Abstract
Family caregivers of Black older adults with dementia are at risk for cognitive decline and premature death. Reducing this risk and filling the void of culturally responsive interventions for caregivers requires the development of participant informed models of care that promote group strengths such as effective coping. In this pilot study, Black family caregivers (n=30) completed a survey comprised of a demographic questionnaire, various measures of function, self-efficacy, social support, and coping. Study findings point to a well-educated population with underlying health concerns such as obesity, hypertension, and diabetes that may be complicated by caregiving stress. Common coping strategies used by participants included spiritual coping (80%), use of past experiences (80%), and information gathering (75%). Clinicians can support dementia family caregivers by promoting spiritual coping and self-care, as well as providing reference resources about respite and managing challenging behaviors. Power analysis suggests a future sample size of 385.
Keywords: African Americans, Alzheimer Disease, Adaptation
Alzheimer’s disease is a leading causes of death in the United States and a primary contributor to both cognitive and functional disability among older adults.1-4 Challenges in clinical differentiation between Alzheimer’s disease and related dementias (ADRD), such as frontotemporal, Lewy body, mixed, and vascular dementia has led to the expansion of Alzheimer’s disease focused policy, health prevention, and promotion efforts to be more inclusive of the related disorders and the framing of these conditions collectively as Alzheimer’s disease and related dementias (ADRD).5 This is particularly important in beginning to address health disparities between Blacks and Whites as Black older adults with Alzheimer’s disease are 20 percent more likely than Whites to have mixed forms of dementia.6 In fact, those most at risk for a new ADRD diagnosis and premature death are Black ADRD family caregivers.7,8 Black family caregivers have increased risk factors for ADRD related to genetics, such as the presence of the Apoplipoprotein E (APOE) genotype, and stress-related health conditions such as obesity, hypertension and cardiovascular disease.9 Further, Black ADRD caregivers often experience significant emotional, financial, and physical health challenges that can diminish satisfaction with caregiving and reduce their ability to assist in care.10-13 There is an immediate need for interventions that will improve both health and caregiving satisfacation outcomes for Black ADRD family caregivers.
Due to cultural norms, Black older adults with ADRD are most likely to be cared for at home by a family rather than in long term care facilities by professional caregiving staff.14 This free, in-home labor, provided by family caregivers, creates a considerable cost savings to health care institutions, however, many families find themselves without adequate support, knowledge of caregiving tasks, or knowledge of anticipated disease progression—this, of course, all contributes to caregiver stress.15 Despite evidence that culture plays an important role in effective intervention implementation, few caregiver interventions have been specifically designed to meet the needs of underserved ethnic and racial populations with Alzheimer’s disease and/or related dementias.14,16
Cultural Values Influence Caregiving Behaviors
Culture, or the learned patterns of behaviors, beliefs, and values shared by individuals of particular social groups, influences health behaviors and decision making.17 In particular, factors such as perceived burden and use of selected coping strategies often have race dependent variances.14,18 It is likely that specific cultural values influence both caregiver stress perception and the coping strategies that family caregivers use when managing stress.19,20 If these shared values and related coping behaviors lead to increased adaptability, they may, and should be, considered a strength of the cultural group. Identifying and reinforcing the adaptive coping strategies cultural groups prefer to use, may strengthen both the group and the at-risk individual. Interestingly, population-focused health interventions are most often developed from deficit-based frameworks that emphasize group failures and needs rather than group strengths.21,22 The resulting interventions then create increased resource dependency which ultimately is not likely to be sustainable.21 Identifying and reinforcing multifaceted group strengths, particularly adaptability, supports sustainable, culturally responsive interventions that can improve population health.
Purpose
The overall objective of this pilot study is to test the feasibility of recruitment and participant burden in completing a battery of assessments that may be used to identify a culturally responsive model of care that can promote adaptive coping among Black family caregivers of persons with Alzheimer’s disease and/ or related dementias. The chosen assessment measures were selected based upon the starting conceptual framework (Figure 1) which was guided by the Roy adaptation model.23 The Roy adaptation model posits that humans are adaptive systems that strive to maintain functionality despite constant interaction with stressors from their internal and external environments. We purport that the behavioral and physical care needs of dementia care recipients cause stress that effects caregivers’ ability to cope. How a caregiver copes with their caregiving responsibilities, in turn, influences adaptation to caregiving as evidenced by increased caregiving self-efficacy, increased self-affirmation, and a positive outlook on life from the caregiving experience. We believe that these relationships are ultimately influenced by the caregiver’s mental and physical health (See Figure 1). Table 1 provides an overview of the study constructs, concepts, and measures. In this study, we focus on the effectiveness of selected recruitment strategies, the feasibility of administering a battery of assessment measures to participants that will allow us to test the proposed model, and developing a better understanding population characteristics that may influence intervention design. Power analysis is also completed to determine future sample size needs. It is anticipated that this study will lay the groundwork for a community-based clinical trial.
Figure 1:
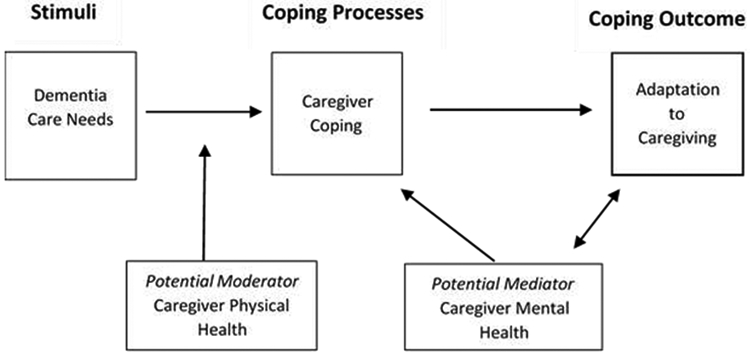
A Model of Coping with Caregiving
Table 1:
Study Concepts and Measures
| Construct | Concept/ Variables | Empirical Measures |
|---|---|---|
| Dementia Care Needs | Care recipient level of physical ability | Barthel Index of Activities of Daily Living |
| Care recipient level of independence | Instrumental Activities of Daily Living | |
| Caregiver Physical Health/Disease Burden | Self-perceived physical health | PROMIS Global Health Scale (PROMIS) |
| Body mass index | Self-report height/ weight | |
| Pain intensity | The Brief Pain Inventory | |
| Pain interference | The Brief Pain Inventory | |
| Caregiver Mental Health | Self-perceived mental health | PROMIS Global Health Scale (PROMIS) |
| Depression | Center for Epidemiological Studies Depression Scale – Revised (CESD-R) | |
| Caregiver Coping | Social Supports | Personal Resource Questionnaire (PRQ2000) |
| Coping | Coping and Adaptation Processing Scale (CAPS) | |
| Adaptation to Caregiving | Self-Affirmation Positive life outlook | Positive Aspects of Caregiving (PAC) |
| Caregiving self-efficacy | Revised Scale for Caregiving Self-Efficacy |
Methods
This cross-sectional pilot study was completed in southeastern Michigan and approved by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board. Family caregivers that self-identified as African American and/or Black, who met the following inclusion criteria participated in the study: 1) over the age of 18, 2) able to speak and understand English, 3) scored of 14 or higher on the Animal Naming Test (a semantic memory test), 4) related to or has a close personal relationship to a person over the age of 55 that has a dementia diagnosis or evidence of cognitive impairment, and 6) is responsible for, monitors and/ or provides assistance in activities of daily living for the care recipient.
Recruitment
Study participants were recruited primarily through two participant registries with academic research centers. Both centers maintain registries of volunteers who are interested in participating in aging-related research and have consented to being contacted regarding studies they may qualify for. Information about the study was included in community newsletters sent out to the registry participants. In addition, telephone contact information for research volunteers with likely eligibility was securely forwarded to research team staff. Potential volunteers were contacted by phone and provided an overview of the study to determine interest. The total number of call attempts for any potential participant was limited to three. Each sequential call after the first was attempted on a different day and at a different time between 10am and 7:30pm, excluding the dinner hour between 5-6:30pm. Once it was determined that a potential participant met the inclusion criteria and were interested in participating, a home visit was scheduled. In addition to registry lists with phone contact information, both research centers sponsored regular community education events in which direct recruitment took place by study staff. Participants were compensated for their participation with a $25 gift card.
Measures
Eligible participants completed a paper survey during a home visit by research staff. Staff monitored length of completion time for the survey, tracked questions participants had about specific survey items, and tracked study enrollment by referral source. Survey measures included a demographic questionnaire and various tools that evaluate function, self-efficacy, social support, and coping. As noted previously, each measure was selected to evaluate a specific concept of interest included in our model (see Figure 1 and Table 1). Particular measures were selected based upon 1) model fit, 2) length of assessment, 3) ease of administration, 4) use in similar studies, and 5) cost. The following provides a brief overview of the measures that were used including reliability findings using Chronbach’s alpha.
Health.
The PROMIS Global Health scale assesses health-related quality of life, an important predictor of disability, within the domains of physical and mental health. The evidenced reliability within the physical and mental health domains is .81 and .86 respectively.24 This free, 10-item tool was tested in a nationally representative sample (n=21,133) of both clinic and community-based participants and can be completed in less than two minutes.
Pain.
The Brief Pain Inventory Short Form25 measures pain intensity and pain interference by asking participants a series of questions about their level of pain in the past 24 hours and how pain has affected various aspects of daily life. It has been validated in various populations including Black older adults for both cancer and non-cancer pain assessment26 and has reliability ranging from .77 to .91.27 The measure contains 9 items and takes about 5-7 minutes to complete. The tool is proprietary by MD Anderson and has associated fees for use in research that range from $150− $400+ based upon funding.
Function.
The Barthel Index of Activities of Daily Living and the Lawton Instrumental Activities of Daily Living (IADL) tools were used to measure care recipient functioning. The Barthel Index28 is a 10-item scale that measures disability by asking a series of questions about independence in personal care activities and mobility. It is commonly used in clinical settings and has been found to be valid when completed by caregivers.29 Reliability ranges from .89 to .97.30 The Lawton-Brody IADL tool31 is another functional assessment tool, but it evaluates some of the more complex activities of daily living that are necessary for independent community living such as telephone use, grocery shopping, managing meals, and normal household chores. Sampling included Black older adults. Reliability is noted at .85.32 Both tools are freely available and take less than 5 minutes to complete.
Self-Efficacy.
Caregiver self-efficacy was measured by means of the Revised Scale for Caregiving Self-Efficacy which evaluates the caregiver’s ability to obtain respite care, respond to disruptive behaviors, and control their own upsetting thoughts about caregiving.33 Reliability ranged from .70 to .76 and the sample include Black older adults.33 Although this tool only has 15 questions, the nature of the questions and the explanations provided prior to some sections can take a bit more processing time for respondents. While the tool is free it can take up to 10 minutes to complete.
Social Support.
Caregiver social supports were measured by means of the Personal Resource Questionnaire (PRQ2000)34 which asks respondents 15 positively worded questions about their perceived level of social support. Reliability ranges from .87 to .93.35 This tool is easily completed under 5 minutes.
Coping.
The Coping and Adaptation Processing Scale Short Form (CAPS)36 is a 15-item tool designed to measure the ability of a person to respond to changes in the environment based upon their patterns of coping. It takes about 7-8 minutes to complete and has been validated internationally in a wide variety of populations. The reliability has been noted at of .82.36
Positive Aspects of Caregiving.
The Positive Aspects of Caregiving tool28 is a brief 9-item tool that asks questions about caregiving experiences that made the caregiver feel good about providing care on a scale from one to five. This quick tool is made of questions that fall into two components, self-affirmation and outlook on life, and can be completed in a couple of minutes. It has been validated in a nationally representative sample, including Black older adults and has a reliability of .89.37
Caregiver Mental Health.
Caregiver mental health was measured by means of the 4 question PROMIS Emotional Distress-Anxiety form38 and the Center for Epidemiological Studies Depression Scale-Revised (CESD-R).39 The PROMIS-Anxiety scale has a reliability of .89 and is completed under a minute. Both measures were validated in samples that included Black older adults. In this study, the CESD-R is being using to qualitatively describe the population and its inclination towards depression. As such, the version of the scale presented to participants in this study had two questions related to suicidal ideation that were removed leaving a total of 18 items. The CESD-R in its original format has a reliability of .90. Participants were able to complete this questionnaire in about 2-3 minutes.
Analysis
In addition to descriptive statistics, Spearman’s correlation coefficients were completed to identify relationships between variables and conduct power analysis. IBM SPSS Statistics 26 and SAS 9.4 were used for statistical analysis.
Results
Thirty-nine participants were successfully recruited over the course of 12 months. Nine individual were excluded after it was determined that they did not meet inclusion criteria or they were no longer interested in participation. The final sample included (n=30) Black family caregivers of persons with ADRD. In-person recruitment at community education events by study team members proved to be the least laborious with the highest number of yields (n= 20). One of the primary concerns that became evident with participant registry lists was the lack of caregiver status information. In instances where registry participants had granted permission to be contacted by phone, study team members surveyed for caregiver status through large phone campaigns, calling more than 100 registry participants using a standardized script. Many registry participants screened their calls, not answering unknown numbers, particularly non-university phone numbers. However, several returned the call when a message was left, also scripted, or answered on a subsequent call. The average time for study visits, including completion of consent forms and assessment measures, was about 45 minutes and ranged from 42 minutes to 60 minutes. Additional conversation time, including time prior completion of the consent forms and assessment measures as well as time spent directly afterwards with caregivers who may not have had an opportunity to talk with someone about their caregiving experiences before, could extend visit length by as much as 30 minutes. There was little participant burden identified--only the directions included with the Revised Scale for Caregiving Self-Efficacy, which were a bit long, was noted as being somewhat confusing for participants.
Participant demographics are outlined in Table 2. Study findings indicate that the sample (n=30) on average is educated, with at least some college (90%). Nearly half (46.6%) earned at least $50,000 per year or more. Similar to national trends, the vast majority of participants (90%) were women with a body mass index of 25 or greater indicating a health status of overweight (34.7%), obese (30.7%), or morbidly obese (30.8%). Most caregivers were over 65 years old and caring for a parent (43.3%) or spouse (23.3%) for either 1-2 years (17%) or greater than 2 years (66.7%). Most participants also lived in the same household as the care recipient (60%). A small, but significant, number of caregivers (23%) had the responsibility of caring for children under the age of 18 in addition to their usual dementia caregiving responsibilities. Care recipients had an average ADL index of 55 indicating severe dependency and an average IADL score of 1 indicating low functioning/ dependency. Caregivers reported being least confident (61%) in obtaining respite care, followed by responding to disruptive behaviors (82%). However, according the results of the Positive Aspects of Caregiving tool, the average participant scores indicated that providing care gave them a more positive attitude toward life (4.7 / 5 ), enabled increased appreciation of life (4.57 / 5), and strengthened their relationships with others (4.43 / 5)—all factors related to outlook on life. Sixty-three percent of caregivers reported hypertension (n=19) and 20% reported diabetes (n = 6). PROMIS global health scores alone were insignificant and indicated that self-rated mental (51.32) and physical health (51.86) were on par with community averages (standardized t-score = 50). However, statistically significant correlations (p < 0.05) were found between the PROMIS global health scores (mental health/ physical health) the Coping and Adaptive Processing summary score (r = .58/ r = .52 respectively). PROMIS mental health findings also supported findings of both the Center for Epidemiological Studies Depression Scale, where there was no evidence of trending towards depression and the PROMIS anxiety measure, where the average score was a 48.6, slightly below the standardized population average of 50. Fifty-three percent of participants reported daily moderate pain with an intensity of 5 on a 0-10 scale and finally, the coping strategies most readily identified by participants included information gathering, taking strength from spirituality, and the use of past experiences to inform current stressful situations.
Table 2.
Participant Demographics
| Study Variables | N (%) | |
|---|---|---|
| Age | 40-49 | 2 (7.69) |
| 50-59 | 3 (11.54) | |
| 60-69 | 11 (42.31) | |
| 70-79 | 9 (34.62) | |
| 80-89 | 1 (3.84) | |
| Education | High school graduate, diploma or equivalent | 3 (10) |
| Some college, no degree | 10 (33.33) | |
| Associate degree | 3 (10) | |
| Bachelor's degree | 9 (30) | |
| Master and PhD | 5 (16.66) | |
| Gender | Male | 3 (10) |
| Female | 27 (90) | |
| Sexual Orientation | Heterosexual | 29 (96.67) |
| Homosexual | 1 (3.33) | |
| Marital Status | Single | 7 (24.14) |
| Married | 14 (48.28) | |
| Widowed | 3 (10.34) | |
| Divorced | 5 (17.24) | |
| Employment Status | Employed full-time 40+ hrs | 6 (20) |
| Employed part-time up to 39 hours | 5 (16.67) | |
| Unemployed and looking | 1 (3.33) | |
| Retired | 17 (56.67) | |
| Self-employed | 1 (3.33) | |
| Income | Less than $20,000 | 5 (16.67) |
| $20,000 to $34,999 | 6 (20) | |
| $35,000 to $49,999 | 5 (16.67) | |
| $50,000 to $74,999 | 7 (23.33) | |
| $75,000 to $99,999 | 6 (20) | |
| Over $100,000 | 1 (3.33) | |
| How often providing care | Less than twice a week | 4 (13.33) |
| more than twice a week | 26 (86.67) | |
| Primary diagnosis of care recipient | Alzheimer's disease | 4 (13.33) |
| Vascular dementia or stroke | 6 (20) | |
| Parkinson's disease | 1 (3.33) | |
| Dementia not specified | 17 (56.67) | |
| mixed type | 1 (3.33) | |
| Other | 1 (3.33) | |
| Care recipient relationship to caregiver | Parent | 13 (43.3) |
| Grandparent | 2 (6.7) | |
| Spouse/ Significant Other | 8 (26.7) | |
| Ex-Spouse | 2 (6.7) | |
| Other Relative | 4 (13.3) | |
| Friend/ Neighbor | 1 (3.3) | |
Power analysis suggests a minimum future sample size of n=385 subjects after considering 10% poor qualified questionnaires. The proposed sample exceeds 80% power to detect statistically significant correlations (2-tailed, uncorrected alpha = 0.05) of .15 or greater between the outcomes and exposures.
Limitations
One of the major limitations of this small study was the lack of inclusion of a specific stress measure for caregivers. The selected nursing conceptual framework guiding this work, the Roy Adaptation Model, does not evaluate stress. Rather, the source of stress, or stimuli is determined and what is assessed is an individual, family or community’s ability to effectively adapt to that stressor. The outcomes within this strength-based model are coping capacity and ultimately improved health. As such, the Coping and Adaptation Process Scale, developed by Roy and based on the model, was used in the study along with the assessment of factors known to contribute to (or reduce) caregiver stress, as well as various measure of health. In future study it will be useful to also have a specific stress measure.
Another study limitation may be the possible sample bias created by the use of the participant registries and related registry activities. Although the sample, mostly educated by some college, reflects similar findings of large samples of Black adults40 some family caregivers may not be connected to a university participant registry or local churches where many of the recruitment activities took place. Future study will consider avenues for larger more inclusive sampling.
Discussion
The development of culturally responsive interventions that integrate the cultural beliefs and behavior patterns of the study population into the plan of care are an important means of addressing dementia related health disparities. This study provided significant information about the demographics, self-efficacy beliefs, and coping behavior patterns of a group of Black ADRD family caregivers along with information on how to improve research engagement with this population. For starters, in-person recruitment was most successful at community-based events, many of which took place at local area churches. Taking the time to engage with potential participants prior to the study visit to review the study protocol and answer any questions led to high levels of rapport with study team members and highly efficient visits. Participant registries are an important means of keeping diverse members of the community engaged with academic research and potentially connected with local resources. More registries must consider collecting the caregiver status of participants to facilitate dementia-related study engagement. There must be some additional attention placed on finding ways to better connect with local communities to more effectively recruit diverse participants and increase intra group heterogeneity. This could include expanding recruitment efforts outside of places of worship and engaging more targeted marketing.
Though this group of caregivers was generally well educated with some form of regular income they were receiving, managing challenging behaviors and accessing important resources, such as respite care services, was not something that the group felt confident about. A primary aim of ADRD caregiver interventions is to find improved mechanisms of supporting caregivers that encourage continued caregiving and facilitate aging in place for older adults. Study finding validate the need for continued caregiver education and training in the functional tasks of caregiving such as effective behavior management. Further, the challenges related to ADRD caregiving responsibilities can lead to diminished prioritization of self-care. Study findings of a population with increased levels of obesity, hypertension, and diabetes point to the need for additional attention to healthy lifestyle and chronic disease management for family caregivers to help them both improve their health and reduce their risk for a future dementia-related diagnosis. Finally, the selected assessment measures were found to be suitable for future study design due to low participant burden, overall low cost, and ease of administration. In future study, the directions to the Revised Scale for Caregiving Self-Efficacy will need be modified for clarity, a stress measure will be added and all of the assessment measures will need to be tested in an electronic delivery format, prior to moving forward with large scale national sampling.
An important opportunity exists for nurses to increase engagement with family caregivers and help them to connect with resources that may support both their caregiving and personal health needs. Finding both easily accessible and culturally responsive resources is uncommon, and warrants further development. However an important opportunity exists for health care providers to inquire about caregiving responsibilities of the patients they care for and connect them early on in the care recipient disease trajectory with resources and support. The high inclination towards spirituality as a primary means of coping, supports the inclusion of spiritual coping strategies, both religious and non-religious, into suggested caregiver supports, if available, and into future intervention design.
Though the small sample size and high homogeneity of the participants within this pilot may limit wide generalizability, this study provides important information that will help to shape the formulation of future inclusive clinical interventions and supportive service designed for diverse family caregivers. A much larger future sample, as suggested by power analysis, will allow for further testing and refinement of current model.
Highlights.
Family caregivers least confident in obtaining respite care
Effective management of challenging dementia-related behaviors a concern
Obesity, hypertension, and diabetes are primary health issues of caregivers
Spiritual coping identified as a primary coping strategy
Acknowledgments
This study was supported by a grant from the National Institutes of Health and the Michigan Center for Urban African American Aging Research (P30 AG015281).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heron M Deaths: Leading Causes for 2017. In: Reports NVS, ed. Hyattsville, MD: National Center for Health Statistics; 2019. [PubMed] [Google Scholar]
- 2.Alzheimer's Association. 2020 Alzheimer's disease facts and figures. 2020;16:391–460. [Google Scholar]
- 3.Muo R, Schindler A, Vernero I, Schindler O, Ferrario E, Frisoni GB. Alzheimer's disease-associated disability: an ICF approach. Disabil Rehabil 2005;27:1405–13. [DOI] [PubMed] [Google Scholar]
- 4.Arrighi HM, Gelinas I, McLaughlin TP, Buchanan J, Gauthier S. Longitudinal changes in functional disability in Alzheimer's disease patients. International psychogeriatrics 2013;25:929–37. [DOI] [PubMed] [Google Scholar]
- 5.National Plan to Address Alzheimer's Disease. 2016. at https://aspe.hhs.gov/sites/default/files/pdf/205581/NatlPlan2016.pdf.)
- 6.Barnes LL, Leurgans S, Aggarwal NT, et al. Mixed pathology is more likely in black than white decedents with Alzheimer dementia. Neurology 2015;85:528–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Z, Hayward MD, Yu Y-L. Life Course Pathways to Racial Disparities in Cognitive Impairment among Older Americans. Journal of Health and Social Behavior 2016;57:184–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manly JJ, Mayeux R. Ethnic Differences in Dementia and Alzheimer’s Disease. In: Anderson NB, Bulatao RA, Cohen B, eds. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 9.AARP, National Alliance for Caregiving. Caregiving in the US: NAC and AARP Policy Institute; 2015. [Google Scholar]
- 10.AARP, National Aliance for Caregiving. Caregiving in the U.S.2020. [Google Scholar]
- 11.Hughes TB, Black BS, Albert M, et al. Correlates of objective and subjective measures of caregiver burden among dementia caregivers: influence of unmet patient and caregiver dementia-related care needs. International psychogeriatrics 2014;26:1875–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Labra C, Millán-Calenti JC, Buján A, et al. Predictors of caregiving satisfaction in informal caregivers of people with dementia. Archives of Gerontology and Geriatrics 2015;60:380–8. [DOI] [PubMed] [Google Scholar]
- 13.Capistrant BD. Caregiving for Older Adults and the Caregivers’ Health: an Epidemiologic Review. Current Epidemiology Reports 2016;3:72–80. [Google Scholar]
- 14.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of Race, Ethnicity, and Culture in Caregiving Research: A 20-Year Review (1980–2000). The Gerontologist 2002;42:237–72. [DOI] [PubMed] [Google Scholar]
- 15.Park M, Choi S, Lee SJ, et al. The roles of unmet needs and formal support in the caregiving satisfaction and caregiving burden of family caregivers for persons with dementia. International psychogeriatrics 2018;30:557–67. [DOI] [PubMed] [Google Scholar]
- 16.Napoles AM, Chadiha L, Eversley R, Moreno-John G. Reviews: Developing Culturally Sensitive Dementia Caregiver Interventions: Are We There Yet? American Journal of Alzheimer's Disease and Other Dementias 2010;25:389–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robinson-Lane SG, Booker SQ. Culturally Responsive Pain Management for Black Older Adults. Journal of gerontological nursing 2017:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richardson VE, Fields N, Won S, et al. At the intersection of culture: Ethnically diverse dementia caregivers’ service use. 2019;18:1790–809. [DOI] [PubMed] [Google Scholar]
- 19.Bardi A, Guerra VM. Cultural Values Predict Coping Using Culture as an Individual Difference Variable in Multicultural Samples. Journal of Cross-Cultural Psychology 2010;42:908–27. [Google Scholar]
- 20.Utsey SO, Bolden MA, Lanier Y, Williams O. Examining the Role of Culture-Specific Coping as a Predictor of Resilient Outcomes in African Americans From High-Risk Urban Communities. 2007;33:75–93. [Google Scholar]
- 21.Bourke L, Humphreys JS, Wakerman J, Taylor J. From ‘problem-describing’ to ‘problem-solving’: Challenging the ‘deficit’ view of remote and rural health. 2010;18:205–9. [DOI] [PubMed] [Google Scholar]
- 22.Lind C, Smith D. Analyzing the state of community health nursing: advancing from deficit to strengths-based practice using appreciative inquiry. ANS Advances in nursing science 2008;31:28–41. [DOI] [PubMed] [Google Scholar]
- 23.Roy C The Roy Adaptation Model. 3rd ed. Upper Saddle River: Pearson; 2009. [Google Scholar]
- 24.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of Physical and Mental Health Summary Scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) Global Items. Quality of Life Research 2009;18:873–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cleeland CS. The Brief Pain Inventory User Guide. Houston, TX: Charles S. Cleeland; 1991. [Google Scholar]
- 26.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for Chronic Nonmalignant Pain. The Journal of Pain 2004;5:133–7. [DOI] [PubMed] [Google Scholar]
- 27.The Brief Pain Inventory. 2020. (Accessed 2020, at https://www.mdanderson.org/research/departments-labs-institutes/departments-divisions/symptom-research/symptom-assessment-tools/brief-pain-inventory.html.)
- 28.Mahoney FI, Barthel DW. FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Maryland state medical journal 1965;14:61–5. [PubMed] [Google Scholar]
- 29.Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: A reliability study. International Disability Studies 1988;10:61–3. [DOI] [PubMed] [Google Scholar]
- 30.Sainsbury A, Seebass G, Bansal A, Young JB. Reliability of the Barthel Index when used with older people. Age and Ageing 2005;34:228–32. [DOI] [PubMed] [Google Scholar]
- 31.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86. [PubMed] [Google Scholar]
- 32.Graf C The Lawton instrumental activities of daily living (IADL) scale. Medsurg nursing : official journal of the Academy of Medical-Surgical Nurses 2008; 17:343. [PubMed] [Google Scholar]
- 33.Steffen AM, McKibbin C, Zeiss AM, Gallagher-Thompson D, Bandura A. The Revised Scale for Caregiving Self-Efficacy: Reliability and Validity Studies. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 2002;57:P74–P86. [DOI] [PubMed] [Google Scholar]
- 34.Weinert C Measuring Social Support: PRQ2000. In: Strickland O CD, eds. Measurement of Nursing Outcomes: Volume 3 Self Care and Coping. Newy York: Springer Publishing Company; 2003:161–72. [Google Scholar]
- 35.Tawalbeh LI, Ahmad MM. Personal Resource Questionnaire: A Systematic Review. Journal of Nursing Research 2013;21:170–7. [DOI] [PubMed] [Google Scholar]
- 36.Roy C, Bakan G, Li Z, Nguyen TH. Coping measurement: Creating short form of Coping and Adaptation Processing Scale using item response theory and patients dealing with chronic and acute health conditions. Applied Nursing Research 2016;32:73–9. [DOI] [PubMed] [Google Scholar]
- 37.Tarlow BJ, Gallagher-Thompson D, Belle SH, Rubert M, Ory MG, Wisniewski SR. Positive aspects of caregiving: contributions of the REACH project to the development of new measures for Alzheimer's caregiving. Research on Aging 2004;26:429. [Google Scholar]
- 38.Kroenke K, Yu Z, Wu J, Kean J, Monahan PO. Operating characteristics of PROMIS four-item depression and anxiety scales in primary care patients with chronic pain. Pain medicine (Malden, Mass) 2014;15:1892–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Dam NT, Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale--Revised (CESD-R): pragmatic depression assessment in the general population. Psychiatry research 2011;186:128–32. [DOI] [PubMed] [Google Scholar]
- 40.Barnes LL, Wilson RS, Hebert LE, Scherr PA, Evans DA, Mendes de Leon CF. Racial differences in the association of education with physical and cognitive function in older blacks and whites. The journals of gerontology Series B, Psychological sciences and social sciences 2011. ;66:354–63. [DOI] [PMC free article] [PubMed] [Google Scholar]


