Abstract
Purpose
To analyze the risk factors and comorbidities among the young Indian adults with hypertension.
Patients and Methods
This was a retrospective, multicentric real-world study which included patients diagnosed with and receiving treatment for hypertension. Data were collected from the medical records of clinics/hospitals across 623 study sites in India. Patients of either sex and aged 18–45 years were included. Demographic details (age, sex, anthropometric measurement), medical and family history, sedentary lifestyle, smoking status and alcohol consumption data were extracted. Descriptive and comparative analysis (Mann–Whitney U and chi-squared test) was done.
Results
Out of 15,006 young patients diagnosed with hypertension (men=63.6%), 65.7% belonged to the age group of >35–45 years. The median body mass index was 27.0 kg/m2. Patients diagnosed with only hypertension were 29.1% while other predominant comorbidities with hypertension were diabetes mellitus (42.4%) and dyslipidemia (7.8%). Hypertension with diabetes mellitus were prevalent in the age group of >35–45 years (43.8%). More than half of the patients with hypertension (n=7656) had a sedentary lifestyle. Overall, 35.6%, 47.3%, and 56.7% of the patients were alcoholic, smokers (present and former), and had a family history of hypertension, respectively.
Conclusion
The results showed that among the young population, hypertension was common in the age group of >35–45 years and diabetes mellitus and dyslipidemia were common comorbidities. Family history, sedentary lifestyle, smoking, alcohol consumption, and body mass index may also contribute to hypertension.
Keywords: diabetes mellitus, dyslipidemia, prevalence, young population
Introduction
Noncommunicable diseases, including hypertension, diabetes and obesity are highly prevalent in developed and developing countries including India. Worldwide, hypertension is emerging as a serious threat to the public health as it is a chief causative factor responsible for global deaths from stroke and coronary heart disease.1,2 The global action plan for the prevention and control of noncommunicable diseases by the World Health Organization (WHO) claimed to reduce the prevalence of hypertension by 25% between 2010 and 2025.3
Several factors are responsible for the growing prevalence of hypertension. These mainly include lifestyle and dietary practices, high body mass index (BMI), alcohol consumption, tobacco, smoking and emotional stress.4 The primary goal of therapy should be effective control of blood pressure in order to prevent, reverse or delay the complications.5,6 However, the prevalence of high blood pressure in the young Indian population is accelerating which creates a worrisome status quo due to higher risk of premature death. Data presented at 70th Annual Conference of the Cardiological Society of India (CSI), 2018 revealed that Indians possess more risk of developing hypertension in early years of life than western cohorts and incidence of first heart attack and strokes a decade earlier on average cannot be ignored.7,8 Ramakrishnan et al reported observations from an Indian blood pressure survey conducted across 24 states and union territories, demonstrating a severity of this crisis with prevalence of 55.3% in the adults of age group 20–44 years.9 Therefore, the evolving and rapidly growing epidemic of hypertension in young Indians should be considered equally important in increasing the burden of noncommunicable diseases and early diagnosis will aid in appropriate treatment and prevention of premature deaths.
Cross-sectional studies in the Asian population have reported various risk factors for hypertension. Nam et al demonstrated that age group, higher salt intake, alcohol consumption, presence of family history, and at least one co-existing disease were the risk factors for hypertension. They also reported significant differences in hypertension rates among factors including age groups, co-existing disease and alcohol consumption.10 A study was conducted in the Indonesian population demonstrating large socioeconomic inequalities in the utilization of hypertension and type 2 diabetes management services. They reported that education level and geographic location were the most important contributors of socioeconomic inequalities and these inequalities in medication use for hypertension and diabetes were predominant in men.11
Large clinical data gathered by national health system registries, health insurance companies, and randomized clinical trials, are an important basis for etiologic investigations and should adopt treatment and prevention strategies that will benefit the youth population in management of hypertension.12,13 In spite of few prior Indian studies revealing high prevalence of hypertension in the young adult population, the heterogeneity in study designs and ethnicities of the Indian population makes it difficult to generalize the management strategies. In addition, lack of awareness of hypertension in young individuals is also a major hurdle in prevention of premature deaths due to hypertension-associated comorbidities.8,14,15
Thus an effort was made in this multicentric, nonrandomized, noncomparative, real-world retrospective study that was conducted nationwide, inclusive of all four zones (north, south, east, west) to analyze the risk factors and associated comorbidities in young Indian patients (18–45 years) receiving medical attention for hypertension.
Patients and Methods
This was a retrospective, multicentric real-world study conducted in young individuals diagnosed with hypertension. The study was approved by the Independent Review Board (CLINICOM Independent Ethics Committee for Evaluation of Protocols for Clinical Research, Bangalore, India: 01441/31.07.2018; 01455/21.08.2018; 01463/30.08.2018; 01471/11.10.2018; 01483/22.11.2018; 01505/11.01.2019; 01516/05.03.2019; 01540/07.05.2019) and the study procedure was in accordance with the principles of the Declaration of Helsinki, International Conference on Harmonization—Good Clinical Practice (ICH-GCP). Considering the retrospective nature of the study consent from participants was waived. Data were collected from medical records of clinics/hospitals across 623 study sites in India. No identifiable details were captured and the patient’s record numbers were replaced with codes ensuring patient confidentiality. Patients of either sex, aged 18 to 45 years were eligible for inclusion if diagnosed and receiving treatment for hypertension. Patients aged above 45 years were excluded.
For patients with hypertension, the baseline characteristics of diagnosis of hypertension including age, sex, smoking habit, alcohol consumption, sedentary lifestyle, anthropometric measurements (height, weight, waist circumference), SBP and DBP were collected. Comorbidities (diabetes mellitus and dyslipidemia) and family history were also noted.
Definitions
According to the 2019 Indian Guideline on Hypertension-IV (IGH-IV) and 2018 European Society of Cardiology (ESC) and European Society of Hypertension (ESH) (ESC/ESH) guidelines, hypertension in adults aged 18 years and older is defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg.5,6 However, in the 2017 American College of Cardiology (ACC) and American Heart Association (AHA) (ACC/AHA) guidelines, hypertension is defined as ≥130/≥80 mmHg.16
Statistical Analysis
The data were presented as number and percentages for categorical data, or median and IQR for non-normally distributed continuous data. Normal distribution of quantitative data was assessed by Shapiro–Wilk test. A comparison of continuous and categorical variables between the groups was done using the Mann–Whitney U-test and chi-squared test, respectively. Odd ratios (OR) and 95%CI were calculated using multivariable logistic regression analyses. A value of p<0.05 was considered statistically significant. The data were analyzed using Statistical Package for The Social Sciences (SPSS) software, version 23.0.
Results
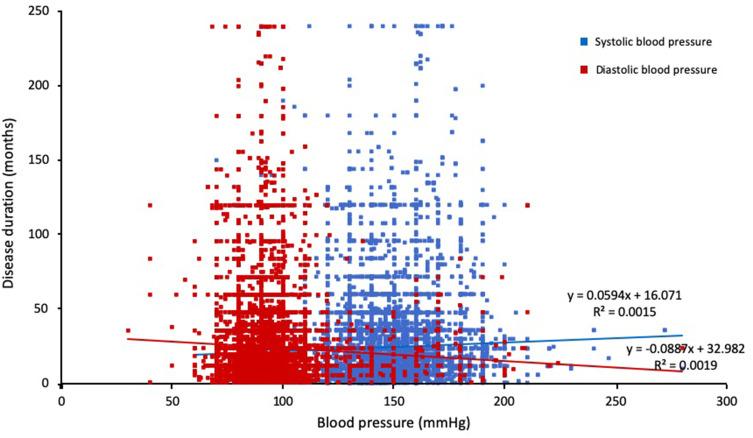
A total of 29,494 eligible patient case files were studied. Of them, a total of 15,006 young patients were diagnosed with hypertension and 63.6% were men. The remaining patients (n=14,488) did not satisfy the inclusion criteria and were excluded. Table 1 depicts the patient demographic characteristics. The majority of patients belonged to the age group of >35–45 years (65.7%), followed by the age group of >25–35 years (31.4%) and ≥18–25 years (2.9%). Most of the patients reported hypertension with diabetes mellitus (42.4%), followed by hypertension (29.1%), hypertension with both dyslipidemia and diabetes mellitus (20.7%) and least one was hypertension with dyslipidemia (7.8%). The majority of the patients (52.7%) were nonsmokers whereas other patients were regular (23.3%), occasional (18.5%) and former (5.3%) smokers. A total of 35.6% patients were regular alcohol consumers and more than 50% of the patients with hypertension were living a sedentary lifestyle (53.4%). The majority of the patients reported a family history of hypertension (56.7%) and hypertension with diabetes mellitus (39.2%) (Table 1). A negative correlation was observed between disease duration and blood pressure (Figure 1).
Table 1.
Patient’s Demographic Characteristics
| Parameters | Number of Patients (n=15,006)a |
|---|---|
| Age (years) | 37.0 (34.0–40.0) |
| Sex, % (n) | |
| Women | 36.4 (5463) |
| Men | 63.6 (9543) |
| Height (cm) | 165.0 (158.0–170.0) |
| Weight (kg) | 74.0 (66.0–82.0) |
| Waist circumference (cm) | 89.0 (76.0–96.5) |
| Body mass index (kg/m2) | 27.0 (24.6–29.8) |
| Diagnosed with, % (n) | |
| Hypertension | 29.1 (4366) |
| Hypertension and DM | 42.4 (6369) |
| Hypertension and dyslipidemia | 7.8 (1170) |
| Hypertension, dyslipidemia, and DM | 20.7 (3101) |
| Family history, % (n) | |
| Hypertension | 56.7 (8289) |
| Hypertension and DM | 39.2 (5876) |
| Hypertension and dyslipidemia | 20.2 (3029) |
| Hypertension, DM, and dyslipidemia | 17.1 (2566) |
| Smoking habits, n=14,324 % (n) | |
| No | 52.7 (7559) |
| Regular | 23.3 (3341) |
| Occasional | 18.5 (2656) |
| Former | 5.3 (768) |
| Alcohol consumption, n=14,524 % (n) | 35.6 (5177) |
| Sedentary lifestyle, n=14,327 % (n) | 53.4 (7656) |
Notes: Data shown as median (IQR), unless otherwise specified. an=15,006 unless otherwise specified.
Abbreviation: DM, diabetes mellitus.
Figure 1.
Scatter plot showing negative correlation between duration of disease and blood pressure.
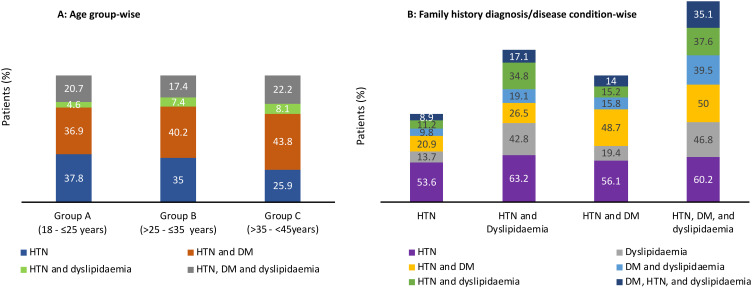
Age-wise Analysis
Figure 2A shows age-wise diagnosis. Table 2 shows age-wise distribution of parameters including sex, waist circumference, BMI, diagnosis, smoking habits, alcohol consumption, lifestyle and BP readings. The median waist circumference was significantly higher in the age group of >35–45 years compared to age group of ≥18–25 years (p=0.018). Among the smokers, the number of regular smokers were common in the age group of >35–45 years (24.1%), alcohol consumption was significantly higher in the age group of >25–35 years (35.1%), (p<0.001). More than half of the patients in all age groups were living a sedentary lifestyle.
Figure 2.
Distribution of patients according to (A) age group and (B) family history of diagnosis/disease condition.
Abbreviations: DM, diabetes mellitus; HTN, hypertension.
Table 2.
Age-wise Distribution of Parameters
| Parameters | Group A (≥18–25 Years) (n=439)* | Group B (>25–35 Years) (n=4705)** | Group C (>35–45 Years) (n=9862)*** | p-value |
|---|---|---|---|---|
| Age (years) | 24.0 (22.0–25.0) | 32.0 (30.0–34.0) | 39.0 (38.0–40.0) | <0.001a,b,c |
| Sex, % (n) | <0.001 | |||
| Female | 37.8 (166) | 38.0 (1787) | 35.6 (3510) | |
| Male | 62.2 (273) | 62.0 (2918) | 64.4 (6352) | |
| Waist circumference (cm) | 88.9 (80.0–96.0) n=327 | 88.0 (76.0–96.0) n=3471 | 90.0 (76.0–97.0) n=6940 | 0.016a, 0.018b, 1.000c |
| Body mass index (kg/m2) | 26.9 (23.4–30.3) n=409 | 26.7 (24.4–29.6) n=4530 | 27.1 (24.8–30.0) n=9585 | 1.000a, 0.490b, 0.049c |
| Diagnosed with, % (n) | <0.001 | |||
| Hypertension | 37.8 (166) | 35.0 (1646) | 25.9 (2554) | |
| Hypertension and DM | 36.9 (162) | 40.2 (1892) | 43.8 (4315) | |
| Hypertension and dyslipidemia | 4.6 (20) | 7.4 (347) | 8.1 (803) | |
| Hypertension, dyslipidemia, and DM | 20.7 (91) | 17.4 (820) | 22.2 (2190) | |
| Smoking habits, % (n) | n=417 | n=4496 | n=9411 | <0.001 |
| Former | 13.4 (56) | 6.2 (279) | 4.6 (433) | |
| No | 60.9 (254) | 53.9 (2426) | 51.8 (4879) | |
| Occasional | 8.8 (37) | 17.5 (787) | 19.4 (1832) | |
| Regular | 16.7 (70) | 22.3 (1004) | 24.1 (2267) | |
| Alcohol consumption, | n=420 | n=4566 | n=9538 | <0.001 |
| % (n) | 23.8 (100) | 35.1 (1602) | 26.4 (3475) | |
| Sedentary lifestyle, % (n) | 51.2 (209) n=408 | 52.4 (2368) n=4517 | 54.0 (5079) n=9402 | 0.139 |
| Duration of hypertension (days) | 540.0 (270.0–1080.0) n=363 | 360.0 (210.0–720.0) n=4120 | 540.0 (300.0–1080.0) n=8703 | <0.001a,b,c |
| Systolic blood pressure (mmHg) | 150.0 (138.0–162.0) | 153.0 (146.0–160.0) | 145.0 (135.0–160.0) | 0.052a, 0.008b, 0.364c |
| Systolic blood pressure mmHg, % (n) | ||||
| <140 | 25.5 (112) | 27.3 (1283) | 27.5 (2711) | - |
| ≥140 | 74.5 (327) | 72.7 (2711) | 72.5 (7151) | |
| Diastolic blood pressure (mmHg) | 90.0 (85.0–100.0) | 90.0 (86.0–100.0) | 90.0 (86.0–100.0) | <0.001a,b, 1.000c |
| Diastolic blood pressure (mmHg), %(n) | - | |||
| <90 | 30.3 (133) | 28.7 (1348) | 28.5 (2808) | |
| ≥90 | 69.7 (306) | 71.3 (3357) | 71.5 (7054) |
Notes: Data shown as median (IQR), unless otherwise specified. *n=439; **n=4705; ***n=9862 unless otherwise specified. aGroup A vs B; bGroup A vs C; cGroup B vs C.
Abbreviations: DM, diabetes mellitus.
Hypertension and Associated Comorbidities
Overall, 29.1% of patients had hypertension only, while remaining had coexistence of one or multiple comorbidities—hypertension with diabetes mellitus (42.4%), hypertension with diabetes mellitus and dyslipidemia (20.7%), and hypertension with dyslipidemia (7.8%) (Table 1). Hypertension with diabetes mellitus were prevalent in the age group of >35–45 years (43.8%). The presentation of triad (hypertension, diabetes mellitus and dyslipidemia) were more common in the age group of >35–45 years (22.2%) and least common in the age group of >25–35 years (17.4%) (Table 2).
Diagnosis-wise Analysis
The majority of the patients were men in all the diagnosis groups (p<0.001). The median age of the patients at hypertension diagnosis was ranging between 36 and 38 years. The majority of the patients diagnosed with hypertension along with diabetes mellitus and dyslipidemia belonged to the age group of >35–45 years. Comparison was based on the SBP and DBP according to ACC/AHA and ESC/ESH guidelines:
As per IGH-IV and ESC/ESH guidelines, majority of patients had stage 1 (40.9%) hypertension, followed by stage 2 (27.8%) hypertension, stage 3 (12.5%) hypertension and elevated BP (10.7%). Similarly, according to ACC/AHA guidelines stratification, 73.2%, 22.7%, and 2.5% patients had stage 2 hypertension, stage 1 hypertension, and elevated BP, respectively; while a small percentage of patients have shown to maintain normal BP (Table 3). According to IGH-IV and ESC/ESH guidelines, 71.5% and 67.1% of patients while according to ACC/AHA guidelines, 88.0% and 93.0% of patients had uncontrolled SBP and DBP, respectively (Table 3).
Table 3.
Prevalence of Uncontrolled Blood Pressure
| Uncontrolleda | IGH-IV 2019 and ESC/ESH 2018 | ACC/AHA 2017 | ||||
|---|---|---|---|---|---|---|
| Men (n=9148a; n=9070b) | Women (n=5244a; n=5148b) | Total (n=14,398a; n=14,254b) | Men (n=5244a; n=5148b) | Women (n=5244a; n=5148b) | Total (n=14,398a; n=14,254b) | |
| SBP | 72.7 (6655) | 69.3 (3632) | 71.5 (10,287) | 88.8 (8123) | 86.5 (4538) | 88.0 (12,661) |
| DBP | 68.0 (6167) | 65.6 (3399) | 67.1 (9566) | 93.7 (8495) | 91.9 (4764) | 93.0 (13,259) |
Notes: Data presented as % (n). aTotal number of patients with available SBP values;bTotal number of patients with available DBP values: uncontrolled SBP defined as SBP ≥140 mmHg (IGH-IV and ESC/ESH) and SBP ≥130 mmHg (ACC/AHA); uncontrolled DBP defined as DBP ≥90 mmHg (IGH-IV and ESC/ESH) and SBP ≥80 mmHg (ACC/AHA).
Abbreviations: ACC/AHA, American College of Cardiology (ACC) and American Heart Association (AHA);ESC/ESH, European Society of Cardiology (ESC) and European Society of Hypertension (ESH); IGH-IV, Indian Guideline on Hypertension-IV.
The anthropometric parameters of patients (BMI and waist circumference) are summarized in Table 4 and distribution of family history is shown in Figure 2B. Among patients in all diagnosis groups, regular smokers had higher prevalence of smoking followed by occasional and former smokers. Alcohol consumption was highest in patients diagnosed with hypertension and dyslipidemia (42.7%). The majority of the patients in all the diagnosis groups were living a sedentary lifestyle (p<0.001). The median levels of SBP were significantly higher in patients diagnosed with hypertension and hypertension with dyslipidemia (150.0 mmHg) while DBP was high in all the diagnosis groups (90.0 mmHg) (Table 4).
Table 4.
Diagnosis-Wise Distribution of Parameters
| Parameters | Diagnosis | p value | |||
|---|---|---|---|---|---|
| Group A: Hypertension Only (n=4366)* | Group B: Hypertension and Dyslipidemia (n=1170)** | Group C: Hypertension and Diabetes Mellitus (n=6369)*** | Group D: Hypertension, Diabetes Mellitus, and Dyslipidemia (n=3101)**** | ||
| Age (years) | 36.0 (32.0–39.0) | 38.0 (34.0–40.0) | 38.0 (34.0–40.0) | 38.0 (35.0–40.0) | <0.001a, b, c, f, 0.651d, 0.055e, |
| Sex, % (n) | <0.001 | ||||
| Women | 38.0 (1660) | 31.8 (372) | 37.0 (2357) | 34.6 (1074) | |
| Men | 62.0 (2706) | 68.2 (798) | 63.0 (4012) | 65.4 (2027) | |
| Waist circumference (cm) | 86.0 (72.0–95.0) | 90.0 (83.0–97.1) | 90.0 (77.0–96.5) | 91.0 (80.0–100.0) | <0.001 a,b,c,f, 0.007d, 0.223e, |
| Body mass index (kg/m2) | 26.2 (24.0–29.0) | 27.5 (25.2–30.4) | 27.1 (24.7–29.7) | 27.7 (25.2–30.8) | <0.001 a,b,c,f, 0.001 d, 0.043e |
| Smoking Habits, % (n) | n=4258 | n=1102 | n=6127 | n=2837 | |
| Former | 4.5 (192) | 5.3 (59) | 5.7 (351) | 5.8 (166) | |
| No | 52.3 (2230) | 48.8 (538) | 53.4 (3274) | 53.4 (1517) | <0.001 |
| Occasional | 19.5 (833) | 17.8 (196) | 18.4 (1128) | 17.5 (499) | |
| regular | 23.5 (1003) | 28.0 (309) | 22.4 (1374) | 23.1 (655) | |
| Alcohol consumption, % (n) | 33.8 (1459) | 42.7 (477) | 34.2 (2121) | 38.9 (1120) | <0.001 |
| Sedentary lifestyle, % (n) | 47.6 (2027) | 56.6 (627) | 52.4 (3196) | 1806 (63.1) | <0.001 |
| Systolic blood pressure (mmHg) | 150.0 (140.0–160.0) | 150.0 (140.0–160.0) | 142.0 (132.0–160.0) | 140.0 (130.0–156.0) | <0.007 a, <0.001 b,c,d,e,f |
| Diastolic blood pressure (mmHg) | 90.0 (90.0–100) | 90.0 (90.0–100) | 90.0 (85.0–98.0) | 90.0 (80.0–98.0) | <0.136 a, <0.001 b,c,d,e,f |
Notes: Data shown as median (IQR), unless otherwise specified. *n=4366; **n=1170; ***n=6369; ****n=3101, unless otherwise specified. aGroup A vs B; bGroup A vs C; cGroup A vs D; dGroup B vs C; eGroup B vs D; fGroup C vs D.
Multiple Regression Analysis
Table 5 depicts the results of multiple regression analysis of independent risk factors associated with hypertension. Age, alcohol, sedentary lifestyle, waist circumference and family history of diabetes, hypertension and dyslipidemia were significantly associated risk factors observed both in the hypertension and dyslipidemia group and hypertension and diabetes group of patients.
Table 5.
Multiple Regression Analysis of Risk Factors Associated with Hypertension
| Parameters | HTN and Dyslipidemia | HTN and DM | ||
|---|---|---|---|---|
| Odds Ratio | (95%CI); p-value | Odds Ratio | (95%CI); p-value | |
| Age (years) | 0.025 | (0.007, 0.034); 0.002 | −0.012 | (−0.017, −0.004); 0.002 |
| Sex | 0.002 | (−0.018, 0.021); 0.844 | −0.001 | (−0.011, 0.009); 0.844 |
| Smoking | 0.016 | (−0.001, 0.013); 0.118 | −0.007 | (−0.006, 0.001); 0.118 |
| Alcohol | −0.042 | (−0.058, −0.021); <0.001 | 0.020 | (0.010, 0.029); <0.001 |
| Sedentary lifestyle | −0.024 | (−0.037, −0.007); 0.004 | 0.011 | (0.004, 0.019); 0.004 |
| Height (cm) | −0.011 | (−0.001, 0.000); 0.266 | 0.005 | (0.000, 0.001); 0.266 |
| Weight (kg) | 0.018 | (0.000, 0.001); 0.055 | −0.009 | (−0.001, 0.000); 0.055 |
| Waist circumference (cm) | 0.027 | (0.000, 0.001); 0.001 | −0.013 | (0.000, 0.000); 0.001 |
| Family history of DM | 0.133 | (0.096, 0.147); <0.001 | −0.062 | (−0.074, −0.048); <0.001 |
| Family history of HTN | −0.094 | (−0.112, −0.062); <0.001 | 0.044 | (0.031, 0.056); <0.001 |
| Family history of DYS | −0.155 | (−0.225, −0.089); <0.001 | 0.073 | (0.045, 0.113); <0.001 |
| Family history of DM and HTN | 0.119 | (0.074, 0.145); <0.001 | −0.056 | (−0.073, −0.037); <0.001 |
| Family history of DM and DYS | −0.015 | (−0.102, 0.069); 0.705 | 0.007 | (−0.035, 0.051); 0.705 |
| Family history of HTN and DYS | −0.077 | (−0.162, 0.000); 0.050 | 0.036 | (0.000, 0.081); 0.050 |
| Family history of DM, HTN, and DYS | −0.004 | (−0.103, 0.095); 0.930 | 0.002 | (−0.047, 0.052); 0.930 |
Abbreviations: DM, diabetes mellitus; DYS, dyslipidemia; HTN, hypertension.
Discussion
This study provides several insights about the risk factors and comorbidities in the young Indian adults (≤45 years) with hypertension. Furthermore, factors including age, sex, BMI, waist circumference, history of disease, alcohol consumption, BP data, smoking habits, and sedentary lifestyle were also taken into consideration. Of these risk factors, age, alcohol, sedentary lifestyle, waist circumference and family history of diabetes, hypertension and dyslipidemia were significantly associated in patients with hypertension and dyslipidemia and hypertension and diabetes. The incidence of hypertension, standardized by age was higher in the age group of >35–45 years. Studies have reported the prevalence of hypertension in young population indicating a significant risk of cardiovascular disease (CVD) at young age in Asian population.17,18 In the present study, comparison of SBP and DBP based on varying definitions provided in IGH-IV, ESC/ESH and ACC/AHA guidelines revealed that more than 67% of youth population failed to achieve target SBP/DBP with given treatment and may suggest the need of extensive BP monitoring and modification in the ongoing management strategies. These results corroborate the high prevalence of hypertension in young adult Indian population, suggesting hypertension screening from a young age could benefit in early diagnosis and implementation of prevention strategies for better management of the disease and associated comorbidities ultimately alleviating rates of premature deaths in Indian population.
In the overall population, among patients with hypertension, diabetes mellitus was the most common comorbidity. Previous studies identified that prevalence levels of hypertension and diabetes mellitus were higher in Indian young adults.8,9 Cross-sectional study conducted in ten Indian states in a series of 15,662 patients showed a positive correlation between hypertension and diabetes mellitus, age, family history, alcohol, diet and medical history of CVD.19 Hypertension and its related comorbidities in young adults are major health problems in India. Furthermore, studies are required to characterize patients affected by hypertension along with the comorbidities such as diabetes mellitus and dyslipidemia with the purpose of development of pharmacotherapy.
Family history of patients related to diabetes mellitus and dyslipidemia was the major finding. Studies from different countries have shown that the patients with family history were nearly 1.4 times more prone to risk of hypertension compared to patients without the presence of family history.20–22 Similarly, the results from the present study confirmed that a family history of hypertension has a significant association with hypertension.
In the overall population, the median BMI was 27.0 kg/m2 which is overweight. In the present study, it was observed that SBP and DBP values were both linearly correlated with BMI precisely, obesity and being overweight were probable causes of hypertension in young adults. Reported literature showed that other than age and gender, BMI is a persistent cause of high prevalence of hypertension. Feng et al found that distribution of body fat is an important risk factor for obesity-based diseases such as hypertension. Some clinical practices demonstrate that waist circumference is used as a replacement marker of abdominal fat mass and is majorly associated with cardiometabolic disease risks.23
The majority of the patients in all the age groups had a sedentary lifestyle which is the most important predictor of hypertension. Other lifestyle factors that play an important role to increase the occurrence of hypertension are smoking habits and alcohol consumption which is in accordance with the present study. Former literature, among the participants with a higher level of education and economic status and even with awareness of risk factors of hypertension, prevalence of hypertension was high because of physical inactivity and nonadherence to medication.4
Recent literature proposed that knowledge of hypertension is related to BP control.24 Furthermore, it was found that the risk of poor BP control increased due to lack of awareness of knowledge of SBP. A recently published Indian study revealed that the proportion of adults with hypertension who are aware of their diagnosis and are treated and achieve control, is low, despite of higher incidence of hypertension among patients 15–49 years of age.25
Kanegae et al reported that in younger patients, the effect of DBP is very important on developing hypertension; hence, need to target DBP lowering in these patients. In the age-wise analysis of this study, the risk of developing hypertension in compliance with BP was higher in the young population. Previous literature suggests that the risk of hypertension was higher in younger individuals than older.26
Among the reported Indian studies, a nationally representative study was conducted, including a large population of 1.3 million adults that determined the region-wise prevalence of hypertension and diabetes. The key findings revealed that the prevalence of hypertension and diabetes mellitus varied depending on location, wealth, age and knowledge.8 It showed that hypertension was common in the younger age group of ≥18–≤25 years (12.1%; 95%CI: 11.8–12.5%) that is concomitant with this study.
This study acknowledges several limitations. Some participants had incomplete clinical information in the available clinical health records. Specifically, this study did not record nutritional, socioeconomic and educational status of the patients that would have been beneficial in concluding the observations. Moreover, information related to geographic region, treatment approach, and ethnicity were not collected. Therefore, these observations cannot be generalized to overall Indian population.
Conclusion
Overall observations demonstrated that hypertension was common in the age group of >35–45 years and significantly associated with diabetes mellitus and dyslipidemia. The major responsible factors of hypertension were family history, sedentary lifestyle, smoking, alcohol consumption, and BMI. Early diagnosis and intervention are the key steps to limit the risk of CVD in the young population.
Acknowledgment
We acknowledge Ms Farida Hussain, Ms Monal Patil, Mr Sagar Patil, and Mr Aji Verghese, from USV Pvt. Ltd for their assistance in carrying out the project. The medical writing support was provided by Dr Pradip Mate from the scientific services team of USV Pvt Ltd and Dr Sapna Patil (Sqarona Medical Communications, Mumbai). We acknowledge BioQuest Solutions Pvt. Ltd for their services in the conduction of the real-world study. The content published herein represents the views and opinions of the various contributing authors and does not necessarily represent the views or opinions of USV and/or its affiliates. The details published herein are intended for informational, educational, academic, and/or research purposes and are not intended to substitute for professional medical advice, diagnosis, or treatment.
Authors also acknowledge following investigators: Dr A Chandra Sekhar, Dr A J Asirvatham, Dr A Sethuraman, Dr A Shahul Hameed, Dr A Syed Sultan Ibrahim, Dr Abhay Kumar Srivastava, Dr Abhijit Ashok Jadhav, Dr Aghosh Pasricha, Dr Ajay Gupta, Dr Alok Agrawal, Dr Ambairam Viswanathan, Dr Amio Sarma, Dr Amrit Nanaiah M M, Dr Anil Adya, Dr Anoop Kumar Srivastava, Dr Arun Bajaj, Dr Arun Kumar Mishra, Dr Arundhati Dasgupta, Dr Arvind Kumar Agarwal, Dr Arvind Kumar Mishra, Dr Ashok Kumar, Dr Ashutosh Saxena, Dr Atul Chandra Saikia, Dr Atul Khanna, Dr Atul Saxena, Dr Atul Srivastava, Dr Avadhut Warake, Dr B Bosco, Dr B R K Reddy, Dr Bala Raju Gundam, Dr Bandaru Shiva Subrahmanyam, Dr Bashir Ahmad Naikoo, Dr Bikash Bhattacharjee, Dr Bongu Karthik Rao, Dr C Somanathan, Dr Chandan Bansal, Dr Chetan B Patil, Dr D Rajitha, Dr Dayal Sadhwani, Dr Devi Ram, Dr Dimple Patel, Dr Durga Kumar Srivastava, Dr E Arunachalam, Dr Easwaran Thangavelu, Dr G S Mahishale, Dr G Satyanarayana Raju, Dr G Shanmugasundar, Dr Gautam Bhandari, Dr Gopal Agarwal, Dr Govind Agrawal, Dr Gurdeep singh kohli, Dr Harish Chandra Mishra, Dr I Periyandavar, Dr Idris Ahmed Khan, Dr J Thiyagarajan, Dr Jawahar Agrawal, Dr Jitendra G Nagar, Dr Joe George, Dr K Balakrishnan, Dr K C Jindal, Dr K Satyanarayana Reddy, Dr K Sudhakar, Dr K V Mallikarjuna Rao, Dr Kamal Kumar, D. Kampa Sarat Chandra Babu, Dr Karra Hanumantha Reddy, Dr Krishnanunni, Dr Kumar Surendra, Dr Kummaraganti Sitarama Swamy, Dr Latif A A, Dr L Sreenivasa Murthy, Dr M Ajay Reddy, Dr M Leelavathi, Dr M Malleswara Rao, Dr M Paul Sudhakar, Dr M Shunmugavelu, Dr M Syed Sulaiman, Dr M Venkata Ramana, Dr Mahendra Patel, Dr Mahendra Singh, Dr Mallikarjuna Rao, Dr Malvika Zantye, Dr Manish Bansal, Dr Manoj Sharma, Dr Mihir P Tanna, Dr Mohammed Idrees, Dr Mohammed Parvez Syed, Dr Mohammed Wasif Azam, Dr Mohan Lal Jain, Dr Mohd Jameel, Dr N Muthukumarasamy, Dr N Sudha, Dr Nasimullah Attaullah Mohammed, Dr Nagaraj S, Dr Nagendra Reddy Jakka, Dr Nanda Kumar L G, Dr Narender Katakam, Dr Narender Katakam, Dr Narendra Prasad Mishra, Dr Nekkanti Narendra Prasad, Dr Nilakshi Deka, Dr Nitin B Agarwal, Dr Nitin Kesarkar, Dr Om Prakash Prasad, Dr P Chakradhar, Dr P Jegan, Dr P Kamalakkannan, Dr P L Saravanan, Dr P Mithun Chakravarthy, Dr P Murali Madhav, Dr P Muthukumar, Dr P Ranga Prasad, Dr P Ravi Kaladhar Reddy, Dr P S Iyengar, Dr P Sreenatha Reddy, Dr P V Ram Prasad, Dr P Vishnuram, Dr Paresh Shah, Dr Parikshit Goswami, Dr Pawan Kumar Goyal, Dr Ponnian John Christopher, Dr Pradeep Kawatra, Dr Pradeep Sehgal, Dr Pradip Gupta, Dr Pranab Jyoti Bhattacharyya, Dr Praveena Kumar, Dr Preamkumar Asokumar, Dr R Anil Kumar, Dr R Arul Prakash, Dr R Niresh Kannan, Dr R Prabakar, Dr R Rajapaul, Dr R Rajarathinam, Dr R Ravi Chandra Reddy, Dr R Saravanan, Dr. R Shashi Kumar, Dr R Thirumurugan, Dr Rajeev Kapoor, Dr Rajendra Kumar Khinvasara, Dr Rajesh Agarwal, Dr Rajesh Bhagchandani, Dr Rajesh Kappala, Dr Rajesh Kumar Agrawal, Dr Rajesh Kumar Marya, Dr Raju A Gopal, Dr Regonda Rajesh, Dr S Azhagam Perumal, Dr S N Ganesha Moorthy, Dr S Palanivelrajan, Dr S Pothiraju, Dr S Rajendra Prasad, Dr S Satya Murthy, Dr S Subashini, Dr Sabeer T K, Dr Sabesan Swaminathan, Dr Sandeep Sudhakaran, Dr Sanjai Mishra, Dr Sanjay More, Dr Sanjeev Gulati, Dr Satish B Kinagi, Dr Saumen Chaudhuri, Dr Shamsudeen M, Dr Shankar Jyoti Parashar, Dr Shardul Kothary, Dr Shashidhara D, Dr Shivanand B Boodihal, Dr Siddappa A Kama, Dr Stanley Ambroise, Dr Subhash Chandra Mandal, Dr Sudhanshu Shanker, Dr Sunil Kumar, Dr Sunil R Karande, Dr Sushil Gattani, Dr Sushil Kumar, Dr T Suman, Dr Tirthankar, Dr U B Padmanaban, Dr Udaya Bhanu K S, Dr Uttam Kumar Nath, Dr V Chitti Babu, Dr V G Subramaniyan, Dr V Manakavala Perumal, Dr V N Selvam, Dr Vijay Shanker Upadhyaya, Dr Vijith Kumar K, Dr Vimlesh Patidar, Dr Vinay M Dipali, Dr Vineet Bansal, Dr Vipin Porwal, Dr Virendrasinh C Chauhan, Dr Vivek Sundaram, Dr Vrind Kumar Bhardwaj, Dr Y V S Prabhakar.
Funding Statement
The study was sponsored by USV Pvt. Ltd, Mumbai.
Abbreviations
ACC/AHA, American College of Cardiology and American Heart Association; BMI, body mass index; CSI, cardiological society of India; CVD, cardiovascular disease; ESC/ESH, European Society of Cardiology/European Society of Hypertension; ICH-GCP, International Conference on Harmonization-Good Clinical Practice.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authorship
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
Dr Mahesh Abhyankar and Dr Santosh Revankar are employees of USV Pvt. Ltd. Mahesh V Abhyankar reports personal fees from USV Pvt. Ltd, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Undhad AM, Bharodiya PJ, Sonani RP. Correlates of hypertension among the bank employees of Surat city of Gujarat. Natl J Community Med. 2011;2(1):112–123. [Google Scholar]
- 2.World Health Organization, World Health Statistics: a snapshot of global health; 2012. Available from: https://apps.who.int/iris/bitstream/handle/10665/70889/WHO_IER_HSI_12.1_eng.pdf;jsessionid=E6DA0889672AC7C3E66F4D83A0E57D83?sequence=1. Accessed March02, 2020.
- 3.World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva, Switzerland: World Health Organization; 2013. Available from: https://www.who.int/nmh/events/ncd_action_plan/en/Accessed. Accessed March02, 2020. [Google Scholar]
- 4.Bhise MD, Patra S. Prevalence and correlates of hypertension in Maharashtra, India: a multilevel analysis. PLoS One. 2018;13(2):e0191948. doi: 10.1371/journal.pone.0191948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. [DOI] [PubMed] [Google Scholar]
- 6.What is new in Indian guidelines on hypertension - IV. JAPI. 2019;67(Special Issue):12. Available from: https://japi.org/q2d4e454/what-is-new-in-indian-guidelines-on-hypertension-iv. [Google Scholar]
- 7.Sessions with ESC faculty held on 23 and 24 November at 70th annual conference of the Cardiological Society of India (CSI). Available from: https://www.escardio.org/The-ESC/Press-Office/Press-releases/One-in-five-young-adults-in-India-has-high-blood-pressure. Accessed March02, 2020.
- 8.Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and hypertension in India: a nationally representative study of 1.3 million adults. JAMA Intern Med. 2018;178(3):363–372. doi: 10.1001/jamainternmed.2017.8094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramakrishnan S, Zachariah G, Gupta K, et al. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2019;71(4):309–313. doi: 10.1016/j.ihj.2019.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nam KD, Van NB, Hoang LV, et al. Hypertension in a mountainous province of Vietnam: prevalence and risk factors. Heliyon. 2020;6(2):e03383. doi: 10.1016/j.heliyon.2020.e03383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mulyanto J, Kringos DS, Kunst AE. Socioeconomic inequalities in the utilization of hypertension and type 2 diabetes management services in Indonesia. Trop Med Int Health. 2019;24(11):1301–1310. doi: 10.1111/tmi.13303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chalmers J, Woodward M, Borghi C, et al. Strategies to meet the need for long-term data. J Hypertens. 2016;34(8):1473–1479. doi: 10.1097/HJH.0000000000000987 [DOI] [PubMed] [Google Scholar]
- 13.Merlo J, Asplund K, Lynch J, et al. Population effects on individual systolic blood pressure: a multilevel analysis of the World Health Organization MONICA Project. Am J Epidemiol. 2004;159(12):1168–1179. doi: 10.1093/aje/kwh160 [DOI] [PubMed] [Google Scholar]
- 14.Anchala R, Kannuri NK, Pant H, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–1177. doi: 10.1097/HJH.0000000000000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1 [DOI] [PubMed] [Google Scholar]
- 16.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 17.Rao CR, Kamath VG, Shetty A, Kamath A. High blood pressure prevalence and significant correlates: a quantitative analysis from coastal Karnataka, India. ISRN Prev Med. 2012;2013:574973. doi: 10.5402/2013/574973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prasad M, Flowers E, Mathur A, et al. Effectiveness of a community screening program for metabolic syndrome and cardiovascular risk factor identification in young South Asians adults. Diabetes Metab Syndr. 2015;9(1):38–41. doi: 10.1016/j.dsx.2014.04.025 [DOI] [PubMed] [Google Scholar]
- 19.Joshi SR, Saboo B, Vadivale M, et al. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India–results from the Screening India’s Twin Epidemic (SITE) study. Diabetes Technol Ther. 2012;14(1):8–15. doi: 10.1089/dia.2011.0243 [DOI] [PubMed] [Google Scholar]
- 20.Ranasinghe P, Cooray DN, Jayawardena R, Katulanda P. The influence of family history of hypertension on disease prevalence and associated metabolic risk factors among Sri Lankan adults. BMC Public Health. 2015;15:576. doi: 10.1186/s12889-015-1927-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corvol P, Jeunemaitre X, Charru A, Soubrier F. Can the genetic factors influence the treatment of systemic hypertension? The case of the renin-angiotensin-aldosterone system. Am J Cardiol. 1992;70(12):14D–20D. doi: 10.1016/0002-9149(92)90267-3 [DOI] [PubMed] [Google Scholar]
- 22.Stamler R, Stamler J, Riedlinger WF, et al. Family (parental) history and prevalence of hypertension. Results of a nationwide screening program. JAMA. 1979;241(1):43–46. doi: 10.1001/jama.1979.03290270033016 [DOI] [PubMed] [Google Scholar]
- 23.Feng RN, Zhao C, Wang C, et al. BMI is strongly associated with hypertension, and waist circumference is strongly associated with type 2 diabetes and dyslipidemia, in northern Chinese adults. J Epidemiol. 2012;22(4):317–323. doi: 10.2188/jea.JE20110120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pirasath S, Kumanan T, Guruparan M. A study on knowledge, awareness, and medication adherence in patients with hypertension from a tertiary care centre from Northern Sri Lanka. Int J Hypertens. 2017;2017:9656450. doi: 10.1155/2017/9656450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prenissl J, Manne-Goehler J, Jaacks LM, et al. Hypertension screening, awareness, treatment, and control in India: a nationally representative cross-sectional study among individuals aged 15 to 49 years. PLoS Med. 2019;16(5):e1002801. doi: 10.1371/journal.pmed.1002801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanegae H, Oikawa T, Okawara Y, Hoshide S, Kario K. Which blood pressure measurement, systolic or diastolic, better predicts future hypertension in normotensive young adults? J Clin Hypertens. 2017;19(6):603–610. doi: 10.1111/jch.13015 [DOI] [PMC free article] [PubMed] [Google Scholar]