Abstract
The emergence of Covid-19 has caused a pandemic and is a major public health concern. Covid-19 has fundamentally challenged the global health care system in all aspects. However, there is a growing concern for the subsequent detrimental effects of continuing delays or adjustments on time-dependent treatments for Covid-19 negative patients. Patients arriving to the ED with STEMIs and acute CVA are currently presumed to have delays due to Covid-19 related concerns. The objective of this paper is to evaluate the implications of the Covid-19 pandemic on non-Covid19 patients in emergency care settings. We conducted a retrospective study from February 2020 to April 2020 and compared this to a parallel period in 2019 to assess the impact of the Covid-19 pandemic on three distinct non-Covid-19 ED diagnosis that require immediate intervention. Our primary outcome measures were time to primary PCI in acute STEMI, time to fibrinolysis in acute CVA, and time to femoral hip fracture correction surgery. Our secondary outcome measure included a composite outcome of length of stay in hospital and mortality. From 1 February 2020 to 30 April 2020, the total referrals to ED diagnosed with STEMI, Hip fracture and CVA of which required intervention were 197 within Covid-19 group 2020 compared to 250 in the control group 2019. Mean duration to intervention (PCI, surgery and tPA, respectively) did not differ between COVID-19 group and 2019 group. Among femoral hip fracture patients', the referral numbers to ED were significantly lower in Covid-19 era (p = 0.040) and the hospitalization stay was significantly shorter (p = 0.003). Among CVA patients', we found statistical differences among the number of referrals and the patients' age. Coping with the Covid-19 pandemic presents a challenge for the general healthcare system. Our results suggest that with proper management, despite the obstacles of isolation policies and social distancing, any negative impact on the quality of health care for the non-Covid-19 patients can be minimized in the emergency department setting.
Keywords: Non-covid-19, Quality indicator, STEMI, CVA, Femoral fracture
Introduction
The emergence of acute respiratory syndrome coronavirus disease (Covid-19) in China towards the end of 2019 has caused a world-wide outbreak and is a major public health concern [1]. The rapid evolution of the Covid-19 pandemic has fundamentally challenged the global health care system with ongoing adjustments.
Hospital emergency departments (EDs) play a crucial role in the acute health care system, providing care for patients with acute illness and injury, and the provision of health care system access [2].
One of the current modifications performed within the ED setting is providing an immediate isolation of patients presenting with symptoms concerning for Covid-19 from non-Covid-19 patients [3]. A month prior to the Covid-19 outbreak in Israel, a facility for isolation and treatment was established in our hospital with the goals of early triage, identification of suspected Covid-19 patients and preventing risk of furthering the spread of disease. The rationale was providing high level care, maximizing protection of medical and logistics personnel from exposure, prevention of contamination of the main hospital campus, all while reducing risk of disease transmission. All goals were to be accomplished without neglecting the routine and urgent lifesaving care of non-Covid-19 patients. Our hospital was the first to admit suspected Covid-19 positive patients in Israel.
On the one hand, social distancing is essential to reduce disease spread to the public and maintain health-care provider safety. On the other hand, this isolation management can potentially endanger healthcare routine, including general healthcare practice and life-savinginterventions [4].
The first wave of Covid-19 in Israel started with the first confirmed case diagnosed on February 21st and thereafter hospitalized at our hospital. Within approximately 1 month, confirmed Covid-19 cases climbed up to 1000, accompanied by an exponential increase within less than 3 days. Approximately 1 week later, the number exceeded 4000 cases total, subsequently followed extreme lockdown measures taken by the Israeli government, after which the daily infection rate witnessed a sharp decline from the peak value of 1131 cases per day down to slightly more than 100 new confirmed cases on April 30.
As of 14 May 2020, the number of covid-19 patients in Israel was 16,548 with 264 cases resulting in death [5]. We sought to evaluate the implications of the Covid-19 pandemic on the management of medical emergencies and acute patient care in the emergency department (ED). To this date, there is limited evidence regarding the impact of Covid-19 outbreak on routine care for non-Covid-19 patients in the hospital.
Methods
Study design
We conducted a retrospective study, 1:1 parallel group, comparing data of a 3-month period, February to April 2020, and of each month separately to the exact data of the parallel period in 2019.
The study was conducted at the Chaim Sheba Medical Center in Tel-Hashomer, a university-affiliated tertiary referral medical center, and largest hospital in Israel.
The institutional review board at our hospital approved this study.
It is true that the spike of the "first wave" in our country was in March, and in February there were a relatively small number of Covid19 cases. To examine the developments in the hospital in its entirety, from the beginning until the end of the first wave, we chose to conduct the study a month prior to the peak impact of pandemic Covid-19.
Data was collected from both the ED and hospitalization wards. Data included patient demographic information, diagnosis at admission, time to immediate intervention, and outcomes (including length of stay, discharge, and mortality). This period comprises 1 month prior to the Covid-19 pandemic outbreak in Israel, and the 2 months into the outbreak period as previously explained. We compared data of the total 3-month period and of each month separately to data of the parallel period in 2019.
Emergency department (ED) reorganization
Facilities
We divided the ED into two main divisions: a general ED dealing with non-Covid-19 patients and an ED dealing with suspected and confirmed Covid-19 patients. A highly trained and experienced triage nurse wearing protective personal equipment (PPE) was placed in front of the main entrance to the ED and directed all incoming patients to one of the aforementioned sections.
Screening for suspected Covid-19 patients was based on epidemiology, medical history, and clinical symptoms. A patient with no epidemiological or clinical criteria entered the standard ED, while a patient exhibiting one or more of the Covid-19 positive criteria was sent to the biological ED. The triage nurse directed each patient to a different section according to the clinical and epidemiological status. The biological section had no contact with the standard ED so that patients and the staff of each section would have no interactions. All suspected patients were screened via nasopharyngeal sampling for SARS-CoV-19 using rtPCR testing for three genes (N gene, E gene, and RdRP gene; Seegene, South Korea).
At risk patients were transferred to the intended biological ED through a separate entrance than that of the regular ED entrance. [6]
Human resources
Our hospital announced the adaptation and implementation of emergency and disaster relief protocols in the setting of an impending epidemic. Specifically including shifts to 12-h working periods from 7AM-7PM. Elective procedures were cancelled, hence allowing for many physicians to assist in our emergency department as well as the Covid-19 ward, additional, internal medical specialists, currently in their sub-specialization, were also recruited to work in the emergency department. The medical team in the ED contained 12 "physicians' capsule" for 12-h shifts compared to routine periods, where there are approximately 6–8 physicians until evening, and 3–5 physicians for the night until the morning. Regarding the para-medical team, former emergency nurses from around the hospital were recruited back to the ED to help, there were 25 nurses and 5 unskilled assistants for 12-h shifts. In a routine time, the morning starts with 10 nurses and every two hours two additional nurses would join the team until there are 17 nurses in the ED and 5 unskilled assistants. From 11 pm, every hour one nurse would be discharged home until 10 nurses remain until the morning.
Study population
We included hospitalized adult patients from the ED in our hospital from February to April 2020. We selected the patients with one of three diagnoses upon arrival: acute ST segment-elevation myocardial infarction (STEMI), acute ischemic cerebral vascular accident (CVA) and femoral neck fracture. Data included patient's demographic information, diagnosis at admission and time to immediate intervention (primary PCI, immediate fibrinolysis and femoral neck correction surgery).
Three different population groups:
A. All patients presenting to the ED with acute STEMI and undergoing primary PCI during their hospital stay in the first 24 h upon arrival to the ED.
The primary aim is urgent reestablishment of reperfusion by means of percutaneous coronary intervention (PCI).
B. All patients above 65 years of age, presenting in the ED with femoral neck fracture and undergoing correction surgery during hospitalization.
C. All patients above 18 years of age presenting with acute ischemic cerebral stroke and receiving intravenous rtPA (recombinant tissue plasminogen activator) treatment.
The three groups mentioned above (STEMI, acute ischemic stroke and femoral fracture groups') constitute for non-Covid-19 patient as Covid-19 patients were excluded from the study. If a patient in the biological ED required emergency treatment that could not be administered in that section, such as surgery, catheterization, computed tomography scan, they were transferred, via a specific route cleared in the hospital, to the designated area for suspected or confirmed Covid-19 patients. Medical staff treating these patients were required to wear the same PPE as the ED personnel [6].
Outcome
Our primary outcome divides into three individual "time windows" defined as Quality Indicator (QI) that are measured routinely in our hospital consisting of three different aspects (cardiovascular, neurological, orthopedic).
A. Door-to-balloon time in primary Percutaneous Coronary Intervention (PCI) in Acute ST segment elevation myocardial infarction (STEMI) on electrocardiogram (ECG): all patients presenting to the ED with acute STEMI and undergoing urgent primary PCI with a time-to-PCI of 90 min or less upon arrival to the ED.
Direct correlation exists between timed primary PCI and mortality and morbidity in patients presenting with acute STEMI in a time window of less than 90 min [9–11].
B. Acute femoral neck fracture- time to correction surgery—all patients above 65 years of age, presenting in the ED with femoral neck fracture and undergoing correction surgery within 48 h of hospital arrival. Surgery for hip fracture correction performed in less than 48 h upon hospital arrival is associated directly with a decrease in morbidity, complication, and post-operative mortality rate [12–14].
C. Recombinant tissue plasminogen activator (rtPA) Door-To-Needle time in acute cerebral ischemia- acute CVA- patients above 18 years of age presenting with acute cerebral ischemic stroke and receiving intravenous rtPA treatment in a time window of ≤ 4.5-h from symptom onset. [16] Fibrinolysis (rtPA) treatment is a class A1 recommendation by American heart association (AHA)/American Stroke Association (ASA) since 2013. Clinical trials have shown the advantage of receiving parenteral rtPA in less than 4.5 h of symptoms onset [16], with a similar QI measured in several countries in Europe and in the US. [16–19].
These three QI were selected to evaluate routine clinical practice. Quality indicators are defined as processes in which the evidence is strong enough that failure to perform such actions reduces the likelihood of optimal patient outcomes [7]. QI serves as a standard of care by which performance of individual hospitals are measured [8]. Quantifying adherence to quality indicators can serve as a direct measure of quality of care and provide a foundation for quality improvement.
The three QIs above represent urgent care of three provisions- cardiovascular, orthopedic, and neurological. All processes are time-critical and require multidisciplinary care of medical and para-medical staff including emergency department, imaging department, cardiological department, orthopedics, neurologists, intensive care units and the operating rooms coordination and availability.
The three QIs above represent urgent care of three provisions- cardiovascular, orthopedic, and neurological. These three measures are, therefore, suggested to provide a complete picture of the overall operation and activity in the hospital.
Our secondary outcome measure included a patient's referral, length of stay, time of discharge, and mortality.
Statistical analysis
Statistical analyses were performed using SPSS version 25.0. The data was presented as the mean ± standard deviation. T test and Anova Test with Post Hoc analysis were used for comparison between groups. Intergroup comparisons and Categorical variables Comparison were made using T test, Fisher's Exact Test Levin's test, ANOVA with PostHoc, or X2 test.
Probability values of less than 0.05 were considered statistically significant.
Results
Three selected performance measures were conducted throughout the first wave of Covid-19 pandemic in our country From February 1, 2020 to April 30, 2020. We measured three separated groups: Door to primary PCI in STEMI, time to correction surgery in acute femoral neck fracture and time to rtPA in acute cerebral ischemic stroke.
The overall patients' referrals in all three groups to the ED were lower compared to the same period in 2019. In the STEMI population, 60 patients vs. 68 patients, while 119 patients vs. to 152 patients presented with femoral neck fractures and 18 patients vs. 30 patients presented with acute ischemic stroke in compared cohorts between 2020 and 2019, respectively. ED Referrals' were lower, most probable due to patient fear of treatments at medical facilities containing Covid-19 patients, as well as the lockdown creating technical issues including less mobilization around the country.
Table 1 summarizes data regarding 128 patients in the STEMI measures consisting of both periods- Covid-19 group 2020 and the control group in 2019.
Table 1.
Summarize data characteristics of 128 patients diagnosed with ST-elevation myocardial infarction require urgent primary coronary intervention and comparison between the two groups: COVID- 19 period to the control group from 2019
| Covid19 | Control | P value | ||
|---|---|---|---|---|
| No. of cases (n) | N = 60 | N = 68 | 0.500 | |
| Age (mean ± SD) | 63 ± 10.6 | 64 ± 12 | 0.732 | |
| Gender | Female (%) | 16 (30) | 14 (16) | 0.418 |
| Male (%) | 44 (70) | 54 (84) | ||
| Length of stay (days) | 5.83 ± 3.3 | 5.50 ± 5.3 | 0.676 | |
| Door to intervention (Minutes) | 85 ± 214 | 46 ± 34.2 | 0.072 | |
| Mortality | No mortality (n) | 57 | 65 | 0.599 |
| In hospital mortality (n) | 3 | 3 | ||
| Out hospital mortality (n) | 0 | 0 |
All data are presented in the form of mean (Standard deviation) unless otherwise specified
No statistical differences in age, gender, length of hospital stay, or mortality rate were found between the groups (P > 0.05 T test and Fisher's Exact Test, X2 test).
Primary outcome measured door to primary PCI in minutes was longer during the Covid-19 2020 period compared to the pre-Covid-19 2019 period, with 85.1 min vs. 45.8 min, respectively; however, this difference was not statistically significant (p = 0.070).
When comparing the "time windows" in the two compared groups for each month separately, analysis of variance (ANOVA) was used, and showed no statistically significant differences between the periods.
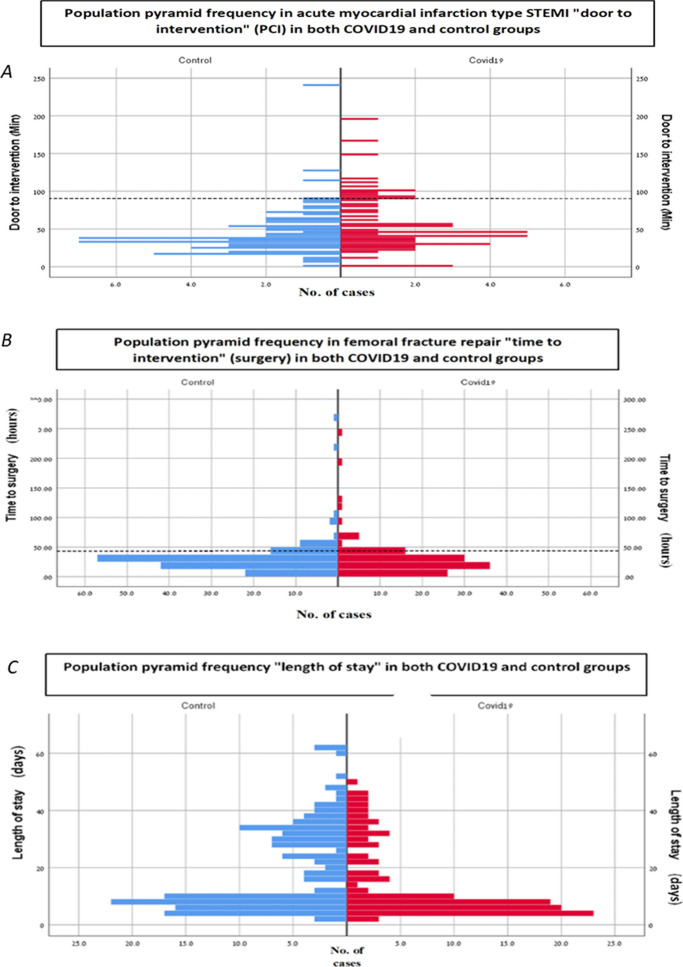
Figure 1a primary outcome demonstrates as a population pyramid histogram by frequency of cases and "door-to-intervention" by minutes in the two groups: in both the Covid-19 group and the control, the time defined best for intervention is less than 90 min.
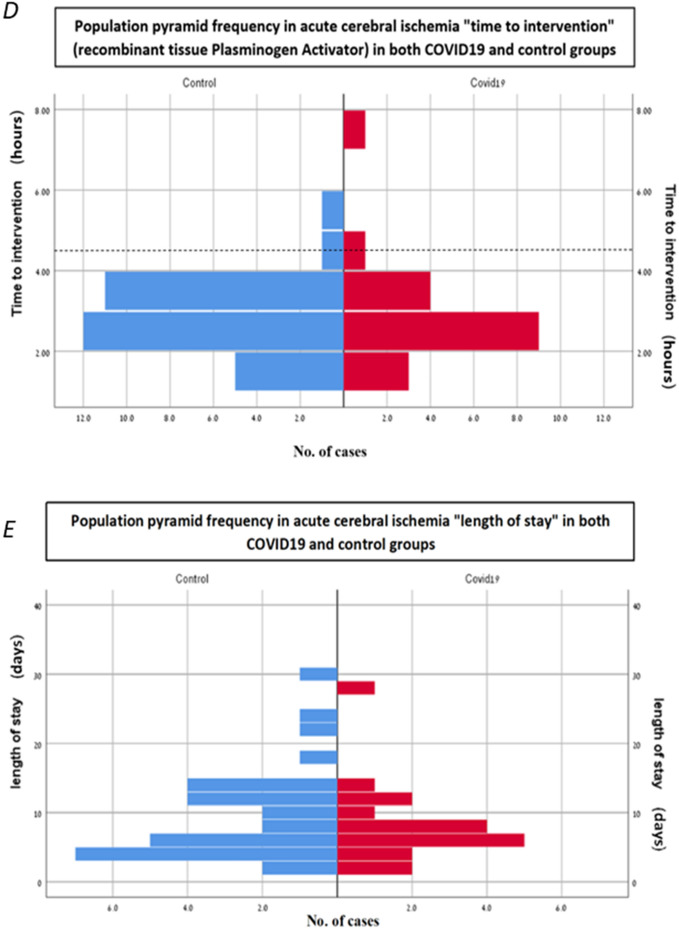
Fig. 1.
Demonstrate a population pyramid histograms concerning the three quality measures: acute ST-segment elevation myocardial infarction, acute femur fracture and acute cerebral ischemia, comparing both parallel periods: covid-19 group and the control group. a Represent time to percutaneous coronary intervention in minutes by frequency cases comparing both parallel periods. The dash line represents the goal established to reduce mortality and morbidity (a time-to-PCI ≤ 90 min). b Represent the time to femoral surgery in hours by frequency cases comparing both parallel periods. The dash line represents the goal established to reduce mortality and morbidity (a time-to-surgery ≤ 48 h). c Demonstrate a population frequency and length of hospitalization in days after femoral repair. d Represent the time to tissue plasminogen activator (thrombolysis) in hours by frequency cases while comparing both parallel periods in acute cerebral ischemia. The dash line represents the goal established to reduce mortality and morbidity (a time-to-tPa ≤ 4.5 h). e Demonstrate a population pyramid by histogram frequency demonstrate length of hospitalization in days while comparing both parallel periods in acute cerebral ischemia
Table 2 summarizes the data regarding all 271 patients in the Covid-19 2020 group and its control group 2019. As mentioned above, the number of patients referred to hospital with femoral neck fracture was significantly lower in the Covid19 group (p = 0.040). No statistical differences in age, gender or mortality rate were found between the groups (P > 0.05 T test and Fisher's Exact Test, X2 test).
Table 2.
Summarize the characteristics data regards 271 diagnosed with femoral fracture and required surgery of both groups and comparison between the COVID- 19 periods of time to the control group in 2019. All data are presented in the form of mean (Standard deviation) unless otherwise specified
| No. of cases (n) | COVID-19 | Control | P value | |
|---|---|---|---|---|
| N = 119 | N = 152 | 0.040 | ||
| Gender | Female (%) | 87 (73) | 98 (64) | 0.130 |
| Male (%) | 32 (27) | 54 (36) | ||
| Age (mean) | 83 ± 8 | 83 ± 8 | 0.895 | |
| Length of stay (days) | 14 | 19 | 0.003 | |
| Time to surgery (hours) | 30.96 ± 32 | 31.74 ± 30 | 0.092 | |
| Mortality | No mortality | 114 | 148 | 0.141 |
| In hospital mortality | 3 | 0 | ||
| Out hospital mortality | 2 | 4 | ||
Interestingly, the mean length of hospital stay (days) was statistically shorter during the Covid-19 period (13.9 days vs. 19 days, respectively, p = 0.003). The decreased length of hospitalization stay can be explained by several aspects: many rehabilitation centers were temporarily closed thereby minimizing the stay in hospital waiting for transfer to these institutions. The few rehabilitation centers that were opened during the pandemic were forced to isolate their patients from all visitors, and neither the families nor the patients wanted to stay in such conditions, hence the mean length of hospital stay had shortened dramatically.
Time to correction surgery (hours) was 30.96 h during the Covid-19 period compared to the control group with 31.74 h. This difference was not statistically significant.
Figure 1b, c demonstrates a population pyramid histogram frequency of "time to correction surgery-femoral neck" in hours and "length of hospital stay" by days in both control and Covid-19 groups, respectively.
Table 3 summarizes the data regarding all 48 patients from both groups and compares between the Covid-19 group and the control group in 2019 (Table 3).
Table 3.
Summarize the characteristics data regards 48 diagnosed with acute cerebral ischemic stroke required urgent Recombinant tissue plasminogen activator and comparison between the COVID- 19 periods of time to the control group from 2019. All data are presented in the form of mean (standard deviation) unless otherwise specified
| No. of cases (n) | Covid19 | Control | P value | |
|---|---|---|---|---|
| 18 | 30 | 0.032 | ||
| Gender | Female (%) | 9 (50) | 11 (37) | 0.252 |
| Male (%) | 9 (50) | 19 (63) | ||
| Age (mean) | 80 ± 9 | 72 ± 14 | 0.015 | |
| Length of stay (days) | 8 ± 6 | 9 ± 7 | 0.408 | |
| Time to intervention (hours) | 3.06 ± 1.5 | 2.77 ± 1 | 0.409 | |
| Mortality | No mortality | 15 | 29 | 0.055 |
| In hospital mortality | 3 | 0 | ||
| Out hospital mortality | 0 | 1 | ||
There was a statistically significant difference in the mean age of patients presenting with acute ischemic stroke in the Covid-19 period (80 years) vs. the same period in the year before (72 years), (p = 0.015). No statistical differences in gender or length of hospital stay were found between the groups (P > 0.05 T test and Fisher's Exact Test, X2 test).
Time to intervention (min) was longer during the Covid-19 period compared with the control group with 3.05 h vs. 2.76 h, respectively; however, this difference was not statistically significant (p = 0.409).
Interestingly, mortality rate presented an upward trend and was higher during the Covid-19 outbreak with 16.66% (3/18) all in-hospital mortality compared to 3.5% (1/29) in the control group out-of-hospital (after home discharge) (p = 0.055). It is plausibly explained by patients' delay or hesitancy in receiving interventional treatment.
Figure 1d, e demonstrates a population pyramid by histogram frequency of "time to intervention" in hours and presenting length of hospital stay by days while comparing both periods covid-19 and the control, respectively. The dash line represents the goal established to reduce mortality and morbidity by a timed rtPA ≤ 4.5 h).
Discussion
To our knowledge, this is the only study regarding variable aspects of urgent routine care for non-Covid-19 patients during the current Covid-19 pandemic. The variables were compared to the parallel period in the previous year. We report a substantial decrease in patient referrals during the Covid-19 period but similar results in aspects of performance and achievement of good quality care outcomes.
Our method of triage and medical staff reorganization as described in the methods section above enabled us to prevent the admission of positive Covid-19 patients into the main hospital, thereby protecting our patients and staff from increased risks of exposure. It allowed the continuity of high-quality care of non-Covid-19 patients and minimized potential harm for those in need of routine urgent care.
Although there was a decrease in ED referrals (owing to quarantine, patients fear, less outside activities and less accidents), the ED burden was higher, but the medical staff/patient ratio and the quality of care remained unchanged.
As Covid-19 emerged in Israel in March 2020, all-cause mortality rapidly increased. Although we are still in an ongoing pandemic and mortality data is not accurate, the mortality rate observed during the pandemic was higher than those noted in the past 5 years [20]. The high mortality rate was attributed to the fact that people could not be treated appropriately in terms of immediate care as hospitals became overwhelmed [21]. We can see this trend in stroke patients referred to the hospital. In the Covid-19 group the patients were older, and mortality was higher.
Our findings suggest that the measures taken to provide a separation between Covid-19 vs. non-Covid-19 from their arrival at the emergency department regardless of the complexity, enabled high quality medical outcomes.
In conclusion, with appropriate preparation, management, and proper investments, life-saving interventions and treatments can be performed within the recommended times for non-Covid-19 patients in the face of the Covid-19 pandemic.
Abbreviations
- ED
Emergency department
- STEMI
ST elevation myocardial infarction
- CVA
Cerebrovascular accident
- tPA
Tissue plasminogen activator
- PCI
Percutaneous coronary intervention
Compliance with ethical standards
Conflict of interest
All authors declare that they have no conflict of interest.
Human and animal rights statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study, formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lai, C.-C., Shih, T.-P., Ko, W.-C., Tang, H.-J. & Hsueh, P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents 105924 (2020). [DOI] [PMC free article] [PubMed]
- 2.He J, Hou X, Toloo S, Patrick JR, Gerald GF. Demand for hospital emergency departments: a conceptual understanding. World J Emerg Med. 2011;2:253. doi: 10.5847/wjem.j.1920-8642.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chavez S, Long B, Koyfman A, Liang SY. Coronavirus Disease (COVID-19): A primer for emergency physicians. Med: Am. J. Emerg; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 5.Worldometers. COVID-19 Coronavirus Pandemic. (2020).(Accessed 14 May 2020).
- 6.Levy, Yuval, et al. Emergency Department Triage in the Era of COVID-19: The Sheba Medical Center Experience. The Israel Medical Association journal: IMAJ, 2020, 22.8: 470–475. [PubMed]
- 7.Spertus JA, et al. American College of Cardiology and American Heart Association methodology for the selection and creation of performance measures for quantifying the quality of cardiovascular care. J Am CollCardiol. 2005;45:1147–1156. doi: 10.1016/j.jacc.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Menees DS, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 9.Liebetrau C, et al. Direct admission versus transfer of AMI patients for primary PCI. Clin Res Cardiol. 2011;100:217–225. doi: 10.1007/s00392-010-0231-x. [DOI] [PubMed] [Google Scholar]
- 10.MEMBERS, W. C. et al. ACC/AHA clinical performance measures for adults with ST-elevation and non–ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Perfo). Circulation 113, 732–761 (2006). [DOI] [PubMed]
- 11.Simpson CR, et al. Five-year prognosis in an incident cohort of people presenting with acute myocardial infarction. PLoS ONE. 2011;6:e26573. doi: 10.1371/journal.pone.0026573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pollard TCB, Newman JE, Barlow NJ, Price JD, Willett KM. Deep wound infection after proximal femoral fracture: consequences and costs. J Hosp Infect. 2006;63:133–139. doi: 10.1016/j.jhin.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Antapur P, Mahomed N, Gandhi R. Fractures in the elderly: when is hip replacement a necessity? ClinInterv Aging. 2011;6:1. doi: 10.2147/CIA.S10204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ossendorf C, Scheyerer MJ, Wanner GA, Simmen H-P, Werner CML. Treatment of femoral neck fractures in elderly patients over 60 years of age-which is the ideal modality of primary joint replacement? Patient SafSurg. 2010;4:1–8. doi: 10.1186/1754-9493-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lowe JA, Crist BD, Bhandari M, Ferguson TA. Optimal treatment of femoral neck fractures according to patient’s physiologic age: an evidence-based review. OrthopClin. 2010;41:157–166. doi: 10.1016/j.ocl.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Saver JL, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309:2480–2488. doi: 10.1001/jama.2013.6959. [DOI] [PubMed] [Google Scholar]
- 17.Wiedmann S, et al. Variations in quality indicators of acute stroke care in 6 European countries: the European Implementation Score (EIS) Collaboration. Stroke. 2012;43:458–463. doi: 10.1161/STROKEAHA.111.628396. [DOI] [PubMed] [Google Scholar]
- 18.Meyers PM, et al. Performance and training standards for endovascular ischemic stroke treatment. J Neurosurg. 2010;113:149–152. doi: 10.3171/2009.12.JNS091813. [DOI] [PubMed] [Google Scholar]
- 19.Jauch EC, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 20.Michelozzi P, et al. Mortality impacts of the coronavirus disease (COVID-19) outbreak by sex and age: rapid mortality surveillance system, Italy, 1 February to 18 April 2020. Eurosurveillance. 2020;25:2000620. doi: 10.2807/1560-7917.ES.2020.25.19.2000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinnathamby MA, et al. All-cause excess mortality observed by age group and regions in the first wave of the COVID-19 pandemic in England. Eurosurveillance. 2020;25:2001239. doi: 10.2807/1560-7917.ES.2020.25.28.2001239. [DOI] [PMC free article] [PubMed] [Google Scholar]