Abstract
Polyarteritis nodosa (PAN) is a rare vasculitis that can cause peripheral ischemia. We present the case of a 49-year-old man who developed PAN causing toe gangrene and severe rest pain in one foot and claudication of the contralateral foot. He was treated with immunosuppression and underwent popliteal-plantar artery bypass with resolution of rest pain and subsequent amputation of his mummified toe. Despite remission of PAN, his contralateral foot claudication was lifestyle limiting; thus, 5 years later he underwent contralateral popliteal-plantar bypass with resolution of claudication. This case demonstrates the anatomically symmetric presentation of PAN induced ischemia with successful open revascularization after resolution of inflammatory markers with systemic therapy.
Keywords: Polyarteritis nodosa, Vasculitis, Chronic limb-threatening ischemia, Intermittent claudication, Peripheral bypass
Polyarteritis nodosa (PAN) is a necrotizing medium vessel vasculitis which causes stenosis, thrombosis, and microaneurysms.1 PAN characteristically affects people in their 40s to 60s with a male predominance2 and involves visceral vessels, however there are case reports of peripheral vascular involvement.3, 4, 5, 6, 7, 8, 9 Criteria for diagnosis of PAN include three or more of the following symptoms or signs: weight loss of ≥4 kg since illness began; livedo reticularis; testicular pain or tenderness; myalgias, weakness, or leg tenderness; mononeuropathy or polyneuropathy; diastolic blood pressure >90 mm Hg; elevated blood urea nitrogen >40 mg/dL or creatinine >1.5 mg/dL; hepatitis B virus; arteriogram showing aneurysms or occlusions of visceral arteries; and biopsy of a small- or medium-sized artery containing neutrophils, granulocytes, or mononuclear leukocytes in the artery wall.10 This case of PAN caused critical limb-threatening ischemia with digital gangrene and contralateral intermittent claudication, and was successfully treated with bilateral revascularization by popliteal-plantar bypass. The patient consented to publication of the details and images included in this report.
Case report
The patient was a 49-year-old man who had been healthy until he presented to an outside institution with 1 month of malaise, low-grade fever, weight loss, new-onset chest pain, and hypertension. He had quit smoking cigarettes about 15 years before presentation; he had smoked two packs per day for 15 years before cessation. He had no other contributing medical or social history. He had an elevated troponin level and underwent a cardiac catheterization, which demonstrated minimal coronary disease. After an extensive evaluation that revealed elevated inflammatory markers, multifocal scarring of bilateral kidneys with mildly elevated creatinine, right foot short distance claudication, early left first toe gangrene, left foot rest pain, and a testicular infarct, he was ultimately diagnosed with PAN. He was initially treated with prednisone, required the addition of oral cyclophosphamide, and transitioned to intravenous cyclophosphamide owing to intolerance of oral dosing. Over the ensuing 4 months, his constitutional symptoms improved and his inflammatory markers returned to normal. He transitioned to oral azathioprine for maintenance remission therapy.
Early in his disease course, he was seen by vascular surgery at an outside institution for his peripheral vascular complaints. His left first toe pressure was unmeasurable. Angiography revealed normal vessels to the proximal calf with occlusion of all three left tibial arteries and reconstitution of the medial plantar artery (Fig 1). As his erythrocyte sedimentation rate and C-reactive protein normalized with treatment, although his constitutional symptoms improved, his left foot rest pain continued to be severe with further progression of dry gangrene. He was referred to the authors' institution for revascularization. Approximately 6 months after his symptoms began and 2 months after stabilization of his inflammatory markers, he underwent an uneventful left below-knee popliteal to plantar artery bypass using the ipsilateral greater saphenous vein. He was observed overnight for pain management and discharged on postoperative day 1. He healed without issue, his rest pain resolved, and he underwent a partial left first toe amputation several months later after his dry gangrene fully demarcated. Over the ensuing 5 years, he was seen regularly for surveillance of his bypass with his most recent left ankle-brachial index normal at 1.1.
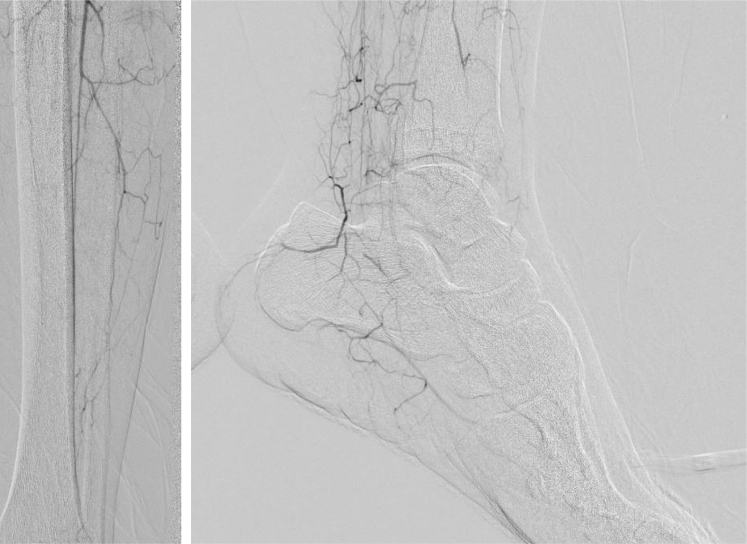
Fig 1.
Left lower extremity angiography revealing occlusion of left tibial arteries and reconstitution of the medial plantar artery.
At each follow-up visit, he continued to complain of cramping in his right foot when he walked more than 75 feet, with an ankle-brachial index of 0.8 and toe pressure of 72 mm Hg. He maintained a walking program; however, this claudication remained lifestyle limiting. For example, he found it quite frustrating and bothersome that he had to take multiple breaks for the foot pain and cramping to resolve while trying to mow his lawn. During this time, his PAN was controlled with stable renal function and no constitutional symptoms. With his right foot claudication symptoms unimproved despite maximal conservative measures, he consented to a right lower extremity angiogram, which confirmed tibial artery disease in a pattern similar to his previously treated left-sided disease (Fig 2). He subsequently underwent a right below-knee popliteal to plantar artery bypass using cephalic vein, as the right greater saphenous vein was sclerotic. Again, he was observed overnight and recovered uneventfully. Seven months postoperatively, he is able to walk unlimited distance with no claudication with an ankle-brachial index of 1.3 and a normal bypass by duplex imaging (Fig 3).
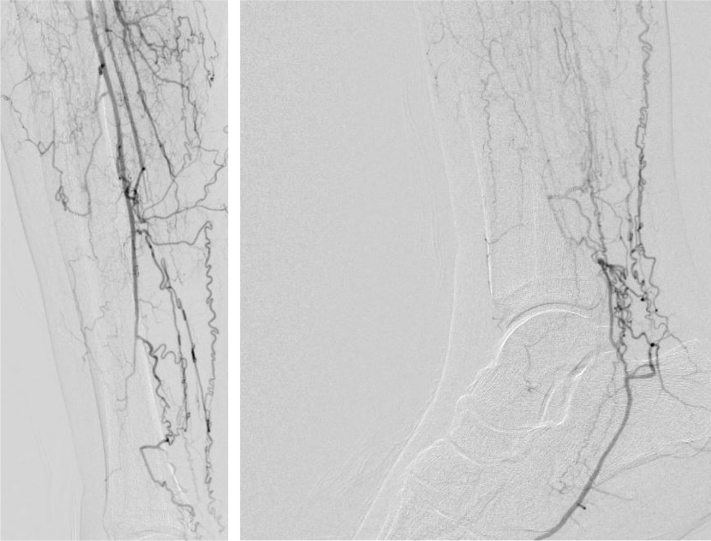
Fig 2.
Right lower extremity angiography revealing occlusion of right tibial arteries and reconstitution of the medial plantar artery.
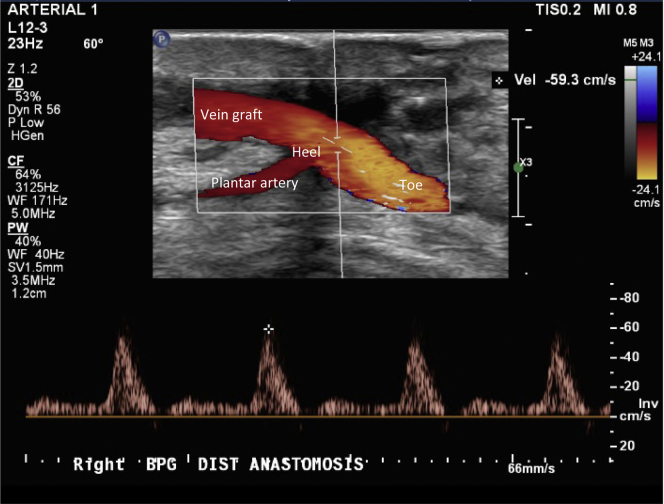
Fig 3.
Duplex imaging of distal anastomosis of right popliteal to plantar artery bypass graft.
Discussion
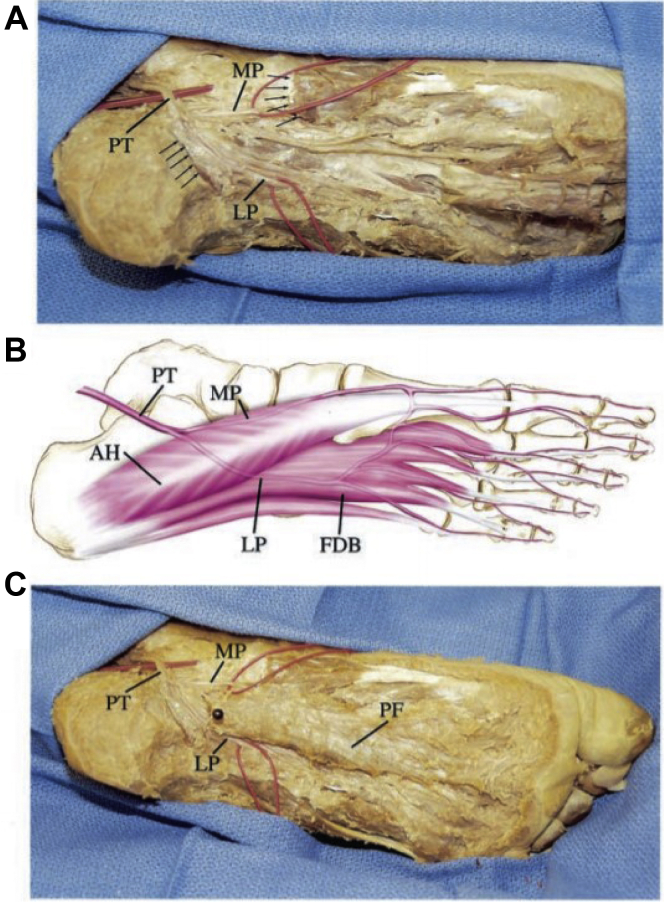
This 49-year-old man developed critical limb-threatening ischemia of his left foot with digital gangrene and intermittent claudication of his right foot as manifestations of PAN. Alongside aggressive medical management of his PAN, both lower extremities were successfully treated with popliteal-plantar bypasses. Beyond the less common exposure of the plantar artery (Fig 4),11 this patient and his treatment must be considered in the context of published reports of peripheral vascular manifestations of PAN (Table).
Fig 4.
Exposure of the medial and lateral plantar arteries. (A) Photograph of cadaver dissection. Plantar fascia and flexor digitorum brevis have been retracted. The posterior tibial (PT) artery has been exposed, identifying its branches with vessel loops placed around lateral plantar (LP) and medial plantar (MP) arteries. Segment of abductor hallucis muscle has been excised (arrows). (B) The course of the PT, LP, and MP arteries in relationship to flexor digitorum brevis (FDB) and abductor hallucis (AH) muscles. (C) Photograph of a cadaver foot shows flexor digitorum brevis muscle (not seen) and plantar fascia (PF) overlying the MP and LP arteries.
From Thornton et al., “Pseudoaneurysm of the lateral plantar artery after foot laceration, J Vasc Surg, 2003.
Table.
Review of case presentations of vascular disease in polyarteritis nodosa (PAN)
| Authors | Case description |
|---|---|
| De Golovine et al3 | A 38-year-old man with claudication found to have bilateral femoral artery stenosis who underwent aortobifemoral bypass, who presented 1 year later with temporal arteritis and mesenteric ischemia that did not respond to corticosteroids and cyclophosphamide. The patient died of mesenteric ischemia and sepsis. |
| Fred et al4 | A 47-year-old man with a 1-month history of arthralgias who presented with abrupt onset of abdominal pain and diarrhea, and had rapid progression of symmetric distal finger and toe gangrene. He was treated with prednisone and cyclophosphamide and underwent amputation of mummified digits. Four months later, he died of a cerebellar hemorrhage. |
| Ninomiya et al5 | A 62-year-old man with history of Raynaud phenomenon who presented with symmetric dry gangrene of the fingertips and toes despite normal peripheral pulses. His peripheral cyanosis and gangrene stopped progressing with corticosteroids and azathioprine. |
| Buhl et al6 | A 42-year-old man with acute myeloid leukemia with bilateral foot ischemia that rapidly progressed despite systemic therapy, ultimately requiring bilateral lower extremity amputation. |
| Venturini et al7 | A 73-year-old man with PAN diagnosed 3 years prior, who presented with a 5-cm ischemic ulcer of the dorsum of the foot with rest pain. Angiography showed occlusion of the posterior tibial artery and multiple stenoses of the anterior tibial artery and peroneal artery. Angioplasty of the anterior tibial artery was performed and a 2.5-mm coronary drug-eluting stent was placed in the pedal artery. The patient's rest pain resolved and the ulcer healed within 3 months. |
| Obara et al8 | A 65-year-old woman who had an ischemic leg ulcer treated with angioplasty of the posterior tibial artery, which healed after the intervention. |
| Fonseka et al9 | A 60-year-old man who presented with rapidly progressive right leg claudication, who was treated with corticosteroids and cyclophosphamide and found to have right iliofemoral artery stenosis, managed with right iliofemoral bypass with resolution of pain. |
| Héron et al12 | A 33-year-old woman who presented with acute limb ischemia of her right foot, with imaging showing renal microaneurysms, numerous lower extremity microaneurysms, and occlusion of the tibial and peroneal arteries of the right leg. She was treated with corticosteroids and anticoagulation with slow improvement of her rest pain to claudication at 6 months, and resolution of claudication by 1 year after presentation. |
| Osada et al13 | A 58-year-old woman with leg ulcerations diagnosed as cutaneous PAN who had new onset of left foot claudication which progressed to rest pain, and was found to have left anterior tibial artery occlusion 40 mm in length and posterior tibial artery stenosis. She underwent angioplasty of the anterior tibial artery with resolution of her rest pain. |
There are several reports of rapidly progressive ischemic presentations of PAN. Buhl et al6 reported the case of a 42-year-old patient with acute myeloid leukemia who developed PAN with bilateral lower extremity gangrene with no attempt at revascularization before bilateral lower extremity amputation owing to rapid progression of symptoms despite systemic therapy including high-dose corticosteroids, cyclophosphamide, and plasmapheresis. There are two reports of patients presenting with symmetric digital gangrene of both upper and lower extremities owing to PAN without revascularization attempt.4,5 The case reported here similarly had quite symmetric disease of his lower extremities. Héron et al12 reported a case of a 33-year-old patient with PAN who developed acute limb ischemia with foot parasthesias and rest pain owing to tibial occlusion which was managed with anticoagulation. This patient had slow improvement of her symptoms over the course of a year.12
In the case reported here, the patient was lucky to have had early diagnosis of his PAN, allowing aggressive systemic treatment and improvement in his constitutional symptoms and inflammatory markers before he underwent operative revascularization. He did require a partial toe amputation, but the timeline of his diagnosis and initial PAN treatment did not preclude limb salvage, as in the cited cases. Other groups have also reported successful revascularization for PAN induced peripheral ischemia. There are several reports of successful healing of cutaneous ulcers through endovascular interventions7,8,13 and a report of a successful bypass for a patient with an iliofemoral stenosis from PAN causing progressive claudication.9 The patient reported here similarly has done well in the 5 years since his initial popliteal-plantar bypass. This limited literature suggests that, alongside systemic medical therapy, open or endovascular revascularization is appropriate for PAN induced ischemia.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal Policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Jennette J.C., Falk R.J., Bacon P.A., Basu N., Cid M.C., Ferrario F. 2012 revised International Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum. 2013;65:1–11. doi: 10.1002/art.37715. [DOI] [PubMed] [Google Scholar]
- 2.Forbess L., Bannykh S. Polyarteritis nodosa. Rheum Dis Clin North Am. 2015;41:33–46. doi: 10.1016/j.rdc.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 3.De Golovine S., Parikh S., Lu L. A case of polyarteritis nodosa presenting initially as peripheral vascular disease. J Gen Intern Med. 2008;23:1528–1531. doi: 10.1007/s11606-008-0683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fred H.L., Serna J.H., McDonald G.A., Ahmed S.S. Polyarteritis nodosa inducing symmetric peripheral gangrene. Circulation. 2003;107:2870. doi: 10.1161/01.CIR.0000068032.38990.85. [DOI] [PubMed] [Google Scholar]
- 5.Ninomiya T., Sugimoto T., Tanaka Y., Aoyama M., Sakaguchi M., Uzu T. Symmetric peripheral gangrene as an emerging manifestation of polyarteritis nodosa. J Rheumatol. 2007;34:440–441. [PubMed] [Google Scholar]
- 6.Buhl T., Bertsch H.P., Raab B.-W., Kaune K.M., Vasko R., Strutz F. Fulminant polyarteritis nodosa associated with acute myeloid leukaemia resulted in bilateral lower leg amputation. Rheumatology (Oxford) 2009;48:1170–1172. doi: 10.1093/rheumatology/kep173. [DOI] [PubMed] [Google Scholar]
- 7.Venturini M., Orsi M., Colombo M., Querques G., Agostini G., Bozzolo E. Drug-eluting stent patency at 6 months in the pedal artery of a patient with polyarteritis nodosa: a case report. J Vasc Interv Radiol. 2013;24:907–910. doi: 10.1016/j.jvir.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 8.Obara H., Matsubara K., Fujimura N., Sekimoto Y., Kitagawa Y. Preliminary report of endovascular treatment for critical limb ischemia patients with connective tissue disease: cases series and review of the literature. Int J Angiol. 2014;24:137–142. doi: 10.1055/s-0035-1547516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fonseka C.L., Galappaththi S.R., Abeyaratne D., Tissera N., Wijayaratne L. A case of polyarteritis nodosa presenting as rapidly progressing intermittent claudication of right leg. Case Rep Med. 2017;2017:4219718. doi: 10.1155/2017/4219718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fries J.F., Hunder G.G., Bloch D.A., Michel B.A., Arend W.P., Calabrese L.H. The American College of Rheumatology 1990 criteria for the classification of vasculitis: summary. Arthritis Rheum. 1990;33:1135–1136. doi: 10.1002/art.1780330812. [DOI] [PubMed] [Google Scholar]
- 11.Thornton B.P., Minion D.J., Quick R., Vasconez H.C., Endean E.D. Pseudoaneurysm of the lateral plantar artery after foot laceration. J Vasc Surg. 2003;37:672–675. doi: 10.1067/mva.2003.31. [DOI] [PubMed] [Google Scholar]
- 12.Héron E., Fiessinger J.-N., Guillevin L. Polyarteritis nodosa presenting as acute leg ischemia. J Rheumatol. 2003;30:1344–1346. [PubMed] [Google Scholar]
- 13.Osada S.I., Akiyama M., Takasaki M., Takagawa S., Nakazawa K., Murata S. Revascularization by percutaneous transluminal angioplasty improved abruptly deteriorated ischaemic symptoms in cutaneous polyarteritis nodosa. Clin Exp Dermatol. 2011;36:502–505. doi: 10.1111/j.1365-2230.2011.04050.x. [DOI] [PubMed] [Google Scholar]