Abstract
Background
This study aimed at evaluating the role of presepsin in early identification of sepsis and prediction of mortality in intensive care unit (ICU) patients in comparison to systemic inflammatory response syndrome (SIRS) and quick sequential organ failure assessment (qSOFA) score.
Materials and methods
Forty patients were selected randomly after admission to adult ICU. Data from emergency room (ER) triaging, and initial laboratory results were gathered to calculate qSOFA score, SIRS criteria, and SOFA score. Presepsin measurement was performed within 6 hours from ER triaging.
The patients were categorized into sepsis and nonsepsis groups depending on the clinical and microbiological criteria and SOFA score changes.
Results
Twenty-six patients were diagnosed as septic with an average age of 68.04 ± 18.60 years, while 14 patients were nonseptic with an average age of 51.71 ± 24.88 years.
Presepsin with a cutoff value >640 pg/mL (area under the curve [AUC] of 0.848 (p < 0.001}) had a significant diagnostic accuracy of identifying septic cases with sensitivity of 73.08% and specificity of 92.86% as compared to the nonsignificant SIRS (AUC, 0.670; sensitivity, 69.23%; and specificity, 57.14%) or qSOFA (AUC, 0.652; sensitivity, 38.46%; and specificity, 78.57%) criteria.
Prespsin with a cutoff value >640 pg/mL also significantly (AUC of 0.920 [p < 0.001]) predicted mortality with sensitivity of 100.0% and specificity of 66.67% compared to the nonsignificant SIRS (AUC, 0.540; sensitivity, 70.0%; and specificity, 43.33%) or qSOFA (AUC, 0.670; sensitivity, 60%; and specificity, 76.67%) criteria.
Conclusion
Early presepsin measurement in ICU patients is more accurate in the diagnosis of sepsis and prediction of mortality as compared to SIRS or qSOFA score.
How to cite this article
Abdelshafey EE, Nasa P, Elgohary AE, Khalil MF, Rashwan MA, Ghezala HB, et al. Role of Presepsin for the Diagnosis of Sepsis and ICU Mortality: A Prospective Controlled Study. Indian J Crit Care Med 2021;25(2):153–157.
Keywords: Biomarkers, Presepsin, Predictive model, qSOFA: quick sequential (sepsis-related) organ failure assessment, Sepsis
Introduction
The timely diagnosis of sepsis is challenging, despite its high morbidity and mortality.1 There are numerous clinical and biological markers being tested for early diagnosis of sepsis. The task force comprising global experts coined revised definition on sepsis (Sepsis 3) in which the conventional systemic inflammatory response syndrome (SIRS) criteria was replaced by the sequential organ failure assessment (SOFA) score for the diagnosis of sepsis.2 A quick SOFA (qSOFA) score was also advocated as a bedside tool to facilitate the early identification of patients potentially at risk of dying from sepsis, especially outside intensive care unit (ICU).3
Presepsin is a novel biological marker produced by the cleavage of the N-terminal of soluble CD14 (sCD14).4 CD14 is a member of Toll-like receptor (TLR) and acts as a coreceptor for various ligands from both gram-positive and gram-negative bacteria (GNB). Lipopolysaccharide (LPS) complex of GNB is the most-studied ligand and in association with LPS-binding protein (LBP) and CD14 binds to TLR.4,5 LPS-LBP-CD14-TLR complex formation on the effector cells (like monocytes and macrophages), causes activation and then contributes to the intracellular signaling and production of cytokines, triggering the initial host inflammatory response against the pathogen. CD14 are of two types: membrane-bound CD14 (mCD14) and soluble CD14 (sCD14). mCD14 is involved in ligand binding and sCD14 is released into the plasma either by the effector cells or by the fall-off from mCD14.5 Presepsin is thus, a biomarker of activated innate immune system to invading pathogen.
We undertook this study, to evaluate the significance of presepsin for early identification of sepsis and prediction of ICU mortality in comparison to the SIRS criteria and the qSOFA score.
Materials and Methods
Data Collection
Between June 2018 and December 2018, 40 adult patients (≥18 years) were randomly selected after admission to ICU from ER. The demographic data on age, sex, and acute physiology and chronic health evaluation II score (APACHE II) were collated.
The data on initial mental status using Glasgow coma score (GCS), systolic blood pressure (SBP), and respiratory rate (RR) were taken from ER to calculate the qSOFA score. The temperature, RR, heart rate (HR), and white blood cell (WBC) count were used to calculate SIRS. qSOFA was defined by Sepsis 3, 2016 criteria altered mentation (GCS <15), SBP <100 mmHg, and RR χ22 breaths/min.3 SIRS was defined as HR >90 beats/min, RR >20 breaths/min, temperature >38 or <36 °C, and WBC >12,000/mm3 or <4000/mm3 or band cells χ10%.
SOFA score was calculated once all the laboratory parameters (serum bilirubin, platelet count, serum creatinine, and arterial blood gas) were available and within 6 hours of triaging in ER. Presepsin measurement in full blood sample was also performed within 6 hours from triaging using PATHFAST 1602D2600 from LSI Medience Corporation, Japan. This is a point-of-care (POC), highly sensitive, and fully automated chemiluminescent enzyme immunoassay-based measurement system that provides its result within 17 minutes.6
The diagnosis of sepsis was made when patients revealed a microbiologically or clinically proven infection with at least one new organ dysfunction assessed by the change of a SOFA score χ2; otherwise patients are claimed to be nonseptic. Comparison of sepsis and nonsepsis groups was done for age, sex, APACHE II, SOFA, qSOFA, SIRS, and presepsin levels.
Statistical Analysis
The continuous variables were expressed as means ± standard deviation (SD), medians, and interquartile ranges (minimum- maximum). The categorical variables were expressed in counts and percentages. Clinical comparison between sepsis and nonsepsis group was done using two-sample T-test and Mann-Whitney test for continuous variables, and chi-square test and Fisher exact test for categorical variables. Receiver operating characteristic (ROC) curves were plotted and areas under the ROC curve (AUC) were calculated using Youden index for the diagnostic accuracy of presepsin, qSOFA, SIRS, and the combination of presepsin with qSOFA or SIRS for sepsis and ICU mortality. Based on the optimal cutoff values of presepsin for discriminating between the two groups of sepsis and nonsepsis, according to the ROC curve analysis, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were also calculated. p-value less than 0.05 was taken as significant. IBM SPSS (version 20.0, Armonk, NY: IBM Corp.) was used for analysis.
Aims and Objectives
Primary
To compare presepsin to SIRS and qSOFA for the diagnosis of sepsis.
To compare presepsin to SIRS and qSOFA for predicting ICU mortality in sepsis patients.
Secondary
To identify the optimal cutoff for presepsin for the diagnosis and ICU mortality in sepsis.
Results
Out of 40 patients included in the study, 26 (65%) patients were diagnosed as septic and 14 (35%) patients were nonseptic. The average age was significantly higher in sepsis group as compared to nonsepsis (mean 68.04 ± 18.60 vs 51.71 ± 24.88 years, p = 0.024) while no significant difference was found regarding sex (males 61.5 vs 57.1%, respectively, p = 0.787). Patients in the sepsis group were significantly sick with an average APACHE II score (18.50 ± 6.13 vs 13.36 ± 7.53, p = 0.029) higher than the nonsepsis group. Similarly, the SOFA score was also significantly higher in the sepsis group (mean of 5.81 ± 3.41 vs 2.86 ± 4.37, p = 0.001) (Table 1). No significant difference was found between the groups in relation to all the elements of qSOFA score and the complete score itself (mean qSOFA of 1.19 ± 0.85 in sepsis vs 0.71 ± 0.83 in nonsepsis group, p = 0.096) (Table 1). SIRS elements were also not significantly different between the groups for temperature, RR, or HR except WBC count which was higher in sepsis group (mean value of 16.41 ± 9.32 vs 10.26 ± 4.46 [×103 cell/mm3], p = 0.0370) (Table 1). Overall, the SIRS criteria was also not significantly different between the groups (mean of 2.0 ± 1.02 in sepsis vs 1.36 ± 1.01 in nonsepsis group, p = 0.068) (Table 1).
Table 1.
Comparison between the two groups based on baseline characteristics and studied sepsis scale
| Sepsis (n = 26) | No sepsis (n = 14) | p-value | |
|---|---|---|---|
| Sex (n (%) | |||
| Male | 16 (61.5) | 8 (57.1) | |
| Female | 10 (38.5) | 6 (42.9) | |
| Age (in years) | |||
| Median (range) | 72.50 (20.0–89.0) | 45.0 (15.0–86.0) | |
| Mean (SD) | 68.04 (18.60) | 51.71 (24.88) | |
| Glasgow Coma Scale | |||
| Median (range) | 14.5 (4.0–15.0) | 15.0 (3.0–15.0) | |
| Mean (SD) | 12.19 (3.48) | 13.50 (3.70) | |
| Heart rate (beats/minute) | |||
| Median (range) | 97.0 (66.0–130.0) | 93.50 (58.0–117.0) | |
| Mean (SD) | 95.50 (15.53) | 91.0 (20.11) | |
| Respiratory rate (per minute) | |||
| Median (range) | 22.0 (16.0–32.0) | 20 (8.0–26.0) | |
| Mean (SD) | 22.35 (3.74) | 19.79 (4.85) | |
| Systolic blood pressure (mm Hg) | |||
| Median (range) | 117.0 (84.0–154.0) | 133.5 (100.0–165.0) | |
| Mean (SD) | 119.5 (19.04) | 129.4 (21.64) | |
| Temp (degree celsius) | |||
| Median (range) | 36.90 (34.50–38.50) | 36.90 (36.80–39.0) | |
| Mean (SD) | 36.95 (0.71) | 37.24 (0.63) | |
| White blood cells (×103/mm3) | |||
| Median (range) | 14.75 (2.0–37.10) | 10.60 (3.89–19.40) | |
| Mean (SD) | 16.41 ± 9.32 | 10.26 ± 4.46 | |
| APACHE II | |||
| Median (range) | 17.50 (11.0–38.0) | 12.0 (0.0–26.0) | 0.029* |
| Mean (SD) | 18.50 (6.13) | 13.36 (7.53) | |
| SOFA | |||
| Median (range) | 5.0 (2.0–14.0) | 1.50 (2.86 ± 4.37) | 0.001* |
| Mean (SD) | 5.81 (3.41) | 2.86 (4.37) | |
| qSOFA | |||
| Median (range) | 1.0 (0.0–3.0) | 0.50 (0.0–2.0) | 0.096 |
| Mean (SD) | 1.19 (0.85) | 0.71 (0.83) | |
| SIRS | |||
| Median (range) | 2.0 (0.0–4.0) | 1.0 (0.0–3.0) | 0.068 |
| Mean (SD) | 2.0 (1.02) | 1.36 (1.01) |
Statistically significant at p ≤ 0.05; SOFA, sequential organ failure assessment; qSOFA, quick SOFA; SIRS, systemic inflammatory response syndrome; APACHE II, acute physiological and chronic health evaluation II score
The comparison of qSOFA, SIRS criteria and presepsin for early identification of septic cases was done using the ROC curve analysis. Presepsin alone has a significantly higher accuracy (AUC of 0.848, p < 0.001) with sensitivity of 73.08% and specificity of 92.86% for the diagnosis of sepsis, and the cutoff value for presepsin was 640 pg/mL. At this cutoff value, the addition of presepsin to qSOFA has a better accuracy than qSOFA alone (AUC of 0.838 vs 0.652 and p-value <0.001 vs 0.116, respectively). The addition of presepsin to SIRS also increases the diagnostic accuracy as compared to the SIRS alone (AUC of 0.849 vs 0.670 and p-value <0.001 vs 0.079, respectively) (Fig. 1, Table 3).
Fig. 1.
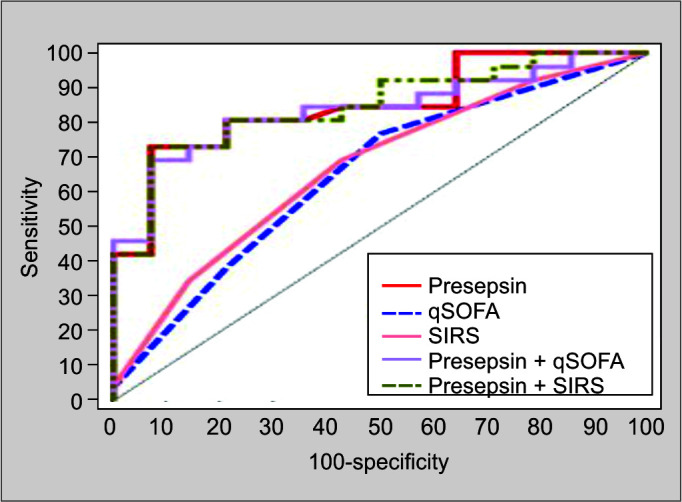
Receiver-operating characteristics for diagnosis of sepsis
Table 3.
Diagnostic accuracy for presepsin, qSOFA, SIRS, presepsin ± qSOFA, and presepsin ± SIRS in sepsis patients
| 95%CI | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| AUC | p–value | LL | LL | Cutoff # | Sensitivity | Specificity | PPV | NPV | |
| Presepsin | 0.848 | <0.001* | 0.727 | 0.968 | >640 | 73.08 | 92.86 | 95.0 | 65.0 |
| qSOFA | 0.652 | 0.116 | 0.472 | 0.833 | ≥2 | 38.46 | 78.57 | 76.92 | 40.74 |
| SIRS | 0.670 | 0.079 | 0.495 | 0.846 | ≥2 | 69.23 | 57.14 | 75.0 | 50.0 |
| Presepsin ± qSOFA | 0.838 | <0.001* | 0.715 | 0.961 | – | 76.92 | 78.57 | 86.96 | 64.71 |
| Presepsin ± SIRS | 0.849 | <0.001* | 0.729 | 0.969 | – | 80.77 | 71.43 | 84.0 | 66.67 |
Cutoff was done by using Youden index;
Statistically significant at p ≤ 0.05; AUC, area under the curve; LL, lower limit; UL, upper limit; PPV, positive predictive value; NPV, negative predictive value; CI, confidence interval; qSOFA, quick sequential organ failure assessment; SIRS, systemic inflammatory response syndrome
Table 2.
Comparison between the two studied groups according to presepsin value (pg/mL) and ICU mortality
| Sepsis (n = 26) | No sepsis (n = 14) | Test of sig. | p–value | |||
|---|---|---|---|---|---|---|
| Presepsin (pg/mL) | ||||||
| Min.−Max. | 163.0–19370.0 | 38.40–1795.0 | ||||
| Mean ± SD | 2726.5 ± 3930.3 | 414.6 ± 445.9 | U = 55.50 | <0.001* | ||
| Median | 1311.5 | 349.0 | ||||
| No. | % | No. | % | |||
| ICU mortality | 9 | 34.6 | 1 | 7.1 | χ2 = 3.663 | 0.070 |
Statistically significant at p ≤ 0.05; χ2, Chi–square test; U: Mann–Whitney test; ICU, intensive care unit
Comparing the significance of qSOFA score, SIRS criteria, and presepsin for early prediction of ICU mortality was done also using the ROC curve analysis. Presepsin levels had a significantly higher prediction ability (AUC of 0.920, p < 0.001) for ICU mortality with a sensitivity of 100.0%, specificity of 66.67%, and a cutoff value of 640 pg/mL. The addition of presepsin to qSOFA increases the prediction accuracy of ICU mortality as compared to qSOFA alone (AUC of 0.917 vs 0.670 and p-value of <0.001 vs 0.111, respectively). The combination of presepsin to SIRS also has a significantly higher prediction accuracy for ICU mortality than SIRS alone (AUC of 0.920 vs 0.540 and p-value of <0.001 vs 0.708, respectively) (Fig. 2, Table 4).
Fig. 2.
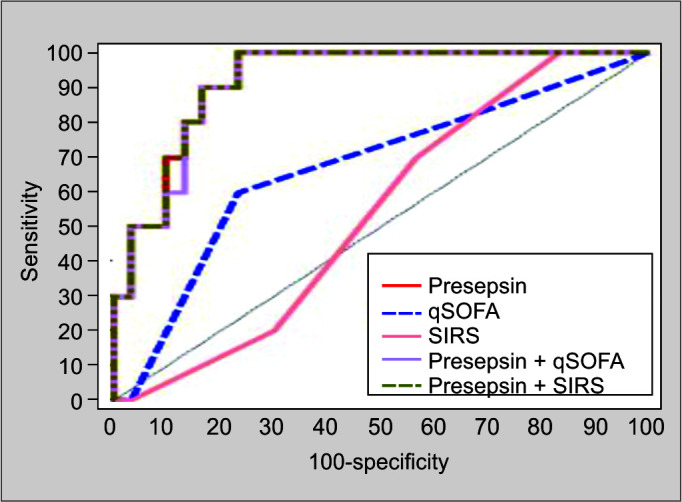
Receiver-operating characteristics for prediction of ICU mortality
Table 4.
Agreement (sensitivity, specificity) for presepsin, qSOFA, SIRS, presepsin + qSOF, and presepsin + SIRS for prediction of ICU mortality
| 95%CI | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| AUC | p–value | LL | UL | Cutoff # | Sensitivity | Specificity | PPV | NPV | |
| Presepsin | 0.920 | <0.001* | 0.838 | 1.00 | >640 | 100.0 | 66.67 | 100.0 | |
| qSOFA | 0.670 | 0.111 | 0.469 | 0.871 | ≥2 | 60.0 | 76.67 | 46.15 | 85.19 |
| SIRS | 0.540 | 0.708 | 0.357 | 0.723 | ≥2 | 70.0 | 43.33 | 29.17 | 81.25 |
| Presepsin + qSOFA | 0.917 | <0.001* | 0.833 | 1.00 | – | 50.0 | 93.33 | 71.43 | 84.85 |
| Presepsin + SIRS | 0.920 | <0.001# | 0.838 | 1.00 | – | 50.0 | 93.33 | 71.43 | 84.85 |
Cutoff was done by using Youden index;
Statistically significant at p ≤ 0.05; AUC, area under the curve; LL, lower limit; UL, upper limit; PPV, positive predictive value; NPV, negative predictive value; CI, confidence interval; qSOFA, quick sequential organ failure assessment; SIRS, systemic inflammatory response syndrome
Discussion
Early identification and timely treatment especially with antimicrobials is associated with reduced mortality in sepsis.7 The bedside clinical screening tools (SIRS and qSOFA) were aimed at recognizing sepsis early and predicting patients with higher risk of mortality.2,3 These traditional tools are either only sensitive (SIRS) or specific (qSOFA) for an organ dysfunction but overall have a poor discrimination ability to diagnose sepsis.8
Sepsis is a life-threatening organ dysfunction due to a dysregulated host-immune response.1 Innate immune system is the primary human barrier to bacterial infection, and presepsin is a biological marker representing its activation.4 In our study, presepsin (cutoff 640 pg/mL [AUC 0.848 and p = <0.001]) could accurately differentiate sepsis patients from nonsepsis patients with a remarkable sensitivity and specificity of 73.08 and 92.86%, respectively (Table 3). Endo et al., in their study showed that presepsin can discriminate bacterial infections from nonbacterial infectious diseases with a cutoff value of 600 pg/mL (AUC of 0.908) and a sensitivity and specificity of 87.8 and 81.4%, respectively.9 In a metanalysis of eight studies with over 1800 patients using the older definition of sepsis, presepsin showed a similar diagnostic accuracy (AUC = 0.89) for the diagnosis of sepsis.10 The diagnostic performance of SIRS and qSOFA was very modest compared to the presepsin alone with an AUC of 0.670 and 0.652, respectively, and the addition of presepsin to these clinical scores increased the diagnostic yield of each of them significantly (AUC of 0.838 and 0.849, respectively, p = <0.001) (Table 3).
The prognostic performance in the prediction of ICU mortality of presepsin (cutoff 640 pg/mL [AUC 0.920 and p = <0.001]) was also significantly better as compared to the SIRS and qSOFA alone (AUC 0.670 and 0.540, respectively). The addition of presepsin level to SIRS and qSOFA increased their prognostic performance significantly (AUC of 0.917 and 0.920, respectively, p = <0.001). This is consistent with a post hoc analysis of albumin Italian outcome sepsis (ALBIOS) trial, which showed a higher level of presepsin on day 1 among survivors as compared to survivors with a level of 2269 pg/ml and 1184 pg/ml, respectively.11 In a metanalysis of 10 studies with 1617 patients, presepsin collected within the first 24 hours was significantly different between survivors and nonsurvivors (AUC of 0.92, p = <0.01) on a random-effect model.12
In our study, presepsin showed a higher accuracy of sepsis diagnosis and ICU mortality than many previous studies. This may be related to inclusion of random cases and also may be early measurement of presepsin level within 6 hours of hospital admission.
The strength of our study is that it is a prospective, controlled study with direct comparison of POC presepsin with the bedside clinical tools in the diagnosis and prognosis of sepsis. We also found that combination of presepsin with these tools can improve their diagnostic accuracy and prediction of outcome. There are a few limitations to our study: the small number of cases, the random selection of patients because of shortage of laboratory reagent for presepsin which may have caused some bias, and also the lack of comparison to other sepsis biomarkers.
Conclusion
Presepsin at a cutoff of 640 ng/mL is an accurate tool for diagnosing and prognosticating sepsis. qSOFA and SIRS when combined with POC presepsin can accurately detect sepsis as compared to when used alone.
Orcid
Eslam E Abdelshafey https://orcid.org/0000-0001-8018-2948
Prashant Nasa https://orcid.org/0000-0003-1948-4060
Ahmed E Elgohary https://orcid.org/0000-0002-8230-6200
Mohammad F Khalil https://orcid.org/0000-0001-7816-8610
Mohammad A Rashwan https://orcid.org/0000-0001-8987-0034
Hassen B Ghezala https://orcid.org/0000-0002-7083-7303
Ashraf A Tayar https://orcid.org/0000-0002-2897-7417
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. doi: 10.1164/rccm.201504-0781OC. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;23;315(8):801–810. doi: 10.1001/jama.2016.0287. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). [Published correction appears in JAMA 2016;315(20):2237]. JAMA. 2016;315(8):762–774. doi: 10.1001/jama.2016.0288. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chenevier-Gobeaux C, Borderie D, Weiss N, Mallet-Coste T, Claessens YE. Presepsin (sCD14-ST), an innate immune response marker in sepsis. Clin Chim Acta. 2015;450:97–103. doi: 10.1016/j.cca.2015.06.026. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Memar MY, Baghi HB. Presepsin: a promising biomarker for the detection of bacterial infections. Biomed Pharmacother. 2019;111:649–656. doi: 10.1016/j.biopha.2018.12.124. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Okamura Y, Yokoi H. Development of a point-of-care assay system for measurement of presepsin (sCD14-ST). Clin Chim Acta. 2011;412(23–24):2157–2161. doi: 10.1016/j.cca.2011.07.024. DOI: [DOI] [PubMed] [Google Scholar]
- 7.Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–2244. doi: 10.1056/NEJMoa1703058. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marik PE, Taeb AM. SIRS, qSOFA and new sepsis definition. J Thorac Dis. 2017;9(4):943–945. doi: 10.21037/jtd.2017.03.125. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Endo S, Suzuki Y, Takahashi G, Shozushima T, Ishikura H, Murai A, et al. Usefulness of presepsin in the diagnosis of sepsis in a multicenter prospective study. J Infect Chemother. 2012;18(6):891–897. doi: 10.1007/s10156-012-0435-2. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Zhang X, Liu D, Liu YN, Wang R, Xie LX. The accuracy of presepsin (sCD14-ST) for the diagnosis of sepsis in adults: a meta-analysis. Crit Care. 2015;19(1):323. doi: 10.1186/s13054-015-1032-4. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masson S, Caironi P, Spanuth E, Thomae R, Panigada M, Sangiorgi G, et al. Presepsin (soluble CD14 subtype) and procalcitonin levels for mortality prediction in sepsis: data from the Albumin Italian Outcome Sepsis trial. Crit Care. 2014;18(1):R6. doi: 10.1186/cc13183. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang HS, Hur M, Yi A, Kim H, Lee S, Kim SN. Prognostic value of presepsin in adult patients with sepsis: systematic review and meta-analysis. PLoS One. 2018;13(1):e0191486. doi: 10.1371/journal.pone.0191486. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]


