Abstract
Pelvic injuries are notorious for causing rapid exsanguination, and also due to concomitant injuries and complications, they have a relatively higher mortality rate. Management of pelvic fractures in hemodynamically unstable patients is a challenging task and has been variably approached. Over the years, various concepts have evolved, and different guidelines and protocols were established in regional trauma care centers based mainly on their previous experience, outcomes, and availability of resources. More recently, damage control resuscitation, pelvic angioembolization, and acute definitive internal fixation are being employed in the management of these unstable injuries, without clear consensus or guidelines. In this background, we have performed a computerized search using the Cochrane Database of Systematic Reviews, Scopus, Embase, Web of Science, and PubMed databases on studies published over the past 30 years. This comprehensive review aims to consolidate available literature on the current epidemiology, diagnostics, resuscitation, and management options of pelvic fractures in polytraumatized patients with hemodynamic instability with particular focus on damage control resuscitation, pelvic angioembolization, and acute definitive internal fixation.
Keywords: Polytrauma, Pelvic fractures, Pelvic injury, Management, External fixation
1. Introduction
Globally, trauma is the sixth leading cause of death, and pelvic fractures occur only in 2–8% of all skeletal injuries. However, pelvic injuries occur in nearly 25% of polytraumatized patients.1 The pelvis, being an inherently stable structure, requires a very high energy blunt trauma for pelvic ring disruption. As a result, damage to vascular and visceral structures are common in pelvic injuries.2 Mortality rates in isolated pelvic injury are around 8% and can be as high as 50% when associated with polytrauma.3 Exsanguination due to recalcitrant hemorrhage contributes to more than half of the mortalities associated with pelvic fractures.4 The anatomical proximity of major vascular structures to the pelvis, concomitant visceral damage, and the higher forces required to break the pelvic integrity predispose pelvic injuries to hemodynamic instability.5 It is estimated that, for every 3 min of hemodynamic instability, the mortality increases by 1% in pelvic fractures.6 Decision-making is crucial in managing these complex injuries, and resuscitation and stabilization must go hand in hand to improve outcomes.7 There has been a shift from traditional massive transfusion protocols to damage control resuscitative measures. Pelvic surgical packing is slowly being replaced or augmented by angioembolization in leading trauma care centers, and the timing of definitive pelvic internal fixation is being debated. This review article summarizes the concepts and evidence behind the management of pelvic fractures presenting with hemodynamic instability.
2. Epidemiology of pelvic fractures
The exact incidence of pelvic fracture remains unknown in India due to the non-availability of a national trauma registry. A leading trauma center reported an incidence of 2.82% (104 in 3680 cases) in northern India.7 In central India, a similar incidence of 2.48% was observed.8 Road traffic accident remains the most common cause of pelvic injuries in India, affecting the young population.7,9 Associated injuries in pelvic fractures occur in more than 50% of individuals.9 Most commonly associated injuries include chest (21.2%), head (16.9%), liver or spleen (8.0%), two or more long bone fractures (7.8%), and rarely urogenital (3.7%), and spine (2%).10 Hemorrhagic shock secondary to pelvic injury is the most common cause of mortality (30%) followed by multiple organ failure (26%), hemorrhagic shock (due to other injuries, 16%), and lastly, septic shock (16%) and other causes such as DVT.11 An increasing trend of pelvic fractures, mainly because of road traffic accidents, warrants critical reformation of traffic regulation policies. The development of emergency care services and standardized national treatment guidelines such as NICE (UK) is essential to reduce morbidity and mortality.
Pelvic injuries may range from stable or avulsion fractures outside the pelvic ring to complex, unstable pelvic ring injury and pose a significant diagnostic and therapeutic challenge in unstable Polytrauma patients. The three most common causes of high energy pelvic trauma include motor vehicle collisions, pedestrian injuries, and fall from height. The younger population is at a higher risk of these highly morbid fractures, and as a result, economic productivity is lost and causes a significant burden to society. In the US, though pelvic fractures are highest with more than 50% occurring in an age >75 years, they are mainly low energy falls involving pubic bone.12 Pelvic injuries have the unique potential of causing occult rapid exsanguinating hemorrhage as the bleeding sources may be multiple and are usually from the exposed fractured ends, arterial and venous damage, soft tissue lacerations, and abdominal organ injuries. In the UK, amongst trauma patients, pelvic fractures’ mortality rate was 14.2%, much higher than the 5.6% observed in non-pelvic injuries. The survival rates are better if the initial steps are initiated at the trauma site and during the prehospital phase. Initial management of any pelvic injury mostly follows the Advanced Trauma Life Support (ATLS) guidelines of the American College of Surgeons Committee on Trauma. A situation adapted multi-disciplinary action involving aggressive resuscitation and surgical intervention in the first few hours since the trauma is essential to improve survival rates in these life-threatening fractures.
3. Care at trauma site and prehospital phase
As in any case of polytrauma, the most crucial time of these devastating injuries is the prehospital phase and time taken to reach a designated trauma care center.13 Emergency Medical Services (EMS) and trauma systems have matured over time in developed countries and follow regional trauma care policies to ensure no transport delay. The concept of ‘Platinum 10 min’ in the golden hour of trauma care is best applicable to these injuries, where a time constraint is placed on prehospital care.14 A ′scoop and run’ approach is best enforced to assure rapid transport of these severely injured to the nearest trauma center for definitive care. The role of a formalized and coordinated trauma care system with a centralized emergency medical care services cannot be overemphasized. India, which contributes to nearly 6% of global trauma, requires a centralized national lead agency. Currently, EMS in India is through a public-private partnership under state governments. Dial 108 (free) and 1298 (paid) are ambulance services that can offer basic and advanced life support. However, there is a considerable disparity in the availability of these services between geographical locations and lack a standardized EMS protocol, unlike developed nations. Currently, very few centers offer training services to qualify as Emergency Medical Technician for EMS, which is mainly categorized into EMT-basic, advanced, and paramedic levels of prehospital care ranging from 4 to 12 months of training depending on educational qualification.15
Early on-site application of noninvasive pelvic supports must be applied in all suspected cases of pelvic ring disruptions to reduce the pelvic volume and venous bleeding. Military AntiShock Trousers (MAST), Geneva belt, London belt, Trauma Pelvic Orthotic Device (T-POD), pelvic sheets, and binders have been variably used. Currently, the Pelvic Binder is the most commonly used device and should be applied at the level of greater trochanter with internal rotation of both legs to obtain maximal benefits. These external applications offer controlled circumferential pelvic compression and provide stability in 61% of injuries.16 Previous studies have documented a significant reduction in the requirement for massive transfusion, length of hospital stay, and mortality rates on the early application of these devices.17 In a survey of EMS services provided across seven states in India, encouraging data on pelvic binders usage in 59% of indicated patients has been recently published compared to a 75% application rate in a study from Switzerland.18 In an extensive retrospective analysis, the prehospital use of these compressive devices was mainly beneficial for Tile B and C pelvic injuries.19However, these Polytrauma patients are at an increased risk of soft tissue damage and skin necrosis. Therefore, a shorter duration of the application and adequate cushioning in the gluteal folds are recommended. Ideally, the pelvic binder must be applied, centering the device at the greater trochanter level and encompassing the pelvis. A higher level of application may be harmful by opening up the pelvic ring.20
4. Initial assessment and resuscitation
Ideally, management starts in the prehospital phase and follows a continuum of care in the emergency department. It should be handled by well-trained emergency medical services team professionals, which unfortunately is not available in most developing nations of the world. While the standard management sequence includes a primary survey (ABCDE) and simultaneous resuscitation as per the Advanced Trauma Life Support (ATLS) principles, recent emphasis has been made over the addition of preparedness, personal protective equipment, and decision making in these highly lethal pelvic injuries.21 It is essential for all trauma care providers to undergo ATLS training, as it reflects in the decision making and response in handling polytrauma patients, thereby reducing mortality rates.22 Logrolling of a hemodynamically unstable patient might be counter-predictive by jeopardizing the pelvic stability and, therefore, should be performed with caution after assessing the risk-benefit ratio. For evaluating soft tissue injuries, indirect evidence through staining of linens or placing gloved hands gently behind the back is suitable. The impact of hypothermia on outcomes of pelvic fractures is tremendous. It should be addressed at the earliest to prevent the vicious cycle of the lethal triad in trauma (acidosis, coagulopathy, and hypothermia).
5. Hemodynamic instability
ATLS classifies hypovolemic shock into four classes based on clinical and physiological parameters to serve as a resuscitation guide. However, its clinical use has been critically questioned as more than 90% of trauma patients from the German trauma registry could not be classified.23 Hemodynamic instability is defined as persistent hypotension (systolic blood pressure [SBP] <90 mmHg) despite resuscitative measures. The modified ATLS protocol guidelines have revised their earlier crystalloid strategy from a volume of 2 L–1 L. The traditional concept of massive non-blood product infusions in trauma, which aimed to normalize the systolic blood pressure, has been detrimental. Massive transfusions by altering mean arterial blood pressure (MAP) can worsen the head injury. Besides, it can also induce dilutional coagulopathy, stimulating the lethal triad. On the other hand, massive transfusion of blood products was considered as a superior alternative in managing hemodynamic instability. This massive transfusion protocol (MTP) involved transfusion of packed red blood cells (PRBC) and fresh frozen plasm (FFP) in varying ratios. FFP to PRBC ratio of 1:1 was considered superior to 1:2 ratio but has been widely debated. Though conceptually sound, MTP has not reduced the mortality rates in pelvic fractures, and compliance to MTP protocol is an added disadvantage.24,25 While MTP does not address coagulopathy associated with active bleeding, Damage control resuscitation (DCR) is a strategic approach to tackle hemodynamically unstable patients using permissive hypotension, hemostatic resuscitation, and Damage control orthopedics (DCO).26
Elevated systolic blood pressure can dislodge premature blood clots (pop the clot phenomenon), further aggravating hemodynamic instability. Hence permissive hypotension is targeted with a systolic blood pressure of 80–90 mmHg, which maintains the end-organ perfusion and MAP in suspected head injury patients. This restrictive fluid administration reduces the incidence of coagulopathy and favors hemostasis. In a prospective randomized clinical trial, Schreiber et al. compared the 24-h mortality rate in blunt trauma patients, amongst patients undergoing controlled and aggressive resuscitation. The controlled resuscitation group had much lower mortality (3%) than the aggressive resuscitation group (18%).27 Results of a recent meta-analysis on the benefits of Hypotensive resuscitation show strong evidence for a reduced need for blood transfusion and reduction in the incidences of ARDS and multiple organ dysfunction.28 The term “aggressive resuscitation,” therefore, has been eliminated from ATLS guidelines.
The optimal fluid for resuscitation has been debated over several decades, from hypertonic saline to Hartmann’s solution, and then to the currently preferred isotonic crystalloid solution. In hypovolemic shock, early use of blood and its products is recommended. Hemostatic resuscitation includes transfusion of RBCs, plasma, and platelets in a 1:1:1 ratio. Tranexamic acid is an anti-fibrinolytic, which, if administered within the first 3 h of polytrauma, significantly reduces mortality rates and is considered as a part of hemostatic resuscitation.29 The endpoints of resuscitation are measured by the base deficit and normalization of serum lactate.30 Their elevated levels have a direct correlation with mortality. However, maintaining the systolic blood pressure of 80–90 mmHg, urinary output, and palpable peripheral pulse are not consistent signs of successful resuscitation.31
6. Diagnostic approach in pelvic injuries with hemodynamic instability
Volumes of bleeding in severe pelvic injuries can go as high as 3000 ml with an intensity of 1000 ml/h.32 Acute bleeding and shock contribute to 80% of all deaths, and therefore early identification of the bleeding source is of paramount importance in controlling hemorrhage. Diagnostic workups must be standardized and streamlined to avoid delays. There could be multiple bleeding sources, which include bone surfaces, vascular structures, soft tissue damage, solid organ injuries, and often be concealed in remote sites such as vagina and perineum. Physical examination suggestive of pelvic fracture includes clinical evidence of urethral injury. A simple digital rectal examination (DRE) might reveal a tear at the rectum or a high riding prostate, which is suggestive of urethral injury. Though it was recommended as a part of the initial evaluation in ATLS protocol, several studies have found high false positivity rates and question its reliability.33 In cases of complete disruption of the parapelvic facia (gluteal muscles and iliopsoas compartment), the tamponade effect of external stabilization devices is not sufficient to control bleeding. This is because pelvic hemorrhage enters the retroperitoneal space and through the rent, may present at a distant region, and this was described as a “chimney effect”. Occasionally, it might present at the anterior aspect of the thigh as “butterfly hematoma” which indicates damage to the perineal membrane and an underlying urethral injury.
Ecchymosis at the scrotum and blood at the urethral meatus is a clear association of pelvic ring disruption with urethral or bladder damage. Other indicators of pelvic injury include limb length discrepancy or a rotational deformity without evidence of any other fracture. While a gentle palpation for bony tenderness may give useful information, application of pelvic distraction can cause dislodgement of the clots. It is well known that “first clot is the best clot” and therefore vigorous examination might cause aggravation of bleeding and is to be strictly avoided. Placement of gastric tubes and urinary catheters are adjuncts to clinical examination. Presence of blood during gastric tube placement indicates oesophageal or upper gastrointestinal injuries. Decompression of gastric dilatation and prevention of aspiration are added advantages. Placement of urinary catheters relieves urinary retention and enables monitoring of tissue perfusion through urinary output, and can also be used to identify urethral injury. Since full bladder enhances ultrasound imaging of pelvis, urinary catheter is usually planned following FAST. Presence of blood at urethral meatus, scrotal hematoma and ecchymosis in the perineum or inability to void urine warrants a retrograde urethrogram and a suprapubic catheter is to be placed if urethral injury is confirmed.
7. Imaging
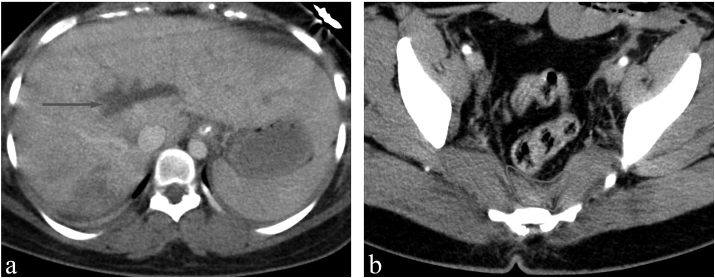
Focused Assessment with Sonography for Trauma (FAST), a widely used screening method to detect blood collection in the peritoneal cavity (Fig. 1), has excellent diagnostic accuracy.34 Many studies have shown high sensitivity of 85–95% and specificity of 95% in detecting hemorrhage.35More importantly, a false-negativity of only 2%, indicates that FAST can reliably diagnose life-threatening bleeding in pelvic injuries.36 FAST requires only 5 min for an experienced physician and much lesser for a radiologist. However, a recent study shows that even non-radiologists have good diagnostic abilities for detecting hemoperitoneum using FAST.37 It is made available inside the emergency room in most of the level-I trauma centers and has been incorporated as a standard protocol in imaging the polytrauma patients. More recently, extended FAST (eFAST) has been included, which additionally screens the thoracic cavity.
Fig. 1.
Anteroposterior radiograph showing anteroposterior compression injury of pelvis with pubic diastasis and bilateral sacroiliac joint widening.
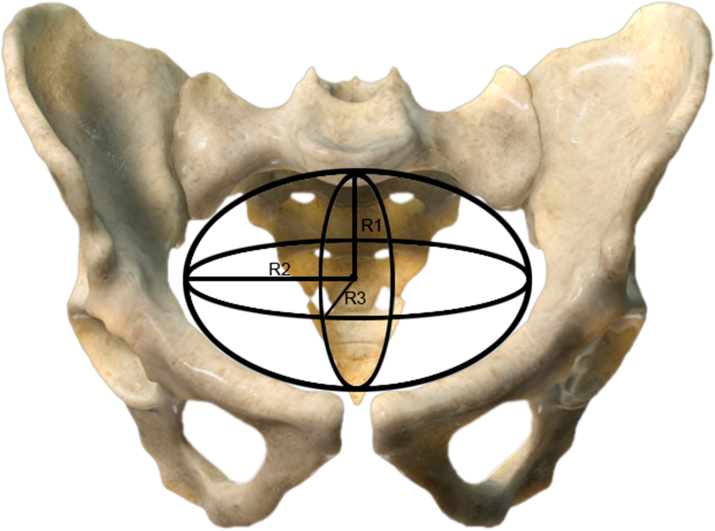
Performing the entire trauma series of radiographs, as described in ATLS guidelines, will result in loss of crucial time in managing these hemodynamically unstable patients. Chest radiographs detect life-threatening injuries such as hemothorax in no time and thereby allow the trauma team to perform immediate intercostal drainage. Pelvic fractures can be easily diagnosed with plain anteroposterior radiographs (Fig. 2), which then allows the team to get a broad idea of how severe the injury and associated hemodynamic instability could be. Early diagnosis paves the way for rapid pelvic stabilization and reduces bleeding and related complications. Pelvic fracture classification determines the stability of the pelvic ring and also indirectly denotes the amount of force involved to cause the disruption. The shape of the human pelvic cavity can be compared to that of an ellipsoid, where three measurements, determine the volume it holds viz height of the pelvis (r1), 2) mediolateral (length) (r2), and 3) anteroposterior (width) (r3) dimensions. It can be calculated as V = 4/3π r1r2r3 (Fig. 3). It can hold nearly 30% of total blood volume when anatomically intact and can even accommodate more than 50% leading to a rapid non-compressible source of internal bleeding. Tile-type A is the least severe pelvic fracture injury, whereas Tile-type B (partially unstable) and Tile-type C (completely unstable). Another commonly used Young and Burgess classification dictates the direction of the force that caused the pelvic ring disruptions. It includes Antero-posterior Compression (APC), Lateral Compression (LC), Vertical Shear (VS), and combined injury patterns. Often the LC-III, APC-III, VS, and combined injuries cause severe hemodynamic instability. The most common pelvic injury are LC injuries, which are not associated with major pelvic bleeding as majority of the posterior stabilizing ligaments remain intact unlike APC and VS injuries. Comparing the two classifications in predicting hemodynamic stability, both fare equally, however fractures considered as unstable by Young and Burgess classification is better in terms of predicting mortality.38,39 While these gross unstable injuries can easily be recognized in plain radiographs, the posterior ring injuries can be missed. Though plain radiograph of pelvis is an integral part of ATLS protocol, the poor sensitivity of 67% in identifying pelvic injuries which were clinically stable yet hemodynamically unstable, favours the usage of pelvic CT in evaluating pelvic injuries.
Fig. 2.
FAST scan done in a polytrauma patient as a part of initial assessment, demonstrating fluid in hepatorenal pouch.plain
Fig. 3.
The anatomy of pelvic cavity can be compared to that of an ellipsoid. The volume of blood it can accommodate is calculated by formula V = 4/3π R1R2R3 where R1 is the height, R2 is the mediolateral length and R3 is the anteroposterior width of the cavity.
Over the last two decades, the Whole-body Computed Tomography (WBCT) protocol has overtaken the Selected Computed Tomography (SCT) approach of the ATLS as WBCT fares superior in terms of the time of imaging, diagnostic accuracy, and mortality rates.40 However, cancer risk due to additional radiation is a concern and is better avoided in children and women of child bearing age.41 The success of the SCT approach depends on the physician’s experience, and the plain radiography findings influence the clinical judgment. Up to 52% of clinically significant injuries can be missed if CT of the thorax was not performed based on chest radiograph interpretations.42 SCT imaging, therefore, can miss injuries, which can be as high as 31.4%.43 In another study, 75% of the unsuspected injuries, which were later diagnosed by WBCT, were severe.44 They included cervical injury, bilateral lung contusion, occult pneumothorax, and brain contusion. WBCT approach, (Fig. 4) which provides for unenhanced head and cervical and contrast-enhanced chest, abdomen, and pelvis CTs, has become widespread mainly to minimize the rate of missed injuries, thereby reducing mortality rates.
Fig. 4.
a) Whole body CT scan done in a polytrauma patient showing liver laceration of size 6 × 1 cm in the 4th lobe (organ injury scale grade 3), b) significant presacral hematoma indicating an underlying sacrum fracture or sacroiliac joint disruption which causes massive internal bleeding due to rupture of presacral venous plexus leading to hemodynamic instability.
8. Damage control surgery (DCS)
DCS aims at maintaining physiology compatible with life. The goals of this approach include rapid control of bleeding, decontamination, and early stabilization of fractures. Anatomic reconstruction is reserved to a later date after physiological recovery to prevent the second hit in these polytraumatized patients. The primary source of bleeding from unstable pelvic injuries includes fracture surfaces and venous rupture. If the pelvic ring opens up by 5 cm, the pelvic volume increases by 10–20%.45 Application of external fixator in compression apposes the fracture ends, reduces pelvic size and also provides a tamponade effect for controlling bleeding. As per Young and Burgess classification APC II, III, LC II, III are amenable for satisfactory stabilization using External fixator in 64–83% of injuries.46,47 However, in vertical shear and combined injuries, apart from external fixation, ipsilateral skeletal traction is also needed in 27% of injuries.48
9. External compressive devices
The anterior external fixator, Pelvic C-clamp, and the trochanteric C-clamp have been variably used in managing these unstable injuries, and their pros and cons are briefly described below.
-
1.
Pin placement at the iliac crest is the most common and quickly performed method without any image control. It requires two Schanz pins for stability. Potential disadvantages include pin loosening and breakage because of the thin iliac blade. More importantly, the construct might interfere with abdominal procedures and do not stabilize the posterior ring. (Fig. 5a)
-
2.
External fixation using pins in the supra-acetabular region that has good bone stock requires only a single Schanz pin, and it can be moved caudally and cranially, thereby provide more extensive access to abdominal procedures. The optimal entry point is cranial to Antero Inferior Iliac Spine directed cranio-caudally towards the superior aspect of greater sciatic notch. Such an inclination not only stops short of the corridor of sacroiliac joint screws but also allows placement of pubic ramus screws.49 (Fig. 5b). Anterior Inferior Iliac Spine (AIIS) is yet another a reasonable corridor for pin placement where one pin would suffice.50 However, to avoid damage to neurovascular structures and joint penetration, considerable surgical expertise and image control are required in both of these (Fig. 5c). Pin placement in supracetabuar region is considered superior to iliac crest pin placement.51
-
3.
Pelvic C-clamp aims to stabilize the posterior pelvic ring, and pins on either side are inserted into ilium adjacent to the sacroiliac joint. It is not useful in iliac wing fractures. In combined and vertical shear injuries, additional skeletal traction is required. An increase in postoperative infections following sacroiliac joint fixation is a concern in patients who are undergoing primary C-clamp application.52 Its use is contraindicated in comminuted and transforaminal sacral fractures, iliac wing fractures, and LC-type pelvic fractures.53
-
4.
Archdeacon et al. modified the C- clamp by applying it to the trochanteric region of the femur. Cadaver models have demonstrated a significant reduction of the anterior pubic diastasis and posterior disruption of the sacroiliac joint after trochanteric pelvic clamp application.54 However, anterior vertical displacements are not ideal for this device.
Fig. 5.
Pelvic EXFIX with pins through a) Iliac crest, b) supra acetabular area and c) anterior inferior iliac spine.
10. Management of recalcitrant hemodynamic instability following external fixation
Recalcitrant bleeding might be secondary to an arterial source of bleeding, which is not uncommon in these high energy pelvic fractures. External fixation does not address arterial bleeding and therefore requires angiography and embolization, which have a success rate of 80–100% in achieving hemostasis. However, they have no role in controlling recalcitrant venous bleeding which forms the primary source of bleeding in pelvic injuries. Besides, angiography is a lengthy procedure and might not be available in all centers. Pohlemann et al. described a technique for pelvic packing, which was later widely adopted by Europe and the United States in managing hemodynamic stability.55
11. Diagnostic peritoneal lavage (DPL)
DPL is a very accurate tool for diagnosing blunt trauma of hollow viscus injuries and can be performed in three methods-open,semi-open and closed. A DPL is considered to be positive if 10 ml gross blood is obtained on initial aspiration. Other parameters included >500/mm3 white blood cells (WBC), >100,000/mm3 red blood cells (RBC), or the presence of enteric/vegetable matter.56 FAST and CT have largely replaced the usage of DPL, and is mainly carried out in centers where there is no access to either of them.
12. The role of pelvic packing
Preperitoneal pelvic packing (PPP) can be performed in an emergency room to efficiently addresses the retroperitoneal recalcitrant presacral venous source of bleeding.57 Through midline incision at the lower abdomen, retropubic and presacral spaces are inserted with packs on either side of the true pelvis. This procedure requires less than 30 min and involves reassessment and removal of the packs within 48 h. Most trauma centers use this technique in conjunction with external fixation, and it has significantly brought down acute deaths. However, Guy Ron et al. reported 100% success in the control of hemodynamic instability associated with pelvic fractures following usage of PPP as a stand-alone surgical treatment.58 Despite well-documented efficacy and having been considered as a paradigm shift, usage of PPP varies widely based on the anecdotal perception of medical directors even amongst level-1 trauma centers in the US.59
13. Pelvic angiography and embolization
The main indication for angioembolization is to control the arterial bleeding, and it has been in practice since 1972.60 However, the primary bleeding source is from an arterial injury, only in 0.01–2.3% of patients.61 Internal iliac artery and its visceral (uterine artery, superior and inferior vesical arteries, middle and inferior rectal arteries) and parietal (ilio-lumbar artery, lateral sacral artery, superior and inferior gluteal arteries, obturator artery and internal pudendal artery) branches are the commonest source of arterial bleeding.62 However branches arising from the aorta (lumbar and median sacral arteries) or external iliac artery (inferior epigastric artery, corona mortis artery, circumflex iliac artery) can also be potential sources of hemorraghe. Longer times, non-availability of round the clock qualified and skilled personnel, and mainly its interference in the management of other Polytrauma care measures, are limitations of this procedure. Complications of embolization include surgical site infection, gluteal muscle necrosis, bowel and bladder infarction, nerve palsies, and cardio-respiratory arrest and, therefore, should be better used only in appropriate indications. Sagawa et al. evaluated the impact of transarterial embolization of bilateral internal iliac arteries (TAE) in unstable pelvic fractures on lower urinary tract symptoms and reported a high incidence of worsening following TAE.63 To identify potential candidates for TAE by identifying arterial source of bleeding, CECT (contrast enhanced CT) is an ideal imaging option with good sensitivity (80–90%), specificity (85–98%) and accuracy (87–98%).64 CECT is useful in predicting the need for angioembolization by demonstrating the presence of a pelvic hematoma or a contrast blush.65 Based on Young and Burgess classification, APC II, III, LC-III, VS, and combined injuries are notorious for arterial injuries. Timely performed angioembolization has a high success rate of 74–100%.66 However, documented evidence of new sites of bleeding and recurrence of bleeding at the same location are concerns following this highly demanding procedure.67
14. Pelvic packing versus angigraphy and embolization
In patients with pelvic fractures and heodynamic instability, there is no current evidence to support the superiority of either of them as there has been no significant difference in mortality rates.68 Angiography is considered a complementary rather than a competitive tool.69 However, it is most effective if done early, which therefore necessitates the availability of an in house experienced interventional radiologist. In most of the current trauma care algorithms, this angioembolization is performed when there is persistent hypotension following damage control resuscitation and external pelvic fixation, or when whole-body CT had demonstrated a contrast blush or hematoma, which is suggestive of arterial source of bleeding.70 If there is no evidence of arterial bleeding in CT or if the patient is not fit to be shifted to the radiology suite, the patient is taken up for emergency pelvic packing along with external pelvic stabilization in cases of hemodynamic instability.
15. Three in one protocol
Sequential early control of bleeding from pelvic fracture by external fixation, retroperitoneal pelvic packing (RPP), and angiographic interventions form the three pillars of this protocol, which was developed in Hongkong for managing pelvic fractures with hemodynamic instability. All these are performed in the operation theatre in the same session. The primary sources of bleeding in pelvic injuries are from the cancellous surface of fractures and venous channels. External fixation of the pelvis as the first measure in this protocol stabilizes the pelvis and reduces volume, which helps in addressing the primary source of uncontrolled bleeding. RPP aids further control of bleeding by providing a tamponade effect. Lastly, angiography and embolization are performed in the same session, which stops the arterial source of bleeding. In a recent multicenter analysis, this protocol was identified as the single most independent predictive factor for 30-day, 7-day, and 24-h mortality rates.71 Implementation of such a protocol reduces unnecessary time spent on discussion, arrangement for the three crucial procedures, and transfers of these highly unstable patients. The three different measures adopted in this sequential protocol are supplementary and complement each other in achieving hemostasis in unstable pelvic fractures. However, to accomplish this one-stop resuscitation and therapeutic action, a vast workforce involving a multi-disciplinary team of anesthetists, orthopedic surgeons, general surgeons, interventional radiologists, radiographers, operating room technicians, and nursing staff should be available round the clock in trauma care centers.
16. Primary internal fixation in pelvic fractures with hemodynamic instability
Definitive fixation of unstable fractures should be timed appropriately, strictly adhering to the principles of DCS and DCR. Delayed definitive fixation is safe and has a predictable outcome in most of these injuries. While external fixation of pelvic fractures has become an integral part of damage control measure, internal fixation remains controversial and have been attempted only by few authors as a part of early total care.72 On the other hand there is an emerging concept of applying percutaneous iliosacral screws, anterior pubic plating using the same corridor used for pelvic packing, and INFIX application as resuscitative measures in severe hemodynamic instability. They can be performed quickly by experienced surgeons and do not involve excessive blood loss, but aid in achieving stability and control bleeding. Ennighorst et al. showed acute fixation of pelvic ring injuries in hemodynamic instability is a feasible option.72 But the study mainly involved APC type simple symphysial disruptions with Sacro-iliac joint separations, which required plating and percutaneous iliosacral screw fixation. Gardner et al. described early internal fixation of sacroiliac joint as a definitive antishock measure in unstable posterior pelvic ring disruptions.73 More recently, a biomechanical study has found the FiberTape® suture device to be a suitable minimally invasive alternative to stabilize the posterior ring.74 Chen et al. performed percutaneous pubic symphysis fixation as an adjunct to external fixator in grossly open anterior pelvic injuries with perineal lacerations and described good outcomes.75 In patients undergoing laparotomy for addressing abdominal and perineal injuries, the same incision can be utilized for simultaneous management of anterior pelvic injuries using plating or retrograde ramus screws for symphysial disruptions and other anterior ring disruptions.76 Anterior subcutaneous internal fixation using spinal pedicle screws and the percutaneous rod has been used as a less invasive alternative for unstable anterior ring disruptions.77 This INFIX application is especially beneficial for managing those with associated urogenital and perineal injuries. Recently, modifications of INFIX application viz, unilateral, and extended unilateral INFIX was compared to that of bilateral and extended bilateral INFIX devices in a biomechanical study.78 The stability of unilateral INFIX was found to be significantly improved by additional application of pubic ramus screws (extended unilateral INFIX) and was suggested to be a feasible alternative.
Proponents of acute pelvic fracture fixation have claimed, easier direct fracture reduction without extensive open surgery, lesser blood loss, better positioning, and respiratory care in ICU, and shorter length of stay as definitive advantages.79 Vallier et al. compared early and late definitive fixation of unstable pelvic and acetabulum fractures, and documented reduction in morbidity amongst those managed soon.80 A nationwide analysis of pelvic injuries in the US also supports these views as internal fixation was associated with decreased odds of mortality.81 Traditionally, definitive fixation of pelvic fractures was suggested beyond 72 h. However, there is increasing evidence which shows the feasibility of safely performing definitive surgery within this timeframe, which is associated with a very low mortality rate of 2.3%.82 However, the time-taken for definitive management of these unstable fracture fixations in an acute setting, and their implications have been less studied. Early Appropriate Care (EAC) involves definitive fixation (within 36 h) for unstable fractures of the thoracolumbar spine, pelvis, acetabulum, and/or femur following achievement of definitive thresholds of physiological parameters. The physiological targets of laboratory parameters include lactate <4.0 mmol/L, pH ≥ 7.25, or base excess (BE) ≥−5.5 mmol/L.83
17. The influence of associated injuries on the management of pelvic fractures
Outcomes of pelvic fractures are strongly influenced by the presence of concomitant head (37–50%) and chest injuries (25–66%.) and their appropriate management.76 Deterioration of head injuries secondary to hemorrhage due to pelvic fractures and resulting coagulopathy is a major concern. Acute hemostatic stabilization of pelvis by external fixation is recommended and definitive fixation delayed considering the excessive blood loss and excessive time taken for definitive fixation in an acute unstable patient.84 Neurosurgeon’s choice of surgical or conservative management of a head injury depends on the nature of head injury and status of physiological stability. Chest injuries with high Injury Severity Score (ISS), increase transfusion requirements and augment the inflammatory response. Current evidence shows that definitive fixation has a significant adverse effect on polytrauma if associated with a chest injury. Hence, the principles of DCS are best applied in managing these injuries to avoid substantial hazards.85 Abdominal injuries occur in 11–16.5% of patients with pelvic fractures, and their severity has a direct correlation with mortality. The liver is the most commonly injured organ (6–18%), followed by splenic injury (5.2%), and bowel injuries (4.4%). An Abbreviated Injury Scale (AIS) ≥ 4 and liver laceration of organ injury severity (OIS) ≥ 4 has the highest death rate of 100%. Urogenital injuries (23–57%) are frequent as the fractured pubic rami fragment usually ruptures the bladder, urethra, and vagina. Retrograde urethrogram is a useful tool to diagnose and locate urethral injuries. Careful placement of a small urinary catheter or suprapubic catheter insertion may be the initial treatment in this situation. A high index of suspicion is essential to rule out all the associated soft tissue and organ injuries in patients presenting with pelvic fractures and should be managed appropriately. Femur fractures are common in a polytrauma situation, and their management is again according to the principles of DCS. However, there is sufficient evidence to support definitive early internal fixation as delayed fixation has a higher rate of pulmonary complications. Bone et al. showed that early nailing of femur fractures had reduced the pulmonary complications and also had a shorter hospital stay.86 Mizra et al. documented improvement in stability and outcomes of polytrauma patients with early appropriate care of pelvic and femoral fractures by definitive fixation.87
Internal degloving injuries can be typically associated with pelvis injuries (Moralle Lavelle lesion) and are managed by hematoma washout and surgical debridement if the collection exceeds 50 ml. However they are not life saving procedures and are usually done along with other orthopedic interventions.88
18. Polytrauma and pelvic injury in geriatric population
An increase in the aging population and associated co-morbidities such as osteoporosis, immune suppression in cancer survivors, and transplant recipients have caused a rise in the incidence of polytrauma and pelvic injuries in the geriatric population.89 However, unlike the violent, traumatic forces in the young, these injuries form a different spectrum. Reduced physiological reserve, consumption of antiplatelet drugs, lowered immune response and compromised cardiovascular status are major concerns and pose a significant challenge. Shozo et al. felt the need for massive transfusion in these patients, causing a severe alteration in the coagulation cascade, which in turn is life-threatening.90
19. Updates in the management of pelvic polytrauma
Resuscitative endovascular balloon occlusion of the aorta (REBOA) has been described as an effective adjunct to those who don’t respond to any of the measures described above. REBOA has the potential to improve the systolic blood pressure by 50 mm of Hg.91 A balloon catheter is inserted through the common femoral artery and temporary occlusion of the thoracic or infrarenal aorta is performed to stop exsanguination and allow perfusion to vital organs such as brain, heart and lungs above the site of injury. However the catheter cannot be advanced if there is severe laceration of the main arterial trunks and crucial time lost in attempting to negate the catheter might lead to catastrophic death.92 More clinical studies are essential to understand the pitfalls and complications of REBOA and its clinical use in pelvic fractures with hemodynamic instability.
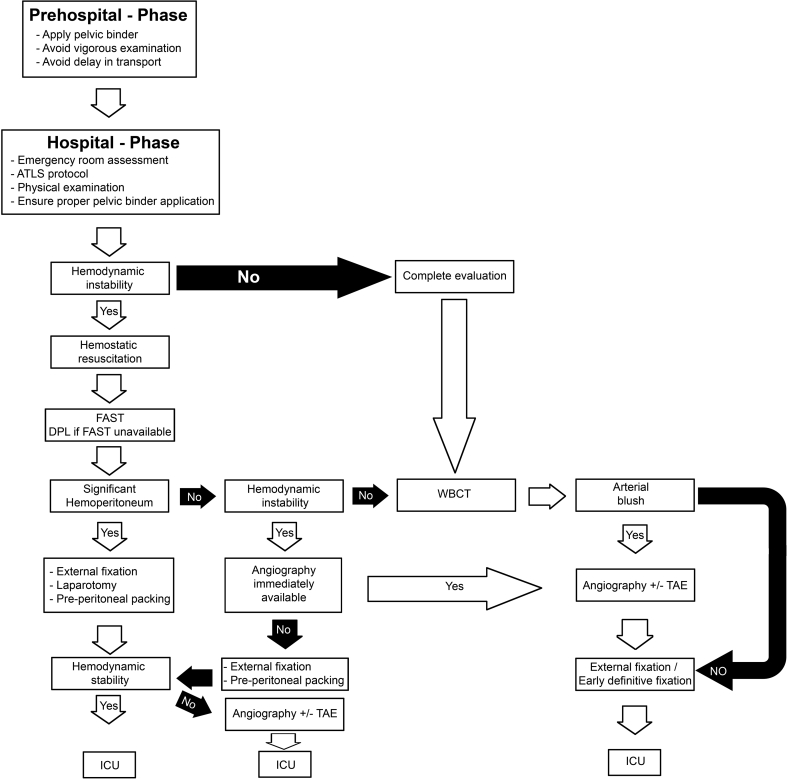
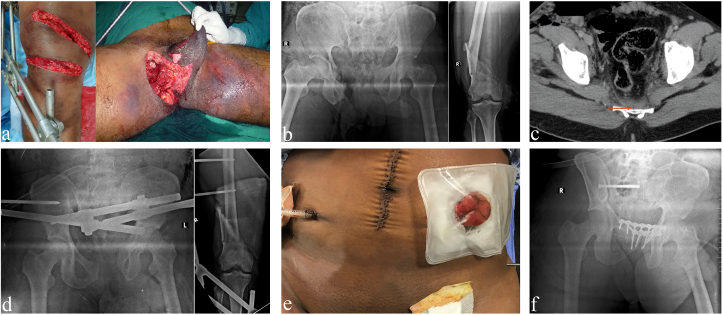
Pelvic fractures with hemodynamic instability require a swift algorithmic approach to ensure early, safe and effective management. Fig. 6 highlights such an approach practiced in the authors trauma center, which can be universally adapted with minor modifications based on the regional resources. Fig. 7 exemplifies a typical case of pelvic injury in polytrauma with the sequence of management performed leading to an effective outcome.
Fig. 6.
Algorithmic approach used to manage pelvic injuries in polytrauma at the authors center.
Fig. 7.
A 36-year-old gentleman with a history of motor vehicle accident was shifted to the hospital in 2 h following injury. On arrival patient was conscious, oriented, hemodynamically unstable, with a pulse rate of 148/min, blood pressure of 86/40 mmHg and SPo2 of 88%. Following initial resuscitation with 1 L crystalloid infusion, immediate hemostatic resuscitation was performed with 2 units of packed red blood cells, fresh frozen plasma and platelets administered in a 1:1:1 ratio. On clinical examination he had a) an open wound over distal 3rd of thigh along with perineal laceration. Per-rectal examination showed absence of muscle tone and a proximal rectal injury was clinically suspected. Once patient achieved hemodynamical stability, E-FAST done which was negative. b)Preoperative plain radiographs showed pubic diastasis with right sided sacroiliac joint disruption, comminuted fracture of right distal femur (type III B open), c) Whole body CT scan done as a part of polytrauma protocol showed presacral hematoma more on right side indicating an underlying sacrum fracture or sacroiliac joint disruption. In addition, surgical emphysema was noted along the right lateral abdominal wall with air fluid level in lower abdomen, tracking into perineum and right upper thigh with tracking of air up to right hemiscrotum. In view of unstable pelvic injury with an associate extremity injury, damage control surgery (exfix for femur ,pelvis and Laparotomy) was performed, d) Plain radiograph following EXFIX of pelvis and knee spanning external fixation for distal femur. Laparotomy revealed a rectal tear for which proximal sigmoid loop colostomy was done and wounds over the perineum, right distal thigh were debrided. e) Clinical picture showing laparotomy wound and colostomy stump. Postoperatively the patient was shifted to ICU for observation. Serum lactate normalization time was 24 h from 8.3 mmol/lit to 2.24 mmol/lit. On 3rd postoperative day f) definitive fixation of pelvis in the form of pubic symphysis plating and percutaneous sacroiliac fixation for the right sacroiliac joint was done. On 7th postoperative day definitive fixation (Exfix removal and retrograde nailing) of distal femur was done.
20. Conclusion
Pelvic fractures are notoriously known for rapid death and high mortality rates. Prehospital care with pelvic binders and transfer of these patients to the nearest trauma care center is of paramount importance. Appropriate damage control measures should complement the early assessment of anatomical injury and its physiological effects. Early external fixation and employment of selective less-invasive measures such as percutaneous iliosacral screws in posterior ring disruption or plating/INFIX applications for anterior ring stability using the same window made for managing associated abdomen/perineum injuries have been successful. An algorithmic approach involving a multi-disciplinary team considering the patient’s pre-injury condition, anesthetic, and surgical risks using available resources is essential in managing these lethal injuries.
Funding
No funding was received towards the preparation of this manuscript.
Acknowledgement
We acknowledge the efforts of all the authors in preparation of this manuscript.
References
- 1.Pizanis A., Pohlemann T., Burkhardt M., Aghayev E., Holstein J.H. Emergency stabilization of the pelvic ring: clinical comparison between three different techniques. Injury. 2013;44(12):1760–1764. doi: 10.1016/j.injury.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Mejaddam A.Y., Velmahos G.C. Randomized controlled trials affecting polytrauma care. Eur J Trauma Emerg Surg. 2012;38(3):211–221. doi: 10.1007/s00068-011-0141-2. [DOI] [PubMed] [Google Scholar]
- 3.Pelvic fractures in paediatric polytrauma patients: classification, concomitant injuries and early mortality. https://openorthopaedicsjournal.com/VOLUME/9/PAGE/303/FULLTEXT/ [Internet]. [cited 2020 Sep 24]. Available from: [DOI] [PMC free article] [PubMed]
- 4.Moreno C., Moore E.E., Rosenberger A., Cleveland H.C. Hemorrhage associated with major pelvic fracture: a multispecialty challenge. J Trauma. 1986;26(11):987–994. doi: 10.1097/00005373-198611000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Mirza A., Ellis T. Initial management of pelvic and femoral fractures in the multiply injured patient. Crit Care Clin. 2004;20(1):159–170. doi: 10.1016/s0749-0704(03)00096-4. [DOI] [PubMed] [Google Scholar]
- 6.Heetveld M.J., Harris I., Schlaphoff G., Sugrue M. Guidelines for the management of haemodynamically unstable pelvic fracture patients. ANZ J Surg. 2004;74(7):520–529. doi: 10.1111/j.1445-2197.2004.03074.x. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh S., Aggarwal S., Kumar V., Patel S., Kumar P. Epidemiology of pelvic fractures in adults: our experience at a tertiary hospital. Chin J Traumatol Zhonghua Chuang Shang Za Zhi. 2019;22(3):138–141. doi: 10.1016/j.cjtee.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta A.A., Mishra S.K., Uikey S., Maravi D. A study - incidence and pattern of musculoskeletal injuries among patients attending the emergency of tertiary health care center in Central India. J Orthop Dis Traumatol. 2019;2(1):11. [Google Scholar]
- 9.NSCB Medical College, Vidyarthi D.A. Study of incidence and prevalence of pelvic fractures in Central India. J Med Sci Clin Res. 2018 Mar 24 [cited 2020 Sep 20];6(3). Available from: http://jmscr.igmpublication.org/v6-i3/141%20jmscr.pdf. [Google Scholar]
- 10.Giannoudis P.V., Grotz M.R.W., Tzioupis C. Prevalence of pelvic fractures, associated injuries, and mortality: the United Kingdom perspective. J Trauma Inj Infect Crit Care. 2007;63(4):875–883. doi: 10.1097/01.ta.0000242259.67486.15. [DOI] [PubMed] [Google Scholar]
- 11.Palmcrantz J., Hardcastle T.C., Naidoo S.R., Muckart D.J.J., Ahlm K., Eriksson A. Pelvic fractures at a new level 1 trauma centre: who dies from pelvic trauma? The inkosi albert luthuli central hospital experience. Orthop Surg. 2012;4(4):216–221. doi: 10.1111/os.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buller L.T., Best M.J., Quinnan S.M. A nationwide analysis of pelvic ring fractures. Geriatr Orthop Surg Rehabil. 2016;7(1):9–17. doi: 10.1177/2151458515616250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adhikari D.D., Florence B., David S.S. Prehospital trauma care in South India: a glance through the last 15 years. J Fam Med Prim Care. 2016;5(1):195–196. doi: 10.4103/2249-4863.184669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pham H., Puckett Y., Dissanaike S. Faster on-scene times associated with decreased mortality in Helicopter Emergency Medical Services (HEMS) transported trauma patients. Trauma Surg Acute Care Open. 2017 doi: 10.1136/tsaco-2017-000122. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5887760/ [cited 2020 Aug 2];2(1). Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma M., Brandler E.S. Emergency medical services in India: the present and future. Prehospital Disaster Med. 2014;29(3):307–310. doi: 10.1017/S1049023X14000296. [DOI] [PubMed] [Google Scholar]
- 16.Bottlang M., Simpson T., Sigg J., Krieg J.C., Madey S.M., Long W.B. Noninvasive reduction of open-book pelvic fractures by circumferential compression. J Orthop Trauma. 2002;16(6):367–373. doi: 10.1097/00005131-200207000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Hsu S.-D., Chen C.-J., Chou Y.-C., Wang S.-H., Chan D.-C. Effect of early pelvic binder use in the emergency management of suspected pelvic trauma: a retrospective cohort study. Int J Environ Res Publ Health. 2017 Oct doi: 10.3390/ijerph14101217. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5664718/ [cited 2020 Aug 2];14(10). Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zingg T., Piaget-Rossel R., Steppacher J. Prehospital use of pelvic circumferential compression devices in a physician-based emergency medical service: a 6-year retrospective cohort study. Sci Rep. 2020 doi: 10.1038/s41598-020-62027-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7083961/ Mar 20 [cited 2020 Sep 23];10. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prehospital use of pelvic circumferential compression devices in a physician-based emergency medical service: a 6-year retrospective cohort study. Sci Rep. 2020 doi: 10.1038/s41598-020-62027-6. [Internet]. [cited 2020 Aug 2]. Available from: https://www.nature.com/articles/s41598-020-62027-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonner T.J., Eardley W.G.P., Newell N. Accurate placement of a pelvic binder improves reduction of unstable fractures of the pelvic ring. J Bone Joint Surg Br. 2011;93(11):1524–1528. doi: 10.1302/0301-620X.93B11.27023. [DOI] [PubMed] [Google Scholar]
- 21.Kam C.W., Law P.K.J., Lau H.W.J. The 10 commandments of exsanguinating pelvic fracture management. Hong Kong J Emerg Med. 2019;26(6):357–370. [Google Scholar]
- 22.Mohammad A., Branicki F., Abu-Zidan F.M. Educational and clinical impact of Advanced Trauma Life Support (ATLS) courses: a systematic review. World J Surg. 2014;38(2):322–329. doi: 10.1007/s00268-013-2294-0. [DOI] [PubMed] [Google Scholar]
- 23.A critical reappraisal of the ATLS classification of hypovolaemic shock: does it really reflect clinical reality? - PubMed. https://pubmed.ncbi.nlm.nih.gov/22835498/ [Internet]. [cited 2020 Sep 23]. Available from: [DOI] [PubMed]
- 24.Söderlund T., Ketonen T., Handolin L. Bleeding pelvic fracture patients: evolution of resuscitation protocols. Scand J Surg. 2017;106(3):255–260. doi: 10.1177/1457496916683092. [DOI] [PubMed] [Google Scholar]
- 25.Bawazeer M., Ahmed N., Izadi H., McFarlan A., Nathens A., Pavenski K. Compliance with a massive transfusion protocol (MTP) impacts patient outcome. Injury. 2015;46(1):21–28. doi: 10.1016/j.injury.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 26.Mizobata Y. Damage control resuscitation: a practical approach for severely hemorrhagic patients and its effects on trauma surgery. J Intensive Care. 2017;5(1):4. doi: 10.1186/s40560-016-0197-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schreiber M.A., Meier E.N., Tisherman S.A. A controlled resuscitation strategy is feasible and safe in hypotensive trauma patients: results of a prospective randomized pilot trial. J Trauma Acute Care Surg. 2015;78(4):687–695. doi: 10.1097/TA.0000000000000600. discussion 695-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Owattanapanich N., Chittawatanarat K., Benyakorn T., Sirikun J. Risks and benefits of hypotensive resuscitation in patients with traumatic hemorrhagic shock: a meta-analysis. Scand J Trauma Resuscitation Emerg Med. 2018;26(1):107. doi: 10.1186/s13049-018-0572-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CRASH-2 collaborators, Roberts I., Shakur H. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet Lond Engl. 2011;377(9771):1096–1101. doi: 10.1016/S0140-6736(11)60278-X. 1101.e1-2. [DOI] [PubMed] [Google Scholar]
- 30.Davis J.W., Shackford S.R., Mackersie R.C., Hoyt D.B. Base deficit as a guide to volume resuscitation. J Trauma. 1988;28(10):1464–1467. doi: 10.1097/00005373-198810000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Porter J.M., Ivatury R.R. In search of the optimal end points of resuscitation in trauma patients: a review. J Trauma. 1998;44(5):908–914. doi: 10.1097/00005373-199805000-00028. [DOI] [PubMed] [Google Scholar]
- 32.Lazarev A., Golokhvast K., Borozda I. Review of the Problems of Diagnosis of Endopelvic Haemorrhage, its Intensity, Volume, and Duration, and Treatment Methods of Circulatory Injuries and Surgical Hemostasis after Pelvic Fractures. Emergency Medicine International. Hindawi. 2019;2019 doi: 10.1155/2019/2514146. https://www.hindawi.com/journals/emi/2019/2514146/ [cited 2020 Aug 2]. p. e2514146. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson M.H., Chang A., Brandes S.B. The value of digital rectal examination in assessing for pelvic fracture–associated urethral injury: what defines a high-riding or nonpalpable prostate? J Trauma Acute Care Surg. 2013;75(5):913–915. doi: 10.1097/TA.0b013e3182a68668. [DOI] [PubMed] [Google Scholar]
- 34.Verbeek D.O.F., Zijlstra I.A.J., van der Leij C., Ponsen K.J., van Delden O.M., Goslings J.C. The utility of FAST for initial abdominal screening of major pelvic fracture patients. World J Surg. 2014;38(7):1719–1725. doi: 10.1007/s00268-013-2412-z. [DOI] [PubMed] [Google Scholar]
- 35.Pearl W.S., Todd K.H. Ultrasonography for the initial evaluation of blunt abdominal trauma: a review of prospective trials [Internet]. Database of Abstracts of Reviews of Effects (DARE): quality-assessed Reviews [Internet] Centre for Reviews and Dissemination (UK) 1996 doi: 10.1016/s0196-0644(96)70273-1. https://www.ncbi.nlm.nih.gov/books/NBK66778/ [cited 2020 Aug 2]. Available from: [DOI] [PubMed] [Google Scholar]
- 36.Christian N.T., Burlew C.C., Moore E.E. The focused abdominal sonography for trauma examination can reliably identify patients with significant intra-abdominal hemorrhage in life-threatening pelvic fractures. J Trauma Acute Care Surg. 2018;84(6):924–928. doi: 10.1097/TA.0000000000001838. [DOI] [PubMed] [Google Scholar]
- 37.Prospective evaluation of non-radiologist performed emergency abdominal ultrasound for haemoperitoneum. Emerg Med J. 2020 doi: 10.1136/emj.2003.006932. https://emj.bmj.com/content/21/5/e5 [Internet]. [cited 2020 Sep 23]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zamani M., Masoumi B., Esmailian M., Habibi A., Khazaei M., Mohammadi Esfahani M. A comparative analysis of diagnostic accuracy of focused assessment with sonography for trauma performed by emergency medicine and radiology residents. Iran Red Crescent Med J. 2015 doi: 10.5812/ircmj.20302. [cited 2020 Sep 23];17(12). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4706728/ [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 39.Cortina Gualdo J., Barastegui Fernandez D., Teixidor Serra J., Tomás Hernández J., Pacha Vicente D., Monforte Alemany R. Pelvic fractures in polytrauma: which classification system better predicts hemodynamic instability? Eur Orthop Traumatol. 2013;4(1):35–39. [Google Scholar]
- 40.Çorbacıoğlu Ş.K., Aksel G. Whole body computed tomography in multi trauma patients: review of the current literature. Turk J Emerg Med. 2018;18(4):142–147. doi: 10.1016/j.tjem.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arora R., Arora A.J. Justification of whole-body CT in polytrauma patients, can clinical examination help selecting patients? Quant Imag Med Surg. 2019;9(4):636–641. doi: 10.21037/qims.2019.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Exadaktylos A.K., Sclabas G., Schmid S.W., Schaller B., Zimmermann H. Do we really need routine computed tomographic scanning in the primary evaluation of blunt chest trauma in patients with “normal” chest radiograph? J Trauma. 2001;51(6):1173–1176. doi: 10.1097/00005373-200112000-00025. [DOI] [PubMed] [Google Scholar]
- 43.Huber-Wagner S., Lefering R., Qvick L.-M. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet Lond Engl. 2009;373(9673):1455–1461. doi: 10.1016/S0140-6736(09)60232-4. [DOI] [PubMed] [Google Scholar]
- 44.Shannon L., Peachey T., Skipper N. Comparison of clinically suspected injuries with injuries detected at whole-body CT in suspected multi-trauma victims. Clin Radiol. 2015;70(11):1205–1211. doi: 10.1016/j.crad.2015.06.084. [DOI] [PubMed] [Google Scholar]
- 45.Rubash H.E., Mears D.C. External fixation of the pelvis. Instr Course Lect. 1983;32:329–348. [PubMed] [Google Scholar]
- 46.Young J.W., Burgess A.R., Brumback R.J., Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160(2):445–451. doi: 10.1148/radiology.160.2.3726125. [DOI] [PubMed] [Google Scholar]
- 47.Burgess A.R., Eastridge B.J., Young J.W. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30(7):848–856. [PubMed] [Google Scholar]
- 48.García J.M., Doblaré M., Seral B., Seral F., Palanca D., Gracia L. Three-dimensional finite element analysis of several internal and external pelvis fixations. J Biomech Eng. 2000;122(5):516–522. doi: 10.1115/1.1289995. [DOI] [PubMed] [Google Scholar]
- 49.Calafi LA, Routt MC. Anterior pelvic external fixation: is there an optimal placement for the supra-acetabular pin? :3. [PubMed]
- 50.Meselhy M.A., Essmat E.E., Ali A.M., Singer M.S. Safe zones of pin insertion in the pelvis and acetabulum: a cadaver study. Curr Orthop Pract. 2017;28(1):79–83. [Google Scholar]
- 51.Stewart R.G., Hammer N., Kieser D.C. External fixation of unstable pelvic fractures: a systematic review and meta-analysis. ANZ J Surg. 2019;89(9):1022–1027. doi: 10.1111/ans.15027. [DOI] [PubMed] [Google Scholar]
- 52.Schmal H., Larsen M.S., Stuby F., Strohm P.C., Reising K., Goodwin Burri K. Effectiveness and complications of primary C-clamp stabilization or external fixation for unstable pelvic fractures. Injury. 2019;50(11):1959–1965. doi: 10.1016/j.injury.2019.08.039. [DOI] [PubMed] [Google Scholar]
- 53.Gänsslen A., Krettek C., Pohlemann T. Emergency stabilization of pelvic instabilities with the pelvic C-clamp. Eur J Trauma. 2004;30(6):412–419. [Google Scholar]
- 54.Archdeacon M.T., Safian C., Le T.T. A cadaver study of the trochanteric pelvic clamp for pelvic reduction. J Orthop Trauma. 2007;21(1):38–42. doi: 10.1097/BOT.0b013e31802ea964. [DOI] [PubMed] [Google Scholar]
- 55.Pohlemann T., Gänsslen A., Bosch U., Tscherne H. The technique of packing for control of hemorrhage in complex pelvic fractures. Tech Orthop. 1994;9(4):267–270. [Google Scholar]
- 56.Whitehouse J.S., Weigelt J.A. Diagnostic peritoneal lavage: a review of indications, technique, and interpretation. Scand J Trauma Resuscitation Emerg Med. 2009;17:13. doi: 10.1186/1757-7241-17-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Papakostidis C., Giannoudis P.V. Pelvic ring injuries with haemodynamic instability: efficacy of pelvic packing, a systematic review. Injury. 2009;40:S53–S61. doi: 10.1016/j.injury.2009.10.037. [DOI] [PubMed] [Google Scholar]
- 58.Ron G., Epstein D., Ben-Galim P., Klein Y., Kaban A., Sagiv S. Extra-peritoneal pressure packing without external pelvic fixation: a life-saving stand-alone surgical treatment. J Emergencies, Trauma, Shock. 2015;8(4):181. doi: 10.4103/0974-2700.166586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blondeau B., Orlando A., Jarvis S. Variability in pelvic packing practices for hemodynamically unstable pelvic fractures at US level 1 trauma centers. Patient Saf Surg. 2019;13(1):3. doi: 10.1186/s13037-019-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Margolies M.N., Ring E.J., Waltman A.C., Kerr W.S., Baum S. Arteriography in the management of hemorrhage from pelvic fractures. N Engl J Med. 1972;287(7):317–321. doi: 10.1056/NEJM197208172870701. [DOI] [PubMed] [Google Scholar]
- 61.Gänsslen A., Giannoudis P., Pape H.-C. Hemorrhage in pelvic fracture: who needs angiography? Curr Opin Crit Care. 2003;9(6):515–523. doi: 10.1097/00075198-200312000-00009. [DOI] [PubMed] [Google Scholar]
- 62.Scemama U., Dabadie A., Varoquaux A. Pelvic trauma and vascular emergencies. Diagn Interv Imaging. 2015;96(7):717–729. doi: 10.1016/j.diii.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 63.Sagawa K., Sawano M. A case series of pelvic fracture patients who developed lower urinary tract symptoms after transarterial embolization of bilateral internal iliac arteries. Acute Med Surg. 2017;4(3):358–362. doi: 10.1002/ams2.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wijffels D.J., Verbeek D.O., Ponsen K.J., Carel Goslings J., van Delden O.M. Imaging and endovascular treatment of bleeding pelvic fractures: review article. Cardiovasc Intervent Radiol. 2019;42(1):10–18. doi: 10.1007/s00270-018-2071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Langford J.R., Burgess A.R., Liporace F.A., Haidukewych G.J. Pelvic fractures: part 1. Evaluation, classification, and resuscitation. J Am Acad Orthop Surg. 2013;21(8):448–457. doi: 10.5435/JAAOS-21-08-448. [DOI] [PubMed] [Google Scholar]
- 66.Broadwell S.R., Ray C.E. Transcatheter embolization in pelvic trauma. Semin Intervent Radiol. 2004;21(1):23–35. doi: 10.1055/s-2004-831402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vaidya R., Waldron J., Scott A., Nasr K. Angiography and embolization in the management of bleeding pelvic fractures. J Am Acad Orthop Surg. 2018;26(4):e68–e76. doi: 10.5435/JAAOS-D-16-00600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Muntasar A.E., Toner E., Alkhazaaleh O.A. Effect of angioembolisation versus surgical packing on mortality in traumatic pelvic haemorrhage: a systematic review and meta-analysis. World J Emerg Med. 2018;9(2):85–92. doi: 10.5847/wjem.j.1920-8642.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Suzuki T., Smith W.R., Moore E.E. Pelvic packing or angiography: competitive or complementary? Injury. 2009;40(4):343–353. doi: 10.1016/j.injury.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 70.Copp J., Eastman J.G. Novel resuscitation strategies in patients with a pelvic fracture. Injury. 2020 doi: 10.1016/j.injury.2020.01.042. https://www.injuryjournal.com/article/S0020-1383(20)30070-X/abstract [cited 2020 Sep 24];0(0). Available from: [DOI] [PubMed] [Google Scholar]
- 71.Cheng M., Lee K.-Y., Chang A.-M.L. Three-in-one protocol reduces mortality of patients with haemodynamically unstable pelvic fractures-a five year multi-centred review in Hong Kong. Int Orthop. 2018;42(10):2459–2466. doi: 10.1007/s00264-018-3842-x. [DOI] [PubMed] [Google Scholar]
- 72.Enninghorst N., Toth L., King K.L., McDougall D., Mackenzie S., Balogh Z.J. Acute definitive internal fixation of pelvic ring fractures in polytrauma patients: a feasible option. J Trauma. 2010;68(4):935–941. doi: 10.1097/TA.0b013e3181d27b48. [DOI] [PubMed] [Google Scholar]
- 73.Gardner M.J., Chip Routt M.L. The antishock iliosacral screw. J Orthop Trauma. 2010;24(10):e86–e89. doi: 10.1097/BOT.0b013e3181c81d65. [DOI] [PubMed] [Google Scholar]
- 74.Becker C.A., Kussmaul A.C., Suero E.M. Tape suture for stabilization of incomplete posterior pelvic ring fractures—biomechanical analysis of a new minimally invasive treatment for incomplete lateral compression pelvic ring fractures. J Orthop Surg. 2019 doi: 10.1186/s13018-019-1509-y. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935107/ [cited 2020 Aug 7];14. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen L., Zhang G., Wu Y., Guo X., Yuan W. Percutaneous limited internal fixation combined with external fixation to treat open pelvic fractures concomitant with perineal lacerations. Orthopedics. 2011 doi: 10.3928/01477447-20111021-10. http://www.slackinc.com/doi/resolver.asp?doi=10.3928/01477447-20111021-10 [cited 2020 Aug 7]; Available from: [DOI] [PubMed] [Google Scholar]
- 76.Gurevitz S., Bender B., Tytiun Y., Velkes S., Salai M., Stein M. The role of pelvic fractures in the course of treatment and outcome of trauma patients. Isr Med Assoc J IMAJ. 2005;7(10):623–626. [PubMed] [Google Scholar]
- 77.Steer R., Balendra G., Matthews J., Wullschleger M., Reidy J. The use of anterior subcutaneous internal fixation (INFIX) for treatment of pelvic ring injuries in major trauma patients, complications and outcomes. SICOT-J. 2020 doi: 10.1051/sicotj/2019019. [Internet]. [cited 2020 Aug 7];5. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6598424/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Becker C.A., Kammerlander C., Kußmaul A.C. Modified less invasive anterior subcutaneous fixator for unstable Tile-C-pelvic ring fractures: a biomechanical study. Biomed Eng Online. 2019;18(1):38. doi: 10.1186/s12938-019-0648-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Plaisier B.R., Meldon S.W., Super D.M., Malangoni M.A. Improved outcome after early fixation of acetabular fractures. Injury. 2000;31(2):81–84. doi: 10.1016/s0020-1383(99)00233-8. [DOI] [PubMed] [Google Scholar]
- 80.Vallier H.A., Cureton B.A., Ekstein C., Oldenburg F.P., Wilber J.H. Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma. 2010;69(3):677–684. doi: 10.1097/TA.0b013e3181e50914. [DOI] [PubMed] [Google Scholar]
- 81.Buller L.T., Best M.J., Quinnan S.M. A nationwide analysis of pelvic ring fractures: incidence and trends in treatment, length of stay, and mortality. Geriatr Orthop Surg Rehabil. 2016;7(1):9–17. doi: 10.1177/2151458515616250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Devaney G.L., Bulman J., King K.L., Balogh Z.J. Time to definitive fixation of pelvic and acetabular fractures. J Trauma Acute Care Surg. 2020 doi: 10.1097/TA.0000000000002860. [cited 2020 Sep 23];Publish Ahead of Print. Available from: https://journals.lww.com/jtrauma/Abstract/9000/Time_to_Definitive_Fixation_of_Pelvic_and.97800.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vallier H.A., Dolenc A.J., Moore T.A. Early appropriate care: a protocol to standardize resuscitation assessment and to expedite fracture care reduces hospital stay and enhances revenue. J Orthop Trauma. 2016;30(6):306–311. doi: 10.1097/BOT.0000000000000524. [DOI] [PubMed] [Google Scholar]
- 84.Coccolini F., Stahel P.F., Montori G. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12(1):5. doi: 10.1186/s13017-017-0117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pape H.C., Andruszkow H., Pfeifer R., Hildebrand F., Barkatali B.M. Options and hazards of the early appropriate care protocol for trauma patients with major fractures: towards safe definitive surgery. Injury. 2016;47(4):787–791. doi: 10.1016/j.injury.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 86.Bone L.B., Johnson K.D., Weigelt J., Scheinberg R. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am. 1989;71(3):336–340. [PubMed] [Google Scholar]
- 87.Mirza A., Ellis T. Initial management of pelvic and femoral fractures in the multiply injured patient. Crit Care Clin. 2004;20(1):159–170. doi: 10.1016/s0749-0704(03)00096-4. [DOI] [PubMed] [Google Scholar]
- 88.McGowan S.P., Fallahi A.-K.M. Degloving injuries. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2020 http://www.ncbi.nlm.nih.gov/books/NBK557707/ [cited 2020 Sep 24]. Available from: [PubMed] [Google Scholar]
- 89.Küper M.A., Trulson A., Stuby F.M., Stöckle U. Pelvic ring fractures in the elderly. EFORT Open Rev. 2019;4(6):313–320. doi: 10.1302/2058-5241.4.180062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rupprecht H., Heppner H.J., Wohlfart K., Türkoglu A. The geriatric polytrauma: risk profile and prognostic factors. Ulus Travma Ve Acil Cerrahi Derg Turk J Trauma Emerg Surg TJTES. 2017;23(2):156–162. doi: 10.5505/tjtes.2016.77177. [DOI] [PubMed] [Google Scholar]
- 91.Borger van der Burg B.L.S., van Dongen T.T.C.F., Morrison J.J. A systematic review and meta-analysis of the use of resuscitative endovascular balloon occlusion of the aorta in the management of major exsanguination. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc. 2018;44(4):535–550. doi: 10.1007/s00068-018-0959-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Özkurtul O., Staab H., Osterhoff G. Technical limitations of REBOA in a patient with exsanguinating pelvic crush trauma: a case report. Patient Saf Surg. 2019;13:25. doi: 10.1186/s13037-019-0204-6. [DOI] [PMC free article] [PubMed] [Google Scholar]