Abstract
Malaysia was faced with a life-threatening crisis in combating COVID-19 with a number of positive cases reaching 5305 and 88 deaths by 18th April 2020 (the first detected case was on 25th January 2020). The government rapidly initiated a public health response and provided adequate medical care to manage the public health crisis during the implementation of movement restrictions, starting 18th March 2020, throughout the country. The objective of this study was to investigate the relative efficiency level of managing COVID-19 in Malaysia using network data envelopment analysis. Malaysia state-level data were extracted from secondary data sources which include variables such as total number of confirmed cases, death cases and recovered cases. These variables were used as inputs and outputs in a network process that consists of 3 sub processes i) community surveillance, ii) medical care I and iii) medical care II. A state-level analysis was performed according to low, medium and high population density categories. The efficiency level of community surveillance was highest compared to medical care processes, indicating that the overall inefficiency is greatly influenced by the inefficiency of the medical care processes rather than the community surveillance process. Results showed that high-density category performed well in both community surveillance and medical care II processes. Meanwhile, low-density category performed better in medical care I process. There was a good overall performance of the health system in Malaysia reflecting a strong preparedness and response level to this pandemic. Furthermore, resource allocation for rapid response was distributed effectively during this challenging period.
Keywords: COVID-19 prevention and treatment, Efficiency measurement, Network DEA, Malaysia
Highlights
Efficiency analysis can potentially be used to measure the performance of health system in managing COVID-19 pandemic that may reflect the preparedness and response level of the country.
Network Data Envelopment Analysis is used to measure relative efficiency of managing COVID-19 in Malaysia involving 3 sub processes i) community surveillance, ii) medical care I and iii) medical care II.
High population density category performed well in both community surveillance and medical care II processes while low population density category performed better in the medical care I process.
Preparedness planning and response actions in the case of COVID-19 in Malaysia should consider population density in the distribution of resources. Fair allocation of government resources is one of the critical success factors in managing COVID-19 crisis more efficiently.
Our findings will provide valuable information to policy makers to understand the level of preparedness and response plan and could be a baseline to establish a transparent and fair assessment of managing this disease.
Introduction
On 30th January 2020, the World Health Organization (WHO) declared the outbreak of coronavirus disease (COVID-19) a public health emergency of international concern and later in March 2020, as a global pandemic [1, 2]. From mid-March to end of April 2020, Malaysia was faced with a life-threatening crisis in combating COVID-19 and the situation has been increasingly difficult. COVID-19 is an outbreak that the world has never encountered before which became pandemic in just a short span of time. As of 18th April 2020, 2,164,588 people had been infected worldwide, with 146,188 deaths [3]. Meanwhile, the number of positive cases in Malaysia had increased to 5305 with 88 deaths [4]. In order to reduce the spread of the disease, the Government of Malaysia implemented the Movement Control Order, a ‘partial lockdown’ throughout the country from March 18th, 2020, to May 12th, 2020. This movement restrictions order had managed to flatten the trajectory of the epidemic and reduce some pressure off the health care services. As of 20th May 2020, the number of confirmed cases in Malaysia was 7009 cases with 114 deaths [4].
With the new virus spreading globally, governments must take due responsibility to ensure the ability of its health system to manage a public health response and provide adequate medical care during this crisis. For this purpose, each country is encouraged to plan its preparedness and response actions considering that all countries are at risk and will need to respond to COVID-19. The National Crisis Preparedness and Response Centre (CPRC) under the Ministry of Health (MOH) Malaysia was activated on the 5th January 2020, even prior to the WHO announcement that the virus was a global health emergency [5]. As a guide to initiate a rapid emergency response, the government adopted the National Influenza Pandemic Preparedness Plan (NIPPP) developed in 2006 that comprises of a comprehensive response to influenza pandemic. An efficient outbreak response management can have a major impact on the outcome of the pandemic. The number of infected cases and deaths in a country during this outbreak, and the rate at which they increase depend highly on the preparedness and robustness of health system of a country. While we learn that the virus can spread rapidly and the outbreak can grow at an exponential rate, there is a need to assess the situation and response appropriately to the COVID-19 disease. Hence in February 2020, the WHO established a strategic preparedness and response plan for COVID-19 which aims to slow and stop transmission, prevent outbreaks and delay spread, provide optimized care for all patients (especially the serious ill cases), and minimize the potential impact of the epidemic on health systems, social services, and economic activity [6].
Recent months following the outbreak reveals that the COVID-19 pandemic has evolved rapidly and exerted an extensive strain on healthcare systems in many countries. During public health emergency, enhanced surveillance, contact tracing and quarantine are of high importance in the early stages to contain the spread in the community. Through surveillance and contract tracing activities, positive COVID-19 cases are promptly identified and effectively isolated to receive appropriate infection prevention and control measures, and supportive medical care. These interventions play a crucial role in mitigating a community - wide epidemic, by 1) delaying the exponential growth of the infection, 2) reducing the number of cases, and 3) spreading the demand of health services over time to meet the capacity of hospitals [7]. In terms of patient care, there is a growing concern regarding the capability of the health systems to respond promptly and effectively to the needs of COVID-19 patients, who may require intensive care. The dramatic increase in patients, particularly those with severe illness that needs critical care facilities, may overwhelm the system’s ability to handle such cases, resulting in shortages of medical supplies, infrastructure, and health care workers. Based on a prediction model reported by JP Morgan, Malaysia would reach its peak at around 6300 infected cases by mid-April 2020 [8]. In order to manage the increasing number of COVID-19 cases in Malaysia, the MOH has made available 926 units of ventilators in Intensive Care Units (ICU), 152 non-invasive ventilators and 142 transport ventilators. Additionally, 40 hospitals with a total of 6917 beds have been allocated to treat COVID-19 patients, with 410 beds in ICUs and some 634 ventilators readily available to the MOH [9]. Despite such numbers looking better than most other countries, the demand may exceed current resources needed to limit onward transmission. The challenge of resource scarcity especially during an epidemic requires re-prioritisation of current resources for effective allocation and distribution across the country. This highlights the importance of assessing the performance of health system in managing COVID-19 that may reflect the preparedness and response level of the country.
Economic efficiency analysis is commonly used to measure how resources are allocated in the best way to produce outputs or service delivery. Data Envelopment Analysis (DEA) allows measure of efficiency by comparing the use of inputs to produce outputs among the units. This tool is advantageous as no specific targets are predetermined particularly during this period when knowledge about the disease is still limited. This type of benchmarking exercise is a well-established tool that could potentially be used to measure health response and evaluate preparedness success. Recent papers have reviewed the performance of healthcare in developed and developing countries (e.g. Chen et al. [10] for Taiwan; Chitnis and Mishra [11] for India; Giménez et al., [12] for Mexico; Giménez et al. [13] for Columbia; Hamzah and See [14] for Malaysia; Mastromarco et al. [15] for Czech Republic; Li and He [16], Li et al. [17], Liu et al. [18] and Shen and Valdmanis [19] for China), however a gap using a more comprehensive measurement to assess performance of health systems in managing public health crisis is still evident. To date, no study on efficiency analysis during a pandemic crisis has been performed. The two operations of community surveillance and medical care to mitigate and manage COVID-19 pandemic involves networks that are connected through interactions that transfer information and workflow for health systems to achieve the outcome of treating infected patients. Therefore, this study provides additional insights on efficiency measurement of each COVID-19 responses that are essential for opportunities to improve performance, productivity and patient care. In this study, we propose a conceptualization model of COVID-19 response as a network consisting of three sub processes: i) community surveillance, ii) medical care I and iii) medical care II.
The objective of this study is to investigate the relative efficiency level of the three sub-processes of managing COVID-19 in Malaysia health system using a network DEA (NDEA) model. The remainder of the paper is organized as follows. Section 2 briefly describes the research methodology and Section 3 highlights the findings of this study. Finally, Section 4 discusses the interpretation and concludes the paper.
Method and data
Network data envelopment analysis
DEA was firstly introduced by Charnes et al. [20] and had been successfully utilized to assess the relative performances of a set of comparable decision-making units (DMUs). In some application areas, it is generally known that the DMU may perform different processes with shared input resources among those operations. The presence of shared resources requires modification of the multi-stages production structure [21] to accommodate the division of shared resources among the various processes. To illustrate, Cook et al. [22] derived a measure of performance that included the level of the bank branch, and also the sales and service components within the bank branch. Nevertheless, real world applications typically involve both desirable and undesirable outputs. Furthermore, DMUs tend to be heterogeneous, operating in different operation environment. Non-discretionary factors also have an important role in production applications [23]. For example, in COVID-19 prevention and treatment performance assessment, an output indicator related to recovery cases of COVID-19 would represent as having more output to better performance, and in different example, output indicator related to the number of cumulative deaths would suggests less output corresponds to better performance. The number of positive cases will differ among the Malaysian states depending on the number of people placed in quarantine stations and the number of incidence rate per 100,000 populations. Ultimately, for a better measurement, performance analyses will need to control for these non-discretionary factors. A revised three-stage NDEA model is proposed that will result in an undistorted efficiency measure. A significant feature of a three-stage production system is that it contains shared input resources, undesirable intermediates and final outputs. A correlation between non-discretionary factors and efficiency is also included.
Assume that there are J DMUs denoted by DMUj(j = 1, ⋯, J) in which the first stage uses inputs to produce some desirable outputs, while the second stage will primarily deal with these desirable outputs as inputs to produce following desirable outputs with some undesirable by-products, then those desirable and undesirable outputs from the second stage become inputs to the third stage to produce desirable and undesirable final outputs. Parts of these inputs are discretionary inputs only to stage 1 and stage 3, while some discretionary inputs are used or shared as inputs in stage 1 and 2, or shared as inputs among stage 1, 2 and 3; the other non-discretionary inputs act as environmental factors. and represents the specific input to DMUj at stage 1 and stage 3, respectively. represents the non-discretionary factors to DMUj at stage 1. represents shared inputs between stage 1 and stage 2, we assume that all are divided into and , β1 + β2 = 1; represents shared inputs between stage 1, stage 2 and stage 3, we assume that all are divided into , and , α1 + α2 + α3 = 1. represents intermediate outputs from the first stage, which then become inputs to the second stage. and refers to desirable and undesirable intermediate outputs from the second stage which then become inputs to the third stage. and represents the desirable and undesirable final outputs to DMUj at stage 3, respectively.
Re-depict
The objective of the three-stage network structure is to identify the DMU that produces the largest values of outputs with the lowest values of undesirable outputs using the least amounts of specific and shared inputs under the influence of an external operating environment beyond the control of management. The efficiency scores are computed using mathematical programming. The three-stage NDEA model for calculating the efficiency of a DMU is shown below:
| 1 |
s.t
System constraints:
| 2 |
Stage 1 constraints:
| 3 |
Stage 2 constraints:
| 4 |
Stage 3 constraints:
| 5 |
| 6 |
| 7 |
The three stages in a weighted average of efficiency scores of stages 1, 2 and 3 are as follows:
where w1, w2 and w3 are weights endogenously derived from the mathematical programming such that w1 + w2 + w3 = 1. This definition ensures that a DMU is overall efficient if and only if each stage is efficient [24]. Similar to Chen et al. [24], we define
The above model is non-linear, however Cook et al. [22] had demonstrated that the above three-stage NDEA model can be linearized to a linear program and provides an overall or aggregate measure of performance across all sub-components. After making changes to the variables, the above model can be converted to a linear program.
For in depth view of the production with undesirable products and ways to control the undesirable production issues, the methods to handle undesirable intermediate outputs and final outputs in a NDEA model can be seen in Wu et al. [25], and Lozano [26]. Due to the influence of external operating environment on the ability of a DMU to transform inputs into outputs, a measure of managerial efficiency that controls for exogenous features of the operating environment is required. Non-discretionary factors were first introduced by Banker and Morey [23], and further modification by Golany and Roll [27] was performed to account for both non-discretionary inputs and non-discretionary outputs simultaneously from the Banker and Morey [23] approach. For more information on how to simultaneously consider both undesirable products and non-discretionary factors into the measurement of network structure efficiencies for the DMUs, the reader may want to refer to those papers mentioned.
Data
Malaysia state-level data were extracted from secondary data sources which include variables such as total number of confirmed cases, death cases and recovered cases. Most data are available in the MOH (http://covid-19.moh.gov.my) and State Health Department websites (accessed on 10th April 2020). The variables used for each process are further described in the next section.
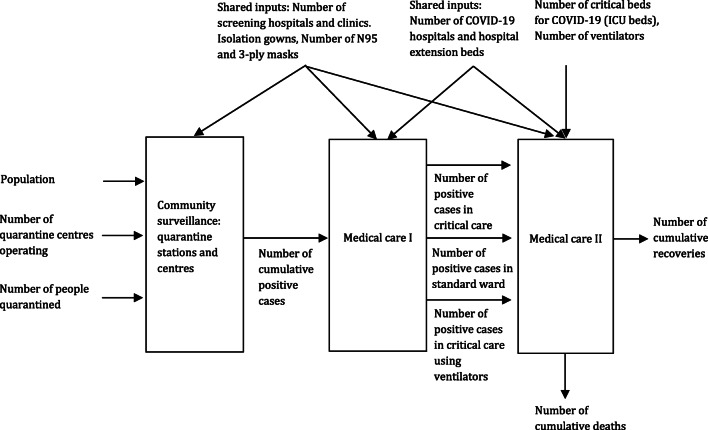
As described earlier, public health and healthcare system must act as a team to contain COVID-19 as effectively as possible by means of assisting surveillance, early detection, case isolation, contact tracing and case management [28]. Figure 1 illustrates the first process i) community surveillance that represents the public health measures, and subsequent two processes ii) medical care I and medical II that represents the clinical management of the disease. Further explanation of each process and variables used are as below:
Fig. 1.
Diagram of the NDEA model for community surveillance and medical care sub processes in managing COVID-19 disease
Community surveillance
The main objective of public health measures is to prevent the spread of the disease from person-to-person by separating them to interrupt the transmission. Case isolation and quarantine are perhaps the most critical steps. Isolation is the separation of ill persons with contagious diseases from non-infected individuals to protect them, and usually takes place in hospital settings [29]. Quarantine means the movement restriction of individuals who are presumed to have been exposed to a contagious disease but may not be ill, either because they are not infected or are still in the incubation period [29]. All quarantine individuals are monitored, and if any symptoms present, they are immediately isolated and transferred to assigned health care facilities. The inputs used for this process are 1) number of designated quarantine centres across each states and 2) cumulative number of people quarantined. The total quantity of personal protective equipment (PPE) (e.g., face masks, isolation gowns) and number of screening centres are considered as shared inputs with medical care process. The intermediate output between community surveillance and medical care is the number of positive cases. In this process, the population size for each state is used as a proxy for environmental factor. This would imply that a higher population size will lead to higher positive cases.
Medical care I
This process represents the initial phase whereby patients with positive cases detected from community surveillance activity are isolated and transferred to receive clinical care in the hospital setting. Some hospitals were transformed into either full ‘COVID’ hospitals that would be able to treat a large number of COVID-19 patients; or hybrid hospitals, whereby certain beds are allocated for COVID-19 cases while still providing safe urgent care for non-COVID-19 patients. In addition, extension hospitals transformed from identified facilities are available to cater for low risk cases requiring treatment. The desirable intermediate output is patients remaining in the standard ward while the undesirable intermediate outputs are patients requiring transfer to critical care units with or without use of ventilators.
Medical care II
Medical care II represents the remaining positive cases receiving treatment and patients that progresses to intensive care requiring admission to critical care unit and use of mechanical ventilation. The number of positive cases being treated and number of cases with patients in critical care unit with or without the use of ventilator are intermediates between the medical care processes. In other words, these variables are considered as inputs together with number of critical care beds and number of ventilators dedicated for COVID-19 cases. The desirable and undesirable outputs are number of recoveries and number of cumulative deaths, respectively.
Results and discussion
A total of 13 states and 3 federal territories in Malaysia were included in the analysis. The descriptive statistics and network efficiency results are presented according to the state population density: 1) low density states of less than 100 per km2 2) medium density states between 100 and 500 per km2 and 3) high density states of more than 500 per km2. This would be followed by the network efficiency results for overall, community surveillance, medical care I and medical care II processes.
Descriptive statistics
The descriptive statistics of selected input and output measures are summarised in Table 1. For community surveillance process, low density states had the highest population size, followed by high density and medium density categories, although wide variations were observed in the low and medium density categories. The population size corresponds with the number of quarantine centres and people under quarantine. The descriptions are expected as higher population size area would need larger capacities to accommodate higher volume of people. The average number of cumulative positive cases detected was highest in the high-density category. This result was also expected as evidence has shown that higher population density area can increase the rate of infections, however results in existing studies tend to be mixed [30].
Table 1.
Descriptive statistics of selected input and output variables
| Activity | Type of variable | Variable | ALL N = 15 |
Low N = 4 |
Medium N = 6 |
High N = 5 |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Community surveillance | Specific inputs | Number of quarantine centres operating | 9 | 8 | 17 | 9 | 5 | 5 | 6 | 6 |
| Number of people quarantined | 645 | 750 | 783 | 195 | 407 | 763 | 656 | 1117 | ||
| Non-discretionary input | Population in million (2019) | 2105.43 | 1659.84 | 2409.13 | 1195.67 | 1787.90 | 1279.29 | 2333.25 | 2879.18 | |
| Medical care II | Specific inputs | Number of critical beds for COVID-19 (ICU beds) | 28 | 27 | 33 | 20 | 22 | 15 | 31 | 49 |
| Number of ventilators | 54 | 31 | 60 | 19 | 50 | 28 | 54 | 54 | ||
| Desirable output | Number of cumulative recoveries | 128 | 201 | 58 | 34 | 119 | 78 | 232 | 393 | |
| Undesirable output | Number of cumulative deaths | 4 | 4 | 4 | 6 | 5 | 4 | 3 | 4 | |
| Community surveillance - > Medical care I | Desirable intermediate 1–2 | Number of cumulative positive cases | 282 | 300 | 210 | 92 | 214 | 171 | 340 | 521 |
| Medical care I - > Medical care II | Desirable intermediate 2–3 | Number of positive cases continue receiving medical care | 144 | 174 | 143 | 77 | 86 | 89 | 96 | 116 |
| Undesirable intermediate 2–3 | Number of positive cases in critical care | 6 | 8 | 5 | 7 | 5 | 3 | 8 | 15 | |
| Number of positive cases in critical care using ventilators | 3 | 4 | 4 | 5 | 3 | 3 | 4 | 7 | ||
| Shared resources | Shared inputs 1–3 | Number of screening hospitals and clinics | 33 | 31 | 71 | 33 | 21 | 14 | 19 | 22 |
| Isolation gowns | 1600 | 1513 | 1642 | 805 | 1173 | 662 | 2098 | 2924 | ||
| N95 masks | 2590 | 1684 | 2962 | 1566 | 2184 | 1569 | 2196 | 1959 | ||
| 3-ply masks | 23,954 | 16,115 | 27,661 | 13,126 | 25,218 | 20,467 | 20,262 | 16,800 | ||
| Shared inputs 2–3 | Number of COVID-19 hospitals and extension centres beds | 522 | 483 | 650 | 343 | 354 | 217 | 595 | 891 | |
For medical care process, similar trends were observed, with higher average values of screening centres and hospital beds in low density category. With higher number of facilities, this category would require more personal protective gears. Likewise, the average number of critical care beds and ventilators were higher in low density category. However, we observed that low density category had a lower average use of N95 masks compared to the other categories. In addition, the average number of screening centres and the use of 3-ply masks were lower in high density category compared to medium density category. The average number of positive cases that continue receiving medical care, labelled as desirable output in the first stage, was higher in low density category followed by high and medium density categories. For undesirable intermediates, high density category had a higher average number of patients requiring transfer to critical care units whereas similar observations were seen in critical care patients requiring ventilators across categories. On the other hand, we found that the average number of recoveries as the desirable output were higher in high density category followed by low and medium categories. In the case of undesirable output, high density category had a lower number of deaths followed by low and medium density categories.
NDEA model results
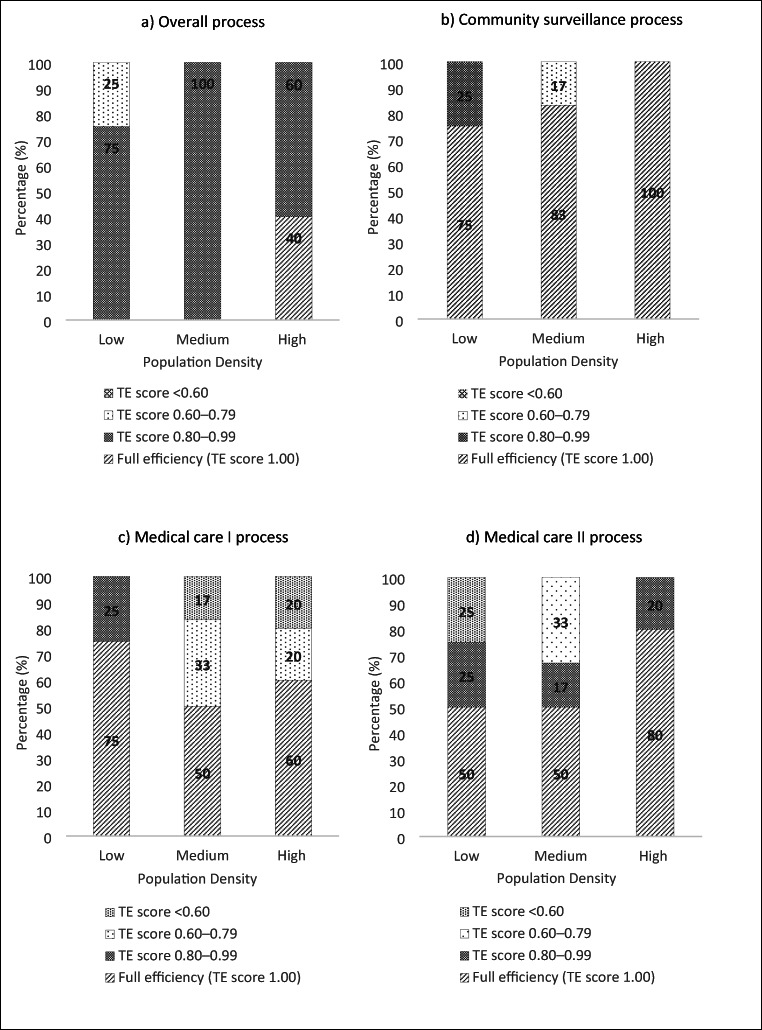
Table 2 shows the average efficiency scores and the distribution levels of the efficiency scores: i) full efficiency (TE score of 1.00) followed by ii) TE score of 0.80–0.99 (good), iii) TE score of 0.60–0.79 (average), and iv) TE score below 0.60 (poor). For all-states result, the overall efficiency showed majority had good level of performance. By exploring the efficiency scores of the sub-processes, the distance differences from the efficient frontier between community surveillance and medical care processes, on average, are relatively small indicating fairness of resource allocation in both processes across the states in Malaysia. In terms of state level self-assessment, we observed that for several states, overall efficiency is greatly influenced by the inefficiency of the medical care rather than the community surveillance process. This average score of medical processes were lower as some states were in the average and poor efficiency categories compared to community surveillance process —indicating that community surveillance, medical care (stage 1) and medical care (stage 2) need to improve their efficiency levels by 2%, 12% and 15%, respectively.
Table 2.
Average efficiency results for overall, community surveillance, medical care I and medical care II services
| Technical efficiency (TE) | Overall efficiency | Community surveillance (Stage 1) | Medical care I (Stage 2) |
Medical care II (Stage 3) |
|
|---|---|---|---|---|---|
| TE score, Mean (SD) | 0.91 (0.06) | 0.98 (0.07) | 0.88 (0.18) | 0.85 (0.20) | |
| Full efficiency (TE score 1.00), % (n) | 13.3 (2) | 86.7 (13) | 60.0 (9) | 60.0 (9) | |
| TE score 0.80–0.99, % (n) | 80.0 (12) | 6.7 (1) | 6.7 (1) | 20.0 (3) | |
| TE score 0.60–0.79, % (n) | 16.7 (1) | 6.7 (1) | 20.0 (3) | 13.3 (2) | |
| TE score <0.60, % (n) | – | – | 13.3 (2) | 6.7 (1) | |
Table 3 presents the results by population density categories. For overall efficiency, high density category had the highest average score, followed by low and medium categories. In terms of distribution levels, the higher density category had states in the good efficiency level whereas low density category had one state in the poor efficiency level. For community surveillance, the high-density category had higher mean efficiency scores, due to states in this category having full efficiency scores. The other categories had almost similar average scores; however medium density category had slightly lower average score due to one state being in the moderate efficiency level.
Table 3.
Average efficiency results for overall, community surveillance, medical care I and medical care II subprocess in low, medium and high population density states
| Technical efficiency (TE) | Overall efficiency | Community surveillance (Stage 1) |
Medical care I (Stage 2) |
Medical care II (Stage 3) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | Low | Medium | High | Low | Medium | High | Low | Medium | High | |
| TE score, Mean (SD) | 0.92 (0.09) | 0.90 (0.03) | 0.94 (0.07) | 0.97 (0.06) | 0.96 (0.10) | 1.00 | 0.98 (0.04) | 0.84 (0.21) | 0.86 (0.22) | 0.85 (0.20) | 0.91 (0.14) | 0.97 (0.08) |
| Full efficiency (TE score 1.00), % (n) | – | – | 40 (2) | 75 (3) | 83 (5) | 100 (5) | 75 (3) | 50 (3) | 60 (3) | 50 (2) | 50 (3) | 80 (4) |
| TE score 0.80–0.99, % (n) | 75 (3) | 100 (6) | 60 (3) | 25 (1) | – | – | 25 (1) | – | – | 25 (1) | 17 (1) | 20 (1) |
| TE score 0.60–0.79, % (n) | 25 (1) | – | – | – | 17 (1) | – | – | 33 (2) | 20 (1) | – | 33 (2) | – |
| TE score <0.60, % (n) | – | – | – | – | – | – | – | 17 (1) | 20 (1) | 25 (1) | – | – |
For medical care I process, low density category had higher average efficiency scores. This can be explained due to higher desirable output which is the number of positive cases remaining in medical care and lower desirable output of number of positive cases that progress to critical care. However, for medical care II process, high density category had the highest average efficiency score due to higher average number of recoveries with lower number of deaths at the current resources. Low density category had the lowest mean efficiency scores, with one state in poor efficiency level which contributed to the overall efficiency score.
The findings of these processes imply that the medium density category could better improve their efficiency levels for community surveillance, medical care I and medical care II processes by approximately 4%, 16% and 9%, respectively. Meanwhile the efficiency level for medical care I and medical care II for high density category could be improved by approximately 14% and 3%, respectively.
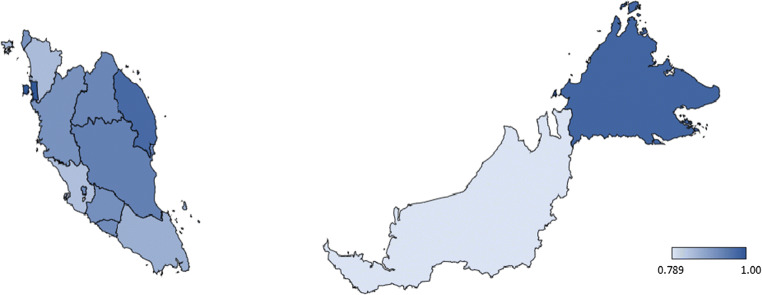
In summary, the findings showed that the high density category performed well in community surveillance and medical care II processes. Meanwhile, low density category performed better in the medical care I process. These results are also presented graphically as shown in Figs. 2 and 3.
Fig. 2.
Map of Malaysia states representing the overall efficiency score
Fig. 3.
Efficiency score distribution levels by population density (low, medium and high) for a overall b community surveillance c medical care I and d medical care II processes
Policy discussions
The results confirmed that the performance gap in managing COVID-19 crisis across all states in Malaysia is relatively small reflecting the remarkable job by the Malaysian government in pandemic preparedness and response planning. Meanwhile, fair allocation of government resources is one of the critical success factors in managing COVID-19 crisis more efficiently. The results represent a period whereby detected cases were at 3-digit numbers involving cluster community, and the number of patients receiving treatment were at its peak.
Several reasons may contribute to the overall level of preparedness of Malaysia to mitigate and manage the outbreak. One main reason is the structure of centralized commanding authorities at different levels that helps to implement coherent strategies involving many stakeholders. At the highest level is the Prime Minister’s Department through the National Disaster Management Agency Malaysia which is the focal point in managing disasters. The top leaders of the country have made major trade-off decisions on the economic and social restrictions. The Movement Control Order as a mitigation strategy, through Prevention and Control of Infectious Diseases Act 1988 and the Police Act 1967, involves limited operation of essential businesses only, closing of international borders and prohibition of non-essential travel and public gatherings. This allows MOH that is entrusted to control the pandemic to improve the health system capacity and focus on contract tracing, isolation and managing care of patients. At the same time, Malaysians returning from abroad must go through a 14-day self-quarantine at designated locations across the country. Supporting agencies such as the National Security Council headed by the Minister of Defense helps to ensure the enforcement of the Movement Control Order. Emergency contingency funding were disbursed from the Ministry of Finance necessary to procure and maintain national stockpiles of PPEs, antivirals and other emergency supplies and equipment. Other initiatives include joint efforts between the Ministry of Science, Technology, and Innovation (MOSTI), Ministry of Higher Education and MOH to increase capacity of diagnostic labs. This governance structure ensures an all government unified approach with a common purpose that is centered on public health crisis. Furthermore, effective communications on decisions undertaken by the government and awareness campaigns has made public compliance possible.
Malaysia also learns from its previous experiences of managing infectious diseases such as (Severe Acute Respiratory Syndrome (SARS), Pandemic Influenza 2009, Middle East Respiratory Syndrome (MERS-CoV), Avian Influenza, Zika and Nipah virus enabling a speedy primary health care response. The learning experiences from these outbreaks has strengthened the core public health functions as well as many key health systems areas such as the health workforce, service delivery, information and technology system, as well as leadership and governance to support a more resilient health system. In addition, historically Malaysian health system priorities were to improve the maternal, infant and child health including communicable diseases. This foundation of the Malaysian health system created a widespread and integrated public healthcare delivery system, distributed across the country including remote and rural areas that is universal and low cost. Malaysia has a dual public-private healthcare system in which provision of public health services are mainly from MOH with central administration. This allows mobilization of appropriate resources from national to state levels to support response at the facilities. To further demonstrate, each health state department that oversees the health services within their states will bring forth their requirements for additional healthcare personnel and medical supplies to the central department. The central department plans for rapid deployment of surge personnel from other states and purchase supplies centrally, and channelled these resources back to the state health departments for implementation at the local level. For instance, during a global shortage of PPEs, the MOH was quick to set up a central online reporting and database system accessible at different level of administrators for monitoring of different types of PPEs stock levels [31]. This report is closely monitored for purchase stock mobilization and distribution of PPEs donated by the public where needed. This coordination highlights the importance of having a public healthcare system supported by government during a public health crisis, at least here in Malaysia.
Findings revealed that high density states outperformed other states due to lesser input resources used to produce better outcomes. This is probably due to better network coordination between healthcare facilities, better infrastructure and transport systems, and availability of experts that leads to efficient use of resources, as this category includes 3 federal territories and 3 west coast states that are mainly urban areas. As illustrated in Fig. 2, the lightly shaded areas represent states that did not performed well in comparison to other states. These are mainly several states in Malaysia that are considered as medium density category in the analysis. This performance level may be explained due to these few states were the earliest worse hit areas involving multiple clusters between end of February and Mid-March 2020. For example, Selangor state had by far the largest cluster from a religious gathering held in 10th March 2020 involving 19,000 local and international participants [32]. Most of the participants went back to their respective states, which also falls in the low and medium density states. This cluster contributed to 48% of total number of COVID-19 cases in Malaysia [33]. Likewise, Sarawak state also had a cluster involving its religious gathering while handling imported clusters from other states [34]. During this period, Malaysia was the worst hit country in Southeast Asia which prompted the government to implement the Movement Control Order (MCO). Death cases were mainly attributable to late presentation to health care facility and patient comorbidities.
Preparation is key, and it should be a major lesson to be learned from COVID-19 pandemic response. Malaysia had earlier published a document on the strategy for emerging disease and public health emergencies to further enhance its public health response and preparedness strategies [35]. Malaysia also complies with the International Health Regulations (IHR 2005) [36] and through reviewing experiences, simulation exercises, and evaluation of IHR 2005 core capacities requirements, has built a strategic and multi-sectoral work plan for implementation. This was evident through a 2019 global health security index study that has rated Malaysia in the 18th place among 195 countries, for its overall readiness to face a disease outbreak, based on its capabilities to prevent, detect and respond to an epidemic, including its overall health system, risk management and compliance with international norms [37].
Our analysis demonstrates the potential strategic role of performance assessment to guide for the efficient and effective planning of scarce resources to fight the pandemic. We believe that our findings will provide valuable information to policy makers to understand the level of preparedness and response plan across Malaysia and could be a baseline to establish a transparent and fair assessment of managing this disease. The information can be substantially utilized to determine appropriate countermeasures in areas that face challenges in their response level. For example, we observed that more resources are available in low density areas that have larger population size, compared to high density areas with slightly lower population size. We believe that preparedness plan and response actions in the case of COVID-19 should consider population density in the distribution of resources. More resources should be reallocated to densely populated areas from low density areas without reducing its current performance. Overall, resource allocation during this challenging period was found to be distributed effectively. As a result, good practices can be identified from efficient peers to further improve overall performance, subsequently their preparedness and response level. For example, Sungai Buloh Hospital in the Selangor state made renovations to accommodate over 2000-bedded patients from an old hospital next door from its actual 900-bedded capacity [38]. The management levels also identified daycare centres and operating theatres that could be converted to ICU beds in case the hospital ICUs gets overwhelmed [38]. In the situation of procuring additional ventilators, when manufacturers were unable to meet the surge in demand, the managers decided to approach private hospitals to lend ventilators to them [38].
There are few limitations in the analysis that should be mentioned here. Human resource capacity is not captured in the study due to unavailability of data. Community surveillance activity requires large manpower to perform contract tracing that is labor intensive, hence data on healthcare workers would be an important variable to include in the future. In light of the spread of the disease, population age plays an important role as the elderly mortality seems to be higher compared to younger patients [39]. Hence, we hope that population characteristics adjustment could be addressed in the medical care process for more accurate measurement. It is also important to note that cross sectional data were used in the analysis and we hope that time series data would be useful to observe the changes as response level to the pandemic shifts rapidly. Few other measurements may offer better accuracy, for example, information on the capacity of quarantine centres instead of total number of quarantine centres. Admittedly, we take note that outbreaks occurred at different time periods in certain states and we hope future research can incorporate time period adjustment to better measure the response level. Due to small number of cross-sectional units, the study made use of available data to examine network structure efficiencies for Malaysia health system. We hope that future work can incorporate second stage of analysis to identify the efficiency determinants of Malaysia health system in dealing with COVID-19. It would be of interest to conduct further analysis using either bootstrap truncated regression or other regression models if the possibility to acquire micro-level data arises in the future.
Conclusions
In summary, Malaysia had successfully flattened the trajectory curve during an uncertain time and performed well in mitigating and managing the COVID-19 crisis that can be benchmarked to other countries. At the time of writing, it is still unclear whether and to what extent, Malaysia will be able to retain its early performance in managing COVID-19 crisis. Despite some limitations, the network efficiency measurement demonstrated in this study reflects the preparedness and response level of managing the pandemic.
Acknowledgements
The authors would like to thank the Director General of Health Malaysia for the permission to publish this paper. We appreciate the support of Dr. Rozita Halina Tun Hussein for her comments on the draft version of this manuscript. The corresponding author thanks the Malaysia Productivity Corporation’s Research Grant on Productivity Development and Implementation (304/PJJAUH/6501035/M141) and the Fulbright Visiting Scholar Award for the possibility of being under research attachment in the United States for the period when part of this research was conducted. We also would like to dedicate our work to frontline workers that helps keep us safe. All the remaining errors are the responsibility of the authors.
Author’s contributors
NMH collated the data and drafted the manuscript. MMY and KFS developed the network structure DEA model, performed the data analyses and edited the manuscript. All authors read and approved of the manuscript.
Funding information
The funding body had no role in the design of the study, data collection, analysis, or interpretation of the data.
Data availability
Data are available upon reasonable request and permission from the Ministry of Health Malaysia.
Compliance with ethical standards
Conflict of interest
We declare no competing interests.
Ethical approval
This study was registered with the National Medical Research Registry [NMRR-20-1060-55,031 (IIR)] and approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia.
Footnotes
Nurhafiza Md Hamzah and Ming-Miin Yu are Co-first author
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO (2020) Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed 20 May 2020
- 2.WHO (2020) WHO director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020. Accessed 20 May 2020
- 3.WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/. Accessed 20 May 2020
- 4.MOH (2020) COVID-19 Latest information. http://covid-19.moh.gov.my/terkini/042020/situasi-terkini-18-april-2020 . Accessed 20 May 2020
- 5.News Straits Times. Health Ministry rejects claim of being 'late' in tackling coronavirus crisis. https://www.nst.com.my/news/nation/2020/02/562044/health-ministry-rejects-claim-being-late-tackling-coronavirus-crisis. Accessed 20 May 2020
- 6.World Health Organization (2020) 2019 Novel Coronavirus (2019-nCoV): Strategic Preparedness And Response Plan. https://www.who.int/publications-detail/strategic-preparedness-and-response-plan-for-the-new-coronavirus. Accessed 1 April 2020
- 7.Chen ATC, Moniz CMV, Ribeiro-Júnior U, Diz MDPE, Salvajoli JV, Da Conceição Vasconcelos KGM, Auler-Júnior JOC., Cecconello I., Abdala E. and Hoff PMG (2020) How should health systems prepare for the evolving COVID-19 pandemic? Reflections from the perspective of a Tertiary Cancer Center. Clinics 75, e1864 [DOI] [PMC free article] [PubMed]
- 8.JP Morgan (2020) COVID-19 update add Malaysia to the Asia infection curve. Asia Pacific Equity Research 23 March 2020 (Unpublished)
- 9.The Edge Markets (2020) Health Ministry places order for 800 new ventilators for Covid-19 treatment. https://www.theedgemarkets.com/article/health-ministry-places-order-800-new-ventilators-covid19-treatment. Accessed 18 March 2020
- 10.Chen KC, Chen HM, Chien LN, Yu MM. Productivity growth and quality changes of hospitals in Taiwan: does ownership matter? Health Care Manag Sci. 2019;22(3):451–461. doi: 10.1007/s10729-018-9465-3. [DOI] [PubMed] [Google Scholar]
- 11.Chitnis A, Mishra DK. Performance efficiency of Indian private hospitals using data envelopment analysis and super-efficiency DEA. J Health Manag. 2019;21(2):279–293. doi: 10.1177/0972063419835120. [DOI] [Google Scholar]
- 12.Giménez V, Keith JR, Prior D. Do healthcare financing systems influence hospital efficiency? A metafrontier approach for the case of Mexico. Health Care Manag Sci. 2019;22(3):549–559. doi: 10.1007/s10729-019-9467-9. [DOI] [PubMed] [Google Scholar]
- 13.Giménez V, Prieto W, Prior D, Tortosa-Ausina E. Evaluation of efficiency in Colombian hospitals: an analysis for the post-reform period. Socio Econ Plan Sci. 2019;65:20–35. doi: 10.1016/j.seps.2018.02.002. [DOI] [Google Scholar]
- 14.Hamzah NM, See KF. Technical efficiency and its influencing factors in Malaysian hospital pharmacy services. Health Care Manag Sci. 2019;22(3):462–474. doi: 10.1007/s10729-019-09470-8. [DOI] [PubMed] [Google Scholar]
- 15.Li B, Mohiuddin M, Liu Q. Determinants and differences of township hospital efficiency among Chinese provinces. Int J Environ Res Public Health. 2019;16(9):1601. doi: 10.3390/ijerph16091601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li SK, He X. The impacts of marketization and subsidies on the treatment quality performance of the Chinese hospitals sector. China Econ Rev. 2019;54:41–50. doi: 10.1016/j.chieco.2018.10.007. [DOI] [Google Scholar]
- 17.Liu W, Xia Y, Hou J. Health expenditure efficiency in rural China using the super-SBM model and the Malmquist productivity index. Int J Equity Health. 2019;18(1):111. doi: 10.1186/s12939-019-1003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mastromarco C, Stastna L, Votapkova J. Efficiency of hospitals in the Czech Republic: conditional efficiency approach. J Prod Anal. 2019;51(1):73–89. doi: 10.1007/s11123-019-00543-y. [DOI] [Google Scholar]
- 19.Shen Z, Valdmanis V. Identifying the contribution to hospital performance among Chinese regions by an aggregate directional distance function. Health Care Manag Sci. 2019;23:142–152. doi: 10.1007/s10729-019-09482-4. [DOI] [PubMed] [Google Scholar]
- 20.Charnes A, Cooper WW, Rhodes E. Measuring the efficiency of decision making units. Eur J Oper Res. 1978;2(4):429–444. doi: 10.1016/0377-2217(78)90138-8. [DOI] [Google Scholar]
- 21.Kao C, Hwang SN. Efficiency decomposition in two-stage data envelopment analysis: Anapplication to non-life insurance companies in Taiwan. Eur J Oper Res. 2008;185(1):418–429. doi: 10.1016/j.ejor.2006.11.041. [DOI] [Google Scholar]
- 22.Cook WD, Hababou M, Tuenter HJH. Multicomponent efficient measurement and shared inputs in data envelopment analysis: an application to sales and service performance in bank branches. J Prod Anal. 2000;14:209–224. doi: 10.1023/A:1026598803764. [DOI] [Google Scholar]
- 23.Banker RD, Morey RC. The use of categorical variables in data envelopment analysis. Manag Sci. 1986;32:1613–1627. doi: 10.1287/mnsc.32.12.1613. [DOI] [Google Scholar]
- 24.Chen Y, Du J, David Sherman H, Zhu J. DEA model with shared resources and efficiency decomposition. Eur J Oper Res. 2010;207(1):339–349. doi: 10.1016/j.ejor.2010.03.031. [DOI] [Google Scholar]
- 25.Wu J, Zhu Q, Chu J, Liang L. Two-stage network structures with undesirable intermediate outputs reused: a DEA based approach. Comput Econ. 2015;46(3):1–23. [Google Scholar]
- 26.Lozano S. Technical and environmental efficiency of a two-stage production and abatement system. Ann Oper Res. 2015;27(2):1–21. [Google Scholar]
- 27.Golany B, Roll Y. Some extensions to techniques to handle non-discretionary factors in data envelopment analysis. J Prod Anal. 1993;4:419–432. doi: 10.1007/BF01073549. [DOI] [Google Scholar]
- 28.Winter G. COVID-19 and emergency planning. British J Commun Nurs. 2020;25(4):184–186. doi: 10.12968/bjcn.2020.25.4.184. [DOI] [PubMed] [Google Scholar]
- 29.Wilder-Smith, A., & Freedman, D. O. (2020). Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of travel medicine, 27(2), taaa020 [DOI] [PMC free article] [PubMed]
- 30.Li R, Richmond P, Roehner BM. Effect of population density on epidemics. Physica A: Statistic Mech Appl. 2018;510:713–724. doi: 10.1016/j.physa.2018.07.025. [DOI] [Google Scholar]
- 31.The Edge Markets. Health Ministry no longer facing PPE shortage. https://www.theedgemarkets.com/article/health-ministry-no-longer-facing-ppe-shortage. (Accessed 16 November 2020)
- 32.New Straits Times. How Sri Petaling tabligh became Southeast Asia's Covid-19 hotspot. https://www.nst.com.my/news/nation/2020/03/575560/how-sri-petaling-tabligh-became-southeast-asias-covid-19-hotspot. (Accessed 3 June 2020)
- 33.New Straits Times. Tabligh cluster now responsible for almost half of Covid-19 cases in Malaysia. https://www.nst.com.my/news/nation/2020/05/593922/tabligh-cluster-now-responsible-almost-half-covid-19-cases-malaysia. (Accessed 3 June 2020)
- 34.The Borneo Post. Covid-19: Sarawak’s latest death linked to Kuching church gathering cluster, says Health DG. https://www.theborneopost.com/2020/04/09/covid-19-sarawaks-latest-death-linked-to-kuching-church-gathering-cluster-says-health-dg/ (Accessed 3 June 2020)
- 35.Ministry of Health Malaysia Malaysia Strategy for Emerging Diseases and Public Health Emergencies (MYSED) II Workplan (2017-2021). https://www.moh.gov.my/moh/resources/Penerbitan/Garis%20Panduan/Pengurusan%20KEsihatan%20&%20kawalan%20pykit/MySED_II.pdf. Accessed 4 April 2020
- 36.World Health Organization (2008) International health regulations (2005) Third Edition. World Health Organization
- 37.2019 GHS Index Global Health Security Index. https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf. Accessed 4 May 2020
- 38.From the Desk of the Director-General of Health Malaysia. The Malaysian response to COVID-19: Building preparedness for ‘surge capacity’, testing efficiency and containment. https://kpkesihatan.com/2020/06/16/the-malaysian-response-to-covid-19-building-preparedness-for-surge-capacity-testing-efficiency-and-containment/. Accessed 16 Nov 2020
- 39.Liu K, Chen Y, Lin R, Han K (2020) Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. Journal of Infection 80(6):14–18 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request and permission from the Ministry of Health Malaysia.