Abstract
The circadian clock controls several aspects of mammalian physiology and orchestrates the daily oscillations of biological processes and behavior. Our circadian rhythms are driven by an endogenous central clock in the brain that synchronizes with clocks in peripheral tissues, thereby regulating our immune system and the severity of infections. These rhythms affect the pharmacokinetics and efficacy of therapeutic agents and vaccines. The core circadian regulatory circuits and clock-regulated host pathways provide fertile ground to identify novel antiviral therapies. An increased understanding of the role circadian systems play in regulating virus infection and the host response to the virus will inform our clinical management of these diseases. This review provides an overview of the experimental and clinical evidence reporting on the interplay between the circadian clock and viral infections, highlighting the importance of virus-clock research.
Keywords: circadian rhythm, viruses, COVID-19, virus-clock, virology
Introduction: Circadian Rhythms from the Macroscale to the Microscale
The Earth’s rotation leads to day/night cycles and drives our daily circadian rhythms right down to microscale processes at the cellular level. In mammals, the primary external time cue (zeitgeber) is the light/dark cycle that transduces signals through the retinohypothalamic tract to the suprachiasmatic nucleus (SCN) or “master clock” in the brain. The SCN communicates with the rest of the body to coordinate the circadian rhythm in every tissue (Astiz et al., 2019), allowing organisms to anticipate and adapt to their changing environment (Figure 1). The SCN comprises a complex neuronal network with multiple neural connections across the brain and transmits signals to the autonomic nervous and endocrine systems (Astiz et al., 2019). The influence of the SCN on the autonomic nervous system alters the sensitivity of peripheral tissues to hormones (Buijs et al., 2006). Consequently, the same hormone stimulus may induce different responses dependent on the time of the day (Becker et al., 2019; Garcia-Garcia and Mendez-Ferrer, 2020). The importance of the SCN as the main pacemaker becomes evident as transplantation of a functioning SCN reestablishes the circadian rhythm in genetically arrhythmic mice (Ralph et al., 1990; Sujino et al., 2003); however, other extracellular cues can independently synchronize peripheral tissues.
Figure 1.
Circadian regulation of the human body. External signals entrain the body’s central clock, the SCN in the brain, which in turn synchronizes peripheral clocks in organs and results in the molecular regulation of each cellular clock. Transcriptional/translational feedback loops coordinate rhythmic gene expression, and proteasomal degradation of the components restarts the system. BMAL1:CLOCK binds to E-Boxes and activates the expression of REV-ERB, RORα, and PER:CRY, which then directly inhibit BMAL1:CLOCK or act on Bmal1 promoter activity. SCN = suprachiasmatic nucleus; BMAL = brain and muscle ARNT-like 1; CLOCK = circadian locomotor output cycles kaput; ROR = related orphan receptor; PER = Period; CRY = Cryptochrome. Created with BioRender.com
Within individual cells, the circadian clock machinery is the self-sustaining product of transcriptional/translational feedback loops (TTFLs) consisting of activators and repressors (Figure 1). The two main activators, the basic helix-loop-helix transcription factors CLOCK (circadian locomotor output cycles kaput) and BMAL1 (brain and muscle ARNT-like 1), form heterodimers that bind genomic regulatory elements called E-boxes to regulate circadian gene expression. This complex induces the expression of the repressors PER (Period) and CRY (Cryptochrome), which dimerize and form a negative feedback loop that represses CLOCK:BMAL1-mediated transcription. A second interlocked TTFL regulates BMAL1 expression, comprising the nuclear receptors REV-ERBα and RORα, which bind retinoic acid–related orphan receptor (ROR) response elements (RORE) in the Bmal1 promoter to activate or inhibit its transcription, respectively (Guillaumond et al., 2005). REV-ERBα and RORα contain E-boxes in their promoters and hence are regulated by BMAL1:CLOCK. Ubiquitination-dependent degradation of these transcription factors resets the TTFL, establishing a 24-h oscillation of the RNA and protein products of these core clock regulators (Takahashi, 2017).
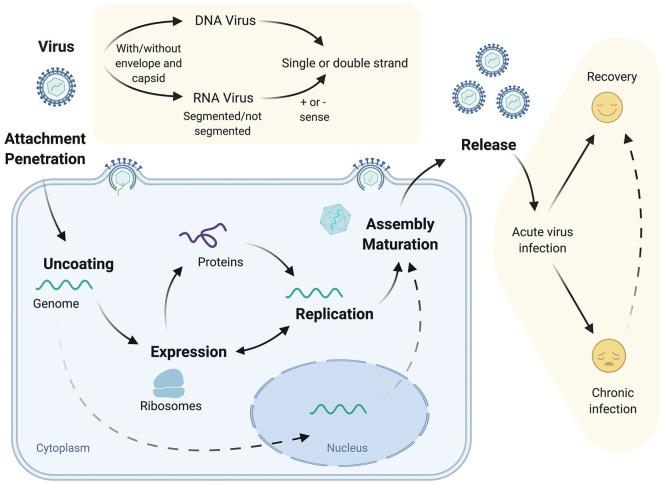
As obligate parasites, viruses are completely reliant on their hosts for replication and dissemination. The first step of the viral life cycle is its entry into the cell, via binding of the virion to host factors or receptors expressed at the cell surface (Helenius, 2018). After viral particle entry and capsid disassembly, the RNA or DNA genomes are released into the cell and exploit host transcriptional and translational pathways to initiate their replication (Figure 2). In simplistic terms, virus infections may be acute, a “hit-and-run” strategy of virus replication as exemplified by influenza virus, or chronic, establishing long-lasting infection such as hepatitis B virus (HBV), reflecting the balance between the host immune response and viral evasion strategies (Virgin et al., 2009). A recent study in primates uncovered that more than 80% of protein coding genes in various tissues show daily rhythmic expression (Mure et al., 2018), and given the dependency of virus replication on cellular pathways, it is unsurprising that host clock components have been reported to directly or indirectly influence virus replication.
Figure 2.
Virus structure, life cycle, and disease outcome. Viruses bear their genetic information as encapsidated RNA or DNA that may be enclosed in a lipid envelope. After the virus entry into the host cell, the genetic material is released, translated, and replicated. For some viruses, their genetic material is imported and replicated in the nucleus. After translation of the viral proteins and replication of the genome, new viral particles are assembled and released to complete the life cycle. Virus infection can be resolved by host immune responses or persist and cause chronic disease. Created with BioRender.com
More recently, a disrupted circadian clock has been linked to increasing susceptibility to several pathogen-associated diseases (Bellet et al., 2013; Kiessling et al., 2017; Hopwood et al., 2018; T. Li et al., 2019; Diallo et al., 2020; Kitchen et al., 2020), and the interplay between viral infections and the circadian clock is of increasing interest with an expansion of work in this area (Zhuang et al., 2017; Mazzoccoli et al., 2020). This review provides an overview of host-virus interactions from a circadian perspective and a summary of reported viral interactions with the circadian components (Table 1).
Table 1.
Overview of virus interactions with the cellular circadian clock.
| Virus | Clock Component | Effects and Proposed Mechanisms | References |
|---|---|---|---|
| Dengue virus | BMAL1, REV-ERB |
• Modulation of host lipid pathway essential for replication • REV-ERB inhibits stearoyl-CoA-desaturase expression (rate-limiting for infection) • Dengue infection increases the locomotor activity of vector Aedes aegypti females |
Lima-Camara et al. (2011); Zhuang et al. (2019) |
| Hepatitis B virus | CLOCK, BMAL1, PER1-3, CRY1,2 |
• Overexpression of HBx protein disrupts expression of circadian genes • Lower mRNA levels of Per1-3 and Cry2 in HCC tissue |
Yang et al. (2014) |
| Hepatitis C virus | BMAL1, REV-ERBPER2,CRY2 |
• HCV infection upregulates miR-10 which downregulates Bmal1 via suppressing RORα • Overexpression of Per2 counteracts HCV replication • Downregulation of Per2 and Cry2 in HCV patients • Modulation of host lipid pathway essential for replication • REV-ERB inhibits stearoyl-CoA-desaturase expression (rate-limiting for infection) |
Benegiamo et al. (2013); Zhuang et al. (2018, 2019); Horii et al. (2019) |
| Herpesvirus | CLOCK, BMAL1 |
• CLOCK activates expression of entry receptor via binding to its promoter • Virus induces BMAL1 expression, and low levels of BMAL1 increase infection • HSV viral protein IPC0 interacts with CLOCK:BMAL1, remodeling of viral chromatin |
Kalamvoki and Roizman (2010, 2011); Edgar et al. (2016); Matsuzawa et al. (2018) |
| Human immunodeficiency virus | CLOCK, BMAL1, REV-ERB, PER2 |
• CLOCK/BMAL1 drive HIV transcription via E-box in LTR, and REV-ERB decreases HIV promoter activity • Tat decreases amplitude of circadian rhythm • SNPs in CLOCK and Per2 genes alter sleep behavior |
Clark et al. (2005); Duncan et al. (2008); Wang et al. (2014); Lee et al. (2015b); Chang et al. (2018); Borrmann et al. (2020) |
| Influenza virus | BMAL1, CLOCK, REV-ERB,PER2 |
• Virus-induced Bmal1 expression • IAV advances Bmal1, Clock, and Rev-erbβ expression and increases Per2 amplitude • Low levels of BMAL1 increase viral load • Regulation of infection through time-dependant host tolerance/immune activation |
Sundar et al. (2015); Edgar et al. (2016); Ehlers et al. (2018); Sengupta et al. (2019) |
| Parainfluenza virus type 3 |
BMAL1 | • BMAL1 decreases viral replication | Majumdar et al. (2017) |
| Respiratory syncytial virus | BMAL1 | • BMAL1 decreases viral replication | Majumdar et al. (2017) |
| Simian immunodeficiency virus | Unknown | • Infection impairs amplitude of circadian rhythm of body temperature and locomotor activity | Huitron-Resendiz et al. (2007) |
| Zika virus | BMAL1, REV-ERB |
• Modulation of host lipid pathway essential for replication • REV-ERB inhibits stearoyl-CoA-desaturase expression (rate-limiting for infection) |
Zhuang et al. (2019) |
Abbreviations: BMAL = brain and muscle ARNT-like 1; CLOCK = circadian locomotor output cycles kaput; PER = Period; CRY = Cryptochrome; ROR = related orphan receptor; HSV = herpes simplex virus; LTR = long terminal repeat; HCC = hepatocellular carcinoma; SNP = single-nucleotide polymorphism; IAV = influenza A virus.
Circadian Pathways Shape Viral Infection
A Role for the Endocrine System in Regulating Viruses
Many factors can synchronize peripheral clocks, including the autonomic nervous system (Becker et al., 2019; Garcia-Garcia and Mendez-Ferrer, 2020), body temperature (Buhr et al., 2010), fasting/feeding cycles (Wehrens et al., 2017; Lewis et al., 2020), and cytokines and hormones (Astiz et al., 2019). The autonomic nervous system is influenced by the circadian clock, and some viruses can infect the peripheral and central nervous system (Koyuncu et al., 2013); however, at the present time, there is no evidence for a direct interaction of viruses, clock, and the autonomic nervous system. The endocrine system is the major route for synchronizing the SCN with peripheral clocks, and glucocorticoid expression is one of the best-studied examples (Oster et al., 2006, 2017; Pezuk et al., 2012). Glucocorticoid receptor signaling shows a bidirectional interaction with the circadian clock (Lamia et al., 2011; Caratti et al., 2018). Therapeutic administration of glucocorticoids (e.g., commonly prescribed cortisol) has been associated with the increased reactivation of HBV (Hatano et al., 2019) and poor clinical outcomes in influenza infection (Tsai et al., 2020). The glucocorticoid dexamethasone was recently shown to reduce the severity of coronavirus disease (COVID-19) (Delaney et al., 2016; Horby et al., 2020). The observation that corticosteroids suppress coronavirus HCoV-229E replication and cytokine production in primary cultures of human nasal and tracheal epithelial cells (Matsuyama et al., 2020; Yamaya et al., 2020) provides a potential mechanism for these clinical observations. Melatonin released from the pineal gland modulates sleep behavior and has been reported to have wide-ranging antiviral activities in virus-induced diseases (reviewed in Anderson and Reiter, 2020). In mouse model systems, melatonin can inhibit the NLRP3 inflammasome (Y. Zhang et al., 2016; Cao et al., 2017; Ma et al., 2018), leading us and others (Shneider et al., 2020) to speculate a role for this inflammatory pathway in COVID-19.
Circadian Regulation of Host Immunity: Impact on Virus Infection
To anticipate environmental changes and minimize the risk of infection, many immune parameters oscillate throughout the day (reviewed in Man et al., 2016; Scheiermann et al., 2018). Certain functions of the innate immune system depend on the cellular clock, where CLOCK, BMAL1, and REV-ERB regulate essential processes such as the expression of pattern recognition receptors (PRRs) that are involved in nucleic acid sensing during viral infections (Silver et al., 2012, 2018). Mice with latent murine γ-herpesvirus infection received an acute inflammatory challenge while being exposed to repeated chronic diurnal disruption that mimics shift work. The authors noted a reactivation of latent virus, leading to increased viral loads and changes in cytokine and chemokine concentrations in the lung (Trammell and Toth, 2016). Sengupta et al. (2019) showed the importance of natural killer T cells, natural killer cells, and inflammatory monocytes (Ly6chi monocytes) in the time-of-day dependency of influenza infection. Nguyen et al (2013) showed that BMAL1 regulated the diurnal oscillation of Ly6Chi monocytes. Other respiratory viruses are circadian-dependent: for example, Majumdar et al. (2017) reported that BMAL1 deficiency increased the susceptibility to respiratory syncytial virus (RSV) and PIV3 (human parainfluenza virus type 3) infection. REV-ERB can repress inflammatory responses and chemokine secretion in the context of pulmonary inflammation (Caratti et al., 2018). Genetic disruption of REV-ERB increased endotoxin responses in macrophages and enhanced secretion of the pro-inflammatory cytokine interleukin 6 (IL-6) (Gibbs et al., 2012). When studying macrophage biology, it is relevant to study their different biological functions separately as phagocytosis is not time-of-day dependent, whereas cytokine expression is rhythmic (Geiger et al., 2019). These patterns are also seen for the adaptive immune response, for example, in lymphocyte development and trafficking (reviewed in Scheiermann et al., 2018). Lymphocyte numbers oscillate over the course of the day, with glucocorticoids inducing diurnal T-cell accumulation in lymphoid organs (Shimba et al., 2018). Loss of lymphocyte circadian clocks ablates rhythmic adaptive immune responses important for combating influenza A virus (Druzd et al., 2017). BMAL1 is linked to mitochondrial function and metabolic pathways, which influences the phenotype and activity of immune cells. Rhythmicity of immunometabolism has become a key aspect of immune defense and disease outcomes (Early and Curtis, 2016; Carroll et al., 2019). These studies illustrate how the circadian clock regulates the immune response that impacts viral replication.
Circadian Regulation of Host Pathways Essential for Virus Infection
The liver is one of the most circadian-regulated organs of the body, with 20% of the transcriptome showing rhythmic expression (R. Zhang et al., 2014), and viruses infecting the liver are likely to be affected by the clock. A recent clinical study showed more rapid hepatitis C virus (HCV) reinfection kinetics following liver transplantation when the surgery was conducted in the morning compared with in the afternoon (Zhuang et al., 2018). In vitro studies showed that HCV infection of circadian-synchronized hepatocytes was linked to rhythmic expression of viral receptors (Zhuang et al., 2019), consistent with the increased infection kinetics observed after liver transplant. In addition, genetic knockout (KO) of Bmal1 or pharmacological activation of REV-ERB inhibited the replication of HCV and the related flaviviruses, dengue and Zika, by repressing lipid pathways that are essential for their replication (Zhuang et al., 2019).
Identifying host factors that associate with viral proteins can uncover new drug targets. A recent mapping of the interactome of SARS-CoV-2 proteins identified 66 druggable host factors (Gordon et al., 2020). It is worth noting that 30% of these host genes show circadian oscillation (Ray and Reddy, 2020), lending further support for circadian regulation of SARS-CoV-2 replication and potential chronotherapies in treating COVID-19 (Meira et al., 2020; Ray and Reddy, 2020).
Chang et al. (2018) reported an association between peripheral viral RNA levels in human immunodeficiency virus type 1 (HIV-1)-infected patients and the time of sampling, with increased levels of unspliced HIV RNAs associated with BMAL1 expression. Furthermore, CLOCK and BMAL1 overexpression induced HIV transcription via an E-box motif in the HIV long terminal repeat (LTR) (Chang et al., 2018). A recent study found that pharmacological activation of REV-ERB decreased BMAL1 and inhibited HIV LTR activity and viral replication in cell lines and primary CD4 T cells and induced pluripotent stem cell–derived macrophages (Borrmann et al., 2020). Importantly, mutations within the E-box reduced basal LTR activity, highlighting the multifunctional nature of this motif and suggest that circadian factors cooperate with other host transcription factors in regulating HIV replication. Interestingly, additional conserved circadian regulatory elements including the RORE and the glucocorticoid response element were found in the HIV-LTR, begging the question whether HIV replication may be synchronized at certain times of day.
Herpes simplex virus 2 (HSV-2) infection of mice was less severe when infection occurred during the rest phase compared with during the active phase (Matsuzawa et al., 2018). The HSV-2 entry receptor Nectin1 (Pvrl1) in mouse and human keratinocytes shows rhythmic expression and is directly regulated by CLOCK. CLOCK silencing decreased Pvrl1 expression, suggesting a role for CLOCK in regulating HSV-2 infection. Disrupting Bmal1 enhanced the replication of murid herpesvirus 4 (MuHV-4) and HSV-1 in vivo and in vitro in null allele Bmal1−/− models (Edgar et al., 2016). MuHV-4 DNA levels were higher when inoculation occurred at the beginning of the resting phase compared with infecting at the start of the active phase. Studies with a bioluminescent reporter virus showed an increased frequency of infected cells when Bmal1 expression was high. Of note, MuHV-4 induced Bmal1 expression regardless of the time of infection, suggesting that herpesviruses can perturb cellular circadian cycling. Similar observations were reported in HSV-1 and influenza A infection (Edgar et al., 2016).
Two independent studies assessed the circadian regulation of influenza virus infection (Ehlers et al., 2018; Sengupta et al., 2019). Both groups reported that Bmal1 KO mice showed greater asthma-like airway changes and worse acute viral bronchitis (Ehlers et al., 2018), and survival was higher when mice were infected before their active phase compared with before the resting phase (Sengupta et al., 2019). In contrast to the earlier Edgar study, Sengupta et al. did not observe differences in viral load when infecting mice at different time points. Infection at the start of the active phase promoted lung inflammation independent of the viral burden, suggesting that the more severe outcome of influenza infection is mediated by time-dependent regulation of host tolerance and immune activation pathways. Together, these studies highlight the importance of model systems in the viral-circadian studies—the in vitro isolated culture or the in vivo multicellular interactions—to characterize the role of circadian components in the viral life cycle.
Viruses and the Circadian CLOCK Shape the Chromatin Landscape
The influence of the circadian clock machinery on epigenetic regulation and chromatin remodeling partly reflects the histone deacetylase activity of CLOCK (Doi et al., 2006; Aguilar-Arnal and Sassone-Corsi, 2015). Time-dependent binding of circadian transcription factors (TFs) (Chen et al., 2015; Y. Xu et al., 2016) influences the chromatin state and RNA Pol II recruitment (Koike et al., 2012; Le Martelot et al., 2012; Pacheco-Bernal et al., 2019). Genome-wide RNA polymerase II profiles revealed rhythmic Pol II recruitment at promoters and dynamic changes in histone marks suggest daily remodeling of the epigenetic landscape (Le Martelot et al., 2012). A single circadian factor can control opposing transcriptional phases to generate complex circadian rhythms with multiple phases of gene expression (Fang et al., 2014). Clock components can define the transcriptionally permissive chromatin landscape that regulates the accessibility and activity of host transcriptional machinery (Menet et al., 2014; Trott and Menet, 2018). Viruses with DNA genomes may exploit this circadian epigenetic machinery to promote their own transcription and replication (Figure 3). HSV establishes a latent infection with periodical reactivation (Nicoll et al., 2012) and induces Bmal1 expression, leading to the reprogramming of clock signaling pathways. Kalamvoki and Roizman showed that the HSV-encoded protein ICP0 interacts with the CLOCK:BMAL1 histone acetyl transferase complex, and infecting cells with small interfering RNA (siRNA)-silenced Clock expression or engineered to express Clock mutants significantly reduced viral replication (Kalamvoki and Roizman, 2010; Kalamvoki and Roizman, 2011). These findings support a model where herpesvirus interaction with circadian clock components leads to a remodeling of viral chromatin that can regulate latency.
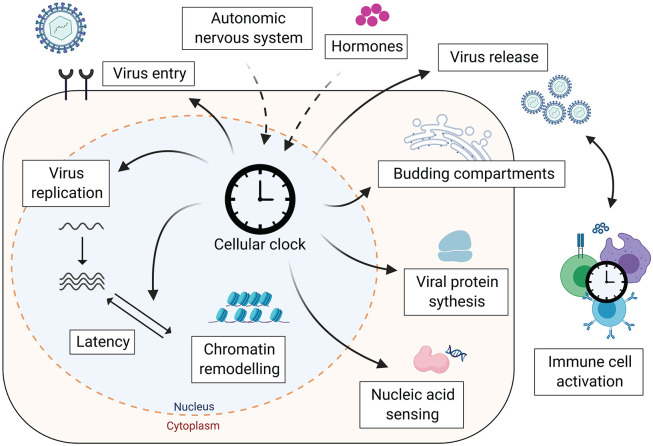
Figure 3.
Cellular clock affects the virus life cycle. The cellular clock can influence viral infection at multiple steps in the virus life cycle, from the regulation of entry receptors to lipid-dependent pathways for particle genesis. In addition, immune responses combating viral infections, such as nucleic acid sensing and the activity of immune cells, are regulated by cellular circadian clocks. Created with BioRender.com
Circadian and Annual Rhythms Affecting Viral Transmission
The mammalian circadian rhythm adapts to seasonal changes in the natural light/dark cycle; thus, the link between viral infections and circadian clock goes beyond the 24-h period. Seasonal differences may explain the increased susceptibility to viral infections during the winter months (Dowell, 2001). Annual cyclic incidence is a feature of epidemic disease, which is driven by environmental and exogenous factors, as well as host behavior and phenology (Martinez, 2018). Gene expression by immune cells and the cellular composition of blood varies by season, with gene expression patterns inverted between Northern and Southern hemispheres. Disease risk biomarkers like IL-6 receptor and C-reactive protein show increased expression in winter, which coincides with lower BMAL1 expression (Dopico et al., 2015). Similarly, immune function shows seasonal variation, with decreased neutrophil activity (Klink et al., 2012) but increased total blood monocyte numbers during winter (Dopico et al., 2015). An important regulator of seasonal physiological changes is altered hormone levels, where thyroid hormone levels vary in the hypothalamus and glucocorticoid receptors show their lowest expression in winter (Wood and Loudon, 2014; Dopico et al., 2015). The host, as well as nonhuman virus reservoirs and vector rhythmicity, impacts acute and chronic diseases outcomes.
Many viruses are transmitted by insect vectors that have their own circadian rhythm and are active at different times of the day (Meireles-Filho and Kyriacou, 2013). This influences whether the virus will encounter the host in its active or resting phase. For example, dengue virus is transmitted to humans by Aedes aegypti mosquitoes that are active during the day and dusk/dawn, and virus infection enhances mosquito activity (Lima-Camara et al., 2011). The transmission of Zika virus (ZIKV) is thought to be dependent on seasonal climate changes, and as more ZIKV incidence data become available, it will be important to define high and low transmission seasons (Petersen et al., 2016). Seasonally adjusted planning of pregnancy could limit vertical transmission by ensuring that sensitive gestational periods do not coincide with the ZIKV season (Martinez, 2016).
Human agricultural and technological interventions may also enhance the spread of viral diseases, for example, rice irrigation in summer months was shown to increase the incidence of Japanese encephalitis virus infection (Tian et al., 2015). Winter-associated light pollution is associated with increased risk of West Nile virus infection (Kernbach et al., 2019). Finally, climate change is altering annual environmental rhythms and disrupting seasonal biology, which may desynchronize biological clocks and impact human health (Stevenson et al., 2015).
Viruses Dictating the Time
Just as the host circadian rhythm can influence virus replication, virus infection can perturb the host circadian system (Figure 3). In vitro studies show that the HBV-encoded regulatory protein HBx perturbed circadian-regulated gene transcripts (Yang et al., 2014). It is worth noting that this study used HBx overexpression systems, and so these conclusions will require validation in authentic viral replication models. Levels of the microRNA miR-10a were elevated in liver biopsies from chronic HCV patients (Horii et al., 2019). In vitro analysis showed that overexpressing miR-10a in hepatocytes reduced Bmal1 expression by suppressing RORα. In a separate study, in vitro cell models expressing HCV core protein and liver biopsies from HCV-infected patients showed reduced PER2 and CRY2 expression (Benegiamo et al., 2013). Viral-dependent disruption of circadian signaling pathways may contribute to liver disease (Mukherji et al., 2019).
Influenza virus altered the timing of Bmal1, Clock, and Rev-erbβ peak expression in the lungs of infected mice and reduced the amplitude of Per2 expression in lung tissue explants (Sundar et al., 2015). Combined smoke exposure and influenza infection reduced locomotor activity in mice and has been associated with more severe asthma in humans (Ehlers et al., 2018). Simian immunodeficiency virus was reported to impair the amplitude and mean of the circadian rhythm of body temperature in monkeys and reduce locomotor activity (Huitron-Resendiz et al., 2007). HIV has also been shown to alter the circadian system in mice and humans. The HIV-encoded transactivator of transcription (Tat) protein resets the murine circadian clock by influencing light entrainment pathways (Clark et al., 2005). Chronic overexpression of Tat decreased the amplitude of the circadian wheel-running rhythm and locomotor activity in mice (Duncan et al., 2008). In HIV-1-infected patients, the Tat protein has been reported to promote melatonin expression, which may contribute to the impaired sleep quality frequently reported by HIV-infected individuals (Wang et al., 2014). In summary, viruses can influence circadian gene expression level by altering the activity of clock transcription factors or more generally via perturbing hormonal and light entrainment pathways. Published studies have largely focused on the direct effect(s) of viral-encoded proteins to interact with circadian regulators; however, additional pathways are likely to play a role and require investigation. For example, viruses that integrate into the host chromatin as part of their life cycle may perturb circadian-regulated gene expression. Many open questions remain, which would be interesting to investigate with a circadian lens in future studies.
Perfect Timing: Approaches for Therapy
Circadian Modulators
The host circadian machinery provides a wealth of therapeutic targets for antiviral interventions. Synthetic agonists of REV-ERB show in vivo activity in murine models (Solt et al., 2012) and alter immune responses by selective regulation of inflammatory cytokines (Gibbs et al., 2012). These agonists were reported to inhibit HCV entry, RNA replication, and release of infectious particles (Zhuang et al., 2019) via repressing expression of the fatty acid biosynthesis pathway component stearoyl-CoA-desaturase (SCD), a rate-limiting enzyme for HCV replication (Lyn et al., 2014; Nio et al., 2016). Similar observations were seen with the related flaviviruses, DENV and ZIKV, that also depend on fatty acid biosynthesis pathways (Paul and Bartenschlager, 2015). More recently, REV-ERB agonists were shown to inhibit HIV transcription and virus replication in primary cells (Borrmann et al., 2020). HSV and HIV can establish latent infection and thereby evade antiviral drugs and host immune responses. The histone deacetylase activity of the clock components could be targeted by circadian-modifying drugs to activate latent virus, complementing existing “shock and kill” eradication approaches for curing HIV (Deeks, 2012).
Additional pharmacological agents that modulate circadian protein activity have been developed (Miller and Hirota, 2020). These include CRY stabilizers (Hirota et al., 2012; J. W. Lee et al., 2015a) that inhibit BMAL1 expression and ROR modulators (Huh et al., 2011; Solt et al., 2011; Chai et al., 2020). ROR inverse agonists (Kumar et al., 2011) could have similar effects on viral replication as REV-ERB agonists, since they compete and bind the same DNA response element and regulate many of the same genes (Takeda et al., 2012). These ligands could be beneficial under certain circumstances to enhance or inhibit inflammatory (T. Xu et al., 2011) and viral responses.
It is interesting to consider the impact of circadian gene polymorphism on virus infection. K. A. Lee et al. (2015b) observed an association between genetic variability in circadian genes and sleep patterns in adults with HIV. In HIV-infected individuals, polymorphism in Clock and Per2 genes was associated with poor sleep maintenance (wake after sleep onset) and increased total sleep time; however, the underlying mechanisms are not well defined (K. A. Lee et al., 2015b).
Time of Day, Drug Administration, and Vaccination
Optimizing the time of day for medication is one aspect of personalized medicine, illustrated by the circadian timing of anticancer treatments (X. M. Li et al., 2013). An improved understanding of the circadian system may alter the time and amount of anti- viral drugs required. Recent studies show that the effective dose of acyclovir required to prevent HSV-2 infection in mice is 4 times higher during the active phase than during rest (Matsuzawa et al., 2018). Drug half-life is dependent on dosing time, such that drugs with short half-lives (6 h or less) may be more sensitive to the time of day of administration (Ruben et al., 2019).
The circadian clock of CD8 T cells modulates their response to vaccination, leading to higher T-cell activation in mice when vaccination with dendritic cells preloaded with ovalbumin peptide was performed during the day compared with during the night (Nobis et al., 2019). Influenza vaccination in humans was more effective when administered in the morning (9-11 a.m.) compared with in the afternoon (3-5 p.m.), with higher antibody responses measured against multiple influenza strains. No associations were observed between sex, steroid hormone or cytokine levels, and antibody responses (Long et al., 2016). The month of vaccine administration in countries with seasonally dependent environments can also affect antibody responses and protection against a range of viruses. The expression of B-cell maturation factor (BCMA or TNFRSF17) shows seasonal variation (Dopico et al., 2015) and expression levels are associated with a favorable response to the trivalent influenza vaccine (Nakaya et al., 2011; S. Li et al., 2014). Significant associations were observed between month of vaccination and antibody response to rabies vaccines in Pakistan compared with in Gambia (Moore et al., 2006). Seasonality in PRR expression that show increased expression during the winter months (Dopico et al., 2015) alters the quality of vaccine responses and correlates with better protection against yellow fever virus (Querec et al., 2009). These simple measures of timing drug or vaccine administration can increase drug efficiency and reduce side effects (Ruben et al., 2019; Zhao et al., 2020).
Conclusions and Keeping Track of Time
Having reviewed this growing field, we find clear evidence for a link between circadian rhythms and viral infection. Studying the interplay between circadian pathways and virus replication can offer many opportunities: a better understanding of viral infections and related immune responses, identification of new antiviral targets, refinement of current therapies, and treatment of chronic infection. The circadian clock is connected to many other pathways, including hypoxia signaling (Adamovich et al., 2017; Manella et al., 2020; Peek, 2020) and metabolism (Panda, 2016; Alexander et al., 2020; Cal-Kayitmazbatir et al., 2020). This crosstalk is likely to influence viral infection, and understanding these interactions will require multidisciplinary approaches involving virology, circadian biology, immunology, and pharmacology. Evolution is defined by the convergence of external rhythms with internal biology. As we live in an era of shift work–related sleep disorders, social jet lag, and global viral pandemics, together with emergent viral drug resistance, exploiting biological rhythms could provide novel treatment modalities and new drugs for treating viral infections. Plato wrote that “Rhythm and harmony find their way into the inward places of the soul” (Plato, The Republic, c. 375 BC): it is our responsibility to study how rhythmicity and synchronization can be integrated into human health.
Acknowledgments
We thank our colleagues Mirjam Schilling, James Harris, and Peter Balfe for helpful discussions and critical reading of our manuscript. The McKeating laboratory is funded by Wellcome Trust IA 200838/Z/16/Z and MRC project grant MR/R022011/1. H.B. is funded by the Wellcome Trust DPhil program in Infection, Immunology and Translational Medicine.
Footnotes
Conflict of Interest Statement: The author(s) have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iDs: Helene Borrmann  https://orcid.org/0000-0001-7269-7925
https://orcid.org/0000-0001-7269-7925
Xiaodong Zhuang  https://orcid.org/0000-0002-6870-9003
https://orcid.org/0000-0002-6870-9003
References
- Adamovich Y, Ladeuix B, Golik M, Koeners MP, Asher G. (2017) Rhythmic oxygen levels reset circadian clocks through HIF1alpha. Cell Metab 25:93-101. [DOI] [PubMed] [Google Scholar]
- Aguilar-Arnal L, Sassone-Corsi P. (2015) Chromatin landscape and circadian dynamics: spatial and temporal organization of clock transcription. Proc Natl Acad Sci U S A 112:6863-6870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander RK, Liou YH, Knudsen NH, Starost KA, Xu C, Hyde AL, Liu S, Jacobi D, Liao NS, Lee CH. (2020) Bmal1 integrates mitochondrial metabolism and macrophage activation. Elife 9:e54090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G, Reiter RJ. (2020) Melatonin: roles in influenza, covid-19, and other viral infections. Rev Med Virol 30:e2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astiz M, Heyde I, Oster H. (2019) Mechanisms of communication in the mammalian circadian timing system. Int J Mol Sci 20:343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker BK, Zhang D, Soliman R, Pollock DM. (2019) Autonomic nerves and circadian control of renal function. Auton Neurosci 217:58-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellet MM, Deriu E, Liu JZ, Grimaldi B, Blaschitz C, Zeller M, Edwards RA, Sahar S, Dandekar S, Baldi P, et al. (2013) Circadian clock regulates the host response to Salmonella. Proc Natl Acad Sci U S A 110:9897-9902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benegiamo G, Mazzoccoli G, Cappello F, Rappa F, Scibetta N, Oben J, Greco A, Williams R, Andriulli A, Vinciguerra M, et al. (2013) Mutual antagonism between circadian protein period 2 and hepatitis C virus replication in hepatocytes. PLoS ONE 8:e60527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrmann H, Davies R, Dickinson M, Pedroza-Pacheco I, Schilling M, Vaughan-Jackson A, Magri A, James W, Balfe P, Borrow P, et al. (2020) Pharmacological activation of the circadian component REV-ERB inhibits HIV-1 replication. Sci Rep 10:13271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhr ED, Yoo SH, Takahashi JS. (2010) Temperature as a universal resetting cue for mammalian circadian oscillators. Science 330:379-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buijs RM, Scheer FA, Kreier F, Yi C, Bos N, Goncharuk VD, Kalsbeek A. (2006) Organization of circadian functions: interaction with the body. Prog Brain Res 153:341-360. [DOI] [PubMed] [Google Scholar]
- Cal-Kayitmazbatir S, Kulkoyluoglu-Cotul E, Growe J, Selby CP, Rhoades SD, Malik D, Oner H, Asimgil H, Francey LJ, Sancar A, et al. (2020) CRY1-CBS binding regulates circadian clock function and metabolism. Febs J. DOI: 10.1111/febs.15360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Z, Fang Y, Lu Y, Tan D, Du C, Li Y, Ma Q, Yu J, Chen M, Zhou C, et al. (2017) Melatonin alleviates cadmium- induced liver injury by inhibiting the TXNIP-NLRP3 inflammasome. J Pineal Res 62:e12389. [DOI] [PubMed] [Google Scholar]
- Caratti G, Iqbal M, Hunter L, Kim D, Wang P, Vonslow RM, Begley N, Tetley AJ, Woodburn JL, Pariollaud M, et al. (2018) REV-ERBa couples the circadian clock to hepatic glucocorticoid action. J Clin Invest 128:4454-4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll RG, Timmons GA, Cervantes-Silva MP, Kennedy OD, Curtis AM. (2019) Immunometabolism around the Clock. Trends Mol Med 25:612-625. [DOI] [PubMed] [Google Scholar]
- Chai C, Cox B, Yaish D, Gross D, Rosenberg N, Amblard F, Shemuelian Z, Gefen M, Korach A, Tirosh O, et al. (2020) Agonist of RORA attenuates nonalcoholic fatty liver progression in mice via up-regulation of MicroRNA 122. Gastroenterology 159:999-1014.e1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CC, Naranbhai V, Stern J, Roche M, Dantanarayana A, Ke R, Tennakoon S, Solomon A, Hoh R, Hartogensis W, et al. (2018) Variation in cell-associated unspliced HIV RNA on antiretroviral therapy is associated with the circadian regulator brain-and-muscle-ARNT-like-1. AIDS 32:2119-2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Chen J, Muir LA, Ronquist S, Meixner W, Ljungman M, Ried T, Smale S, Rajapakse I. (2015) Functional organization of the human 4D Nucleome. Proc Natl Acad Sci U S A 112:8002-8007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark JP, III, Sampair CS, Kofuji P, Nath A, Ding JM. (2005) HIV protein, transactivator of transcription, alters circadian rhythms through the light entrainment pathway. Am J Physiol Regul Integr Comp Physiol 289:R656-R662. [DOI] [PubMed] [Google Scholar]
- Deeks SG. (2012) HIV: shock and kill. Nature 487:439-440. [DOI] [PubMed] [Google Scholar]
- Delaney JW, Pinto R, Long J, Lamontagne F, Adhikari NK, Kumar A, Marshall JC, Cook DJ, Jouvet P, Ferguson ND, et al. (2016) The influence of corticosteroid treatment on the outcome of influenza A(H1N1pdm09)-related critical illness. Crit Care 20:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diallo AB, Coiffard B, Leone M, Mezouar S, Mege JL. (2020) For whom the clock ticks: clinical chronobiology for infectious diseases. Front Immunol 11:1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doi M, Hirayama J, Sassone-Corsi P. (2006) Circadian regulator CLOCK is a histone acetyltransferase. Cell 125:497-508. [DOI] [PubMed] [Google Scholar]
- Dopico XC, Evangelou M, Ferreira RC, Guo H, Pekalski ML, Smyth DJ, Cooper N, Burren OS, Fulford AJ, Hennig BJ, et al. (2015) Widespread seasonal gene expression reveals annual differences in human immunity and physiology. Nature Commun 6:7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell SF. (2001) Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis 7:369-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druzd D, Matveeva O, Ince L, Harrison U, He W, Schmal C, Herzel H, Tsang AH, Kawakami N, Leliavski A, et al. (2017) Lymphocyte circadian clocks control lymph node trafficking and adaptive immune responses. Immunity 46:120-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan MJ, Bruce-Keller AJ, Conner C, Knapp PE, Xu R, Nath A, Hauser KF. (2008) Effects of chronic expression of the HIV-induced protein, transactivator of transcription, on circadian activity rhythms in mice, with or without morphine. Am J Physiol Regul Integr Comp Physiol 295:R1680-R1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Early JO, Curtis AM. (2016) Immunometabolism: is it under the eye of the clock? Semin Immunol 28:478-490. [DOI] [PubMed] [Google Scholar]
- Edgar RS, Stangherlin A, Nagy AD, Nicoll MP, Efstathiou S, O’Neill JS, Reddy AB. (2016) Cell autonomous regulation of herpes and influenza virus infection by the circadian clock. Proc Natl Acad Sci U S A 113:10085-10090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, Xie W, Agapov E, Brown S, Steinberg D, Tidwell R, Sajol G, Schutz R, Weaver R, Yu H, et al. (2018) BMAL1 links the circadian clock to viral airway pathology and asthma phenotypes. Mucosal Immunol 11:97-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang B, Everett LJ, Jager J, Briggs E, Armour SM, Feng D, Roy A, Gerhart-Hines Z, Sun Z, Lazar MA. (2014) Circadian enhancers coordinate multiple phases of rhythmic gene transcription in vivo. Cell 159:1140-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Garcia A, Mendez-Ferrer S. (2020) The autonomic nervous system pulls the strings to coordinate circadian HSC functions. Front Immunol 11:956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiger SS, Curtis AM, O’Neill LAJ, Siegel RM. (2019) Daily variation in macrophage phagocytosis is clock-independent and dispensable for cytokine production. Immunology 157:122-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs JE, Blaikley J, Beesley S, Matthews L, Simpson KD, Boyce SH, Farrow SN, Else KJ, Singh D, Ray DW, et al. (2012) The nuclear receptor REV-ERBα mediates circadian regulation of innate immunity through selective regulation of inflammatory cytokines. Proc Natl Acad Sci U S A 109:582-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K, White KM, O’Meara MJ, Rezelj VV, Guo JZ, Swaney DL, et al. (2020) A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 583:459-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillaumond F, Dardente H, Giguere V, Cermakian N. (2005) Differential control of Bmal1 circadian transcription by REV-ERB and ROR nuclear receptors. J Biol Rhythms 20:391-403. [DOI] [PubMed] [Google Scholar]
- Hatano M, Mimura T, Shimada A, Noda M, Katayama S. (2019) Hepatitis B virus reactivation with corticosteroid therapy in patients with adrenal insufficiency. Endocrinol Diabetes Metab 2:e00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helenius A. (2018) Virus entry: looking back and moving forward. J Mol Biol 430:1853-1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirota T, Lee JW, St John PC, Sawa M, Iwaisako K, Noguchi T, Pongsawakul PY, Sonntag T, Welsh DK, Brenner DA, et al. (2012) Identification of small molecule activators of cryptochrome. Science 337:1094-1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood TW, Hall S, Begley N, Forman R, Brown S, Vonslow R, Saer B, Little MC, Murphy EA, Hurst RJ, et al. (2018) The circadian regulator BMAL1 programmes responses to parasitic worm infection via a dendritic cell clock. Sci Rep 8:3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, et al. (2020) Dexamethasone in hospitalized patients with covid-19: preliminary report. N Engl J Med. DOI: 10.1056/ NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horii R, Honda M, Shirasaki T, Shimakami T, Shimizu R, Yamanaka S, Murai K, Kawaguchi K, Arai K, Yamashita T, et al. (2019) MicroRNA-10a impairs liver metabolism in hepatitis C virus-related cirrhosis through deregulation of the circadian clock gene brain and muscle aryl hydrocarbon receptor nuclear translocator-like 1. Hepatol Commun 3:1687-1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh JR, Leung MW, Huang P, Ryan DA, Krout MR, Malapaka RR, Chow J, Manel N, Ciofani M, Kim SV, et al. (2011) Digoxin and its derivatives suppress TH17 cell differentiation by antagonizing RORγt activity. Nature 472:486-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huitron-Resendiz S, Marcondes MC, Flynn CT, Lanigan CM, Fox HS. (2007) Effects of simian immunodeficiency virus on the circadian rhythms of body temperature and gross locomotor activity. Proc Natl Acad Sci U S A 104:15138-15143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalamvoki M, Roizman B. (2010) Circadian CLOCK histone acetyl transferase localizes at ND10 nuclear bodies and enables herpes simplex virus gene expression. Proc Natl Acad Sci U S A 107:17721-17726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalamvoki M, Roizman B. (2011) The histone acetyltransferase CLOCK is an essential component of the herpes simplex virus 1 transcriptome that includes TFIID, ICP4, ICP27, and ICP22. J Virol 85:9472-9477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernbach ME, Newhouse DJ, Miller JM, Hall RJ, Gibbons J, Oberstaller J, Selechnik D, Jiang RHY, Unnasch TR, Balakrishnan CN, et al. (2019) Light pollution increases West Nile virus competence of a ubiquitous passerine reservoir species. Proc Biol Sci 286:20191051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiessling S, Dubeau-Laramée G, Ohm H, Labrecque N, Olivier M, Cermakian N. (2017) The circadian clock in immune cells controls the magnitude of Leishmania parasite infection. Sci Rep 7:10892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitchen GB, Cunningham PS, Poolman TM, Iqbal M, Maidstone R, Baxter M, Bagnall J, Begley N, Saer B, Hussell T, et al. (2020) The clock gene Bmal1 inhibits macrophage motility, phagocytosis, and impairs defense against pneumonia. Proc Natl Acad Sci U S A 117:1543-1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klink M, Bednarska K, Blus E, Kielbik M, Sulowska Z. (2012) Seasonal changes in activities of human neutrophils in vitro. Inflamm Res 61:11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koike N, Yoo SH, Huang HC, Kumar V, Lee C, Kim TK, Takahashi JS. (2012) Transcriptional architecture and chromatin landscape of the core circadian clock in mammals. Science 338:349-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koyuncu OO, Hogue IB, Enquist LW. (2013) Virus infections in the nervous system. Cell Host Microbe 13:379-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar N, Kojetin DJ, Solt LA, Kumar KG, Nuhant P, Duckett DR, Cameron MD, Butler AA, Roush WR, Griffin PR, et al. (2011) Identification of SR3335 (ML-176): a synthetic RORα selective inverse agonist. ACS Chem Biol 6:218-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamia KA, Papp SJ, Yu RT, Barish GD, Uhlenhaut NH, Jonker JW, Downes M, Evans RM. (2011) Cryptochromes mediate rhythmic repression of the glucocorticoid receptor. Nature 480:552-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Martelot G, Canella D, Symul L, Migliavacca E, Gilardi F, Liechti R, Martin O, Harshman K, Delorenzi M, Desvergne B, et al. (2012) Genome-wide RNA polymerase II profiles and RNA accumulation reveal kinetics of transcription and associated epigenetic changes during diurnal cycles. PLoS Biol 10:e1001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JW, Hirota T, Kumar A, Kim NJ, Irle S, Kay SA. (2015. a) Development of small-molecule cryptochrome stabilizer derivatives as modulators of the circadian clock. ChemMedChem 10:1489-1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KA, Gay C, Byun E, Lerdal A, Pullinger CR, Aouizerat BE. (2015. b) Circadian regulation gene polymorphisms are associated with sleep disruption and duration, and circadian phase and rhythm in adults with HIV. Chronobiol Int 32:1278-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis P, Oster H, Korf HW, Foster RG, Erren TC. (2020) Food as a circadian time cue: evidence from human studies. Nat Rev Endocrinol 16:213-223. [DOI] [PubMed] [Google Scholar]
- Li S, Rouphael N, Duraisingham S, Romero-Steiner S, Presnell S, Davis C, Schmidt DS, Johnson SE, Milton A, Rajam G, et al. (2014) Molecular signatures of antibody responses derived from a systems biology study of five human vaccines. Nature Immunol 15:195-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, Shao W, Li S, Ma L, Zheng L, Shang W, Jia X, Sun P, Liang X, Jia J. (2019) H. pylori infection induced BMAL1 expression and rhythm disorder aggravate gastric inflammation. EBioMedicine 39:301-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li XM, Mohammad-Djafari A, Dumitru M, Dulong S, Filipski E, Siffroi-Fernandez S, Mteyrek A, Scaglione F, Guettier C, Delaunay F, et al. (2013) A circadian clock transcription model for the personalization of cancer chronotherapy. Cancer Res 73:7176-7188. [DOI] [PubMed] [Google Scholar]
- Lima-Camara TN, Bruno RV, Luz PM, Castro MG, Lourenco-de-Oliveira R, Sorgine MH, Peixoto AA. (2011) Dengue infection increases the locomotor activity of Aedes aegypti females. PLoS ONE 6:e17690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long JE, Drayson MT, Taylor AE, Toellner KM, Lord JM, Phillips AC. (2016) Morning vaccination enhances antibody response over afternoon vaccination: a cluster-randomised trial. Vaccine 34:2679-2685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyn RK, Singaravelu R, Kargman S, O’Hara S, Chan H, Oballa R, Huang Z, Jones DM, Ridsdale A, Russell RS, et al. (2014) Stearoyl-CoA desaturase inhibition blocks formation of hepatitis C virus-induced specialized membranes. Sci Rep 4:4549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma S, Chen J, Feng J, Zhang R, Fan M, Han D, Li X, Li C, Ren J, Wang Y, et al. (2018) Melatonin ameliorates the progression of atherosclerosis via mitophagy activation and NLRP3 inflammasome inhibition. Oxid Med Cell Longev 2018:9286458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar T, Dhar J, Patel S, Kondratov R, Barik S. (2017) Circadian transcription factor BMAL1 regulates innate immunity against select RNA viruses. Innate Immun 23:147-154. [DOI] [PubMed] [Google Scholar]
- Man K, Loudon A, Chawla A. (2016) Immunity around the clock. Science 354:999-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manella G, Aviram R, Bolshette N, Muvkadi S, Golik M, Smith DF, Asher G. (2020) Hypoxia induces a time- and tissue-specific response that elicits intertissue circadian clock misalignment. Proc Natl Acad Sci U S A 117:779-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez ME. (2016) Preventing Zika Virus infection during pregnancy using a seasonal window of opportunity for conception. PLoS Biol 14:e1002520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez ME. (2018) The calendar of epidemics: seasonal cycles of infectious diseases. PLoS Pathog 14:e1007327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuyama S, Kawase M, Nao N, Shirato K, Ujike M, Kamitani W, Shimojima M, Fukushi S. (2020) The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting the viral replication-transcription complex in cultured cells. J Virol. DOI: 10.1128/JVI.01648-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuzawa T, Nakamura Y, Ogawa Y, Ishimaru K, Goshima F, Shimada S, Nakao A, Kawamura T. (2018) Differential day-night outcome to HSV-2 cutaneous infection. J Invest Dermatol 138:233-236. [DOI] [PubMed] [Google Scholar]
- Mazzoccoli G, Vinciguerra M, Carbone A, Relógio A. (2020) The circadian clock, the immune system, and viral infections: the intricate relationship between biological time and host-virus interaction. Pathogens 9:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meira ECM, Miyazawa M, Gozal D. (2020) Putative contributions of circadian clock and sleep in the context of SARS-CoV-2 infection. Eur Respir J 55:2001023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meireles-Filho AC, Kyriacou CP. (2013) Circadian rhythms in insect disease vectors. Mem Inst Oswaldo Cruz 108:48-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menet JS, Pescatore S, Rosbash M. (2014) CLOCK:BMAL1 is a pioneer-like transcription factor. Genes Dev 28:8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S, Hirota T. (2020) Pharmacological interventions to circadian clocks and their molecular bases. J Mol Biol 432:3498-3514. [DOI] [PubMed] [Google Scholar]
- Moore SE, Collinson AC, Fulford AJ, Jalil F, Siegrist CA, Goldblatt D, Hanson LA, Prentice AM. (2006) Effect of month of vaccine administration on antibody responses in The Gambia and Pakistan. Trop Med Int Health 11:1529-1541. [DOI] [PubMed] [Google Scholar]
- Mukherji A, Bailey SM, Staels B, Baumert TF. (2019) The circadian clock and liver function in health and disease. J Hepatol 71:200-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mure LS, Le HD, Benegiamo G, Chang MW, Rios L, Jillani N, Ngotho M, Kariuki T, Dkhissi-Benyahya O, Cooper HM, et al. (2018) Diurnal transcriptome atlas of a primate across major neural and peripheral tissues. Science 359:eaao0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakaya HI, Wrammert J, Lee EK, Racioppi L, Marie-Kunze S, Haining WN, Means AR, Kasturi SP, Khan N, Li G-M, et al. (2011) Systems biology of vaccination for seasonal influenza in humans. Nature Immun 12:786-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen KD, Fentress SJ, Qiu Y, Yun K, Cox JS, Chawla A. (2013) Circadian gene Bmal1 regulates diurnal oscillations of Ly6C(hi) inflammatory monocytes. Science 341:1483-1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicoll MP, Proenca JT, Efstathiou S. (2012) The molecular basis of herpes simplex virus latency. FEMS Microbiol Rev 36:684-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nio Y, Hasegawa H, Okamura H, Miyayama Y, Akahori Y, Hijikata M. (2016) Liver-specific mono-unsaturated fatty acid synthase-1 inhibitor for anti-hepatitis C treatment. Antivir Res 132:262-267. [DOI] [PubMed] [Google Scholar]
- Nobis CC, Dubeau Laramee G, Kervezee L, Maurice De, Sousa D, Labrecque N, Cermakian N. (2019) The circadian clock of CD8 T cells modulates their early response to vaccination and the rhythmicity of related signaling pathways. Proc Natl Acad Sci U S A 116:20077-20086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster H, Challet E, Ott V, Arvat E, de Kloet ER, Dijk DJ, Lightman S, Vgontzas A, Van Cauter E. (2017) The functional and clinical significance of the 24-hour rhythm of circulating glucocorticoids. Endocr Rev 38:3-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster H, Damerow S, Kiessling S, Jakubcakova V, Abraham D, Tian J, Hoffmann MW, Eichele G. (2006) The circadian rhythm of glucocorticoids is regulated by a gating mechanism residing in the adrenal cortical clock. Cell Metab 4:163-173. [DOI] [PubMed] [Google Scholar]
- Pacheco-Bernal I, Becerril-Perez F, Aguilar-Arnal L. (2019) Circadian rhythms in the three-dimensional genome: implications of chromatin interactions for cyclic transcription. Clin Epigenetics 11:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda S. (2016) Circadian physiology of metabolism. Science 354:1008-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul D, Bartenschlager R. (2015) Flaviviridae replication organelles: oh, what a tangled web we weave. Annu Rev Virol 2:289-310. [DOI] [PubMed] [Google Scholar]
- Peek CB. (2020) Metabolic implications of circadian-HIF crosstalk. Trends Endocrinol Metab 31:459-468. [DOI] [PubMed] [Google Scholar]
- Petersen LR, Jamieson DJ, Powers AM, Honein MA. (2016) Zika virus. N Engl J Med 374:1552-1563. [DOI] [PubMed] [Google Scholar]
- Pezuk P, Mohawk JA, Wang LA, Menaker M. (2012) Glucocorticoids as entraining signals for peripheral circadian oscillators. Endocrinology 153:4775-4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Querec TD, Akondy RS, Lee EK, Cao W, Nakaya HI, Teuwen D, Pirani A, Gernert K, Deng J, Marzolf B, et al. (2009) Systems biology approach predicts immunogenicity of the yellow fever vaccine in humans. Nature Immun 10:116-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralph MR, Foster RG, Davis FC, Menaker M. (1990) Transplanted suprachiasmatic nucleus determines circadian period. Science 247:975-978. [DOI] [PubMed] [Google Scholar]
- Ray S, Reddy AB. (2020) COVID-19 management in light of the circadian clock. Nat Rev Mol Cell Biol 21:494-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruben MD, Smith DF, FitzGerald GA, Hogenesch JB. (2019) Dosing time matters. Science 365:547-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheiermann C, Gibbs J, Ince L, Loudon A. (2018) Clocking in to immunity. Nature Rev Immun 18:423-437. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Tang SY, Devine JC, Anderson ST, Nayak S, Zhang SL, Valenzuela A, Fisher DG, Grant GR, Lopez CB, et al. (2019) Circadian control of lung inflammation in influenza infection. Nature Commun 10:4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimba A, Cui G, Tani-Ichi S, Ogawa M, Abe S, Okazaki F, Kitano S, Miyachi H, Yamada H, Hara T, et al. (2018) Glucocorticoids drive diurnal oscillations in T cell distribution and responses by inducing interleukin-7 receptor and CXCR4. Immunity 48:286-298.e286. [DOI] [PubMed] [Google Scholar]
- Shneider A, Kudriavtsev A, Vakhrusheva A. (2020) Can melatonin reduce the severity of COVID-19 pandemic? Inter Rev Immun 39:153-162. [DOI] [PubMed] [Google Scholar]
- Silver AC, Arjona A, Walker WE, Fikrig E. (2012) The circadian clock controls toll-like receptor 9-mediated innate and adaptive immunity. Immunity 36:251-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver AC, Buckley SM, Hughes ME, Hastings AK, Nitabach MN, Fikrig E. (2018) Daily oscillations in expression and responsiveness of Toll-like receptors in splenic immune cells. Heliyon 4:e00579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solt LA, Kumar N, Nuhant P, Wang Y, Lauer JL, Liu J, Istrate MA, Kamenecka TM, Roush WR, Vidović D, et al. (2011) Suppression of TH17 differentiation and autoimmunity by a synthetic ROR ligand. Nature 472:491-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solt LA, Wang Y, Banerjee S, Hughes T, Kojetin DJ, Lundasen T, Shin Y, Liu J, Cameron MD, Noel R, et al. (2012) Regulation of circadian behaviour and metabolism by synthetic REV-ERB agonists. Nature 485:62-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson TJ, Visser ME, Arnold W, Barrett P, Biello S, Dawson A, Denlinger DL, Dominoni D, Ebling FJ, Elton S, et al. (2015) Disrupted seasonal biology impacts health, food security and ecosystems. Proc Biol Sci 282:20151453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sujino M, Masumoto K-H, Yamaguchi S, van der Horst GTJ, Okamura H, Inouye S-IT. (2003) Suprachiasmatic nucleus grafts restore circadian behavioral rhythms of genetically arrhythmic mice. Curr Biol 13:664-668. [DOI] [PubMed] [Google Scholar]
- Sundar IK, Ahmad T, Yao H, Hwang JW, Gerloff J, Lawrence BP, Sellix MT, Rahman I. (2015) Influenza A virus-dependent remodeling of pulmonary clock function in a mouse model of COPD. Sci Rep 4:9927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi JS. (2017) Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet 18:164-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda Y, Jothi R, Birault V, Jetten AM. (2012) RORγ directly regulates the circadian expression of clock genes and downstream targets in vivo. Nucleic Acids Res 40:8519-8535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian HY, Bi P, Cazelles B, Zhou S, Huang SQ, Yang J, Pei Y, Wu XX, Fu SH, Tong SL, et al. (2015) How environmental conditions impact mosquito ecology and Japanese encephalitis: an eco-epidemiological approach. Environ Int 79:17-24. [DOI] [PubMed] [Google Scholar]
- Trammell RA, Toth LA. (2016) Effects of chronic diurnal disruption and acute inflammatory challenge on mice with latent murine gammaherpesvirus infection. Comp Med 66:445-454. [PMC free article] [PubMed] [Google Scholar]
- Trott AJ, Menet JS. (2018) Regulation of circadian clock transcriptional output by CLOCK:BMAL1. PLoS Genet 14:e1007156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai MJ, Yang KY, Chan MC, Kao KC, Wang HC, Perng WC, Wu CL, Liang SJ, Fang WF, Tsai JR, et al. (2020) Impact of corticosteroid treatment on clinical outcomes of influenza-associated ARDS: a nationwide multicenter study. Ann Intensive Care 10:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virgin HW, Wherry EJ, Ahmed R. (2009) Redefining chronic viral infection. Cell 138:30-50. [DOI] [PubMed] [Google Scholar]
- Wang T, Jiang Z, Hou W, Li Z, Cheng S, Green LA, Wang Y, Wen X, Cai L, Clauss M, et al. (2014) HIV Tat protein affects circadian rhythmicity by interfering with the circadian system. HIV Med 15:565-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehrens SMT, Christou S, Isherwood C, Middleton B, Gibbs MA, Archer SN, Skene DJ, Johnston JD. (2017) Meal timing regulates the human circadian system. Curr Biol 27:1768-1775.e1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood S, Loudon A. (2014) Clocks for all seasons: unwinding the roles and mechanisms of circadian and interval timers in the hypothalamus and pituitary. J Endocrinol 222:R39-R59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu T, Wang X, Zhong B, Nurieva RI, Ding S, Dong C. (2011) Ursolic acid suppresses interleukin-17 (IL-17) production by selectively antagonizing the function of RORγt protein. J Biol Chem 286:22707-22710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Guo W, Li P, Zhang Y, Zhao M, Fan Z, Zhao Z, Yan J. (2016) Long-range chromosome interactions mediated by cohesin shape circadian gene expression. PLoS Genet 12:e1005992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaya M, Nishimura H, Deng X, Sugawara M, Watanabe O, Nomura K, Shimotai Y, Momma H, Ichinose M, Kawase T. (2020) Inhibitory effects of glycopyrronium, formoterol, and budesonide on coronavirus HCoV-229E replication and cytokine production by primary cultures of human nasal and tracheal epithelial cells. Respir Investig 58:155-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SL, Yu C, Jiang JX, Liu LP, Fang X, Wu C. (2014) Hepatitis B virus X protein disrupts the balance of the expression of circadian rhythm genes in hepatocellular carcinoma. Oncol Lett 8:2715-2720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. (2014) A circadian gene expression atlas in mammals: implications for biology and medicine. Proc Natl Acad Sci U S A 111:16219-16224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Li X, Grailer JJ, Wang N, Wang M, Yao J, Zhong R, Gao GF, Ward PA, Tan DX, et al. (2016) Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J Pineal Res 60:405-414. [DOI] [PubMed] [Google Scholar]
- Zhao M, Xing H, Chen M, Dong D, Wu B. (2020) Circadian clock-controlled drug metabolism and transport. Xenobiotica 50:495-505. [DOI] [PubMed] [Google Scholar]
- Zhuang X, Lai AG, McKeating JA, Rowe I, Balfe P. (2018) Daytime variation in hepatitis C virus replication kinetics following liver transplant. Wellcome Open Res 3:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang X, Magri A, Hill M, Lai AG, Kumar A, Rambhatla SB, Donald CL, Lopez-Clavijo AF, Rudge S, Pinnick K, et al. (2019) The circadian clock components BMAL1 and REV-ERBα regulate flavivirus replication. Nature Commun 10:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang X, Rambhatla SB, Lai AG, McKeating JA. (2017) Interplay between circadian clock and viral infection. J Mol Med 95:1283-1289. [DOI] [PMC free article] [PubMed] [Google Scholar]