Abstract
Objective
To determine the prevalence, sociodemographic features, and clinical presentation of temporomandibular joint disorder in otorhinolaryngological practice.
Methods
This prospective hospital-based study involved patients diagnosed with temporomandibular joint disorder in our institution’s ear, nose, and throat department. Data for this study were obtained from the patients using pretested interviewer-assisted questionnaires.
Results
The prevalence of temporomandibular joint disorder in this study was 1.3%. The study population included 17 (26.2%) male patients with a male:female ratio of 1.0:2.8. Joint disorder accounted for 75.4% of all disorders, while both mastication muscle and joint disorder accounted for 21.5%. A majority of the patients (47.7%) presented between weeks 1 and 13 of the illness. Unilateral temporomandibular joint disorder accounted for 98.5% of all disorders. The main otologic clinical features were earache and a dull tympanic membrane in 100% and 35.4% of patients, respectively. Middle ear assessment revealed type A in 73.8% of patients and type B in 20.0% according to Jerger’s classification system of tympanometry. Most patients (81.5%) were referred by their family physician. All patients had undergone prehospital treatment prior to presentation.
Conclusion
Temporomandibular joint disorder is a common presentation in medical practice. Common clinical features include ear, joint, and mastication muscle disorders.
Keywords: Temporomandibular joint disorder, otorhinolaryngology, earache, otological manifestations, tympanometry, Ekiti
Introduction
Temporomandibular joint (TMJ) disorder (TMJD) comprises a range of clinicopathologic conditions of the masticatory muscles, the TMJ, and associated structures such as the ear.1 The TMJ aids Eustachian tube opening during its various movements, including yawning, chewing, biting, and opening and closing of the mouth.2–4 The causes of TMJD are multifactorial and include excessive masticatory muscle activity, harmful habits, TMJ trauma, degenerative disorders, and psychosocial factors.5,6 TMJ pain may also result from a combination of genetics, clenching or grinding of the teeth (bruxism), arthritis, autoimmune diseases, dental surgery, and infections.7
TMJD occurs in more than 70% of the general population in developed countries.8,9 Unfortunately, the knowledge and awareness of TMJD is very low at only about 25% of studied populations.8,9 Additionally, less than 10% of people with TMJD reportedly present for medical intervention, and most patients present with severe dysfunctional TMJD.9,10 The clinical presentations of TMJD include pain involving the TMJ and masticatory muscles, earache, and headache. Patients with severe TMJD may experience limited movement or dysfunction of chewing or mouth opening, difficulties in performing mandibular movements, a limited range of mandibular movements, and trismus.11–14 Otorhinolaryngological and head and neck manifestations include earache, tinnitus, hearing impairment, ear fullness, and vertigo.15,16 However, the mechanism underlying the development of these associated otological clinical features are poorly understood.17 In developing countries, especially Nigeria, there are few reports of TMJD. Additionally, there are few published reports by oral and maxillofacial surgeons or by otorhinolaryngological and head and neck surgeons. The present study was therefore designed to examine the knowledge and awareness of TMJD among patients seen in otorhinolaryngological practice in a developing country. This study was specifically performed to determine the prevalence, sociodemographic features, and clinical presentation of TMJD in otorhinolaryngological practice in Ekiti, Nigeria.
Materials and methods
This was a prospective hospital-based study of all patients diagnosed with and treated for TMJD in the Ear, Nose, and Throat Department of Ekiti State University Teaching Hospital in Ado Ekiti, Nigeria. The study was carried out over a period of 5 years (from September 2014 to August 2019).
Ethical clearance for this study was obtained from the ethics committee of the hospital. Verbal informed consent was obtained from all patients enrolled in the study. Data for this study were obtained from all patients with TMJD who were seen or referred for further evaluation from other departments using pretested interviewer-assisted questionnaires. The patients’ baseline and sociodemographic characteristics, clinical features, and diagnoses were obtained and documented. The inclusion criteria were a diagnosis of TMJD in our department during the study period and provision of informed consent for participation in the study. The exclusion criteria were a diagnosis other than TMJD, incomplete data, lack of informed consent, and an age of <11 years.
Otologic examinations including otoscopy were performed on all patients using a headlight and battery-operated hand otoscope to examine the external auditory canal and tympanic membrane for wax, foreign bodies, discharge, and tympanic membrane retraction or perforation. Patients with impacted wax underwent wax removal by ear syringing. Clinical examinations of the TMJ and muscles of mastication were performed by inspection and palpation, and all findings were recorded. Radiological imaging was performed for some patients, and those who were referred from other clinics for further evaluation underwent such imaging upon presentation. Hearing assessment was performed by tympanometry and pure tone audiometry using a tympanometer and a diagnostic audiometer, respectively. The resulting tympanogram was classified as type A, As, Ad, B, or C according to Jerger’s classification system of tympanometry.18 The patients’ hearing thres hold. was classified as follows: normal thres hold. (≤25 dB HL), mild hearing loss (26–40 dB HL), moderate hearing loss (41–55 dB HL), moderately severe hearing loss (56–70 dB HL), severe hearing loss (71–91 dB HL), and profound hearing loss (>91 dB HL).19 A hearing thres hold. of ≤25 dB HL was considered normal, and a hearing thres hold. of >25 dB HL was considered abnormal. All data were collated and analyzed using IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY, USA). The data are expressed using descriptive statistics in frequency tables, as percentages, and in bar charts and pie charts.
Results
In total, 4892 patients were seen in our ear, nose, and throat department during the study period. Among these patients, 65 were diagnosed with TMJD. The prevalence of TMJD in this study was 1.3%. TMJD is a relatively common disorder, and it occurred in all age groups in this study. The age range with the highest occurrence of TMJD was 51 to 60 years; 24 (36.9%) patients presented within this age range. This is illustrated in Table 1.
Table 1.
Age group distribution of the patients.
| Age (years) | Frequency (n) | Percentage (%) |
|---|---|---|
| 11–20 | 1 | 1.6 |
| 21–30 | 2 | 3.1 |
| 31–40 | 11 | 16.9 |
| 41–50 | 16 | 24.6 |
| 51–60 | 24 | 36.9 |
| ≥61 | 11 | 16.9 |
| 65 | 100.0 |
The patients’ sociodemographic characteristics are shown in Table 2. The study population comprised 17 (26.2%) male patients and 48 (73.8%) female patients with a male:female ratio of 1.0:2.8. Urban dwellers accounted for 41 (68.1%) of the patients, while rural dwellers accounted for 24 (36.9%). Fifty-three (81.5%) patients were Christians and 12 (18.5%) were Muslims. The most common education level was secondary school [24 (36.9%) patients], followed by post-secondary school [19 (29.2%)] and primary school [12 (18.5%)]. The main occupations among the patients in this study were civil service, business, and farming in 21 (32.3%), 16 (24.6%), and 14 (21.5%) patients, respectively.
Table 2.
Sociodemographic features of the patients.
| Sociodemographic features | Frequency (n) | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 17 | 26.2 |
| Female | 48 | 73.8 |
| Dwelling | ||
| Urban | 41 | 63.1 |
| Rural | 24 | 36.9 |
| Education level | ||
| No formal education | 10 | 15.4 |
| Primary | 12 | 18.5 |
| Secondary | 24 | 36.9 |
| Post-secondary | 19 | 29.2 |
| Occupation | ||
| Student/apprentice | 2 | 3.1 |
| Business | 16 | 24.6 |
| Artisan | 12 | 18.5 |
| Civil servant | 21 | 32.3 |
| Farming | 14 | 21.5 |
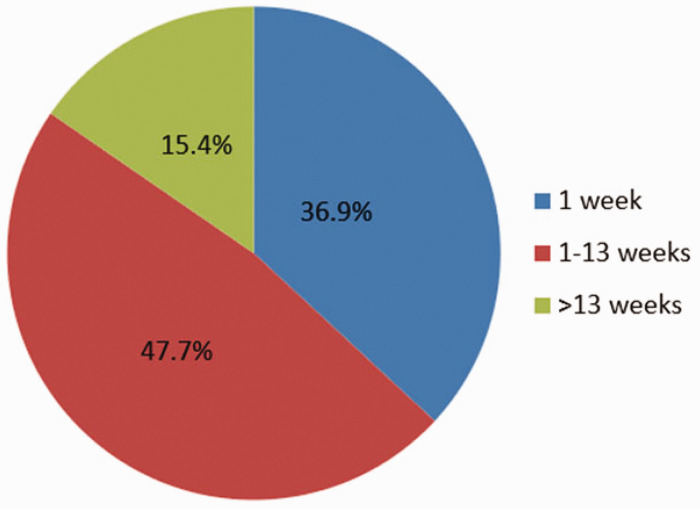
The TMJD in this study affected the joint, muscle, or both; it most commonly affected the TMJ [49 (75.4%) patients]. This was followed by disorder of both the masticatory muscles and the joint [14 (21.5%) patients] (Figure 1).
Figure 1.
Distribution of temporomandibular joint disorders.
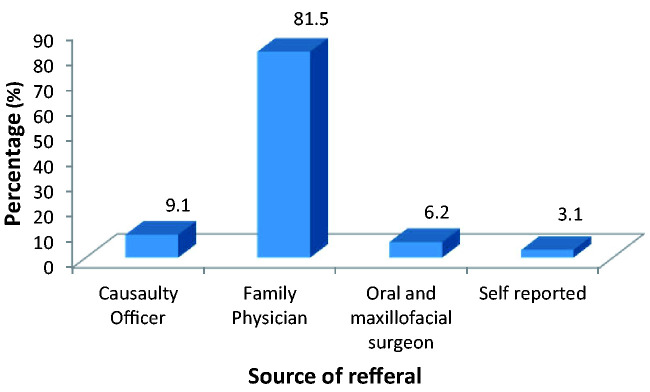
A majority of the patients (47.7%) presented between week 1 and 13 after onset of the disorder. Presentation within 1 week accounted for 24 (36.9%) patients, and presentation after 13 weeks accounted for 10 (15.4%) (Figure 2).
Figure 2.
Duration prior to presentation.
Unilateral TMJD was more common than bilateral TMJD [64 (98.5%) vs. 1 (1.5%) patient, respectively]. Additionally, right-side disorder was more common than left-side disorder [36 (55.4%) and 28 (43.1%) patients, respectively].
All patients presented with otologic features. The main otologic clinical features were earache and a dull tympanic membrane in 65 (100%) and 23 (35.4%) patients, respectively. Other clinical features included a sensation of water in the ear [15 (23.1%)] and itchy ear [12 (18.5%)] (Table 3).
Table 3.
Otologic clinical features among the patients.
| Otologic clinical features | Frequency (n) | Percentage (%) |
|---|---|---|
| Earache | 65 | 100 |
| Dizziness/vertigo | 2 | 3.1 |
| Tinnitus | 7 | 10.8 |
| Hearing impairment | 9 | 13.8 |
| Itchy ear | 12 | 18.5 |
| Water sensation in ear | 15 | 23.1 |
| Dull tympanic membrane | 23 | 35.4 |
NB: Some patients had more than one clinical feature.
All patients in this study had associated TMJ features. All patients had a painful and tender TMJ. This was followed in frequency by headache, masticatory muscle pain, and a popping/clicking joint in 31 (47.7%), 14 (21.5%), and 11 (16.9%) patients, respectively.
In the middle ear assessment, type A tympanometry was the most common finding [48 (73.8%) patients]. Type B was found in 13 (20.0%) patients, and type C was found in 4 (6.2%). Pure tone audiometry revealed normal hearing in 47 (72.3%) patients, and the most common degree of hearing impairment was mild hearing loss [17 (26.2%) patients]. The most common type of hearing loss was conductive hearing loss [16 (24.6%) patients] (Table 4).
Table 4.
Audiometry findings among the patients.
| Audiometry findings | Frequency (n) | Percentage (%) |
|---|---|---|
| Tympanometry | ||
| Type A | 48 | 73.8 |
| Type B | 13 | 20.0 |
| Type C | 4 | 6.2 |
| Degree of hearing impairment | ||
| Normal | 47 | 72.3 |
| Mild | 17 | 26.2 |
| Moderate | 1 | 1.5 |
| Type of hearing impairment | ||
| Conductive | 16 | 24.6 |
| Mixed | 2 | 3.1 |
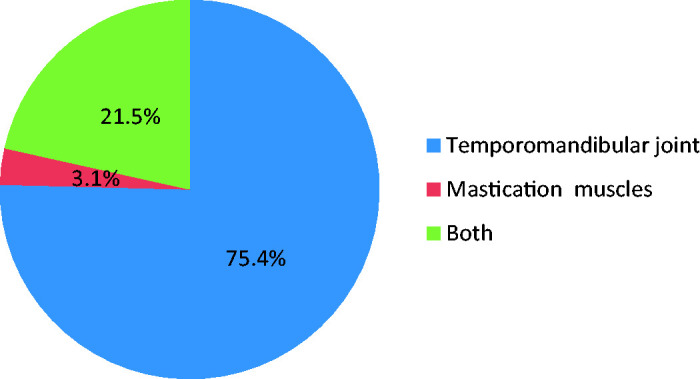
Most patients [53 (81.5%)] in this study were referred by their family physician; 2 (3.1%) were self-reported patients. Six (9.2%) patients were referred by a casualty officer (Figure 3).
Figure 3.
Source of referral among patients.
All patients had undergone prehospital treatment prior to presentation. The most common type of consultation was pharmacy consultation [39 (60.0%) patients]. This was followed by consultations for over-the-counter drugs and herbs in 33 (50.8%) and 14 (21.5%) patients, respectively. The most common prehospital treatments were ear drops, analgesics, and antibiotics in 65 (100%), 65 (100%), and 61 (93.8%) patients, respectively. Three (4.6%) patients were referred to an oral and maxillofacial surgeon.
Discussion
This study revealed an otologic presentation as a common finding among patients with TMJD in otorhinolaryngological practice.16 The observed prevalence of TMJD among patients presenting for otorhinolaryngological services in this study was lower than that in a study from Saudi Arabia.20 This difference is likely because the patients presented to other specialties for care, such as oral and maxillofacial surgeons and family physicians, and many of the patients never presented for an otological review. In patients with TMJD, ear manifestations result from either ear innervation disorders or an impaired Eustachian tube due to restricted jaw movement.
TMJD affected all age groups in the present study, but the peak incidence was noted in the 51- to 60-year age group. This might have been due to the predominant aging-related and degenerative changes among patients in this age group. The predominant age group with respect to the incidence of TMJD was found to be the fifth decade in an Iraqi study.21 TMJD was more common in female than male patients in our study, probably because female patients are more conscious of their health and seek earlier medical attention than male patients. However, male predominance was found in a study by Dawood.22 Another finding is that more urban dwellers than rural dwellers had TMJD in the present study. This may have been due to easier transportation and more accessible and high-quality health information among urban than rural dwellers. This is similar to the findings of a previous study that revealed a higher predominance of otorhinolaryngologists in cities.23
The high number of civil servants recorded in this study was not unexpected because the people of the state are predominantly government workers. In most patients, the pathology originated from the TMJ instead of the masticatory muscles. The particular anatomic relationships between the ear and the TMJ accounted for the variety of clinical features that were observed in this study. For example, there is anatomic proximity and trigeminal nerve innervation of both the ear and the joint. In a few patients, the pathology involved both the masticatory muscles and the TMJ. Rarely does a disorder of only the masticatory muscles lead to the observed presentation of TMJD. A similar observation was reported in another study.24 This shows that TMJD precedes otological manifestations upon presentation to an otorhinolaryngologist.
TMJD was associated with pain in all patients in the present study. In severe cases, this pain was responsible for the patients’ early presentation. Close to half of the patients presented between week 1 and 13 after the onset of symptoms. These patients presented because of persistent symptoms or failed treatment with analgesics. The analgesic failure was likely associated with all forms of analgesics and other drugs used by the patients in this study being easily accessed in pharmacies and over the counter without a doctor’s prescription in our country.
Most cases of TMJD in this study were on the right side, followed by the left side. This may have occurred because most of the patients were right-handed and chewed on the right side. Bilateral pathology was uncommon. These findings are consistent with those of previous studies.25,26
Earache or otalgia was the only driving indication for patients seeking otorhinolaryngological interventions. Such pain is referred or secondary otalgia due to trigeminal nerve innervation of both structures. Other observed clinical manifestations, such as tinnitus, hearing impairment, itchy ear, a sensation of water in the ear, and a dull tympanic membrane were secondary to Eustachian tube dysfunction and otitis media. This is consistent with the findings reported in previous studies.25–31
All patients exhibited both TMJ pain and demonstrable tenderness. A popping/clicking noise from the joint was present in some patients. In severe cases, restricted jaw movement due to either joint pain or ankylosis was present, and this was usually indication for team management with an oral and maxillofacial surgeon. The patients’ masticatory muscle pain and tenderness involved the temporalis, lateral pterygoid, medial pterygoid, and masseter muscles to various degrees. TMJD was associated with headache in about half of our patients. These findings are consistent with previous reports.27–29
Middle ear abnormalities and hearing disorders were also found among patients with TMJD.30,31 Normal tympanometric findings (type A) were observed in more than half of the patients. Less than half of the patients exhibited abnormalities of the middle ear, most of which were otitis media secondary to Eustachian tube dysfunction. Type B tympanometric findings were more common than type C in this study.30 Associated hearing impairment was present in less than half of the patients. Mild degrees of hearing loss were more common than moderate degrees, whereas severe degrees of hearing loss were not observed in this study.30,31 This lack of severe hearing loss probably accounted for the low percentage of these patients presenting to otorhinolaryngologists. No sensorineural hearing loss was observed in this study, and conductive hearing loss was more common than mixed hearing loss. The sensorineural component of mixed hearing loss was likely secondary to ototoxicity from prehospital medication.
Only a few patients with TMJD and associated otologic symptoms were referred to ear, nose, and throat department for expert review and management. The most common sources of referral were family physicians and casualty officers because they were the first contacts in the health care delivery system. Additionally, few patients with otologic complaints were referred by oral and maxillofacial surgeons for otorhinolaryngological treatment.
Prior to their medical consultations, a majority of the patients had been self-treated with a variety of drugs obtained over the counter and from pharmacies. This was due to the lack of laws guiding drug procurement, dispensary, and administration in developing countries such as ours. Most of these drugs comprised various types of analgesics and antibiotics. Other drugs included herbs from hawkers. Treatment failure using these medications prompted patients to seek medical intervention. Patients with severe trismus and associated TMJ ankylosis were referred and co-managed with an oral and maxillofacial surgeon in our center.
Conclusion
The findings in this study indicate a high prevalence of TMJD among ear, nose, and throat patients. We have highlighted the involvement of both the external ear and middle ear cleft among such patients. Referred otalgia from TMJD requires an otorhinolaryngological referral from all stakeholders managing this disorder. Large-population community studies on this subject in other developing countries are advised.
Acknowledgments
The authors are most grateful to Ekiti State University Teaching Hospital and to the staff and all patients who participated in this study.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Gabriel Toye Olajide https://orcid.org/0000-0002-8994-2699
References
- 1.Cavalcante BLL, Gabriel FCT, Da Cruz KR, et al. Prevalence of otological symptoms and parafunctional habits in patients with temporomandibular dysfunction. Rev CEFAC 2019; 21: e5318. 10.1590/1982-0216/20192115318 [DOI] [Google Scholar]
- 2.Kusdra PM, Stechman-Neto J, Cavalcante-Leao BL, et al. Relationship between otological symptoms and TMD. Int Tinnitus J 2018; 22: 30–34. [DOI] [PubMed] [Google Scholar]
- 3.Skog C, Fjellner J, Ekberg E, et al. Tinnitus as a comorbidity to temporomandibular disorders - a systematic review. J Oral Rehabil 2019; 46: 87–99. [DOI] [PubMed] [Google Scholar]
- 4.Farella MA, Michelotti A, Bocchino T, et al. Effects of orthognathic surgery for class III malocclusion on signs and symptoms of temporomandibular disorders and on pressure pain thresholds of the jaw muscles. Int J Maxilofac Oral Surg 2007; 2: 101–110. [DOI] [PubMed] [Google Scholar]
- 5.Sharma S, Gupta DS, Pal US, et al. Etiological factors of temporomandibular joint disorders. Natl J Maxillofac Surg 2011; 2: 116–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caria PHF, Faria RJA, Sgobbi of Faria CR, et al. Efficiency of occlusal splints on police officers with TMD. Braz J Oral Sci 2014; 13: 292–296. [Google Scholar]
- 7.Stepan L, Shaw CKL, Oue S. Temporomandibular disorder in otolaryngology: systematic review. J Laryngol Otol 2017; 131: S50–S56. [DOI] [PubMed] [Google Scholar]
- 8.Silvinelli F, Casale M, Paparo F, et al. Subjective tinnitus, temporomandibular joint dysfunction, and serotonin modulation of neural plasticity: causal or causal triad? Med Hypotheses 2003; 61: 444–448. [DOI] [PubMed] [Google Scholar]
- 9.Galdón MJ, Durá E, Andreu Y, et al. Multidimensional approach to the differences between muscular and articular temporomandibular patients: coping, distress and pain characteristics. Oral Radiol 2006; 102: 40–46. [DOI] [PubMed] [Google Scholar]
- 10.Machado IM, Bianchini EMG, Andrada e Silva MA, et al. Voz e disfunção temporomandibular em professores. Rev CEFAC 2009; 11: 630–643. 10.1590/S1516-18462009000800012 [DOI] [Google Scholar]
- 11.Oyetola EO, Adesina OM, Oluwadaisi A, et al. Temporomandibular joint pain: clinical presentations and response to conservative treatments in a Nigerian tertiary hospital. J Int Soc Prev Community Dent 2017; 7: 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nitzan DW, Palla S. “Closed reduction” principles can manage diverse conditions of temporomandibular joint vertical height loss: from displaced condylar fractures to idiopathic condylar resorption. J Oral Maxillofac Surg 2017; 75: 1163.e1–1163.e20. [DOI] [PubMed] [Google Scholar]
- 13.Choudhary SH, Kale LM, Mishra SS, et al. An institutional survey for knowledge-based and self-awareness assessment in temporomandibular joint disorders among dental students. Indian J Dent Res 2016; 27: 262. [DOI] [PubMed] [Google Scholar]
- 14.Sidebottom AJSF, Shahme F, Cascarini L. Current management of temporomandibular joint (TMJ) disease. J Arthritis 2014; 3: 1–4. 10.4172/2167-7921.1000138 [DOI] [Google Scholar]
- 15.Adegbiji WA, Olajide GT. Pattern of otalgia in Ekiti, Nigeria. American Journal of Medical Sciences and Medicine 2017; 5: 56–61. http://eprints.abuad.edu.ng/427/1/ajmsm-5-3-4%20a.pdf [Google Scholar]
- 16.Adegbiji WA, Olajide GT. Referred otalgia in Ekiti, Nigeria. European Journal of Pharmaceutical and Medical Research (ejpmr) 2017; 4: 141–147. [Google Scholar]
- 17.Mota LAA, Albuquerque KMG, Santos MHP, et al. Sinais e sintomas associados à otalgia na disfunção temporomandibular. Arq Int Otorrinolaringol 2007; 11: 411–415. [Google Scholar]
- 18.Onusko E. Tympanometry. Am Fam Physician 2004; 70: 1713–1720. [PubMed] [Google Scholar]
- 19.Jamaldeen J, Basheer A, Sarma AC, et al. Prevalence and patterns of hearing loss among chronic kidney disease patients undergoing haemodialysis. Australas Med J 2015; 8: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Habib SR, Al Rifaiy MQ, Awan KH, et al. Prevalence and severity of temporomandibular disorders among university students in Riyadh. Saudi Dent J 2015; 27: 125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buraa MF, Alazzawi HS. The relationship among otic clinical findings and temporomandibular joint disorders population. Iraqi Postgrad Med J 2013; 12: 546–550. https://ipmj.iraqiboard.edu.iq/article_85368.html [Google Scholar]
- 22.Dawood MR. The otological manifestation of temporomandibular disorders. Mustansiriya Medical Journal Volume 2013; 12: 45–48. http://mmj.uomustansiriyah.edu.iq/index.php/MMJ/article/view/177 [Google Scholar]
- 23.Adegbiji WA, Aremu SK, Lasisi AO. Patients barrier to ear, nose and throat surgical care in Nigeria. American Scientific Research Journal for Engineering, Technology, and Sciences (ASRJETS) 2017; 32: 96–104. https://asrjetsjournal.org/index.php/American_Scientific_Journal/article/view/2987 [Google Scholar]
- 24.Martins PFA, Stechman-Neto J, Marques JM, et al. Tinnitus and temporomandibular disorders: the knowledge of professionals for primary health care in the city of Curitiba. Int Tinnitus J 2016; 20: 18–23. [DOI] [PubMed] [Google Scholar]
- 25.Pihut M, Majewski P, Wisniewska G, et al. Auriculo-vestibular symptoms related to structural and functional disorders of stomatognatic system. J Physiol Pharmacol 2011; 62: 251–256. [PubMed] [Google Scholar]
- 26.Mohammad D, Kamal N, Abbassi S, et al. Assessment of the effect of temporomandibular joint bony ankylosis on Eustachian tube functions. International Journal of Clinical Oral and Maxillofacial Surgery 2017; 3: 1–6. 10.11648/j.ijcoms.20170301.11 [DOI] [Google Scholar]
- 27.Hilgenberg PB, Saldanha ADD, Cunha CO, et al. Temporomandibular disorders, otologic symptoms and depression levels in tinnitus patients. J Oral Rehabil 2012; 39: 239–244. [DOI] [PubMed] [Google Scholar]
- 28.Stechman-Neto J, Porporatti AL, Porto De Toledo I, et al. Effect of temporomandibular disorder therapy on otologic signs and symptoms: a systematic review. J Oral Rehabil 2016; 43: 468–479. [DOI] [PubMed] [Google Scholar]
- 29.Alkhudhairy MW, Al Ramel F, Al Jader G, et al. A self-reported association between temporomandibular joint disorders, headaches, and stress. J Int Soc Prev Community Dent 2018; 8: 371–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Totta T, Santiago G, Gonçales ES, et al. Auditory characteristics of individuals with temporomandibular dysfunctions and dentofacial deformities. Dental Press J Orthod 2013; 18: 70–77. [DOI] [PubMed] [Google Scholar]
- 31.Maciejewska-Szaniec Z, Maciejewska B, Mehr K, et al. Incidence of otologic symptoms and evaluation of the organ of hearing in patients with temporomandibular disorders (TDM). Med Sci Monit 2017; 23: 5123–5129. [DOI] [PMC free article] [PubMed] [Google Scholar]