Abstract
Robert's uterus is a rare Müllerian malformation first characterized by a French gynecologist Héléne Robert in 1969. It represents an asymmetric division of the uterine cavity. A 45-year-old female patient presented with vaginal bleeding and vague abdominal pain for the course of 20 days, with a blood human chorionic gonadotropin level of 10331.00 mIU/mL, and a gestational sac in the right uterine horn without a fetal heart beat revealed by the ultrasound. Ectopic pregnancy in the right uterine horn seemed to be the most likely diagnosis. Laparoscopic and hysteroscopic attempts to terminate the pregnancy failed. A pelvic magnetic resonance imaging (MRI) performed after the surgery demonstrated Robert's uterus with pregnancy in the blind hemicavity. When a pregnancy sac has been revealed by an ultrasound but nothing has been found by a hysteroscopy, a possibility of uterine malformation should be considered. Radiologists and gynecologists should consider the application of MRI for diagnosis of congenital Müllerian uterine anomalies.
Keywords: Müllerian malformation, Robert's uterus, Septate uterus
Abbreviations: MRI, magnetic resonance imaging; CT, computed tomography; ASRM, American Society for Reproductive Medicine
Introduction
Robert's uterus is a rare Müllerian malformation, first characterized by a French gynecologist Héléne Robert in 1969 [1]. It represents an asymmetric division of the uterine cavity [2], [3], [4]. Structural malformations are associated with abnormal fetal presentation, preterm labor, recurrent pregnancy loss, and infertility [5,6]. Only a few cases of pregnancy in the blind hemicavity have been reported so far. We report the first case of this rare event in Xinjiang Uygur Autonomous Region, China due to a failed attempt to terminate an ectopic pregnancy to aide radiologists and gynecologists to avoid inappropriate diagnosis and management of this condition.
Case report
A 45-year-old patient presented with mild vaginal bleeding and vague abdominal pain for the course of 20 days. Her left fallopian tube and ovary were surgically removed by surgery for an ectopic pregnancy 24 years ago. She had given birth to 2 children via natural labor after the surgery. Her previous menstruation cycle was normal without complaint of dysmenorrhea.
The patient provided informed consent for the publication of this case.
Gynecological examination revealed mild vaginal bleeding without obvious abnormalities. Her blood human chorionic gonadotropin level was 10331.00 mIU/mL. Ultrasound examination revealed gestational sac in the right rudimentary horn (30 × 30 × 20 mm). Fetal heart beat was absent. Multiple uterine fibroids and adenomyosis of the uterus were also considered. The left adnexa was absent, while the right one was normal. Ectopic pregnancy in the right uterine horn was declared as a provisional diagnosis. Laparoscopy and hysteroscopy were performed to induce abortion.
Laparoscopy revealed that the uterus was asymmetrically enlarged for 7 weeks of gestation especially on the right side. Induced abortion was attempted using laparoscopic and hysteroscopic guidance but failed due to failure to locate the gestational sac in the uterus (Fig. 1). The operation was terminated, and a pelvic MRI was performed after the surgery for further inspection.
Fig 1.
Hysteroscopy failed to locate gestational sac in the uterus.
After evaluation using pelvic MRI, the patient received a diagnosis of Robert's uterus. The uterine cavity was divided into a blind hemicavity in the right posterior side and a hemicavity connected to the cervix in the left anterior side by an asymmetric septum. The septum was partially complete with a defect of 5 × 5 mm in the upper third. A gestational sac was observed in the blind hemi-cavity. T2-hyposignal within suggested old bleeding. Uterine adenomyosis and fibroids were present as well (Figs. 2–5). The left adnexa were absent. Hysterectomy and right salpingectomy confirmed the MRI findings.
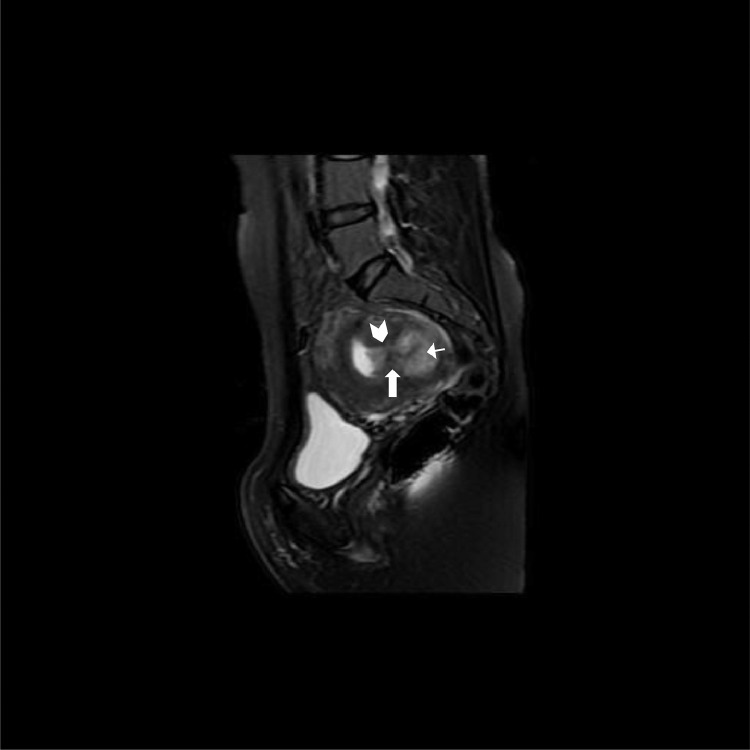
Fig 3.
Sagittal MRI shows partially complete septum (arrow) with a 5 × 5 mm defect (arrow head). Pregnancy in posterior blind hemicavity (short arrow).
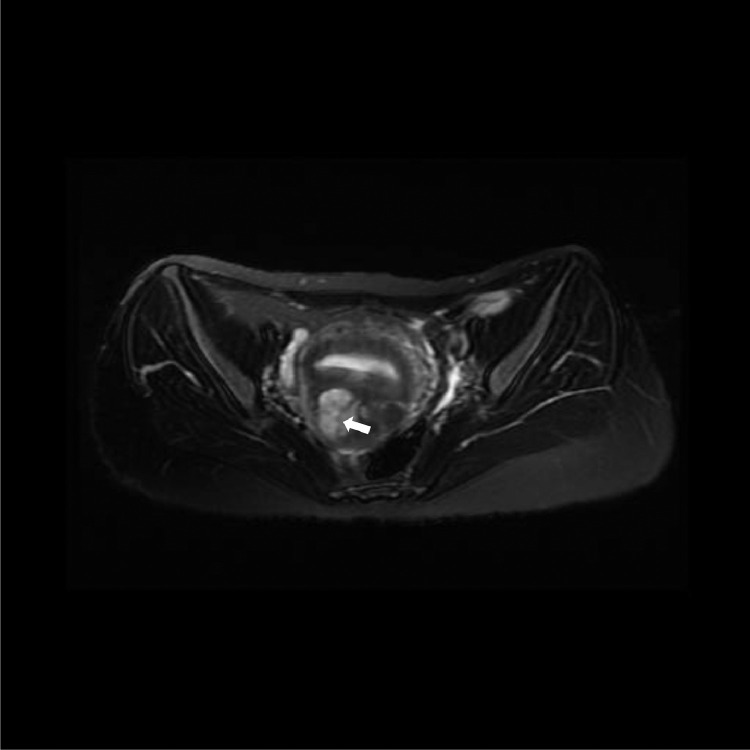
Fig 4.
T2-hyposignal suggests old bleeding in the gestational sac (arrow).
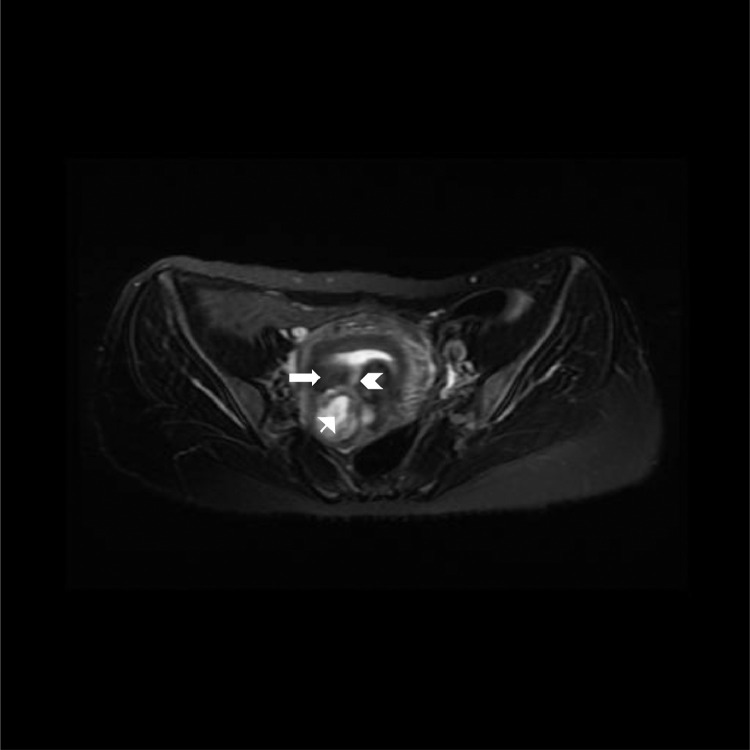
Fig 2.
Partially complete septum (arrow) with a 5 × 5 mm defect (arrow head) divides the uterine cavity into two parts. Pregnancy in the posterior blind hemicavity (short arrow).
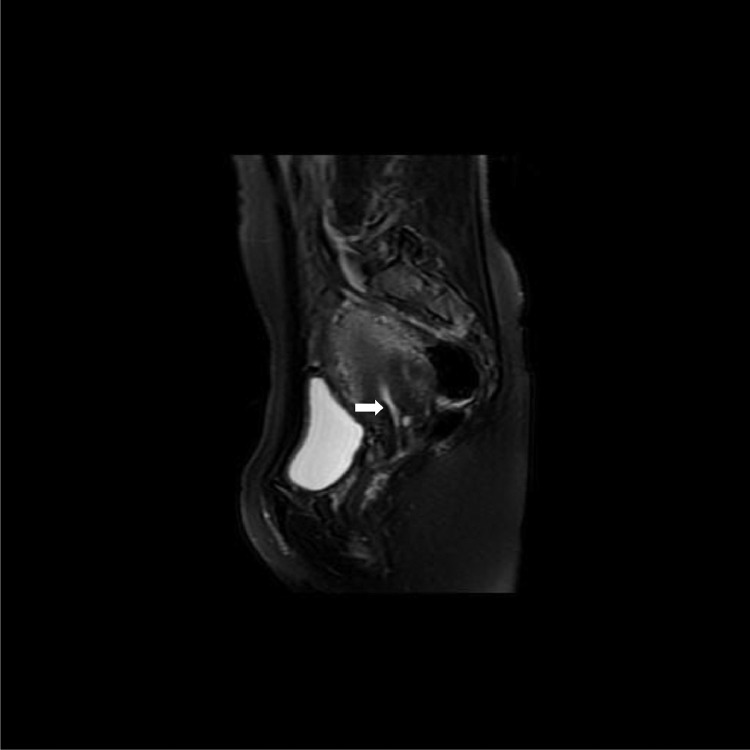
Fig 5.
Hemicavity in the left anterior side of the uterus connects the cervix (arrow).
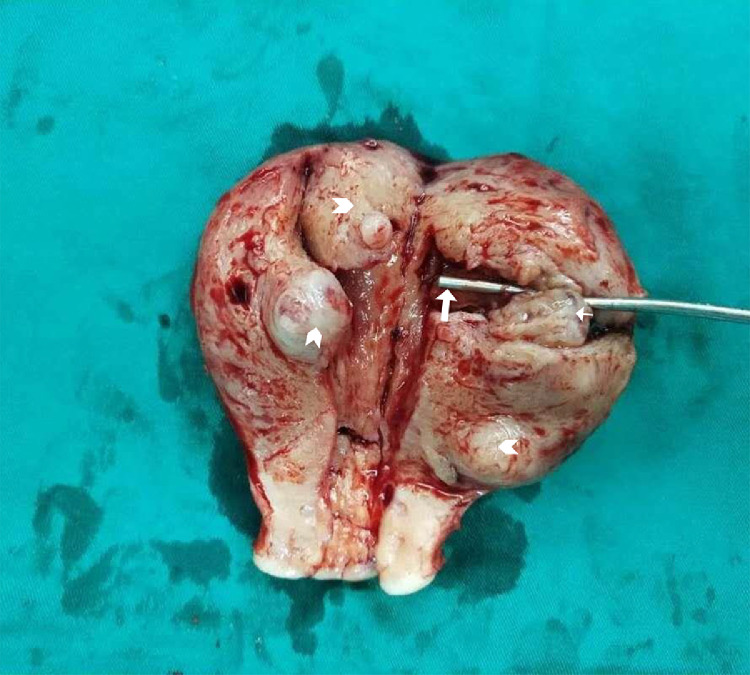
Pathological findings demonstrated that, the uterus was asymmetrically enlarged, especially on the right side. The uterine cavity was divided into 2 hemicavities by an incomplete septum with a defect of 5 × 5 mm in the upper third. The blind hemicavity containing the gestational sac (30 × 30 × 20 mm) was on the right posterior side. Another hemicavity that connected to the cervix was on the left anterior side. Multiple uterine fibroids and adenomyosis were present (Fig. 6). Histological analysis showed the same findings, and focal placenta accreta was observed on the wall of the blind hemicavity.
Fig 6.
Pregnancy in the blind hemicavity (short arrow). Upper third of the septum revealed communication with the other half of the uterus (arrow). Uterine adenomyosis and fibroids (arrow head).
The hysterectomy and right salpingectomy were successful and the patient was discharged from the hospital on postoperative day 3.
Discussion
Robert's uterus is a rare obstructive form of Müllerian duct anomaly with American Society for Reproductive Medicine (ASRM) classification class of Ⅴb [7,8]. It is associated with the poorest reproductive outcome in terms of fetal survival rates and a high rate of spontaneous miscarriage [6]. In the ectopic pregnancy the patient experienced 24 years ago on her left fallopian tube was one of the complications associated with Robert's uterus.
Classical clinical presentation of Robert's uterus includes irregular menstrual cycle and progressive dysmenorrhea attributed to the rising pressure of the blind cavity [2,3]. The blind uterine cavity communicates with the ipsilateral fallopian tube and permits a small amount of menstrual blood flow into the peritoneal cavity, which might be the reason for the occurrence of endometriosis [9,10]. Contrary to the presentation in existing reports, the absence of similar clinical symptoms and focal placenta accreta on the wall of the blind cavity in the present case may suggest that the partially functional endometrial cavity played an important role in the patient's condition.
The patient in the present case had surgery for left adnexa ectopic pregnancy 24 years ago. We speculate that the right fallopian tube that communicates with the blind uterine cavity became the only way for the ovum from the right adnexa to pass through. The defect on the septum uterus provided a passage for the sperm.
Singhal et al have reported that pregnancy in the asymmetric blind hemicavity of Robert's uterus, complete septate uterus, and fetus lying in the noncommunicating right blind hemicavity suggest transperitoneal migration of the sperm via the cervix, contralateral cavity, and fallopian tube [5], which is an extremely rare event.
A combined laparoscopic and hysteroscopic approach for cutting the septum open and then suturing the uterus for appropriate restoration of normal uterine anatomy was used as a treatment for Robert's uterus [11]. Hysterectomy and right salpingectomy were performed in order to prevent this condition in the future.
Even though satisfactory treatment of Robert's uterus is not intricate [12,13], it is crucial that with a history of ectopic pregnancy and 2 natural labors. Robert's uterus was not diagnosed until an MRI was performed 24 years later in the present case. Radiologists and gynecologists should consider using the MRI for early diagnosis of congenital Müllerian uterine anomalies.
Patient consent
The patient consent has been obtained.
Acknowledgment
This study received no funding.
We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Contributor Information
Hui Li, Email: Lizhuren856@sina.com.
Yan Wang, Email: wangyandoct@sina.com.
References
- 1.Robert H. Asymmetrical bifidities with unilateral menstrual retention (apropos of l2 cases) Chirurgie. 1970;96:796. [PubMed] [Google Scholar]
- 2.Benzineb N, Bellasfar M, Merchaoui J. Robert's uterus with menstrual retention in the blind cavity. J Gynecol Obstet Biol Reprod (Paris) 1993;22:366. [PubMed] [Google Scholar]
- 3.Gupta N., Mittal S., Dadhwal V., Misra R. A unique congenital mullerian anomaly: Robert's uterus. Arch Gynecol Obstet. 2007;276(6):641–643. doi: 10.1007/s00404-007-0389-2. [DOI] [PubMed] [Google Scholar]
- 4.Perino A, Chianchiano N, Simonaro C. Endoscopic management of a case of, complete septate uterus with unilateral haematometra. Hum Reprod. 1995;10:2171. doi: 10.1093/oxfordjournals.humrep.a136256. [DOI] [PubMed] [Google Scholar]
- 5.Singhal S, Agarwal U, Sharma D, Sirohiwal D. Pregnancy in asymmetric blind hemicavity of Robert’s uterus a previously unreported phenomenon. Eur J Obstet Gynecol Reprod Biol. 2003;107(1):93–95. doi: 10.1016/s0301-2115(02)00238-5. [DOI] [PubMed] [Google Scholar]
- 6.Heinonen PK, Saarikoski S, Pystynen P. Reproductive performance of women with uterine anomalies. Acta Obstet Gynecol Scand. 1982;61:157±60. doi: 10.3109/00016348209156548. [DOI] [PubMed] [Google Scholar]
- 7.Ludwin A, Ludwin I. Comparison of the ESHRE-ESGE and ASRM classifications of Müllerian duct anomalies in everyday practice. Hum Reprod. 2015;30:569–580. doi: 10.1093/humrep/deu344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nasri MN, Setchell ME, Chard T. Transvaginal ultrasound for diagnosis of uterine malformations. Br J Obstet Gynecol. 1990;97:1043±5. doi: 10.1111/j.1471-0528.1990.tb02480.x. [DOI] [PubMed] [Google Scholar]
- 9.Jayasinghe Y, Rane A, Stalewski H, Grover S. The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol. 2005;105:1456–1467. doi: 10.1097/01.AOG.0000161321.94364.56. [DOI] [PubMed] [Google Scholar]
- 10.Capito C, Sarnacki S. Menstrual retention in a Robert's uterus. J Pediatr Adolesc Gynecol. 2009;22:e104–e106. doi: 10.1016/j.jpag.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Lima M, Cantone N, Destro F, Ruggeri G. Combined laparoscopic and hysteroscopic approach for the treatment of a hybrid Müllerian duct anomaly: a case report. J Laparoendosc Adv Surg Tech A. 2013;23:960–964. doi: 10.1089/lap.2013.0171. [DOI] [PubMed] [Google Scholar]
- 12.Ludwin A, Ludwin I, Bhagavath B, Lindheim SR. Pre-, intra-, and postoperative management of Robert's uterus. Fertil Steril. 2018;110:778–779. doi: 10.1016/j.fertnstert.2018.05.033. [DOI] [PubMed] [Google Scholar]
- 13.Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38:371–382. doi: 10.1002/uog.10056. [DOI] [PubMed] [Google Scholar]