Abstract
Objective
To estimate differences in emergency contraception (EC) use, access, and counseling by rural-urban residence among reproductive age women in the United States.
Study design
We examined respondent data (2006–2017) from the National Survey of Family Growth for women ages 15-44 (n = 28,448) to estimate EC use, access, and counseling by rural-urban county of residence. Rural-urban prevalence ratios for EC outcome measures were estimated using predicted margins from logistic regression models, which were adjusted for demographic differences and current contraceptive method use. Changes in ever-use of EC over time were estimated for rural and urban respondents, separately, using Chi-square tests and trends were estimated using inverse variance weighted linear regression models.
Results
During 2006 to 2017, 10% of rural and 19% of urban women who had ever had sex reported ever using EC pills. Among rural women, ever-use increased from 6% in 2006-2008 to 15% in 2015-2017 (Chi-square p < 0.01; trend p-value < 0.01); among urban women, ever-use increased from 11% to 27% (Chi-square p < 0.01; trend p-value < 0.01). Rural and urban women were similarly likely to have obtained EC without a prescription and from a drug store. Rural women were less likely to have received EC counseling than urban women; however, counseling rates were low among all women.
Conclusion
We observed differences in EC ever-use and receipt of EC counseling by rural-urban residence among US women ages 15 to 44, adding to the evidence that rural-urban residence is an important factor in reproductive health. More research is needed to explore factors contributing to rural-urban differences in EC use.
Implications
Our key finding that EC use varied by rural-urban county residence offers additional evidence that rural-urban residence should be considered in reproductive health practice and policy. We discuss areas for future research into potential barriers to EC use in rural populations.
Keywords: Contraceptive counseling, Emergency contraception, Reproductive health, Rural health
1. Introduction
Access to effective contraception is critical in preventing unintended pregnancies, which account for almost half of all pregnancies in the United States (US) [1]. In cases where usual contraception methods fail, are used incorrectly, or are not used at all, emergency contraception (EC) can be used after intercourse to prevent pregnancy. Timely access to and accurate knowledge of EC can be especially important for rural women, who are more likely to experience an unintended pregnancy resulting in a live birth as compared with urban women [2]. Recent regulatory changes have aimed to increase the availability of EC, and EC use has increased since the early 2000s among US women overall [3,4], but research on rural-urban differences in trends in EC use and access has been limited.
EC is currently available in the US in pill form over-the-counter as levonorgestrel (LNG) and by prescription as ulipristal acetate (UPA), or through the insertion of a copper intrauterine device (IUD). LNG, though less effective than UPA or the copper IUD, is the most widely used form of EC [5]. LNG is sold without age restriction in pharmacies throughout the US in generic and brand name form (e.g., Plan B One-Step) [5]. LNG and UPA are also available to order online, and some websites offer online telehealth consultations for UPA prescriptions.
As EC has become more available, the percentage of US women who report ever using EC pills has increased, from 4% in 2002 to 20% in 2015 (among those who had ever had sexual intercourse) [4]; however, barriers to access remain [6,7]. Studies examining rural-urban differences in EC access have mostly focused on pharmacy availability using provider surveys or “mystery caller” approaches, and have covered limited geographic areas [7], [8], [9]. No known prior studies have examined the association between rural-urban residence and history of EC use in a nationally representative sample of US women.
This study estimated the association between rural-urban residence and measures of EC use, access, and counseling: ever-use of EC pills, number of times EC has been used, where and how EC is obtained, and receipt of EC counseling. We also examined changes in EC use from 2006 to 2017, a time period where access to EC was greatly expanded: first with US Food and Drug Administration approval of LNG for over-the-counter purchase by those age 18 and older in 2006, then with the Patient Protection and Affordable Care Act (ACA) contraceptive mandate that private insurers cover EC with no out-of-pocket cost in 2012, and finally with the removal of age restrictions for over-the-counter purchases of LNG in 2013 [10].
2. Materials and methods
2.1. Study population
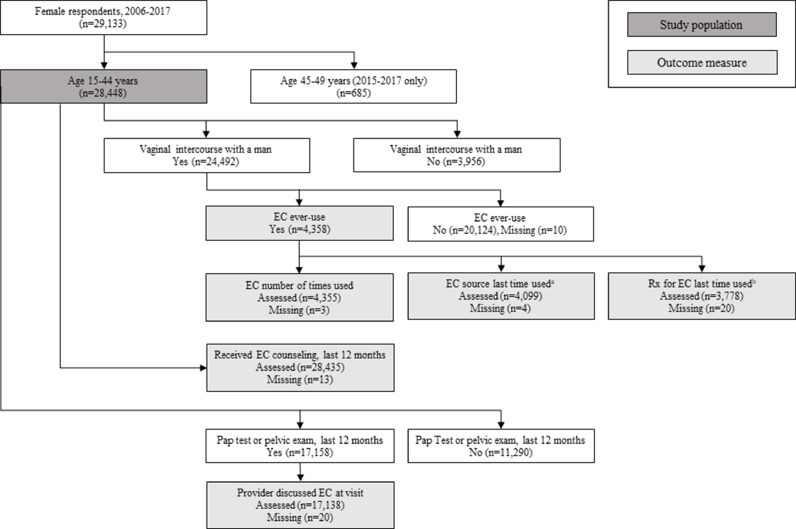
This study analyzed publicly available female respondent data from the National Survey of Family Growth (NSFG) for the 2006-2010, 2011-2013, 2013-2015, and 2015-2017 survey periods (n = 29,133). The NSFG is a nationally representative in-person household survey of the non-institutionalized reproductive age US population. Surveys covered topics related to relationships, family life, pregnancy, and reproductive health, including contraceptive use [11]. We restricted our analysis to female respondents 15 to 44 years old at the time of the interview. The final study population included 28,448 women (Fig. 1).
Fig. 1.
Study population selection criteria, National Survey of Family Growth, 2006-2017
EC = emergency contraception.
aQuestion introduced in year 2 of 2006-2010 survey.
bQuestion introduced in year 3 of 2006-2010 survey.
2.2. Study variables
2.2.1. Rural-urban status
The NSFG categorized respondents’ addresses at the time of the interview into a 3-level county-based measure of rurality in accordance with the Office of Management and Budget classification [12]. To create the dichotomous rural-urban variable for our study, we considered participants living in either a county containing a principal city of Metropolitan Statistical Area (MSA) or other MSA to be urban, and those living in a county without an MSA to be rural.
2.2.2. Emergency contraception measures
The NSFG collected several items related to EC use, access, and counseling. Women who reported ever having had vaginal intercourse with a man were asked about lifetime ever-use of EC pills [13]. Valid response options were yes or no. Respondents who reported EC use were asked a series of follow up questions about EC use and access. For EC number of times used, we categorized responses as once, twice, or 3 or more times, consistent with the NSFG key statistic categorization [4]. We categorized responses as to where EC was last obtained (added in year 2 of the 2006-2010 survey cycle) into 4 groups: Doctor's office (including health maintenance organization); community or family planning clinic; drug store or in-store clinic; and other (hospital or emergency room, urgent care facility, employer or school-based clinic, mail order/internet, friend, partner/spouse, or other). Whether respondents received a prescription for EC the last time they used it (added in year 3 of the 2006-2010 survey cycle) was categorized as either yes or no.
We also examined rural-urban differences in receipt of EC counseling. The NSFG asked all female survey respondents if they received counseling or information about EC pills in the last year, regardless of sexual history [13]. Respondents who received a Pap test or pelvic exam in the last year (regardless of sexual history) were asked if their doctor or health care provider talked to them about using EC pills at that visit [13]. For each measure, responses were categorized as either yes or no. For all EC outcome measures, we recoded responses of refused or don't know (generally <1% of respondents) as missing.
2.2.3. Respondent characteristics
Our analysis included the following respondent demographic characteristics: age, race/Hispanic origin, income as a percentage of poverty level, highest educational level attained, current insurance status, and current religion. Because the study population included teenagers and young adults, we categorized women who reported their highest educational level attainment as less than a Bachelor's degree and also reported being in school at the time of the interview as “still in school”. We included current religious affiliation as a characteristic in our analysis because religious beliefs may influence choices around contraceptive use [14]. We also included several characteristics related to sexual and reproductive health that were used by the NSFG to determine eligibility for the EC use and counseling questions: sexual history (ever had vaginal intercourse with a man) and whether the respondent received a Pap test or pelvic exam in the last year [12]. We examined current contraceptive method, which could have affected receipt of EC counseling in the past year, and because of known rural-urban differences in type of contraception method use [15].
2.3. Statistical analysis
To estimate the association between rural-urban residence and measures of EC use and access, we first conducted a descriptive analysis, tabulating the distribution of respondent characteristics by rural-urban residence. We then used logistic regression to calculate rural-urban predicted prevalence ratios (PR) and 95% confidence intervals (CI). We ran unadjusted models, and then ran models adjusted for age, race/Hispanic origin, education, poverty, current health insurance, current religion, and current contraceptive method. We also estimated linear trends in the prevalence of EC ever-use over time in rural and urban women, separately, using inverse variance weighted linear regression. We used Chi-square tests to estimate differences in EC ever-use prevalence between rural and urban respondents within each of the 4 survey cycles, and between the first and last survey periods within each residency group. p-values ≤ 0.05 were considered statistically significant. We conducted analyses with SAS 9.4 (SAS Institute, Cary, North Carolina) and SUDAAN 11.0 (RTI International, Research Triangle Park, North Carolina) using survey procedures and population weights. The University of Southern Maine Institutional Review Board determined the study to be exempt from review.
3. Results
3.1. Respondent characteristics
Table 1 presents respondent characteristics at the time of the NSFG interview by rural-urban residence. Approximately 17% of respondents lived in a rural county at the time of the interview. A greater proportion of rural respondents was white, had income below the poverty level, and was Medicaid-insured or uninsured compared with their urban counterparts. More rural than urban women reported sterilization or LARC as their current contraceptive method (35% vs 26%).
Table 1.
Characteristics of female respondents ages 15-44 (n = 28,448), by rural-urban residence, National Survey of Family Growth, 2006-2017
| Characteristics at the time of interview | Rural | Urban |
|---|---|---|
| No. of participants, (%, SE) | 4253 (16.9, 1.3) | 24,195 (83.1, 1.3) |
| Age, in years, mean (SE) | 29.5 (0.2) | 29.6 (0.1) |
| Race/Hispanic origin, % (SE) | ||
| Non-Hispanic White | 73.3 (3.0) | 54.5 (1.2) |
| Non-Hispanic Black | 8.9 (1.9) | 14.7 (0.7) |
| Hispanic | 8.2 (1.3) | 21.1 (1.1) |
| Non-Hispanic other/multiple race | 9.5 (3.0) | 9.7 (0.4) |
| Education, % (SE) | ||
| Still in school (high school or college) | 23.6 (1.4) | 24.8 (0.5) |
| Less than high school | 9.9 (0.9) | 8.9 (0.4) |
| High school or GED | 29.1 (1.1) | 19.9 (0.5) |
| Some college | 21.8 (1.0) | 17.9 (0.4) |
| Bachelor's degree or higher | 15.7 (1.1) | 28.5 (0.8) |
| Income as a percentage of poverty level, % (SE) | ||
| Less than 100% | 29.9 (1.4) | 24.2 (0.6) |
| 100–199% | 25.8 (1.1) | 21.7 (0.4) |
| 200–399% | 30.1 (1.3) | 31.1 (0.5) |
| More than 400% | 14.3 (1.1) | 23.0 (0.7) |
| Insurance coverage, % (SE) | ||
| Private insurance or Medi-Gap | 53.6 (2.0) | 62.1 (0.9) |
| Medicaid, CHIP, or state-sponsored plan | 20.1 (1.1) | 17.0 (0.6) |
| Medicare, military health care, or other government health care | 3.4 (0.8) | 4.1 (0.4) |
| Single-service plan, Indian Health Service, or no coverage | 22.9 (1.8) | 16.8 (0.6) |
| Religion, % (SE) | ||
| No religion | 19.5 (1.5) | 20.8 (0.7) |
| Catholic | 15.1 (1.4) | 24.6 (0.8) |
| Protestant | 59.8 (2.3) | 45.3 (0.9) |
| Other religiona | 5.7 (1.7) | 9.4 (1.0) |
| Current contraceptive method, % (SE) | ||
| Sterilization/LARC | 34.9 (1.4) | 26.0 (0.5) |
| Moderately effective methodsb | 21.3 (0.9) | 20.1 (0.4) |
| Less effective methodsc | 11.0 (0.7) | 16.3 (0.4) |
| No method, sex in past 3 months | 6.6 (0.5) | 7.6 (0.3) |
| No method, not at risk for unintended pregnancyd | 26.3 (1.0) | 30.1 (0.6) |
| Ever had vaginal intercourse with a man, % (SE) | 89.4 (0.7) | 86.4 (0.5) |
| Pap test or pelvic exam, last 12 months, % (SE) | 60.9 (1.6) | 60.4 (0.6) |
CHIP, Children's Health Insurance Program; GED, General Educational Development; LARC, long-acting reversible contraception; SE, standard error.
Notes: Percentages are weighted to the population level using weights provided in the NSFG. Sample Ns are unweighted. Results in bold are significant at p < 0.05.
Other religion includes: Jewish, LDS/Mormon, Jehovah's Witness, Unitarian-Universalist, Greek Orthodox, other Orthodox, Muslim, Buddhist, Hindu, Native American religions, Taoic religions, Neopagan religions, or other.
Moderately effective methods include: injectable, patch, ring, birth control pill.
Less effective methods include: diaphragm, condom, withdrawal, or other less effective.
Not at risk for pregnancy includes respondents who are: pregnant, seeking pregnancy, postpartum, infecund, or those who have not had sex in the last 3 months.
3.2. Emergency contraception ever-use, number of times used, and source
During 2006-2017, 17% of women who had ever had vaginal intercourse with a man reported ever-use of EC pills. EC use varied by rural-urban residence (Table 2), with 10% of rural women reporting EC use, compared with 19% of urban women (PR = 0.56, 95% CI: 0.46, 0.66); this association remained after we adjusted for potential confounders (PR = 0.64, 95% CI: 0.55, 0.74). Rural EC users were more likely to have only used EC once and less likely to have used EC 3 or more times compared with urban women. We found no association between rural-urban residence and whether women used a prescription to obtain EC (approximately 20% for each group) or the source of EC at the last time of reported use. Roughly half of rural and urban women reported obtaining EC from a drug store the last time they used it.
Table 2.
The association between rural-urban residencea and measures of emergency contraception use and counseling among female respondents ages 15-44 (n = 28,448), National Survey of Family Growth, 2006-2017
| Rural | Urban | Rural vs. Urban | |||
|---|---|---|---|---|---|
| Emergency contraception use and counseling measures | Respondents assessed n | Prevalence % (SE) | Prevalence % (SE) | Unadjusted prevalence ratioa (95% CI) | Adjusted prevalence ratioa,b (95% CI) |
| Ever used EC pillsc | 24,482 | 10.4 (0.9) | 18.7 (0.5) | 0.56 (0.46, 0.66) | 0.64 (0.55, 0.74) |
| EC times usedd | 4,355 | ||||
| Once | 66.5 (2.7) | 54.4 (1.3) | 1.22 (1.12, 1.34) | 1.19 (1.09, 1.31) | |
| Twice | 21.6 (2.5) | 25.2 (1.0) | 0.86 (0.67, 1.09) | 0.88 (0.70, 1.12) | |
| Three or more times | 11.9 (2.0) | 20.3 (1.1) | 0.59 (0.41, 0.83) | 0.62 (0.43, 0.89) | |
| Source of EC last time usedd,e | 4,099 | ||||
| Doctor's office | 6.1 (1.3) | 9.0 (0.7) | 0.68 (0.43, 1.07) | 0.79 (0.49, 1.27) | |
| Community or family planning clinic | 30.9 (4.4) | 27.3 (1.4) | 1.13 (0.84, 1.52) | 1.04 (0.76, 1.42) | |
| Drug store or in-store clinic | 54.3 (4.0) | 54.6 (1.6) | 0.99 (0.85, 1.17) | 1.02 (0.87, 1.19) | |
| Otherf | 8.7 (1.8) | 9.2 (0.8) | 0.95 (0.60, 1.48) | 0.96 (0.60, 1.53) | |
| Prescription for EC last time usedd,g | 3,778 | 20.2 (3.2) | 21.5 (1.2) | 0.94 (0.67, 1.32) | 0.99 (0.72, 1.36) |
| Received EC counseling in the last year | 28,435 | 1.8 (0.3) | 3.2 (0.2) | 0.57 (0.40, 0.81) | 0.59 (0.40, 0.88) |
| Doctor discussed EC during Pap/Pelvic exam in the last yearh | 17,138 | 7.7 (0.8) | 9.8 (0.4) | 0.78 (0.62, 0.98) | 0.86 (0.70, 1.07) |
CI, confidence interval; EC, emergency contraception; SE, standard error.
Notes: Percentages are weighted to the population level using weights provided in the NSFG. Sample Ns are unweighted. Results in bold are significant at p < 0.05.
Prevalence estimates excluding missing observations for the following EC measures: ever used EC (n = 10), EC times used (n = 3), source of EC last time used (n = 4), prescription for EC last time used (n = 20), received EC counseling in the last year (n = 13), and doctor discussed EC during Pap/Pelvic exam in the last year (n = 20).
Urban residence was used as the reference group.
Models were adjusted for age, race/Hispanic origin, education, poverty level, health insurance coverage, religion, and current contraceptive method.
Among women who reported ever having vaginal intercourse with a man.
Among women who reported ever using EC pills.
This question was added to the NSFG interview in year 2 of 2006-10 survey cycle.
Other includes: Hospital or emergency room, urgent care facility, employer or school-based clinic, mail order/internet, friend, partner/spouse, other.
This question was added to the NSFG interview in year 3 of 2006-10 survey cycle.
Among women who reported having a Pap test or pelvic exam in the last 12 months.
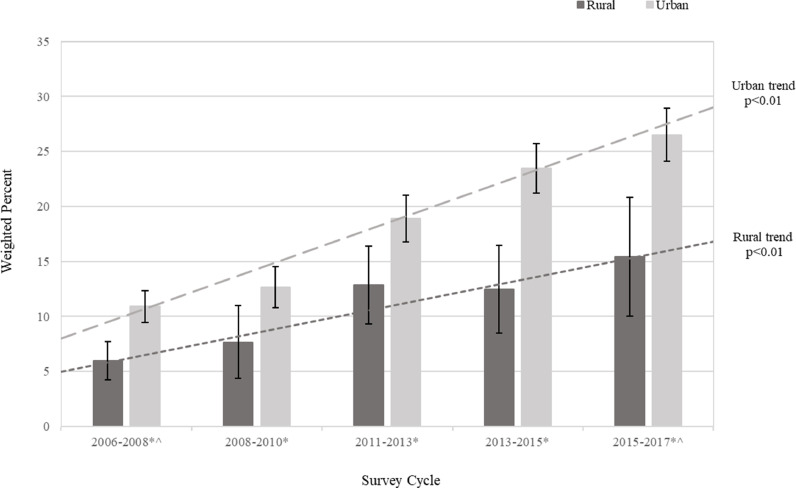
Across the 4 survey cycles included in our study, the percentage of women reporting ever-use of EC increased in both rural and urban populations (Fig. 2); the linear trend was significant among both rural and urban residents (trend p-values < 0.01). Among rural women, prevalence of EC ever-use increased from 6% in 2006-2008 to 15% in 2015-2017 (Chi-square p-value < 0.01). In urban women, EC ever-use increased from 11% in 2006-2008 to 27% in 2015-2017 (Chi-square p-value < 0.01). Prevalence of ever-use among rural respondents was lower than among urban respondents in each time period (each Chi-square p-value < 0.05).
Fig. 2.
Ever-use of emergency contraception pills (percentage and 95% confidence interval) by rural-urban residence among female respondents ages 15-44 who have ever had vaginal intercourse with a man, National Survey of Family Growth, 2006-2017
*Rural vs. urban comparison Chi-square p-values < 0.05.
^Rural and urban 2006-2008 vs 2015-2017 comparison Chi-square p-values <0.01.
3.3. Receipt of emergency contraception counseling and information
Rural and urban respondents reported low rates of EC counseling (2% and 3%, respectively), as shown in Table 2. Compared with urban residents, rural women were significantly less likely to have received counseling on EC in the last year in our unadjusted model (PR = 0.57, 95% CI: 0.40, 0.81) and adjusted model (PR = 0.59, 95% CI: 0.40, 0.88). Rural women were also less likely than urban women to have had a doctor discuss EC with them at their last Pap test or pelvic exam in the unadjusted model (8% vs 10%, PR = 0.78, 95% CI: 0.62, 0.98); however, the association was no longer significant after adjusting for respondent characteristics.
4. Discussion
In a nationally representative sample of reproductive age women, we observed increasing use of EC pills among rural and urban residents, with prevalence of EC ever-use more than doubling in each group from 2006-2008 to 2015-2017. These findings reflect an overall increase in EC use during a period in which the federal government enacted several policies aimed at improving access to EC pills [3,16] and suggest that these efforts have expanded access for both rural and urban populations. EC ever-use was lower among rural compared with urban women across the study period, however, even after controlling for rural-urban demographic differences and current contraceptive method use.
It is unclear whether lower use of EC by rural women is a function of preference or barriers to access. Availability of EC does not appear to differ between rural and urban pharmacies [7], [8], [9], and our findings suggest that rural and urban women obtain EC in similar ways (i.e., from a drug store and without a prescription). However, disparities in health care access [17] may limit EC access for rural women. Furthermore, given that rural populations have lower incomes and higher rates of uninsurance than urban residents [17], rural women may be particularly sensitive to out-of-pocket EC costs. We found that EC obtained by prescription, which is the primary way insurance policies cover this medication, represents a small portion (approximately 20%) of actual EC use.
The NSFG does not include questions about perceived need for or willingness to use EC, so it is possible that rural-urban differences in EC use reflect differences in these underlying factors. In particular, privacy concerns may be heightened in rural places, where patients may perceive, or experience, more barriers to patient confidentiality [18]. Concern for privacy and fear of embarrassment has been identified by female college students as a barrier to EC use [19], and by rural adolescents seeking sexual health services [20].
Our findings also highlight the need for improved counseling on EC. Rural women were less likely than urban women to have received counseling on EC, and overall prevalence of EC counseling was low among all women, consistent with previous research [16,21]. In rural areas, low prevalence of EC counseling may be coupled with other barriers to accessing information on contraception and reproductive health. These include rural disparities in adolescents’ receipt of formal sex education [22] and women's awareness of family planning services [23].
Telehealth services, such as direct-to-consumer “telecontraception” models offering online contraceptive counseling, digital consultations for prescription EC, and home delivery (e.g., Wisp, Nurx) have the potential to improve rural access to EC and may also help to address possible confidentiality concerns. However, age restrictions, insurance coverage constraints, and varying state regulations may limit telehealth access for some populations [24], in addition to rural-specific barriers such as limited broadband access [25]. More research is needed to evaluate the impact of telehealth contraceptive services on rural populations and to inform effective and targeted messaging of such services for underserved rural communities.
Our study has several limitations. Respondent characteristics reflect those at the time of the interview, and may not reflect characteristics at the time of EC use or counseling. Respondent self-report, especially regarding questions about lifetime use, could lead to misclassification of EC measures, potentially introducing bias. The NSFG assessment of EC ever-use does not include the copper IUD, resulting in an undercount of EC ever-use. Furthermore, EC access in our study only included women who had used EC; we were unable to estimate the percentage of women who sought EC pills but were unable to obtain them. Though frequently used to differentiate rural and urban places, MSAs are a relatively crude measure of rurality and may mask important rural-urban distinctions within counties [26]. In addition, further analyses stratified by current method use were not feasible given the small sample size of rural women and the low prevalence of many of our EC measures.
Our study found that although EC use increased overall during 2006-2017, women living in rural areas were less likely to have used EC pills or to have received counseling on EC compared with urban women. Our findings contribute to knowledge about rural women's access to the full range of contraceptive options and add to the evidence that rural-urban residence is a distinguishing factor in reproductive health. Policies and programs to reduce unintended pregnancy and enhance reproductive autonomy, including telehealth and direct-to-consumer contraceptive services, should include ways to close the rural-urban disparities gap. More research is needed to explore factors contributing to rural-urban differences in EC use.
Footnotes
Funding statement: Katherine Ahrens is supported by a faculty development grant from the Maine Economic Improvement Fund.
Declaration of competing interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Finer L.B., Zolna M.R. Declines in unintended pregnancy in the United States, 2008-2011. N Engl J Med. 2016;374:843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sutton A., Lichter D.T., Sassler S. Rural-urban disparities in pregnancy intentions, births, and abortions among US adolescent and young women, 1995-2017. Am J Public Health. 2019;109:1762–1769. doi: 10.2105/AJPH.2019.305318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels K., Jones J., Abma J. Use of emergency contraception among women aged 15-44: United States, 2006-2010. NCHS Data Brief. 2013:1–8. [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Key statistics from the National Survey of Family Growth: Emergency contraception. Available from: https://www.cdc.gov/nchs/nsfg/key_statistics/e.htm#emergency; 2017. [Accessed: March 11, 2020].
- 5.Haeger K.O., Lamme J., Cleland K. State of emergency contraception in the U.S., 2018. Contracept Reprod Med. 2018;3:20. doi: 10.1186/s40834-018-0067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilkinson T.A., Clark P., Rafie S., Carroll A.E., Miller E. Access to emergency contraception after removal of age restrictions. Pediatrics. 2017;140:1–5. doi: 10.1542/peds.2016-4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uysal J., Tavrow P., Hsu R., Alterman A. Availability and accessibility of emergency contraception to adolescent callers in pharmacies in four southwestern states. J Adolesc Health. 2019;64:219–225. doi: 10.1016/j.jadohealth.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 8.Chuang C.H., Shank L.D. Availability of emergency contraception at rural and urban pharmacies in Pennsylvania. Contraception. 2006;73:382–385. doi: 10.1016/j.contraception.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Samson F.D., Loren R., Downing N., Schroeppel S., Kelly P.J., Ramaswamy M. Availability of emergency contraception in rural and urban pharmacies in Kansas. J Rural Health. 2013;29:113–118. doi: 10.1111/j.1748-0361.2012.00429.x. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser Family Foundation. Emergency contraception. Available from: https://www.kff.org/womens-health-policy/fact-sheet/emergency-contraception/; September 6, 2018. [Accessed: April 30, 2020].
- 11.National Center for Health Statistics. About the National Survey of Family Growth. Available from: https://www.cdc.gov/nchs/nsfg/about_nsfg.htm. [Accessed: June 17, 2020].
- 12.National Center for Health Statistics. Public-use data file documentation: 2015-2017 National Survey of Family Growth user's guide. Hyattsville, MD; 2018 December.
- 13.National Center for Health Statistics. 2015-2017 NSFG questionnaires. Available from: https://www.cdc.gov/nchs/nsfg/nsfg_2015_2017_questionnaires.htm#female; 2018. [Accessed: June 25, 2020].
- 14.Hill N.J., Siwatu M., Robinson A.K. “My religion picked my birth control”: The influence of religion on contraceptive use. J Relig Health. 2014;53:825–833. doi: 10.1007/s10943-013-9678-1. [DOI] [PubMed] [Google Scholar]
- 15.Daniels K., Martinez G.M., Nugent C.N. Urban and rural variation in fertility-related behavior among U.S. Women, 2011-2015. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 16.Kavanaugh M.L., Williams S.L., Schwarz E.B. Emergency contraception use and counseling after changes in United States prescription status. Fertil Steril. 2011;95:2578–2581. doi: 10.1016/j.fertnstert.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Rural health. Available from: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/rural-health.htm; 2019. [Accessed: October 19, 2020].
- 18.Nelson W., Pomerantz A., Howard K., Bushy A. A proposed rural healthcare ethics agenda. J Med Ethics. 2007;33:136–139. doi: 10.1136/jme.2006.015966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hickey M.T., White J. Female college students' experiences with and perceptions of over-the-counter emergency contraception in the United States. Sex Reprod Healthc. 2015;6:28–32. doi: 10.1016/j.srhc.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Elliott B.A., Larson J.T. Adolescents in mid-sized and rural communities: Foregone care, perceived barriers, and risk factors. J Adolesc Health. 2004;35:303–309. doi: 10.1016/j.jadohealth.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 21.McCall-Hosenfeld J.S., Weisman C.S. Receipt of preventive counseling among reproductive-aged women in rural and urban communities. Rural Remote Health. 2011;11:1617. [PMC free article] [PubMed] [Google Scholar]
- 22.Lindberg L.D., Maddow-Zimet I., Boonstra H. Changes in adolescents' receipt of sex education, 2006-2013. J Adolesc Health. 2016;58:621–627. doi: 10.1016/j.jadohealth.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yarger J., Decker M.J., Campa M.I., Brindis C.D. Rural-urban differences in awareness and use of family planning services among adolescent women in California. J Adolesc Health. 2017;60:395–401. doi: 10.1016/j.jadohealth.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 24.Weigel G., Frederiksen B., Ranji U., Salganicoff A. Kaiser Family Foundation; San Francisco, CA: November 2019. Telemedicine in sexual and reproductive health. [Google Scholar]
- 25.Perrin A. Digital gap between rural and nonrural America persists. Available from: https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/; 2019. [Accessed: November 5, 2020].
- 26.Bennett K.J., Borders T.F., Holmes G.M., Kozhimannil K.B., Ziller E. What is rural? Challenges and implications of definitions that inadequately encompass rural people and places. Health Aff (Millwood) 2019;38:1985–1992. doi: 10.1377/hlthaff.2019.00910. [DOI] [PubMed] [Google Scholar]