoperative hypotension during fixation of long bones within 2 h of admission and 2-fold within 24 h of admission. 74% of these patients experienced a low cerebral perfusion pressure of <70 mm Hg and this risk lasted even longer than 24 h which warrants a delay of 24 h between injury and fracture fixation to prevent hypoxia, hypotension, and low cerebral perfusion pressure.32 Contrary to these publications, few authors have recommended early fracture fixation in patients with TBI as it simplifies treatment while delayed fixation worsens outcomes. Smith and Cunningham reported extended hospitalization with increased ICU stay and more pulmonary and neurologic problems in patients with delayed fracture fixation33. Starr et al. reported an increased incidence of pulmonary, cerebral complications, and mortality in delayed fixation34. Lu et al reported their findings of metaanalysis of fourteen studies on the timing of extremity fracture fixation in patients with Traumatic Brain Injury. They reported no statistically significant association between fixation timing and mortality, the incidence of adverse neurologic events, pneumonia, ARDS, and ICU length of stay. On the other hand, they reported that delayed fracture fixation results in extended ICU stay, pulmonary complications, neurological worsening, nonunion, and malunion.31 Thus management of extremity fracture with concomitant TBI should depend on the physiological reserve, the severity of brain injury, hemodynamic stability at presentation, nature of extremity injury, and if general condition permits, early definitive fixation should be the norm rather than the exception. (Fig. 1, Fig. 2).
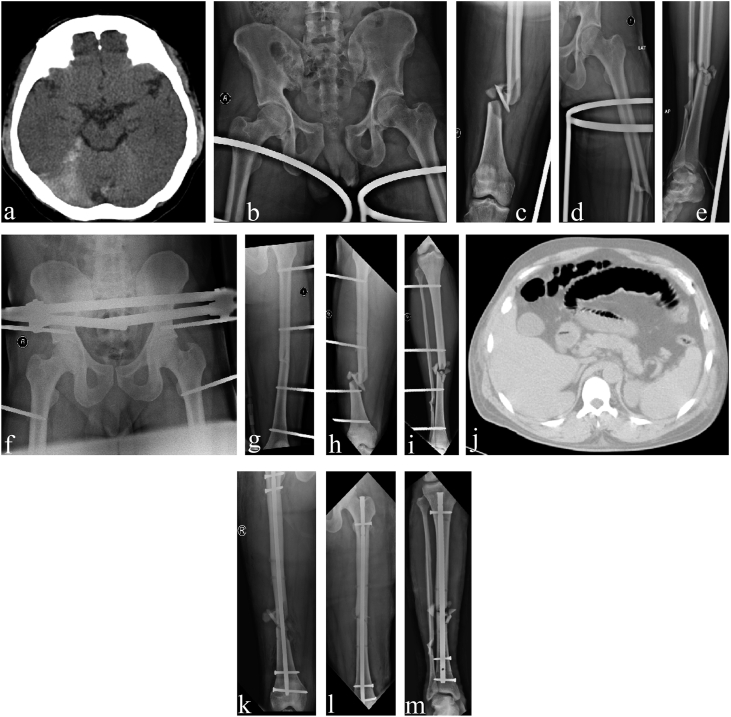
Fig. 1.
A 23-year-old gentleman diagnosed with closed fracture shaft of the right femur (a), closed fracture right tibia (b), closed fracture both bone right forearm (c), closed fracture left distal radius (d), and traumatic brain injury-Right frontal lobe contusion with SAH right parietal region (e). On arrival his vitals were stable, GCS was E4, V5, and M6 (15/15), Serum lactate was 1.7 mmol/L. He underwent external fixator application for the right femur and tibia fractures on day 1. Subsequently, he underwent definitive fixation of right femur (h) and tibia fractures (i) and both upper limb fractures (j,k) and achieved a good outcome.
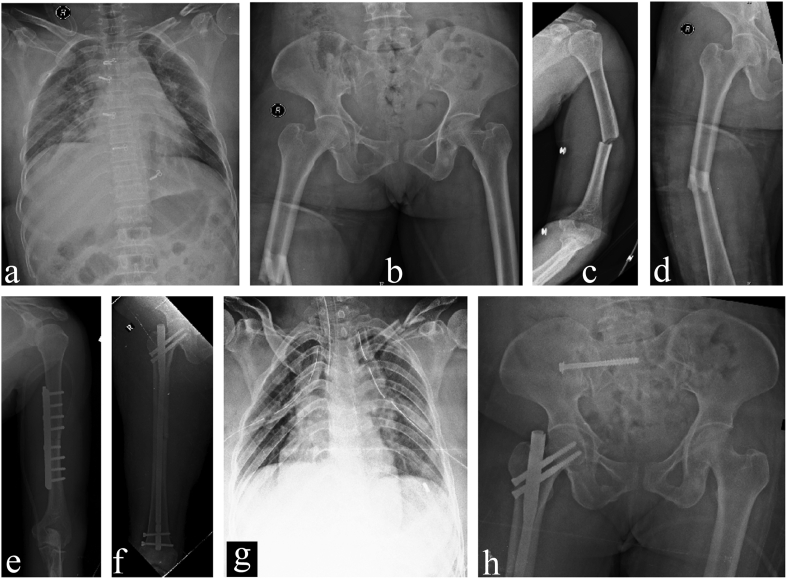
Fig. 2.
A 41-year-old gentleman diagnosed with traumatic brain injury-Subarachnoid hemorrhage with extradural hemorrhage right parietal lobe (a), APC type 2 pelvic injury (b), closed bilateral shaft of femur fracture (c,d) and closed both bone fracture right leg (e). On arrival, vitals were stable, GCS was E4, V4, and M5 (13/15), serum lactate was 4.6 mmol/L. He underwent external fixator application for pelvic injury (f), bilateral femur fractures (g,h), and tibia fracture (i) on day 1. On day 5, the patient became unstable with abdominal distension and was diagnosed with ileal perforation with closed-loop small bowel obstruction (j). Emergency laparotomy was performed with ileal resection and anastomosis. Subsequently, definitive fixation of both femur (k,l) and tibia fractures (m) were performed. The patient achieved a satisfactory outcome.
7. Chest injury and extremity injury management
Patients with chest injury are at a higher risk of developing ARDS, and it is pertinent that DCO or EAC measures be applied appropriately to prevent the “second hit” in Polytrauma (Fig. 3). While early and overzealous definitive fracture fixation increases the risk of ARDS, delayed fixation increases the rate of pulmonary complications. In a retrospective review of 106 patients with multiple injuries, who underwent early intramedullary nail femur fixation, Pape et al. observed an overall reduction in morbidity in those with lesser severity of chest injury compared to an increased risk of both ARDS and death in severe chest injuries.35 Their recommendation of alternate methods of fixation or delayed nailing in those having severe chest injury (Abbreviated Injury Scale > 2), stands valid considering the increased levels of inflammatory markers (IL-6 and Elastase) following intramedullary reaming observed by Giannoudis et al..36 However, Charash et al. and Bone et al. recommended early femur fixation in Polytrauma to avoid pulmonary and other complications.37,38
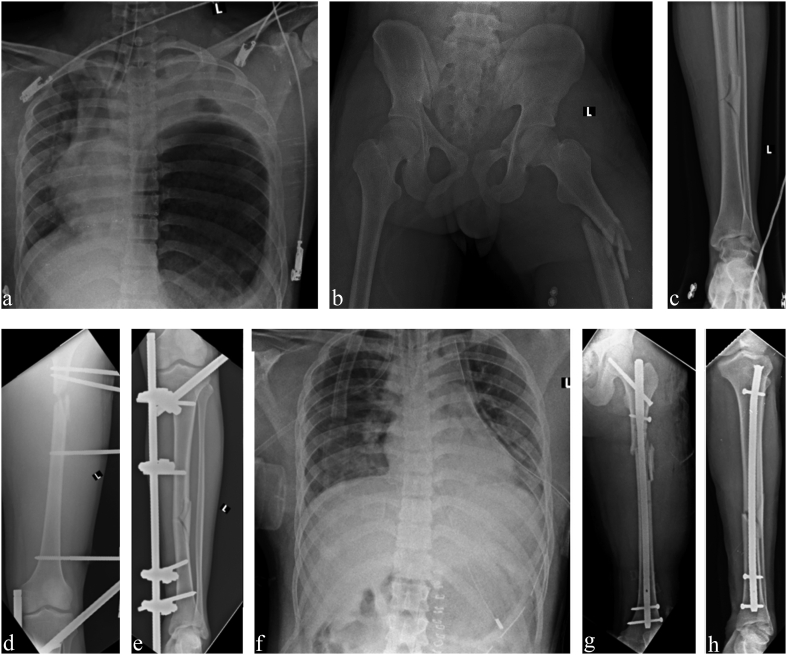
Fig. 3.
A 45-year-old lady was diagnosed with bilateral hemopneumothorax with multiple rib fractures (a), pelvic injury (b), closed shaft of left humerus (c) and right femur fractures (d). On arrival, her vitals were stable, serum lactate was 2.6 mmol/L, pH was 7.34, and base excess was −0.3 mmol/L. She underwent definitive fixation of the humerus (e), femur (f), bilateral ICD insertion (g), and Right sacroiliac joint (h) as per EAC protocol within 36 h.
Given these controversies, the quantification of the severity of chest trauma was thought to allow the prediction of complications and allow better management of polytrauma patients with a chest injury. Subsequently, the availability of scoring systems regarding chest trauma like Thoracic Trauma Severity (TTS) has improved the prediction of complications.39 Pape et al. published recommendations regarding fracture management in polytrauma patients. They advocated a staged surgical approach for fracture stabilization instead of simultaneous multiple fracture fixations within 24 h of injury in unstable patients at risk and definitive fracture fixation in stable patients based on individual patient physiology rather than a “window of opportunity”.40 Considering the benefits of early fracture fixation in polytrauma patients with chest injury with reduced complications and mortality, definitive fracture fixation should probably continue to be performed on stable polytrauma patients with a chest injury.
8. Abdominal injury and extremity injury management
Abdominal injuries constitute one of the most common causes of uncontrolled bleeding in trauma. Humeral shaft fractures have been associated with a higher chance of other upper extremity and lower extremity injuries in motor vehicle collisions. They also serve as a predictor for concomitant abdominal injuries, especially that of the liver.41 Similarly, lower extremity fractures are frequently associated with intraabdominal injuries in pedestrians.42 The high-energy mechanisms related to these injuries result in pelvic disruption and acetabular fractures. Proximal femoral fractures are commonly present along with these injuries. Utmost care is essential to diagnose and manage these highly unstable abdominal injuries and pelvic fractures in this case are usually managed by external fixators accompanied by diagnostic laparotomy or pelvic packing to avoid rapid exsanguination. Early internal fixation can be deleterious and definitive surgery is best delayed and performed only in stable patients.43 The open abdomen is a relatively new and increasingly common strategy for the management of abdominal emergencies in both trauma and general surgery for the prevention and mitigation of abdominal compartment syndrome. The use of an abbreviated laparotomy can reduce mortality associated with conditions such as abdominal compartment syndrome; however, the resulting open abdomen is a complex clinical problem44. Another concern is the perception of cross-contamination of elective open surgical approaches, which might mandate an obligatory delay of stabilizing major fractures after abdominal wall closure. However, a postponement over three weeks has been proven to be associated with a worse surgical outcome, especially regarding reduction quality in pelvic and acetabulum fractures.43,45 Further, Glass et al. reported a significant decrease in clinically relevant surgical site infections, following definitive early fracture fixation, including long bones, pelvic ring, acetabular fractures, and spinal fusions, even in the presence of an open abdomen when compared with delayed fracture fixation.44 Similarly, Vallier et al reported that early definitive fracture fixation including spine fixations are safe in polytrauma patients as part of the “Early Appropriate Care” protocol26. Because of the benefits of early fracture fixation on pulmonary function and overall mortality, early fracture fixation should probably continue to be performed on carefully selected stable patients with an abdominal injury (Fig. 2, Fig. 4).
Fig. 4.
A 18-year-old male diagnosed with grade 2 splenic laceration, intraperitoneal bladder rupture with diaphragmatic hernia left side (a) with left superior and inferior pubic rami fracture and closed diaphyseal fractures of the left femur (b) and tibia (c). On arrival, patient showed bradycardia, blood pressure of 114/60 mm Hg, GCS was E4, V5, and M6 (15/15) with absent breath sounds on the left side chest. Serum lactate was 7.2 mmol/L. After resuscitation, bladder and diaphragmatic hernia repair along with ICD insertion (f), splenectomy and external fixator application for the left femur (d) and tibia (e) fractures on day 1 were performed. Definitive fixation of the left femur (g) and tibia fractures (h) was performed later.
9. Open extremity injuries
Irrespective of the zone of injury, the management of any open extremity involves simultaneous stabilization (temporary/definitive) and debridement. Bacterial contamination can be as high as 70% in open injuries, and antibiotic prophylaxis must be initiated much earlier.46 The timing of surgical debridement and reconstructive procedures has been controversial.47 No significant differences were noted in 10-day infection rates when patients undergoing debridement within 6 h were compared to those between 6 and 72 h in a prospective, double-blind study.48 Currently, it is recommended to perform debridement within 24 h of injury.49 Cimbanassi et al. published the results of the 11th trauma update consensus conference held in Milan, Italy. The overall consensus was that “In open fractures, early debridement within 24 h should be recommended and early closure of most grade I, II, IIIa performed. In mangled extremities, limb salvage should be considered for non–life-threatening injuries, mostly of upper limb”46. While meticulous surgical debridement plays an important role in preventing the risk of infections and nonunions, its extent and adequacy are beyond the scope of discussion here. An orthoplastic approach is recommended in all these injuries (Fig. 5).50
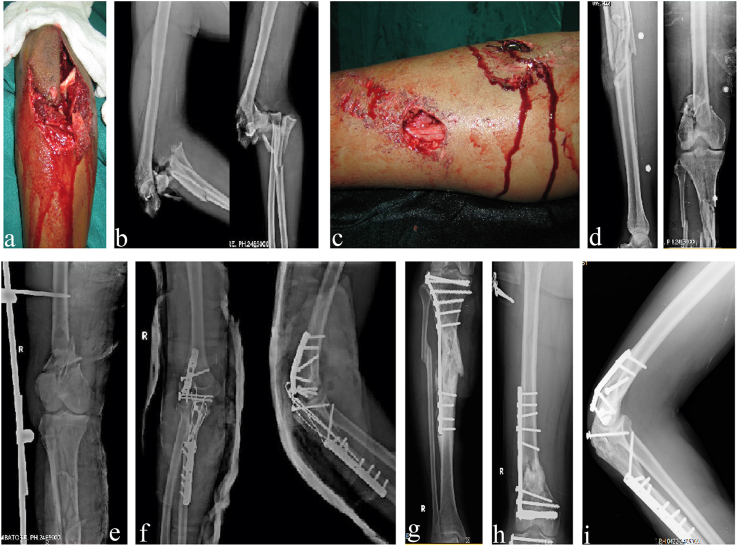
Fig. 5.
A 40-year-old gentleman diagnosed with type 3b open side swipe injury right elbow (a,b) and Open floating knee injury right lower limb (c,d). On arrival his vitals were stable, GCS was E4, V5, and M6 (15/15), serum lactate was 2.5 mmol/L. He underwent external fixator application for the right femur and tibia fractures (e) and debridement and definitive fixation of right elbow injury on day 1 (f, i). Subsequently, he underwent definitive fixation of the right femur (g) and tibia fractures (h) and achieved good outcome.
Recently, Mauffrey et al. had summarised current evidence-based strategies to minimize the risk of infection in fractures.51 These include.
-
1.
Early Initiation of systemic antibiotic coverage directed at Gram-positive organisms
-
2.
Addition of Gram-negative coverage for type III open fractures.
-
3.
High-dose penicillin for fecal or potential clostridial contamination (farm injuries).
-
4.
Avoidance of Fluoroquinolones as they offer no advantage compared with cephalosporin or aminoglycoside and also because they have a detrimental effect on fracture healing and higher infection rates in type III open fractures.
-
5.
Continuation of antibiotics for 72 h in type III open fractures, following injury but not beyond 24 h after the achievement of soft-tissue coverage.
-
6.
Once-daily aminoglycoside dosing as a safe and effective measure for types II and III open fractures.
Based on this evidence, they recommend patients with type I or II open fractures to receive a first-generation cephalosporin beginning with a 2 g intravenous (IV) loading dose, then 1 g IV every 8 h for three doses (24 h). Alternatives in Penicillin allergy is a 900-mg loading dose of clindamycin and then 900 mg q 8 h × 3 (24 h). Type III open fractures should receive either a third-generation cephalosporin or a first-generation cephalosporin in addition to aminoglycoside for three days. Patients with possible fecal type contamination should also receive penicillin prophylaxis to address Clostridia. Although it is impossible to eliminate infectious complications, these guidelines can optimize the outcomes.
10. Fixation strategies in open extremity fractures associated with polytrauma
While the primary aim is to provide adequate mechanical stability with minimal complications, fixation strategies of open fractures vary depending on the overall physiological condition of the patient, type, and pattern of fracture, the degree of bone loss, soft tissue condition, type of soft tissue coverage needed, and level of contamination. Skeletal stabilization should be undertaken quickly, especially in the setting of the vascular deficit, and it must be designed to allow future soft tissue reconstruction.52 External fixation, especially half unilateral pin frames, is the workhorse for skeletal stabilization in open fractures as it provides a swift versatile method of providing stability without the need for additional exposure or periosteal stripping.53 However, their use as a means of definitive management is no longer recommended. Recently, a meta-analysis comparing the management of open tibial fractures showed no difference in the rate of nonunion and infection with external fixation when compared with internal fixation methods. However, there were statistically significant differences in the rates of malunion and the need for further surgery, favoring the use of internal fixation as definitive treatment.54 The external fixator can be used as a temporary stabilization method with conversion to internal fixation at an appropriate time (Fig. 5).
Primary internal fixation can be considered if soft tissue cover could be achieved within 48–72 h. The choice of plate or nailing depends on the location of the injury. Periarticular injuries with or without articular surface involvement can be managed by plating. In the case of lower limb diaphyseal fractures, IM nailing either as a primary or secondary procedure is the method of choice for definitive fixation. The choice of reamed or unreamed nail is still a matter of debate. Both show comparable outcomes in terms of infection rates, risk of nonunion, and rates of reoperation. Recent advances include plate assisted nailing of Type III B diaphyseal tibia fractures, which allows greater cortical contact aiding fracture stability and is not associated with an increased rate of deep infection or nonunion.55,56
11. Author’s preferred management of extremity fractures in polytrauma
Our treatment protocol for extremity fractures associated with polytrauma is based on the following considerations: hemodynamic stability, the physiological reserve of the patient, and associated injuries. Early definitive fixation is preferred for isolated long bone diaphyseal fractures of lower extremities in hemodynamically stable patients with a good physiological reserve. In borderline and hemodynamically unstable cases or patients with low physiological reserve, in patients with multiple lower extremity diaphyseal fractures and periarticular fractures, we prefer rapid primary stabilization using an external fixator initially followed by the definitive fixation once the patient’s general condition improves, preferably within two weeks. In the case of multiple lower extremity diaphyseal fractures, we prefer to fix the fractures around the hip and femur first, followed by other lower extremity fractures. This enables us for the early mobilization of the patient in bed and simplifies the care of the patient. Although no suggestions have been made for the management of multiple lower extremity fractures, we avoid multiple simultaneous intramedullary nailing procedures and follow a staged protocol especially in case of borderline patients. In the hierarchy of Polytrauma with extremity fractures, the priority of fixation of upper extremity fractures generally follows the axial and lower extremity injuries. Routinely, upper extremity fractures are managed after the definitive stabilization of lower extremity fractures. The current recommendations for management of extremity injuries in polytrauma patients and the future research areas are summarised in Table 1.
Table 1.
Current recommendations and future research in management of extremity fractures in polytrauma patients.
| Parameters | Current recommendations | Future research |
|---|---|---|
| Diagnostic protocol and imaging techniques |
|
|
| Endpoints of Resuscitation, and predictive models of complications |
|
|
| Traumatic Brain Injury (TBI) and Extremity injury management |
|
|
| Chest Injury and Extremity injury management |
|
|
| Abdominal Injury and Extremity injury management |
|
|
| Open Extremity Injuries |
|
Future recommendations in extremity fracture management in polytrauma:
-
1.
The strategy of management of polytrauma patients is evolving rapidly. The newly developed strategies of treatment like “Early Appropriate Care” needs to be validated across large and heterogeneous population groups before their large-scale application across different geographical areas.
-
2.
The advent of various Clinical Decision Support Tools in other fields of medicine encourages further research in the case of polytrauma patients to develop such tools that can help in choice and timing of surgical interventions in polytrauma patients with varying patterns of injury.28
-
3.
With rapid advances in identifying immunological markers, the development of validated scoring systems and prognostic indicators with the help of precision medicine could be the next step in improving the care of polytrauma patients.28
-
4.
Current research in the field of immunological markers associated with injury is targeted on validating theoretical beliefs of a complex interplay of pro and anti-inflammatory cytokines during the treatment of polytrauma patients for developing treatment algorithms. With the help of bioinformatics tools like topological data analysis might improve the phenotyping of injury patterns, precision diagnosing, and treatment planning.57,58
-
5.
Identification of specific immunological markers associated with the development of complications and poor or good outcomes needs to be researched more extensively.28
12. Conclusion
The management of the extremities in polytrauma patients is determined mainly by hemodynamic stability and the presence of life-threatening associated injuries. Damage control resuscitation has been successful in achieving hemodynamic stability much earlier than traditional measures. With reliable, measurable parameters available for assessing physiological recovery from systemic traumatic insult, early definitive management of extremities is favorably considered for reaping the benefits of mobilization and ambulation. Future research should be directed towards identifying precision methods and utilization of big data and artificial intelligence in improving the management and outcome of polytrauma patients.
Disclosure of funding
Ganga Orthopaedic Research and Education Foundation (GOREF) has provided non financial help in preparation of the manuscript and writing assistance.
References
- 1.Nicola R. Early total care versus damage control: current concepts in the orthopedic care of polytrauma patients. ISRN Orthop. 2013;2013:1–9. doi: 10.1155/2013/329452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee M., Bouillon B., Shafizadeh S., Paffrath T., Lefering R., Wafaisade A. Epidemiology of extremity injuries in multiple trauma patients. Injury. 2013;44(8):1015–1021. doi: 10.1016/j.injury.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Braun B.J., Holstein J., Fritz T. Polytrauma in the elderly: a review. EFORT Open Rev. 2016;1(5):146–151. doi: 10.1302/2058-5241.1.160002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dhar S.A., Bhat M.I., Mustafa A. “Damage control orthopaedics” in patients with delayed referral to a tertiary care center: experience from a place where Composite Trauma Centers do not exist. J Trauma Manag Outcome. 2008;2(1) doi: 10.1186/1752-2897-2-2. 2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gray M., Chung J., Aguila F., Williams T.G., Teraoka J.K., Harris O.A. Long-term functional outcomes in military service members and veterans after traumatic brain injury/polytrauma inpatient rehabilitation. Arch Phys Med Rehabil. 2018;99(2):S33–S39. doi: 10.1016/j.apmr.2017.08.465. [DOI] [PubMed] [Google Scholar]
- 6.Stevens N.M., Tejwani N. Commonly missed injuries in the patient with polytrauma and the orthopaedist’s role in the tertiary survey. JBJS Rev. 2018;6(12):e2. doi: 10.2106/JBJS.RVW.18.00014. [DOI] [PubMed] [Google Scholar]
- 7.Pfeifer R., Pape H.-C. Missed injuries in trauma patients: a literature review. Patient Saf Surg. 2008;2(1) doi: 10.1186/1754-9493-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gruen R.L., Jurkovich G.J., McIntyre L.K., Foy H.M., Maier R.V. Patterns of errors contributing to trauma mortality: lessons learned from 2594 deaths. Ann Surg. 2006;244(3):371–378. doi: 10.1097/01.sla.0000234655.83517.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Enderson B.L., Reath D.B., Meadors J., Dallas W., DeBoo J.M.M.K. The tertiary trauma survey: a prospective study of missed injury. J Trauma. 1990;30(6):666–670. https://pubmed.ncbi.nlm.nih.gov/2352294/ [PubMed] [Google Scholar]
- 10.Kurtoğlu M., Dolay K., Karamustafaoğlu B., Yanar H., Kuzkaya M. The role of the ankle brachial pressure index in the diagnosis of peripheral arterial injury. Ulus Travma Ve Acil Cerrahi Derg Turk J Trauma Emerg Surg TJTES. 2009;15(5):448–452. [PubMed] [Google Scholar]
- 11.Montorfano M.A., Montorfano L.M., Perez Quirante F., Rodríguez F., Vera L., Neri L. The FAST D protocol: a simple method to rule out traumatic vascular injuries of the lower extremities. Crit Ultrasound J. 2017;9(1) doi: 10.1186/s13089-017-0063-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Montorfano M.A., Pla F., Vera L., Cardillo O., Nigra S.G., Montorfano L.M. Point-of-care ultrasound and Doppler ultrasound evaluation of vascular injuries in penetrating and blunt trauma. Crit Ultrasound J. 2017;9(1) doi: 10.1186/s13089-017-0060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cannon J.W. Hemorrhagic shock. N Engl J Med. 2018;378(4):370–379. doi: 10.1056/NEJMra1705649. [DOI] [PubMed] [Google Scholar]
- 14.Wang C.H., Hsieh W.H., Chou H.C. Liberal versus restricted fluid resuscitation strategies in trauma patients: a systematic review and meta-analysis of randomized controlled trials and observational studies. Crit Care Med. 2014;42(4):954–961. doi: 10.1097/CCM.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 15.Cotton B.A., Reddy N., Hatch Q.M. Damage control resuscitation is associated with a reduction in resuscitation volumes and improvement in survival in 390 damage control laparotomy patients. Ann Surg. 2011;254(4):598–605. doi: 10.1097/SLA.0b013e318230089e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duchesne J.C., McSwain N.E., Cotton B.A. Damage control resuscitation: the new face of damage control. J Trauma Inj Infect Crit Care. 2010;69(4):976–990. doi: 10.1097/TA.0b013e3181f2abc9. [DOI] [PubMed] [Google Scholar]
- 17.Brenner M., Stein D.M., Hu P.F., Aarabi B., Sheth K., Scalea T.M. Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. J Trauma Acute Care Surg. 2012;72(5):1135–1139. doi: 10.1097/TA.0b013e31824af90b. [DOI] [PubMed] [Google Scholar]
- 18.Baraniuk S., Tilley B.C., Del Junco D.J. Pragmatic randomized optimal platelet and plasma ratios (PROPPR) trial: design, rationale and implementation. Injury. 2014;45(9):1287–1295. doi: 10.1016/j.injury.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ishikura H., Kitamura T. Trauma-induced coagulopathy and critical bleeding: the role of plasma and platelet transfusion. J Intensive Care. 2017;5(1):2. doi: 10.1186/s40560-016-0203-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johansson P.I., Oliveri R.S., Ostrowski S.R. Hemostatic resuscitation with plasma and platelets in trauma. J Emergencies, Trauma, Shock. 2012;5(2):120–125. doi: 10.4103/0974-2700.96479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kudo D., Yoshida Y., Kushimoto S. Permissive hypotension/hypotensive resuscitation and restricted/controlled resuscitation in patients with severe trauma. J Intensive Care. 2017;5(1):1–8. doi: 10.1186/s40560-016-0202-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang C.H., Hsieh W.H., Chou H.C. Liberal versus restricted fluid resuscitation strategies in trauma patients: a systematic review and meta-analysis of randomized controlled trials and observational studies. Crit Care Med. 2014;42(4):954–961. doi: 10.1097/CCM.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 23.Huber W., Zanner R., Schneider G., Schmid R., Lahmer T. Assessment of regional perfusion and organ function: less and non-invasive techniques. Front Med. 2019;6:50. doi: 10.3389/fmed.2019.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mutschler M., Nienaber U., Brockamp T. Renaissance of base deficit for the initial assessment of trauma patients: a base deficit-based classification for hypovolemic shock developed on data from 16,305 patients derived from the TraumaRegister DGU®. Crit Care. 2013;17(2) doi: 10.1186/cc12555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cotton B.A., Faz G., Hatch Q.M. Rapid thrombelastography delivers real-time results that predict transfusion within 1 hour of admission. J Trauma Inj Infect Crit Care. 2011;71(2):407–417. doi: 10.1097/TA.0b013e31821e1bf0. [DOI] [PubMed] [Google Scholar]
- 26.Vallier H.A., Moore T.A., Como J.J. Complications are reduced with a protocol to standardize timing of fixation based on response to resuscitation. J Orthop Surg Res. 2015;10(1):1–9. doi: 10.1186/s13018-015-0298-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Halvachizadeh S., Baradaran L., Cinelli P., Pfeifer R., Sprengel K., Pape H.C. How to detect a polytrauma patient at risk of complications: a validation and database analysis of four published scales. PloS One. 2020;15(1):1–16. doi: 10.1371/journal.pone.0228082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKinley T.O., Lisboa F.A., Horan A.D., Gaski G.E., Mehta S. Precision medicine applications to manage multiply injured patients with orthopaedic trauma. J Orthop Trauma. 2019;33(6):S25–S29. doi: 10.1097/BOT.0000000000001468. [DOI] [PubMed] [Google Scholar]
- 29.McDonald S.J., Sun M., Agoston D.V., Shultz S.R. The effect of concomitant peripheral injury on traumatic brain injury pathobiology and outcome. J Neuroinflammation. 2016;13(1) doi: 10.1186/s12974-016-0555-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stein S.C., Young G.S., Talucci R.C., Greenbaum B.H., Ross S.E. Delayed brain injury after head trauma: significance of coagulopathy. Neurosurgery. 1992;30(2):160–165. doi: 10.1227/00006123-199202000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Lu S., Du T., Sun Z., Xu L., Tong X., Yan H. Timing of extremity fracture fixation in patients with traumatic brain injury: a meta-analysis of prognosis. World Neurosurg. 2020;133:227–236. doi: 10.1016/j.wneu.2019.09.136. [DOI] [PubMed] [Google Scholar]
- 32.Townsend R.N., Lheureau T., Protetch J., Riemer B., Simon D. Timing fracture repair in patients with severe brain injury (Glasgow Coma Scale Score <9) J Trauma Inj Infect Crit Care. 1998;44(6):977–983. doi: 10.1097/00005373-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Smith J.M., Cunningham T.J. Timing of femur fracture fixation in patients with head injury. J Orthop Trauma. 2000 125-125. [Google Scholar]
- 34.Starr A.J., Hunt J.L., Chason D.P., Reinert C.M., Walker J. Treatment of femur fracture with associated head injury. J Orthop Trauma. 1998;12(1):38–45. doi: 10.1097/00005131-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Pape H.C., Auf’M’kolk M., Paffrath T., Regel G., Sturm J.A., Tscherne H. Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion—a cause of posttraumatic ARDS? J Trauma Inj Infect Crit Care. 1993;34(4):540–548. doi: 10.1097/00005373-199304000-00010. [DOI] [PubMed] [Google Scholar]
- 36.Giannoudis P.V., Smith R.M., Bellamy M.C., Morrison J.F., Dickson R.A., Guillou P.J. Stimulation of the inflammatory system by reamed and unreamed nailing of femoral fractures. An analysis of the second hit. J Bone Jt Surg - Ser B. 1999;81(2):356–361. doi: 10.1302/0301-620X.81B2.8988. [DOI] [PubMed] [Google Scholar]
- 37.Charash W.E., Fabian T.C., Croce M.A. Delayed surgical fixation of femur fractures is a risk factor for pulmonary failure independent of thoracic trauma. J Trauma Inj Infect Crit Care. 1994;37(4):667–672. doi: 10.1097/00005373-199410000-00023. [DOI] [PubMed] [Google Scholar]
- 38.Bone L.B., Johnson K.D., Weigelt J., Scheinberg R. Early versus delayed stabilization of femoral fractures. A p... : JBJS. JBJS. 1989;71(3):336–340. [PubMed] [Google Scholar]
- 39.Daurat A., Millet I., Roustan J.P. Thoracic Trauma Severity score on admission allows to determine the risk of delayed ARDS in trauma patients with pulmonary contusion. Injury. 2016;47(1):147–153. doi: 10.1016/j.injury.2015.08.031. [DOI] [PubMed] [Google Scholar]
- 40.Pape H.C., Halvachizadeh S., Leenen L., Velmahos G.D., Buckley R., Giannoudis P.V. Timing of major fracture care in polytrauma patients – an update on principles, parameters and strategies for 2020. Injury. 2019;50(10):1656–1670. doi: 10.1016/j.injury.2019.09.021. [DOI] [PubMed] [Google Scholar]
- 41.Adili A., Bhandari M., Sprague S., Dunlop R.B., Schemitsch E.H. Humeral shaft fractures as predictors of intra-abdominal injury in motor vehicle collision victims. Arch Orthop Trauma Surg. 2002;122(1):5–9. doi: 10.1007/s004020100315. [DOI] [PubMed] [Google Scholar]
- 42.Hannon M., Hadjizacharia P., Chan L., Plurad D., Demetriades D. Prognostic significance of lower extremity long bone fractures after automobile versus pedestrian injuries. J Trauma Inj Infect Crit Care. 2009;67(6):1384–1388. doi: 10.1097/TA.0b013e31819ea3e0. [DOI] [PubMed] [Google Scholar]
- 43.Katsoulis E., Giannoudis P.V. Impact of timing of pelvic fixation on functional outcome. Injury. 2006;37(12):1133–1142. doi: 10.1016/j.injury.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 44.Glass N.E., Burlew C.C., Hahnhaussen J. Early definitive fracture fixation is safely performed in the presence of an open abdomen in multiply injured patients. J Orthop Trauma. 2017;31(12):624–630. doi: 10.1097/BOT.0000000000000959. [DOI] [PubMed] [Google Scholar]
- 45.Küper M.A., Bachmann R., Wenig G.F. Associated abdominal injuries do not influence quality of care in pelvic fractures-a multicenter cohort study from the German Pelvic Registry. World J Emerg Surg. 2020;15:8. doi: 10.1186/s13017-020-0290-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cimbanassi S., O’Toole R., Maegele M. Orthopedic Injuries In Patients With Multiple Injuries: Results Of The 11th Trauma Update International Consensus Conference Milan. 2017;88:2020. doi: 10.1097/TA.0000000000002407. December 11. [DOI] [PubMed] [Google Scholar]
- 47.Schenker M.L., Yannascoli S., Baldwin K.D., Ahn J., Mehta S. Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review. J Bone Jt Surg - Ser A. 2012;94(12):1057–1064. doi: 10.2106/JBJS.K.00582. [DOI] [PubMed] [Google Scholar]
- 48.Arti H.R. Comparison of early versus delayed debridement in open fractures. Pak J Med Sci. 2012;28(5):856–859. www.pjms.com.pk [Google Scholar]
- 49.British Orthopaedic Association and the British Association of Plastic RaAS . Open Fractures. 2017. Audit standards for trauma.https://www.boa.ac.uk/%0Auploads/assets/uploaded/6418c4a3–d355–4f15-a258cfef62b4729f.pdf Accessed August 1, 2020. [Google Scholar]
- 50.Al-Hourani K., Fowler T., Whitehouse M.R., Khan U., Kelly M. Two-stage combined ortho-plastic management of type IIIB open diaphyseal tibial fractures requiring flap coverage: is the timing of debridement and coverage associated with outcomes? J Orthop Trauma. 2019;33(12):591–597. doi: 10.1097/BOT.0000000000001562. [DOI] [PubMed] [Google Scholar]
- 51.Mauffrey C., Hak D.J., Rojas D. Prevention of the infected fracture: evidence-based strategies for success! J Orthop Trauma. 2019;33(6):1–5. doi: 10.1097/BOT.0000000000001469. [DOI] [PubMed] [Google Scholar]
- 52.Duyos O.A., Beaton-Comulada D., Davila-Parrilla A. Management of open tibial shaft fractures: does the timing of surgery affect outcomes? J Am Acad Orthop Surg. 2017;25(3):230–238. doi: 10.5435/JAAOS-D-16-00127. [DOI] [PubMed] [Google Scholar]
- 53.Cross W., Swiontkowski M. Treatment principles in the management of open fractures. Indian J Orthop. 2008;42(4):377–386. doi: 10.4103/0019-5413.43373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Elniel A.R., Giannoudis P.V. Open fractures of the lower extremity: current management and clinical outcomes. EFORT Open Rev. 2018;3(5):316–325. doi: 10.1302/2058-5241.3.170072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Al-Hourani K., Stoddart M., Khan U., Riddick A., Kelly M. Orthoplastic reconstruction of type IIIB open tibial fractures retaining debrided devitalized cortical segments: the Bristol experience 2014 to 2018. Bone Jt J. 2019;101 B(8):1002–1008. doi: 10.1302/0301-620X.101B8.BJJ-2018-1526.R2. [DOI] [PubMed] [Google Scholar]
- 56.Stoddart M.T., Al-Hourani K., Fowler T., Khan U., Kelly M.B. Plate-assisted intramedullary nailing of gustilo type IIIB open tibial diaphyseal fractures: does adjunctive plate retention affect complication rate? J Orthop Trauma. 2020;34(7):363–369. doi: 10.1097/BOT.0000000000001738. [DOI] [PubMed] [Google Scholar]
- 57.Huber-Lang M., Lambris J.D., Ward P.A. Innate immune responses to trauma review-article. Nat Immunol. 2018;19(4):327–341. doi: 10.1038/s41590-018-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nielson J.L., Paquette J., Liu A.W. Topological data analysis for discovery in preclinical spinal cord injury and traumatic brain injury. Nat Commun. 2015;6(1):1–12. doi: 10.1038/ncomms9581. [DOI] [PMC free article] [PubMed] [Google Scholar]