Key Points
Question
What is the association between telestroke capacity and care patterns and outcomes for patients with acute ischemic stroke?
Findings
In this study including 153 272 patients treated for stroke, those who received care at hospitals with telestroke capacity had higher rates of reperfusion treatment and lower 30-day mortality compared with those treated at hospitals without telestroke. Increases in reperfusion treatment were largest in smaller hospitals, among rural residents, and among patients 85 years and older.
Meaning
Patients who present to hospitals with telestroke capacity were more likely to receive reperfusion treatment and have lower mortality.
This study describes differences in care patterns and outcomes among patients with acute ischemic stroke who present to hospitals with and without telestroke capacity.
Abstract
Importance
Telestroke is increasingly used in hospital emergency departments, but there has been limited research on its impact on treatment and outcomes.
Objective
To describe differences in care patterns and outcomes among patients with acute ischemic stroke who present to hospitals with and without telestroke capacity.
Design, Setting, and Participants
Patients with acute ischemic stroke who first presented to hospitals with telestroke capacity were matched with patients who presented to control hospitals without telestroke capacity. All traditional Medicare beneficiaries with a primary diagnosis of acute ischemic stroke (approximately 2.5 million) who presented to a hospital between January 2008 and June 2017 were considered. Matching was based on sociodemographic and clinical characteristics, hospital characteristics, and month and year of admission. Hospitals included short-term acute care and critical access hospitals in the US without local stroke expertise. In 643 hospitals with telestroke capacity, there were 76 636 patients with stroke who were matched 1:1 to patients at similar hospitals without telestroke capacity. Data were analyzed in July 2020.
Main Outcomes and Measures
Receipt of reperfusion treatment through thrombolysis with alteplase or thrombectomy, mortality at 30 days from admission, spending through 90 days from admission, and functional status as measured by days spent living in the community after discharge.
Results
In the final sample of 153 272 patients, 88 386 (57.7%) were female, and the mean (SD) age was 78.8 (10.4) years. Patients cared for at telestroke hospitals had higher rates of reperfusion treatment compared with those cared for at control hospitals (6.8% vs 6.0%; difference, 0.78 percentage points; 95% CI, 0.54-1.03; P < .001) and lower 30-day mortality (13.1% vs 13.6%; difference, 0.50 percentage points; 95% CI, 0.17-0.83, P = .003). There were no differences in days spent living in the community following discharge or in spending. Increases in reperfusion treatment were largest in the lowest-volume hospitals, among rural residents, and among patients 85 years and older.
Conclusions and Relevance
Patients with ischemic stroke treated at hospitals with telestroke capacity were more likely to receive reperfusion treatment and have lower 30-day mortality.
Introduction
Reperfusion treatment for acute ischemic strokes via thrombolysis or thrombectomy reduces disability associated with acute ischemic stroke by restoring blood flow.1,2,3,4,5,6,7,8 Time to return of blood flow is critical; for every minute that a stroke goes untreated, an estimated 1.9 million brain cells die, and shorter door-to-needle times are associated with decreased mortality.9,10,11 The decision on whether to administer reperfusion treatment is both time-sensitive and complex, as a clinician must rule out conditions that mimic stroke, identify contraindications to treatment, and appraise the expertise at the local hospital vs the logistics and timing of a transfer to a tertiary center. While some hospitals have around-the-clock stroke expertise to rapidly evaluate patients with potential stroke, many do not. The lack of on-site expertise likely contributes to lower rates of reperfusion treatment among eligible patients and worse outcomes.12,13,14
Telestroke can extend stroke expertise to hospitals without on-site stroke expertise. A telestroke consultation is a real-time videoconference between the patient, remotely located stroke specialist, and a bedside health care professional in the emergency department (ED).15,16,17,18 The remote stroke expert can interview and examine the patient, review brain imaging, determine candidacy for thrombolysis or thrombectomy, assess the need for transfer, and recommend other treatments, including secondary stroke prevention. The potential benefits of telestroke capacity at the local hospital could extend beyond individual consultations via improved education and better ties to certified stroke centers. Telestroke has becoming increasingly common; roughly 30% of all hospital EDs in the US now use telestroke technology.19,20,21
Despite increasing use of telestroke, there have been few clinical studies assessing the impact of telestroke and, to our knowledge, no broad assessment of its impact on care patterns and outcomes. A major barrier has been the inability to accurately identify which hospitals have telestroke capacity or which patients had a telestroke consultation in administrative data, such as insurance claims.22 Important prior studies have generally focused on hospitals from a single program. One study from Germany examined stroke admissions in 5 telestroke hospitals from 2003 to 2005 and found that telestroke capacity was associated with increased rates of thrombolysis and had a beneficial impact on a composite measure of patient outcomes.23 A 2019 study24 from the US compared care at 4 telestroke hospitals with controls and found no difference in thrombolysis or mortality. Limitations of prior studies include smaller sample size and comparisons of telestroke with in-person stroke consultations, and most were conducted before thrombectomy was recommended for acute ischemic stroke in 2015.25
To advance knowledge on the impact of telestroke, we identified a national sample of US hospitals that lacked on-site stroke expertise and compared the care of patients with stroke who first presented at 643 hospitals that had introduced telestroke capacity vs those who first presented at control hospitals that remained without stroke expertise on site or via telestroke. Our primary outcomes were receipt of reperfusion treatment through thrombolysis with alteplase or thrombectomy, mortality at 30 days from admission, spending at 90 days, and functional status as measured by days spent living in the community after discharge.
Methods
Overview
Our analyses focused only on patients presenting to a hospital without on-site stroke expertise. Among these hospitals, we matched patients with acute ischemic stroke who presented to a hospital who recently introduced telestroke capacity to control patients who presented to a hospital without telestroke. Matching was done 1:1 using both hospital and patient characteristics. Patients were categorized based on the first ED or hospital where they received care. Our outcomes are based on all care the patient received regardless of whether this care was provided at the presenting site or, if there was a transfer, at another hospital. Our subgroup analyses compared patients and hospitals with similar characteristics (eg, comparing telestroke hospitals with low stroke volume with control hospitals with low stroke volume). Our study was approved by the institutional review board at Harvard Medical School where patient consent to use their data was waived because it was deidentified and presented no additional risks in terms of patient privacy and protection.
Study Population
Using 100% Medicare Inpatient and Outpatient Standard Analytic Files, we identified all acute stroke admissions in the US within the traditional fee-for-service Medicare program from January 2008 to June 2017. Admissions included inpatient or outpatient ED/observation stays in any short-term acute care or critical access hospital with a primary diagnosis for acute ischemic stroke (International Classification of Diseases, Ninth Revision [ICD-9] codes 433.X [except 433.10], 434.X and 43625; ICD-10 codes I63-I66 [except I65.2] and I67.89) (eTable 1 in the Supplement). For patients with multiple, contiguous claims for stroke at the same hospital or across different hospitals, we consolidated their claim records into a single admission. For example, if a patient with stroke was cared for in the ED of one hospital, then transferred and admitted to another hospital, those different claims were combined into a single admission episode that was classified based on the first hospital where they received care. We limited our sample to the first stroke admission per patient observed over the study period. We extracted demographic characteristics (age, sex, race/ethnicity, residential zip code), Medicare enrollment data (original entitlement reason, monthly parts A and B status, eligibility for Medicaid), and chronic condition information from the Master Beneficiary Summary Files.
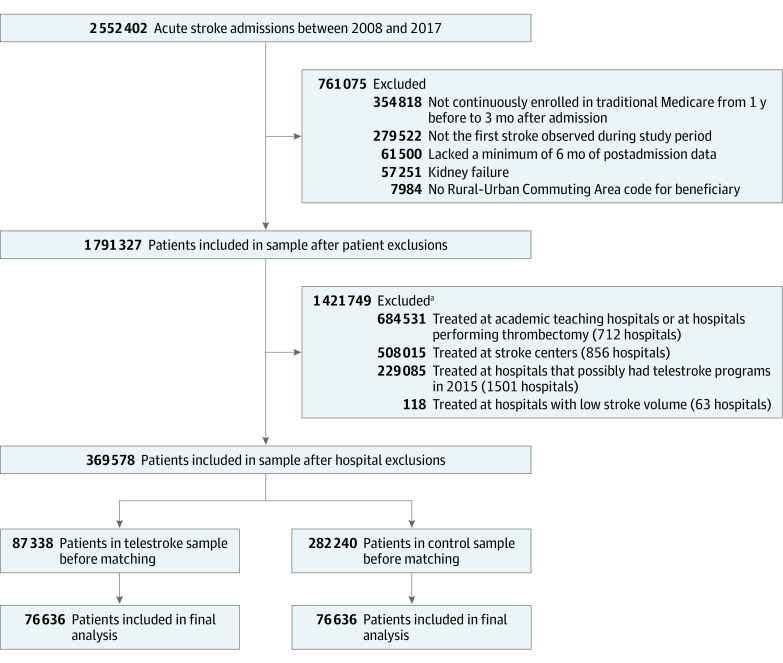
To ensure capture of each patient’s claim history before and after their admission, we limited our study sample to patients with at least 1 year of continuous enrollment in Medicare parts A and B before their admission and 3 months of continuous enrollment after their discharge (or until death, whichever came first). We excluded patients for whom we could not link zip codes and patients currently enrolled in Medicare with kidney failure (Figure 1).
Figure 1. Study Sample.
aExclusion was based on the initial hospital where the patient presented.
Categorizing Telestroke and Control Hospitals
We excluded hospitals with less than 1 stroke admission per year from January 2008 to June 2017 and hospitals that likely had substantive local stroke expertise (comprehensive and primary stroke centers, academic teaching hospitals, hospitals performing thrombectomy) (eFigure 1 in the Supplement). We excluded hospitals that already had local stroke expertise because their telestroke programs are likely used to complement substantive in-person stroke services rather than provide expertise that is otherwise lacking. For example, at these hospitals, local stroke specialists can use telestroke to avoid traveling from home or clinic to perform consultations. The remaining hospitals were divided into telestroke and control hospitals.
To our knowledge, there is currently no comprehensive list of hospitals with telestroke capacity. As detailed previously,26 working with all 15 academic centers and commercial companies that provide telestroke (eFigure 1 in the Supplement) that we were aware of, we obtained lists of which hospitals were in their networks and the month and year in which each hospital began using telestroke. To our knowledge, this is the largest and most comprehensive list of hospitals with telestroke, but we recognize that some control hospitals may have had telestroke capacity through another network. We therefore limited the set of potential control hospitals to those that self-reported not having a telestroke program in the 2016 National Emergency Department Inventory survey.21 We did not use this survey response to create our telestroke sample because it was limited to 1 year and did not include when telestroke was introduced.
At treatment and control hospitals, we focused on all admissions with a diagnosis of stroke regardless of whether they received a telestroke consultation. We chose this intention-to-treat framework as it best addresses the population-level question of what impact the introduction of telestroke capacity at a hospital has on care patterns and outcomes.
Outcomes
We measured receipt of reperfusion treatment through administration of intravenous thrombolysis with alteplase or endovascular thrombectomy using procedure codes (ICD-9 codes 99.10 and 39.74; ICD-10 codes 3E03317-3E08317 and 03CG3ZZ-03CV3ZZ) and diagnosis codes (ICD-9 code V45.88; ICD-10 code Z9282), which are used when the patient receives alteplase in an ED before being transferred to another hospital (a method known as drip and ship27). Using the date of death field from the beneficiary summary files, we created indicators for mortality 7, 30, 90, and 180 days from admission. As a proxy for patient disability and functional status following a stroke,28,29 in lieu of a modified Rankin Scale score at 90 days, we used a previously validated measure30,31 that captures patient days spent living in the community following discharge, which are the number of days not spent in an inpatient, rehabilitation, skilled nursing, or hospice facility in the 90 days after discharge. Patients who died in the hospital were given a value of 0 days at home. We also created a binary indicator for whether the patient was back in the community on the 90th day after discharge. To evaluate any differences in returns to hospital after a stroke admission, we created an indicator for any inpatient or outpatient ED/observation stay in the 30 days after discharge. To measure spending, we calculated the total payments paid for inpatient, outpatient, and skilled nursing facility stays, hospice, home health agency services, and durable medical equipment (which we defined as institutional spending) from admission through 90 days after discharge. This spending measure does not capture spending for inpatient or outpatient evaluation and management visits. Spending on services that began before the 90th day but ended after the 90th day were prorated to only include the time within the 90-day postdischarge window.
Statistical Analysis
In this observational study design, our goal was to approximate a randomized clinical trial in which patients are randomized to hospitals with and without telestroke capacity. We used risk set and cardinality matching to address the temporal nature of the data and the staggered adoption dates of the telestroke programs. In each 6-month period from January 1, 2008, through June 30, 2017, we optimally matched admissions that started in hospitals with a telestroke program to admissions that started in control hospitals without a telestroke program. By matching cases in the same time period, we address temporal trends in the care for patients with stroke.
Matching was based on prespecified patient and hospital characteristics believed to be key prognostic indicators of patient mortality following an acute stroke. These included age (7 groups, including younger than 65 years, aged 65 to 69 years, 70 to 74 years, 75 to 79 years, 80 to 84 years, 85 to 89 years, and 90 years and older), sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Asian, Hispanic, or other), the patient’s original Medicare entitlement reason (age, disability, or kidney failure), dual enrollment in Medicaid, rural patient residence, history of acute and chronic conditions as captured in Medicare’s Chronic Conditions Data Warehouse (history of atrial fibrillation, diabetes, stroke, ischemic heart disease, acquired hypothyroidism, acute myocardial infarction, and hyperlipidemia), and categories of the presenting hospital’s 6-month stroke volume going from less than 2 per month to 8 or more per month (1 to 11, 12 to 23, 23 to 52, and 53 to 163), teaching status, hospital rurality, and census division (9 divisions).
Cardinality matching uses integer programming to find the largest matched sample of admissions that balances the observed covariates, with optimality guarantees.32,33 For each 6-month period, we found the largest pair-matched sample of telestroke and control admissions where the joint distribution of age group, sex, atrial fibrillation, and rural patient residence—factors most predictive of patient mortality following stroke (eMethods and eTable 2 in the Supplement)—was perfectly balanced, and the standardized difference in sample means between the telestroke admissions and the control admissions for the remaining matching variables did not exceed 0.1 absolute standardized mean differences, a commonly accepted threshold for balance (Table 1). After this initial step, our sample included an equal number of telestroke and control admissions that satisfy our criteria for sample balance in covariate means.
Table 1. Characteristics of Stroke Admissions Before and After Matching, January 2008 to June 2017.
| Characteristic | Before matching | After matching | ||||
|---|---|---|---|---|---|---|
| Hospitals, % | Standardized difference in means | Hospitals, % | Standardized difference in means | |||
| Telestroke | Control | Telestroke | Control | |||
| Admissions, No. | 87 338 | 282 240 | NA | 76 636 | 76 636 | NA |
| Age, ya | ||||||
| <65 | 8.3 | 8.2 | 0.004 | 7.9 | 7.9 | 0 |
| 65-69 | 11.8 | 11.0 | 0.026 | 11.3 | 11.3 | 0 |
| 70-74 | 15.1 | 14.5 | 0.017 | 15.1 | 15.1 | 0 |
| 75-79 | 16.6 | 16.7 | −0.004 | 16.7 | 16.7 | 0 |
| 80-84 | 18.1 | 19.0 | −0.023 | 18.6 | 18.6 | 0 |
| 85-90 | 16.7 | 17.2 | −0.014 | 17.1 | 17.1 | 0 |
| >90 | 13.3 | 13.3 | 0.001 | 13.4 | 13.4 | 0 |
| Femalea | 56.4 | 57.8 | −0.028 | 57.5 | 57.5 | 0 |
| Race/ethnicity | ||||||
| Non-Hispanic | ||||||
| White | 87.7 | 86.9 | 0.025 | 88.0 | 87.7 | 0.009 |
| Black | 8.6 | 9.1 | −0.019 | 8.6 | 8.7 | −0.006 |
| Hispanic | 1.4 | 1.5 | −0.005 | 1.4 | 1.2 | 0.011 |
| Asian | 0.6 | 0.9 | −0.038 | 0.5 | 0.7 | −0.020 |
| Other race/ethnicity | 1.7 | 1.6 | 0.006 | 1.6 | 1.7 | −0.008 |
| Original reason for Medicare enrollment | ||||||
| 65 y and older | 80.5 | 80.7 | −0.006 | 81.4 | 81.6 | −0.005 |
| Disability | 19.4 | 19.1 | 0.007 | 18.5 | 18.3 | 0.006 |
| Kidney failureb | 0.1 | 0.2 | −0.009 | 0.1 | 0.1 | −0.003 |
| Dually enrolled in Medicaid | 23.1 | 26.6 | −0.081 | 22.8 | 22.8 | 0 |
| Rural residencea | 39.3 | 50.2 | −0.222 | 39.2 | 39.2 | 0 |
| Other conditionsc | ||||||
| Atrial fibrillationa | 25.8 | 25.1 | 0.016 | 22.9 | 22.9 | 0 |
| Diabetes | 45.1 | 43.7 | 0.029 | 44.8 | 43.6 | 0.024 |
| Cerebrovascular disease | 27.6 | 30.6 | −0.066 | 27.4 | 27.0 | 0.010 |
| Coronary artery disease | 59.5 | 60.8 | −0.027 | 58.9 | 57.7 | 0.024 |
| Hyperlipidemia | 79.8 | 75.4 | 0.106 | 79.5 | 78.3 | 0.028 |
| 6-mo Hospital volume of strokes | ||||||
| 1-11 | 16.3 | 29.9 | −0.327 | 17.7 | 20.5 | −0.069 |
| 12-23 | 24.2 | 27.7 | −0.080 | 25.1 | 25.8 | −0.017 |
| 24-52 | 38.5 | 33.1 | 0.112 | 38.0 | 37.0 | 0.020 |
| 53-163 | 21.1 | 9.3 | 0.332 | 19.1 | 16.7 | 0.065 |
| Hospital teaching status | ||||||
| Major | 4.9 | 4.9 | 0.002 | 5.0 | 5.7 | −0.028 |
| Minor | 17.6 | 17.8 | −0.006 | 17.6 | 18.8 | −0.031 |
| No teaching | 77.5 | 77.3 | 0.004 | 77.3 | 75.5 | 0.043 |
| Hospital in a rural community | 32.7 | 44.9 | −0.251 | 33.3 | 33.5 | −0.005 |
Abbreviation: NA, not applicable.
Indicates variable on which exact matching conducted. Matching was also conducted on census division, and this comparison is included in eTable 3 in the Supplement. Additional characteristics not used for matching the telestroke and control samples are provided in eTable 4 in the Supplement.
Patients with kidney failure currently enrolled in Medicare were removed as part of our patient exclusions; this row describes patients originally enrolled because of kidney failure but currently enrolled because of age or disability.
Other acute and chronic conditions included in the match include acute myocardial infarction and hypothyroidism.
We evaluated differences in outcomes using nonparametric statistical tests, including the McNemar test for dichotomous outcomes and the Wilcoxon signed rank test for continuous outcomes. We assessed the sensitivity of our results to biases using Rosenbaum bounds (eTable 6 in the Supplement),34,35 which quantify the extent of hidden bias due to an unobserved covariate that would need to be present to explain our statistically significant findings.
In secondary analyses, we examined outcome differences by subgroups of admissions, including admission date before or after 2015 (when thrombectomy became more common), hospitals’ 6-month stroke volume (less than 2 per month, 2 to 4 per month, 4 to 8 per month, and 2 or more per week), and by years from telestroke adoption (ie, outcome differences by program maturity). In a sensitivity analysis, we evaluated whether care patterns at intervention and control hospitals in the year prior to telestroke implementation were different.
We conducted our analyses using R version 3.5.0 (The R Foundation) and Stata version 16 (StataCorp) and considered 2-tailed P values less than .05 to be statistically significant. Differences in outcome means, as well as ratios of risks, were calculated along with 95% CIs.
Results
From January 1, 2008, through June 30, 2017, we identified 369 578 stroke episodes that met our patient and hospital inclusion criteria. Of these, 87 338 patients received care at 1 of 643 hospitals with telestroke capacity. Before matching, patients treated at a hospital with telestroke capacity were more likely to live in an urban area and have hyperlipidemia and diabetes (Table 1). From this sample, we matched 76 636 telestroke admissions (87.7%) to controls, balancing our criteria for distributional and mean covariate balance. In the final sample of 153 272 patients, 88 386 (57.7%) were female, and the mean (SD) age was 78.8 (10.4) years. Prior to the introduction of telestroke, we found no evidence that care was superior at telestroke hospitals vs controls (eTable 5 in the Supplement).
Primary Analysis
Among patients treated initially at a hospital with telestroke capacity and their matched controls, 5181 of 76 636 (6.8%) and 4583 of 76 636 (6.0%), respectively, received reperfusion treatment (absolute difference, 0.78 percentage points; 95% CI, 0.54-1.03; P < .001) (Table 2). Compared with their matched controls, the risk ratios for treatment were higher for patients cared for at telestroke hospitals for any reperfusion treatment (risk ratio, 1.13; 95% CI, 1.09-1.17; P < .001), drip-and-ship cases (risk ratio, 1.38; 95% CI, 1.30-1.45; P < .001), and thrombectomies (risk ratio, 1.42; 95% CI, 1.25-1.62; P < .001) (Table 2).
Table 2. Treatment and Outcome Risk Ratios in Telestroke vs Control Hospitals, 2008-2017.
| Outcome | Hospitals, % | Difference (95% CI) | P valuea | Risk ratio (95% CI) | |
|---|---|---|---|---|---|
| Telestroke | Control | ||||
| Reperfusion treatmentb | 6.76 | 5.98 | 0.78 (0.54 to 1.03) | <.001 | 1.13 (1.09 to 1.17) |
| Thrombolysis via alteplase | 6.47 | 5.77 | 0.70 (0.46 to 0.94) | <.001 | 1.12 (1.08 to 1.17) |
| Thrombolysis and transferc | 3.78 | 2.75 | 1.03 (0.85 to 1.21) | <.001 | 1.38 (1.30 to 1.45) |
| Thrombectomy use | 0.70 | 0.49 | 0.21 (0.13 to 0.29) | <.001 | 1.42 (1.25 to 1.62) |
| Mortality from admission | |||||
| 7 d | 6.03 | 6.33 | −0.30 (−0.54 to −0.06) | .02 | 0.95 (0.92 to 0.99) |
| 30 d | 13.12 | 13.62 | −0.50 (−0.83 to −0.17) | .003 | 0.96 (0.94 to 0.99) |
| 90 d | 18.35 | 18.75 | −0.39 (−0.77 to −0.02) | .04 | 0.98 (0.96 to 1.00) |
| 180 d | 22.60 | 22.95 | −0.35 (−0.75 to 0.05) | .09 | 0.98 (0.97 to 1.00) |
| All-cause returns to hospital 30 d from discharge | 25.79 | 26.20 | −0.41 (−0.85 to 0.03) | .07 | 0.98 (0.97 to 1.00) |
| Living in community at 90 d | 73.11 | 72.86 | 0.25 (−0.18 to 0.67) | .26 | 1.00 (1.00 to 1.01) |
| Community time within 90 d, No. of days | 60.25 | 60.22 | 0.03 (−0.32 to 0.39) | .93 | NA |
| Institutional spending, $ | 26 560 | 26 524 | 36 (−212 to 283) | .31 | NA |
Abbreviation: NA, not applicable.
For statistical significance, we used the McNemar test for dichotomous outcomes and the Wilcoxon signed rank test for continuous outcomes. Risk ratios and 95% CIs are shown for dichotomous outcomes.
Reperfusion treatment includes delivery of thrombolysis via alteplase or thrombectomy at the presenting hospital or after transfer.
Thrombolysis via alteplase delivered before admission (drip and ship) is recorded in the patient’s diagnosis codes at the admitting hospital.
We found lower mortality (13.1% vs 13.6%; difference, 0.50 percentage points; 95% CI, 0.17-0.83, P = .003) at 30 days from admission. The risk ratios for postadmission mortality were 0.95 (95% CI, 0.92-0.99; P = .02) at 7 days, 0.96 (95% CI, 0.94-0.99; P = .003) at 30 days, 0.98 (95% CI, 0.96-1.00; P = .04) at 90 days, and 0.98 (95% CI, 0.97-1.00; P = .09) at 180 days. For the remaining outcomes of returns to hospital, spending, and living in the community, we did not observe significant differences between telestroke and control patients. Sensitivity analyses to biases due to unmeasured confounders could not rule out small to moderate biases (eTable 6 in the Supplement).
Subgroup Analyses
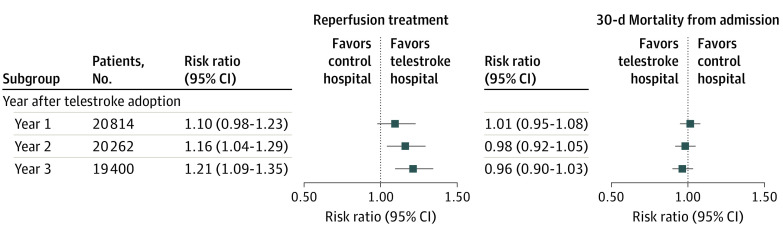
The risk ratio for reperfusion treatment was largest among patients 85 years and older (1.18; 95% CI, 1.09-1.27), rural patients (1.24; 95% CI, 1.17-1.32), admissions that occurred after 2015 (1.17; 95% CI, 1.11-1.23), and hospitals treating fewer than 2 strokes per month (1.30; 95% CI, 1.19-1.43) (Figure 2). There were no substantive differences in 30-day mortality from admission across these characteristics (Figure 2). Limiting our analysis to telestroke hospitals that had at least 3 years of data following telestroke adoption (ie, telestroke introduced January 2008 to June 2014), reperfusion treatment increased in each of the 3 years after adoption (Figure 3).
Figure 2. Risk Ratios for Reperfusion Treatment and 30-Day Mortality Among Subgroups of Patient and Hospitals, Telestroke vs Control Hospitals, 2008 to 2017.
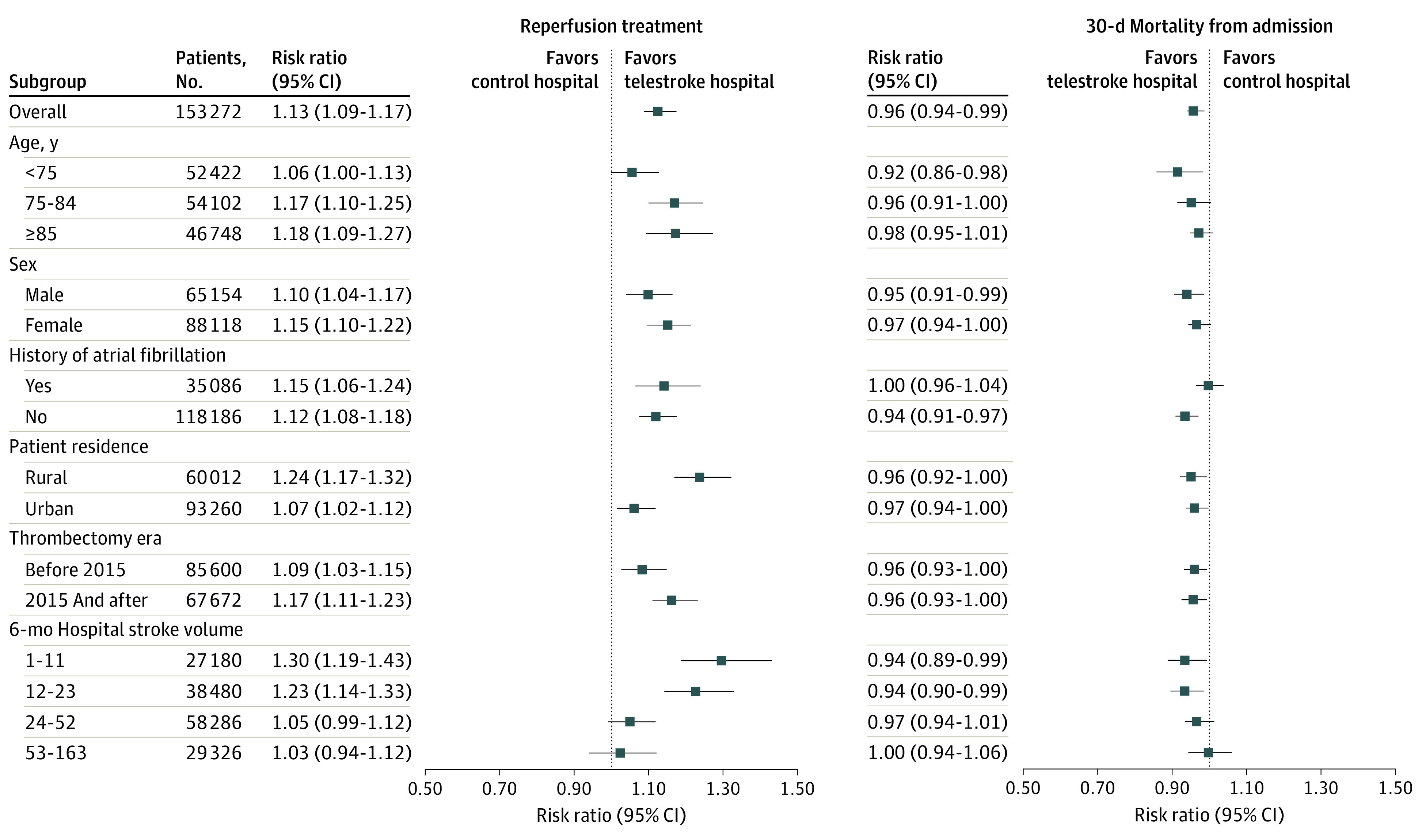
Figure 3. Risk Ratios for Reperfusion Treatment and 30-Day Mortality in the First 3 Years After Adoption, Telestroke vs Control Hospitals, 2008 to 2017.
Subsample of telestroke hospitals (n = 339) that had at least 3 years of postadoption claim history.
Discussion
Across more than 600 hospitals in the US, we found that telestroke capacity was associated with a 15% relative increase in receiving reperfusion treatment (thrombolysis with alteplase or thrombectomy) and reduced short-term mortality. Increases in reperfusion treatment at telestroke hospitals were largest among older patients and rural patients and were incrementally higher in each of the 3 years following telestroke implementation. We found sizable reperfusion differences in our comparison of low-volume hospitals, which suggests that telestroke had more impact in locations that treat fewer than 2 strokes per month. We did not see any differences in locations that average more than 2 strokes per week, indicating that volume (ie, experience) may be providing sufficient stroke expertise in those locations. The benefits we did observe did not result in higher spending. Given the increasing prevalence of telestroke in EDs and current state of evidence, it is unlikely that a randomized clinical trial of telestroke vs placebo is feasible given the ethics of not offering patients effective stroke care. Therefore, we believe this form of rigorous observational study is likely to be the best evidence available on the association of telestroke with treatment and outcomes for patients with acute ischemic stroke.
Our findings are consistent with prior research that find an association between telestroke capacity and increased reperfusion treatment, although the increases we observed are more modest.23 These more modest effects may be driven in part because we examined a more recent time period in which emergency medicine physicians have become more comfortable with thrombolysis and therefore may be more likely to use it without specialist consultation.36,37 It is notable that the increase in reperfusion treatment in telestroke hospitals is largest among the oldest age group (older than 85 years); a potential explanation for this difference is that emergency medicine physicians are uncomfortable using thrombolysis in this age group given the associated increased risk of intracerebral hemorrhage.38
The average number of patients with stroke who received care each year at our cohort of hospitals was relatively low (22 per year) because we excluded hospitals with local stroke expertise (41 per year before making this exclusion), which typically have higher volume.39,40 Among these relatively low-volume hospitals, the largest increases in reperfusion associated with telestroke capacity were seen among the hospitals with the lowest volume (average less than 2 strokes per month) and rural hospitals. Many lower-volume and rural EDs rely on physicians not trained in emergency medicine and sometimes are staffed solely by advanced practice clinicians without physicians on site. These clinicians may have less exposure to stroke care and thus lower comfort levels with reperfusion decisions.
To our knowledge, this is the first study to demonstrate that telestroke is associated with a clinically meaningful reduction in mortality and improved use of reperfusion treatments with no increase in health care spending. Though cost-effective from the perspective of Medicare, it is important to emphasize that local hospitals must pay for telestroke capacity, and these payments are not captured in our data.
Unfortunately, the subgroup of hospitals where we observe the greatest benefits of telestroke, low-volume and rural hospitals, are the least likely to have telestroke capacity.26 To encourage more hospitals to have telestroke capacity may require increased reimbursement or direct financial support.41,42 Targeted policy interventions to increase telestroke capacity at low-volume hospitals may be necessary given that these hospitals may face greater barriers to adopting telestroke capacity, including insufficient financial investment, lack of high-speed internet in rural communities, and regulations that limit financial support from tertiary hospitals.
We used an intention-to-treat design and examined the care across all patients with stroke at a hospital. Given that many of these patients at hospitals with telestroke capacity did not receive a telestroke consultation, we are likely underestimating the impact of telestroke at the individual patient level. By focusing on the impact telestroke capacity had for all patients with stroke at a hospital, we captured the broader clinical impact of telestroke adoption at the community level, incorporating any additional clinical benefits telestroke capacity might bring to a local hospital through educational interventions and feedback mechanisms that improve the quality of care for patients with stroke who do not receive a telestroke consultation.43,44
Limitations
Our study has several key limitations. It is possible that other components of telestroke outside of direct consultations, such as better ties with stroke centers, could be contributing to the differences we observed. Moreover, it is important to be cautious in the interpretation of our observed benefit on mortality, given the effect size is small, not evident at 6 months, and, as we show in our sensitivity analyses, may be driven by unmeasured factors, such as stroke severity at time of presentation. However, as noted in subanalyses (eFigure 2 in the Supplement), in the limited sample of cases where we have National Institutes of Health Stroke Scale severity scores, there is balance between telestroke and control sites. Other important patient factors, such as symptom onset, were not available in the data. We only have a proxy measure of functional outcomes (ie, days spent living in the community), and we may not be identifying all cases of stroke using the primary diagnosis code. Further, hospitals that introduce telestroke capacity may also be more committed to quality improvement, and this could be driving differences rather than telestroke. However, we believe these factors unlikely to be playing a major role given that we found no evidence of superior treatment patterns or outcomes in the year prior to when these hospitals implemented telestroke. Also, because our analysis focused on the association of telestroke capacity with all hospital stroke admissions, we believe our results are not sensitive to biases stemming from unobserved patient factors that may drive which patient receives a telestroke consultation. Additionally, we focused on the introduction of telestroke capacity at hospitals without local stroke expertise. Many academic teaching hospitals and stroke centers have introduced telestroke, and the impact of telestroke in these hospitals is likely different.
Conclusions
In summary, we found that patients with stroke first cared for at a hospital with telestroke capacity were more likely to receive reperfusion treatment with alteplase or thrombectomy and have lower short-term mortality compared with those first cared for at a hospital without telestroke capacity.
eMethods. Selection of matching variables.
eTable 1. Crosswalk of ICD-9 to ICD-10 acute stroke diagnosis codes.
eTable 2. Coefficients in 180-day mortality model (admissions in 2008 only).
eTable 3. Census divisions of stroke admissions before and after matching, 2008-2017.
eTable 4. Additional sample characteristics.
eTable 5. Outcome differences and risk ratios in telestroke vs control hospitals in the year prior to telestroke introduction.
eTable 6. Sensitivity of unobserved factors using Rosenbaum bounds.
eFigure 1. Sample of study hospitals.
eFigure 2. Severity score densities for telestroke/control admissions, January to June 2017.
References
- 1.Emberson J, Lees KR, Lyden P, et al. ; Stroke Thrombolysis Trialists’ Collaborative Group . Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929-1935. doi: 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hacke W, Kaste M, Bluhmki E, et al. ; ECASS Investigators . Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. doi: 10.1056/NEJMoa0804656 [DOI] [PubMed] [Google Scholar]
- 3.Berkhemer OA, Fransen PSS, Beumer D, et al. ; MR CLEAN Investigators . A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20. doi: 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Demchuk AM, Menon BK, et al. ; ESCAPE Trial Investigators . Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030. doi: 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 5.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group . Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333(24):1581-1587. doi: 10.1056/NEJM199512143332401 [DOI] [PubMed] [Google Scholar]
- 6.Lees KR, Bluhmki E, von Kummer R, et al. ; ECASS, ATLANTIS, NINDS and EPITHET rt-PA Study Group . Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695-1703. doi: 10.1016/S0140-6736(10)60491-6 [DOI] [PubMed] [Google Scholar]
- 7.Albers GW, Marks MP, Kemp S, et al. ; DEFUSE 3 Investigators . Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718. doi: 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nogueira RG, Jadhav AP, Haussen DC, et al. ; DAWN Trial Investigators . Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11-21. doi: 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 9.Saver JL. Time is brain—quantified. Stroke. 2006;37(1):263-266. doi: 10.1161/01.STR.0000196957.55928.ab [DOI] [PubMed] [Google Scholar]
- 10.Maggiore WA. Stroke of the clock: ‘time is brain’ when treating stroke patients. JEMS. 2012;37(6):56-58, 60-62, 64-65. [PubMed] [Google Scholar]
- 11.Man S, Xian Y, Holmes DN, et al. Association between thrombolytic door-to-needle time and 1-year mortality and readmission in patients with acute ischemic stroke. JAMA. 2020;323(21):2170-2184. doi: 10.1001/jama.2020.5697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kleindorfer D, Kissela B, Schneider A, et al. ; Neuroscience Institute . Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: a population-based study. Stroke. 2004;35(2):e27-e29. doi: 10.1161/01.STR.0000109767.11426.17 [DOI] [PubMed] [Google Scholar]
- 13.Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409. doi: 10.1002/jhm.689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With The Guidelines-Stroke hospitals. Circ Cardiovasc Qual Outcomes. 2013;6(5):543-549. doi: 10.1161/CIRCOUTCOMES.111.000095 [DOI] [PubMed] [Google Scholar]
- 15.Adeoye O, Nyström KV, Yavagal DR, et al. Recommendations for the establishment of stroke systems of care: a 2019 update. Stroke. 2019;50(7):e187-e210. doi: 10.1161/STR.0000000000000173 [DOI] [PubMed] [Google Scholar]
- 16.Wechsler LR, Demaerschalk BM, Schwamm LH, et al. ; American Heart Association Stroke Council; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research . Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(1):e3-e25. doi: 10.1161/STR.0000000000000114 [DOI] [PubMed] [Google Scholar]
- 17.Akbik F, Hirsch JA, Chandra RV, et al. Telestroke—the promise and the challenge. part one: growth and current practice. J Neurointerv Surg. 2017;9(4):357-360. doi: 10.1136/neurintsurg-2016-012291 [DOI] [PubMed] [Google Scholar]
- 18.Pervez MA, Silva G, Masrur S, et al. Remote supervision of IV-tPA for acute ischemic stroke by telemedicine or telephone before transfer to a regional stroke center is feasible and safe. Stroke. 2010;41(1):e18-e24. doi: 10.1161/STROKEAHA.109.560169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwamm LH, Rosenthal ES, Hirshberg A, et al. Virtual TeleStroke support for the emergency department evaluation of acute stroke. Acad Emerg Med. 2004;11(11):1193-1197. doi: 10.1197/j.aem.2004.08.014 [DOI] [PubMed] [Google Scholar]
- 20.Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke. 2012;43(8):2078-2085. doi: 10.1161/STROKEAHA.111.645861 [DOI] [PubMed] [Google Scholar]
- 21.Zachrison KS, Boggs KM, M Hayden E, Espinola JA, Camargo CA. A national survey of telemedicine use by US emergency departments. J Telemed Telecare. 2020;26(5):278-284. doi: 10.1177/1357633X18816112 [DOI] [PubMed] [Google Scholar]
- 22.Zhang D, Wang G, Zhu W, et al. Expansion of telestroke services improves quality of care provided in super rural areas. Health Aff (Millwood). 2018;37(12):2005-2013. doi: 10.1377/hlthaff.2018.05089 [DOI] [PubMed] [Google Scholar]
- 23.Audebert HJ, Schenkel J, Heuschmann PU, Bogdahn U, Haberl RL; Telemedic Pilot Project for Integrative Stroke Care Group . Effects of the implementation of a telemedical stroke network: the Telemedic Pilot Project for Integrative Stroke Care (TEMPiS) in Bavaria, Germany. Lancet Neurol. 2006;5(9):742-748. doi: 10.1016/S1474-4422(06)70527-0 [DOI] [PubMed] [Google Scholar]
- 24.Zhang D, Shi L, Ido MS, et al. Impact of participation in a telestroke network on clinical outcomes. Circ Cardiovasc Qual Outcomes. 2019;12(1):e005147. doi: 10.1161/CIRCOUTCOMES.118.005147 [DOI] [PubMed] [Google Scholar]
- 25.Powers WJ, Derdeyn CP, Biller J, et al. ; American Heart Association Stroke Council . 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020-3035. doi: 10.1161/STR.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 26.Richard JV, Wilcock AD, Schwamm LH, et al. Assessment of telestroke capacity in US hospitals. JAMA Neurol. 2020;77(8):1035-1037. doi: 10.1001/jamaneurol.2020.1274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheth KN, Smith EE, Grau-Sepulveda MV, Kleindorfer D, Fonarow GC, Schwamm LH. Drip and ship thrombolytic therapy for acute ischemic stroke: use, temporal trends, and outcomes. Stroke. 2015;46(3):732-739. doi: 10.1161/STROKEAHA.114.007506 [DOI] [PubMed] [Google Scholar]
- 28.O’Brien EC, Xian Y, Xu H, et al. Hospital variation in home-time after acute ischemic stroke: insights from the PROSPER study (Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research). Stroke. 2016;47(10):2627-2633. doi: 10.1161/STROKEAHA.116.013563 [DOI] [PubMed] [Google Scholar]
- 29.Xian Y, Xu H, O’Brien EC, et al. Clinical effectiveness of direct oral anticoagulants vs warfarin in older patients with atrial fibrillation and ischemic stroke: findings from the Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) study. JAMA Neurol. 2019;76(10):1192-1202. doi: 10.1001/jamaneurol.2019.2099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quinn TJ, Dawson J, Lees JS, Chang TP, Walters MR, Lees KR; GAIN and VISTA Investigators . Time spent at home poststroke: “home-time” a meaningful and robust outcome measure for stroke trials. Stroke. 2008;39(1):231-233. doi: 10.1161/STROKEAHA.107.493320 [DOI] [PubMed] [Google Scholar]
- 31.Fonarow GC, Liang L, Thomas L, et al. Assessment of home-time after acute ischemic stroke in Medicare beneficiaries. Stroke. 2016;47(3):836-842. doi: 10.1161/STROKEAHA.115.011599 [DOI] [PubMed] [Google Scholar]
- 32.Zubizarreta JR, Paredes RD, Rosenbaum PR. Matching for balance, pairing for heterogeneity in an observational study of the effectiveness of for-profit and not-for-profit high schools in Chile. Ann Appl Stat. 2014;8:204-231. doi: 10.1214/13-AOAS713 [DOI] [Google Scholar]
- 33.Visconti G, Zubizarreta JR. Handling limited overlap in observational studies with cardinality matching. Observational Stud. 2018;4:2017-2249. [Google Scholar]
- 34.Cappello A, Cevenini G, Avanzolini G. Model selection for ventricular mechanics: a sensitivity analysis approach. J Biomed Eng. 1987;9(1):13-20. doi: 10.1093/biomet/74.1.13 [DOI] [PubMed] [Google Scholar]
- 35.Rosenbaum PR. Design of Observational Studies. Springer; 2010.doi: 10.1007/978-3-030-46405-9 [DOI] [Google Scholar]
- 36.Scott PA, Xu Z, Meurer WJ, et al. Attitudes and beliefs of Michigan emergency physicians toward tissue plasminogen activator use in stroke: baseline survey results from the Increasing Stroke Treatment Through Interactive Behavioral Change Tactic (INSTINCT) trial hospitals. Stroke. 2010;41(9):2026-2032. doi: 10.1161/STROKEAHA.110.581942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scott PA, Meurer WJ, Frederiksen SM, et al. ; INSTINCT Investigators . A multilevel intervention to increase community hospital use of alteplase for acute stroke (INSTINCT): a cluster-randomised controlled trial. Lancet Neurol. 2013;12(2):139-148. doi: 10.1016/S1474-4422(12)70311-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arora R, Salamon E, Katz JM, et al. Use and outcomes of intravenous thrombolysis for acute ischemic stroke in patients ≥90 years of age. Stroke. 2016;47(9):2347-2354. doi: 10.1161/STROKEAHA.116.012241 [DOI] [PubMed] [Google Scholar]
- 39.Reeves MJ, Gargano J, Maier KS, et al. Patient-level and hospital-level determinants of the quality of acute stroke care: a multilevel modeling approach. Stroke. 2010;41(12):2924-2931. doi: 10.1161/STROKEAHA.110.598664 [DOI] [PubMed] [Google Scholar]
- 40.Zachrison KS, Onnela JP, Reeves MJ, et al. Hospital factors associated with interhospital transfer destination for stroke in the northeast United States. J Am Heart Assoc. 2020;9(1):e011575. doi: 10.1161/JAHA.118.011575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwamm L. Written statement of Dr. Lee Schwamm, MD, FAHA. Accessed August 6, 2020. https://www.finance.senate.gov/imo/media/doc/20170516SchwammStmt.pdf
- 42.Telemedicine for stroke expanded with passage of FAST Act. News release. American Academy of Neurology. February 9, 2018. Accessed August 6, 2020. https://www.aan.com/PressRoom/Home/PressRelease/1618
- 43.Tatlisumak T, Soinila S, Kaste M. Telestroke networking offers multiple benefits beyond thrombolysis. Cerebrovasc Dis. 2009;27(suppl 4):21-27. doi: 10.1159/000213055 [DOI] [PubMed] [Google Scholar]
- 44.Schwamm LH, Audebert HJ, Amarenco P, et al. ; American Heart Association Stroke Council; Council on Epidemiology and Prevention; Interdisciplinary Council on Peripheral Vascular Disease; Council on Cardiovascular Radiology and Intervention . Recommendations for the implementation of telemedicine within stroke systems of care: a policy statement from the American Heart Association. Stroke. 2009;40(7):2635-2660. doi: 10.1161/STROKEAHA.109.192361 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Selection of matching variables.
eTable 1. Crosswalk of ICD-9 to ICD-10 acute stroke diagnosis codes.
eTable 2. Coefficients in 180-day mortality model (admissions in 2008 only).
eTable 3. Census divisions of stroke admissions before and after matching, 2008-2017.
eTable 4. Additional sample characteristics.
eTable 5. Outcome differences and risk ratios in telestroke vs control hospitals in the year prior to telestroke introduction.
eTable 6. Sensitivity of unobserved factors using Rosenbaum bounds.
eFigure 1. Sample of study hospitals.
eFigure 2. Severity score densities for telestroke/control admissions, January to June 2017.