Abstract
Objective
We assessed the clinical survival of a high-viscosity glass ionomer (HVGI) at the 2-year follow-up to restore molar incisors severely affected by hypomineralization after selective carious tissue removal (SCR). The null hypothesis tested was that there are no differences in the overall survival times in the categories of the variables of interest.
Methods
A total of 134 fully erupted first molar incisors with hypomineralization, cavitated and with moderate-to-deep carious lesions without hypersensitivity or pain (MIH treatment need index 2a–c), were included in the study. HVGI (Equia Forte®; GC, Tokyo, Japan) restorations were applied after SCR to soft carious dentin. The follow-up lasted 2 years. The end point was defined as the absence of endodontic and restorative complications. Two-year, and 18-, 12-, and 6-month survival probabilities and standard errors were calculated using the Kaplan-Meier method. Survival probabilities according to patient gender, jaw, and lesion severity groups were compared using the log-rank test. Restorations were evaluated using the modified US Public Health Service criteria.
Results
HVGI restorations showed cumulative survival probabilities of 95.5% at 6 months, 94% at 12 months, 87.5% at 18 months, and 87.5% at 24 months. Survival probabilities according to patient gender, jaw, and lesion severity groups were not statistically significantly different (p > 0.05). Therefore, the null hypothesis was accepted.
Conclusion
Following SCR, HVGI restoration provided moderate survival probabilities, suggesting that the SCR technique is effective.
Keywords: Molar incisor hypomineralization, Survival probabilities, High-viscosity glass ionomer, Selective carious tissue removal
Highlights of the Study
Molar incisor hypomineralization is a growing public dental health problem, with no scientific evidence on the appropriate restorative material.
Restoration using a high-viscosity glass ionomer after selective carious tissue removal (SCR) has been observed to be an effective approach to maintain tooth structure integrity.
This study presents promising survival results from restorations after SCR.
Introduction
Molar incisor hypomineralization (MIH) is characterized by demarcated, qualitative, developmental defects of systemic origin of the enamel of one or more permanent first molars [1] with or without involvement of the incisors. Hypomineralized enamel is more porous than the normal enamel [2], which can result in posteruptive breakdown soon after tooth eruption or later under the effect of masticatory forces [1]. Due to unfavorable enamel consistency, posteruptive breakdown often leads to the development of carious lesions, as biofilm is sheltered in the formed cavity, and oral hygiene is usually also impaired due to hypersensitivity of the affected teeth (mainly molars).
The restorative management of such atypical cavitated carious MIH lesions depends on the extension and depth of the defect as well as the child's cooperation and age [3, 4]. Especially for deep lesions, recommendations for non-MIH teeth favor selective (incomplete, partial) over nonselective (complete) carious tissue removal in vital teeth [5]. Selective carious tissue removal (SCR) is based on the concept that that caries activity is stopped under a restoration with a good seal causing remaining bacteria to be deprived of dietary carbohydrates, which leads to lesion arrest. During SCR, excavation is performed until hard dentin is in the periphery, while in proximity to the pulp, soft or leathery dentin is left. Such selective removal has been further shown to significantly reduce the risk of pulp exposure, which is especially relevant in children, where further endodontic procedures, especially root canal treatment, are to be avoided [5, 6, 7, 8].
A number of recent studies have assessed the longevity of restorations performed in young permanent teeth following minimally invasive techniques such as SCR and atraumatic restorative treatment (ART) [9, 10, 11]. For MIH, the SCR concept has been applied in limited cases. Moreover, different restorative materials have been employed to restore MIH cavities, such as composites, glass ionomer (GI), amalgam, or indirect restoration [1]. A systematic review found GI to be associated with relatively high MIH failure rates [12], and, so far, only 2 studies applying GI for MIH are available [13, 14]. One of these used the GI in a hand-mixed application with limited standardization and lower survival rates, while the other applied it as part of the ART technique [13, 14]. Success rates were not similar, with 78% at 12 months in one study and 98% at 24 months in the other. Whether a high-viscosity GI (HVGI) is suitable to restore MIH cavities is therefore unclear, especially if SCR is performed prior to the restoration.
We thus aimed to assess the survival and clinical performance of an HVGI after SCR in MIH using a single-arm prospective study. The null hypothesis tested was that there are no differences in the overall survival times in the categories of the variables of interest.
Materials and Methods
The study was approved by the Research Ethics Committee of the Faculty of Dentistry, University of Marmara (No. 569123). The reporting of this study follows the STROBE checklist [15].
Study Design
A prospective single-arm interventional study was conducted using patients with at least 1 MIH restoration. Molars were treated using HVGI (Equia Forte®; GC, Tokyo, Japan), and 2-year, and 18-, 12- and 6-month survival probabilities were calculated using the Kaplan-Meier method. The absence of endodontic and restorative complications was considered a success.
Setting and Participants
The children who were diagnosed with MIH on the basis of clinical examination at the Department of Pediatric Dentistry, School of Dentistry, Marmara University, were enrolled in the study. Clinical examinations were performed in a dental chair using an oral mirror (No. 4 plain mirror) under a dental light source. The teeth were examined under wet conditions, and, if needed, clean cotton rolls were used to clean the tooth surface to better visualize a tooth surface. The case definition for MIH followed the modified European Academy of Pediatric Dentistry criteria and the MIH treatment need index (TNI) [16, 17]. The following inclusion criteria were applied: (1) children aged 8–11 years with a fully erupted molar(in occlusion = B code) [16] with cavitated MIH defects, additionally affected by caries, indicated by signs of plaque stagnation or softness without hypersensitivity, pain or signs of pulp necrosis (MIH TNI 2a–c) [17], and a symptomless periodontal status; (2) treatment under local or no anesthesia was expected; and (3) a signed the consent form of the children or parents of children.
Treatment
A pediatric dentist with 10 years of clinical experience provided the restorations. The access cavity preparation and removal of MIH-affected enamel was performed using high-speed, water-cooled diamond instruments. Carious tissue was removed peripherally including the enamel-dentin junction using low-speed rosehead burs (HM 1, size 014, Meisinger) until hard, dry dentin remained. The hardness of the dentin was checked using a blunt-tipped dental probe. Pulpo-axial carious dentin was removed using a sharp sterile spoon double-ended excavator (Hu-Friedy 131/132, 151/152, USA) until leathery, slightly moist, and soft dentin remains (i.e., dentin which cannot be removed using an excavator without force being applied; subjective removal). The operating pediatric dentist was instructed prior to the study regarding these criteria and methods using extracted teeth. No local anesthesia was used or needed during treatments. The Houpt behavior rating scale was used to assess and record the behavior of the patients during treatment [18]. An HVGI (Equia Forte GC, Tokyo, Japan) was placed according to the manufacturer's instructions. Isolation was maintained using cotton rolls and a saliva ejector. Cavities were first cleansed using a water spray and briefly dried. The HVGI was mixed in a capsule and injected into the cavity. The material was lightly pressed down with a finger coated in petroleum jelly, and excess material removed with a dental carver (Medesy No. 604/2). After a 2.5-min setting time, the occlusion was checked using fine carbon paper and then adjusted. Equia Coat (GC) was applied and light cured for 20 s (D-Light Duo, GC, 1,400 mW/cm2). After finishing the restoration procedure, the children were instructed not to eat for at least 1 h.
Evaluation
Restorations were evaluated using modified United States Public Health Service (USPHS) criteria consisting of anatomical form, marginal adaptation, surface texture, marginal discoloration, retention, secondary carious lesions, and postoperative sensitivity [19]. Another pediatric dentist with over 5 years of clinical experience evaluated restorations under the supervision of the study director in a clinical setting. Potential restoration failures were presented to this pediatric dentist prior to the study. At this point, this pediatric dentist who did not participate in restoration application sessions was considered accredited to evaluate the restorative procedures. When the restoration rated as Charlie in any of the modified USPHS criteria was included into the failure, restoration complications, such as marginal adaptation or retention, were retreated. Endodontic complications including pulpal complications, such as continuous pain and hypersensitivity, were planned for root canal treatment or extraction.
Statistical Analysis
The follow-up study lasted 2 years. The end point evaluated was defined as the absence of endodontic and restorative complications. Two-year, and 18-, 12-, and 6-month survival probabilities and standard errors were calculated using the Kaplan-Meier method. Survival probabilities according to patient gender, jaw, and lesion severity groups were compared using the log-rank test. Categorical variables of USPHS criteria were described as frequencies and percentages. Statistical significance was defined as p < 0.05. SPSS 15.0 was used for statistical analysis.
Results
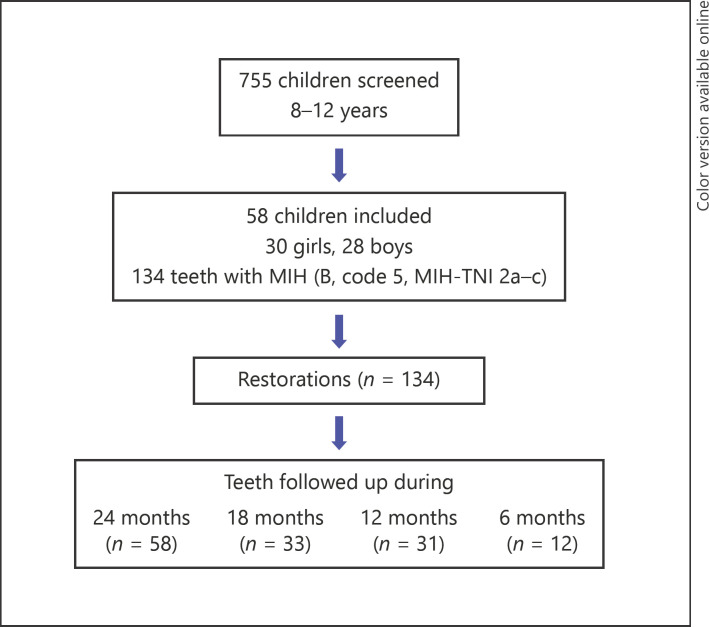
Overall, 58 children (30 girls and 28 boys) with 134 restorations were treated (Fig. 1). The mean age (± SD) of the children was 8.94 (±1.41) years. The mean dft and DMFT was 3.96 (± 3.46) and 3.63 (± 1.44), respectively. Of the 134 teeth, 69 (51.5%) were upper molars, and 65 (49.5%) were lower molars; all showed MIH (B code, MIH TNI 2a–c). During SCR, the most frequent Houpt score (n = 27; 46.5%) was 6 (“excellent, no crying or movement”).
Fig. 1.
Flowchart of the study phase.
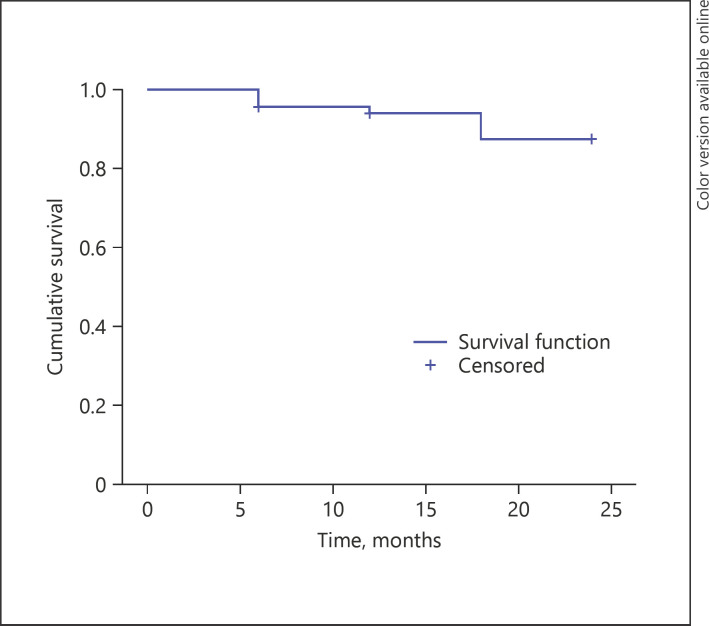
Table 1 presents the survival proportions at event times. Therefore, the probability of failure at the 24-month follow-up was calculated as 0.125. The estimated mean survival time was 22.62 ± 0.375 months (Fig. 2). Survival probability at 24 months was 87.5%. Table 2 shows survival probabilities according to patient gender, jaw, and lesion severity groups, which were compared using the log-rank test. No statistically significant differences existed between survival probabilities.
Table 1.
Kaplan-Meier survival analysis of selectively removed HVGI restorations followed up for 6, 12, 18, and 24 months
| Follow-up | n | Cumulative failure | Cumulative survival probability |
|
|---|---|---|---|---|
| estimate | SD | |||
| 6 months | 12 | 6 | 0.955 | 0.018 |
| 12 months | 31 | 8 | 0.94 | 0.021 |
| 18 months | 33 | 13 | 0.875 | 0.034 |
| 24 months | 58 | 13 | 0.875 | 0.034 |
Fig. 2.
Kaplan-Meier survival function.
Table 2.
Comparisons of survival probabilities among gender, jaw, and severity groups
| Variables | Success, n (%) | Failure, n (%) | Total, n | Estimated survival, months |
log-rank | p value | |
|---|---|---|---|---|---|---|---|
| mean | 95% CI | ||||||
| Gender | |||||||
| Girl | 57 (81.4) | 13 (18.6) | 70 | 21.634 | 20.409–22.859 | 0.002 | 0.961 |
| Boy | 52.1 (81.3) | 12 (18.8) | 64 | 21.94 | 20.690–23.198 | ||
| Jaw | |||||||
| Upper | 56 (81.2) | 13 (18.8) | 69 | 22.095 | 21.006–23.183 | 0.017 | 0.897 |
| Lower | 53 (81.5) | 12 (18.5) | 65 | 21.450 | 20.072–22.828 | ||
| Severity | |||||||
| 5–2a | 26 (86.7) | 4 (13.3) | 30 | 22.440 | 933–23.947 | 0.6 | 0.439 |
| 5–2b, c | 83 (79.8) | 21 (20.2) | 104 | 21.590 | 20.548–22.632 | ||
Apart from Kaplan-Meier survival analysis and log-rank test, the status of the restorations according to USPHS criteria at 24 months are shown in Table 3. With regard to the clinical status of 134 restorations, most Charlie scores were secondary caries (14%) and postoperative sensitivity (14%).
Table 3.
Status of the SCR-HVGI restorations according to USPHS criteria at the 24-month follow-up
| USPHS criteria | USPHS Scores | Total (n = 134), n (%) |
|---|---|---|
| Anatomical form | Alpha Bravo Charlie |
97 (72) 24 (18) 13 (10) |
| Marginal adaptation | Alpha Bravo Charlie |
100 (75) 19 (14) 15 (11) |
| Retention | Alpha Bravo Charlie |
109 (81) 12 (9) 13 (10) |
| Secondary caries | Alpha Charlie |
115 (86) 19 (14) |
| Surface texture | Alpha Bravo Charlie |
109 (81) 11 (8) 14 (11) |
| Marginal discoloration | Alpha Bravo Charlie |
101 (75) 18 (13) 15 (12) |
| Color match | Alpha Bravo Charlie |
107 (80) 13 (10) 14 (10) |
| Postoperative sensitivity | Alpha Charlie |
114 (86) 19 (14) |
Discussion
SCR is becoming more common in daily practice, as this minimally invasive technique helps treat deep carious lesions and reduces the risk of exposure to the pulp. However, there is currently no evidence for the appropriate restorative material for selective removal to firm dentin [20, 21]. Furthermore, there is a lack of consensus on the ideal restorative material to be applied on MIH-affected teeth [1]. The present clinical study evaluates survival and clinical performance of an HVGI after SCR in MIH over 24 months.
In the current study, HVGI restorations after SCR in permanent molars with MIH were performed during the same visit. The absence of local anesthesia during treatment is considered an advantage, especially as chronic pulpal inflammation complicates local anesthesia. Fagrell et al. [2] reported that in noncarious teeth affected by MIH, bacteria had penetrated into both the enamel and dentin, suggesting that irritants can reach the dentin through the porous enamel and cause subclinical inflammatory reactions in the pulp. This may lead to inadequate tooth anesthesia, which renders treatment more painful [22]. Teeth affected by MIH may cause distress to the child as a result of sensitivity to thermal and mechanical stimuli. Additionally, teeth severely affected by MIH are more susceptible to restoration failure and repeated treatments [23, 24]. This combination may have an effect on the quality of life of these children and increase their risk of developing behavior management problems. The benefits of SCR-HVGI in clinical practice (mainly in public dental clinics) are its simplicity, lower operation time, and better handling of behavioral problems in MIH compared to conventional caries removal [8, 9, 10].
Restorative treatment success usually depends on the severity of the MIH lesions, as well as the child's hygiene habits, cooperation, and age [25]. Regarding the type of material survival, few studies are comparable with ours. Fragelli et al. [13] evaluated the clinical performance of GI cement restorations in molars that were affected by MIH and found lower survival rates (91.7% after 6 months and 78.7% after 12 months). This may be due to the restorative technique and the type of restorative material used. In the present investigation, the restorations were placed using the SCR technique and filled with a new encapsulated hybrid restorative system. Fragelli et al. [13] used an HVGI cement that was hand mixed. Grossi et al. [14] evaluated the survival rate of glass hybrid restorations placed under the ART technique in first permanent molars affected by MIH. They concluded a success rate of 98.3% after 6 and 12 months. Composite resin material has much longer-term stability than other restorative materials in MIH-affected teeth, with a median survival of 5.2 years [1] and a success rate of 74–100% [1, 26, 27] during a 4-year follow-up period. Comparing the success rate obtained in the present study (87.5%) at 24 months, better clinical performance of the hybrid system tested here was observed. Differences in clinical success could be attributed to cavity preparation with different-sized remaining hypomineralized enamel defects. In the present study, the sample was selected based on strict inclusion and exclusion criteria. Thus, the sample was composed of severe cases of MIH with posteruptive enamel breakdown, caries lesions, and opacities associated with atypical multifaced restorations.
The overall survival rate of HVGI restorations of 87.5% after 24 months is considered good for hypomineralized young permanent teeth, given that molars affected by MIH have more retreatments [23]. Comparing the survival rates with previous studies, a recent clinical trial found survival rates of around 68 and 54% for self-etching and total-etching, respectively, at the end of 18 months [25]. The cumulative success of 87.5% observed in this study could be considered even better due to the longer clinical follow-up time. The categories of the variables of interest such as gender, type of jaw, and severity of MIH lesions had no influence on restoration survival (p > 0.05).
In 2007, a new HVGI cement restorative system (Equia; GC Europe, Tokyo, Japan) was introduced, which could be an alternative to composite resins in the posterior region, and was designed for the use in the permanent restoration of class I and II cavities by combining the advantages of HVGI cement and a surface-coating resin [28, 29]. Although used for temporary restoration material over carious dentin, the dentin is more mineralized over time, and it hardens until permanent restoration with less tissue removal is planned. Further, the facility of the technique, which is extremely important in the management of difficult patient behavior, makes it an ideal treatment option [7, 13]. The null hypothesis was accepted in the current study with the 12- and 24-month cumulative survival scores with HVGI as high as 94 and 87.5%, respectively, with no statistically significant difference.
Elhennawy et al. [30] reported that severe MIH has long-term consequences both clinically and economically. Certain treatments such as direct restorations are initially far less costly than others, such as indirect restorations or extraction and orthodontic alignment. However, they might require more follow-up treatments and ensue earlier restoration loss, which increases long-term costs. Therefore, Elhennawy et al. [30] concluded that both a direct composite restoration and extraction and orthodontic treatment might be options to consider in managing severe cases of MIH regarding cost-effectiveness. They noted 2 factors as the most important drivers of cost-effectiveness: the timing of extraction (and the associated need for orthodontic alignment, generating significant costs) and the number of molars per patient to be treated. However, one should consider that orthodontic treatment is time consuming and requires a specific amount of compliance from the patient throughout the treatment time. Extracting all the affected permanent molars is also challenging, especially for anxious children with local anesthesia. Therefore, sedation or general anesthesia should be planned for patient comfort, which, expectedly, increases the costs. Additionally, only 1 study compared the cost-effectiveness of indirect versus preformed metal crowns for defective molars and found indirect restorations significantly more expensive due to laboratory costs [31]. Here again, as an advantage of the encapsulated HVGI system, several restorations may be performed at the same visit.
There are some limitations to the present study. One is the cavity patterns of molars affected by MIH, which should be taken into consideration given how much affected enamel has to be removed for SCR. An additional limitation is the lack of a control group. Further survival analysis with different materials and their likely cost-effectiveness should be determined.
This study appears to be the first clinical trial longitudinally evaluating the survival of restorations in MIH-affected molars using HVGI. The treatment showed satisfactory survival results at the 24-month follow-up, suggesting the effectiveness of this minimally invasive approach for MIH-affected molars. Nevertheless, the long-term effects of treatment should be evaluated in future studies.
Conclusion
New strategies for the management of carious tissue in MIH may target alternative approaches to treatment of the most advanced stages of affected teeth, with particular benefits for children. Restoration using HVGI after SCR was observed to be an effective approach to maintain tooth structure integrity. Based on the current lack of consensus, more randomized clinical trials should evaluate the strategies of caries removal and restorative procedures with HVGI.
Statement of Ethics
All procedures used were in accordance with the guidelines of the Helsinki Declaration on Human Experimentation.
Disclosure Statement
None of the authors declared a conflict of interest.
Funding Sources
No financial support was received for this study.
References
- 1.Lygidakis NA, Wong F, Jälevik B, Vierrou AM, Alaluusua S, Espelid I. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an EAPD policy document. Eur Arch Paediatr Dent. 2010 Apr;11((2)):75–81. doi: 10.1007/BF03262716. [DOI] [PubMed] [Google Scholar]
- 2.Fagrell TG, Dietz W, Jälevik B, Norén JG. Chemical, mechanical and morphological properties of hypomineralized enamel of permanent first molars. Acta Odontol Scand. 2010 Jul;68((4)):215–22. doi: 10.3109/00016351003752395. [DOI] [PubMed] [Google Scholar]
- 3.Fayle SA. Molar incisor hypomineralisation: restorative management. Eur J Paediatr Dent. 2003 Sep;4((3)):121–6. [PubMed] [Google Scholar]
- 4.Mahoney EK. The treatment of localised hypoplastic and hypomineralised defects in first permanent molars. N Z Dent J. 2001 Sep;97((429)):101–5. [PubMed] [Google Scholar]
- 5.Thompson V, Craig RG, Curro FA, Green WS, Ship JA. Treatment of deep carious lesions by complete excavation or partial removal: a critical review. J Am Dent Assoc. 2008 Jun;139((6)):705–12. doi: 10.14219/jada.archive.2008.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Innes NP, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res. 2016 May;28((2)):49–57. doi: 10.1177/0022034516639276. [DOI] [PubMed] [Google Scholar]
- 7.Casagrande L, Seminario AT, Correa MB, Werle SB, Maltz M, Demarco FF, et al. Longevity and associated risk factors in adhesive restorations of young permanent teeth after complete and selective caries removal: a retrospective study. Clin Oral Investig. 2017 Apr;21((3)):847–55. doi: 10.1007/s00784-016-1832-1. [DOI] [PubMed] [Google Scholar]
- 8.Franzon R, Guimarães LF, Magalhães CE, Haas AN, Araujo FB. Outcomes of one-step incomplete and complete excavation in primary teeth: a 24-month randomized controlled trial. Caries Res. 2014;48((5)):376–83. doi: 10.1159/000357628. [DOI] [PubMed] [Google Scholar]
- 9.Maltz M, Garcia R, Jardim JJ, de Paula LM, Yamaguti PM, Moura MS, et al. Randomized trial of partial vs. stepwise caries removal: 3-year follow-up. J Dent Res. 2012 Nov;91((11)):1026–31. doi: 10.1177/0022034512460403. [DOI] [PubMed] [Google Scholar]
- 10.Maltz M, Jardim JJ, Mestrinho HD, Yamaguti PM, Podestá K, Moura MS, et al. Partial removal of carious dentine: a multicenter randomized controlled trial and 18-month follow-up results. Caries Res. 2013;47((2)):103–9. doi: 10.1159/000344013. [DOI] [PubMed] [Google Scholar]
- 11.Farag A, Frencken JE. Acceptance and discomfort from atraumatic restorative treatment in secondary school students in Egypt. Med Princ Pract. 2009;18((1)):26–30. doi: 10.1159/000163042. [DOI] [PubMed] [Google Scholar]
- 12.Elhennawy K, Schwendicke F. Managing molar-incisor hypomineralization: A systematic review. J Dent. 2016 Dec;55((55)):16–24. doi: 10.1016/j.jdent.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Fragelli CM, Souza JF, Jeremias F, Cordeiro RC, Santos-Pinto L. Molar incisor hypomineralization (MIH): conservative treatment management to restore affected teeth. Braz Oral Res. 2015;29((29)):1–7. doi: 10.1590/1807-3107BOR-2015.vol29.0076. [DOI] [PubMed] [Google Scholar]
- 14.Grossi JA, Cabral RN, Ribeiro AP, Leal SC. Glass hybrid restorations as an alternative for restoring hypomineralized molars in the ART model. BMC Oral Health. 2018 Apr;18((1)):65. doi: 10.1186/s12903-018-0528-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007 Oct;370((9596)):1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 16.Ghanim A, Silva MJ, Elfrink ME, Lygidakis NA, Mariño RJ, Weerheijm KL, et al. Molar incisor hypomineralisation (MIH) training manual for clinical field surveys and practice. Eur Arch Paediatr Dent. 2017 Aug;18((4)):225–42. doi: 10.1007/s40368-017-0293-9. [DOI] [PubMed] [Google Scholar]
- 17.Steffen R, Krämer N, Bekes K. The Würzburg MIH concept: the MIH treatment need index (MIH TNI) : A new index to assess and plan treatment in patients with molar incisior hypomineralisation (MIH) Eur Arch Paediatr Dent. 2017 Oct;18((5)):355–61. doi: 10.1007/s40368-017-0301-0. [DOI] [PubMed] [Google Scholar]
- 18.Shindova MP, Belcheva AB. Behaviour evaluatıon scales for pediatric dental patients − review and clinical experience. Folia Med (Plovdiv) 2014 Oct-Dec;56((4)):264–70. doi: 10.1515/folmed-2015-0006. [DOI] [PubMed] [Google Scholar]
- 19.Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig. 2005 Dec;9((4)):215–32. doi: 10.1007/s00784-005-0018-z. [DOI] [PubMed] [Google Scholar]
- 20.Franzon R, Opdam NJ, Guimarães LF, Demarco FF, Casagrande L, Haas AN, et al. Randomized controlled clinical trial of the 24-months survival of composite resin restorations after one-step incomplete and complete excavation on primary teeth. J Dent. 2015 Oct;43((10)):1235–41. doi: 10.1016/j.jdent.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Schwendicke F, Dörfer CE, Paris S. Incomplete caries removal: a systematic review and meta-analysis. J Dent Res. 2013 Apr;92((4)):306–14. doi: 10.1177/0022034513477425. [DOI] [PubMed] [Google Scholar]
- 22.Rodd HD, Boissonade FM, Day PF. Pulpal status of hypomineralized permanent molars. Pediatr Dent. 2007 Nov-Dec;29((6)):514–20. [PubMed] [Google Scholar]
- 23.Jälevik B, Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002 Jan;12((1)):24–32. [PubMed] [Google Scholar]
- 24.Kotsanos N, Kaklamanos EG, Arapostathis K. Treatment management of first permanent molars in children with Molar-Incisor Hypomineralisation. Eur J Paediatr Dent. 2005 Dec;6((4)):179–84. [PubMed] [Google Scholar]
- 25.de Souza JF, Fragelli CB, Jeremias F, Paschoal MA, Santos-Pinto L, de Cássia Loiola Cordeiro R. Eighteen-month clinical performance of composite resin restorations with two different adhesive systems for molars affected by molar incisor hypomineralization. Clin Oral Investig. 2017 Jun;21((5)):1725–33. doi: 10.1007/s00784-016-1968-z. [DOI] [PubMed] [Google Scholar]
- 26.Mejàre I, Bergman E, Grindefjord M. Hypomineralized molars and incisors of unknown origin: treatment outcome at age 18 years. Int J Paediatr Dent. 2005 Jan;15((1)):20–8. doi: 10.1111/j.1365-263X.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 27.Lygidakis NA, Chaliasou A, Siounas G. Evaluation of composite restorations in hypomineralised permanent molars: a four year clinical study. Eur J Paediatr Dent. 2003 Sep;4((3)):143–8. [PubMed] [Google Scholar]
- 28.Gurgan S, Kutuk ZB, Ergin E, Oztas SS, Cakir FY. Four-year randomized clinical trial to evaluate the clinical performance of a glass ionomer restorative system. Oper Dent. 2015 Mar-Apr;40((2)):134–43. doi: 10.2341/13-239-C. [DOI] [PubMed] [Google Scholar]
- 29.Balkaya H, Arslan S, Pala K. A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in Class II cavities: one-year results. J Appl Oral Sci. 2019 Oct;27:e20180678. doi: 10.1590/1678-7757-2018-0678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elhennawy K, Jost-Brinkmann PG, Manton DJ, Paris S, Schwendicke F. Managing molars with severe molar-incisor hypomineralization: A cost-effectiveness analysis within German healthcare. J Dent. 2017 Aug;63((63)):65–71. doi: 10.1016/j.jdent.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 31.Zagdwon AM, Fayle SA, Pollard MA. A prospective clinical trial comparing preformed metal crowns and cast restorations for defective first permanent molars. Eur J Paediatr Dent. 2003 Sep;4((3)):138–42. [PubMed] [Google Scholar]