1. Introduction
Higher-quality diets are reported to lead to better health outcomes, but have also been associated with higher per calorie diet costs1–10. In particular, adherence to the Dietary Guidelines for Americans has been associated with higher estimated food expenditures.11–13 Conversely, families with lower incomes are often forced to stretch their food budgets leading to the purchase of more cost effective options, which are often lower in nutrient quality.5,14 The lack of affordable nutrition may be one reason why lower socio-economic groups do not adhere to dietary guidelines 15,16 and have higher rates of obesity, diabetes and other diet-related non-communicable diseases.
Non-compliance with the dietary guidelines, may be explained, at least in part, by the lower cost of energy-dense refined grains, added sugars, and fats.2,16 Such palatable, energy-dense foods have been associated with over-eating in clinical and in laboratory studies.17 Taste, cost, and convenience along with health and variety are among the recognized drivers of food choice.18–22 Socio-demographic variables such as age, gender, race/ethnicity, and education also play a role. 14,23,24
The monetary cost of adhering to the dietary guidelines needs to be explored in detailed analyses of diet quality in relation to food spending. There are several ways to assess per capita food expenditures and individual-level diet costs. Among measures of household food spending are self-reported food expenditures,25–27 sometimes backed with food purchase receipts.11,28,29 Studies have also estimated household food purchases using sales data from supermarkets and grocery stores.30–33
Joining dietary records with retail food prices to estimate diet costs at the individual level has become the preferred technique in nutritional epidemiology.2,3,7,8,10,4 In effect, the monetary price of a food item, expressed per 100g, edible portion, is treated as a nutrient vector.34 The total cost of a given diet is calculated in a manner that is exactly analogous to the calculations of the diet’s content of vitamins or minerals. The method of joining dietary intakes with retail food prices has been used to calculate diet costs in the US13 and in other countries – Malaysia, Japan, Spain, UK, and France.6,31,35–37 The same method is used by the USDA to calculate food assistance benefits.34
Few studies have been able to compare self-reported per capita food expenditures with estimated individual-level diet costs in relation to diet quality across socio-demographic groups in the US. This study compared two measures of food spending (self-reported food expenditures and Food Frequency Questionnaire (FFQ)-estimated diet costs) in relation to Healthy Eating Index 2015 (HEI-2015) scores, a measure of compliance with the US 2015–2020 Dietary Guidelines for Americans (DGA). To our knowledge, this study is the first to examine the shape of the cost-quality curve to specifically determine the point at which a change in diet cost would be associated with the greatest increase in HEI-2015.
2. Methods
2.1. Sampling and recruitment
2.1. Study population
The Seattle Obesity Study (SOS) III was a two-year longitudinal study conducted in King, Pierce, and Yakima counties in WA State. Eligible participants were adults aged 21–59 y, not pregnant or breastfeeding, with no issues impacting mobility, and primary food shoppers of their household. The three counties differed in socio-demographic composition. Median incomes were $71,811 in King, $58,204 in Pierce, and $43,506 in Yakima.38 Percent Hispanic ethnicity was 7.5% in King, 7.2% in Pierce and 37.5% in Yakima.38 Participation in the Supplemental Nutrition Assistance Program (SNAP) was higher in Yakima as compared to King or Pierce.39
Study sites were University of Washington (King), MultiCare Institute for Research and Innovation (Pierce), and the Center for Community Health Promotion——a satellite office of the Fred Hutchinson Cancer Research Center (FHCRC)—(Yakima). Address-based sampling schemes tailored to each site were employed to achieve geographic and socioeconomic representation. To address challenges with traditional randomized telephone-based recruitment methods among hard-to-reach populations, community outreach was also employed at each site.
As with past SOS studies, the King County address-based sampling scheme used 3 residential property values strata ($199K; $200–299K; and $300K+).40 Potential participants were sent pre-notification letters and then contacted by phone to screen for eligibility. Participants were also recruited from lower-income neighborhoods through community outreach to increase representation of low-income groups. The sample size for King County at baseline was 356. The Pierce County sampling scheme was a random ZCTA-based sample of MultiCare Health System members, sampling by census-level incomes (3 categories) and distance to MultiCare (≤5 miles or > 5 miles). Additional participants were recruited through community outreach. The Pierce County sample at baseline was 167. The Yakima County sampling frame included randomly selected individuals who participated in previous FHRC studies.41,42 Pre-notification letters, followed by recruitment phone calls in both English and Spanish, were employed, as well as participants recruited via community outreach. No stratification by property values or income was used for the Yakima sampling frame since most individuals in the sampling frame had lower income. The sample size in Yakima at baseline was 349.
The final baseline sample for SOS III was 872; however, not all sociodemographic and dietary variables were available for all participants. The sample over-represented women but was otherwise broadly consistent with the socio-demographic composition of each county.38,43
Upon determining eligibility and receiving verbal consent to join the study, participants were invited to complete the first in-person visit at local study sites within each county. Written consent was provided in the in-person visit before completing the study protocols. Data collection was conducted in English and Spanish (in Yakima only). Spanish data collection was conducted by trained bilingual and bicultural staff members. Compensation was provided for completion of the first in-person visit. Recruitment and baseline data collection occurred from July 2016 to May 2017. All study protocols received the necessary approvals by the institutional IRBs at the respective sites.
2.2. Health behaviors survey
Self-reported data on socio-demographics, food shopping, and other behaviors were collected via a computer-assisted survey. Survey questions were adapted from the SOS I and II, the Behavioral Risk Factor Surveillance System and the National Health and Nutrition Examination Surveys (NHANES).40,44,45 Socio-demographic variables assessed were age, gender, race/ethnicity, education, marital status, and food assistance use (food banks, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), the Supplemental Nutrition Assistance Program (SNAP)). In SOS III, race and ethnicity were captured using NHANES questions.44 For cultural sensitivity, “Hispanic” was added as a race, based on the site PI’s feedback that Hispanic participants in Yakima self-identified as Hispanic as both a race and ethnicity. Race/ethnicity were grouped into three categories for analyses: non-Hispanic White, Hispanic, and others (i.e. African American, Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or other).
Participants self-reported the name and location of their primary food store, which were categorized by cost using a coding scheme based on the method developed in SOS II.20 In SOS II, market basket prices were collected for 13 food stores reported by participants. Prices were collected in-person or online. Cluster analysis was used to categorize stores into three categories based on store prices; low, medium, and high-cost stores. In SOS III, the same categories were used. Examples of high-cost stores included Puget Consumer Co-op (PCC), QFC, and Whole Foods. Medium-cost stores included Costco, Fred Meyer, Safeway. Examples of low-cost stores included Albertson’s, Grocery Outlet, Walmart, and WinCo foods.
Participants also reported their monthly at-home household food expenditures based on NHANES questions,44 defined as food purchased to be prepared at home, as well as their monthly away from home expenditures, defined as purchases on food that was prepared outside the home (i.e. restaurants, cafeterias, etc.). Monthly at-home and away from home expenditures were summed to create a monthly total food expenditures variable. Total food expenditures were then divided by household size to create monthly total food expenditures per capita.
2.3. Food frequency questionnaire and HEI-2015 scores
Dietary data was collected using the Fred Hutchinson Cancer Research Center (FHCRC) FFQ, a validated data collection tool for dietary intake assessment, available to participants in both English and Spanish. 46 On the FFQ, participants reported their average consumption of >100 foods during the past year.
FFQ data were used to calculate HEI-2015 scores, a diet quality measure of compliance with the 2015 DGA.46–48 The HEI score is a 100-point scale, based on intakes of food groups to encourage: fruits (10 points), vegetables (10), grains (10), dairy (10), proteins (10), and fats (10) and foods to limit: refined grains (10), sodium (10), added sugars (10) and saturated fats (10). The USDA suggests interpreting the HEI scores on a graded scale, where a score of 100 represents the highest quality diet, a score of 99–90 represents an “A,” 80–89 a “B”, etc.47 According to 2013–14 NHANES data, Adult Americans averaged an HEI score of 59, which would receive an F on the graded scale, representing diets with room for improvement.49 Component food items from the FFQ were linked to food items from the MyPyramid Equivalents Database (MPED) in order to estimate the food group equivalents for each line item on the FFQ.50 These food group equivalents along with a few items outputted by Nutrition Data System for Research software (developed by the University of Minnesota)51 were used to calculate HEI-2015 and its components.
2.4. Method to estimate monthly diet costs
Market basket data were collected in-person and compared to web prices in Safeway stores in the three counties (King, Pierce, Yakima) using standard data collection protocols.30 The lowest price for each component food in the FHCRC FFQ was collected in the three counties. Diet costs for each participant were calculated using the county-specific market basket prices, which were adjusted for food waste using the standard USDA reference to compute costs per 100 g edible portion.52 The costs for each food reported were summed for each individual to create the total daily cost of their diet, with the exception of non-caloric beverages (i.e. water, unsweetened tea, unsweetened coffee). This total diet cost per day was then divided by calories and multiplied by 2,000 to create estimated daily diet cost per 2,000 kcal, as a way to denote the money spent on food if consuming 2,000 kcal per day, the FDA’s reference value for daily caloric intake.53 Daily diet cost was then multiplied by 30 to create the monthly diet cost variable.
2.4. Residential property values
The residential property value metric at the tax parcel level was developed using King, Pierce, and Yakima County 2016 tax assessor records, as has been used in previous.40,54,55 If a parcel had multiple units, the mean value per unit was applied. Thus, property values were split into tertiles to be used for as a proxy for income (tertile 1: <129,401, tertile 2: 129,700–293,500, tertile 3: 295,000 −1,492,000). In past studies, residential property values were highly correlated with income and wealth.56
2.5. Statistical analyses
Only baseline data were used. The following outliers greater than 3 SD above the mean were removed: n=14 for total food expenditures and n=5 for estimated diet cost derived from the FFQ. Similarly, implausible values for FFQ intake data were removed (n=11 for greater than 5000 kcal/day and n=3 for less than 500kcal/day). After excluding participants with missing data for socio-demographics (n=40) or property values (n=31), the analytical sample was 768.
First, we characterized the socio-demographic distribution along with primary food store category of the study population. Mean and SD’s of self-reported monthly total food expenditures per capita (food expenditures) and estimated monthly diet cost per 2,000 kcal (diet cost) were compared across each socio-demographic variable. Univariate linear regressions were conducted to test for unadjusted differences in mean food expenditures and diet costs across population subgroups.
Next, the relations between food expenditures, diet costs, and the HEI-2015 diet quality score were tested using a series of linear regressions. Food expenditures and diet cost were divided by 100 to standardize the regression models to estimate the mean HEI per $100 increase in monthly spending. Univariate regressions testing the unadjusted associations were followed by separate multiple linear regression models, controlling for age (21-<40y, 40–50y, >50y), gender, education (< High school or less, Some college or technical school, College graduate or more), race/ethnicity (non-Hispanic White, Hispanic, other), marital status (married, unmarried), use of food assistance (food banks, WIC, and/or SNAP vs. no food assistance use), property value tertiles, and county (King, Pierce, Yakima). Multiple curvilinear regression models were conducted to test the significance of the quadratic relationship of food expenditures and diet costs with HEI-2015, controlling for the same set of covariates. Scatterplots with quadratic regression lines were created to visualize the curvilinear relationship between the two measures of food spending and HEI-2015.
All regression models were conducted with robust standard errors through Generalized Linear Estimating Equations (GEE) to address non-normality distributions of the outcome (HEI). All data analyses were conducted in SAS 9.4 (SAS institute, Cary, NC).
3. Results
3.1. Study sample demographics
Table 1 summarizes the socio-demographic distribution for the SOS III sample. The majority of the sample were female (81.8%), and had a college degree or more (44.7%) but with 33.3% of the sample who had a high school education or less. The sample racial/ethnic composition was 49.2% non-Hispanic White, 39.9% Hispanic, and 10.9% other. Food assistance use (food banks, WIC, and/or SNAP) was reported by 33.7%. Most participants shopped at medium price stores (45.1%) followed by low price stores (36.4%) and high price stores (18.5%).
Table 1.
Participant characteristics for total SOS III sample
| N | % | |
|---|---|---|
| OVERALL | 768 | 100 |
| Gender | ||
| Male | 140 | 18.2 |
| Female | 628 | 81.8 |
| Age | ||
| 21-<40y | 257 | 33.4 |
| 40–50y | 223 | 29.1 |
| >50y | 288 | 37.5 |
| Race and Ethnicity | ||
| Non-Hispanic White | 378 | 49.2 |
| Hispanic | 306 | 39.9 |
| Other | 84 | 10.9 |
| Marital Status | ||
| Married | 448 | 58.3 |
| Unmarried | 320 | 41.7 |
| Education | ||
| High school or less | 255 | 33.3 |
| Some college or technical school | 169 | 22.0 |
| College graduate or more | 344 | 44.7 |
| Property values (tertiles) | ||
| Tertile 1: <129k | 255 | 33.3 |
| Tertile 2: 130–294k | 256 | 33.2 |
| Tertile 3: 295–1,492k | 257 | 33.5 |
| Food Assistance (Food bank, WIC, SNAP) | ||
| Yes | 258 | 33.6 |
| No | 510 | 66.4 |
| Food store type | ||
| Low cost | 280 | 36.4 |
| Medium cost | 346 | 45.1 |
| High cost | 142 | 18.5 |
Notes: Hispanic includes those who reported Hispanic as ethnicity and race
SNAP: Supplemental Nutrition Assistance Program, WIC: Special
Supplemental Nutrition Program for Women, Infants, and Children
Table 2 shows the means (in $/month) for per capita self-reported food expenditures and FFQ-derived individual diet cost for the whole sample and by socio-demographic subgroup. Mean monthly per capita food expenditures were $225.39($132.46); mean monthly diet cost per 2000 kcal was $284.67($59.82).
Table 2.
Distribution of socio-demographics and mean values for food expenditures and diet cost
| Food expenditures per capita (USD/month) | Diet cost per 2,000 kcal (USD/2,000 kcal/month) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | p-value | Mean | SD | p-value | |
| OVERALL (N=768) | 225.39 | 132.46 | 284.67 | 59.82 | ||
| Gender | ||||||
| Male | 268.08 | 145.32 | ref | 282.70 | 55.05 | ref |
| Female | 215.88 | 127.61 | <0.0001 | 285.11 | 60.86 | 0.65 |
| Age | ||||||
| 21-<40y | 188.30 | 107.11 | ref | 273.81 | 52.40 | ref |
| 40–50y | 212.89 | 122.45 | 0.02 | 281.17 | 58.56 | 0.15 |
| >50y | 268.18 | 147.87 | <0.0001 | 297.07 | 64.73 | <0.0001 |
| Race and Ethnicity | ||||||
| Non-Hispanic White | 279.28 | 142.42 | ref | 302.18 | 59.10 | ref |
| Hispanic | 155.19 | 76.37 | <0.0001 | 260.57 | 51.65 | <0.0001 |
| Other | 238.65 | 130.38 | 0.01 | 293.67 | 61.45 | 0.25 |
| Marital Status | ||||||
| Married | 213.21 | 122.64 | 0.004 | 287.12 | 59.53 | 0.16 |
| Unmarried | 242.45 | 143.56 | ref | 281.24 | 60.15 | ref |
| Education | ||||||
| High school or less | 149.31 | 76.04 | <0.0001 | 257.55 | 46.91 | <0.0001 |
| Some college or technical school | 227.40 | 127.56 | <0.0001 | 286.84 | 60.83 | 0.003 |
| College graduate or more | 280.81 | 139.99 | ref | 303.71 | 60.39 | ref |
| Property values (tertiles) | ||||||
| Tertile 1: <129k | 153.07 | 79.70 | <0.0001 | 257.89 | 46.12 | <0.0001 |
| Tertile 2: 130–294k | 237.04 | 139.32 | <0.0001 | 287.53 | 57.99 | <0.0001 |
| Tertile 3: 295–1,492k | 285.87 | 133.95 | ref | 308.51 | 63.10 | ref |
| Food Assistance (Food bank, WIC, or SNAP) | ||||||
| Yes | 142.98 | 68.51 | ref | 256.54 | 45.87 | ref |
| No | 267.09 | 137.42 | <0.0001 | 298.90 | 61.04 | <0.0001 |
| Food store type | ||||||
| Low cost | 169.86 | 97.20 | ref | 264.12 | 54.41 | ref |
| Medium cost | 227.35 | 128.28 | <0.0001 | 288.65 | 56.36 | <0.0001 |
| High cost | 330.12 | 138.93 | <0.0001 | 315.51 | 63.23 | <0.0001 |
Notes: Hispanic includes those who reported Hispanic as ethnicity and race; SNAP: Supplemental Nutrition Assistance Program, WIC: Special Supplemental Nutrition Program for Women, Infants, and Children; food expenditures per capita equal the sum of self-reported at-home and away from home food expenditures divided by household size; diet cost was estimated from FFQ intake data, divided by calories, multiplied by 30 to create a monthly diet cost variable, and adjusted to $/2,000kcal; unadjusted p-values
Both food expenditures and diet costs showed significant univariate differences by all socio-demographic variables. Food expenditures were positively associated with age, education, and property values. Non-Hispanic Whites had higher mean food expenditures (mean (SD): $279.28($142.42)) as compared to Hispanic/others (mean (SD): $155.19($76.37)). Groups using food assistance had lower mean total food expenditures (mean (SD): $142.98($68.51)) than those not using food assistance (mean (SD): $267.09($137.42)). Shopping at a medium or high cost store was positively associated with food expenditures, where those shopping at high cost stores reported almost double the food expenditures as those shopping at low cost stores ($330.12 ($138.93) vs. $169.86 ($97.20) respectively).
Diet costs were also positively associated with age, education, and property values. Non-Hispanic Whites had higher diet costs (mean (SD): $302.18 ($59.10)) as compared to Hispanic/others (mean (SD): $260.57($51.65)) Groups using food assistance had lower mean total food expenditures (mean (SD): $256.54($45.87)) than those not using food assistance and (mean (SD): $298.90($61.04)). Shopping at medium or high cost stores was associated with higher diet costs than shopping at low cost stores, where those shopping at high cost stores had diet costs that were about $50 more per month than those shopping at low cost stores ($315.51($63.23) vs. $264.12($54.41) respectively).
Table 3 presents the results of the univariate and fully adjusted multiple linear regression models relating food expenditures and diet costs to HEI-2015 scores. Both food expenditures and diet costs were positively associated with HEI-2015 in the univariate models. After adjustment, only diet cost remained significant. Overall, each $100 increase in diet cost was associated with an increase of 5.33 points in HEI-2015.
Table 3.
Comparing multiple linear regression models with food expenditures and diet cost predicting HEI 2015 (n=768)
| Unadjusted models | Adjusted Models | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean HEI per $100 | (95% CI) | p-value | Mean HEI per $100 | (95% CI) | p-value | |||
| Linear models | ||||||||
| Food expenditures per capita ($/month) | 1.20 | 0.71 | 1.70 | <0.0001 | 0.09 | −0.49 | 0.67 | 0.77 |
| Diet cost per 2,000 kcal ($/2,000 kcal/month) | 6.54 | 5.51 | 7.56 | <0.0001 | 5.33 | 4.15 | 6.50 | <0.0001 |
| Curvilinear models | ||||||||
| Diet cost per 2,000kcal ($/2,000kcal/month) | 19.98 | 11.83 | 28.14 | <0.0001 | 17.82 | 9.76 | 25.88 | <0.0001 |
| Diet cost per 2,000 kcal ($/2,000kcal/month) squared | −2.23 | −3.54 | −0.91 | 0.0009 | −2.06 | −3.35 | −0.78 | <0.002 |
Notes: food expenditures per capita equal the sum of self-reported at-home and away from home food expenditures divided by household size; diet cost was estimated from FFQ intake data, divided by calories, multiplied by 30 to create a monthly diet cost variable, and adjusted to $/2,000kcal; both food expenditures and diet cost variables were then divided by $100 to estimate the mean HEI per $100 increase in monthly spending; unadjusted models: two separate unadjusted models were conducted- one with food expenditures per capita as the primary independent variable and another with diet cost as the independent variable; adjusted models: two separate generalized linear regressions with robust standard errors adjusting for age, gender, race/ethnicity, marital status, education, property values, food assistance, and county were conducted - one including food expenditures as the primary independent variable, another with diet cost as the primary independent variable.
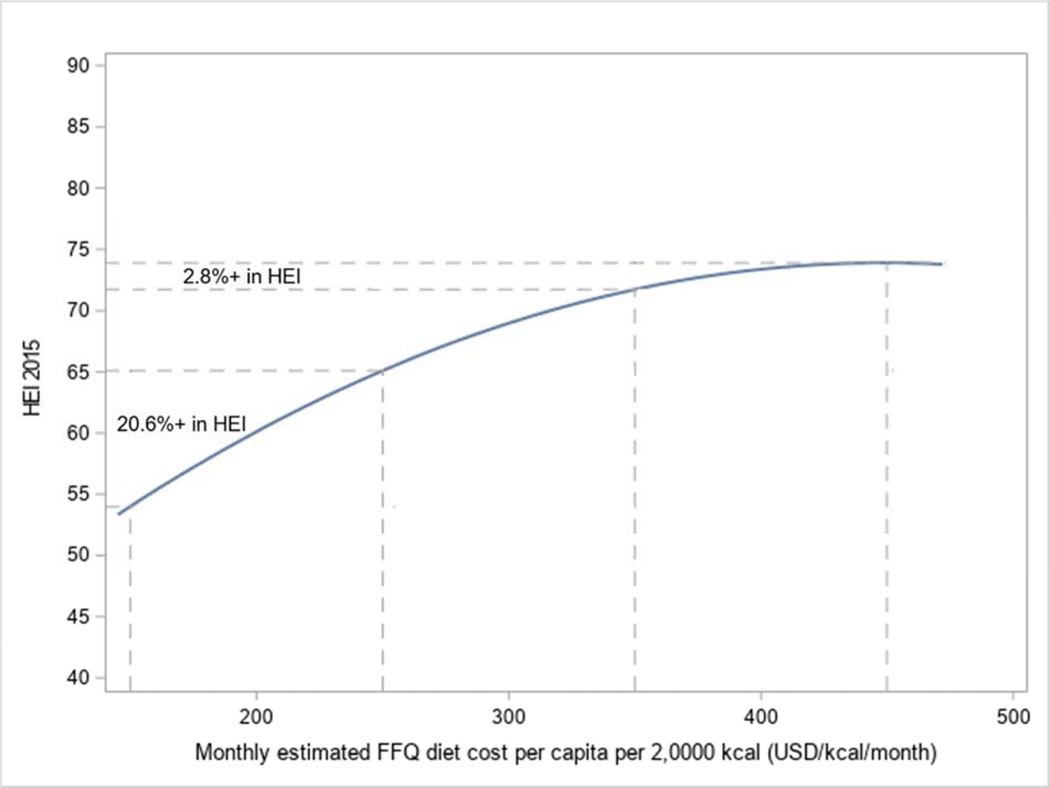
Table 3 also shows the results of a fully adjusted multiple linear regression testing the significance of a quadratic effect of diet cost (diet cost squared) on HEI-2015. There was evidence of a curvilinear relationship between diet cost and HEI-2015 even after controlling for potential covariates. There was no evidence of a curvilinear relationship for total food expenditures and HEI-2015 (data not shown).
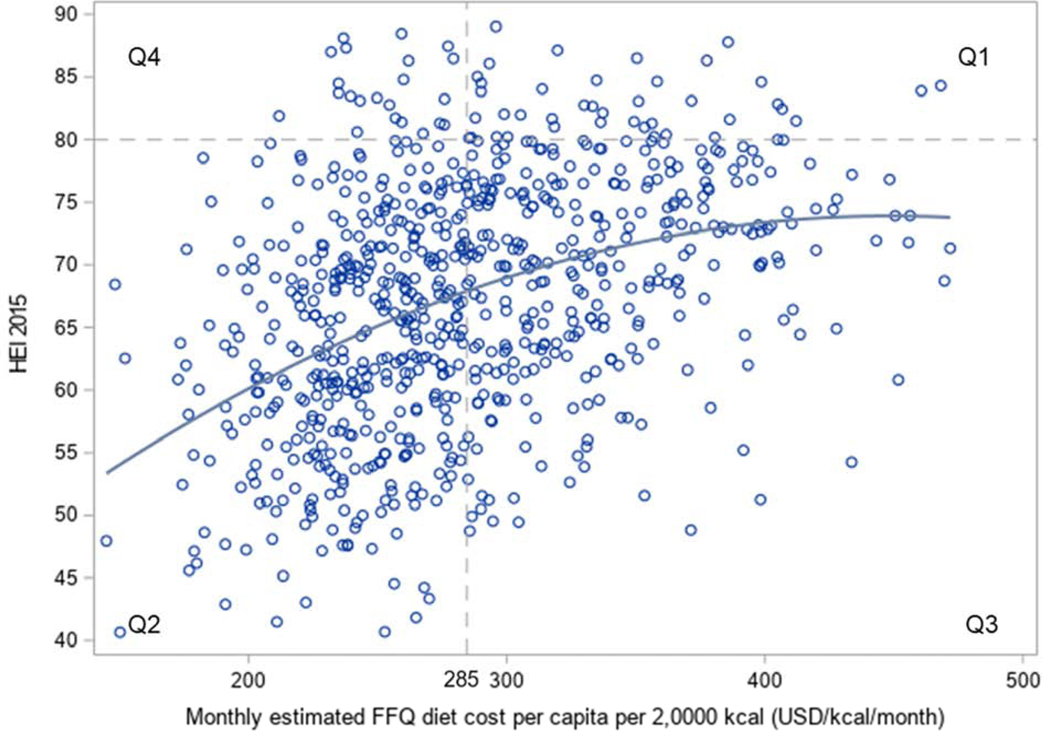
Figure 1 scatterplot depicts the quadratic relation between diet cost and HEI-2015 scores, with an asymptote reached as diet costs reach about $350/month. The greatest increase in HEI scores was obtained within the lower range of diet costs. Using the sample mean of $285 per month and an HEI of 80 (considered a “B” on the HEI scale) as reference points, the graph is split into four quadrants: Q1, Q2, Q3, and Q4. Most of the sample had HEI scores below 80 (Q2 and Q3), however, there was also large individual variation in HEI scores for a given diet cost.
Figure 1:
Scatterplot depicting the quadratic relationship between diet cost (standardized per 2,000 kcal) ($/2,000kcal/month) and HEI-2015 diet quality scores derived from the FFQ (n=768). The graph is split into four quadrants (Q1-Q4) by using the sample mean was $285 per month and an HEI of 80 (considered a “B” on the HEI scale) as reference points.
Figure 2 illustrates the differential gains in HEI-2015 with increasing diet costs. An increase in diet cost from $150 per day to $250 per day was associated with a 20.6% increase in HEI-2015 (54.00 to 65.10), but the same increment increase of diet cost from $350 to $450 was associated with only a 2.8% increase in HEI-2015 (72.00 to 74.00).
Figure 2:
Trend line for the quadratic relationship between estimated monthly diet cost (standardized per 2,000 kcal) and HEI-2015 diet quality scores derived from the FFQ, (n=768) depicting the maximal returns of diet cost for diet quality below ~$350/day. Shifts from $150 to $250 in estimated monthly diet cost were compared to shifts from $350 to $450 in estimated monthly diet cost.).
4. Discussion
The present results showed that while healthier diets and higher HEI-2015 scores were associated with greater food spending, there was much variability at the individual level. At any level of spending, a wide range of HEI-2015 diet quality scores was observed, just as compliance with the DGA could be achieved with a highly variable diet cost.
For example, lower food expenditures and FFQ-estimated diet costs. Both variables were associated with socioeconomic status (SES), consistent with prior research. Lower food expenditures and lower diet costs were associated with being younger, unmarried, having less than a high school education, using food assistance5,14,23,24 and having lower property values. Also in line with previous research, higher food expenditures and diet costs were associated with shopping at high cost stores, just as lower food expenditures and diet costs were associated with shopping at low cost stores.20
For the SOS III sample as a whole, the present results showed a strong positive association between compliance with DGA and estimated diet cost. These observations are consistent with past analyses of the nationally representative NHANES sample, based on 24-hour dietary recalls joined with the national USDA food prices database, which showed that higher estimated diet costs were linked to higher HEI-2010 scores.13 Similarly, a meta-analysis of 27 studies from 10 countries found that compliance with the highly recommended Mediterranean diet pattern was associated with an average increase in diet cost of about $1.50 per day or about $45 per person per month as compared to a less healthy diet pattern consisting of processed foods and refined grains.3
For the most part, past studies have examined a linear relationship between diet cost and diet quality.2–10,16 The present results show that the relation between dietary compliance and cost may include a quadratic term, which would indicate the potential for maximal returns in diet quality at the lower end of the food spending spectrum. To our knowledge, only one study has explored this issue in a youth population and using a different diet quality metric.6 The present analyses showing a curvilinear relation between diet cost and HEI−2015 scores are the first to demonstrate that increases in diet cost ($100/month) for lower cost diets can assist compliance with the DGA. For diet costs above ~$350 per month, there were diminishing returns.
The present results parallel research in health economics and the “absolute income hypothesis,” which states that income and health are positively associated but at a decreasing curvilinear rate.57,58 In other words, the hypothesis suggests that there are maximal returns for health with increasing income at the lower end of the income spectrum, whereas at higher income levels the benefits begin to plateau. This has been examined in the context of mortality risk 57,58 and happiness.59 Our results suggest that compliance with the DGA follows the same rules. Increasing monthly food spending may be prohibitive to those at the lower end food spending, as lower diet costs and expenditures were associated with lower education, lower residential property values, and shopping at lower cost stores. To increase the affordability of healthy diets that are compliant with the DGA, the cost of nutrient-dense foods must come down. Future research on the implementation of dietary advice could benefit from exploring further ways to improve diet quality among lower SES groups.
The present finding that the overall relation between diet cost and adherence to the DGA does not hold for every individual participant has implications for personalized nutrition. Considering the positive association between diet cost and HEI, one might expect most participants to fall in Q1 and Q2. However, as the scatterplot shows, there was great individual variation in the relation between diet cost and diet quality, with some participants showing high diet costs and low diet quality (Q3) and several with low diet costs and higher diet quality (Q4). The Q4 quadrant participants had been identified as showing nutrition resilience— described in past studies as being able to eat better for less. Previous work examining this idea of nutrition resilience has found that participants with high diet quality but low diet cost had lower BMI’s, cooked more at home, and had diets characterized by more whole grains, dairy, total protein, seafood/plant protein and less saturated fat, sodium, and empty calories but did not differ by demographics or income.60 These results suggest that there are groups who are able to achieve healthier diets despite having fewer resources. More work is needed to understand the underlying mechanisms that enable these nutrition resilient individuals to consume high quality diets despite economic constraints. Such work could inform targeted intervention designs.
The present results documenting lower food spending by recipients of food assistance were not surprising, given that food assistance is likely associated with lower diet costs for two reasons: 1) governmental food assistance programs have strict household income qualifications and 2) using food assistance allows families to re-budget food costs for other basic needs such as housing or healthcare. The $100 increases in diet cost as depicted in Figure 2 correspond to shifts between the four food plans created by the USDA to represent “healthy” diets at differing costs. These include the Thrifty plan, Low-cost plan, Moderate-cost plan, and Liberal plan. An increase from $150 to $250 is comparable to an increase from the Thrifty plan to the Low-cost plan, which according to current results, corresponded to a 20.6% increase in HEI (Figure 2). Whereas an increase from $350 to $450 was more comparable to an increase from the Moderate-cost plan to the Liberal plan, which corresponded to a much smaller increase in HEI (2.8%). These results make a case that increasing SNAP benefits may go a long way in improving adherence to the DGA, as the Thrifty plan is used as the basis for SNAP allotments.
4.1. Study limitations and strengths
The limitations of the current study should be considered. The estimated household food expenditures were based on standard questions from NHANES.44 However, these types of self-reported questions on food expenditures can be subject to misreporting and rounding errors. For present purposes, the household food expenditures were divided by number of people per household, which may not be the most accurate way of capturing individual-level food expenditures. In addition to food expenditures, food shopping behaviors were also collected via self-report, which subject to social desirability and recall biases.61,62 The FFQ used to collect the dietary data is a standard, validated tool that has been employed in several large-scale studies.46 However, it is a self-report measure, used to estimated diet cost. Linking dietary intakes with retail prices has now become standard procedure. The county-specific pricing of the FFQ component foods was based on the lowest price for each item, with the same price being assigned to all participants. This technique measures the intrinsic monetary cost of the diet rather than actual food expenditures. The SOS III focused on studying food purchases made in retail outlets (i.e. supermarkets, bulk stores, convenience stores) without including questions about alternative food sources (e.g. community gardens), an area for future research. The SOS III study purposely oversampled low-income and minority populations as well as women (primary food shoppers), so the results may not be generalizable to other populations. Finally, the current findings were based on cross-sectional data, thus causality cannot be inferred.
The study had some notable strengths. First, the population sample was geographically and ethnically diverse, with a wide range of education and incomes. Our measure of residential property values minimized loss of data, often due to missing incomes. To our knowledge, this was the first study to compare self-reported food expenditures to FFQ-estimated diet costs. Both measures captured SES variation, suggesting that food expenditures can be useful in the evaluation of a population’s food purchasing patterns. Diet costs were less subject to direct misreporting and bias though they do depend on the underlying quality of FFQ data. Importantly, this is the first study to explore a nonlinear relationship between diet cost and HEI-2015. Finally, multiple linear regressions using GEE allows for robust standard errors were run, which is a more rigorous method than traditional linear regression models.
4. 2. Conclusions
There was a positive and curvilinear relation between HEI-2015 scores, a measure of compliance with the DGA, and two measures of food spending—self-reported food expenditures and estimated diet cost. First, lower food spending was associated with younger age and lower SES. Second, increases in diet cost of $100/month in the lower diet cost range were associated with greater HEI-2015 gains; such increases in the higher range had diminishing returns. Present analyses show how compliance with the DGA may be promoted by targeted economic interventions to make healthy foods more affordable to lower SES groups.63
Highlights.
Food expenditures and diet costs were linked to socioeconomics in the same way
Costs and expenditures were lower when shopping at low cost vs. high cost stores
Diet cost was positively associated with diet quality in a curvilinear manner
Small diet cost increases had maximal returns for HEI-2015 for lower end diet costs
Acknowledgements:
This work was supported by the National Institute of Health [grant R01 DK076608]. The funding source had no involvement in any part of the preparation of this manuscript.
Declaration of Interest: AD has received grants, honoraria, and consulting fees from numerous food, beverage, and ingredient companies and from other commercial and nonprofit entities with an interest in diet quality and nutrient density of foods. The University of Washington receives research funding from public and private sectors.
Footnotes
Data statement: The data generated as part of this study are not publicly available as the study is ongoing.
None of other authors have any conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Schwingshackl L, Bogensberger B, Hoffmann G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet. 2018;118(1):74–100.e11. doi: 10.1016/j.jand.2017.08.024 [DOI] [PubMed] [Google Scholar]
- 2.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–660. doi: 10.1093/nutrit/nuv027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rao M, Afshin A, Singh G, Mozaffarian D. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ. 2013;3(12):e004277. doi: 10.1136/bmjopen-2013-004277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackenbach JD, Dijkstra SC, Beulens JWJ, et al. Socioeconomic and ethnic differences in the relation between dietary costs and dietary quality: the HELIUS study. Nutr J. 2019;18(1):21. doi: 10.1186/s12937-019-0445-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pechey R, Monsivais P. Socioeconomic inequalities in the healthiness of food choices: Exploring the contributions of food expenditures. Prev Med (Baltim). 2016;88:203–209. doi: 10.1016/j.ypmed.2016.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schröder H, Gomez SF, Ribas-Barba L, et al. Monetary diet cost, diet quality, and parental socioeconomic status in Spanish Youth. PLoS One. 2016;11(9):1–13. doi: 10.1371/journal.pone.0161422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang X, Gong Y, Jia P, et al. Monetary diet cost is positively associated with diet quality and obesity: an analysis of school-aged children in Southwest China. J Public Health (Bangkok). 2019;41(2):250–258. doi: 10.1093/pubmed/fdy100 [DOI] [PubMed] [Google Scholar]
- 8.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82(1 Suppl). doi: 10.1093/ajcn/82.1.265s [DOI] [PubMed] [Google Scholar]
- 9.Drewnowski A, Darmon N, Briend A. Replacing Fats and Sweets With Vegetables and Fruits—A Question of Cost. Am J Public Health. 2004;94(9):1555–1559. doi: 10.2105/AJPH.94.9.1555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrieu E, Darmon N, Drewnowski A. Low-cost diets: More energy, fewer nutrients. Eur J Clin Nutr. 2006;60(3):434–436. doi: 10.1038/sj.ejcn.1602331 [DOI] [PubMed] [Google Scholar]
- 11.Clark RL, Famodu OA, Barr ML, et al. Monetary Cost of the MyPlate Diet in Young Adults: Higher Expenses Associated with Increased Fruit and Vegetable Consumption. J Nutr Metab. 2019;2019. doi: 10.1155/2019/2790963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.USDA. Official USDA Food Plans: Cost of Food at Home at Four Levels, U.S. Average, June 2020. https://fnsprod.azureedge.net/sites/default/files/media/file/CostofFoodJun2020.pdf. Published 2020. Accessed August 17, 2020.
- 13.Rehm CD, Monsivais P, Drewnowski A. Relation between diet cost and healthy eating index 2010 scores among adults in the United States 2007–2010. Prev Med (Baltim). 2015;73:70–75. doi: 10.1016/j.ypmed.2015.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Venn D, Dixon J, Banwell C, Strazdins L. Social determinants of household food expenditure in Australia: The role of education, income, geography and time. Public Health Nutr. 2018;21(5):902–911. doi: 10.1017/S1368980017003342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fulgoni V, Drewnowski A. An Economic Gap Between the Recommended Healthy Food Patterns and Existing Diets of Minority Groups in the US National Health and Nutrition Examination Survey 2013–14. Front Nutr. 2019;6:37. doi: 10.3389/fnut.2019.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107–1117. doi: 10.1093/ajcn/87.5.1107 [DOI] [PubMed] [Google Scholar]
- 17.Hetherington MM. Symposium on “Molecular mechanisms and psychology of food intake” Cues to overeat: psychological factors influencing overconsumption. 2020. doi: 10.1017/S0029665107005344 [DOI] [PubMed] [Google Scholar]
- 18.Aggarwal A, Monsivais P, Cook AJ, Drewnowski A. Positive attitude toward healthy eating predicts higher diet quality at all cost levels of supermarkets. J Acad Nutr Diet. 2014;114(2):266–272. doi: 10.1016/j.jand.2013.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aggarwal A, Rehm CD, Monsivais P, Drewnowski A. Importance of taste, nutrition, cost and convenience in relation to diet quality: Evidence of nutrition resilience among US adults using National Health and Nutrition Examination Survey (NHANES) 2007–2010. Prev Med (Baltim). 2016;90:184–192. doi: 10.1016/j.ypmed.2016.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drewnowski A, Aggarwal A, Hurvitz PM, Monsivais P, Moudon AV. Obesity and supermarket access: proximity or price? Am J Public Health. 2012;102(8):e74–80. doi: 10.2105/AJPH.2012.300660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dubowitz T, Zenk SN, Ghosh-Dastidar B, et al. Healthy food access for urban food desert residents: examination of the food environment, food purchasing practices, diet and BMI. Public Health Nutr. 2015;18(12):2220–2230. doi: 10.1017/S1368980014002742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Minaker LM, Olstad DL, Thompson ME, Raine KD, Fisher P, Frank LD. Associations between frequency of food shopping at different store types and diet and weight outcomes: Findings from the NEWPATH study. Public Health Nutr. 2016;19(12):2268–2277. doi: 10.1017/S1368980016000355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bozeman JF, Ashton WS, Theis TL. Distinguishing Environmental Impacts of Household Food-Spending Patterns Among U.S. Demographic Groups. Environ Eng Sci. 2019;36(7):763–777. doi: 10.1089/ees.2018.0433 [DOI] [Google Scholar]
- 24.Cornelsen L, Berger N, Cummins S, Smith RD. Socio-economic patterning of expenditures on ‘out-of-home’ food and non-alcoholic beverages by product and place of purchase in Britain. Soc Sci Med. 2019;235(May):112361. doi: 10.1016/j.socscimed.2019.112361 [DOI] [PubMed] [Google Scholar]
- 25.Tiwari A, Aggarwal A, Tang W, Drewnowski A. Cooking at Home: A Strategy to Comply With U.S. Dietary Guidelines at No Extra Cost. Am J Prev Med. 2017;52(5):616–624. doi: 10.1016/J.AMEPRE.2017.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Langellier BA. Consumption and expenditure on food prepared away from home among Mexican adults in 2006. Salud Publica Mex. 2015;57(1):4–13. doi: 10.21149/spm.v57i1.7397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turner-McGrievy GM, Leach AM, Wilcox S, Frongillo EA. Differences in Environmental Impact and Food Expenditures of Four Different Plant-based Diets and an Omnivorous Diet: Results of a Randomized, Controlled Intervention. J Hunger Environ Nutr. 2016;11(3):382–395. doi: 10.1080/19320248.2015.1066734 [DOI] [Google Scholar]
- 28.French SA, Tangney CC, Crane MM, Wang Y, Appelhans BM. Nutrition quality of food purchases varies by household income: The SHoPPER study. BMC Public Health. 2019;19(1):1–7. doi: 10.1186/s12889-019-6546-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanjeevi N, Freeland-Graves J, Sachdev PK, Sands J. Do food expenditure patterns of Supplemental Nutrition Assistance Program households meet Thrifty Food Plan recommendations? J Hunger Environ Nutr. 2019;14(3):352–364. doi: 10.1080/19320248.2018.1540323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monsivais P, McLain J, Drewnowski A. The rising disparity in the price of healthful foods: 2004–2008. Food Policy. 2010;35(6):514–520. doi: 10.1016/j.foodpol.2010.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reidlinger DP, Sanders TA, Goff LM. How expensive is a cardioprotective diet? Analysis from the CRESSIDA study. Public Health Nutr. 2017;20(8):1423–1430. doi: 10.1017/S1368980016003529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nansel T, Haynie D, Lipsky L, Mehta S, Laffel L. Little variation in diet cost across wide ranges of overall dietary quality among youth with type 1 diabetes. J Acad Nutr Diet. 2015;115(3):433–439.e1. doi: 10.1016/j.jand.2014.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buszkiewicz J, House C, Aggarwal A, Long M, Drewnowski A, Otten JJ. The Impact of a City-Level Minimum Wage Policy on Supermarket Food Prices by Food Quality Metrics: A Two-Year Follow Up Study. Int J Environ Res Public Health. 2019;16(1):102. doi: 10.3390/ijerph16010102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carlson A, Lino M, Juan W, et al. Development of the CNPP Prices Database.; 2008. doi: 10.22004/AG.ECON.45851 [DOI] [Google Scholar]
- 35.Pondor I, Gan WY, Appannah G. Higher dietary cost is associated with higher diet quality: A cross-sectional study among selected malaysian adults. Nutrients. 2017;9(9):12–14. doi: 10.3390/nu9091028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shiraki K, Murakami K, Okubo H, et al. Nutritional correlates of monetary diet cost in young, middle-aged and older Japanese women. J Nutr Sci. 2017:1–11. doi: 10.1017/jns.2017.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marty L, Dubois C, Gaubard MS, et al. Higher nutritional quality at no additional cost among low-income households: Insights from food purchases of “positive deviants.” Am J Clin Nutr. 2015;102(1):190–198. doi: 10.3945/ajcn.114.104380 [DOI] [PubMed] [Google Scholar]
- 38.U.S. Census Bureau QuickFacts: Washington. https://www.census.gov/quickfacts/fact/table/WA/POP010210. Published 2010. Accessed October 21, 2019.
- 39.Food Research & Action Center (FRAC). SNAP Participation Map. https://www.frac.org/snap-county-map/snap-counties.html. Published 2019. Accessed September 19, 2019.
- 40.Drewnowski A, Aggarwal A, Tang W, Moudon AV. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity. 2015;23(3):671–676. doi: 10.1002/oby.20989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Briant KJ, Espinoza N, Galvan A, et al. An Innovative Strategy to Reach the Underserved for Colorectal Cancer Screening. J Cancer Educ. 2015;30(2):237–243. doi: 10.1007/s13187-014-0702-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duggan C, Carosso E, Mariscal N, et al. Diabetes prevention in hispanics: Report from a randomized controlled trial. Prev Chronic Dis. 2014;11(2). doi: 10.5888/pcd11.130119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Behavioral Risk Factor Surveillance System (BRFSS): Washington State Department of Health. https://www.doh.wa.gov/DataandStatisticalReports/DataSystems/BehavioralRiskFactorSurveillanceSystemBRFSS. Published 2016. Accessed October 21, 2019.
- 44.National Center for Health Statistics. NHANES - About the National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Published 2017. Accessed July 22, 2019.
- 45.Centers for Disease Control and Prevention - Behavioral Risk Factor Surveillance System (BRFSS). https://www.cdc.gov/brfss/index.html. Published 2019. Accessed September 11, 2019.
- 46.Fred Hutchinson Cancer Research Center. Food Frequency Questionnaires (FFQ). https://sharedresources.fredhutch.org/services/food-frequencyquestionnaires-ffq. Published 2016. Accessed August 2, 2019.
- 47.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. doi: 10.1016/J.JAND.2018.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.US Department of Health and Human Services. Dietary Guidelines for Americans 2015–2020. 8th editio. Skyhorse Publishing Inc.; 2015. https://health.gov/dietaryguidelines/2015/. Accessed July 23, 2019. [Google Scholar]
- 49.HEI Scores for Americans | USDA-FNS. https://www.fns.usda.gov/hei-scores-americans (2019), Accessed 15th May 2020
- 50.Bowman SA, Friday JE, Moshfegh AJ MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003–2004: documentation and User Guide. US Department of Agriculture (2008) https://www.researchgate.net/profile/Shanthy_Bowman/publication/266213030_MyPyramid_Equivalents_Database_20_for_USDA_Survey_Foods_2003-2004_Documentation_and_User_Guide/links/552fd5790cf2f2a588aa7192/MyPyramid-Equivalents-Database-20-for-USDA-Survey-Foods-2003-2004-Documentation-and-User-Guide.pdf [Google Scholar]
- 51.Sally Schakel. Maintaining a nutrient database in a changing marketplace: keeping pace with changing food products - A research perspective J. Food Compos. Anal, 14 (3) (2001), pp. 315–322, 10.1006/jfca.2001.0992 [DOI] [Google Scholar]
- 52.Matthews R, Garrison Y. Food Yields Summarized by Different Stages of Preparation.; 1975. https://books.google.com/books?hl=en&lr=&id=hI41AAAAIAAJ&oi=fnd&pg=PA4&ots=oq_zzqQvgl&sig=rRMW7LjcnGnbZep4nS9VD4UcDkg. Accessed April 2, 2020.
- 53.How to Understand and Use the Nutrition Facts Label | FDA. https://www.fda.gov/food/new-nutrition-facts-label/how-understand-and-usenutrition-facts-label. Accessed August 13, 2020.
- 54.Jiao J, Drewnowski A, Moudon AV, et al. The impact of area residential property values on self-rated health: A cross-sectional comparative study of Seattle and Paris. Prev Med Reports. 2016;4:68–74. doi: 10.1016/j.pmedr.2016.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vernez Moudon A, Cook AJ, Ulmer J, Hurvitz PM, Drewnowski A. A neighborhood wealth metric for use in health studies. Am J Prev Med. 2011;41(1):88–97. doi: 10.1016/j.amepre.2011.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Drewnowski A, Aggarwal A, Cook A, Stewart O, Moudon AV. Geographic disparities in Healthy Eating Index scores (HEI-2005 and 2010) by residential property values: Findings from Seattle Obesity Study (SOS). Prev Med (Baltim). 2016;83:46–55. doi: 10.1016/j.ypmed.2015.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lorgelly PK, Lindley J. What is the relationship between income inequality and health? Evidence from the BHPS. Health Econ. 2008;17(2):249–265. doi: 10.1002/hec.1254 [DOI] [PubMed] [Google Scholar]
- 58.Wagstaff A, van Doorslaer E. Income Inequality and Health: What Does the Literature Tell Us? Annu Rev Public Health. 2000;21(1):543–567. doi: 10.1146/annurev.publhealth.21.1.543 [DOI] [PubMed] [Google Scholar]
- 59.Kahneman D, Deaton A. High income improves evaluation of life but not emotional well-being. Proc Natl Acad Sci U S A. 2010;107(38):16489–16493. doi: 10.1073/pnas.1011492107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aggarwal A, Delaney JA, Drewnowski A. Nutrition Resilience in the Seattle Obesity Study: How to Eat Better for Less. FASEB J. 2017;31(1_supplement):4548. https://www.fasebj.org/doi/abs/10.1096/fasebj.31.1_supplement.45.8. [Google Scholar]
- 61.Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res. 2011;2(4):320–332. doi: 10.1504/IJBHR.2011.043414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211–217. doi: 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Otten J, Buszkiewicz J, Tang W, et al. The Impact of a City-Level Minimum-Wage Policy on Supermarket Food Prices in Seattle-King County. Int J Environ Res Public Health. 2017;14(9):1039. doi: 10.3390/ijerph14091039 [DOI] [PMC free article] [PubMed] [Google Scholar]