Abstract
Background and Objective
Adolescence is considered to be a pivotal point in which optimum nutrition and eating habits are developed. Although tackling the obesity epidemic has been much discussed, addressing the issue of underweight and body image is often neglected. This study was carried out to get a better understanding of underweight status among adolescents in Saudi Arabia, and exploring self-perceptions of body image and weight loss measures among underweight adolescents.
Methods
Data from Jeeluna®, a national cross-sectional school-based survey were utilized. Jeeluna® assessed the health status and health-risk behaviors of adolescents in school through data obtained by a self-administered questionnaire, anthropologic measurements, and laboratory investigations.
Results
A total of 12,463 adolescents participated. Eighteen percent of adolescent males and 12.4% of females were found to be underweight, representing 14.9% of adolescents collectively. Forty-five percent of underweight participants were happy with their weight. Underweight females between the age group of 10 and 14 years were the most likely to believe that they still need to lose weight (16.0%) followed by females aged 15–19 years (9.7%). Underweight females aged 10–14 years were also the group most likely to engage in purging (1.6%). Stepwise logistic regression found that the strongest association with being underweight was with having a lower household income (OR 2.0, CI 1.5–2.7) and having more than 5 siblings (OR 1.8, CI 1.5–2.3).
Conclusion
Underweight status is prevalent among adolescents in Saudi Arabia and deserves more attention as a public health issue. Distorted body image and disordered eating behaviors exist, necessitating further investigation of underlying causes.
Keywords: Adolescent, Underweight, Body image, Low BMI, Health status, Kingdom of Saudi Arabia
List of abbreviations
- KSA
Kingdom of Saudi Arabia
- WHO
World Health Organization
- BMI
Body Mass Index
- CDC
Centers for Disease Control
- SES
Socioeconomic status
- MENA
Middle East and North Africa
1. Introduction
Adolescence, the age from 10 to 19 years, is a time of critical development in an individual’s cognitive, emotional, and social characteristics, as well as their physical growth and development. The study of this important age group has gained global attention as it represents a critical intervention point, as we now know through the life course lens to health, that to decrease disease burden in adulthood, we need to promote a healthy lifestyle and prevent risky behaviors in adolescence [[1], [2], [3]].
Around 1.2 billion of the world’s total population are considered to be in the adolescent age group, 88% of which are in developing countries including the Arab world [4]. As for the Kingdom of Saudi Arabia (KSA), around 14.5% of the 33 million total population are comprised of this age group [5]. Yet, focused attention and literature dedicated to the health needs of adolescents in the region, which is essential in guiding policy, has been generated only in the past several years [6].
One area of study is the nutritional profile of adolescents, which is essential to informed decision-making because of dietary behavior playing a crucial role in development, and is a prerequisite for decreasing disease burden in adulthood. While obesity in adolescents is on the rise and certainly receives much attention, this condition now coexists with being underweight. The consequence of this paradox is often referred to as “the double burden of malnutrition” and presents a challenge to public health [7]. Being underweight has been associated with a variety of conditions including musculoskeletal, respiratory, intestinal, adverse pregnancy outcomes, and psychiatric disorders [8,9] as well as stunting, pubertal delay, and a weakened immune system [10].
Global health reports have shown that although obesity rates are on the rise, rates of moderate or severe underweight are higher than rates of obesity among children and adolescents – as defined by World Health Organization (WHO) guidelines. This burden is increasingly concentrated in Africa and South Asia. Globally, the prevalence of moderate to severe underweight was 8.4% and 12.4% among boys and girls, respectively, in 2016 [11].
While available studies on adolescent nutritional profile in KSA have largely focused on obesity, which is seen as an epidemic, there are very limited studies examining the other extreme of body mass index (BMI) in adolescents. One available study done in Riyadh seems to suggest that underweight prevalence is alarmingly high compared to other similar countries in the region [12]. However, their sample size was limited and only included females in the age group of 12–15 years. The only nationally representative study addressing this in the KSA is the Jeeluna® study in which we reported the prevalence of underweight (BMI below the 5th centile for age and gender) to be 15.2% among a sample of over 12,500 adolescents [6].
In our current study, we aim to build on previously reported results by using the Jeeluna data to obtain a better understanding of underweight among adolescents in the KSA. We explore self-perceptions of body image and weight loss measures among underweight adolescents and identify gender differences.
2. Methods
Data for this study were taken from the Jeeluna® study, which is a school-based, national, cross-sectional study conducted in 282 schools across all 13 regions of KSA in the academic year of 2011–2012. The study used a student population proportionate, stratified, multi-stage, clustered sampling method to select a representative sample of adolescents. Data collection teams in all regions received standardized training for data collection. Data collection involved a self-administered questionnaire, anthropometric measurements, and blood samples for laboratory investigations.
The self-administered questionnaire was guided by preexisting internationally recognized surveys with psychometric properties aimed to address health risk behaviors among adolescents. Details of the study methods have been previously published [6]. Trained staff measured the height to the nearest 0.5 cm using a wall-mounted height chart and weight to the nearest 0.1 kg using a digital scale while students were lightly dressed and without shoes. BMIs were interpreted based on percentiles of the norm for age and sex, to be underweight if < 5th, healthy weight if between 5th and <85th, overweight if between 85th and <95th, or obese if 95th or more, in accordance with the Center for Disease Control (CDC) growth charts [13]. Data were weighted to ensure that it is nationally representative. Domains relevant to this study include (1) family; (2) educational level; (3) nutrition and dietary behaviors; (4) activities, including physical activity; and (5) health status. These relevant variables were extracted from the data set and analyzed.
Dietary behavior was assessed by participants answering the following questions in the self-administered questionnaire: “during the past 7 days, why did you skip meals?,” “are you currently on a diet for weight loss?,” and “what have you done in order to lose weight?” Those who answered the last question as “I took weight-loss medications” or “I vomited after eating” were considered to be purging and coded as such in the analysis. Body image was assessed by the question “what do you think of your body” in which participants could answer: “I am happy with the way my body looks,” “I think I need to lose some weight,” “I think I need to gain some weight.”
Additionally, other variables of interest in the questionnaire were: age, gender, area of residence (urban or rural), nationality, school grade, how often they engaged in exercise, and whether they have been diagnosed with a chronic or mental illness. To get an idea about socioeconomic status (SES), the following two questions were asked: “What is your family’s total monthly income?” and “How many full siblings do you have?”
Data analysis was performed using SPSS version 25.0 (SPSS Inc., 2017). Descriptive analysis was conducted as the first step of analysis. Participants were described in terms of their sociodemographic characteristics. The association between dietary behaviors and weight of the participants was evaluated using the chi-square test. Odds ratio and 95% confidence intervals were calculated for each of the potential explanatory variables in relation to the outcome (underweight). A significance level of less than 0.05 was used for all statistical tests.
Ethical approval for the study was obtained from the Institutional Review Board at King Abdullah International Medical Research Center (KAIMRC), and the Ministry of Education. Consent forms were obtained from parents and students, prior to participation in the study.
3. Results
A total of 12,463 adolescents participated. Fifty-one percent were adolescent males. Participants’ ages ranged between 10 and 19 years, with a mean of 15.8 years (1.8). The large majority of the students was of Saudi nationality (82.8%) and lived in urban cities (97.9%). Eighteen percent of adolescent males and 12.4% of females were found to be underweight according to the CDC definition, representing 14.9% of adolescents collectively. Of the participants (52.6%) had more than 5 siblings, and (34.9%) had between 3 and 5 siblings.
Disparities can be noted among adolescents in different regions within the KSA as shown in (Table 1). With Madinah having the highest frequency of underweight males (28.3%) and Najran having the highest frequency among females (29.0%), the Northern Borders region has the lowest for males (1.0%), and Aljouf has the lowest for females (3.1%), P value < .05.
Table 1.
Prevalence of underweight by region.
| Region | Male |
Female |
||
|---|---|---|---|---|
| Total (N) | Underweight N (%) |
Total (N) | Underweight N (%) |
|
| Riyadh | 1218 | 219 (18.0) | 1377 | 172 (12.5) |
| Qasim | 380 | 44 (11.6) | 344 | 36 (10.5) |
| Makkah | 1598 | 261 (16.3) | 1185 | 172 (14.5) |
| Madinah | 509 | 144 (28.3) | 426 | 58 (13.6) |
| Eastern province | 878 | 117 (13.3) | 959 | 75 (7.8) |
| Tabuk | 133 | 12 (9.0) | 200 | 9 (4.5) |
| Aljouf | 164 | 34 (20.7) | 194 | 6 (3.1) |
| Hail | 200 | 24 (12.0) | 154 | 13 (8.4) |
| Northern borders | 98 | 1 (1.0) | 114 | 10 (8.8) |
| Albaha | 117 | 28 (23.9) | 191 | 23 (12.0) |
| Aseer | 409 | 102 (24.9) | 360 | 72 (20.0) |
| Jizan | 377 | 106 (28.1) | 223 | 47 (21.1) |
| Najran | 191 | 42 (22.0) | 107 | 31 (29.0) |
| All | 6272 | 1134 (18.1) | 5834 | 724 (12.4) |
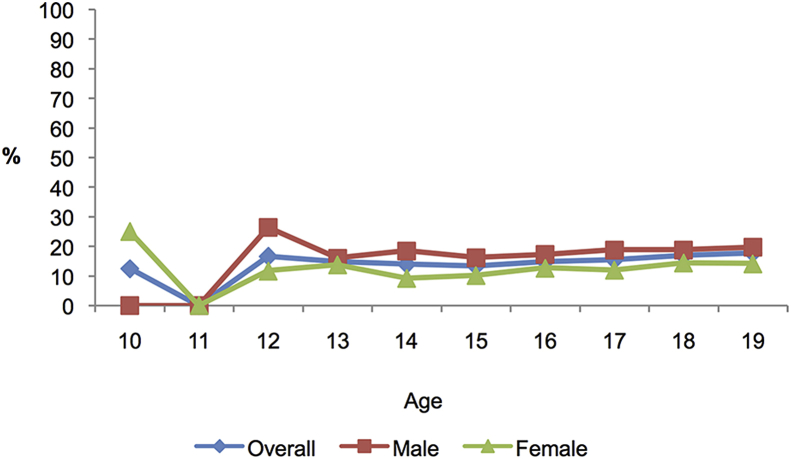
Fig. 1 depicts the prevalence of underweight by age for both males and females. A similar trend is observed among both genders where prevalence peaks at the age of 12 for males and 13 for females, then declines and stabilizes for the rest of adolescence. However, males start off at the age of 10 and 11 with much lower rates compared to females, then rapidly increase to the peak. This peak may be explained by the growth spurt occurring at puberty, which may coincide with the time of the peak.
Fig. 1.
Prevalence of underweight by age.
The relationship between body image perception, weight loss behaviors, and weight status is summarized in Table 2. Underweight participants were more likely to report that they did not skip meals in the past 7 days. Forty-five percent of underweight participants said that they were happy with their body, not acknowledging that they need to gain weight, compared with 51.1% of healthy weight. This was further examined in Table 3, where the results were broken down based on age group and gender. It was found that underweight females between the age group of 10 and 14 were the most likely group to believe that they need to lose weight despite being underweight (16.0%), followed by females between the age group of 15 and 19 years (9.7%). Females between the age group of 15 and 19 years were also most likely to believe they needed to gain weight (50.9%).
Table 2.
Relationship between body image perception, weight loss behaviors, and weight of the participants.
| Nutritional behavior | Underweight (%) | Normal weight (%) | P value |
|---|---|---|---|
| Why did you skip some meals in the past seven days? | <.01 | ||
| I did not skip meals | 695 (38.2) | 2254 (34.8) | |
| I did not feel hungry | 610 (33.5) | 2009 (31.0) | |
| I want to lose weight | 92 (5.1) | 989 (15.3) | |
| No food | 31 (1.7) | 93 (1.4) | |
| I did not feel comfortable to the available food | 168 (9.2) | 531 (8.2) | |
| Other reasons | 223 (12.3) | 598 (9.2) | |
| What do you think about your weight/body? | <.01 | ||
| Happy with my body | 806 (44.5) | 3296 (51.1) | |
| I need to lose weight | 181 (10.0) | 2271 (35.2) | |
| I need to gain weight | 826 (45.6) | 881 (13.7) | |
| Are you following a diet plan? | <.05 | ||
| Yes | 182 (10.1) | 766 (11.9) | |
| No | 1627 (89.9) | 5657 (88.1) | |
| What do you do if you want to lose weight? | <.01 | ||
| I have not tried to reduce my weight | 1281 (70.1) | 2823 (44.1) | |
| Decreased calorie intake | 272 (14.9) | 2019 (31.6) | |
| Exercise | 258 (14.1) | 1491 (23.3) | |
| Purging | 17 (0.9) | 62 (1.0) | |
Table 3.
Body satisfaction and weight loss methods among underweight by age and gender.
| Underweight male |
Underweight female |
|||||
|---|---|---|---|---|---|---|
| 10–14 years (%) | 15–19 years (%) | P value | 10–14 years (%) | 15–19 years (%) | P value | |
| Body satisfaction | NS | <.01 | ||||
| Happy with my body | 134 (49.4) | 365 (45.2) | 81 (44.8) | 200 (39.4) | ||
| I need to lose weight | 14 (5.2) | 74 (9.2) | 29 (16.0) | 49 (9.7) | ||
| I need to gain weight | 123 (45.4) | 369 (45.7) | 71 (39.2) | 258 (50.9) | ||
| Weight loss methods | NS | <.05 | ||||
| I have not tried to reduce my weight | 190 (68.6) | 571 (69.8) | 120 (65.9) | 378 (74.9) | ||
| Decreased calorie intake | 43 (15.5) | 107 (13.1) | 27 (14.8) | 77 (15.2) | ||
| Exercise | 41 (14.8) | 134 (16.4) | 32 (17.6) | 45 (8.9) | ||
| Purging | 3 (1.1) | 6 (0.7) | 3 (1.6) | 5 (1.0) | ||
NS - Not significant.
Furthermore, of all groups, underweight females between the age group of 10 and 14 years most commonly engaged in purging to lose weight (1.6%). This was followed by underweight females between the age group of 15 and 19 years (1.0%). The latter group was also the one most likely to report never attempting to lose weight (74.9%). In general, 13.1%–15.5% of underweight participants reported trying to further decrease their weights using caloric restriction.
Stepwise logistic regression was carried out to determine the independent predictors of underweight adolescents (Table 4). The strongest association was found with having a monthly family income of <5000 Saudi Riyals (OR 2.0, CI 1.5–2.7) and having more than 5 siblings (OR 1.8, CI 1.5–2.3), followed by being male (OR 1.6, CI 1.4–1.7). The effect of family income is more pronounced for females (OR 2.4, CI 1.3–4.3) compared to males (OR 1.9, CI 1.3–2.6), whereas the effect of number of siblings was similar for those with >5 siblings (OR 1.8 for both).
Table 4.
Factors associated with underweight among adolescents in Saudi Arabia by gender.
| Both Genders |
Male |
Female |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Gender | |||||||||
| Male | 1.6 | 1.4–1.7 | <.01 | ||||||
| Female (Ref.) | |||||||||
| Age | |||||||||
| 10–14 | 0.9 | 0.8–1.1 | NS | 0.9 | 0.8–1.1 | NS | 1.0 | 0.8–1.3 | NS |
| 15-19 (Ref.) | |||||||||
| Areas of residence | |||||||||
| Urban | 1.5 | 1.0–2.3 | <.05 | 2.0 | 1.1–3.5 | <.05 | 0.9 | 0.5–1.8 | NS |
| Rural (Ref.) | |||||||||
| Grade | |||||||||
| Intermediate | 0.9 | 0.8–1.1 | NS | 1.0 | 0.9–1.2 | NS | 0.7 | 0.6–0.9 | <.05 |
| Secondary (Ref.) | |||||||||
| Number of siblings | |||||||||
| >5 | 1.8 | 1.5–2.3 | <.01 | 1.8 | 1.4–2.4 | <.01 | 1.8 | 1.3–2.6 | <.01 |
| 3–5 | 1.4 | 1.1–1.8 | <.01 | 1.3 | 1.0–1.8 | <.05 | 1.6 | 1.1–2.3 | <.05 |
| <3 (Ref.) | |||||||||
| Monthly income | |||||||||
| <5000 riyals | 2.0 | 1.5–2.7 | <.01 | 1.9 | 1.3–2.6 | <.01 | 2.4 | 1.3–4.3 | <.01 |
| 5000-20000 riyals | 1.5 | 1.2–2.0 | <.01 | 1.3 | 1.0–1.8 | <.05 | 2.2 | 1.2–3.9 | <.01 |
| >20000 riyals (Ref.) | |||||||||
| Engage in exercise | |||||||||
| >5 days | 0.9 | 0.8–1.1 | NS | 1.1 | 0.9–1.3 | NS | 0.6 | 0.4–0.9 | <.05 |
| 2–5 days | 0.8 | 0.7–0.9 | <.05 | 1.0 | 0.8–1.1 | NS | 0.6 | 0.4–0.8 | <.01 |
| <2 days (Ref.) | |||||||||
| Chronic diseases | |||||||||
| Yes | 1.1 | 0.9–1.4 | NS | 1.3 | 1.1–1.7 | <.01 | 0.8 | 0.6–1.2 | NS |
| No (Ref.) | |||||||||
| Mental illness | |||||||||
| No | 1.1 | 1.0–1.3 | <.05 | 1.3 | 1.0–1.6 | <.05 | 1.0 | 0.8–1.2 | NS |
| Yes (Ref.) | |||||||||
NS - Not significant.
Finally, logistic regression analysis was performed to identify predictors of underweight after control for confounding effects. Results showed that predisposing factors for underweight among adolescents include: skipping meals (OR = 1.1, 95% CI = 1.0–1.2) and not being satisfied with body image (OR = 1.7, 95% CI = 1.5–1.9) (Table 5).
Table 5.
Predisposing factors for underweight among adolescents.
|
Nutritional behavior |
Number (%) | Adjusted odds ratioa | Confidence limits (95%) |
|
|---|---|---|---|---|
| Lower | Upper | |||
| Skipped meal | 7916 (65.8) | 1.1 | 1.0 | 1.2 |
| Not satisfied with body | 7184 (60.0) | 1.7 | 1.5 | 1.9 |
| Following a diet plan | 1677 (14.0) | 1.0 | 0.8 | 1.2 |
Adjusted for age, gender, and areas of residence.
4. Discussion
This is the first national study to investigate the correlates of underweight among adolescents in KSA, including perceptions of body image and weight loss behaviors, and has thus provided many valuable insights. The study shows that 14.9% of adolescents are underweight, which is alarmingly high compared to countries of similar socioeconomic and/or cultural landscape. A high proportion of underweight participants report being happy with their weight (44.5%) or wanting to lose more weight (10.0%), which should be addressed in the context of body image disturbance. Furthermore, we need to consider possible reasons for the high disparities in the prevalence of underweight adolescents among different regions of the country, which ranges from over 25% to under 10% among some regions in the country. Finally, being of low SES was the strongest predictor of being underweight.
Similar studies conducted in KSA are limited, but report similar trends. One such study conducted in Riyadh on 107 female adolescents between the age group of 12 and 15 years found that 28.6% were underweight [12]. Furthermore, a high prevalence of underweight status was also found among female university students where a study of 663 randomly selected participants between the age group of 18 and 24 years found 19.2% to be underweight. The number of siblings was also among the significantly associated factors along with the age and presence of obese family members [14]. Researchers in these studies agree that given the high prevalence of underweight compared to other countries, more emphasis should be given in future research to this understudied subject.
It is relevant to contrast these rates with those found in other countries in the Middle East and North African (MENA) region. A study in Qatar found that 8.6% and 5.8% of boys and girls, respectively, were underweight [15]. The prevalence of underweight among adolescents between the age group of 11 and 17 years in Egypt was 12.6% based on WHO charts, with males more commonly affected [16]. Regarding Palestine, underweight prevalence varied between 5% and 12% in two different cities, respectively [17]. One study in Istanbul found that 14.4% of boys and 11.1% of girls were underweight [18].
Regarding studies conducted elsewhere, the prevalence rates of moderate and severe thinness, as defined by the WHO growth reference, across 61,603 girls from 40 low- and middle-income countries was 6.30% [19]. In European countries and Australia, the prevalence of underweight status among children and adolescents is about 4–8% [20,21]. However, these results may not be comparable because of the use of different methodology and cut offs. In one study, the highest rates of underweight prevalence were found in China (11.5% in girls and 14.4% in boys), while the lowest were in the United States (3% in girls and 3.6% in boys). Brazilian adolescents and Russian adolescents had values that were in between (6.5% in girls, 10.6% in boys and 8.6% in girls, 7.7% in boys, respectively) [22]. These rates draw attention to the fact that rates in the KSA seem to be much higher, and there is a definite need for intervention.
The peak at the age of 12–13 years could be due to the variable onset of puberty among pupils, where the rate steadily goes down in subsequent years [23]. The age of puberty and hormonal profile were not assessed in this study, but other studies reported the onset of puberty to be inversely associated with underweight, as a higher proportion of the well-nourished were among those who have reached puberty in the sample [24]. Our study also revealed that males have higher rates of underweight than females in Saudi Arabia. This trend seen in some other countries was substantiated by the findings of previous studies, which suggest that adolescent girls may be more health-conscious, and therefore, more likely to follow dietary recommendations compared with similarly aged boys [25]. The findings suggest that more effort should be made to spread awareness about the importance of maintaining healthy weights among boys as well as girls.
The study also demonstrates that 44.5% of those who were underweight were happy with their body, and 35.2% of those who had normal BMIs wanted to lose weight. Additionally, 10.1% of underweight participants reported being on a diet to lose weight compared to 11.9% of normal weight participants. These rates are higher than those found in a similar study in Palestine where only 7% of underweight participants were on a diet to lose weight [26]; however, the Palestinian study also reported much higher rates of unhealthy weight control methods among underweight participants: 3.75% used pills/laxatives and 9.08% self-induced vomiting. In our study, only 0.9% used unhealthy purging methods. Although this is a good sign, it is difficult to draw a definitive conclusion due to the possibility of underreporting of this information, which may be considered sensitive. Underweight females between the age group of 10 and 14 years were the most likely group to report being unsatisfied with their weight and wanting to lose more weight at 16.0%, compared to 5.2% of males in the same age groups. One suggested reason for this disparity implicates mass media, which promotes and glamorizes thinness as the standard of beauty rather than health [27]. Studies suggest that women at the adolescent age can be particularly influenced by unrealistic body ideals of the media, which convey inaccurate messages [28]. There is a lack of literature to suggest whether this is the case in the KSA; however, the media that is available and viewed in Western countries, has now become the same media available locally. Future studies should investigate the role of mass media in the KSA, and its effects on body perception among adolescents and increasing rates of eating disorders.
The disparities of underweight prevalence reported by the study may be due to several underlying factors, such as differences in socioeconomic conditions, urbanization, culture, and health-promoting behaviors, including diet and exercise [29]. The findings provide a foundation for prioritizing these regions for intervention efforts and further research. It is also possible that students tend to be influenced by the weight status of the social majority in their schools, causing them to adapt to it [30]. A statistically significant difference was also found for underweight prevalence among those residing in urban cities versus rural areas (OR 1.5, CI 1.0–2.3), which suggests that the urban lifestyle may predispose adolescents to being underweight. Furthermore, there was no significant difference in the prevalence of underweight among Saudis and non-Saudis, which suggests that the role of the environment and lifestyle may be the main contributing factors over genetic factors in influencing the pattern of weight status.
In exploring the association between SES and underweight status, SES was inferred using adolescent-reported family income and the number of siblings. The study showed that these two factors were the largest risk factors for underweight status, suggesting that SES plays a big role and should be targeted with intervention strategies. However, it should be noted that although these measures provide an indication, they cannot fully capture the various dimensions of family SES. The association with low SES should be put into context, as the finding does not necessarily imply that access to food is the only implicated factor. Other related factors such as parenting practices, may explain a significant part of the difference as families with low SES may be less educated or have less time, thus are unable to teach kids about nutrition [31,32].
Some studies have found that poorer children who live in high SES neighborhoods have better educational outcomes and fewer behavioral problems than poor children who live in lower SES neighborhoods possibly suggesting that education and social norms are the dominant factors [33,34]. This suggests that there is room for affective intervention beyond simply improving SES. The literature also suggests that in developing countries, high SES is sometimes associated with increased overweight status; however, the opposite trend is seen in developed countries where low SES is associated with increased overweight status [35,36]. Therefore, the literature supports the idea that low-income individuals are more likely to be either underweight or overweight compared to high-income peers [37].
Given that the study is cross-sectional, we cannot establish causality between the dependent and independent variables; however, our study offers several possible risk factors associated with being an underweight adolescent in the KSA, more in-depth longitudinal studies should be done to better reflect on this situation to gain better understanding. Additionally, self-administered surveys may be associated with recall bias, and a high cognitive burden as physical activity and dietary assessment were based on individuals’ assessments and memory and not objective measurements. Additionally, some of the information may have been considered sensitive, and despite repeated reassurance that confidentiality would be maintained, some items may have been under reported. Finally, the hormonal profile of adolescents was not measured to be taken into consideration when evaluating heights and weights, which may not be comparable among participants who have reached puberty and others who have not.
On the other hand, the large sample size and the generalizability of the results speak of its strengths, as the study explores underweight status and associated risk factors among a nationally representative sample of adolescents in the KSA. Furthermore, standardized protocols were used to obtain anthropometric measurements, rather than relying on self-reported values. The questionnaire used had underwent several rounds of review by experts, and was pilot-tested for clarity and appropriate wording to ensure comprehension among the target study group. The questions were formulated in congruence with those included in the Youth Risk Behavior Survey [38] and the Global School-based Student Health Survey with cultural adaptations [39].
Ministry of Health and School Health Programs should work concurrently to address underweight as it represents a substantial disease burden. The aim is to improve the overall health of the youth in the country, and to prevent a multitude of health consequences in adults [9] as well as reproductive complications for girls [8]. It is important to note that while strategies to curb the rates of obesity among school-aged children is also paramount, certain strategies may have a negative impact on children with normal or below normal weight, and special attention should be taken to address the double burden of malnutrition with a holistic approach [40]. This can be done through effective school and community-based interventions that are tailored to the Saudi cultural context.
In looking forward, research should aim to better our understanding of how factors within family SES, school SES, and community SES interact to influence healthy nutritional status. Furthermore, the implementation of a surveillance program should be considered to observe changing trends and monitor results of intervention programs. It is suggested that underweight frequency is increasing in European countries [11]; further studies would need to be conducted to determine whether KSA is following a similar trend.
5. Conclusion
Underweight status is prevalent among adolescents in the KSA, and deserves more attention as a public health issue. Although obesity is now seen as an epidemic, policy makers should not neglect the other extreme of malnutrition, and adopt effective strategies and intervention programs to also tackle underweight. Our study demonstrates that there is an alarmingly high prevalence of underweight among adolescents in the KSA compared to other similar countries. Furthermore, it suggests that socioeconomic factors and body image disturbance play a dominant role. Though some knowledge has been generated from this study, many more questions have arisen. Are our adolescents simply seeking time-limited weight loss measures and fad diets, or could there be a more serious underlying problem, such as an eating disorder, which has gone unnoticed? This is a topic which is under addressed and, in our opinion, lacks much awareness in the society. A holistic, evidence-based approach that is specifically tailored to the Saudi cultural context is in need to tackle this issue of underweight among adolescents through educational programs, and policy-driven interventions in schools and in high-risk subpopulations.
Sources of funding
This work was supported by King Abdullah International Medical Research Center (Protocol RC08-092).
Implications and contributions statement
Although adolescents constitute a significant portion of Saudi Arabia’s population, little is known about the prevalence of correlates of underweight status. This nationally representative study has identified that the prevalence of underweight adolescence is alarmingly high and serves as evidence for possible educational programs and policy-driven interventions.
CRediT authorship contribution statement
Talal M. Hijji: Conceptualization, Methodology, Project administration, Writing - original draft. Hassan Saleheen: Conceptualization, Formal analysis, Software, Methodology, Writing - review & editing. Fadia S. AlBuhairan: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Supervision, Writing - review & editing.
Declaration of competing interest
The named authors all declare that they have no conflicts of interest, real or perceived, to disclose.
Acknowledgments
This work was supported by King Abdullah International Medical Research Center (Protocol RC08-092).
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
References
- 1.Unicef.org 2019. https://www.unicef.org/sowc2011/pdfs/SOWC-2011-Main-Report_EN_02092011.pdf Published.
- 2.Mokdad A.H., Jaber S., Aziz M.I., AlBuhairan F., AlGhaithi A., AlHamad N.M. The state of health in the Arab world, 1990–2010: an analysis of the burden of diseases, injuries, and risk factors. The Lancet. 2014 Jan 25;383(9914):309–320. doi: 10.1016/S0140-6736(13)62189-3. [DOI] [PubMed] [Google Scholar]
- 3.Catalano R.F., Fagan A.A., Gavin L.E., Greenberg M.T., Irwin C.E., Jr., Ross D.A. Worldwide application of prevention science in adolescent health. The Lancet. 2012 Apr 28;379(9826):1653–1664. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unicef.org 2019. https://www.unicef.org/adolescence/files/SOWC_2011_Main_Report_EN_02092011.pdf Published.
- 5.Population Estimates . 2019. General authority for statistics.https://www.stats.gov.sa/en/43 Published. [Google Scholar]
- 6.AlBuhairan F.S., Tamim H., Al Dubayee M., AlDhukair S., Al Shehri S., Tamimi W. Time for an adolescent health surveillance system in Saudi Arabia: findings from “Jeeluna”. J Adolesc Health. 2015 Sep 1;57(3):263–269. doi: 10.1016/j.jadohealth.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Kosaka S., Umezaki M. A systematic review of the prevalence and predictors of the double burden of malnutrition within households. Br J Nutr. 2017;117:1118–1127. doi: 10.1017/s0007114517000812. 08. [DOI] [PubMed] [Google Scholar]
- 8.Han Z., Mulla S., Beyene J., Liao G., McDonald S. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. 2010;40(1):65–101. doi: 10.1093/ije/dyq195. [DOI] [PubMed] [Google Scholar]
- 9.McDonald C.M., Olofin I., Flaxman S., Fawzi W.W., Spiegelman D., Caulfield L.E. Nutrition Impact Model Study. The effect of multiple anthropometric deficits on child mortality: meta-analysis of individual data in 10 prospective studies from developing countries. Am J Clin Nutr. 2013 Feb 20;97(4):896–901. doi: 10.3945/ajcn.112.047639. [DOI] [PubMed] [Google Scholar]
- 10.Vasunilashorn S., Martinson M. Weight status in adolescence is associated with later life functional limitations. J Aging Health. 2013;25(5):758–775. doi: 10.1177/0898264313491426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abarca-Gómez L., Abdeen Z.A., Hamid Z.A., Abu-Rmeileh N.M., Acosta-Cazares B., Acuin C. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. The Lancet. 2017 Dec 16;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al Muammar M., El Shafie M., Feroze A. Association between dietary habits and body mass index of adolescent females in intermediate schools in Riyadh, Saudi Arabia. East Mediterr Health J. 2014;20(1):39–45. doi: 10.26719/2014.20.1.39. [DOI] [PubMed] [Google Scholar]
- 13.Growth charts - homepage. Cdc.gov. 2019. http://www.cdc.gov/growthcharts Published.
- 14.Khalaf A., Westergren A., Berggren V., Ekblom Ö., Al-Hazzaa H. Prevalence and association of female weight status and dietary habits with sociodemographic factors: a cross-sectional study in Saudi Arabia. Public Health Nutr. 2014;18:784–796. doi: 10.1017/s1368980014001797. 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bener A. Prevalence of obesity, overweight, and underweight in Qatari adolescents. Food Nutr Bull. 2006;27(1):39–45. doi: 10.1177/156482650602700106. [DOI] [PubMed] [Google Scholar]
- 16.Manyanga T., El-Sayed H., Doku D., Randall J. The prevalence of underweight, overweight, obesity and associated risk factors among school-going adolescents in seven African countries. BMC Public Health. 2014;14(1) doi: 10.1186/1471-2458-14-887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jildeh C., Papandreou C., Mourad T.A., Hatzis C., Kafatos A., Qasrawi R. Assessing the nutritional status of Palestinian adolescents from East Jerusalem: a school-based study 2002–03. J Trop Pediatr. 2010 Jul 31;57(1):51–58. doi: 10.1093/tropej/fmq042. [DOI] [PubMed] [Google Scholar]
- 18.Yang L., Bovet P., Ma C., Zhao M., Liang Y., Xi B. Prevalence of underweight and overweight among young adolescents aged 12-15 years in 58 low-income and middle-income countries. Pediatr Obes. 2018 doi: 10.1111/ijpo.12468. [DOI] [PubMed] [Google Scholar]
- 19.Candler T., Costa S., Heys M., Costello A., Viner R. Prevalence of thinness in adolescent girls in low- and middle-income countries and associations with wealth, food security, and inequality. J Adolesc Health. 2017;60(4):447–454. doi: 10.1016/j.jadohealth.2016.11.003. e1. [DOI] [PubMed] [Google Scholar]
- 20.Ferrar K., Olds T. Thin adolescents: who are they? What do they do? Socio-demographic and use-of-time characteristics. Prev Med. 2010;51(3–4):253–258. doi: 10.1016/j.ypmed.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 21.Marques-Vidal P., Ferreira R., Oliveira J., Paccaud F. Is thinness more prevalent than obesity in Portuguese adolescents? Clin Nutr. 2008;27(4):531–536. doi: 10.1016/j.clnu.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y., Monteiro C., Popkin B. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr. 2002;75(6):971–977. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 23.Coly A.N., Milet J., Diallo A., Ndiaye T., Bénéfice E., Simondon F. Preschool stunting, adolescent migration, catch-up growth, and adult height in young Senegalese men and women of rural origin. J Nutr. 2006 Sep 1;136(9):2412–2420. doi: 10.1093/jn/136.9.2412. [DOI] [PubMed] [Google Scholar]
- 24.Shi Z., Lien N., Nirmal Kumar B., Dalen I., Holmboe-Ottesen G. The sociodemographic correlates of nutritional status of school adolescents in Jiangsu Province, China. J Adolesc Health. 2005;37(4):313–322. doi: 10.1016/j.jadohealth.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 25.Lattimore P., Halford J. Adolescence and the diet-dieting disparity: healthy food choice or risky health behaviour? Br J Health Psychol. 2003;8(4):451–463. doi: 10.1348/135910703770238301. [DOI] [PubMed] [Google Scholar]
- 26.Al Sabbah H., Vereecken C., Abdeen Z., Kelly C., Ojala K., Németh Á. Weight control behaviors among overweight, normal weight and underweight adolescents in Palestine: findings from the national study of Palestinian schoolchildren (HBSC-WBG2004) Int J Eat Disord. 2010 May;43(4):326–336. doi: 10.1002/eat.20698. [DOI] [PubMed] [Google Scholar]
- 27.Lee J., Lee Y. The association of body image distortion with weight control behaviors, diet behaviors, physical activity, sadness, and suicidal ideation among Korean high school students: a cross-sectional study. BMC Public Health. 2015;16(1) doi: 10.1186/s12889-016-2703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MacCallum F., Widdows H. Altered images: understanding the influence of unrealistic images and beauty aspirations. Health Care Anal. 2016;26(3):235–245. doi: 10.1007/s10728-016-0327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pawlińska-Chmara R., Wronka I., Suliga E., Broczek K. Socio-economic factors and prevalence of underweight and overweight among female students in Poland. Homo. 2007;58(4):309–318. doi: 10.1016/j.jchb.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 30.Larson N., Wall M., Story M., Neumark-Sztainer D. Home/family, peer, school, and neighborhood correlates of obesity in adolescents. Obesity. 2013 doi: 10.1002/oby.20360. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martínez-Vizcaíno V., Solera-Martínez M., Cavero-Redondo I., García-Prieto J.C., Arias-Palencia N., Notario-Pacheco B. Association between parental socioeconomic status with underweight and obesity in children from two Spanish birth cohorts: a changing relationship. BMC Public Health. 2015 Dec;15(1):1276. doi: 10.1186/s12889-015-2569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WRONKA I. Socioeconomic status, body mass index and prevalence OF underweight And overweight Among polish girls aged 7–18: a longitudinal study. J Biosoc Sci. 2013;46:449–461. doi: 10.1017/s002193201300031x. 04. [DOI] [PubMed] [Google Scholar]
- 33.Ludwig J., Sanbonmatsu L., Gennetian L., Adam E., Duncan G.J., Katz L.F. Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med. 2011 Oct 20;365(16):1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gurzkowska B., Kułaga Z., Grajda A., Góźdź M., Wojtyło M., Litwin M. The relationship between selected socioeconomic factors and thinness among Polish school-aged children and adolescents. Eur J Pediatr. 2017;176(6):797–806. doi: 10.1007/s00431-017-2912-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sobal J., Stunkard A. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105(2):260–275. doi: 10.1037//0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 36.Hanson M., Chen E. Socioeconomic status and health behaviors in adolescence: a review of the literature. J Behav Med. 2007;30(3):263–285. doi: 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 37.Monteiro C., Conde W., Popkin B. Part I. What has happened in terms of some of the unique elements of shift in diet, activity, obesity, and other measures of morbidity and mortality within different regions of the world? Public Health Nutr. 2002;5(1a) doi: 10.1079/phn2001281. [DOI] [Google Scholar]
- 38.Kann L., Kinchen S.A., Williams B.I., Ross J.G., Lowry R., Grunbaum J.A., Kolbe L.J. Youth risk behavior surveillance—United States, 1999. J Sch Health. 2000 Sep;70(7):271–285. doi: 10.1111/j.1746-1561.2000.tb07252.x. [DOI] [PubMed] [Google Scholar]
- 39.Global school-based student health survey (GSHS) World Health Organization; 2019. http://www.who.int/chp/gshs/en/ Published. [Google Scholar]
- 40.Doak C., Adair L., Bentley M., Monteiro C., Popkin B. The dual burden household and the nutrition transition paradox. Int J Obes. 2004;29(1):129–136. doi: 10.1038/sj.ijo.0802824. [DOI] [PubMed] [Google Scholar]