Abstract
Objective:
Suicidality is common in clinical trials and health services research, but approaches to suicide risk assessment and mitigation vary widely. Studies involving vulnerable populations with limited access to care raise additional ethical concerns. Here, a community-partnered approach was applied to develop and implement a suicide risk management protocol (SRMP) in a depression study carried out in an under-resourced setting.
Methods:
The SRMP was designed and adapted using a community-partnered participatory research framework. Qualitative data regarding SRMP implementation included notes from SRMP development meetings and from study clinicians conducting outreach calls to study participants. Analyses use baseline, six- and 12-month telephone survey data from 1018 enrolled adults with moderate to severe depressive symptoms (8-item Patient Health Questionnaire score >=10), 87% Black and Latino, in Los Angeles.
Results:
Community stakeholders prioritized a robust SRMP to ensure participant safety. Features included rapid telephone outreach by study clinicians in all cases of reported recent suicidality, and facilitated, expedited access to treatment. Using a suicidality timeframe prompt of “in the past two weeks,” endorsement of suicidality was common (15% baseline, 32% cumulative). Mid-way through the study, the SRMP was modified to assess for present suicidality, which reduced the frequency of clinician involvement. Overall, 318 outreach calls were placed, none requiring emergency response. Treatment referrals were provided in 157 calls. Outreach was well received.
Conclusions:
Implementation of SRMPs in research involving under-resourced communities and other vulnerable populations merit additional considerations. Partnering with community stakeholders can facilitate development of feasible and acceptable SRMP procedures.
Introduction
Suicidality is common, with an estimated 12-month prevalence of 4% in U.S. adults (1), and suicide prevention is a national research priority (2). Although there is growing literature describing interventions to address suicidality in clinical practice, addressing suicidality detected in research study activities, such as participant enrollment and surveys, remains understudied (3).
Both the Food and Drug Administration and the National Institute of Mental Health have issued guidelines for developing study-specific suicide risk management protocols (SRMPs) to address suicidal ideation and behaviors arising during research study operations (4-6). Nonetheless, with the absence of empirically-supported procedures to address suicidality while conducting clinical research, many studies exclude individuals with suicidal thoughts or behavior, citing safety concerns, potential impact on study retention and outcomes, and protection of study participants (3,5-7). In studies where participants with suicidality are not excluded, SRMPs vary widely, from direct outreach by a trained mental health professional in response to every statement of suicidal ideation, to multi-step, automated algorithms with direct clinician evaluation and intervention in only high risk cases (8-12).
Thoughts of suicide are common, but suicide attempts are rare, and suicide risk is difficult to predict with commonly used screening tools (1,13). For example, while a positive screen for suicidality on the nine-item Patient Health Questionnaire (PHQ-9) predicts increased relative risk of attempted suicide, absolute risk remains low (14,15). Challenges in efficient and accurate screening, combined with a need to manage study costs and demands on study staff (11,16,17)—as well as concern for potential impact of suicide interventions on study outcomes (6)—may lead researchers to favor low-intervention SRMPs, particularly in large pragmatic trials.
These practical concerns are weighed against an ethical one: What obligation do clinical researchers have to ensure the safety of study participants expressing suicidality? This question is particularly salient in studies involving low-income, historically marginalized communities—groups underrepresented in clinical research. In such communities, SRMP implementation may be complicated by limited availability of formal mental health services, as well as hesitation of study participants to seek treatment due to stigma surrounding depression and suicidality (18-20). Furthermore, distrust of mental health providers and researchers persists in some communities of color due to a legacy of racism and research abuses such as the Tuskegee Study (21), coupled with negative experiences, including involuntary hospitalization, when seeking treatment (19,22). To our knowledge, the existing literature has not addressed standards for responsible and ethical response to suicidality arising in research in under-resourced, racial and ethnic minority communities.
Here we describe how a community-academic partnership applied a community-partnered participatory research (CPPR) framework to design a unique SRMP for use in the Community Partners in Care (CPIC) depression study, carried out in two under-resourced, predominantly Black and Latino Los Angeles communities (23). A variant of community-based participatory research (24), CPPR emphasizes community-academic co-leadership, co-ownership, and knowledge exchange in all research phases (25,26). We describe the subsequent implementation and adaptation of the SRMP, using data from SRMP workgroup notes and study clinician email summaries of outreach calls to study participants expressing suicidality. We assess the burden of suicidality among research participants at baseline, six- and 12-month follow-up surveys. Finally, we discuss the implications of these findings, and future directions for an ethical approach to addressing suicidality in clinical research involving under-resourced communities.
Methods
Setting
Community Partners in Care was a group-level randomized comparative effectiveness trial designed to compare two depression collaborative care implementation approaches (23). Participants were enrolled from 93 participating programs, including primary care clinics, outpatient mental health clinics, substance outpatient and residential treatment programs, homeless and housing services, social services, and other community-based services (faith-based organizations, hair salons, exercise centers, and park and recreation senior centers), in two Los Angeles communities. Potential participants were screened for eligibility in program waiting rooms and events. Surveys were completed by telephone at baseline, six months, and 12 months from April 2010 through March 2012. The project was approved by the institutional review board (IRB) of RAND and agencies requiring separate review. All participants provided informed consent.
Participants
Study eligibility was limited to adults (≥18 years) speaking English or Spanish, and with at least moderate depressive symptoms indicated by an eight-item Patient Health Questionnaire (PHQ-8 [27]) score ≥10 at screening. The analytic sample includes 1018 enrolled individuals who completed at least one survey (baseline, six months, and/or 12 months). Participant demographics have been previously described (28). Briefly, the study sample was 57% female; 46% Black, 41% Latino, and 9% white; mean age was 46±13 years. Relevant social characteristics include 53% with multiple risk factors for homelessness, 74% meeting federal poverty criteria, 20% working for pay, and 54% uninsured. Additional details on recruitment, enrollment, and outcomes can be found in prior publications (23,28).
Community-Partnered Approach to SRMP Development and Implementation
Employing a CPPR framework (25,26), the CPIC SRMP was developed by a workgroup comprised of academic and community partners, including a community health advocate, a nurse from a local mental health clinic, a Department of Mental Health clinical administrator, a substance abuse agency administrator, a public health nurse, and the director of a safety-net primary care clinic. The workgroup modified the SRMP described in the study grant proposal, based on the prior Partners in Care study (29), during biweekly meetings over the course of four months. The revised SRMP was reviewed at a community forum attended by over 80 local stakeholders, including representatives from community groups, consumer organizations, faith-based organizations, and local health clinics and social services agencies, with subsequent review and approval by the CPIC Executive Committee. The SRMP content and subsequent modifications are described in the Results.
Data Sources
Participants self-reported gender and race/ethnicity at screening. Suicidality screening was conducted by telephone during baseline, six-month, and 12-month surveys. Qualitative data included meeting notes from the SRMP development workgroup, and study clinicians’ emails summarizing contact with study participants endorsing suicidal ideation. Email text was abstracted into Microsoft Excel and included participant study ID; event date; study data collection phase (i.e., screening, baseline, six-, or 12-month survey); study clinician; assessment of imminent risk; intervention, such as referral to a clinic or emergency room, or call to 911; and narrative comments.
Suicidality Screening Measures
Screening for suicidality in the baseline survey utilized the Mini-International Neuropsychiatric Interview (MINI) item: “Over the past two weeks, when you felt depressed or uninterested, did you repeatedly consider hurting yourself, feel suicidal, or wish that you were dead? Did you attempt suicide or plan a suicide?” (30). At six and 12 months, screening utilized the nine-item Patient Health Questionnaire (PHQ-9) item: “In the past two weeks, have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” (31). In the modified SRMP, participants responding affirmatively to the PHQ-9 suicidality item were asked the follow-up question: “Are these thoughts bothering you now?”
Statistical Analysis
A chi-square test of independence was performed to examine the relationship between demographics (race/ethnicity, gender) and cumulative prevalence of suicidal ideation. Analysis was conducted using SAS software.
Qualitative Analysis
Workgroup meeting notes were summarized to describe the process of SRMP development and adaptation. For analysis of outreach call notes, three study team members drafted codes based on both a priori areas of interest (e.g., “problems with access to care” and “referral provided”) and emergent themes (e.g., “knows how to get help”). After several rounds of analysis in which emails were independently coded and reviewed for agreement, a final codebook was developed and applied.
Results
Community-Partnered SRMP Themes
During initial workgroup meetings, several broad themes emerged that guided the SRMP development, adaptation, and implementation. Community partners emphasized the importance of ensuring participant safety over and above IRB requirements, with a high priority placed on suicide prevention. At the same time, community partners were conscious of the stigma of mental illness as well as potential distrust of law enforcement involved with mental health crisis interventions. Both community and academic partners shared concerns about ensuring the feasibility of timely implementation of SRMP procedures, within the constraints of study resources. Finally, the group agreed that an iterative process, using CPPR principles, would be used during study implementation to modify the SRMP, if necessary. Feedback and subsequent modifications are summarized in Table 1.
Table 1.
Community-partnered adaptations to the suicide risk management protocol
| Initial SRMP design | ||
|---|---|---|
| Components of SRMP detailed in study grant |
Community feedback | Partnered solution |
| Completion of outreach calls within 24 hours of initial endorsement of suicidality. | A delayed response may be insufficient for emergent suicidality. | Completion of outreach calls by study clinicians within 30 minutes whenever possible. |
| Study participants with suicidal ideation would receive a list of referrals to local emergency rooms, community mental health clinics, and counseling centers. | Participants may face barriers in accessing care, including fear and stigma; unfamiliarity with how to navigate referral clinics; and challenges getting an expedited appointment in a busy safety-net system. | Written agreements were developed with local mental health and primary care clinics to provide facilitated referrals through a “warm handoff,” with appointments in 1-2 business days. Participants already in treatment were coached on how to discuss suicidal ideation with their current providers. |
| Low threshold for study clinicians to contact 911 or the Los Angeles County Psychiatric Mobile Response Team (PMRT) for further evaluation of suicidality. | Due to historical relationships, study communities may be distrustful of local law enforcement and fearful of the possibility of involuntary detainment or hospitalization. | 911 and/or PMRT would be contacted by study clinicians only if, on detailed assessment, there was concern for imminent threat of self-harm and there were no other reasonable options for ensuring study participant safety. |
| Mid-study SRMP modification | ||
| Original SRMP component |
Research staff feedback | Partnered solution |
| Direct outreach by a study clinician to every participant with a positive suicidality screen on the MINI (at baseline) or PHQ-9 (on six- and 12-month surveys). | Positive suicidality screening was very common, leading to a heavy burden of outreach calls on clinical staff. Despite frequency of suicidality, no participants were assessed by study clinicians to be at imminent risk of self-harm. | To study participants screening positive via the MINI or PHQ-9 suicide item, survey staff posed an additional question: “Are these thoughts bothering you now?” based on the approach initially used by clinicians in their follow-up telephone contacts. Study clinician outreach was limited to participants who responded affirmatively to this “current suicidality” follow-up question. |
SRMP Procedures
The SRMP was activated in response to suicidality endorsed on the MINI or PHQ-9, or volunteered to survey staff. Upon activation, staff immediately paged the on-call study clinician (a licensed physician or psychologist), sharing the participant’s name, telephone number, preferred language, and the reason that the SRMP was activated. Within 30 minutes, the study clinician placed an outreach call to the participant, with ongoing attempts if initially unsuccessful. For Spanish speakers, translation was provided via three-way call. At least one of six study clinicians was on-call during all hours of survey operation, which included evenings and weekends, over a period of 18 months.
Study clinicians received guidelines for follow-up and resources for referrals. If the clinician determined a participant to be at high risk of self-harm, he or she would facilitate a referral to an emergency department or, for imminent risk and as a last resort, call 911. Participants deemed at low immediate risk, and with a current outpatient provider, would be coached on how to discuss suicidality with the provider; if assistance was needed, permission could be obtained for the study clinician to speak to the provider. For participants with no current provider, the study clinician would provide a referral to a partner mental health or primary care agency where the patient would be seen within two business days, with a “warm hand-off” in which study staff would speak directly to a clinic staff member.
Prevalence of Suicidality
Suicidal thoughts were common, endorsed by 32% of study participants at one or more of the three survey time points, and by 15% of participants at baseline, 24% at six-month follow-up, and 20% at twelve-month follow-up (Table 2). Of all participants endorsing suicidal thoughts during the study, 215 (65%) did so at a single time point, 89 (27%) at two time points, and 25 (8%) at all three survey time points. As shown in Table 3, overall prevalence was higher for men than women (37% versus 29%, p=.01); no significant differences were noted by race/ethnicity.
Table 2.
Prevalence of suicidal ideation by survey and screening tool
| Positive SI by MINI/PHQ-9 |
Positive current SIc |
|||||
|---|---|---|---|---|---|---|
| Survey | Suicidality screening tool(s) | N | N | % | N | % |
| Baseline | MINIa | 980 | 144 | 15 | n/a | |
| 6 months | PHQ-9b | 424 | 100 | 24 | n/a | |
| 6 months (modified SRMP) | PHQ-9 + current SI questionb,c | 336 | 79 | 24 | 30 | 9 |
| 12 months (modified SRMP) | PHQ-9 + current SI questionb,c | 733 | 146 | 20 | 44 | 6 |
SI, suicidal ideation
MINI, Mini-International Neuropsychiatric Interview suicidality item: “Over the past two weeks, when you felt depressed or uninterested, did you repeatedly consider hurting yourself, feel suicidal, or wish that you were dead? Did you attempt suicide or plan a suicide?”
PHQ-9, 9-item Patient Health Questionnaire item: “In the past two weeks, have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?”
Under the modified SRMP, participants responding affirmatively to the PHQ-9 suicidality item were asked a follow-up “current SI” question: “Are these thoughts bothering you now?” Prior to addition of the current SI question, positive screening by MINI/PHQ-9 activated the SRMP and led to an outreach call from a study clinician to the individual. Under the modified SRMP, outreach calls were placed only to individuals screening positive and answering the current SI question affirmatively.
Table 3.
Cumulative prevalence of suicidal ideation by race and gender
| Positive SI | ||||
|---|---|---|---|---|
| Group | N | N | % | p |
| Overall | 1018 | 329 | 32 | |
| Race/ethnicity | 0.86 | |||
| Latino | 409 | 136 | 33 | |
| Black | 487 | 153 | 31 | |
| Non-Hispanic white | 86 | 27 | 31 | |
| Other | 35 | 13 | 37 | |
| Gender | 0.01 | |||
| Male | 423 | 155 | 37 | |
| Female | 595 | 174 | 29 | |
SI, suicidal ideation based on PHQ-9 or MINI suicidality screening item
Modification of the SRMP
As the study progressed, it was noted that no participants had been deemed to be at high immediate risk of self-harm on the outreach calls, despite the frequency of SRMP activation; some participants reported passive thoughts of death or hopelessness without intent or plan to act on those thoughts, while others reported current resolution of suicidal thoughts. Midway through the six-month follow-up survey, following discussions involving community partners, research staff, and the RAND IRB, the decision was made to modify the SRMP (Table 1). Subsequently, participants screening positive for recent suicidality on the PHQ-9 (used for six- and 12-month surveys) were asked an additional question to assess current suicidality: “Are these thoughts bothering you now?” Outreach was triggered only when a participant answered this follow-up question affirmatively. Prior to the SRMP modification, this was a key question posed by study clinicians during outreach calls, and its incorporation allowed outreach calls to be limited to assessment of ongoing suicidal ideation, reducing burden on study staff.
Implementation of the SRMP
Of 1018 participants surveyed, study clinician outreach was triggered in 318 instances across 253 unique participants during telephone surveys at three time points (Figure 1). Participants were successfully contacted in 300 instances; all cases were found at low immediate risk of suicide. In 157 outreach calls, participants were provided one or more referrals, which included mental health clinics (N=83), emergency room recommendations for future reference (N=80), and/or a suicide hotline number (N=66). Referrals were either declined or deemed unnecessary (e.g., because the participant was already in treatment) in 137 calls. Study clinicians were unable to reach the participant in 18 cases, six of which were determined to be low immediate risk based on further discussion with the participant’s study survey administrator or outpatient clinician; the 12 remaining cases were coded as lost to follow-up.
Figure 1. Implementation of the CPIC suicide risk management protocol.
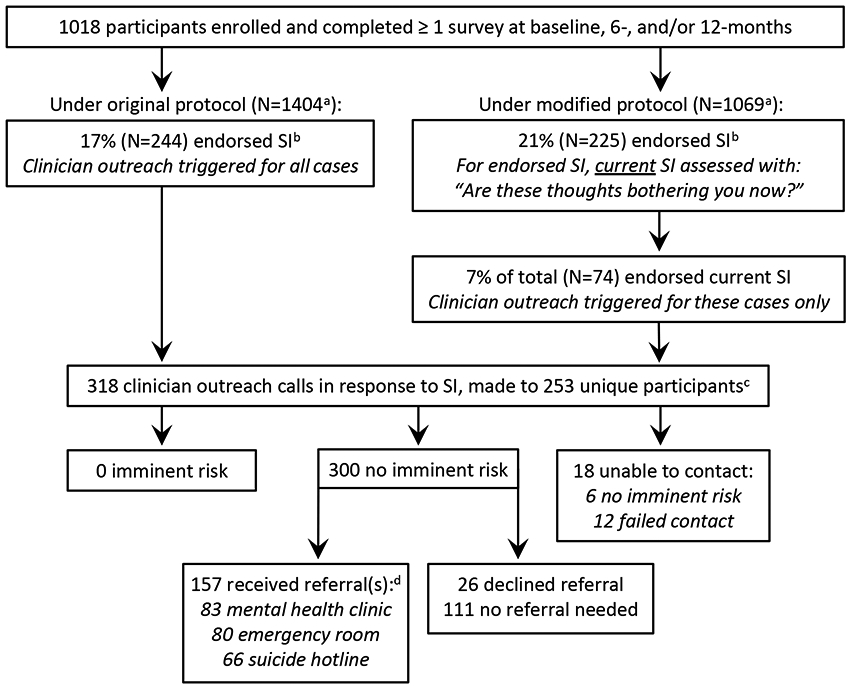
a Includes surveys from multiple time points
b SI, suicidal ideation; assessed with MINI or PHQ-9 under original protocol and PHQ-9 under modified protocol
c Some participants received calls at more than one type point
d Some participants received multiple referrals
As detailed above, the SRMP was modified midway through the study, leading to a higher threshold for study clinician outreach. Under the original protocol, 244 calls were triggered, representing 17% of telephone surveys (N=1404). Under the modified protocol, 74 calls were triggered from 225 initial reports of suicidal ideation, representing 7% and 21% of telephone surveys (N=1069), respectively (Table 2). Outreach frequency did not vary by CPIC study arm (see online supplement).
In the four-year follow-up of the CPIC study, which included intensive tracking of all enrolled participants, as well as review of death records, there were no known suicide deaths. One study participant was hospitalized for a non-fatal suicide attempt three weeks after the baseline survey, at which time he had endorsed suicidal thoughts, received a study clinician outreach call, and was determined to be at low immediate risk of suicide.
Participant Response to Study Clinician Outreach
Key themes identified from study clinician notes included discussion of current stressors, such as personal or family illness; housing, financial, or legal problems; trauma history; and difficulty either obtaining or remaining in mental health treatment. Participants often expressed surprise and appreciation in response to outreach. Quotes from participants included: “This program is wonderful--it should be a national resource for communities like ours”; “I wish this project could be available to everyone in the community”; “You’re the only person who has ever called me just to check on how I’m doing.” Some participants expressed skepticism about treatment: “What would an old person like me do talking to someone about how I feel? I mean, how could it help?” There were no complaints noted about violation of privacy.
Discussion
Exclusion of people of color from clinical research has limited the widespread applicability of findings (18,32). Correction of this pattern is increasingly viewed as a national priority, highlighted by a mandate that NIH-funded studies address inclusion of women and minority groups (33). In our study, community stakeholders made clear that conducting research in Black and Latino communities with limited access to health care and a legacy of negative interactions with the academic and medical establishments requires careful consideration of how to address suicidality ethically and responsibly.
Using a CPPR framework, our community-academic partnership developed an SRMP with significant differences from those in the published literature, grounded in community partners’ emphasis that the protocol go beyond basic risk assessment and mitigation, and actively prevent any study-related suicides. First, the SRMP featured a low threshold for rapid, high-quality outreach, assessment, and brief counseling by a licensed clinician. Although the study was not designed to measure the impact of clinician outreach, the calls themselves may have served as a therapeutic intervention. Second, the SRMP included arrangements with local outpatient clinics to facilitate expedited mental health intake for individuals not currently in treatment. Given that access to appropriate care is a well-established barrier to depression treatment, particularly for Black and Latino individuals (18,34,35), these referrals may have served as an important bridge to treatment.
Outreach calls were well received, but labor intensive, and it was challenging to ensure adequate staffing to respond to the high volume of positive screenings. Thus, midway through the study, the protocol was modified to raise the threshold for study clinician outreach. Similar to findings by Corson et al (36), only about one-third of participants endorsing the PHQ-9 screening item reported ongoing suicidality in the follow-up question (“Are these thoughts bothering you now?”). Given the poor predictive value of many suicide screening items (13), researchers may consider incorporating key follow-up questions into study surveys, as we did in the modified protocol. Our results highlight the tension around how to design an SRMP that reflects a commitment to the safety of the study community, while also being feasible to implement, particularly in large trials such as this one. Academic-community partnerships must weigh these considerations when developing future SRMPs.
The CPIC study was not designed to track suicidality or SRMP implementation, leading to several limitations here. First, clinicians’ emails summarizing outreach calls varied in detail, limiting the depth and precision of analyses. Second, two different suicidality screening tools were employed: the MINI at baseline, and the PHQ-9 in subsequent surveys. Both items address thoughts of self-harm or death, but the MINI includes the word “suicide” (see Methods for full items); this may explain the lower endorsement when using the MINI (15%) than the PHQ-9 (22%). Finally, due to the somewhat non-specific language of the screening items, our results do not provide detailed information on forms of ideation, which may range from thoughts of non-suicidal self-harm, to passive thoughts of death, to a specific suicide plan.
The results of our study reveal a high burden of suicidality among depressed individuals in two low-income, predominantly Black and Latino Los Angeles communities, with 32% of participants endorsing suicidal ideation at one or more time point. Despite researchers’ concerns about community stigma associated with depression and suicidality, study clinician outreach calls were largely welcomed and appreciated. Our data on SRMP implementation were included in an annual report shared with community members and stakeholders, who expressed appreciation for the efforts taken to ensure the safety of potentially vulnerable study participants. We believe that engagement of community stakeholders in SRMP development facilitated the high degree of acceptability of SRMP procedures by study participants and the broader community.
Conclusions
This work adds to the limited literature on development of SRMPs for clinical and services research, and is, to our knowledge, the first to address the particular implications of SRMPs in under-resourced communities. Further research is necessary to determine the impact of interventions related to suicidality in research studies, and whether similar protocols could be implemented as part of community services in response to suicidality, beyond the context of research study operations. We argue that government agencies, funders, and investigators have an obligation to assess the feasibility and effectiveness of efforts to address suicidality emerging in research studies, particularly in research involving under-resourced communities.
Supplementary Material
Highlights:
A community-partnered participatory research framework was applied to develop and implement a suicide risk management protocol (SRMP) for use in a depression study carried out in an under-resourced urban setting.
Community stakeholders prioritized participant safety, leading to unique protocol features such as rapid telephone outreach by study clinicians in all cases of endorsement of suicidality, and facilitated, expedited access to mental health treatment.
Suicidality was endorsed by nearly a third of all study participants at one or more survey time point.
Outreach by study clinicians was labor intensive but well received.
Acknowledgments
This study was supported by the Patient-Centered Outcomes Research Institute contract 1845; the National Institute on Minority Health and Health Disparities grant 1R01MD007721; the National Institute of Mental Health grants 01MH078853, P30MH082760, and P30MH068639; the California Community Foundation grant CMCH-12-97088; the National Center for Advancing Translational Sciences Clinical and Translational Science Institute grant UL1TR001881; and the Robert Wood Johnson Foundation grant 64244, and the National Library of Medicine grant G08LM011058.
Footnotes
The authors report no conflicts of interest. Dr. Goodsmith was supported by the VA Office of Academic Affiliations through the UCLA National Clinician Scholars Program. The contents do not represent the views of the U.S. Department of Veterans Affairs, the United States Government, or affiliated institutions.
This work has not been presented elsewhere.
References
- 1.Piscopo K, Lipari RN, Cooney J, et al. : Suicidal Thoughts and Behavior among Adults: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review, 2016 [Google Scholar]
- 2.2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention. Washington, DC, US Department of Health & Human Services, 2012 [PubMed] [Google Scholar]
- 3.Iltis AS, Misra S, Dunn LB, et al. : Addressing risks to advance mental health research. JAMA Psychiatry 70: 1363–1371, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guidance for Industry: Suicidal Ideation and Behavior: Prospective Assessment of Occurrence in Clinical Trials. Silver Spring, MD, Office of Medical Products and Tobacco, Center for Drug Evaluation and Research, 2012 [Google Scholar]
- 5.Fisher CB, Pearson JL, Kim S, et al. : Ethical issues in including suicidal individuals in clinical research. IRB 24: 9–14, 2002 [PubMed] [Google Scholar]
- 6.Pearson JL, Stanley B, King CA, et al. : Intervention research with persons at high risk for suicidality: safety and ethical considerations. J Clin Psychiatry 62 Suppl 25: 17–26, 2001 [PubMed] [Google Scholar]
- 7.Oquendo MA, Stanley B, Ellis SP, et al. : Protection of human subjects in intervention research for suicidal behavior. Am J Psychiatry 161: 1558–1563, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Campbell DG, Bonner LM, Bolkan CR, et al. : Suicide risk management: development and analysis of a telephone-based approach to patient safety. Transl Behav Med 1: 372–383, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langhinrichsen-Rohling J, Snarr JD, Slep AMS, et al. : Risk for suicidal ideation in the U.S. Air Force: an ecological perspective. J Consult Clin Psychol 79: 600–612, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Nierenberg AA, Trivedi MH, Ritz L, et al. : Suicide risk management for the sequenced treatment alternatives to relieve depression study: applied NIMH guidelines. J Psychiatr Res 38: 583–589, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Vannoy S, Whiteside U, Unützer J: Current practices of suicide risk management protocols in research. Crisis 31: 7–11, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson CM, Christensen BK: Ethical issues relevant to the assessment of suicide risk in nonclinical research settings. Crisis 33: 54–59, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Gaynes BN, West SL, Ford CA, et al. : Screening for Suicide Risk in Adults: A Summary of the Evidence for the U.S. Preventive Services Task Force. Ann Intern Med 140: 822–835, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Simon GE, Rutter CM, Peterson D, et al. : Does Response on the PHQ-9 Depression Questionnaire Predict Subsequent Suicide Attempt or Suicide Death? Psychiatr Serv 64: 1195–1202, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Louzon SA, Bossarte R, McCarthy JF, et al. : Does Suicidal Ideation as Measured by the PHQ-9 Predict Suicide Among VA Patients? Psychiatr Serv Wash DC 67: 517–522, 2016 [DOI] [PubMed] [Google Scholar]
- 16.Palinkas LA, Zatzick D: Rapid Assessment Procedure Informed Clinical Ethnography (RAPICE) in Pragmatic Clinical Trials of Mental Health Services Implementation: Methods and Applied Case Study. Adm Policy Ment Health 46: 255–270, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Califf RM, Sugarman J: Exploring the ethical and regulatory issues in pragmatic clinical trials. Clin Trials J Soc Clin Trials 12: 436–441, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office of the Surgeon General, Center for Mental Health Services, National Institute of Mental Health: Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2001 [PubMed] [Google Scholar]
- 19.Meinert JA, Blehar MC, Peindl KS, et al. : Bridging the gap: recruitment of African-American women into mental health research studies. Acad Psychiatry 27: 21–28, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Wexler L, Chandler M, Gone JP, et al. : Advancing suicide prevention research with rural American Indian and Alaska Native populations. Am J Public Health 105: 891–899, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gamble VN: Under the shadow of Tuskegee: African Americans and health care. Am J Public Health 87: 1773–1778, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George S, Duran N, Norris K: A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health 104: e16–31, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung B, Jones L, Dixon EL, et al. : Using a community partnered participatory research approach to implement a randomized controlled trial: planning community partners in care. J Health Care Poor Underserved 21: 780–795, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallerstein N, Duran B, Oetzel JG, et al. (eds): Community-based participatory research for health: advancing social and health equity, Third edition. San Francisco, CA, Jossey-Bass, 2018 [Google Scholar]
- 25.Jones L, Meade B, Forge N, et al. : Begin your partnership: the process of engagement. Ethn Dis 19: S6-8–16, 2009 [PMC free article] [PubMed] [Google Scholar]
- 26.Jones L, Wells K: Strategies for academic and clinician engagement in community-participatory partnered research. JAMA 297: 407–410, 2007 [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Strine TW, Spitzer RL, et al. : The PHQ-8 as a measure of current depression in the general population. J Affect Disord 114: 163–173, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Wells KB, Jones L, Chung B, et al. : Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med 28: 1268–1278, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells KB, Sherbourne C, Schoenbaum M, et al. : Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 283: 212–220, 2000 [DOI] [PubMed] [Google Scholar]
- 30.Sheehan DV, Lecrubier Y, Sheehan KH, et al. : The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59 Suppl 20: 22–33, 1998 [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16: 606–613, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oh SS, Galanter J, Thakur N, et al. : Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled. PLOS Med 12: e1001918, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.NIH Policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research. NOT-OD-02-001. National Institutes of Health, 2001 [Google Scholar]
- 34.McGuire TG, Miranda J: New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff 27: 393–403, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Young AS, Klap R, Sherbourne CD, et al. : The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry 58: 55–61, 2001 [DOI] [PubMed] [Google Scholar]
- 36.Corson K, Gerrity MS, Dobscha SK: Screening for depression and suicidality in a VA primary care setting: 2 items are better than 1 item. Am J Manag Care 10: 839–845, 2004 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


