Abstract
Background: We investigated the current medical and social conditions and outcomes of heart failure (HF) patients in Hiroshima Prefecture, a local district in Japan.
Methods and Results: From March 2017 to February 2018 we enrolled all adult patients with hospitalized HF in 8 regional core hospitals that provided an interprofessional team approach for HF patients. We collected patients’ clinical characteristics and information regarding living circumstances, cognitive function, quality of life, and interprofessional team approach. For patients discharged home, we followed up the primary endpoint (all-cause death and all-cause unscheduled readmission), conditions of outpatient cardiac rehabilitation, and home nursing-care services over a 1-year period after discharge. Of the registered patients (n=1,218), 39.2% were super-elderly (≥85 years old); more than half of these patients had preserved ejection fraction (≥50%). In the follow-up cohort (n=632), 140 patients (22.2%) were readmitted with HF exacerbation as the primary endpoint, and almost half (n=295, 46.7%) experienced any primary endpoint. The multivariate analysis adjusted for medical and social factors showed that completion of outpatient cardiac rehabilitation (5-month program) remained a strong negative predictor of the primary endpoint (hazard ratio: 0.15; 95% confidence interval: 0.05–0.48; P=0.0013).
Conclusions: Our cohort study highlighted the super-aging of current HF patients in Japan. Cardiac rehabilitation through continuous team approach appears to be associated with favorable overall outcomes in this population.
Key Words: Aging, All-cause events, Cardiac rehabilitation, Heart failure, Medical and social conditions
Heart failure (HF) is an important public health problem, because chronic HF is refractory, impairs patents’ quality of life (QOL), and has a poor prognosis. Moreover, considerable medical resources are consumed in caring for patients with HF because of repeated hospital admissions and discharges. Given the “heart failure pandemic”,1 the management of patients with chronic HF has become a worldwide issue from both the clinical and social perspective.
In Japan, some large-scale studies targeting patients with HF have been conducted, including the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD),2 the Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART) study,3 the Heart Institute of Japan-Department of Cardiology (HIJC),4 and the acute decompensated heart failure syndromes (ATTEND) registry.5,6 These studies have provided information regarding the clinical characteristics of patients with HF, such as HF causes, history, clinical data, treatment status, and clinical factors that affect patient outcomes (e.g., anemia and atrial fibrillation).7,8 A recent multicenter cohort of Japanese patients with HF (the Kitakawachi Clinical Background and Outcome of Heart Failure [KICKOFF] Registry) described patients’ social backgrounds, including life style, family support, dietary and drug management, exercise habits, and long-term care insurance.9 Although previous studies have focused on the real conditions of Japanese patients with HF, substantial changes in Japanese society, including a drastic increase in the older adult population and increased survival rate in patients with acute disorders, may affect current real conditions and outcomes for patients with chronic HF in Japan. To successfully manage the medical and social issues faced by patients with HF in Japan, we need to understand their current real conditions and outcomes.
A registry and follow-up study of the medical and social conditions and outcomes of hospitalized heart failure patients (REAL-HF) prospectively studied the medical and social conditions of patients with hospitalized HF in the Hiroshima area of Japan over 1 year from March 2017.10 Additionally, events after discharge home, including all-cause death and all-cause unscheduled readmission, were followed through 2019. The REAL-HF program initially enrolled patients hospitalized in 8 institutions participating in the Hiroshima Heart Health Promotion Project.
The present study aimed to provide an epidemiologic database of current real conditions (both medical and social) of patients with HF in Hiroshima Prefecture, a typical local district in Japan. We also investigated factors for improving patients’ outcomes based on the REAL-HF database.
Methods
Study Patients
Details of the REAL-HF protocol have been described previously.10 Briefly, all adult patients (aged ≥20 years) hospitalized with symptomatic HF were enrolled. The diagnosis of symptomatic HF was confirmed according to the Framingham Study (congestive HF),11 or by the presence of low-output syndrome (general fatigue, coldness of limbs, cyanosis, digestive symptoms, and hepatic or renal dysfunction assumed to be due to low cardiac output) diagnosed by primary physicians. For each patient, baseline data at admission included: (1) living circumstances before admission; (2) past history of hospitalization for HF; (3) underlying heart diseases as the etiology of HF; (4) ongoing HF symptom severity; (5) comorbidities exacerbating HF; and (6) clinical data for serum B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-proBNP), echocardiography, and chest X-ray. Additional data collected at hospital discharge included: (1) treatment status (medication and treatment by device); (2) cognitive function status (Mini Mental State Examination [MMSE]); (3) QOL questionnaire (EuroQol 5 dimensions [EQ5D]) scores; (4) physical activity (independent gait ability); and (5) presence or absence of inpatient cardiac rehabilitation and interprofessional team approach (based on our established notebook for HF management) during hospitalization.
The REAL-HF enrolled 1,218 patients with hospitalized HF from March 2017 to February 2018. Patients who were discharged home and agreed to a follow-up observation after discharge were included in the follow-up cohort.
Follow-up After Discharge Home
The status of patients in the follow-up cohort was surveyed at 3 and 12 months after discharge home. Information was obtained through face-to-face or telephone interviews and included: (1) all-cause death, (2) all-cause unscheduled readmission, (3) outpatient cardiac rehabilitation (introduction and completion [5-month program that is allowed under health insurance in Japan]), and (4) home nursing-care services (presence or absence and level of certification of public nursing-care need in Japanese nursing insurance system).
Patients hospitalized for HF are reportedly at high risk for all-cause rehospitalization.12 In this study, we defined the primary endpoints as all-cause death and all-cause unscheduled readmission due to cardiovascular or non-cardiovascular diseases requiring treatment. Additionally, we defined the conditions of outpatient cardiac rehabilitation and home nursing-care services as secondary endpoints. We did not examine how outpatient cardiac rehabilitation and home nursing-care services were executed (e.g., content or frequency).
Statistical Analysis
Serum BNP and NT-pro-BNP levels are expressed as median and interquartile range because they showed non-parametric distributions. Other continuous values were expressed as mean±standard deviation. Student’s t-tests or Mann-Whitney U tests were used for comparison of continuous variables between groups. Categorical variables are reported as number (proportion, %) and compared using Pearson’s chi-square tests. Event rates for the primary endpoint were estimated with Kaplan-Meier curves and compared with a log-rank test. A Cox proportional hazard regression model was used to assess predictors of the primary endpoint. Additionally, a propensity-matched analysis was used to examine the effect of outpatient cardiac rehabilitation on the primary endpoint. A multivariate logistic regression model was used to calculate the propensity score, and 2 cohorts were created based on the score for the comparison. All analyses were performed using JMP Pro 14.2.0 statistical software (SAS Institute Inc., NC, USA). A P-value of <0.05 was considered statistically significant.
Ethical Consideration
The institutional review boards of Hiroshima University and the other participating institutions approved this prospective study. The protocol has been published in the Japan UMIN Clinical Trials Registry (ID: UMIN000025651).
For all recruited patients with HF, baseline information during the indexed hospitalization was collected based on the extraction and review of medical records. As this was performed anonymously, the need for patient consent was waived. For patients included in the follow-up cohort, information regarding the endpoint was collected after obtaining written informed consent.
Results
Patients’ Data at Baseline and Hospital Discharge
The baseline characteristics of the entire cohort were described in the previous report.10 Included patients (n=1,218) were much older (79±13 years) compared with patients enrolled in previous large HF cohorts in Japan. The super-elderly (aged ≥85 years) comprised a considerable portion of the cohort (n=477, 39.2%), and more than half of these patients (53.1%) had preserved left ventricular ejection fraction (EF ≥50%).
Table 1 shows patient data at hospital discharge. Most patients received loop diuretic (84.4%), and β-blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, and aldosterone antagonists were moderately administered (41.9–66.5%). Treatments using devices were given to a small proportion of patients (<10%). During hospitalization, most patients (84.2%) underwent inpatient cardiac rehabilitation. For each multidisciplinary approach, a description of clinical status by physicians and drug administration guidance by pharmacists were available for most patients (>80%), but other approaches varied in frequency.
Table 1.
Patients’ Data at Hospital Discharge
| Variable | n=1,218 |
|---|---|
| Treatment status | |
| Medication | |
| Catecholamine (during hospitalization) | 207 (17.0) |
| β-blocker | 810 (66.5) |
| ACEI or ARB | 627 (51.5) |
| Thiazide diuretic | 82 (6.7) |
| Loop diuretic | 1,028 (84.4) |
| Aldosterone antagonist | 510 (41.9) |
| Tolvaptan | 279 (22.9) |
| Antidiabetic drug | 233 (19.1) |
| Device | |
| ASV | 62 (5.1) |
| Pacemaker | 110 (9.0) |
| ICD | 25 (2.1) |
| CRT | 35 (2.9) |
| Cognitive function: MMSE score (n=789)† | 24±5 |
| QOL: EQ5D score (n=780)‡ | 0.74±0.23 |
| Physical function: independent gait (possible) | 859 (70.5) |
| Inpatient cardiac rehabilitation | 1,025 (84.2) |
| Multidisciplinary approach | |
| Description of clinical status | 1,073 (88.1) |
| Antismoking education | 115 (9.4) |
| Guidance for HF notebook | 630 (51.7) |
| Self-monitoring education | 596 (48.9) |
| Drug administration guidance | 1,016 (83.4) |
| Nutritional guidance | 839 (68.9) |
| Exercise guidance | 922 (75.7) |
| Care environment adjustment | 512 (42.0) |
| Outcome | |
| Discharged home | 904 (74.2) |
| Other hospital | 252 (20.7) |
| Death | 62 (5.1) |
MMSE and EQ5D scores expressed as mean±standard deviation; other data expressed as number (proportion, %). †,‡Data acquired during hospitalization. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ASV, adaptive servo-ventilation; CRT, cardiac resynchronization therapy; EQ5D, EuroQol 5 dimensions; HF, heart failure; ICD, implantable cardiac defibrillator; MMSE, Mini Mental State Examination; QOL, quality of life.
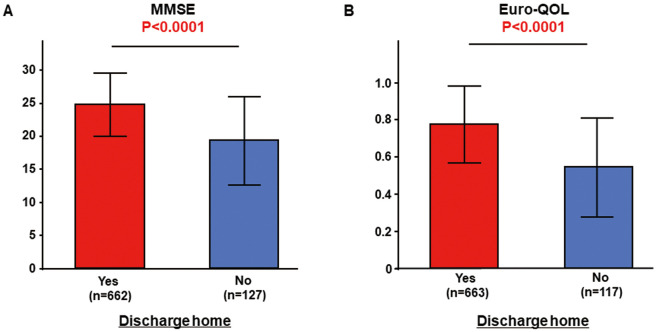
Of the entire cohort, 904 (74.2%) were discharged home, 252 (20.7%) were moved to another hospital, and 62 died during hospitalization (mortality: 5.1%). Patients discharged home (aged 77±13 years, 532 males) had higher MMSE (25±5 vs. 19±7, P<0.0001) and EQ5D (0.78±0.21 vs. 0.54±0.27, P<0.0001) scores than those who were not discharged home (Figure 1). Of the patients discharged home, independent gait was possible for most patients (87.1%, 787/904), but this was observed less often in patients who were moved to another hospital (28.6%, 72/252, P<0.0001).
Figure 1.
Comparison of Mini Mental State Examination (MMSE) and EuroQol 5 dimensions (EQ5D) scores between patients discharged home and those not discharged home.
Outcomes After Discharge Home
Of the patients discharged home, 641 (70.9%) who agreed to a follow-up observation were included in the follow-up cohort; 9 patients were excluded because of incomplete information. The remaining 632 patients (aged 78±13 years, 363 males) were studied regarding the endpoint (information acquisition rate: 98.6%).
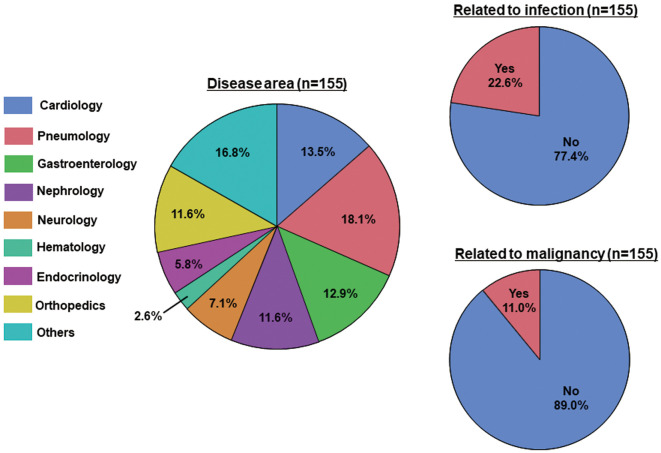
Figure 2 shows the Kaplan-Meier curves for the primary endpoint. Within 3 months, 91 patients (14.4%) were rehospitalized with HF exacerbation as the primary endpoint, and 157 (24.8%; 7 deaths and 150 readmissions) experienced any primary endpoint. During the 1-year follow-up period, 140 patients (22.2%) were rehospitalized with HF exacerbation as the primary endpoint, and almost half (n=295, 46.7%; 15 deaths and 280 readmissions) experienced any primary endpoint. Figure 3 summarizes the primary diagnoses other than HF causing death or unscheduled readmission. For the secondary endpoints, outpatient cardiac rehabilitation was introduced to 63 patients (10.0%), of whom 33 (5.2%) completed the 5-month program. The proportion of use of home nursing-care services was 33.2% (210/632) at discharge home, but increased to 39.2% (248/632) at 3 months after discharge.
Figure 2.
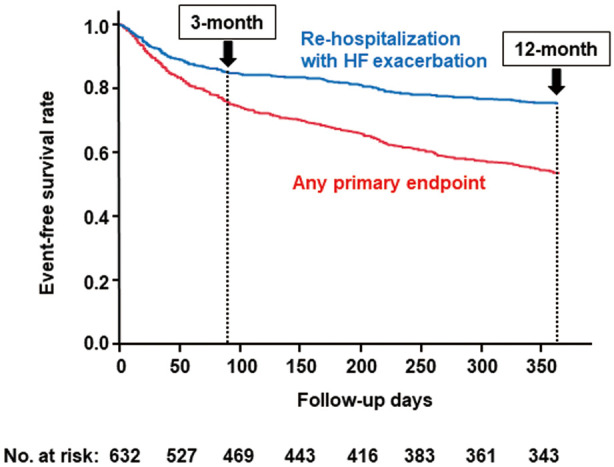
Kaplan-Meier curves for the primary endpoint (rehospitalization with heart failure (HF) exacerbation and any primary event) in patients discharged home.
Figure 3.
Distribution of primary diagnosis other than heart failure causing death or unscheduled readmission.
Factors for Improving Outcomes
Table 2 shows patients’ medical and social characteristics based on the presence or absence of the primary endpoint. Compared with patients without the primary endpoint (non-event group), patients experiencing the primary endpoint (event group) were older (80±12 vs. 76±14 years, P<0.0001), and more frequently had a history of being hospitalized for HF at study registration (P<0.0001). There were no differences in underlying heart diseases and New York Heart Association (NYHA) classes at admission between these 2 groups. In terms of comorbidities exacerbating HF, chronic kidney disease was more frequent in the event group than in the non-event group (45.4% vs. 32.6%, P=0.0010), but rates of other comorbidities were similar. There were no differences in serum BNP or NT-proBNP levels, but the event group had slightly higher EF than the non-event group (48.2±15.8% vs. 45.5±16.4%, P=0.047). However, the distribution of the EF classes (EF <40%, EF 40–50%, EF ≥50%) in the 2 groups was similar. Patients in the event group had lower MMSE (24±5 vs. 26±4, P=0.001) and EQ5D (0.75±0.21 vs. 0.81±0.19, P=0.0002) scores than those in the non-event group. Living circumstances were similar in the 2 groups. Compared with the non-event group, the event group showed lower introduction (7.1% vs. 12.5%, P=0.025) and completion rates (1.0% vs. 8.9%, P<0.0001) of outpatient cardiac rehabilitation, and a higher proportion of use of home nursing-care services (48.5% vs. 31.2%, P<0.0001).
Table 2.
Patients’ Characteristics According to the Presence or Absence of the Primary Endpoint
| Primary endpoint | P value | ||
|---|---|---|---|
| Presence (n=295) | Absence (n=337) | ||
| Age (years) | 80±12 | 76±14 | <0.0001 |
| Male (%) | 163 (55.3) | 200 (59.4) | 0.30 |
| History of hospitalization for HF | <0.0001 | ||
| 1 st time | 164 (55.6) | 248 (73.6) | |
| 2nd time | 54 (18.3) | 54 (16.0) | |
| ≥3 times | 77 (26.1) | 35 (10.4) | |
| Underlying heart disease* | |||
| Ischemic | 82 (27.8) | 84 (24.9) | 0.41 |
| Valvular | 115 (39.0) | 108 (32.1) | 0.069 |
| Hypertensive | 89 (30.2) | 94 (27.9) | 0.53 |
| Other | 100 (33.9) | 127 (37.7) | 0.32 |
| HF severity at admission | 0.34 | ||
| NYHA I | 3 (1.0) | 10 (3.0) | |
| NYHA II | 50 (17.0) | 59 (17.5) | |
| NYHA III | 159 (53.9) | 182 (54.0) | |
| NYHA IV | 83 (28.1) | 86 (25.5) | |
| Comorbidity | |||
| Hypertension | 199 (67.5) | 218 (64.7) | 0.46 |
| Diabetes mellitus | 86 (29.2) | 97 (28.8) | 0.92 |
| Dyslipidemia | 69 (23.4) | 86 (25.5) | 0.53 |
| Atrial fibrillation | 140 (47.5) | 138 (41.0) | 0.10 |
| CKD | 134 (45.4) | 110 (32.6) | 0.001 |
| Obesity (BMI ≥28) | 19 (6.4) | 22 (6.5) | 0.96 |
| Smoking | 70 (23.7) | 94 (27.9) | 0.23 |
| COPD | 26 (8.8) | 24 (7.1) | 0.43 |
| Biomarker (pg/mL)† | |||
| BNP | 581 (376–1,003) (n=237) |
529 (282–940) (n=284) |
0.090 |
| NT-proBNP | 4,395 (1,509–6,643) (n=51) |
2,702 (1,398–5,729) (n=48) |
0.13 |
| EF (%)† | 48.2±15.8 (n=265) |
45.5±16.4 (n=311) |
0.047 |
| HF class based on EF† | 0.15 | ||
| HFrEF (EF <40%) | 79 (29.8) | 116 (37.3) | |
| HFmrEF (40%≤EF<50%) | 57 (21.5) | 55 (17.7) | |
| HFpEF (EF ≥50%) | 129 (48.7) | 140 (45.0) | |
| MMSE score† | 24±5 (n=270) |
26±4 (n=307) |
0.001 |
| EQ5D score† | 0.75±0.21 (n=271) |
0.81±0.19 (n=307) |
0.0002 |
| Living circumstances | 0.68 | ||
| Alone | 51 (17.3) | 66 (19.6) | |
| With family member | 236 (80.0) | 264 (78.3) | |
| In a nursing home | 8 (2.7) | 7 (2.1) | |
| Outpatient cardiac rehabilitation | |||
| Introduction | 21 (7.1) | 42 (12.5) | 0.025 |
| Completion | 3 (1.0) | 30 (8.9) | <0.0001 |
|
Use of home nursing-care services (at 3 months after discharge) |
143 (48.5) | 105 (31.2) | <0.0001 |
Biomarker levels expressed as the median value (interquartile range); other data expressed as mean±standard deviation or number (proportion, %). *Some patients had ≥2 underlying heart diseases. †Data acquired during hospitalization. BMI, body mass index; BNP, B-type natriuretic peptide; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; EF, ejection fraction; EQ5D, EuroQol 5 dimensions; HF, heart failure; HFpEF, heart failure with preserved EF; MMSE, Mini Mental State Examination; NT-proBNP, N-terminal pro-B-type natriuretic peptide; NYHA, New York Heart Association.
To assess predictors of the primary endpoint, we performed a Cox proportion analysis adjusted for age, sex, living circumstances (alone or not), history of hospitalization for HF at registration, underlying heart diseases, NYHA class at admission, comorbidities exacerbating HF, use of home nursing-care services, and introduction or completion of outpatient cardiac rehabilitation (5-month program). This information was acquired for all followed patients. The presence of history of hospitalization for HF (hazard ratio: 1.66; 95% confidence interval [CI]: 1.30–2.12; P<0.0001) and presence of use of home nursing-care services (hazard ratio: 1.33; 95% CI: 1.02–1.75; P=0.039) remained a positive predictor of the primary endpoint. However, completion of outpatient cardiac rehabilitation remained a strong negative predictor of the primary endpoint (hazard ratio: 0.15; 95% CI: 0.05–0.48; P=0.0013), whereas the introduction of outpatient cardiac rehabilitation did not (Table 3).
Table 3.
Cox Proportional Analysis of Predictors of the Primary Endpoint
| Variable | Univariate | Multivariate (model 1) | Multivariate (model 2) | |||
|---|---|---|---|---|---|---|
| Hazard ratio | P value | Hazard ratio | P value | Hazard ratio | P value | |
| Age (per 1-year increase) | 1.02 (1.01–1.03) | 0.0001 | 1.01 (0.99–1.02) | 0.21 | 1.01 (0.99–1.02) | 0.31 |
| Sex (male) | 0.90 (0.71–1.13) | 0.35 | ||||
| Living circumstances (alone) | 0.86 (0.63–1.16) | 0.31 | ||||
| History of hospitalized HF (presence) | 1.79 (1.43–2.26) | <0.0001 | 1.63 (1.274–2.08) | <0.0001 | 1.66 (1.30–2.12) | <0.0001 |
| Underlying heart disease (ischemic) | 1.11 (0.86–1.44) | 0.41 | ||||
| Underlying heart disease (valvular) | 1.27 (1.00–1.60) | 0.048 | 1.19 (0.88–1.61) | 0.27 | 1.17 (0.86–1.58) | 0.32 |
| Underlying heart disease (hypertensive) |
1.05 (0.82–1.35) | 0.68 | ||||
| Underlying heart disease (others) | 0.88 (0.69–1.12) | 0.32 | ||||
| NYHA (per 1-class increase) | 1.12 (0.95–1.31) | 0.17 | ||||
| Comorbidity (hypertension) | 1.07 (0.84–1.37) | 0.58 | ||||
| Comorbidity (diabetes mellitus) | 1.02 (0.80–1.31) | 0.86 | ||||
| Comorbidity (dyslipidemia) | 0.90 (0.68–1.17) | 0.42 | ||||
| Comorbidity (atrial fibrillation) | 1.22 (0.97–1.53) | 0.093 | 1.02 (0.80–1.31) | 0.85 | 1.03 (0.80–1.32) | 0.84 |
| Comorbidity (CKD) | 1.48 (1.18–1.86) | 0.0008 | 1.22 (0.95–1.56) | 0.11 | 1.21 (0.95–1.54) | 0.13 |
| Comorbidity (obesity [BMI ≥28]) | 1.02 (0.64–1.62) | 0.93 | ||||
| Comorbidity (smoking) | 0.84 (0.64–1.10) | 0.20 | ||||
| Comorbidity (COPD) | 1.23 (0.82–1.84) | 0.32 | ||||
| Use of home nursing-care services (at 3-month after discharge) |
1.63 (1.30–2.05) | <0.0001 | 1.33 (1.01–1.75) | 0.040 | 1.33 (1.02–1.75) | 0.039 |
| Outpatient cardiac rehabilitation (introduction) |
0.63 (0.40–0.98) | 0.039 | 0.70 (0.44–1.11) | 0.13 | NA | NA |
| Outpatient cardiac rehabilitation (completion) |
0.14 (0.04–0.43) | 0.0007 | NA | NA | 0.15 (0.05–0.48) | 0.0013 |
Data expressed as hazard ratio (95% confidence interval). Model 1: adjusted for introduction of outpatient cardiac rehabilitation and other variables. Model 2: adjusted for completion of outpatient cardiac rehabilitation and other variables. Abbreviations as in Table 2.
Effect of Outpatient Cardiac Rehabilitation on Outcomes
We further examined the effect of outpatient cardiac rehabilitation on the primary endpoint using propensity-matched analysis. Propensity scores estimating the probability of introduction or completion of outpatient cardiac rehabilitation were calculated for the patients. The multivariate logistic regression model for the propensity score included the following variables: age, sex, living circumstances (alone or not), history of hospitalization for HF at registration, underlying heart diseases, NYHA class at admission, comorbidities exacerbating HF, EF, MMSE score, EQ5D score, and use of home nursing-care services.
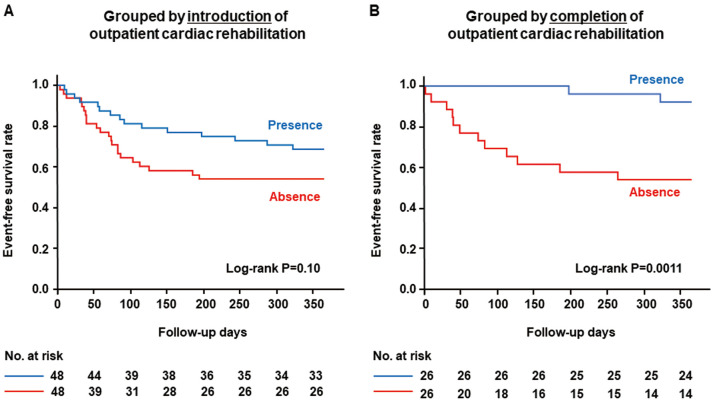
The matching process for introduction of outpatient cardiac rehabilitation created 2 cohorts of 48 patients, one with introduction and another without. The 2 groups were well balanced with respect to all the variables (Supplementary Table 1). There was no significant difference in the proportion of patients experiencing the primary endpoint by introduction of outpatient cardiac rehabilitation (with introduction 31.3% vs. without introduction 45.8%, P=0.14). The Kaplan-Meier curves demonstrated that the outcome for the primary endpoint was similar between the 2 groups (P=0.10 by log-rank test) (Figure 4A). Similarly, the matching process for completion of outpatient cardiac rehabilitation created 2 cohorts of 26 patients, one with completion and another without. The 2 groups were well balanced with respect to all the variables (Supplementary Table 2). The group with completion of outpatient cardiac rehabilitation experienced the primary endpoint much less frequently than the group without completion (7.7% vs. 46.2%, P=0.0018). The Kaplan-Meier curves demonstrated that patients with completion of outpatient cardiac rehabilitation had more favorable outcomes for the primary endpoint than those without completion (P=0.0011 by log-rank test) (Figure 4B). Even after the 5-month program, patients with completion of outpatient cardiac rehabilitation experienced many fewer events.
Figure 4.
Kaplan-Meier curves for the primary endpoint stratified by (A) introduction or (B) completion of outpatient cardiac rehabilitation. The groups were created using propensity-matched analysis.
Discussion
Hiroshima Prefecture is a typical local district of Japan that covers both urban and rural areas and has a total population of 2,800,000. We investigated the current medical and social conditions and outcomes of patients with HF in 8 regional core hospitals providing an interprofessional team approach for this population. The important insights from this cohort study are summarized as follows. (1) Our cohort study highlighted the super-aging of current HF patients in Japan, in whom the proportion of patients with preserved EF is increasing. (2) Cognitive function and QOL status assessed during HF hospitalization were related to discharge home and outcomes after discharge home. (3) In institutions providing comprehensive HF care, there were fewer rehospitalizations because of HF exacerbation as a primary endpoint, although almost half of the HF patients had any all-cause event (death or unscheduled readmission) within a 1-year period after discharge home. (4) Even in such institutions, the rates of introduction and completion of outpatient cardiac rehabilitation were low. (5) Despite these low rates, outpatient cardiac rehabilitation, especially completion (5-month program), was associated with favorable overall outcomes in HF patients. Our REAL-HF study provided a unique database clarifying current real conditions and outcomes of Japanese HF patients from medical and social perspectives. Notably, the follow-up study of patients discharged home after HF hospitalization highlighted the close association of a continuous team approach through cardiac rehabilitation with patients’ overall outcomes.
HF Patients in Japan’s Aging Society
The first notable point in the REAL-HF cohort was the super-aging of current HF patients in Japan. Compared with patients in previous large HF cohorts in Japan (aged 71±13 years in JCARE-CARD and 69±13 years in CHART), the mean age of our cohort was almost 10 years older. The super-elderly (≥85 years) accounted for a substantial proportion (≈40%) of our cohort. HF patients with preserved EF are reported to be older,13 and as expected, more than half of the super-elderly in our cohort had preserved EF. Large-scale registry databases (e.g., the EuroHeart Failure Survey, Acute Decompensated Heart Failure National Registry [ADHERE), and Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure [OPTIMIZE-HF)] demonstrated a similar prognosis between patients with preserved EF and those with reduced EF.14–16 A report from a previous cohort study in Japan (JCARE-CARD) showed that HF patients with preserved HF and those with reduced EF experienced similar rates of mortality and rehospitalization as a result of worsening HF.17 In the REAL-HF cohort, we focused on all-cause events (death and unscheduled readmission) as the primary endpoint after discharge home, and found no difference in the distribution of HF classes based on EF between the event group and the non-event group (Table 2). This suggested that factors beyond cardiac function should be considered and managed to improve overall outcomes in current HF patients.
Cognitive Function or QOL Status and Outcomes in HF Patients
Patients with HF reportedly incur cognitive impairment frequently,18,19 have impaired QOL status (assessed by EQ5D score), and may become care-dependent.20 For these factors, aside from cardiovascular dysfunction, we confirmed that patients discharged home after HF hospitalization had better cognitive function and QOL status than those who were not discharged home. Additionally, we found that HF patients experiencing no all-cause events during a 1-year period after discharge home had better cognitive function and QOL status than those who experienced any event. However, we need to be mindful that even patients discharged home or those experiencing no events have some reduction in cognitive function and QOL status (Figure 1, Table 2). This reflects a key aspect of HF patients in the current Japanese aging society, which suggests an important target for successfully managing the medical and social issues of these patients in Japan.
All-Cause Events in HF Patients
In the follow-up cohort, we defined all-cause events (death or unscheduled readmission due to cardiovascular or non-cardiovascular diseases requiring treatment) as the primary endpoint, which was a key feature of this cohort study. A previous cohort study in Japan reported that 35% of hospitalized patients with HF were readmitted because of exacerbation of HF within 1 year of hospital discharge, with the most common factor for the readmission being lack of compliance with medical and dietary treatment.21 The 8 institutions participating in the REAL-HF cohort study have focused on preventing readmission of HF patients through interprofessional team approaches and this might have contributed to the fewer rehospitalizations with HF exacerbation after discharge home in this study compared with rates reported from previous epidemiologic data. However, almost half of our patients experienced any all-cause event within a 1-year period after discharge home. As shown in Figure 3, the primary diagnoses other than HF causing death or unscheduled readmission included a variety of non-cardiovascular diseases, such as infectious and malignant diseases (22.6% and 11.0%, respectively). The incidence rate of rehospitalization with HF exacerbation as a primary endpoint was 14.4% within 3 months and it increased to 22.2% during the 1-year follow-up period, while that of any primary endpoint (all-cause events) was 24.8% within 3 months and increased to 46.7% during the 1-year follow-up period. This indicated that rehospitalization for HF exacerbation occurs more often in the early phase (3 months) after discharge home, and that all-cause events are likely to occur consistently over the 1-year period.
Outpatient Cardiac Rehabilitation
A critical message from this cohort study for management of HF patients was the importance of a continuous team approach through cardiac rehabilitation. A multidisciplinary team approach is expected to reduce the mortality and all-cause hospitalizations of HF patients.22 Hiroshima University Hospital and the other 7 regional core hospitals participating in the REAL-HF cohort study have built a network to provide interprofessional team approaches for HF patients. The team in each hospital comprises multidisciplinary medical care personnel, including physicians, nurses, physical therapists, nutritionists, pharmacists, and social workers. The main activity of the team is inpatient/outpatient rehabilitation covering aerobic exercise, patient education about HF, and lifestyle guidance using our established notebook for HF management. We previously reported single-center data showing that our institutional team approach reduced all-cause hospitalizations and medical costs in patients with an elevated serum HF biomarker (NT-proBNP).23 Inpatient cardiac rehabilitation was applied to the majority of the patients in the participating institutions; however, we found that the rate of application of outpatient cardiac rehabilitation was low. Our follow-up study indicated that HF patients undergoing outpatient cardiac rehabilitation were likely to live without all-cause events. In particular, the completion of a 5-month program was related to 1-year event-free survival in HF patients, irrespective of their medical and social conditions. We speculated that one reason for the low application rate of outpatient cardiac rehabilitation might be the difficulty in frequent hospital visits for patients. However, there is a lack of understanding about the need for and effectiveness of continuous cardiac rehabilitation for HF patients. Our results may lead to a greater focus on this issue.
Study Limitations
First, according to the standard strategy for HF, optimal medical therapy (administration of β-blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, and aldosterone antagonists) appeared to be insufficient in this study. We need to consider this treatment condition when we assess the effects of a multidisciplinary approach for HF and cardiac rehabilitation. Second, the rate of patients being followed up after discharge home was low. We confirmed there were no significant differences in patient characteristics between the followed (n=632) and non-followed patients (n=272), except for the frequency of smoking (26.0% vs. 34.9%, P=0.0062) and MMSE score (24.9±4.6 vs. 23.3±5.7, P=0.017). On the other hand, our follow-up cohort had an excellent rate of completion of information acquisition (98.6%). Third, in the propensity-matched analyses, the extracted patients were younger than those in the entire cohort. Therefore, the effectiveness of outpatient cardiac rehabilitation in super-elderly patients cannot be discussed based on these analyses. However, the multivariate Cox proportion analysis after adjustment for age demonstrated that completion of outpatient cardiac rehabilitation remained a strong inhibitory factor for all-cause events, suggesting the universal value of cardiac rehabilitation program after discharge home. Fourth, the differences in the real conditions of HF patients according to area characteristics (e.g., urban or rural) are of interest; these factors have not yet been assessed and will be our next focus. Finally, how to beneficially apply the multidisciplinary approach, cardiac rehabilitation, and home nursing-care services for HF patients was not fully understood through this study. A prospective interventional study may be helpful in this regard.
Conclusions
The REAL-HF cohort study conducted in Hiroshima Prefecture as a local district of Japan has provided a unique database that clarifies current medical and social conditions and outcomes of Japanese HF patients. It highlights the super-aging of current HF patients in Japan. Our follow-up study also demonstrated that a continuous multidisciplinary team approach through cardiac rehabilitation is closely associated with favorable overall outcomes in this population.
Disclosures
This study was supported by the Japan Agency for Medical Research and Development (AMED) under Grant No. JP17ek0210058. This study was also supported by a local medical program of the Hiroshima Prefecture Government in Japan (Hiroshima Heart Health Promotion Project).
IRB Information
Name of the ethics committee, Ethical Committee for Epidemiology of Hiroshima University; the reference number, E-613.
Supplementary Files
REAL-HF Investigators Supplementary Table 1. Patient Characteristics for the Propensity-Matched Cohort-1 Supplementary Table 2. Patient Characteristics for the Propensity-Matched Cohort 2
Acknowledgments
We thank Ayano Michimura for assistance with aggregating and summarizing the patient data. We also thank Audrey Holmes, MA, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
References
- 1. Starling RC.. The heart failure pandemic: Changing patterns, costs, and treatment strategies. Cleve Clin J Med 1998; 65: 351–358. [DOI] [PubMed] [Google Scholar]
- 2. Tsutsui H, Tsuchihashi-Makaya M, Kinugawa S, Goto D, Takeshita A; JCARE-CARD Investigators.. Clinical characteristics and outcome of hospitalized patients with heart failure in Japan. Circ J 2006; 70: 1617–1623. [DOI] [PubMed] [Google Scholar]
- 3. Shiba N, Watanabe J, Shinozaki T, Koseki Y, Sakuma M, Kagaya Y, et al.. Analysis of chronic heart failure registry in the Tohoku district: Third year follow-up. Circ J 2004; 68: 427–434. [DOI] [PubMed] [Google Scholar]
- 4. Kawashiro N, Kasanuki H, Ogawa H, Matsuda N, Hagiwara N; Heart Institute of Japan – Department of Cardiology (HIJC) Investigators.. Clinical characteristics and outcome of hospitalized patients with congestive heart failure: Results of the HIJC-HF registry. Circ J 2008; 72: 2015–2020. [DOI] [PubMed] [Google Scholar]
- 5. Sato N, Kajimoto K, Asai K, Mizuno M, Minami Y, Nagashima M, et al.. Acute decompensated heart failure syndromes (ATTEND) registry: A prospective observational multicenter cohort study: Rationale, design, and preliminary data. Am Heart J 2010; 159: 949–955.e1. [DOI] [PubMed] [Google Scholar]
- 6. Sato N, Kajimoto K, Keida T, Mizuno M, Minami Y, Yumino D, et al.. Clinical features and outcome in hospitalized heart failure in Japan (from the ATTEND Registry). Circ J 2013; 77: 944–951. [DOI] [PubMed] [Google Scholar]
- 7. Hamaguchi S, Tsuchihashi-Makaya M, Kinugawa S, Yokota T, Takeshita A, Yokoshiki H, et al.. Anemia is an independent predictor of long-term adverse outcomes in patients hospitalized with heart failure in Japan: A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 2009; 73: 1901–1908. [DOI] [PubMed] [Google Scholar]
- 8. Hamaguchi S, Yokoshiki H, Kinugawa S, Tsuchihashi-Makaya M, Yokota T, Takeshita A, et al.. Effects of atrial fibrillation on long-term outcomes in patients hospitalized for heart failure in Japan: A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 2009; 73: 2084–2090. [DOI] [PubMed] [Google Scholar]
- 9. Takabayashi K, Ikuta A, Okazaki Y, Ogami M, Iwatsu K, Matsumura K, et al.. Clinical characteristics and social frailty of super-elderly patients with heart failure: The Kitakawachi Clinical Background and Outcome of Heart Failure Registry. Circ J 2016; 81: 69–76. [DOI] [PubMed] [Google Scholar]
- 10. Kitagawa T, Hidaka T, Naka M, Isobe M, Kihara Y; for the REAL-HF Investigators.. Current medical and social conditions and outcomes of hospitalized heart failure patients: Design and baseline information of the cohort study in Hiroshima. Circ Rep 2019; 1: 112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ho KK, Pinsky JL, Kannel WB, Levy D.. The epidemiology of heart failure: The Framingham Study. J Am Coll Cardiol 1993; 22: 6A–13A. [DOI] [PubMed] [Google Scholar]
- 12. Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, et al.. Patterns of hospital performanc in acute myocardial infarction and heart failure 30-day morality and readmission. Circ Cardiovasc Qual Outcomes 2009; 2: 407–413. [DOI] [PubMed] [Google Scholar]
- 13. Hogg K, Swedberg K, McMurray J.. Heart failure with preserved left ventricular systolic function: Epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol 2004; 43: 317–327. [DOI] [PubMed] [Google Scholar]
- 14. Lenzen MJ, Scholte op Reimer WJ, Boersma E, Vantrimpont PJ, Follath F, Swedberg K, et al.. Differences between patients with a preserved and a depressed left ventricular function: A report from the EuroHeart Failure Survey. Eur Heart J 2004; 25: 1214–1220. [DOI] [PubMed] [Google Scholar]
- 15. Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC.. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: A report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol 2006; 47: 76–84. [DOI] [PubMed] [Google Scholar]
- 16. Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al.. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: A report from the OPTIMIZE-HF Registry. J Am Coll Cardiol 2007; 50: 768–777. [DOI] [PubMed] [Google Scholar]
- 17. Tsuchihashi-Makaya M, Hamaguchi S, Kinugawa S, Yokota T, Goto D, Yokoshiki H, et al.. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction: Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 2009; 73: 1893–1900. [DOI] [PubMed] [Google Scholar]
- 18. Vogels RL, Scheltens P, Schroeder-Tanka JM, Weinstein HC.. Cognitive impairment in heart failure: A systematic review of the literature. Eur J Heart Fail 2007; 9: 440–449. [DOI] [PubMed] [Google Scholar]
- 19. Sauvé MJ, Lewis WR, Blankenbiller M, Rickabaugh B, Pressler SJ.. Cognitive impairments in chronic heart failure: A case controlled study. J Card Fail 2009; 15: 1–10. [DOI] [PubMed] [Google Scholar]
- 20. Janssen DJ, Franssen FM, Wouters EF, Schols JM, Spruit MA.. Impaired health status and care dependency in patients with advanced COPD or chronic heart failure. Qual Life Res 2011; 20: 1679–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tsuchihashi M, Tsutsui H, Kodama K, Kasagi F, Takeshita A.. Clinical characteristics and prognosis of hospitalized patients with congestive heart failure: A study in Fukuoka, Japan. Jpn Circ J 2000; 64: 953–959. [DOI] [PubMed] [Google Scholar]
- 22. McAlister FA, Stewart S, Ferrua S, McMurray JJ.. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: A systematic review of randomized trials. J Am Coll Cardiol 2004; 44: 810–819. [DOI] [PubMed] [Google Scholar]
- 23. Kitagawa T, Oda N, Mizukawa M, Hidaka T, Naka M, Nakayama S, et al.. Hospitalization and medical cost of patients with elevated serum N-terminal pro-brain natriuretic peptide levels. PLoS One 2018; 13: e0190979. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
REAL-HF Investigators Supplementary Table 1. Patient Characteristics for the Propensity-Matched Cohort-1 Supplementary Table 2. Patient Characteristics for the Propensity-Matched Cohort 2