Significance
The question of whether firstborn children have a height advantage over later-born children is important, given the persistently poor height outcomes in developing countries. Using data on young Indian children, we show that later-born children lag behind firstborns in stunting outcomes. This is only true, though, if higher birth-order children were born within 3 y of the birth of their elder siblings. No difference in height-for-age is observed for children born with spacing of 3 or more years. India’s family planning interventions have largely focused on reducing the total fertility rate with less attention given to length of birth spacing between children. A stronger focus on increasing the time interval between births could prevent adverse stunting outcomes for surviving children.
Keywords: stunting, birth spacing, nutrition, family planning, India
Abstract
Do firstborn children have a height advantage? Empirical findings have found mostly that, yes, second or higher-order children often lag behind firstborns in height outcomes, especially in developing countries. However, empirical investigations of birth-order effects on child height overlook the potential impact that birth spacing can have. We provide an explanation for the negative birth-order effect on stunting outcomes for young Indian children and show it is driven by short preceding-birth spacing. We find that firstborn children are taller than children of higher birth order: The height-for-age gap for third (or higher)-order children is twice the gap for children second in birth order. However, this pattern is observed when spacing between later-born children and their immediate elder siblings is fewer than 3 y. Interestingly, the firstborn height advantage disappears when later-born children are born at least 3 y after their elder siblings. Thus, our findings indicate that spacing length between children explains differences in height, over birth order. Although India’s family planning policy has resulted in a substantial reduction in total fertility, its achievement in spacing subsequent births has been less impressive. In showing that spacing can alleviate or aggravate birth-order effects on attained height, our study fills an evidence gap: Reducing fertility alone may not be sufficient in overcoming negative birth-order effects. To reduce the detrimental effects of birth order on child stunting, policy responses—and therefore research priorities—require a stronger focus on increasing the time period between births.
Child undernutrition continues to be a problem in low-and middle-income countries, and adversely affects child survival and well being (1). While child undernutrition is gauged by several indicators, stunting—a key marker of chronic undernutrition obtained by comparing child height with that of children in the same age group in a healthy reference population—is at the forefront of discussion because of its vast prevalence across all developing regions and its important consequences for health and development. Almost all of stunting takes place in the first 1,000 d from conception to 2 y of age, but its consequences follow throughout adulthood. These consequences are largely irreversible, making stunting an extremely critical condition (2, 3). Children who are stunted are vulnerable to disease and mortality during childhood and run a much higher risk of developing deficits in later-life outcomes, including in adult height, cognitive and intellectual ability, and as a consequence, on schooling attainment, productivity, and earnings (4–10). Furthermore, if stunting is accompanied by excessive weight gain later in childhood, there is an increased risk of developing adult obesity and nutrition-related chronic diseases, including cardiovascular disease, stroke, and type 2 diabetes in adult life (see, for example, ref. 6). In addition, stunted girls carry additional risk of having adverse pregnancy outcomes and reproductive complications as adults, leading to detrimental intergenerational effects (11, 12). Nevertheless, stunting is preventable, and reducing it is an important component of overall development for the well being of children.
In recognition of the high social and economic costs of stunting, efforts are ongoing to address this public health issue, including programs aimed at reducing poverty and inequality, improving dietary intake and access to healthcare services, and improving the hygiene environment. Childhood stunting has declined by 35% from a global estimate of 253 million in 1990, with over 90 million children protected from suboptimal growth and a large number of child deaths prevented. However, this decrease is small relative to the overall burden, as over 161 million children under 5 y were reported to be stunted in 2011 (13). Furthermore, there is a large disparity in numbers across regions, with the highest number of over 69 million stunted children living in South Asia and with India bearing 90% of this regional burden (14). Thus, although stunting levels have been reduced, the progress has been both uneven and suboptimal (15). There is need to develop strategies, policies, and programs tailored to local conditions, which in turn require a case-by-case approach to identify what other conditions may be predisposing children to poor height in certain regions, and also, within regions.
Birth order—an indicator of a child’s position in the age hierarchy of siblings—has been used time and again to explain variation in height outcomes in children. Children born to the same parents share the same genetic make-up; yet, the order in which they are born exposes them to different biological and behavioral environments (16, 17). Through differences in health endowments and parental investments, birth order often affects the health and nutritional outcomes of children. Hence, birth-order effects reflect differences in the unshared environment within a family. The literature on child stunting has provided significant evidence from across countries that children of lower birth order are at an advantage, compared to children of higher birth order. Firstborn children are taller compared to those born subsequently, and this height advantage increases sharply over the higher order of birth of siblings. Explanations for the firstborn height advantage have addressed issues, such as better health endowments of the firstborn at birth and parental favoritism toward some offspring over others—usually the eldest son—generating more prenatal and postnatal investments, greater time investment in child care, longer duration of breastfeeding, and also affecting the desire for having more children (18–24).
However, an important factor in assessing the birth-order effects on child health and nutritional outcomes is the length of interval between two consecutive births: That is, birth spacing. A wealth of studies have shown that a short length of birth spacing is associated with higher risk of maternal mortality and adverse subsequent birth outcomes, such as child mortality, preterm birth, small for gestational age, and low birthweight, though the degree to which the relationship holds varies substantially across countries (25–29). These associations stem from the biological factor commonly referred to as maternal depletion syndrome (26, 30). Closely spaced pregnancies may not allow sufficient time for the mother to restore her depleted micronutrient and macronutrient stores from the previous birthing, which in turn may reduce her ability to provide a favorable fetal growth environment in subsequent pregnancies and sufficient breast milk production postdelivery. Literature also suggests short birth spacing is associated with suboptimal parental care practices, which adversely affect the health and nutritional outcomes of siblings born close to each other. For example, the birth of a new baby may reduce the parental care time devoted to older siblings, as well as result in poor postnatal investment; similarly, a new pregnancy may reduce or curtail breast milk production, which may lead to suboptimal feeding for older siblings.
While the aforementioned channels show the potential for longer birth spacing to influence nutritional outcomes of children more positively, especially for the later born, empirical inquiry into the spacing order linkages is limited. We believe that birth order and height linkage can be better understood by examining the interaction between birth order and birth spacing. Using an illustrative example of India in this paper, we demonstrate that the negative association between increasing birth order and child height is driven by the short length of interval between births. We link height-for-age standardized scores (HAZ) of children under 5 y, recorded in the latest Indian Demographic and Health Survey (DHS), to an indicator of birth order, disaggregated by the length of preceding birth spacing. When birth order is considered alone, we find that firstborn children on average are taller than children of higher birth order. This result is consistent with previous research on birth order. However, we discover noteworthy changes in the patterns of the HAZ gap between firstborn and subsequent children on combining birth order with preceding birth spacing. We find that the firstborn height advantage is significant if birth spacing between the higher-order child and its immediate elder sibling is less than 3 y, and this advantage gets steeper with increasing order of birth; that is, the height advantage for firstborns, compared to children from third or higher-order births, is almost twice the height advantage for firstborns, compared to children of second-birth order. Interestingly, if the birth spacing between the higher birth-order child and its immediate elder sibling is 3 or more years, the firstborn height advantage disappears and becomes insignificant. This is true with respect to the gap for all higher birth-order children. Thus, higher birth-order children, on average, are as tall as firstborn children if they are appropriately spaced. Our results emphasize the importance of time between births in determining height outcomes of young children, over birth order, and demonstrate how spacing length may weaken or strengthen the birth-order effect on child height. Designing and implementing policies and interventions that affect knowledge and attitude toward healthy spacing could significantly impact the health, nutrition, and accomplishments of young children.
However, we emphasize at the outset that our analysis is exploratory in nature. An ideal dataset for comparing height outcomes across birth orders would require longitudinal data, recording all pregnancies conceived by a woman with predelivery and postdelivery information related to healthcare, as well as feeding practices for every living child. Because of the absence of datasets that cover all these aspects, we rely on DHS data, which are closely but imperfectly suited to the question at hand. The nature of DHS is such that anthropometry is recorded only for children below 5 y, and for many healthcare and dietary intake variables the information is collected only for the youngest child born to the mother. Hence, the reduced sample size and data limitations preclude our ability to establish causality. However, the large sample size is sufficient to assess subgroup and interaction effects. We address several possible biases or limitations of using survey data with additional analyses.
Variation in Child Height by Birth Order and Birth Spacing
The data used in this paper come from the fourth round of India’s DHS, commonly known as National Family Health Survey-4 (NFHS-4), which was conducted in 2015 to 2016. The survey provides nationally representative sample data on the health and demography of the Indian population. Since NFHS-4 collected height data only for living children under 5 y, our analysis is restricted to this age group and the analytical sample is comprised of 223,662 children. Additional sample details are covered in Data Description and summary statistics are provided in SI Appendix, Table S1.
The birth order of the children in our sample averages around 2.26 (for details, see SI Appendix, Table S1), slightly less than the average number of children Indian women have over their lifetime (total fertility rate is 2.54 children per woman). We, therefore, classify birth order into three categories: Firstborn for children with birth order 1, secondborn for children with birth order 2, and third(+)-born for children with birth order 3 and higher. SI Appendix, Fig. S1A shows that ∼63% of the sample is comprised of later-born births [i.e., secondborn and third(+)-born]. Later-born children, by definition, have elder siblings, who may or may not be surviving. We term the length of time between the birth of a later-born child and the birth of its immediate elder sibling as preceding birth spacing (PBS). This is commonly known as an interbirth interval in the literature [see, for example, Winikoff (29)]. By this definition, first-born children have no PBS. We disaggregate later-born children by their PBS and classify them as later born with PBS less than 3 y (PBS < 3 y) or later born with PBS equal to or greater than 3 y (PBS ≥ 3 y). This classification results in four categories of later-born children: Secondborn and third(+)-born, each combined with PBS < 3 y and PBS ≥ 3 y, respectively. SI Appendix, Fig. S1B shows that 60% of later-born children fall in PBS < 3 y category. The criteria of using 3 y as the cutoff is based on the World Health Organization (WHO) recommendation for women of reproductive age to have a minimum interval of at least 24 mo after a live birth before attempting the next pregnancy, to reduce the risk of adverse maternal, perinatal, and infant outcomes (31). Assuming that a healthy pregnancy should last for 9 mo, this recommendation corresponds to spacing length of 33 mo between two live births. The average PBS for later-born children in India is just a month lower than the WHO recommended level; a median of 32 mo, PBS varies widely by age group: ∼85% of the women aged 15 to 19 y and 60% of the women aged 20 to 29 y have birth spacing of less than 32 mo (for details, see SI Appendix, Table S2).
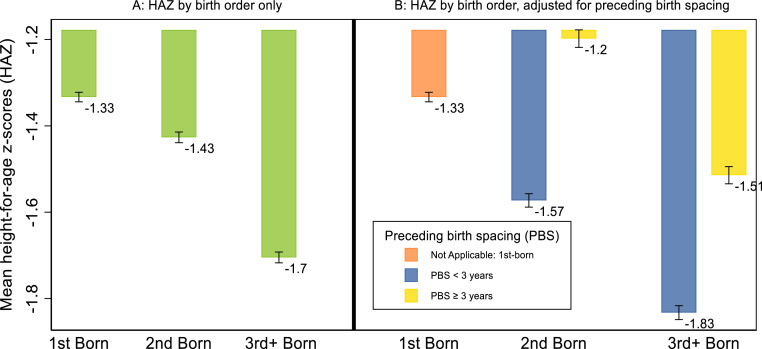
To establish the relationship between birth order, birth spacing, and child height, we begin by comparing the average HAZ by birth order. Fig. 1A shows the change in HAZ by birth order, pooling all children under 5 y, living in either rural or urban areas.
Fig. 1.
Child height by birth order. The bars represent the mean HAZ for Indian children. (A) Plot of the mean HAZ by birth order only. (B) Split of the later-born children [secondborn and third(+)-born] by length of PBS (PBS < 3 y and PBS ≥ 3 y) and plot of the mean HAZ by order-spacing categories. The mean HAZ is calculated over all children under 5 y living in rural and urban India. The confidence band is constructed at the 5% level of significance.
Moving from firstborns to higher-order births, we see that a height deficit emerges, and this deficit increases sharply with birth order; the height gap between third(+)-born and firstborns is four times the gap between secondborns and firstborns. The gap explains the negative effect of higher birth order. Fig. 1B substantiates the key fact that underlies our analysis: Short PBS largely explains the firstborn height advantage. Upon plotting HAZ against the combined measure of birth order and PBS with five categories, firstborn plus four interacted categories of later-born children [secondborn and third(+)-born categories interacted with two PBS categories], we observed that height has greater reactivity to birth spacing, over birth order, leading to worse HAZ outcomes for those born with PBS < 3 y, but relatively better outcomes for those with PBS ≥ 3 y. For example, the average HAZ deficit for secondborn, relative to firstborn, is 0.1 SD, without adjusting for PBS. After adjusting for spacing length, the deficit more than doubles for secondborn with PBS < 3 y, and changes sign to show a surplus of 0.1 SD for those with PBS ≥ 3 y.* A similar pattern of widening and shrinking height deficit is observed with shorter and longer PBS, respectively, for third(+)-born children, although the mean HAZ for third(+)-born continues to be worse than firstborn across different PBS categories. Thus, on average, the negative-order effects on HAZ outcomes, as seen in Fig. 1A, are largely seen for children with PBS < 3 y in Fig. 1B.
To establish how the relationship works in a regression approach, we first show the independent association between child HAZ outcomes and birth order by estimating Eq. 1, below. As poor height may result from a complex interaction of deep social, economic, and political processes, as well as water quality, disease burdens, and sanitation, driving these intermediate outcomes, we include several background variables and controls in our regressions to rule out the possibility of spurious association. The summary statistics on the relevant controls are presented in SI Appendix, Table S1.
| [1] |
where Yimd is the HAZ outcome for child i born to mother m in district d; β1 (β2), commonly referred to as the birth-order gradient, estimates the order effect, that is, the height gap between secondborn children [third(+) birth-order children] and the firstborn children (omitted birth order category); δ is a vector of coefficients for Ximd, which is a matrix of controls for background characteristics that affect children’s height outcomes.
Column 1 in Table 1 shows the coefficients of the linear regression of HAZ for children below 5 y of age. The birth-order effect persists when we control for a broad set of demographics and socioeconomic and environmental predictors of child height, although the magnitudes have changed slightly. Relative to being born first, children born later have worse height outcomes. In terms of magnitude, the height deficit is double in size for third(+)-born (–0.22 SD) than secondborn (–0.11 SD), implying the farther the rank of the child in the age-hierarchy of all its siblings, the poorer the HAZ.
Table 1.
The effect of birth order on child HAZ, by preceding birth spacing
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Secondborn | −0.11*** (0.01) | |||||
| Third(+)-born | −0.22*** (0.01) | |||||
| Secondborn × PBS < 3 y | −0.16*** (0.01) | −0.16*** (0.01) | −0.16*** (0.03) | −0.15*** (0.03) | −0.39*** (0.07) | |
| Secondborn × PBS ≥ 3 y | 0.01 (0.02) | 0.01 (0.02) | 0.02 (0.03) | 0.03 (0.03) | −0.18** (0.08) | |
| Third(+)-born × PBS < 3 y | −0.26*** (0.02) | −0.26*** (0.02) | −0.25*** (0.03) | −0.22*** (0.04) | −0.65*** (0.08) | |
| Third(+)-born × PBS ≥ 3 y | −0.06*** (0.02) | −0.05** (0.02) | −0.04 (0.03) | −0.01 (0.04) | −0.25*** (0.08) | |
| Mean outcome of firstborn | −1.35 | −1.35 | −1.35 | −1.35 | −1.35 | −1.35 |
| PSU FE | No | No | Yes | Yes | Yes | No |
| Mother’s FE | No | No | No | No | No | Yes |
| Gestation length | No | No | No | Yes | Yes | Yes |
| Previous pregnancy status | No | No | No | Yes | Yes | Yes |
| Sibling size | No | No | No | No | Yes | No |
| Observations | 212,774 | 212,774 | 211,787 | 211,461 | 211,461 | 91,653 |
| R2 | 0.165 | 0.165 | 0.324 | 0.325 | 0.325 | 0.676 |
Authors’ calculation using sample of children aged 0 to 60 mo with valid data on child height, birth order, and birth spacing, extracted from NFHS-4 (2015/16). SEs appear in brackets and are clustered by mother in all regressions. Firstborn is an indicator for children whose birth order is 1 and is the omitted category; secondborn is an indicator for children whose birth order is 2; third(+)-born is an indicator for children whose birth order is 3 or higher; PBS < 3 y is an indicator for children who were born within 36 mo of the preceding birth to their mother; PBS ≥ 3 y is an indicator for children who were born 36 or more months after the preceding birth to their mother. Columns 1 and 2 include child-level variables: An indicator for child’s age (in months), gender and type of pregnancy outcome (single or multiple); mother-level variables, such as mother’s age at birth, height (in centimeters), a measure of diet diversity, and indicator variables for mother’s education, daily television viewing, reading of news weekly or more frequently, and low body mass index; household controls, which include a measure for household wealth computed using International Wealth Index, the number of people living in the household, and indicators for caste and religion of the head of the household head, access to safe handwashing facilities, access to piped water for drinking, open defecation, following of safe stool disposal practices, and a measure of community-level availability of improved toilet and location-specific controls (rural or urban and district dummies). Column 3 is the PSU FE and is on the sample of clusters with two or more children less than 5 y old. Cluster in NFHS sampling refers to the PSU, which is a village in rural India and a block or neighborhood in urban India. Column 4 is PSU FE + additional control for the confounding effect of duration of pregnancy and outcome of previous pregnancy of the mother (alive, dead, or terminated); this is our preferred/main specification. Column 5 controls for the confounding effect of sibling size along with column 4 controls. Column 6 is a mother’s FE is on the sample of mothers with two or more children less than 5 y of age. **P < 0.05, ***P < 0.01.
To document how the HAZ gap unfolds across different lengths of birth spacing, we estimate Eq. 2, which expands the later-born birth-order categories to include the length of PBS†:
| [2] |
By considering an interaction of birth order with PBS, we disaggregate the height disadvantage by spacing length. Column 2 in Table 1 shows the regression coefficients obtained upon replacing the birth-order variable in the previous model (column 1 in Table 1) with an interacted measure of birth order and birth spacing. We find that the HAZ deficit for children of higher birth order widens if they were born with a PBS < 3 y; secondborns are 0.16 SD shorter than firstborns, whereas the deficit for third(+)-borns is 0.26 SD. Interestingly, with the recommended PBS ≥ 3 y, the deficit completely disappears for secondborns (0.01 SD) and for third(+)-borns, although it remains weakly significant at 5%, the deficit decreases considerably in magnitude (–0.06 SD). Hence, consistent with the pattern previously observed in Fig. 1, the strength and direction of the relationship between birth order and child height vary by spacing length.
As mentioned earlier, DHS does not offer the ideal structure to estimate the effect of birth spacing. There are endogeneity concerns, which could potentially confound our estimates of interest, and we have made several attempts to account for them within the bounds imposed by the nature of the NFHS/DHS data. The first confounding effect arises from unobserved community-level heterogeneity (32). It is well established that height outcomes in India differ substantially by location; it may happen that fertility behavior is correlated within a community. To overcome this, we ran a cluster-level fixed-effect (FE) regression that accounts for time-invariant geographical differences that might affect child outcomes. This automatically controls for rural and urban differences. Cluster in NFHS-4 sampling refers to the primary sampling unit (PSU), which is a village in rural India and a block or neighborhood in urban India. Column 3 of Table 1 reports the cluster-level FE (or PSU FE), and we see there is no significant change in the magnitude of coefficient estimates. The second important confounding effect may arise from the definition of the birth spacing variable, as highlighted in the child mortality literature [see, for example, Winikoff (29)]. Some might argue that the interpregnancy interval (i.e., the length of time between two conceptions) is a better way to measure spacing length, as it also accounts for terminated pregnancies. This can also be a cause of concern, as the recommended level of spacing following a terminated pregnancy is different from that after a live birth. However, given that reproductive history is based on recall, it is difficult to get at the exact timing of conception of all births of women, and we use the interbirth interval. To rule out the possibility of any bias, we controlled for whether there were any terminated pregnancies in between the two births considered to calculate the PBS, as well as the approximate duration of pregnancy of the reference child. In addition, we controlled for the living status of the elder sibling of later born children, as literature has shown that for the same spacing and order, a child whose previous sibling is surviving has poor HAZ compared to a child with an elder sibling that has not survived (33). Controlling for these factors in column 4 of Table 1 does not change the pattern or magnitude of the coefficients attached with PBS < 3 y. Interestingly, for PBS ≥ 3 y, we saw that the coefficient on the interaction with third(+)-born becomes insignificant, like that with secondborns, implying that PBS of 3 or more years has the potential to completely offset the firstborn height advantage, even for third and higher birth-order children. We call this specification of covariates our main specification.
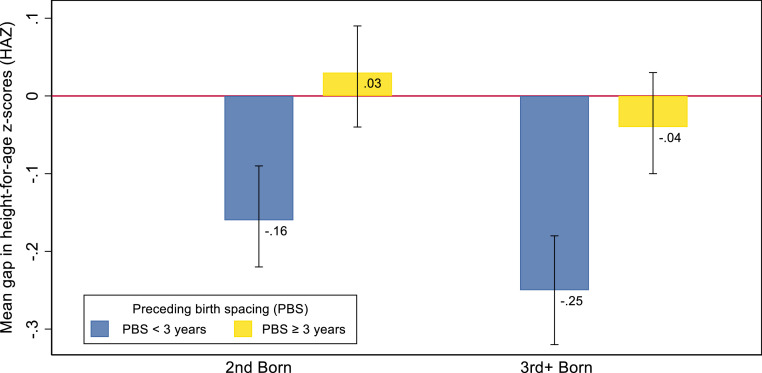
To ascertain whether the spacing effect changes with birth order, we plotted the coefficients for our main specification (column 4 of Table 1) in Fig. 2: There was no significant HAZ gap for PBS ≥ 3 y. This can be seen from the yellow bars in in Fig. 2, as they always include 0 in the confidence band. The confidence band for secondborn and third(+)-born overlap, indicating third(+)-born are as tall as secondborns as well as firstborns. An interesting takeaway from this result is that the positive effect of having a longer spacing is similar in each category of later-born children. This can be seen by adding up the coefficients in the blue and yellow bar (Fig. 2), –0.19 SD for secondborn and –0.21 SD for third(+)-born. Our finding strengthens the instrumental role that birth spacing plays in defining birth-order effects. However, for PBS < 3 y, it is important to highlight that the HAZ gap increases with birth order, indicating that negative-order effects emerge due to short spacing.
Fig. 2.
Child height gap by birth order. The bars represent the mean gap in HAZ-scores between firstborn and later-born children [secondborn and third(+)-born]. The gap is estimated for two lengths of PBS, i.e., with PBS < 3 y and PBS ≥ 3 y. The confidence band is constructed at 5% level of significance.
In column 8 of SI Appendix, Table S5, we report the results of using the WHO recommendation of 33 mo as the cutoff to classify PBS instead of 36 mo. On using this alternative criterion, we continue to see a significant height deficit for third(+)-born with PBS ≥ 33 mo. This suggests that there are threshold effects and justifies the usefulness of using the 36-mo criterion. Next, we reran the model using a continuous variable in months for PBS instead of using a 3-y cutoff and found similar patterns. The results are presented in SI Appendix, Table S6 and Fig. S4.
A potential source of bias frequently highlighted in the birth-order literature is the effect of “sibship size” (34). The height difference between firstborns and later-born children might emerge because later-born children come from larger families and larger families are more likely to be poor, which in turn may lead to poor child nutritional outcomes. We find that our estimated patterns are robust to controlling for sibling size, as seen in column 5 of Table 1. A common approach to handle the sibling size issue is to estimate a “within-family FE” (or “mother FE”) model that holds fixed the unobserved and observed mother-level factors that are common among siblings. Thus, eventual family size and genetic factors are controlled for by construction, as they are same across siblings. This specification also absorbs the unobserved heterogeneity at the household as well as cluster level. However, the way in which NFHS data are collected limits the appropriateness of the mother FE model for our analysis. NFHS only collects anthropometry for children born within 5 y preceding the survey. Since mother FE is restricted to the subsample of mothers who have more than one child, the subsample will primarily include children born with a shorter birth spacing. We see the sample size is significantly lower in column 6 of Table 1. We find that the coefficients for interaction with PBS < 3 y are significantly larger (in absolute terms) than those seen in column 4 of Table 1, across all birth-order categories. Thus, HAZ outcomes are worse for secondborns and worst for third(+)-born for PBS < 3 y. The coefficients on the interaction with PBS ≥ 3 y are smaller in comparison to those with PBS < 3 y, implying a similar pattern of reducing deficits with longer spacing. However, they are not insignificant, suggesting the firstborn height advantage persists. Because of the limited sample in the category of PBS ≥ 3 y, we cannot establish the effect of longer spacing length, and the mother FE can be criticized on the basis that this subsample of women might not be representative of all women. Nevertheless, the analysis helps in strengthening the results with respect to the short length of spacing.
For many predictors of child health and nutrition, the NFHS does not collect information for all children under 5 y. Two useful predictors include prenatal and postnatal healthcare given to the child and child-feeding practices adopted by the mother. The prenatal and postnatal healthcare utilization information is available for the youngest child below 5 y in the family, and information on child-feeding practices is available for the youngest children between 6 and 24 mo in the family. SI Appendix, Table S3 reports the results for these subsamples using the covariates from our main specification, along with additional controls available for them. Restricting our analysis to subsample with the youngest child under 5 y (see column 1 of SI Appendix, Table S3), we see a slight decrease in the magnitude of coefficients associated with interaction with PBS < 3 y across birth orders, but they remain significant and the pattern is similar to our main specification. For the second subsample with children between age 6 and 24 mo (child-feeding practices sample), there is a significant decline in the magnitude as well as loss of significance in the coefficients associated with interaction with PBS < 3 y (see column 2 of SI Appendix, Table S3). For interaction with PBS ≥ 3 y, we see a height premium accorded to secondborns, over firstborn, as the gradient is significantly positive; the interaction for third(+)-born is insignificant, as before. We suspect that differences in the results could be driven by demographic differences rather than those on information related to feeding practices.‡
To understand these results better, we split our entire sample of children into two age categories, one below 2 y and the other between 2 and 5 y, and estimated our main specification by subgroups of age. The results are reported in columns 3 and 4 of SI Appendix, Table S3. For the between 2- and 5-y sample, we observed the same pattern with similar magnitude and significance as in the main analysis (column 3 of SI Appendix, Table S3). For the 0- to 2-y sample, however, we noticed that the coefficient for interaction with PBS < 3 y are lower in magnitude as well as significance (column 4 of SI Appendix, Table S3). This leads us to believe that significant and important changes happen in the child’s body in the first 2 y of life and some factors may take more time to manifest their true impact on child health.
Several studies have shown that young girls have better HAZ outcomes compared to boys in India at a given point in time. In SI Appendix, Table S4, we carry out a disaggregated analysis by gender of the children to determine if there are any differences in spacing order estimates. Column 1 of SI Appendix, Table S4, shows that, indeed, girls have better outcomes than boys in terms of HAZ. Firstborn girls are 0.12 SD taller than firstborn boys. The advantage of girls in HAZ is seen across higher birth-order categories, although the difference is insignificant at birth order 3 (or higher). Furthermore, to show whether the short birth spacing is significant for the short stature of subsequent children varied by the gender of the elder siblings, we split the spacing order categories by the gender of the first child (column 2 of SI Appendix, Table S4) and gender of the second child (column 3 of SI Appendix, Table S4). We found no difference in the spacing-order estimates by the gender of the firstborn (column 2 of SI Appendix, Table S4) and secondborn (column 3 of SI Appendix, Table S4) siblings, except for third(+)-born children with PBS ≥ 3 y, which is weakly significant at the 10% level in column 2 of SI Appendix, Table S4. In this case, third(+)-born children with PBS ≥ 3 y continue to experience a height disadvantage if the firstborn sibling is a boy. However, the difference is insignificant if the firstborn is a girl. The results do not vary when we account for the gender of the second child.
Wide regional heterogeneity among Indian states in child height outcomes, as well in key development indicators, is well known. The same is also true for fertility patterns. In SI Appendix, Table S5, we estimate the spacing-order linkage for children living in seven high-fertility states of Uttar Pradesh, Bihar, Rajasthan, Madhya Pradesh, Chhattisgarh, Jharkhand, and Assam. Interestingly, the magnitude of coefficients on the interaction with PBS < 3 y in high-fertility states (column 1 of SI Appendix, Table S5) is not meaningfully different from the main results observed in our main analysis, but the coefficients for interaction with PBS ≥ 3 y is significantly positive for secondborns. This shows the potential of a height premium enjoyed by secondborns once the fertility levels are reduced in high-fertility states, which also happens to be the states with the worst HAZ outcomes.
Finally, to find out whether short birth intervals have more detrimental effects on illiterate vs. educated mothers and in younger vs. older mothers, we carried out sensitivity analysis based on mothers’ characteristics. In columns 2 to 4 of SI Appendix, Table S5, we compared our spacing-order estimates across different mother’s education categories by dividing the sample into three groups based on educational qualifications of the mother—illiterate, below secondary, and secondary and above—and reran the analysis. The only difference is seen in the significance of coefficients for children born to mothers with more than secondary education. The coefficients are insignificant across all birth-order (and spacing) categories. In columns 5 to 7 of SI Appendix, Table S5, we divided the sample into three groups based on mother’s age at the time of birth: Age 24 y or below, between 25 and 29, and age 30 or above. The coefficients for the age groups below 24 y and between 25 and 29 are in line with our main result: That is, that later-born children with PBS < 3 y are at a disadvantage, compared to firstborns, but not if the PBS ≥ 3 y. In fact, the coefficients associated with PBS ≥ 3 y are significantly positive for children of higher birth order who wore born to mothers 24 y old or younger. Given that Indian women begin childbearing early, this result emphasizes the benefits and importance of increasing spacing length for younger mothers and advancing the age at birth. The coefficients for the sample of children born to women age 30 and older are insignificant across all spacing order categories, but this is mainly because of the very low sample size observed for this set of children. The estimations here demonstrate the consistently strong spacing order linkages with child height outcomes across several specifications of covariates and for different subsamples. In the next section, we proceed with the implications of our results for policymaking.
Discussion
Maternal and child health and nutritional outcomes in developing countries are global health priorities. The United Nations’ Sustainable Development Goal 3, “Ensure healthy lives and promote well-being for all at all ages,” sets targets to improve maternal, child health, and nutritional outcomes in the lagging regions by 2030. In this paper, we present some facts on India’s fertility behavior and outline a coherent story of poor child height outcomes consistent with the facts. Specifically, we demonstrate that the firstborn height advantage is essentially an outcome of short interbirth spacing. Later-born children tend to be as tall as firstborns if spacing of at least 3 y is maintained between children. From a policy perspective, birth-order effects are particularly interesting, as they are not systematically related to genetic endowments, and thus, have biological or behavioral underpinnings. A better understanding of how the length of birth spacing drives the height outcomes of higher birth-order children could inform policies aimed at improving the health and nutrition status of the population.
This paper contributes to the research on child health and nutrition in several ways. First, a range of predictors of poor height outcomes in India have been documented in the literature. For example, Coffey and Spears (35) pointed out the high rate of open defecation and disease environment as important predictor of poor child height in India; Jayachandran and Pandi (19) argued for intrahousehold gender dynamics as an explanation of poor height; Headey et al. (36) highlighted low dietary diversity and poor food systems in India; and Das Gupta et al. (37) pointed to the inefficacy of India’s nutrition policy, showing shortcomings of the nutritional programs. A recent study by Nguyen et al. (38), using the same round of NFHS as our study, showed that teen pregnancy is strongly related to child stunting in India. Our paper focuses on the extent to which the spacing between births influences height outcomes of young children, an area on which the literature is more limited. Several studies in the Indian context have used logistic regressions to link binary indicators of child undernutrition with the length of birth spacing (see, for example, refs. 39–41). We contribute to this literature by demonstrating the importance of including birth spacing in the ongoing debate on birth-order and child-stunting outcomes in India, and identify patterns within the order effects. The spacing effects continue to hold when we control for sibling size. Second, unlike many other risk factors for child (and maternal) undernutrition, such as socioeconomic status, women’s empowerment, or sanitation, the length of time between births is easily modifiable—through improved access to family planning and contraceptive counseling and services—making it an attractive target for public health intervention. The results from the analysis help to develop an evidence base for effective interventions to put optimal birth-spacing recommendations into practice for India.
In India, the average number of children born to a woman during her lifetime has been declining, though it still stands slightly over the replacement level of 2.1. However, it is alarming to see that there has not been any significant change in the pattern of birth spacing observed over the years, despite birth spacing being a key component of India’s Family Planning program. In 2015, ∼60% of women surveyed waited less than the recommended level of at least 3 y before delivering their next child, a drop of only 2% since 1992 to 1993 (NFHS-1). Adolescent marriage and pregnancies continue to be a major challenge in India: 27% of adolescent girls reported to be married before the legal age of 18 y, and 31% of these married girls had delivered a child by age 18 y. These figures point to the disproportionately large share of births occurring below the recommended levels of birth spacing, as well as age at which the woman experience their first pregnancy. At the same time, however, these figures highlight the potential for substantial increase in spacing length and postponing of births to later ages, and hence, reducing adverse maternal and child health and nutritional outcomes.
While postponing marriage and childbirth is acknowledged as an important measure for improving maternal outcomes in India, the importance given to the benefits of healthy spacing in current maternal and child nutritional policies and interventions is not sufficient. Birth spacing is one of the components of family-planning policies to limit fertility and lower population growth; however, Indian women continue to bear children early in their reproductive period. By the age of 27 y, the average Indian woman has already given birth to 2.5 children, and 60% of these women reported no desire to have more children. This reflects ineffective delivery of the birth-spacing component in family planning. Recently, the Ministry of Health and Family Welfare launched Mission Parivar Vikas in 145 high-fertility districts in seven high-fertility states§ to accelerate access to high-quality family-planning choices, based on information, reliable services, and supplies (42). Our results for these high-fertility states, which coincides with states with relatively poor child HAZ, shows that second-born children with PBS ≥ 3 y, experience a height premium over that of firstborns. Such support for family-planning programs would contribute not only to reductions in maternal and child mortality, but to improved child health and overall development. Hence, there is a need to integrate family-planning approaches with nutritional interventions.
Our results also provide necessary support for children to be breastfed for extended time periods. Research from many developing countries have found adverse effects of suboptimal breastfeeding and complementary feeding practices on child undernutrition. The WHO and the United Nations Children’s Fund (UNICEF) recommend exclusive breastfeeding for the first 6 mo of a baby’s life and continued breastfeeding for 2 or more years, along with complementary feeding from 6 mo. If longer birth spacing is maintained, it will allow for greater care time for older children, including the possibility of longer breastfeeding, which in turn has a profound impact on a child’s survival, health, nutrition, and development, as well as health of mothers because it helps reduce the risk of postpartum hemorrhage.
The accumulating evidence on causes of stunting has established that it is a multidimensional problem. It is a problem of the quality of diet, as well as knowledge of timely introduction of complementary foods; of mother’s health at the time of pregnancy and lactation; of adequate breastfeeding; of frequent illness, poor care practices, and lack of access to health and other social services; and of sanitation and the disease environment. Stunting is preventable but requires a strong behavioral change, which is possible by spreading awareness and knowledge. Hence, education plays a very important role. Education in India is still distributed differently by gender, with very high rates of illiteracy among women. It is necessary to educate women about the benefits of healthy fertility patterns. Since childbearing in India starts early, and the interval between marriage and first birth is small, it is important to introduce interventions that target girls attending school. Furthermore, interventions cannot ignore the important role that men play in deciding the number of children to have and the time at which to have them. Women in India have low social status, which limits their ability to be vocal about their reproductive preferences or to do what they want. The benefits from educating young girls and females about the importance of healthy fertility behavior may not be a sufficient intervention if their husbands do not allow such fertility changes to be made. Hence, behavioral change interventions should target all those who have direct or indirect influence on pregnancy decisions. Public interventions should focus on spreading information on the risks associated with frequent pregnancies that may affect the mother, fetus, and child using mass media technology.
Data Description
The data used in this paper comes from the fourth round of the National Family Health Survey (NFHS 2015/16). These data provide a nationally representative sample on the health and demography of the Indian population. The survey structure corresponds to the typical structure of demographic and health surveys conducted in several other countries; hence, the analysis can easily be replicated by other countries. The survey collects separate rural and urban samples for each district in a state, using a two-stage stratified random sampling design and relevant sampling weights to select households. At the first stage, the PSU, which are a village in rural areas and a census enumeration block in urban areas, were selected using probability proportional to size, and 22 households were then randomly sampled from each PSU. All women in the age group of 15 to 49 y in the selected households were interviewed, and height and weight biomarkers were collected for each one of them, as well as for their children under 5 y. Our analytical sample is restricted to all live births (single or multiple births) occurring within 5 y preceding the survey and for whom valid anthropometric data are available.
For height outcomes, we focus on age-adjusted HAZ z-scores, which express a child’s height outcomes relative to a reference population of well-nourished children of the same age. These z-scores are measured against WHO growth standards, as described in de Onis et al. (43). HAZ is a cumulative measure of child health; a HAZ less than 2 SDs below the reference group is in indicator of stunting, which indicates that a child has been unable to reach their full potential both physically and mentally due to chronic malnutrition. The HAZ were converted to missing if they were less than −6 or greater than 6 SDs away from the reference median (this conversion to missing occurred for ∼8% of cases).
We assessed how length of preceding birth spacing can alter the birth-order effects on child HAZ. When assigning birth order, we included all children born to a woman, living or dead. Since children from multiple outcome pregnancies were assigned the same rank, we dropped all but one living child from such pregnancies. This was necessary because for many healthcare and dietary intake variables, NFHS collected information only for one and the youngest child born to the mother. Hence, each child in the sample has a unique birth order. However, as children born from a multiple-outcome pregnancy have a considerably higher risk of mortality and poor health, compared to single births, we controlled for multiple births in our analysis. The control may also act as a proxy for child health at the time of birth (44).
The birth interval has been defined in multiple ways in the literature: Interpregnancy interval measures the interval between the outcome of two consecutive pregnancies, irrespective of the outcome. The birth-to-birth interval measures the interval between two live births and absorbs any terminated pregnancy in between. The conception-to-birth interval differs from the preceding definition in treating the length of gestation, which is counted as 9 mo when data for pregnancy duration do not exist. We used the birth-to-birth interval definition since reproductive history is collected using woman’s recall and it is difficult to get at the exact timing of conception of pregnancies. However, we took due care of its caveats. This classification also corresponds to those commonly used in the mortality literature and those considered in policy debate, and hence, facilitate comparisons.
As child undernutrition is a multifactorial phenomenon including factors like lack of adequate, nutritious food, as well as poor care practices and lack of access to health and other social services, we controlled for basic, underlying, and immediate causes, including socioeconomic and environmental conditions of undernutrition, as first outlined in UNICEF’s conceptual framework of child undernutrition almost three decades ago (45). The framework has evolved to incorporate new knowledge and evidence on the causes, consequences, and impacts of undernutrition and we account for them to rule out the possibility of spurious association. SI Appendix, Table S1 provides summary statistics on the key variables used in the regression. The final sample consists of 223,662 children, of which 170,559 children are from rural India and 53,103 from urban India, after excluding 19,506 (7.98%) observations because of invalid height data, and a further 13,604 (5.64%) observations because of missing values for the control variables.
Supplementary Material
Acknowledgments
This research has been carried out at the Tata–Cornell Institute for Agriculture and Nutrition, Cornell University.
Footnotes
The authors declare no competing interest.
*The deficits are obtained by subtracting the mean HAZ of firstborns from that of later-born children.
†The meaning of preceding birth spacing depends on the birth-order variable by construction (spacing is valid or applicable only for later-born children). Hence, having birth spacing as an interaction with birth order seems more appropriate. Conceptually, we see birth order and spacing representing a classic case of nested designs, where spacing is a nested factor and birth order is a nesting variable. In such models, having both factors acting independently as well as interactively does not make sense.
‡SI Appendix, Fig. S2 plots average HAZ by child’s age in months by birth-spacing categories (for other than firstborns). We find that the HAZ continuously decreases up to the age of 20 mo for all PBS and stabilizes after the age of 20 mo.
§These include Uttar Pradesh, Bihar, Rajasthan, Madhya Pradesh, Chhattisgarh, Jharkhand, and Assam.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2017834118/-/DCSupplemental.
Data Availability
All data used in this study are publicly available from “The Demographic Health Survey Program's” data distribution system (https://dhsprogram.com/data/available-datasets.cfm). Replication files are available at Harvard Dataverse, V1 (https://doi.org/10.7910/DVN/I4QY7G).
References
- 1.Lopez A. D., Mathers C. D., Ezzati M., Jamison D. T., Murray C. J., Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 367, 1747–1757 (2006). [DOI] [PubMed] [Google Scholar]
- 2.Victora C. G., de Onis M., Hallal P. C., Blössner M., Shrimpton R., Worldwide timing of growth faltering: Revisiting implications for interventions. Pediatrics 125, e473–e480 (2010). [DOI] [PubMed] [Google Scholar]
- 3.Bhutta Z. A.et al.; Maternal and Child Undernutrition Study Group , What works? Interventions for maternal and child undernutrition and survival. Lancet 371, 417–440 (2008). [DOI] [PubMed] [Google Scholar]
- 4.Gandhi M., et al., Height gain during early childhood is an important predictor of schooling and mathematics ability outcomes. Acta Paediatr. 100, 1113–1118 (2011). [DOI] [PubMed] [Google Scholar]
- 5.Walker S. P., et al., Inequality in early childhood: Risk and protective factors for early child development. Lancet 378, 1325–1338 (2011). [DOI] [PubMed] [Google Scholar]
- 6.Victora C. G.et al.; Maternal and Child Undernutrition Study Group , Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 371, 340–357 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grantham-McGregor S.et al.; International Child Development Steering Group , Developmental potential in the first 5 years for children in developing countries. Lancet 369, 60–70 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alderman H., Hoddinott J., Kinsey B., Long term consequences of early childhood malnutrition. Oxf. Econ. Pap. 58, 450–474 (2006). [Google Scholar]
- 9.Glewwe P., Jacoby H. G., King E. M., Early childhood nutrition and academic achievement: A longitudinal analysis. J. Public Econ. 81, 345–368 (2001). [Google Scholar]
- 10.Martorell R., Khan L. K., Schroeder D. G., Reversibility of stunting: Epidemiological findings in children from developing countries. Eur. J. Clin. Nutr. 48 (suppl. 1), S45–S57 (1994). [PubMed] [Google Scholar]
- 11.Behrman J. R., et al., Nutritional supplementation in girls influences the growth of their children: Prospective study in Guatemala. Am. J. Clin. Nutr. 90, 1372–1379 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oniang’o R., Mukudi E., “Nutrition and gender” in Nutrition: A Foundation for Development, United Nations, Ed. (ACC/SCN, Geneva: ), pp. 1–4 (2002). [Google Scholar]
- 13.Black R. E.et al.; Maternal and Child Nutrition Study Group , Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382, 427–451 (2013). [DOI] [PubMed] [Google Scholar]
- 14.United Nations Children’s Fund , The State of the World’s Children 2015: Reimagine the Future: Innovation for Every Child (UNICEF, New York, 2014). [Google Scholar]
- 15.United Nations Children’s Fund , State of the World’s Children 2019: Children, Food and Nutrition (UNICEF, New York, 2019). [Google Scholar]
- 16.Plomin R., Daniels D., Why are children in the same family so different from one another? Int. J. Epidemiol. 40, 563–582 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elliott B. A., Birth order and health: Major issues. Soc. Sci. Med. 35, 443–452 (1992). [DOI] [PubMed] [Google Scholar]
- 18.Lehmann J. Y. K., Nuevo-Chiquero A., Vidal-Fernandez M., The early origins of birth order differences in children’s outcomes and parental behavior. J. Hum. Resour. 53, 123–156 (2018). [Google Scholar]
- 19.Jayachandran S., Pandi R., Why are Indian children so short? The role of birth order and son preference. Am. Econ. Rev. 107, 2600–2629 (2017). [PubMed] [Google Scholar]
- 20.Black S. E., Devereux P. J., Salvanes K. G., Healthy(?), wealthy, and wise: Birth order and adult health. Econ. Hum. Biol. 23, 27–45 (2016). [DOI] [PubMed] [Google Scholar]
- 21.Buckles K., Kolka S., Prenatal investments, breastfeeding, and birth order. Soc. Sci. Med. 118, 66–70 (2014). [DOI] [PubMed] [Google Scholar]
- 22.Monfardini C., See S. G., Birth order and child outcomes: Does maternal quality time matter? Discussion paper no. 6825 (IZA Institute of Labor Economics, 2012). [Google Scholar]
- 23.Price J., Parent-child quality time: Does birth order matter? J. Hum. Resour. 43, 240–265 (2008). [Google Scholar]
- 24.Da Vanzo J., Starbird E., Leibowitz A., Do women’s breastfeeding experiences with their first-borns affect whether they breastfeed their subsequent children? Soc. Biol. 37, 223–232 (1990). [DOI] [PubMed] [Google Scholar]
- 25.Gribble J. N., Murray N. J., Menotti E. P., Reconsidering childhood undernutrition: Can birth spacing make a difference? An analysis of the 2002-2003 El Salvador National Family Health Survey. Matern. Child Nutr. 5, 49–63 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conde-Agudelo A., Rosas-Bermúdez A., Kafury-Goeta A. C., Rosas-Bermudez A., Kafury-Goeta A. C., Effects of birth spacing on maternal, perinatal, infant, and child health: A systematic review of causal mechanisms. Am. J. Obstet. Gynecol. 196, 297–308 (2007). [DOI] [PubMed] [Google Scholar]
- 27.Conde-Agudelo A., Rosas-Bermúdez A., Kafury-Goeta A. C., Birth spacing and risk of adverse perinatal outcomes: A meta-analysis. JAMA 295, 1809–1823 (2006). [DOI] [PubMed] [Google Scholar]
- 28.Rutstein S. O., Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: Evidence from the demographic and health surveys. Int. J. Gynaecol. Obstet. 89 (suppl. 1), S7–S24 (2005). [DOI] [PubMed] [Google Scholar]
- 29.Winikoff B., The effects of birth spacing on child and maternal health. Stud. Fam. Plann. 14, 231–245 (1983). [PubMed] [Google Scholar]
- 30.Dewey K. G., Cohen R. J., Does birth spacing affect maternal or child nutritional status? A systematic literature review. Matern. Child Nutr. 3, 151–173 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization , Report of a WHO Technical Consultation on birth spacing (WHO, Geneva, Switzerland, 2007). [Google Scholar]
- 32.Menon P., Headey D., Avula R., Nguyen P. H., Understanding the geographical burden of stunting in India: A regression-decomposition analysis of district-level data from 2015-16. Matern. Child Nutr. 14, e12620 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DaVanzo J., Hale L., Razzaque A., Rahman M., The effects of pregnancy spacing on infant and child mortality in Matlab, Bangladesh: How they vary by the type of pregnancy outcome that began the interval. Popul. Stud. (Camb.) 62, 131–154 (2008). [DOI] [PubMed] [Google Scholar]
- 34.Behrman J. R., Spears D., Coffey D., Birth order, fertility, and child height in India and Africa. Discussion Paper no. 12289 (IZA Institute of Labor Economics, 2019). [Google Scholar]
- 35.Coffey D., Spears D., Child height in India: Facts and interpretations from the NFHS-4, 2015–16. Econ. Polit. Wkly. 53, 210–215 (2018). [PMC free article] [PubMed] [Google Scholar]
- 36.Headey D., Chiu A., Kadiyala S., Agriculture’s role in the Indian enigma: Help or hindrance to the crisis of undernutrition? Food Secur. 4, 87–102 (2012). [Google Scholar]
- 37.Das Gupta M., Lokshin M., Gragnolati M., Ivaschenko O., Improving child nutrition outcomes in India: Can the integrated Child Development Services Program be more effective? Policy Research Working Paper no. 3647 (World Bank, Washington, DC, 2005). [Google Scholar]
- 38.Nguyen P. H., Scott S., Neupane S., Tran L. M., Menon P., Social, biological, and programmatic factors linking adolescent pregnancy and early childhood undernutrition: A path analysis of India’s 2016 National Family and Health Survey. Lancet Child Adolesc. Health 3, 463–473 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chungkham H. S., Sahoo H., Marbaniang S. P., Birth interval and childhood undernutrition: Evidence from a large scale survey in India. Clin. Epidemiol. Glob. Health 8, 1189–1194 (2020). [Google Scholar]
- 40.Rana M. J., et al., Planning of births and maternal, child health, and nutritional outcomes: Recent evidence from India. Public Health 169, 14–25 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rana M. J., Goli S., Does planning of births affect childhood undernutrition? Evidence from demographic and health surveys of selected South Asian countries. Nutrition 47, 90–96 (2018). [DOI] [PubMed] [Google Scholar]
- 42.Pachauri S., Priority strategies for India’s family planning programme. Indian J. Med. Res. 140 (suppl.), S137–S146 (2014). [PMC free article] [PubMed] [Google Scholar]
- 43.de Onis M., Garza C., Onyango A. W., Borghi E., Comparison of the WHO child growth standards and the CDC 2000 growth charts. J. Nutr. 137, 144–148 (2007). [DOI] [PubMed] [Google Scholar]
- 44.Palloni A., Millman S., Effects of inter-birth intervals and breastfeeding on infant and early childhood mortality. Popul. Stud. 40, 215–236 (1986). [Google Scholar]
- 45.United Nations Children’s Fund Policy Review , Strategy for Improved Nutrition of Children and Women in Developing Countries (UNICEF, New York, 1990). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used in this study are publicly available from “The Demographic Health Survey Program's” data distribution system (https://dhsprogram.com/data/available-datasets.cfm). Replication files are available at Harvard Dataverse, V1 (https://doi.org/10.7910/DVN/I4QY7G).