Highlights
-
•
The management of mandibular angle fractures is often challenging and has a high complication rate.
-
•
The treatment of mandibular angle fractures aims to achieve a good reduction, stable fixation, and early recovery of masticatory function.
-
•
The contemporary practice uses a variety of surgical techniques for the fixation of angular fractures.
-
•
The single miniplate has recently become the technique of choice.
Keywords: Osteosynthesis, Complications, Standard miniplate, Mandibular angle fracture, Rigid fixation, Surgical treatment
Abstract
Introduction
The aim of this paper is to compare the clinical results between the different methods of fixation of standard mini-plates for the management of mandibular angle fractures.
Study design
This was a retrospective analysis study of 196 patients with mandibular angle fractures divided into 3 groups at our hospital 20 august 1953 specialist hospital, which is a referral center between January 2015 and January 2020. The patients were assessed for malocclusion, infection, wound dehiscence, neuro-sensory deficit, mouth opening, stability, operating time, blood loss, and hardware failure. Group (I) comprised 72 men and 40 women with a mean age of 43 years. Group (II) comprised 36 men and 12 women with a mean age of 47 years. Group (II) comprised 29 men and 7 women with a mean age of 33 years. The assessment of surgical outcomes after the last follow-up visit clearly showed a lack of stability in patients group II compared to the other groups. The operating time was reduced in group I compared to Group II/ III. (P = 0.03) The wound dehiscence occurred mostly in Group III unless it was statistically no significant. The infection events occurred in 36 patients of the sample, which was not statistically significant (Table 4).
Discussion
Fractures of the mandibular angle represent 23–42% of all mandibular fractures, in our context road accidents followed by aggression are the most frequent mechanisms found. A various types of treatment approaches for the treatment of angular fractures have been described. Our analysis revealed that surgical time and complication rate has been reduced when using the Group I technique compared to the other groups.
Conclusion
The use of the monocortical external oblique miniplate provides the best results. Successful treatment of mandibular fractures depends on stability in the ideal anatomical position since abnormal mobility at the fracture site will lead to non-union, malocclusion, and infection.
1. Introduction
The management of mandibular angle fractures is often challenging and has a high complication rate. The most appropriate treatment of angle fractures remains controversial [1,2].
Biomechanical analysis has revealed that the best site for plating is the flat, vestibular bone part located in the third molar region. The easiness of access and the extreme strength of the cortex make this site the preferred site for angle osteosynthesis. However, lower osteosynthesis, on the external surface of the mucosa, is sufficiently strong to support the stress generated by masticatory forces in the angular region [3,4].
The mandibular angle area is submitted to biomechanical forces (due to muscle insertion) and the presence of the third molar [5], therefore the treatment of mandibular angle fractures requires an in-depth understanding of the anatomy of the region. The treatment of mandibular angle fractures aims to achieve a good reduction, stable fixation, and early recovery of masticatory function [6].
The contemporary practice uses a variety of surgical techniques for the fixation of angular fractures. The single noncompression monocortical miniplate fixation of the angular fractures has recently become the technique of choice [7].
2. Patients and methods
This was a retrospective analysis study of 196 patients with mandibular angle fractures divided into 3 groups at our hospital 20 august 1953 specialist hospital, which is a referral center between January 2015 and January 2020. All patients underwent an open reduction under general anesthesia. The surgeries were performed by a team of residents under the supervision of the chief professor of the maxillofacial surgery department.
Inclusion criteria were patients diagnosed with angular fractures of the mandible and surgically treated with open reduction.
Patients with any associated mandibular fractures, patients not fit to undergo procedures under general anesthesia, treated by orthopedic approach were excluded from this study.
This study's data were collected using the files' analysis focused on the epidemiological, clinical, radiological explorations, therapeutic aspects. The patients were assessed for malocclusion, infection, wound dehiscence, mouth opening, stability, operating time, blood loss, and hardware failure.
Data management and analysis were performed using IBM SPSS Statistics for Windows, version 25.0.0 (IBM Corporation, Armonk, NY). Categorical data were summarized as frequencies, and cross-tabulations and x2 tests for significance made comparisons across allocated groups. Continuous variables were summarized as the mean and range, and comparisons between groups were made using the ANOVA test. All significance tests used a two-sided P-value of 0.05.
This case series has been reported in line with the PROCESS criteria [8].
3. Surgical technique
After placement of arch bars, the surgical incision was performed. A reduction of fracture is done, and the jaws were placed into postoperative maxilla-mandibular fixation if it’s necessary (MMF).
Group I: A single 4-hole non-compression miniplate (2 mm) was fixed in the external oblique line at the superior border of the mandible (Picture 1).
Picture 1.
A single 4-hole non-compression miniplate (2 mm) was fixed in the external oblique line at the superior border of the left mandible.
Group II: A single 4-hole non-compression miniplate (2 mm) was fixed at the ventral border of the mandible (Picture 2).
Picture 2.
A single 4-hole non-compression miniplate (2 mm) was fixed at the ventral border of the left mandible.
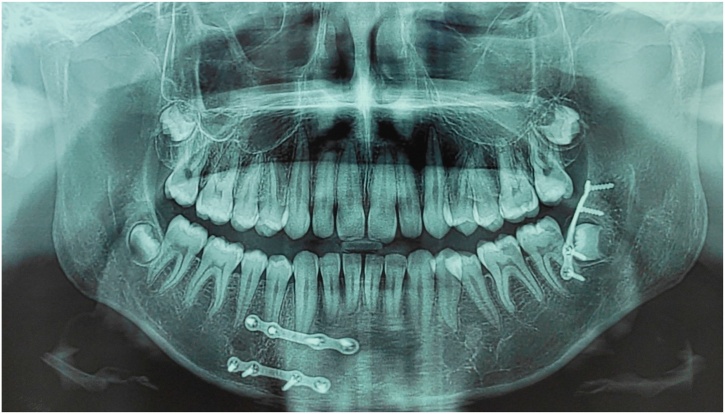
Group III: two 4-hole non-compression mini plates in which 1 plate was fixed like that in group I and the other plate was fixed to the lateral aspect of the angle of the mandible (Picture 3).
Picture 3.
Two 4-hole non-compression mini plates in which 1 plate was fixed like that in group I and the other plate was fixed to the lateral aspect of the angle of the mandible.
After the plates were placed, MMF was released and occlusion was checked. The intraoral incision was closed with resorbable sutures. Patients were reviewed at 1, 2, 4, and 6 weeks after surgery. The arch bars were removed after the fourth postsurgical week. The patients received amoxicillin/clavulanic acid 1 g twice daily and antalgics for 8 days.
To examine the neuro-sensory deficit, the ability to feel touch or pain in the lower lips was tested. Our patients' eyes were closed. Using a piece of cotton, we applied a light touch to one or both sides of the third trigeminal division and asked the patient to show or tell if the sensation is the same on both sides.
4. Results
The characteristics of the patients divided into groups, as well as the clinical considerations are presented in Table 1.
Table 1.
Characteristic of Population.
| Groups |
|||
|---|---|---|---|
| G(1) | G(2) | G(3) | |
| Mean age (yr.) | 43±19 | 47±17 | 33±12 |
| Gender | |||
| Female | 40 | 12 | 7 |
| Male | 72 | 36 | 29 |
| Oral hygiene | |||
| Poor | 20 | 11 | 16 |
| Average | 68 | 18 | 10 |
| good | 24 | 29 | 10 |
| TOTAL | 112 | 48 | 36 |
We included in Group (I), 112 patients who were treated with a single non-compression mini-plate fixed in the oblique line at the superior border through an intraoral approach. In Group (II), 48 patients were treated with a mini-plate fixed to the lateral aspect of the angle of the mandible with the intraoral approach. 36 patients were included in the group (III) which two mini-plates in which one miniplate was fixed like that in the group (I) and the other was fixed in the ventral aspect of the angular area of the mandible.
Group (I) comprised 72 men and 40 women with a mean age of 43 years.
Group (II) comprised 36 men and 12 women with a mean age of 47 years.
Group (II) comprised 29 men and 7 women with a mean age of 33 years (Table 2).
Table 2.
Comparison among the groups depending on occlusion, mouth opening, infection, stability at the 7th post-op days.
| Occlusion |
Mouth opening |
Stability |
||||
|---|---|---|---|---|---|---|
| Satisfactory (%) | Deranged (%) | Adequate (%) | Inadequate (%) | Stable (%) | Unstable (%) | |
| Group I (n = 112) | 91 (81.25) | 21 (18.75) | 103 (91.96) | 9 (8.04) | 95 (84.82) | 17 (15.18) |
| Group II (n = 48) | 19 (39.58) | 29 (60.42) | 31 (64.58) | 17 (35.42) | 10 (20.83) | 38 (79.17) |
| Group III (n = 36) | 24 (66.67) | 12 (33.33) | 22 (61.11) | 14 (38.89) | 32 (88.89) | 4 (11.11) |
| P value | 0.021 | 0.843 | 0.07 | |||
The assessment of surgical outcomes after the last follow-up visit clearly showed a lack of stability in patients group II compared to the other groups. The operating time was reduced in group I compared to Group II/ III. (P = 0.03) (Table 3).
Table 3.
Comparison among the groups depending on operating time, blood loss, hospital stay.
| Operating time (mean minutes) | Blood loss (ml) | Hospital stay (mean) | Postoperative MMF (n) | |
|---|---|---|---|---|
| Group (I) | 33 ± 12 | 50 | 2.33 ± 1.27 | 45 |
| Group (II) | 43 ± 11 | 55 | 2.44 ± 1.02 | 15 |
| Group (III) | 83 ± 21 | 91 | 3,78 ± 2.45 | 24 |
| P value | 0.03 | 0.042 | 0.06 | 0.89 |
The wound dehiscence occurred mostly in Group III unless it was statistically no significant. The infection events occurred in 36 patients of the sample, which was not statistically significant (Table 4).
Table 4.
Comparison among the groups depending on occlusion, mouth opening, infection, stability.
| Wound dehiscence (%) |
Hardware failure (%) |
Non-union (%) |
Neuro-sensory deficit (%) |
Infection (%) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| yes | no | yes | no | yes | no | yes | no | yes | no | |
| Group I (n = 112) | 17 (15.18) | 95 (84.82) | 3 (2.68) | 109 (97.32) | 8 (7.14) | 104 (92.86) | 34 (30.36) | 78 (69.64) | 13 (11.6) | 99 (88.4) |
| Group II (n = 48) | 7 (14.58) | 41(85.42) | 9 (18.75) | 39 (81.25) | 7 (14.58) | 41 (85.42) | 16 (33.33) | 32 (66.67) | 17 (35.42) | 31 (64.58) |
| Group III (n = 36) | 22 (61.11) | 14 (38.89) | 7 (19.44) | 29 (80.56) | 7 (19.44) | 29 (80.56) | 29 (80.56) | 7 (19.44) | 6 (16.67) | 30 (83.33) |
| P value | 0.08 | 0.32 | 0.076 | 0.057 | 0.066 | |||||
Routine follow-up 1, 3, 6, and 12 months in our specialized consultation; any clinical signs that appeared were mentioned on the patient's discharge form. Mild edema and paresthesia were common during the first week postoperatively in our study; no vascular damage was noted. Nineteen patients from all groups required plate removal given the evolution towards cervicofacial cellulitis.
5. Discussion
Fractures of the mandibular angle represent 23–42% of all mandibular fractures, in our context road accidents followed by aggression are the most frequent mechanisms found. Unerupted and impacted wisdom teeth create an area of weakness. A various types of treatment approaches for the treatment of angular fractures have been described [9].
Successful treatment of mandibular fractures depends on stability in the ideal anatomical position since abnormal mobility at the fracture site will lead to non-union, malocclusion, and infection [10].
The first classification of nerve injury was established by Seddon in 1947, who described nerve damage in three grades of injury [11]. In 1951, Sunderland enlarged the histologically based classification to include five degrees of lesions, which corresponded to Seddon's three-level classification overall, with a more accurate prognosis of the outcome of axonotrimary lesions [12] (Table 5).
Table 5.
Nerve injury classification in increasing severity.
| Sunderland [12] | Seddon [11] | Features |
|---|---|---|
| Type 1 | Neuropraxia | Damage to local myelin only |
| Type 2 | Axonotmesis | Division of intraneural axons only |
| Type 3 | Axonotmesis | Division of axons and endoneurium |
| Type 4 | Axonotmesis | Division of axons, endo- and perineurium |
| Type 5 | Neurotmesis | Complete division of all elements including epineurium |
| Type 6 | Mixed | Combination of types 2–4 |
The aim of this paper was to check by retrospective study, whether there is a significant difference in clinical outcome between the different fixation methods in the management of angular fractures of the mandible.
Our analysis revealed that surgical time and complication rate has been reduced when using the Group I technique compared to the other groups, but recently, based on advanced design and modeling of 3D mini-plates using the finite element method combined with CAD/CAM technology that could further reduce surgical time, since the surgeon would not have to model the plates intra-operatively [[13], [14], [15]].
The difference between the techniques regarding the incidence of wound dehiscence (15.17% in Group I) may be related to the proximity of the mini-plate to the incision, when placed on the external oblique line. However, the differences between the groups were not statistically significant (P = 0.08).
No statistically significant difference in the incidence of paresthesia was observed between the three techniques (P = 0.057). In the course of the operation, aggressive manipulation due to the displacement of the fracture may account for additional nerve damage. Therefore, it is important to seek paresthesia before surgery because if it’s not checked before the operation, it may appear as an iatrogenic complication of the surgery.
The follow-up period in the study was 1–12 months. Several complications may not appear immediately, such as plaque exposure or infection, which may occur months or years after successful healing [16].
6. Conclusion
In summary, the results of this study identified lower complication rates with the use of oblique line mini-plate fixation compared to other methods of standard miniplate fixation in the management of angular fractures of the mandible.
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
The authors declared that this study has received no financial support.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Ouassime kerdoud: Corresponding author writing the paper.
Rachid Aloua: writing the paper.
Amine kaouani: writing the paper.
Faiçal Slimani: Correction of the paper.
Registration of research studies
researchregistry6471.
Guarantor
Ouassime Kerdoud.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Gear A.J.L., Apasova E., Schmitz J.P., Schubert W. Treatment modalities for mandibular angle fractures. J. Oral Maxillofac. Surg. 2005 doi: 10.1016/j.joms.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 2.Ellis E. Treatment methods for fractures of the mandibular angle. Int. J. Oral Maxillofac. Surg. 1999 doi: 10.1016/s0901-5027(99)80152-0. [DOI] [PubMed] [Google Scholar]
- 3.Champy M., Loddé J.P., Schmitt R., Jaeger J.H., Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J. Maxillofac. Surg. 1978;6:14–21. doi: 10.1016/S0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- 4.Michelet F.X., Deymes J., Dessus B. Osteosynthesis with miniaturized screwed plates in maxillo-facial surgery. J. Maxillofac. Surg. 1973 doi: 10.1016/S0301-0503(73)80017-7. [DOI] [PubMed] [Google Scholar]
- 5.Meisami T., Sojat A., Sàndor G.K.B., Lawrence H.P., Clokie C.M.L. Impacted third molars and risk of angle fracture. Int. J. Oral Maxillofac. Surg. 2002 doi: 10.1054/ijom.2001.0215. [DOI] [PubMed] [Google Scholar]
- 6.Kim M.Y., Kim C.H., Han S.J., Lee J.H. A comparison of three treatment methods for fractures of the mandibular angle. Int. J. Oral Maxillofac. Surg. 2016 doi: 10.1016/j.ijom.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Levy F.E., Smith R.W., Odland R.M., Marentette L.J. Monocortical miniplate fixation of mandibular angle fractures. Arch. Otolaryngol. Neck Surg. 1991;117:149–154. doi: 10.1001/archotol.1991.01870140037002. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O’Neill N., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Pagano D., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Chi-Yong Ngu J., Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K., Mei Z. The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Chrcanovic B.R. Fixation of mandibular angle fractures: clinical studies. Oral Maxillofac. Surg. 2014 doi: 10.1007/s10006-012-0374-1. [DOI] [PubMed] [Google Scholar]
- 10.Choi B.H., Kim K.N., Kang H.S. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 1995 doi: 10.1016/S1079-2104(05)80301-4. [DOI] [PubMed] [Google Scholar]
- 11.Seddon H.J. The use of autogenous grafts for the repair of large gaps in peripheral nerves. Br. J. Surg. 1947 doi: 10.1002/bjs.18003513808. [DOI] [PubMed] [Google Scholar]
- 12.McQuarrie I.G. Nerve injuries and their repair: a critical appraisal. Neurology. 1991 doi: 10.1212/wnl.41.11.1858-a. [DOI] [Google Scholar]
- 13.Hart R.T., Hennebel V.V., Thongpreda N., Van Buskirk W.C., Anderson R.C. Modeling the biomechanics of the mandible: a three-dimensional finite element study. J. Biomech. 1992 doi: 10.1016/0021-9290(92)90025-V. [DOI] [PubMed] [Google Scholar]
- 14.Kim K.Y., Bayome M., Park J.H., Kim K.B., Mo S.S., Kook Y.A. Displacement and stress distribution of the maxillofacial complex during maxillary protraction with buccal versus palatal plates: finite element analysis. Eur. J. Orthod. 2015;37:275–283. doi: 10.1093/ejo/cju039. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen-Xuan H., Rabczuk T., Bordas S., Debongnie J.F. A smoothed finite element method for plate analysis. Comput. Methods Appl. Mech. Eng. 2008 doi: 10.1016/j.cma.2007.10.008. [DOI] [Google Scholar]
- 16.Barry Conor P., Kearns Gerard J. Superior border plating technique in the management of isolated mandibular angle fractures: a retrospective study of 50 consecutive patients. J. Oral Maxillofac. Surg. 2007;65(8):1544–1549. doi: 10.1016/j.joms.2006.10.069. [DOI] [PubMed] [Google Scholar]