Abstract
Background
Approximately 2.6 million babies are stillborn each year globally, of which 98% occur in low- and middle-income countries (LMICs). A 2019 individual participant data meta-analysis of 6 studies from high-income countries found that maternal supine going-to-sleep position increased the risk of stillbirth. It is not clear whether this impact would be the same in LMICs, and the normal sleep behaviour of pregnant women in LMICs is not well understood.
Objective
Determine the prevalence of different sleeping positions among pregnant women in LMICs, and what (if any) positions were associated with stillbirth using a systematic review.
Search strategy
We systematically searched the databases Medline, Embase, Emcare, CINAHL and Global Index Medicus for relevant studies, with no date or language restrictions on 4 April 2020. Reference lists of included studies were also screened.
Selection criteria
Observational studies of maternal sleep position during pregnancy in LMICs
Data collection and analysis
Recovered citations were screened and eligible studies were included for extraction. These steps were performed by two independent reviewers. Risk of bias was assessed using the Newcastle–Ottawa Scale.
Main results
A total of 3480 citations were screened but only two studies met the inclusion criteria. The studies were conducted in Ghana and India and reported on different maternal sleep positions: supine and left lateral. In Ghana, a prevalence of 9.7% for supine sleeping position amongst 220 women was found. The primary outcome could not be extracted from the Indian study as sleep position information was only reported for women who had a stillbirth (100 of the 300 participants).
Conclusion
There is limited information on maternal sleeping position in LMICs. Since sleep position may be a modifiable risk factor for stillbirth, there is a need for further research to understand the sleep practices and behaviours of pregnant women in LMICs.
PROSPERO registration: CRD42020173314
Keywords: Sleep position, Pregnancy, Stillbirth, Low- and middle-income countries
Plain english summary
In 2015, there were an estimated 2.6 million stillborn babies worldwide, and 98% of these babies were born in LMICs. In order to decrease the global incidence of stillbirth there has been recent interest in investigating aspects of maternal lifestyle during pregnancy that may be associated with an increased risk of stillbirth. One particular aspect of interest is maternal sleep position. There have been two recent systematic reviews that have evaluated the impact of maternal sleep on fetal outcomes and investigated the effect of maternal sleep positions on stillbirth. Both reviews found that maternal supine sleep position was associated with an increased risk of late stillbirth. However, the vast majority of included studies were conducted in HICs indicating that the normal sleep behaviour of pregnant women in LMICs is not well understood.
We aimed to conduct a systematic review to determine the prevalence of different sleep positions during pregnancy amongst pregnant women in LMICs and investigate if these positions were associated with stillbirth. In order to conduct this systematic review, we created a search strategy to systematically search online databases for observational studies of maternal sleep position during pregnancy in LMICs. We searched five databases on 4 April 2020, these were: Medline, Embase, Emcare, CINAHL and Global Index Medicus. Reference lists of included studies were also screened. The recovered citations were screened in duplicate and studies deemed eligible by two independent reviewers were included for extraction. The risk of bias of the included studies was assessed using NOS.
Background
In 2015, there was an estimated 2.6 million late (at or after 28 weeks’ pregnancy) stillbirths worldwide, which equates to more than 7178 deaths per day [1]. This makes stillbirth the fifth leading cause of death globally; surpassing HIV/AIDS, road traffic accidents and any type of cancer [2]. The majority of stillborn babies are born in low- and middle-income countries (LMICs)—an estimated 98% of all cases [1]. In order to decrease the global incidence of stillbirth, it is critical to identify innovative, effective and low-cost strategies to prevent stillbirth. Interest in modifying maternal sleep position during pregnancy followed the publication of a novel study by Stacey et al. in 2011 [3]. This study, undertaken in New Zealand, found an association between maternal supine sleep position during pregnancy and an increased risk of stillbirth.
The association of maternal supine sleep position with an increased risk of stillbirth is biologically plausible. As pregnancy progresses there is increased aortic and inferior vena caval compression by the gravid uterus [4]. In the supine position this compression is exacerbated and can result in up to an 85% decrease in blood flow through the woman’s inferior vena cava and up to a 30% decrease through the aorta [5–7]. This can in turn lead to a decrease in maternal cardiac output and stroke volume, reducing perfusion of the placental and fetal circulation [8–11]. This can decrease fetal oxygenation and may compromise fetal wellbeing [5, 11, 12].
Similar findings to Stacey et al. have been observed in other studies with similar methodologies and similar effect sizes conducted in high-income countries (HICs) [3, 13–15]. As a result, going-to-sleep on the side positions from 28 weeks of pregnancy are now recommended in Australia, New Zealand and the United Kingdom and have been targeted through stillbirth prevention campaigns [16–18]. There have also been two recent systematic reviews—a 2018 scoping review by Warland et al. and a 2019 individual participant data (IPD) meta-analysis by Cronin et al. that have evaluated the impact of maternal sleep on fetal outcomes [19, 20]. Both reviews found an association between supine sleep position and stillbirth, however the IPD meta-analysis did not include any studies from LMICs, as no studies met the inclusion criteria. The findings from these reviews are of interest because maternal sleep behaviours are potentially modifiable, even in low-resource settings [21]. However, since the vast majority of stillbirths occur in LMICs it is important that maternal sleep behaviours in LMICs be evaluated. We also chose to examine the association in studies from LMICs only, as there is considerable variation in what constitutes normal sleep practices between countries and cultures [22–25]. This systematic review aims to fill this knowledge gap by summarizing the available data on the prevalence of maternal sleep positions during pregnancy in LMICs, and assessing whether there is an association between maternal sleep positions and stillbirth among women in LMICs.
Methods
This systematic review was conducted in accordance with PRISMA guidelines (see Additional file 1: for PRISMA checklist), and PROSPERO registration number is: CRD42020173314 [26].
Eligibility criteria
For this systematic review, eligible studies were those reporting prevalence of maternal sleeping position during pregnancy in LMICs (as defined using the World Bank classification for 2021) [27]. Peer-reviewed, non-randomised studies (including observational and cross-sectional studies) were eligible for inclusion. The population of interest was pregnant women from LMICs, regardless of maternal age, gestation, singleton or multiple pregnancy or risk of pregnancy complications.
Literature searching, data collection and analysis
We searched Medline, Global Index Medicus, Embase, Emcare and CINAHL for relevant studies with no date or language restrictions, and excluded animal studies (see Additional file 2: for search strategy). Additionally, the reference lists of included studies were also screened. All recovered citations were imported into Covidence and duplicates were automatically removed [28] Two authors independently screened titles and abstracts of all identified citations for eligibility, followed by the full-texts. Data were then extracted from the eligible studies and risk of bias was assessed using the Newcastle Ottawa-Scale (NOS).
We extracted data including study design, setting, location, population, and prevalence of maternal sleeping positions using a pre-designed tool (Additional file 3). Data were extracted separately by each reviewer, with results compared to identify differences which were resolved through discussion or consulting a third, more senior, reviewer. Insufficient data were identified to perform a meta-analysis and all data were reported descriptively. Future updates of this review may identify further data, in which case a meta-analysis can be performed. To assess the risk of bias for included studies we used the NOS tool for cohort and case–control studies, and an adapted NOS tool for cross-sectional studies [29, 30].
Results
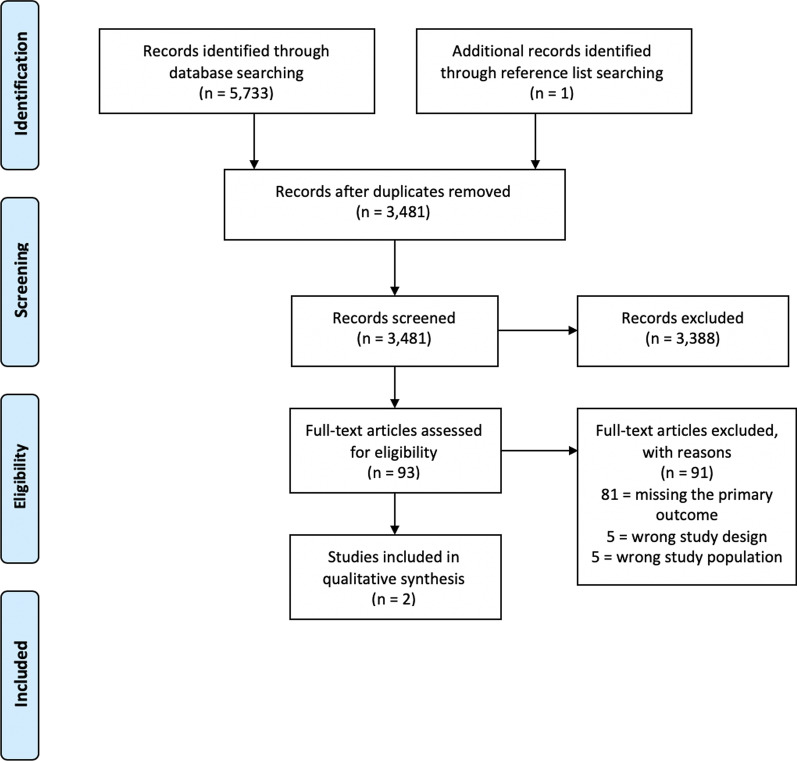
A total of 5733 citations were identified through the search, and one unique citation through reference list screening. After duplicates were removed, 3481 unique citations remained (Fig. 1). In total, 3388 citations were excluded during the title and abstract screening and 93 full-text articles were reviewed. Of these, two citations were eligible [31, 32]. The remaining studies were excluded due to not reporting the primary review outcome of interest (81 citations), ineligible study design (5 citations) or ineligible study population (5 citations).
Fig. 1.
PRISMA flow diagram showing the selection of eligible studies
The two eligible studies were a 2013 cross-sectional study conducted in Ghana, and a 2017 case–control study conducted in India [31, 32]. Table 1 describes the study level characteristics of the included studies, and Table 2 reports the differences in maternal and pregnancy characteristics and sleep practices between study participants, though both studies provided limited demographic data. The risk of bias of both studies as per NOS assessment was high (score of one) for the Lakshmi et al. study and moderate (score of six) for the Owusu et al. study (Table 3).
Table 1.
Characteristics of included studies
| Study level characteristics | Owusu et al. [31] | Lakshmi et al. [32] |
|---|---|---|
| Location | Accra, Ghana | Trivandrum, India |
| Length of study | June 2011–July 2011 | March 2014–September 2015 |
| Study design | Retrospective hospital-based cross-sectional study | Hospital-based case–control study |
| Population | Postpartum women; 0–48 h postpartum | Postpartum women |
| Main outcome measure | To investigate the prevalence of sleep disruption and sleep practices among Ghanaian women and to investigate its association with maternal and neonatal outcomes | To identify any possible modifiable risk factors and reduce stillbirth rate on a long-term perspective |
| Description of sleep position | Most common sleep position during pregnancy | Not defined |
| Data collection—sleep position | Self-reported | Self-reported |
| Data collection—stillbirth information | Clinical notes | Hospital data |
Table 2.
Participant level characteristics and going-to-sleep position
| Characteristics | Owusu et al. [31] | Lakshmi et al. [32] |
|---|---|---|
| Total participants | 220 |
Case (participants who had a stillbirth) n = 100 Control (participants who had a live birth) n = 200 Total = 300 |
| Nationality | Ghanaian | Indian |
| Age—mean (SD) | 29 (5.7) years | Not reported |
| Age range | Not reported | 18–40 years |
|
Parity—n (%) Nulliparous 1–2 3–4 ≥ 5 |
71 (32.3) 113 (51.4) 31 (14.1) 5 (2.3) |
Not reported |
|
Sleep position – n (%) Supine Non-supine |
21 (9.7) 195 (90.3) |
Not reported Not reported |
| Stillbirth | 9 (4.1) | 100 (percentage could not be extracted due to study design)* |
Data are number (percentage) or mean (standard deviation)
*Cases were identified as women who had a stillbirth, therefore the prevalence of stillbirth amongst participants could not be extracted
Table 3.
Newcastle–Ottawa Scale (NOS) scores for the included studies
| Selection score | Comparability score | Exposure/Outcome score | Overall score | |
|---|---|---|---|---|
| Owusu et al. 2013 | 2/5 | 2/2 | 2/3 | 6/10 |
| Lakshmi et al. 2017 | 1/4 | 0/2 | 0/3 | 1/9 |
NOS adapted for cross-sectional studies was used for the Owusu et al. study
Maximum scores: selection = 5, comparability = 2, outcome = 3, and overall = 10
High risk of bias: score ≤ 3
Medium risk of bias: score 4–7
Low risk of bias: score ≥ 8
The traditional NOS tool was used for the Lakshmi et al. study
Maximum scores: selection = 4, comparability = 2, exposure = 3 and overall = 9
High risk of bias: score ≤ 3
Medium risk of bias: score 4–6
Low risk of bias: score ≥ 7
The cross-sectional study by Owusu et al. with a sample size of 220 postpartum women found that 9.7% of participants reported supine sleep position. The remaining 90.3% had varied lateral sleep positions. The prevalence of stillbirth among participants was 4.09%. Owusu et al. found an increase in the odds of stillbirth associated with supine sleeping position compared to non-supine sleeping positions, reporting an odds ratio of 8.00, 95% CI 1.50–43.20, p = 0.016.
The 2017 case–control study by Lakshmi et al. aimed to identify possible modifiable risk factors for stillbirth. An included risk factor was maternal sleep position, so the study reported the prevalence of maternal left lateral sleep position during pregnancy. Due to the study design, sleep position data were only reported from participants who had a stillbirth, the cases in this case–control study. Sleep position data was not collected for the controls, women who had a live birth. Therefore, the prevalence of left lateral sleeping position during pregnancy among all women could not be extracted and the risk of stillbirth associated with sleep position could not be calculated. Among women who experienced stillbirth, Lakshmi et al. found an increase in the odds of non-left lateral sleeping positions compared to a left lateral sleeping position during pregnancy (OR 2.27, 95% CI 1.37–3.76, p < 0.001).
The risk of bias of studies as per NOS assessment was considered to be high for the Lakshmi et al. study and moderate for the Owusu et al. study (Table 3). Publication bias could not be assessed due to the small number of eligible studies.
Discussion
Main findings
This systematic review identified very limited data on maternal sleep position during pregnancy in LMICs, and it is currently not possible to draw conclusions. Two eligible studies were identified and reported on different sleep positions; supine and left lateral [31, 32]. In Ghana, Owusu et al. found that women who reported they most commonly slept in a supine sleep position in pregnancy were 8.0 times more likely to experience stillbirth than women who did not (OR 8.00, 95% CI 1.50–43.20, p = 0.016) [31]. In India, Lakshmi et al. reported women who had experienced stillbirth were 2.3 times more likely to report sleeping in a non-left lateral sleep position, compared to a left lateral sleep position (OR 2.27, 95% CI 1.37–3.76, p < 0.00) [32]. Overall, this systematic review has demonstrated that the sleep behaviours of women in LMICs during pregnancy are not well documented, despite the established association between maternal sleep position and stillbirth. However, the limited information available aligns with existing evidence from HICs that maternal going-to-sleep position is associated with an increased risk of stillbirth [19]. The very limited available information also suggests that the effect size may be consistent with those from HICs, though this might change with additional evidence. There remains a need for further high-quality research to investigate maternal sleep practices and behaviours in pregnant women from LMICs.
Strengths and limitations
This systematic review has some limitations. Firstly, although a comprehensive search was undertaken, only peer-reviewed studies were eligible. There is a possibility that eligible studies were not found in the search, although we consider this to be unlikely because reference list screening was performed in conjunction with a broad search strategy. Second, a meta-analysis could not be performed due to differences in outcome reporting between the two eligible studies. Third, the findings of this systematic review are based on two studies with small sample sizes. Both studies were also conducted in a hospital setting so the samples are not representative of all pregnant women in either country, or in LMIC settings broadly, given the high proportion of women who do not attend hospital during pregnancy. Both included studies were reliant on the postpartum participants recalling their sleep position during pregnancy. The participants stillbirth status may have also influenced the accuracy of recall. It is possible that the experience of the stillbirth may have influenced the accuracy of recall of maternal sleep position [33, 34]. If families know that supine position is associated with an increased risk then this may alter their recollection; though whether this experience improves or worsens recall of sleep position is not yet known. Another limitation is that there are differing definitions of sleep position [13]. Furthermore, the gestational age at which sleep position was measured varied between the included studies. Should advice on sleep position be incorporated into antenatal care more widely, the optimal timing of this intervention and how best to communicate it to pregnant women and healthcare providers needs to be carefully considered. A strength of our systematic review is that a broad search strategy was conducted across multiple databases and reference lists were searched for additional studies. Also, the search strategy had no limitations on language or publication date.
Interpretation
Two recent publications, a scoping review and IPD meta-analysis, have reviewed the evidence regarding supine sleep position and stillbirth [19, 20]. The IPD meta-analysis reported on all available, eligible studies on the topic. The 2013 study from Ghana by Owusu et al. was not included in that review due to ineligibility of study design. Both of the eligible studies for this review were included in the meta-analysis of the scoping review but the odds ratio estimate is not reliable due to the heterogeneous data Warland et al. used [19, 20]. The findings from the publications conducted in HICs has instigated the creation of educational stillbirth prevention campaigns in Australia, New Zealand and the United Kingdom [35]. These campaigns are targeted at pregnant women with a gestational age from 28 weeks with advice to modify going-to-sleep positions to adopt a left lateral sleep position.
Since our review identified only two studies conducted exclusively in LMICs, insufficient data was found to confirm the prevalence of maternal sleep positions. An observational study conducted in a low- and middle-income setting will be required to determine the prevalence of different maternal sleep positions among pregnant women from LMICs and if any positions are associated with an increased risk of stillbirth. Only once further research in this area is conducted can public health campaigns be created.
Conclusion
This systematic review provides a summary of the available evidence regarding the prevalence of different maternal sleep positions during pregnancy and associated risk of stillbirth in LMICs. There is limited evidence available and as such the prevalence of sleep positions and associated stillbirth risk in LMICs remains inconclusive, given the lack of robustly conducted studies in these settings. Given supine going-to-sleep position has been found to be associated with an increased risk of late stillbirth in high-income settings, this suggests that sleep position may be a modifiable risk factor for stillbirth in LMICs. However, there is a need for further research to understand the sleep practices and behaviours of pregnant women in LMICs before public health initiatives can be developed and implemented.
Supplementary Information
Additional file 3. Data extraction tool.
Acknowledgements
We acknowledge Ms Lorena Romero for her assistance in developing the search strategy. The manuscript represents the views of the named authors only.
Abbreviations
- AOR
Adjusted odds ratio
- CI
Confidence interval
- HIC
High-income country
- IPD
Individual participant data
- LMIC
Low- and middle-income country
- NOS
Newcastle–Ottawa Scale
- OR
Unadjusted odds ratio
Authors’ contributions
The concept of this systematic review was conceived by JPV and CSEH. The protocol was written by SKR and JPV. Screening and data extraction were performed by SKR and SA. SKR, SA, ANW, LCT, TS, CSEH and JPV contributed to the write up. All authors read and approved the final manuscript.
Funding
No external funding was received.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12978-021-01106-x.
References
- 1.World Health Organization. Stillbirths 2020. https://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/. Accessed 17 Feb 2021.
- 2.Aminu M, van den Broek N. Stillbirth in low- and middle-income countries: addressing the 'silent epidemic'. Int Health. 2019;11(4):237–239. doi: 10.1093/inthealth/ihz015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stacey T, Thompson JM, Mitchell EA, Ekeroma AJ, Zuccollo JM, McCowan LM. Association between maternal sleep practices and risk of late stillbirth: a case-control study. BMJ. 2011;342:d3403. doi: 10.1136/bmj.d3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kember AJ, Scott HM, O'Brien LM, Borazjani A, Butler MB, Wells JH, et al. Modifying maternal sleep position in the third trimester of pregnancy with positional therapy: a randomised pilot trial. BMJ Open. 2018;8(8):e020256. doi: 10.1136/bmjopen-2017-020256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Humphries A, Mirjalili SA, Tarr GP, Thompson JMD, Stone P. The effect of supine positioning on maternal hemodynamics during late pregnancy. J Matern Fetal Neonatal Med. 2019;32(23):3923–3930. doi: 10.1080/14767058.2018.1478958. [DOI] [PubMed] [Google Scholar]
- 6.Milsom I, Forssman L. Factors influencing aortocaval compression in late pregnancy. Am J Obstet Gynecol. 1984;148(6):764–771. doi: 10.1016/0002-9378(84)90563-5. [DOI] [PubMed] [Google Scholar]
- 7.Rossi A, Cornette J, Johnson MR, Karamermer Y, Springeling T, Opic P, et al. Quantitative cardiovascular magnetic resonance in pregnant women: cross-sectional analysis of physiological parameters throughout pregnancy and the impact of the supine position. J Cardiovasc Magn Reson. 2011;13:31. doi: 10.1186/1532-429X-13-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerr MG, Scott DB, Samuel E. Studies of the inferior vena cava in late pregnancy. Br Med J. 1964;1(5382):5224–5233. doi: 10.1136/bmj.1.5382.522. [DOI] [PubMed] [Google Scholar]
- 9.Kauppila A, Koskinen M, Puolakka J, Tuimala R, Kuikka J. Decreased intervillous and unchanged myometrial blood flow in supine recumbency. Obstet Gynecol. 1980;55(2):203–205. [PubMed] [Google Scholar]
- 10.Jeffreys RM, Stepanchak W, Lopez B, Hardis J, Clapp JF., 3rd Uterine blood flow during supine rest and exercise after 28 weeks of gestation. BJOG. 2006;113(11):1239–1247. doi: 10.1111/j.1471-0528.2006.01056.x. [DOI] [PubMed] [Google Scholar]
- 11.Khatib N, Weiner Z, Beloosesky R, Vitner D, Thaler I. The effect of maternal supine position on umbilical and cerebral blood flow indices. Eur J Obstet Gynecol Reprod Biol. 2014;175:112–114. doi: 10.1016/j.ejogrb.2013.12.043. [DOI] [PubMed] [Google Scholar]
- 12.Stone PR, Burgess W, McIntyre J, Gunn AJ, Lear CA, Bennet L, et al. An investigation of fetal behavioural states during maternal sleep in healthy late gestation pregnancy: an observational study. J Physiol. 2017;595(24):7441–7450. doi: 10.1113/JP275084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordon A, Raynes-Greenow C, Bond D, Morris J, Rawlinson W, Jeffery H. Sleep position, fetal growth restriction, and late-pregnancy stillbirth: the Sydney stillbirth study. Obstet Gynecol. 2015;125(2):347–355. doi: 10.1097/AOG.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 14.McCowan LME, Thompson JMD, Cronin RS, Li M, Stacey T, Stone PR, et al. Going to sleep in the supine position is a modifiable risk factor for late pregnancy stillbirth; Findings from the New Zealand multicentre stillbirth case-control study. PLoS ONE. 2017;12(6):e0179396. doi: 10.1371/journal.pone.0179396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heazell A, Li M, Budd J, Thompson J, Stacey T, Cronin RS, et al. Association between maternal sleep practices and late stillbirth - findings from a stillbirth case-control study. BJOG. 2018;125(2):254–262. doi: 10.1111/1471-0528.14967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cure Kids. ‘Sleep on side; stillbirth prevention campaign’ launched nationally 2018. https://curekids.org.nz/news/sleep-on-side-stillbirth-prevention-campaign-launched-nationally/. Accessed 17 Feb 2021.
- 17.United Kingdom National Health Service. Reducing the risk of stillbirth 2018. https://www.nhs.uk/conditions/pregnancy-and-baby/reduce-risk-of-stillbirth-safer-pregnant/. Accessed 17 Feb 2021.
- 18.Stillbirth Centre of Research Excellence. Safer Baby Bundle 2020. https://www.stillbirthcre.org.au/safer-baby-bundle/. Accessed 17 Feb 2021.
- 19.Cronin RS, Li M, Thompson JMD, Gordon A, Raynes-Greenow CH, Heazell AEP, et al. An Individual Participant Data Meta-analysis of Maternal Going-to-Sleep Position, Interactions with Fetal Vulnerability, and the Risk of Late Stillbirth. EClinicalMedicine. 2019;10:49–57. doi: 10.1016/j.eclinm.2019.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warland J, Dorrian J, Morrison JL, O'Brien LM. Maternal sleep during pregnancy and poor fetal outcomes: A scoping review of the literature with meta-analysis. Sleep Med Rev. 2018;41:197–219. doi: 10.1016/j.smrv.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Cronin RS, Chelimo C, Mitchell EA, Okesene-Gafa K, Thompson JMD, Taylor RS, et al. Survey of maternal sleep practices in late pregnancy in a multi-ethnic sample in South Auckland, New Zealand. BMC Pregnancy Childbirth. 2017;17(1):190. doi: 10.1186/s12884-017-1378-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knutson KL. Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Soc Sci Med. 2013;79:7–15. doi: 10.1016/j.socscimed.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prall SPYG, Scelza BA, Siegel JM. The influence of age- and sex-specific labor demands on sleep in Namibian agropastoralists. Sleep Health. 2018;4(6):500–508. doi: 10.1016/j.sleh.2018.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knutson KL. Sleep duration, quality, and timing and their associations with age in a community without electricity in Haiti. Am J Hum Biol. 2014;26(1):80–86. doi: 10.1002/ajhb.22481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crittenden AN, Samson DR, Herlosky KN, Mabulla IA, Mabulla AZP, McKenna JJ. Infant co-sleeping patterns and maternal sleep quality among Hadza hunter-gatherers. Sleep Health. 2018;4(6):527–534. doi: 10.1016/j.sleh.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 26.PRISMA. PRISMA checklist 2015 [Available from: http://prisma-statement.org/PRISMAStatement/Checklist. Accessed 17 Feb 2021.
- 27.The World Bank Group. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 17 Feb 2021.
- 28.Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia. Available at: www.covidence.org. Accessed 17 Feb 2021.
- 29.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2019. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 17 Feb 2021.
- 30.Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in europe: a systematic review and meta-analysis. PLoS ONE. 2016;11(1):e0147601. doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Owusu JT, Anderson FJ, Coleman J, Oppong S, Seffah JD, Aikins A, et al. Association of maternal sleep practices with pre-eclampsia, low birth weight, and stillbirth among Ghanaian women. Int J Gynaecol Obstet. 2013;121(3):261–265. doi: 10.1016/j.ijgo.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lakshmi ST, Thankam U, Jagadhamma P, Ushakumari A, Chellamma N, Hariharan SV. Risk factors for still birth: a hospital based case control study. Int J Reprod Contracept Obstet Gynecol. 2017;6(3):970–974. doi: 10.18203/2320-1770.ijrcog20170567. [DOI] [Google Scholar]
- 33.Mackenzie SG, Lippman A. An investigation of report bias in a case-control study of pregnancy outcome. Am J Epidemiol. 1989;129(1):65–75. doi: 10.1093/oxfordjournals.aje.a115125. [DOI] [PubMed] [Google Scholar]
- 34.Drews CD, Kraus JF, Greenland S. Recall bias in a case-control study of sudden infant death syndrome. Int J Epidemiol. 1990;19(2):405–411. doi: 10.1093/ije/19.2.405. [DOI] [PubMed] [Google Scholar]
- 35.Perinatal Society of Australia and New Zealand, Stillbirth Centre of Research Excellence. Position statement: Mothers’ going-to-sleep position in late pregnancy 2019. https://sanda.psanz.com.au/assets/Uploads/Position-Statement-Side-Sleeping.pdf. Accessed 17 Feb 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 3. Data extraction tool.
Data Availability Statement
Not applicable.