Abstract
Hoffa fracture is a rare type of distal femoral fracture occurs in the coronal plane of either femoral epicondyle. To date, screws in combination with lateral plate fixation is widely accepted to achieve stable fixation and good results. However, up to now there has not been a specially designed anatomical plate for lateral fixation of Hoffa fracture. In this report, we demonstrate a case of Hoffa fracture fixed with reverse application of “L” shaped contralateral proximal tibia plate and cannulated screws, resulting in good one-year results.
Keywords: Hoffa fracture, Reverse contralateral proximal tibia plate, Open reduction, Internal fixation
Introduction
Distal femur fracture is typically confined in the axial and the sagittal plane. A rare type of distal femoral fracture occurs in the coronal plane of either femoral condyle, termed Hoffa fracture, which accounts for 8.7% to 13% of all distal femoral fractures [1]. Hoffa fractures are challenging to treat because of its size, anatomical location, and exposed shear stresses. The Letenneur classification is the most well-known and widely accepted classification for Hoffa fracture. For Letenneur Type I and Type III Hoffa fractures, some studies suggested that the preferred surgical technique is the use of screws in combination with lateral plate fixation rather than screws only [2,3] with good results at one year follow up [2,4]. However, up to now there has not been a specially designed anatomical plate for lateral fixation of Hoffa fracture. In this report, we would demonstrate a case of Hoffa fracture fixed with contralateral proximal tibial locking plate and cannulated screws, which eventually achieved a good functional outcome.
Case presentation
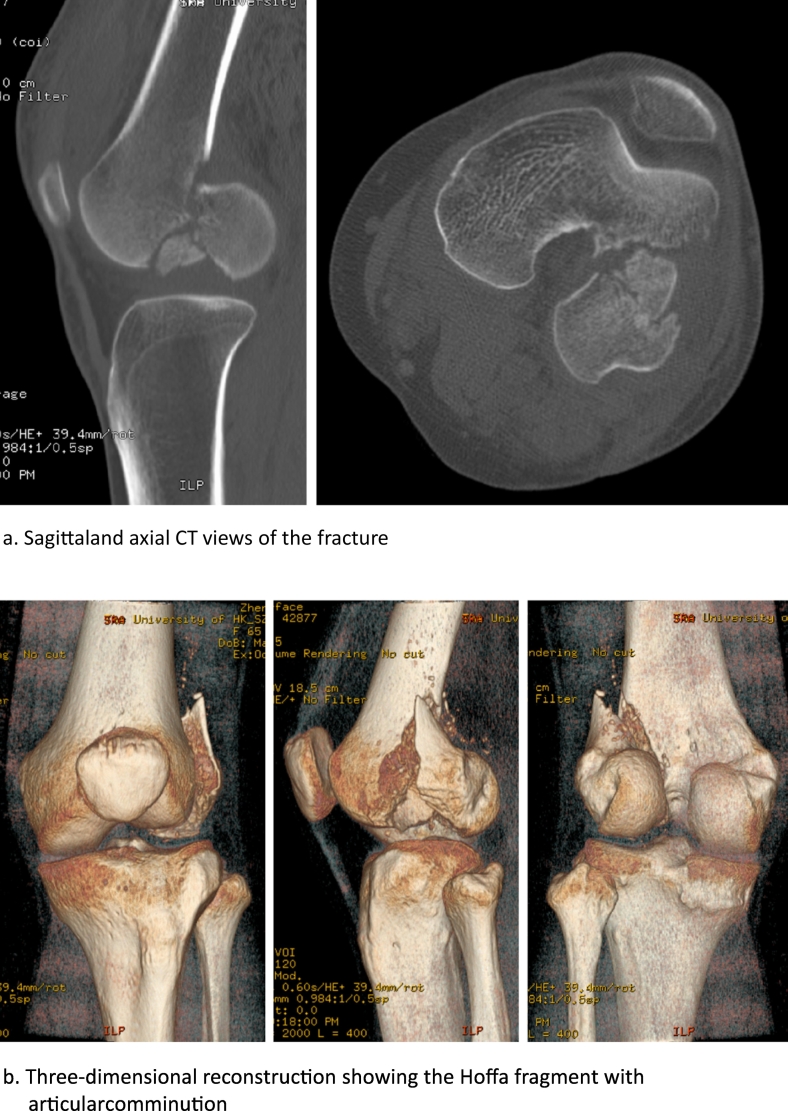
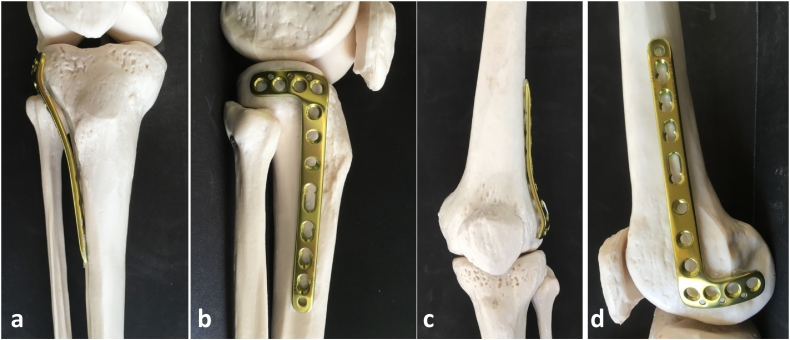
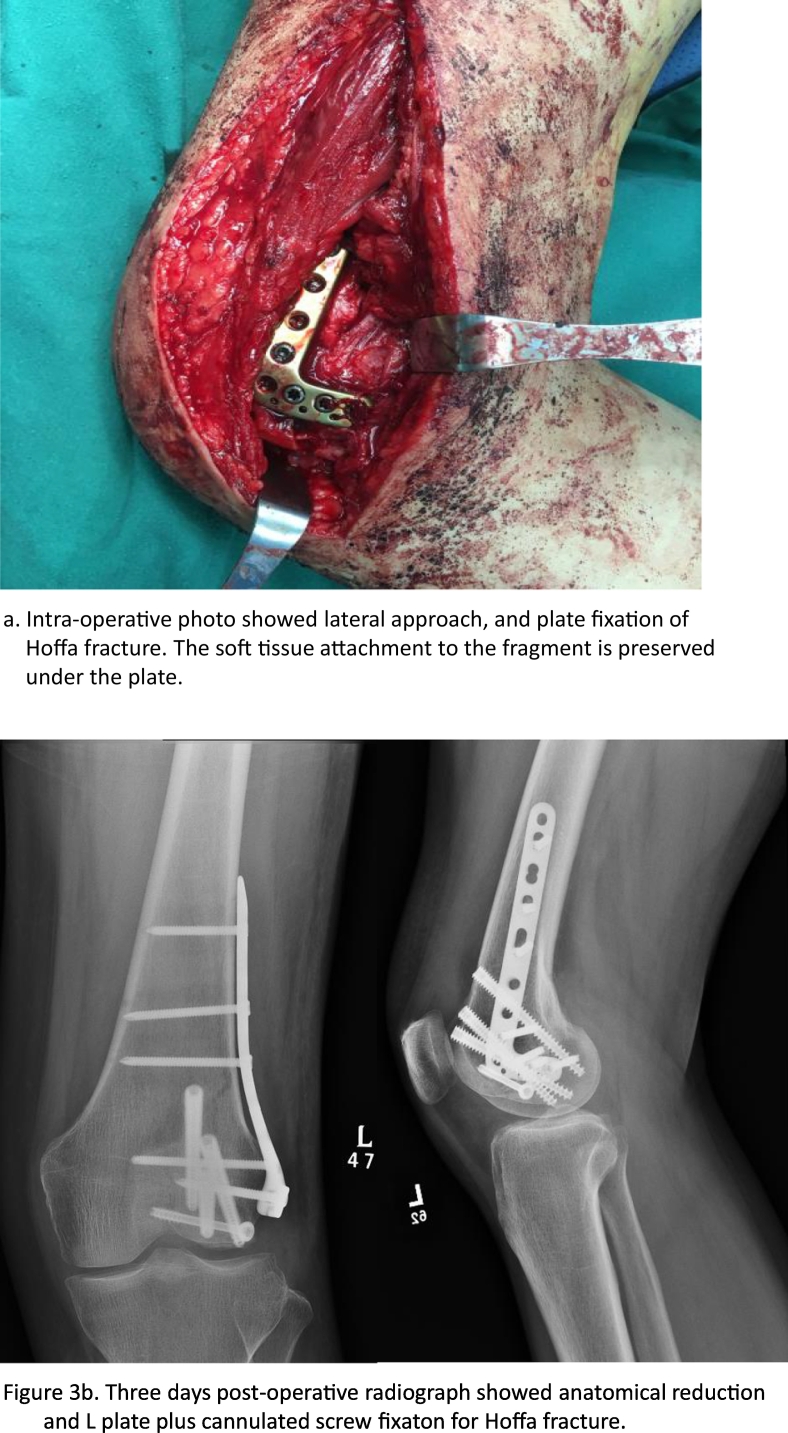
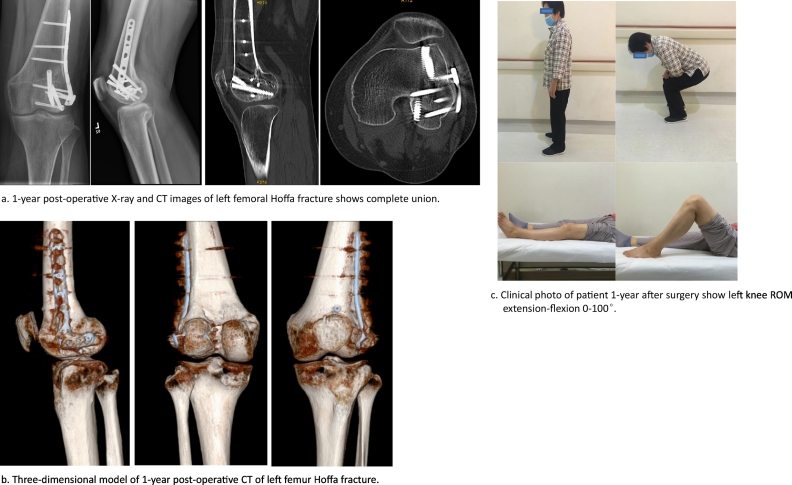
A 65-year-old female suffered from left thigh pain and limited movement for one day after a fall. Radiograph showed left distal femur fracture. After admission, computed tomography showed Hoffa fracture of left distal femur (Fig. 1a&b). Based on the morphology of fracture, L-shaped contralateral proximal tibial plate was optimally chosen and matched well with the distal lateral femur on a 1:1 scale human skeletal model(Fig. 2). She received surgery in lateral recumbent position. The surgery was performed with left lateral sub-vastus approach to expose lateral femoral condyle and epicondyle (Fig. 3a) with the lateral collateral ligament preserved. The two fragments found after exposure were reduced and then fixed with a L-shaped contralateral proximal tibial locking plate without contouring, in combination with three anterior to posterior 5.0 mm headless cannulated differential pitch screws (Fig. 3b). Knee stability was satisfactory from full extension to flexion after fixation. After surgery, the patient received physiotherapy with range of motion exercise encouraged. Full weight bearing walking was allowed at 3 months post-surgery. At one year follow up, she could walk unaided with a slight limp. Her left knee ROM is 0–100°(extension-flexion), and she could squat well (Fig. 4c). The HSS score is 78. CT and X-ray revealed stable fixation and healed fracture (Fig. 4a&b).
Fig. 1.
a. Sagittal and axial CT views of the fracture
b. Three-dimensional reconstruction showing the Hoffa fragment with articular comminution.
Fig. 2.
Pre-operative planning of contralateral proximal tibial plating for Hoffa fracture. a & b: right lateral proximal tibia plate; c & d: left lateral femur condyle.
Fig. 3.
a. Intra-operative photo showed lateral approach, and plate fixation of Hoffa fracture. The soft tissue attachment to the fragment is preserved under the plate.
b. Three days post-operative radiograph showed anatomical reduction and L plate plus cannulated screw fixation for Hoffa fracture.
Fig. 4.
a. 1-year post-operative X-ray and CT images of left femoral Hoffa fracture shows complete union.
b. Three-dimensional model of 1-year post-operative CT of left femur Hoffa fracture.
c. Clinical photo of patient 1-year after surgery show left knee ROM extension-flexion 0–100°.
Discussion
Diagnosis and classification
Hoffa fractures were first described by Busch in 1869 [5]. The Letenneur classification [6] divides Hoffa fractures into three types. In this case, the fracture line is oblique from the base of lateral condyle top to anterior part of distal femur, which is different from either type I or type III Letenneur classification. Another classification [7] based on CT images uses the anatomic femoral axis and a line parallel to the posterior cortex of the femoral condyle to divide the femoral condyle into a, b, and c regions, and the Hoffa fracture in this case fits this CT classification type II bc. A research found that Hoffa fractures occurred more frequently in the lateral femoral condyle [8]. In the axial plane, fractures commonly extended from anterolateral to posteromedial in the lateral condyle. CT shows that Hoffa fracture we presented is a relatively common type among Hoffa fractures.
Surgical technique
Anatomical reduction of the femoral articular surface is crucial to good long-term function. It was reported that lateral approach facilitates the exposure of fracture as well as reduction [9]. Biomechanically, lag screws plus lateral plate fixation provides the highest stiffness and load to failure [10] when compared to screws plus posterior plating or AP placed screws alone. Previous clinical study reported that screw plus lateral plating showed good results at one year follow up [4].
Conventional straight or reconstruction plates only allows limited number of screws for the fixation of the Hoffa fragment [2]. On the other hand, anatomically pre-contoured distal femur plates are designed for a more anterior placement also do not provide sufficient fixation at locations posterior to the lateral epicondyle. While a specially designed Hoffa fragment specific plate is not available, the “L” shape contralateral proximal tibial appears to fit well as demonstrated in this case which does not require pre-bending. The “L” plate allowed three orthogonally oriented locking screws for fixation of posterior fragment in addition to the AP placed lag screw, which ensured sufficient stability. Important for the biology, soft tissue attachments to the Hoffa fragment including the lateral collateral ligament is not detached under the plate. The proximal part of the plate is parallel to the anatomic axis of femur, which can extend to far proximal levels and provide sufficient fixation in cases with metaphyseal fractures.
In conclusion, we successfully demonstrated that the lateral approach plus lateral tibial plateau plate delivers ease of reduction and fixation with good stability to tolerate early mobilization. The technique combined with headless cannulated screw fixation is our preferred method to fix Letenneur type I, type IIa and type III Hoffa fracture.
Acknowledgment
This study is supported by Shenzhen Science and Technology Innovation Committee grant (Project Ref. No. JCYJ20180507182637685) and Shenzhen Municipal Health Commission grant (Project Ref. No. SZXK2020084 & SZSM201612055).
Footnotes
All patients provided the informed consent for the publication of the clinical history. The study was authorized by the local ethical committee and was performed in accordance with the Ethical standards of the 1964 Declaration of Helsinki as revised in 2000.
Contributor Information
Zhao-Hua Liu, Email: liuzh2@hku-szh.org.
Frankie Leung, Email: klleunga@hku.hk.
References
- 1.Patel P.B., Tejwani N.C. The Hoffa fracture: coronal fracture of the femoral condyle a review of literature. J. Orthop. 2018;15(2):726–731. doi: 10.1016/j.jor.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin T. Cannulated lag screw combined with lateral supporting plate for treatment of Hoffa fracture of Letenneur type I and type III. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27(9):1050–1053. [PubMed] [Google Scholar]
- 3.Zhao L.L., Tong P.J., Xiao L.W. Internal fixation with lag screws plus an anti-sliding plate for the treatment of Hoffa fracture of the lateral femoral condyle. Zhongguo Gu Shang. 2016;29(3):266–269. [PubMed] [Google Scholar]
- 4.Lu B. Compression screws and buttress plate versus compression screws only for Hoffa fracture in Chinese patients: a comparative study. J Int Med Res. 2019;47(1):142–151. doi: 10.1177/0300060518798224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartonicek J., Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int. Orthop. 2015;39(6):1245–1250. doi: 10.1007/s00264-015-2730-x. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Y. Hoffa fracture of the femoral condyle: injury mechanism, classification, diagnosis, and treatment. Medicine (Baltimore) 2019;98(8) doi: 10.1097/MD.0000000000014633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xie X. Two and three-dimensional CT mapping of Hoffa fractures. J. Bone Joint Surg. Am. 2017;99(21):1866–1874. doi: 10.2106/JBJS.17.00473. [DOI] [PubMed] [Google Scholar]
- 8.Dhillon M.S. Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literature. Musculoskelet. Surg. 2012;96(1):49–54. doi: 10.1007/s12306-011-0165-0. [DOI] [PubMed] [Google Scholar]
- 9.Orapiriyakul W., Apivatthakakul T., Phornphutkul C. Relationships between Hoffa fragment size and surgical approach selection: a cadaveric study. Arch. Orthop. Trauma Surg. 2018;138(12):1679–1689. doi: 10.1007/s00402-018-3022-x. [DOI] [PubMed] [Google Scholar]
- 10.Schemitsch E.H., Tencer A.F., Henley M.B. Biomechanical evaluation of methods of internal fixation of the distal humerus. J. Orthop. Trauma. 1994;8(6):468–475. [PubMed] [Google Scholar]