Abstract
Background:
Elder abuse is common and has serious health consequences but is under-recognized by health care providers. An important reason for this is difficulty in distinguishing between elder abuse and unintentional trauma. Our goal was to identify injury patterns associated with physical elder abuse in comparison with patients presenting to the emergency department (ED) with unintentional falls.
Methods:
We partnered with a large, urban district attorney’s office and examined medical, police, and legal records from successfully prosecuted cases of physical abuse of victims aged ≥60 from 2001–2014.
Results:
We prospectively enrolled patients who presented to a large, urban, academic ED after an unintentional fall. We matched 78 cases of elder abuse with visible injuries to 78 unintentional falls. Physical abuse victims were significantly more likely than unintentional fallers to have bruising (78% vs. 54%) and injuries on the maxillofacial/dental/neck (67% vs. 28%). Abuse victims were less likely to have fractures (8% vs. 22%) or lower extremity injuries (9% vs. 41%). Abuse victims were more likely to have maxillofacial/dental/neck injuries combined with no upper and lower extremity injuries (50% vs. 8%). Examining precise injury locations yielded additional differences, with physical elder abuse victims more likely to have injuries to the left cheek / zygoma (22% vs. 3%) or on the neck (15% vs. 0%) or ear (6% vs. 0%).
Conclusion:
Specific, clinically identifiable differences may exist between unintentional injuries and those from physical elder abuse. This includes specific injury patterns that infrequently occur unintentionally.
INTRODUCTION
Background
Elder abuse is common,1–3 has serious consequences,4–10 and is under-recognized.1,3,11 It is estimated that 5–10% of U.S. older adults are victims of elder abuse annually.1–3 Victimization is associated with adverse health outcomes including: depression,4 exacerbation of chronic illnesses, hospitalization,5 nursing home placement,6,7 and dramatically increased mortality.8–10 Although not easily quantified, abuse is estimated to cost many billions of dollars annually.12,13 Anticipated growth in the geriatric population will likely dramatically increase this disease burden and cost.14–16 This mistreatment may include physical abuse, sexual abuse, neglect, psychological abuse, or financial exploitation, and many victims suffer from multiple types of abuse.1–3,17 While physical abuse occurs less frequently, with a reported prevalence of 0.2–2.1% among community-dwelling older adults,1,18–20 this violent mistreatment may be particularly devastating for an older adult.
Importance
As few as 1 in 24 cases of elder abuse is reported to the authorities,1,3,11 and much of the associated morbidity and mortality results from this delay in identification and intervention.21 For many older adults, assessment by health care providers may represent their only contact outside the home. These providers, therefore, have a unique opportunity to identify suspected elder abuse, report it to Adult Protective Services and other authorities,22–28 and initiate intervention. Given that physical abuse may cause acute injury leading to a health care visit more commonly than other types of elder mistreatment, health care providers may have a unique opportunity to identify this abuse and initiate intervention. Despite this, health care providers seldom identify or report elder abuse.29 An important reason for this is the difficulty in distinguishing between physical elder abuse and the sequelae of unintentional trauma.21,30–33 Identifying evidence-based injury patterns that very seldom occur due to an accident is the cornerstone of detecting child abuse,34–47 which physicians do commonly. This approach is based on literature that includes systematic reviews and large comparison studies describing key features that distinguish abuse from unintentional injury. Though injuries potentially suggestive of elder abuse have been anecdotally described,21–28,48–56 very little rigorous research21,57–59 comparing all injuries in confirmed cases of physical elder abuse to those in non-abused older adults has been conducted to identify injury patterns to aid clinicians in identifying physical elder abuse when evaluating purportedly unintentional injuries. Differentiating intentional and unintentional injuries in older adults is more challenging due to normal physiologic changes that occur with aging 21,30–33 including osteopenia, thinning of the skin, and easy bruising as well as the impact of medications commonly used including anti-coagulants.
Existing studies have begun to describe bruise location and size57,58 and body regions frequently injured in physical elder abuse.21,59 Additional research is critically needed to inform elder abuse detection, with the goal of identifying potentially highly specific injury patterns and forensic findings.
Goals of this Investigation
We collaborated with the Elder Abuse Unit of the King’s County District Attorney’s Office in Brooklyn, New York to examine in detail injury characteristics and patterns from a large series of legally adjudicated cases of physical elder abuse. As the limited existing literature suggests that victims and abusers often falsely report that abuse-related injuries are due to an unintentional “fall,”58–60 we used geriatric patients presenting to the emergency department after an unintentional fall as a comparison group. Our goal was to identify differences between injury patterns associated with physical elder abuse and those associated with unintentional falls to assist health care providers in identification of abuse.
METHODS
Study Design and Setting
We conducted a comparative study with a case-control design to identify differences in injury characteristics and patterns between physical elder abuse and unintentional injuries, similar to approaches used to identify injury patterns in child abuse43,61 and in smaller studies focused on elder abuse.4,26 In our study, we compared injuries in elder abuse cases where the perpetrator had been convicted or pled guilty to those in patients presenting to the ED after unintentional falls. We followed STROBE guidelines regarding the reporting of observational research.62
Assessment of Physical Elder Abuse Cases
In order to assess elder abuse cases, we partnered with the King’s County District Attorney’s Office, which maintains an Elder Abuse Unit, a legal team devoted exclusively to the investigation of cases, prosecution of abusers, and protection of these vulnerable victims. We examined 100 successfully prosecuted cases of physical abuse of a victim aged ≥60 years where the perpetrator had been convicted or pled guilty from 2001–2014. We did not include cases sealed by the court because the abuser elected to enter and successfully completed a substance abuse or mental health treatment program.
We defined physical abuse using New York State Social Services Law, Article 9B, Adult Protective Services, Section 473(6) as: “the non-accidental use of force that results in bodily injury, pain or impairment, including but not limited to, being slapped, burned, cut, bruised or improperly restrained” by a person in a relationship with the victim with an expectation of trust. This law is similar to the consensus definition from National Research Council,17 which incorporates the content of statutes from different U.S. states, and the definitions recently proposed in the Elder Justice Roadmap12 and by the Centers for Disease Control and Prevention.63
We reviewed police, legal, and medical records, including photographs and victim statements, to gather detailed information about the injuries, the victim, the abuser, and the circumstances surrounding the physical abuse incident and its detection.
To facilitate the complete and accurate characterization of injuries, we developed a novel taxonomy64 that uses a 3-step process to describe and classify visible, acute, injuries in geriatric victims. It includes 9 unique types of visible injury and 7 characteristics common to all injury types, including 6 body regions and 247 precise anatomic locations. Research team members reviewed photographs and abstracted data from medical records including physical exam descriptions and imaging reports using a protocol developed by three of the authors (TR, VML, EMB), who trained other authors (AE, TM) who participated in the process. Two separate researchers, one of whom was a physician (TR or VML), independently evaluated each photograph to ensure consistency and accuracy of the descriptions. To increase the utility of our findings for clinicians, we grouped the 247 precise anatomic locations into 99 meaningful sub-regions for analysis (available in Online Supplemental Material).
Enrollment of Control Patients
We prospectively enrolled control patients aged ≥60 years who presented to the ED after an unintentional fall from September 2014 – June 2018 in a large, urban, academic medical center in Manhattan, New York City. Trained Research Associates (RAs) recruited patients from 7:30AM-11:30PM 7 days a week. The use of RAs is common in Emergency Medicine research and is well-described.65 We excluded patients if they did not speak English, were acutely intoxicated, or were deemed medically or psychiatrically unstable by the treating physician. We enrolled study patients unable to provide informed consent if a legally-authorized representative was able to consent on their behalf.
We conducted a standardized interview to collect information on demographics, health, functional status, and circumstances surrounding the fall injury, and a structured data abstraction form was used to gather information from the medical record for the ED visit. To allow for optimal comparison with injuries sustained by victims of physical elder abuse, we instructed RAs to photograph each injury using a standardized photography protocol developed by our group.66 The protocol describes in detail appropriate types of photographs and body positioning to characterize injuries on various body regions and includes instructional diagrams. We described and categorized injuries using the same process used for injuries in the elder abuse cases.
To ensure that injuries were truly due to unintentional falls and not the result of physical elder abuse, we included the validated Elder Abuse Suspicion Index67 which we administered privately to each potential study patient. We excluded from the study patients who screened positive, and the results of these screens were reported to the clinical care team and the on-duty social worker. The research team also reviewed all hospital medical records for the enrollment visit and for visits for six months after enrollment to ensure that elder abuse was not subsequently identified.
Statistical Analysis
We matched elder abuse cases and unintentional fall controls with injuries 1:1 using individual matching on age (5-year age groups), sex, and living in the community vs. institution. These factors were determined a priori given their potential to confound our analysis of injury patterns. We conducted sensitivity analyses that examined the effect of additionally matching on race.
Results are presented as percentages and 95% confidence intervals (CIs) or medians (with interquartile range). We compared elder abuse cases and fall patients with McNemar’s tests, Paired t-tests, and Wilcoxon sign-rank tests, as appropriate. All P values were two-tailed, with P<0.05 considered statistically significant. We also performed conditional multivariable logistic regression to identify differences in injury patterns between cases and controls while adjusting for injury severity, time between injury and presentation, and total number of injuries. We used Stata 14.0 (StataCorp, College Station, TX) for all analyses.
This project was reviewed and approved by the Weill Cornell Medicine Institutional Review Board.
RESULTS
Characteristics of Study Patients
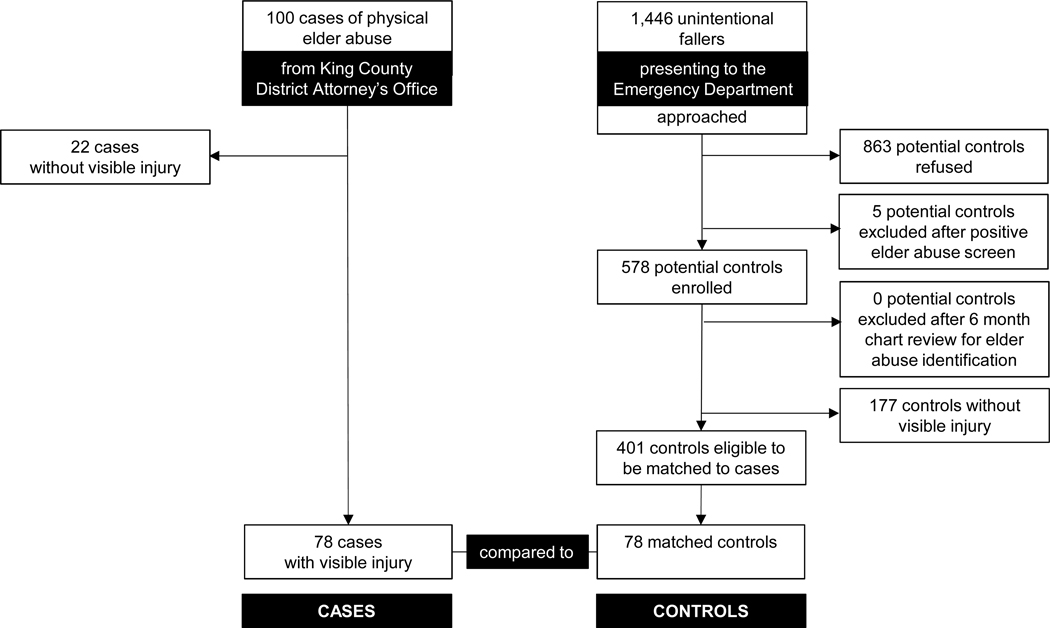
We examined 100 successfully prosecuted physical elder abuse cases. Of these, 78 had visible injuries resulting from the abuse. We matched these 78 cases to 78 control patients on age, sex, and living in the community vs. institution drawn from among 578 enrolled patients who sought ED care for injuries after an unintentional fall. 863 potential study patients declined study participation. Five potential patients screened positive on the Elder Abuse Suspicion Index and were excluded. None were found to be victims of physical elder abuse after a more complete evaluation. No additional patients were excluded after medical records review. Figure 1 summarizes the sources of case and control patients. Notably, we had originally anticipated requiring the enrollment of 200 control patients during 12 months to match to cases, but, given differences in characteristics, particularly age, between cases and initially enrolled controls, we extended the control enrollment period by 34 months.
Figure 1:
Flow diagram showing sources of case and control patients
Overall, cases and controls had a mean age of 71(SD 9) years, 73% were female, and 97% lived in the community. Cases and control patients differed according to race/ethnicity (cases: 46% white, 45% black, 4% other race, and 5% unknown vs. controls: 78% white, 5% black, 3% other race, and 14% unknown). (Table 1). Only one-third of victims received care in the ED after abuse was detected, with many refusing Emergency Medical Services transport. The most common mechanisms of physical abuse were blunt assault with hands/fists (62%) and push/shove or fall during altercation (23%).
Table 1:
Characteristics of physical elder abuse victims, abusers, and circumstances surrounding abuse
| Physical Elder Abuse Cases (n=100) |
|
|---|---|
| Abuser’s relationship to victim | |
| Spouse / Companion | 17 |
| Male abuser* | 71 |
| Female abuser* | 29 |
| Former spouse / Companion | 6 |
| Male abuser** | 50 |
| Female abuser** | 50 |
| Son | 41 |
| Daughter | 8 |
| Grandchild | 18 |
| Other family | 6 |
| Home attendant | 2 |
| Other non-relative | 2 |
| Victim’s living situation | |
| Community-dwelling with abuser | 65 |
| Community dwelling – other | 33 |
| Nursing home / group home | 2 |
| Abuser identified as victim’s primary caregiver | 3 |
| Type of Physical Abuse / Mechanism*** | |
| Blunt assault with hand/fist | 62 |
| Push/shove, fall during altercation | 23 |
| Blunt assault with object | 21 |
| Blunt assault with foot/knee | 17 |
| Strangulation/suffocation | 12 |
| Grabbing/twisting/pinching | 9 |
| Penetrating assault with object | 5 |
| Using body weight/sitting on victim | 4 |
| Other | 7 |
| Multiple Mechanisms | 36 |
| Detection Method | |
| Victim calls 911 | 58 |
| Other person calls 911 | 25 |
| Law enforcement non-911 response | 6 |
| Victim goes to police precinct to report | 2 |
| Other | 9 |
Percentage of Spouse / Companion abusers (total n=17)
Percentage of Former spouse / Companion abusers (total n=6)
Percentage of victims with visible injuries (total n=78)
Law enforcement or medical provider photographs of at least one of the victim’s injuries at the time of elder abuse identification or injury evaluation were available for (47/78) 60% of physical elder abuse cases, and medical records were available for 26% (20/78).
Main Results
We examined 264 injuries in these 78 physical elder abuse victims. Photographs were available for 166 (63%) injuries and medical record and police report descriptions were relied upon for 98 (37%) injuries. For some cases, photographs were available for some injuries but not others. We compared the injuries suffered by abuse victims to 217 injuries in 78 fall control patients. Photographs were available for 119 (55%) injuries and medical record descriptions were relied upon for 97 (45%) injuries in fall control patients. Based on available information, we were able to describe the sub-region for a total of 417 injuries in cases and controls (87%) and the precise location of 408 (85%).
Though intentional fall injuries were slightly more severe, neither cases nor controls typically suffered severe injuries. (Table 2) The most common types of abuse-related injuries were bruises (78% of victims), lacerations (32%), and abrasions (32%). Clear differences in injury patterns between abuse victims and fallers were observed. Physical abuse victims were significantly more likely to have bruising (78% vs. 54%, 24% difference (95% confidence interval of difference: 8–41%) and injuries on the maxillofacial/dental/neck region (67% vs. 28%, 38% difference (22,55)) or chest/abdomen/back (19% vs. 4%, 15% difference (4,27)). Abuse victims were less likely to have fractures (8% vs. 22%, −14% difference (−26,−2)) or injuries on the lower extremities (9% vs. 41%, −32% difference (−45,−19)).
Table 2:
Characteristics of injuries in physical elder abuse victims with visible injuries vs. matched unintentional fallers with visible injuries presenting to an urban, academic emergency department
| Physical Elder Abuse Cases (n=78) % | Unintentional Fall Controls (n=78) % | Difference % (95% CI) | P value | |
|---|---|---|---|---|
| Injury Severity Score (ISS), median (IQR) | 1 (1 – 2) | 2 (1 – 3) | 0 (0, 1.0) | 0.06 |
| Time between injury and evaluation | 0.06 | |||
| <1 day | 92% | 83% | 9% (−3, 21) | |
| 1–2 days | 6% | 12% | 5% (−16, 5) | |
| >2 days | 0% | 5% | 5% (−11, 1) | |
| Unknown | 1% | 0% | 1% (−2, 5) | |
| Number of injuries, median (IQR) | 2 (1 – 5) | 3 | 0.0 (−2.0, 1.8) | 0.59 |
| Range: 1 – 18 | Range 1 – 10 | |||
| Injury Type(s), frequency (95% CI) | ||||
| Bruise | 78% | 54% | 24% (8, 41) | 0.003 |
| Abrasion | 32% | 46% | −14% (−31, 3) | 0.08 |
| Laceration | 32% | 23% | 9% (−5, 23) | 0.16 |
| Fracture | 8% | 22% | −14% (−26, −2) | 0.02 |
| Skin tear | 3% | 8% | −5% (−12, 2) | 0.10 |
| Other | 17% | 30% | −13% (−27, 1) | 0.05 |
| Multiple injury types | 47% | 59% | −12% (−29, 6) | 0.18 |
| Body region(s) injured | ||||
| Maxillofacial / dental / neck | 67% | 28% | 38% (22, 55) | <0.001 |
| Upper extremity | 40% | 59% | −19% (−35, −3) | 0.01 |
| Skull / brain | 22% | 13% | 9% (−4, 22) | 0.14 |
| Chest / abdomen / back | 19% | 4% | 15% (4, 27) | 0.005 |
| Lower extremity | 9% | 41% | −32% (−45, −19) | <0.001 |
| Pelvis / buttocks | 1% | 6% | −5% (−12, 2) | 0.10 |
| Multiple body regions injured | 44% | 41% | −3% (−14, 19) | 0.74 |
Cases and controls were matched by age (5 year intervals), sex, and whether they lived in the community or institution.
ISS denotes injury severity score; IQR, interquartile range.
We also examined patterns that included both presence and absence of injuries in body regions. We found that abuse victims were significantly more likely to have visible injuries in the maxillofacial/dental/neck region without injuries to the upper or lower extremities (50% vs. 8%, 42% difference (28,57)). Significant differences also existed when examining maxillofacial/dental/neck injuries and the absence of upper extremities, lower extremities, and pelvis/buttocks injuries individually or in any combination.
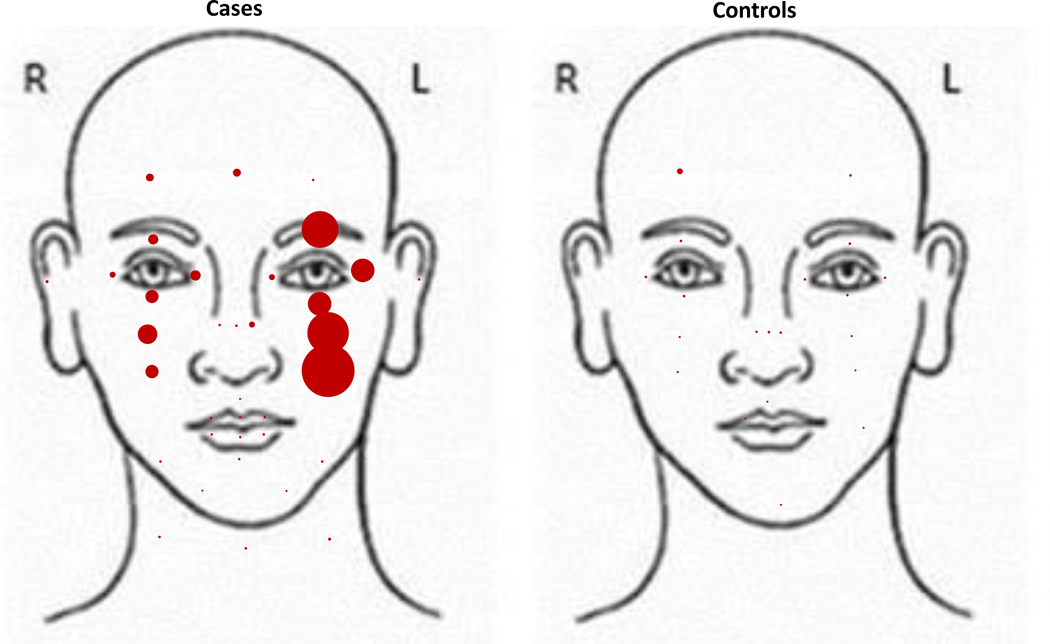
We also identified 8 sub-regions more commonly injured in physical elder abuse victims than fallers (Table 3), including the left check/zygoma, the ears, and the neck. These findings further suggest differences in patterns between abuse and falls that may be used by clinicians at the bedside. (Figure 2)
Table 3:
Sub-regions of body more commonly injured in physical elder abuse victims with visible injuries vs. matched unintentional fallers with visible injuries presenting to an urban, academic emergency department
| Physical Elder Abuse Cases (n=78) % (95% CI) | Unintentional Fall Controls (n=78) % (95% CI) | Difference % (95% CI) | P value | |
|---|---|---|---|---|
| Maxillofacial / Dental / Neck | ||||
| Face | 60% | 28% | 32% (15, 49) | <0.001 |
| Left Peri-Orbital Area | 22% | 9% | 13% (1, 25) | 0.03 |
| Left Peri-Orbital Area / Zygoma | 22% | 9% | 13% (1, 25) | 0.03 |
| Left Cheek / Zygoma | 22% | 3% | 19% (8, 30) | <0.001 |
| Left Cheek / Mandible | 17% | 3% | 14% (4, 25) | 0.005 |
| Ears | 6% | 0% | 6% (0, 13) | 0.03 |
| Jaw | 14% | 3% | 11% (2, 21) | 0.01 |
| Neck | 15% | 0% | 15% (6, 25) | <0.001 |
Cases and controls were matched by age (5 year intervals), sex, and whether they lived in the community or institution.
Figure 2: Comparison of precise locations of bruises in the maxillofacial/dental/neck region in physical elder abuse victims with visible injuries vs. matched unintentional fallers with visible injuries presenting to an urban, academic emergency department.
Note: This figure is a visual representation of how commonly bruises were found in precise locations among case and control patients. Within the figure, we have placed a circle in each precise location where bruise(s) were found. 171 bruises in cases and 61 bruises in controls contributed to this diagram because they were in at least one precise location within the maxillofacial / dental / neck body region. For bruises that covered multiple precise locations, the diagram represents them in all of these precise locations. The size of each circle’s area corresponds directly to the total number of bruises in that precise location among all case or control patients. To ensure visibility of circles, precise locations with 1–3 bruises are shown with circles with the same area.
Notably, we found differences that were not significant between cases and controls in injuries to the ulnar and posterior forearm (9% vs. 4%, 5% difference (−4,14)) on either or both sides and to the left ulnar and posterior forearm (4% vs. 0%, 4% difference (−2,9)).
All findings of significant difference in injuries between cases and controls remained significant in multivariable logistic regression that adjusted for injury severity, time between injury and evaluation, and total number of injuries in individual models and a combined model.
Because of the difference in race/ethnicity between elder abuse cases and unintentional fall controls, we conducted a sensitivity analysis matching on race in addition to age, sex, and living situation. The number of available matched pairs was reduced to 54. Among this subset, no material changes in our results were observed (available in Online Supplemental Material).
Among the 22 elder abuse victims who did not sustain visible injury, pain was most commonly reported in the chest/abdomen/back (32%), maxillofacial/dental/neck (22%), and upper extremities (22%). Twenty-seven percent had documentation of no indication of pain.
LIMITATIONS
Our research examines physical elder abuse in a New York City and may not be generalizable to other populations. We only included cases of physical elder abuse that were identified and successfully adjudicated by the legal system. This represents a small percentage of all cases, and victims of the mistreatment analyzed here may have experienced more acute or severe abuse allowing identification. Subtle cases of abuse that are more challenging to detect and prosecute likely haven’t been included. Cases examined here also may reflect victims with a better support system, increased ability to report abuse, and better health care and legal literacy. This is highlighted by the fact that, in the large majority of cases in this analysis, abuse was detected when the victim him/herself contacted 911.
Victims with cognitive impairment are underrepresented in our research yet are thought to be at greater risk for elder abuse.60 Additionally, our sample includes very few abuse victims who live in institutions, and as such our research findings may not apply to those populations or settings. The majority of the abuse victims included in this research were not evaluated in the ED, with many refusing transport after abuse was detected. It is possible that victims who present to EDs differ in important ways from those who do not. Although our study was not powered for this purpose, we did not observe differences between elder abuse victims who did and did not present to the ED.
Case files were assembled for law enforcement and prosecution purposes rather than research, and, therefore, medical records and photographs were not available for many cases. Additionally, photographs examined were of variable quality and medical records had variable detail and completeness. We did not find any sexual abuse among the cases we examined, but given that sexual abuse and physical abuse may co-occur and that sexual abuse is underrecognized, it is possible that it was missed.
Our control group was recruited from a single urban ED, which increases feasibility, but nearly all physical elder abuse victims who were transported to an ED were taken to other institutions than the one where we enrolled controls. The potential for this to impact results is highlighted by racial differences between cases and controls, and other important differences, such as socioeconomic status, may exist between the groups. While our results did not materially change in sensitivity analyses adjusting for race/ethnicity, it remains possible that the two groups differed according to socioeconomic status and other characteristics we were not able to measure. While injuries in control patients were photographed using a standardized protocol, those available for cases were not. Differences in photograph quality may have led to differential identification of visible injuries.
Many potential control patients refused participation, and these fallers may have differed from those who participated. While we attempted to ensure that unintentional fall controls were not victims of elder abuse at the time of enrollment, it remains possible that injuries in control patients were from undetected physical elder abuse rather than unintentional fall.
Additionally, it wasn’t possible to blind the investigators reviewing photographs to whether the injuries were due to physical elder abuse or unintentional fall given differences in the image format. This may have introduced bias, as reviewing authors may have had preconceived notions about the appearance of injuries in elder abuse cases.
In nearly all cases where information was available, photographs of injuries among cases was taken soon after the injury at the time of elder abuse identification or initial injury evaluation. Nevertheless, our findings about the frequency of the presence of bruising may have been impacted by differences between cases and controls in the time between the injury and photographs, given that bruising may take time to develop.
DISCUSSION
. Our approach represents a significant methodologic advance, allowing for the in-depth evaluation of injuries in a large number of legally adjudicated elder abuse cases in which the presence of abuse has been established by the criminal justice system, thus establishing a potential new “gold standard.” This represents a rich, previously unexplored data source to examine in detail characteristics of this poorly understood phenomenon. Additionally, previous research has suffered from challenges in identifying and confirming cases, with the most rigorous studies typically convening an “expert panel” to assess cases to determine that abuse occurred.57,68
Our finding that the most common mechanisms were an abuser assaulting the victim with hands/fists as well as pushing/shoving them or causing a fall during altercation suggests that abuse may have been precipitated by the escalation of an argument. The mechanism of physical abuse of push/shove or fall during altercation, common among the patients within our study, may be particularly difficult to distinguish from unintentional fall.
We found that, even among successfully prosecuted cases of physical abuse, 22% did not have any visible injuries, further underscoring challenges in identification. These victims most commonly complained of pain in their chest/abdomen/back, maxillofacial/dental/neck, and upper extremities, a finding which may provide insight in how to approach patients without injury in whom abuse is suspected.
Our research suggests that injuries in physical elder abuse are commonly found in the maxillofacial/dental/neck area and the upper extremities, which confirms previous findings.21,59 Research comparing geriatric assault injuries to unintentional injuries has also found similar patterns, with assault injuries more commonly found on the head and face.69
We found that physical abuse victims were significantly more likely than unintentional fallers to have bruising and injuries on the maxillofacial/dental/neck region and were less likely to have abrasions, fractures, or injuries on the lower extremities. In the only other published study, to our knowledge, comparing cases of physical elder abuse to unintentional injuries, Wiglesworth and colleagues compared bruises in elder abuse victims to older adults with unintentional trauma, finding that victims of elder abuse had bruises that were more often large (>5 cm) and found on the face, lateral right arm, or posterior torso.57
Though not described before, our finding that injuries to the head and neck without injury to other parts of the body were much more common in abuse victims may be most helpful to clinicians. Due to aging-related physiologic changes and medications, older adults may sustain visible injuries on the extremities with a minor mechanism making the absence of these injuries suspect. Additional systematic research is needed to further explore and confirm this finding, however we feel that this may become a powerful tool for clinicians to use at the bedside.
The specific anatomic sub-regions which were identified as differing between abuse victims and falls may be of most help for clinicians. We found that physical elder abuse victims were more likely to have injuries in the left face. This supports existing literature examining younger adult assault victims, which has found that left-sided facial injuries are more frequent after assault than right-sided, likely because most assailants are right-handed.70–72 Neck injuries were also found much more commonly in abuse, as may be expected since the neck is typically protected during a fall by the shoulders or face. This supports existing research comparing geriatric assault to unintentional injuries which found that neck injuries were 6 times more likely in assault.69 Ear injuries occurred in assault but not in falls, replicating prior findings in child abuse injury patterns .73
While we found differences in the ulnar and posterior forearm between cases and controls, they did not reach significance. This pattern has been shown in previous research57, as it may occur when a victim attempts to defend him/herself from an abuser.57,74
That injuries in the neck or ears did not occur in any of the controlpatients suggests that these may represent potentially highly specific injury patterns. These preliminary results suggest clinically identifiable differences may exist between physical elder abuse injuries and those from unintentional falls.
Many abuse victims refused Emergency Medical Services transport to the ED for evaluation after abuse was detected, suggesting a resistance to seeking care that highlights challenges in elder abuse detection by health providers and should be further explored.
In summary, these promising preliminary findings suggest that differences may exist between injuries from physical elder abuse and those from unintentional falls. Specifically, physical elder abuse victims were more likely to have injuries to the left cheek/zygoma, neck, or ear. Also, abuse victims were more likely to have bruising and injuries to the maxillofacial/dental/neck region, particularly combined with no upper or lower extremity injuries. These patterns may provide clinicians with a powerful tool to be able to differentiate injuries from falls and physical abuse; clarifying one of the more complicated differentials in geriatric. Future research is needed to confirm these injury pattern findings. Ideally, research would prospectively enroll and comprehensively evaluate victims of physical elder abuse. Ultimately, an important goal of this forensic research should be using the findings to derive and validate an easy-to-use clinical prediction rule75 to assist busy clinical providers in identifying physical elder abuse. Currently, the findings we describe may be helpful to practicing clinicians as red flags to increase concern for the possibility of physical elder abuse and recommend that providers maintain a high index of suspicion for this very dangerous and under-recognized phenomenon.
Supplementary Material
Acknowledgments
Grants: Tony Rosen’s participation has been supported by a GEMSSTAR (Grants for Early Medical and Surgical Subspecialists’ Transition to Aging Research) grant (R03 AG048109) and a Paul B. Beeson Emerging Leaders Career Development Award in Aging (K76 AG054866) from the National Institute on Aging. He is also the recipient of a Jahnigen Career Development Award, supported by the John A. Hartford Foundation, the American Geriatrics Society, the Emergency Medicine Foundation, and the Society of Academic Emergency Medicine. Mark S. Lachs is the recipient of a mentoring award in patient-oriented research from the National Institute on Aging (K24 AG022399).
Meetings: Preliminary results were presented at the Society of Academic Emergency Medicine Annual Scientific Meeting, San Diego, May 2015 and American Geriatrics Society Annual Scientific Meeting, National Harbor, May 2015.
Clinically Meaningful Sub-Regions: Combination of Precise Anatomic Locations for Physical Elder Abuse Injury Pattern Analysis
These 98 clinically meaningful sub-regions are combinations of the XXX precise anatomic locations described by Rosen et al in their Comprehensive Classification System for Visible Intentional and Unintentional Acute Injuries:
Rosen T, Reisig C, LoFaso VM, Bloemen EM, Clark S, McCarthy TJ, Mtui EP, Flomenbaum NE, Lachs MS.Describing visible acute injuries: development of a comprehensive taxonomy for research and practice. Inj Prev. 23(5):340–345.
The sub-regions are shown organized within the 6 body regions (skull / brain, maxillofacial / dental / neck, chest / abdomen / back, pelvis / gluteal region, upper extremity, lower extremity) also described by Rosen et al. Notably, for sub-regions for which there are two sub-regions for left and right, we have shown as left (right) for simplicity.
Developed by: Tony Rosen MD MPH, Veronica M. LoFaso MD MS, Elizabeth M. Bloemen MPH, Sunday Clark ScD MPH, Thomas J. McCarthy BA, Christopher Reisig MD, Kiti Gogia MPH, Alyssa Elman LMSW, Arlene Markarian JD, Neal E. Flomenbaum MD, Rahul Sharma MD MBA, Mark S. Lachs MD MPH
Skull / Brain
Lateral Skull – Left (Right)
Left (Right) Temporal Region
Left (Right) Mastoid Process
Left (Right) Parietal Region
Occiput
Left Occipital Region
Right Occipital Region
Mid Occipital Region
Maxillofacial / Dental / Neck
Face
Left Frontal Region / Forehead
Right Frontal Region / Forehead
Mid Frontal Region / Forehead
Forehead - Unspecified
Left Supra-orbit
Left Infra-orbit
Left Medial Orbit
Left Lateral Orbit
Left Globe / Eye
Left Orbit - Unspecified
Right Supra-orbit
Right Infra-orbit
Right Medial Orbit
Right Lateral Orbit
Right Globe / Eye
Right Orbit - Unspecified
Left Nasal
Right Nasal
Nasal Bridge / Septum
Nose - Unspecified
Left External Ear
Right External Ear
Left Zygoma / Cheekbone
Right Zygoma / Cheekbone
Left External Buccal
Right External Buccal
Left Mandible
Right Mandible
Supra Peri-oral
Left Upper Lip
Right Upper Lip
Middle Upper Lip
Left Lower Lip
Right Lower Lip
Middle Lower Lip
Infra Peri-oral
Peri-oral / Lips - Uspecified
Left Mental / Chin
Right Mental / Chin
Mid Mental / Chin
Mental / Chin - Unspecified
Upper Lip
Lower Lip
Lateral Face – Left (Right)
Left (Right) Frontal Region / Forehead
Left (Right) Supra-orbit
Left (Right) Infra-orbit
Left (Right) Medial Orbit
Left (Right) Lateral Orbit
Left (Right) Globe / Eye
Left (Right) Nasal
Left (Right) External Ear
Left (Right) Zygoma / Cheekbone
Left (Right) External Buccal
Left (Right) Mandible
Left (Right) Upper Lip
Left (Right) Lower Lip
Left (Right) Mental / Chin
Left (Right) Orbit - Unspecified
Midline Face
Mid Frontal Region / Forehead
Nasal Bridge / Septum
Middle Upper Lip
Middle Lower Lip
Mid Mental / Chin
Forehead
Left Frontal Region / Forehead
Right Frontal Region / Forehead
Mid Frontal Region / Forehead
Forehead - Unspecified
Peri-orbit/orbit – Left (Right)
Left (Right) Supra-orbit
Left (Right) Infra-orbit
Left (Right) Medial Orbit
Left (Right) Lateral Orbit
Left (Right) Globe / Eye
Left (Right) Orbit - Unspecified
Peri-orbit/orbit/zygoma – Left (Right)
Left (Right) Supra-orbit
Left (Right) Infra-orbit
Left (Right) Medial Orbit
Left (Right) Lateral Orbit
Left (Right) Globe / Eye
Left (Right) Zygoma / Cheekbone
Left (Right) Orbit - Unspecified
Ears
Left External Ear
Right External Ear
Nose
Left Nasal
Right Nasal
Nasal Bridge / Septum
Nose – Unspecified
Buccal/Zygoma - Left (Right)
Left (Right) Zygoma / Cheekbone
Left (Right) External Buccal
Buccal/Mandible - Left (Right)
Left (Right) External Buccal
Left (Right) Mandible
Perioral/Oral
Supra Peri-oral
Left Upper Lip
Right Upper Lip
Middle Upper Lip
Left Lower Lip
Right Lower Lip
Middle Lower Lip
Infra Peri-oral
Peri-oral / Lips - Unspecified
Upper Lip
Lower Lip
Midline Perioral/Oral
Middle Upper Lip
Middle Lower Lip
Jaw
Left Mandible
Right Mandible
Left Mental / Chin
Right Mental / Chin
Mid Mental / Chin
Mental / Chin - Unspecified
Chin
Left Mental / Chin
Right Mental / Chin
Mid Mental / Chin
Mental / Chin - Unspecified
Neck
Anterior Neck
Left Lateral Neck
Right Lateral Neck
Cervical Spine / Midline Posterior Neck
Neck – Unspecified
Chest / Abdomen / Back
Chest / Thorax
Left Supraclavicular
Right Supraclavicular
Left Clavicular
Right Clavicular
Left Pectoral / Anterior Thorax
Right Pectoral / Anterior Thorax
Sternal
Left Breast
Left Areola
Left Nipple
Right Breast
Right Areola
Right Nipple
Left Axilla
Left Lateral Thorax / Infra-Axillary Region
Right Axilla
Right Lateral Thorax / Infra-Axillary Region
Chest / Anterior Thorax - Unspecified
Anterolateral Chest – Left (Right)
Left (Right) Supraclavicular
Left (Right) Clavicular
Left (Right) Pectoral / Anterior Thorax
Left (Right) Breast
Left (Right) Areola
Left (Right) Nipple
Left (Right) Axilla
Left (Right) Lateral Thorax / Infra-Axillary
Region
Abdomen
Left Upper Quadrant
Right Upper Quadrant
Left Lower Quadrant
Right Lower Quadrant
Periumbilical
Left Inguinal
Right Inguinal
Abdomen - Unspecified
Abdomen – Left (Right)
Left (Right) Upper Quadrant
Left (Right) Lower Quadrant
Left (Right) Inguinal
Back
Left Scapular Region
Right Scapular Region
Thoracic Spine
Left Paraspinal Thoracic
Right Paraspinal Thoracic
Thoracic Back - Unspecified
Lumbar Spine
Left Paraspinal Lumbar
Right Paraspinal Lumbar
Left Lumbar Back
Right Lumbar Back
Lumbar Back – Unspecified
Back - Unspecified
Back – Left (Right)
Left (Right) Scapular Region
Left (Right) Paraspinal Thoracic
Left (Right) Paraspinal Lumbar
Left (Right) Lumbar Back
Thoracic Back – Left (Right)
Left (Right) Scapular Region
Left (Right) Paraspinal Thoracic
Lumbar Back – Left (Right)
Left (Right) Paraspinal Lumbar
Left (Right) Lumbar Back
Pelvis / Gluteal Region
Anterior Pelvis
Pubic symphysis
Vulvar
Vaginal
Penile
Posterior Pelvis
Sacral
Coccygeal
Left Gluteal
Right Gluteal
Upper Extremity
Upper Extremity – Left (Right)
Left (Right) Anterior Shoulder
Left (Right) Lateral Shoulder
Left (Right) Posterior Shoulder
Left (Right) Anterior Arm
Left (Right) Lateral Arm
Left (Right) Medial Arm
Left (Right) Posterior Arm
Left (Right) Anterior / Antecubital Elbow
Left (Right) Posterior / Olecranon Elbow
Left (Right) Anterior Forearm
Left (Right) Radial / Lateral Forearm
Left (Right) Ulnar / Medial Forearm
Left (Right) Posterior Forearm
Left (Right) Volar Wrist
Left (Right) Radial / Lateral Wrist
Left (Right) Ulnar / Medial Wrist
Left (Right) Dorsal Wrist
Left (Right) Thenar Eminence
Left (Right) Hypothenar Eminance
Left (Right) Mid-Palmar Hand
Left (Right) Lateral Hand
Left (Right) Medial Hand
Left (Right) Dorsal Hand
Left (Right) Palmar Surface of Thumb
Left (Right) Lateral Surface of Thumb
Left (Right) Medial Surface of Thumb
Left (Right) Dorsal Surface of Thumb
Left (Right) Palmar Surface of Finger(s)
Left (Right) Lateral Surface of Finger(s)
Left (Right) Medial Surface of Finger(s)
Left (Right) Dorsal Surface of Finger(s)
Left (Right) Hand - Unspecified
Left (Right) Shoulder – Unspecified
Left (Right) Elbow – Unspecified
Left (Right) Forearm - Unspecified
Left (Right) Wrist - Unspecified
Left (Right) Arm - Unspecified
Left (Right) Palmar Hand
Upper Extremity without Hand
Right Anterior Shoulder
Right Lateral Shoulder
Right Posterior Shoulder
Right Anterior Arm
Right Lateral Arm
Right Medial Arm
Right Posterior Arm
Right Anterior / Antecubital Elbow
Right Posterior / Olecranon Elbow
Right Anterior Forearm
Right Radial / Lateral Forearm
Right Ulnar / Medial Forearm
Right Posterior Forearm
Right Volar Wrist
Right Radial / Lateral Wrist
Right Ulnar / Medial Wrist
Right Dorsal Wrist
Right Shoulder – Unspecified
Right Elbow – Unspecified
Right Forearm - Unspecified
Right Wrist - Unspecified
Left Anterior Shoulder
Left Lateral Shoulder
Left Posterior Shoulder
Left Anterior Arm
Left Lateral Arm
Left Medial Arm
Left Posterior Arm
Left Anterior / Antecubital Elbow
Left Posterior / Olecranon Elbow
Left Anterior Forearm
Left Radial / Lateral Forearm
Left Ulnar / Medial Forearm
Left Posterior Forearm
Left Volar Wrist
Left Radial / Lateral Wrist
Left Ulnar / Medial Wrist
Left Dorsal Wrist
Left Shoulder – Unspecified
Left Elbow – Unspecified
Left Forearm - Unspecified
Left Wrist – Unspecified
Upper Extremity without Hand – Left (Right)
Left (Right) Anterior Shoulder
Left (Right) Lateral Shoulder
Left (Right) Posterior Shoulder
Left (Right) Anterior Arm
Left (Right) Lateral Arm
Left (Right) Medial Arm
Left (Right) Posterior Arm
Left (Right) Anterior / Antecubital Elbow
Left (Right) Posterior / Olecranon Elbow
Left (Right) Anterior Forearm
Left (Right) Radial / Lateral Forearm
Left (Right) Ulnar / Medial Forearm
Left (Right) Posterior Forearm
Left (Right) Volar Wrist
Left (Right) Radial / Lateral Wrist
Left (Right) Ulnar / Medial Wrist
Left (Right) Dorsal Wrist
Left (Right) Shoulder – Unspecified
Left (Right) Elbow – Unspecified
Left (Right) Forearm - Unspecified
Left (Right) Wrist - Unspecified
Upper Arm
Right Anterior Shoulder
Right Lateral Shoulder
Right Posterior Shoulder
Right Anterior Arm
Right Lateral Arm
Right Medial Arm
Right Posterior Arm
Right Anterior / Antecubital Elbow
Right Posterior / Olecranon Elbow
Left Anterior Shoulder
Left Lateral Shoulder
Left Posterior Shoulder
Left Anterior Arm
Left Lateral Arm
Left Medial Arm
Left Posterior Arm
Left Anterior / Antecubital Elbow
Left Posterior / Olecranon Elbow
Right Shoulder – Unspecified
Right Elbow – Unspecified
Left Shoulder – Unspecified
Left Elbow – Unspecified
Upper Arm – Left (Right)
Left (Right) Anterior Shoulder
Left (Right) Lateral Shoulder
Left (Right) Posterior Shoulder
Left (Right) Anterior Arm
Left (Right) Lateral Arm
Left (Right) Medial Arm
Left (Right) Posterior Arm
Left (Right) Anterior / Antecubital Elbow
Left (Right) Posterior / Olecranon Elbow
Left (Right) Shoulder – Unspecified
Left (Right) Elbow – Unspecified
Lower Arm without Hand
Right Anterior / Antecubital Elbow
Right Posterior / Olecranon Elbow
Right Anterior Forearm
Right Radial / Lateral Forearm
Right Ulnar / Medial Forearm
Right Posterior Forearm
Right Volar Wrist
Right Radial / Lateral Wrist
Right Ulnar / Medial Wrist
Right Dorsal Wrist
Left Anterior / Antecubital Elbow
Left Posterior / Olecranon Elbow
Left Anterior Forearm
Left Radial / Lateral Forearm
Left Ulnar / Medial Forearm
Left Posterior Forearm
Left Volar Wrist
Left Radial / Lateral Wrist
Left Ulnar / Medial Wrist
Left Dorsal Wrist
Right Elbow – Unspecified
Right Forearm - Unspecified
Right Wrist - Unspecified
Left Elbow – Unspecified
Left Forearm - Unspecified
Left Wrist - Unspecified
Lower Extremity
Lower Arm without Hand – Left (Right)
Left (Right) Anterior / Antecubital Elbow
Left (Right) Posterior / Olecranon Elbow
Left (Right) Anterior Forearm
Left (Right) Radial / Lateral Forearm
Left (Right) Ulnar / Medial Forearm
Left (Right) Posterior Forearm
Left (Right) Volar Wrist
Left (Right) Radial / Lateral Wrist
Left (Right) Ulnar / Medial Wrist
Left (Right) Dorsal Wrist
Left (Right) Elbow – Unspecified
Left (Right) Forearm - Unspecified
Left (Right) Wrist – Unspecified
Shoulder
Right Anterior Shoulder
Right Lateral Shoulder
Right Posterior Shoulder
Left Anterior Shoulder
Left Lateral Shoulder
Left Posterior Shoulder
Left Shoulder – Unspecified
Right Shoulder – Unspecified
Shoulder – Left (Right)
Left (Right) Anterior Shoulder
Left (Right) Lateral Shoulder
Left (Right) Posterior Shoulder
Left (Right) Left Shoulder – Unspecified
Upper Arm (excluding shoulder or elbow)
Right Anterior Arm
Right Lateral Arm
Right Medial Arm
Right Posterior Arm
Left Anterior Arm
Left Lateral Arm
Left Medial Arm
Left Posterior Arm
Upper Arm (excluding shoulder, elbow) – Left (Right)
Left (Right) Anterior Arm
Left (Right) Lateral Arm
Left (Right) Medial Arm
Left (Right) Posterior Arm
Elbow
Right Anterior / Antecubital Elbow
Right Posterior / Olecranon Elbow
Left Anterior / Antecubital Elbow
Left Posterior / Olecranon Elbow
Left Elbow – Unspecified
Right Elbow – Unspecified
Elbow – Left (Right)
Left (Right) Anterior / Antecubital Elbow
Left (Right) Posterior / Olecranon Elbow
Left (Right) Elbow – Unspecified
Forearm
Right Anterior Forearm
Right Radial / Lateral Forearm
Right Ulnar / Medial Forearm
Right Posterior Forearm
Left Anterior Forearm
Left Radial / Lateral Forearm
Left Ulnar / Medial Forearm
Left Posterior Forearm
Left Forearm - Unspecified
Right Forearm – Unspecified
Forearm – Left (Right)
Left (Right) Anterior Forearm
Left (Right) Radial / Lateral Forearm
Left (Right) Ulnar / Medial Forearm
Left (Right) Posterior Forearm
Left (Right) Forearm - Unspecified
Ulnar / Medial / Posterior Forearm
Right Ulnar / Medial Forearm
Right Posterior Forearm
Left Ulnar / Medial Forearm
Left Posterior Forearm
Ulnar / Medial / Posterior Forearm – Left (Right)
Left (Right) Ulnar / Medial Forearm
Left (Right) Posterior Forearm
Radial / Lateral / Anterior Forearm
Right Radial / Lateral Forearm
Right Anterior Forearm
Left Radial / Lateral Forearm
Left Anterior Forearm
Radial / Lateral / Anterior Forearm – Left (Right)
Left (Right) Radial / Lateral Forearm
Left (Right) Anterior Forearm
Wrist
Right Volar Wrist
Right Radial / Lateral Wrist
Right Ulnar / Medial Wrist
Right Dorsal Wrist
Left Volar Wrist
Left Radial / Lateral Wrist
Left Ulnar / Medial Wrist
Left Dorsal Wrist
Left Wrist - Unspecified
Right Wrist - Unspecified
Wrist – Left (Right)
Left (Right) Volar Wrist
Left (Right) Radial / Lateral Wrist
Left (Right) Ulnar / Medial Wrist
Left (Right) Dorsal Wrist
Left (Right) Wrist – Unspecified
Hand
Right Thenar Eminence
Right Hypothenar Eminance
Right Mid-Palmar Hand
Right Lateral Hand
Right Medial Hand
Right Dorsal Hand
Right Palmar Surface of Thumb
Right Lateral Surface of Thumb
Right Medial Surface of Thumb
Right Dorsal Surface of Thumb
Right Palmar Surface of Finger(s)
Right Lateral Surface of Finger(s)
Right Medial Surface of Finger(s)
Right Dorsal Surface of Finger(s)
Left Thenar Eminence
Left Hypothenar Eminance
Left Mid-Palmar Hand
Left Lateral Hand
Left Medial Hand
Left Dorsal Hand
Left Palmar Surface of Thumb
Left Lateral Surface of Thumb
Left Medial Surface of Thumb
Left Dorsal Surface of Thumb
Left Palmar Surface of Finger(s)
Left Lateral Surface of Finger(s)
Left Medial Surface of Finger(s)
Left Dorsal Surface of Finger(s)
Right Hand - Unspecified
Left Hand - Unspecified
Left Palmar Hand
Right Palmar Hand
Hand – Left (Right)
Left (Right) Thenar Eminence
Left (Right) Hypothenar Eminance
Left (Right) Mid-Palmar Hand
Left (Right) Lateral Hand
Left (Right) Medial Hand
Left (Right) Dorsal Hand
Left (Right) Palmar Surface of Thumb
Left (Right) Lateral Surface of Thumb
Left (Right) Medial Surface of Thumb
Left (Right) Dorsal Surface of Thumb
Left (Right) Palmar Surface of Finger(s)
Left (Right) Lateral Surface of Finger(s)
Left (Right) Medial Surface of Finger(s)
Left (Right) Dorsal Surface of Finger(s)
Left (Right) Hand - Unspecified
Left (Right) Palmar Hand
Lower Extremity – Left (Right)
Left (Right) Anterior Thigh
Left (Right) Lateral Thigh
Left (Right) Medial Thigh
Left (Right) Posterior Thigh
Left (Right) Thigh - Unspecified
Left (Right) Anterior / Patellar Knee
Left (Right) Lateral Knee
Left (Right) Medial Knee
Left (Right) Posterior / Popliteal Knee
Left (Right) Knee – Unspecified
Left (Right) Anterior Lower Leg
Left (Right) Lateral Lower Leg
Left (Right) Medial Lower Leg
Left (Right) Posterior Lower Leg
Left (Right) Lower Leg - Unspecified
Left (Right) Anterior Ankle
Left (Right) Lateral Ankle
Left (Right) Medial Ankle
Left (Right) Posterior Ankle
Left (Right) Ankle - Unspecified
Left (Right) Dorsum of Foot
Left (Right) Lateral Foot
Left (Right) Medial Foot
Left (Right) Plantar Foot
Left (Right) Foot - Unspecified
Left (Right) Dorsal Surface of Toe(s)
Left (Right) Lateral Surface of Toe(s)
Left (Right) Medial Surface of Toe(s)
Left (Right) Plantar Surface of Toe(s)
Lower Extremity without Foot
Left Anterior Thigh
Left Lateral Thigh
Left Medial Thigh
Left Posterior Thigh
Left Thigh - Unspecified
Left Anterior / Patellar Knee
Left Lateral Knee
Left Medial Knee
Left Posterior / Popliteal Knee
Left Knee – Unspecified
Left Anterior Lower Leg
Left Lateral Lower Leg
Left Medial Lower Leg
Left Posterior Lower Leg
Left Lower Leg - Unspecified
Left Anterior Ankle
Left Lateral Ankle
Left Medial Ankle
Left Posterior Ankle
Left Ankle - Unspecified
Right Anterior Thigh
Right Lateral Thigh
Right Medial Thigh
Right Posterior Thigh
Right Thigh - Unspecified
Right Anterior / Patellar Knee
Right Lateral Knee
Right Medial Knee
Right Posterior / Popliteal Knee
Right Knee – Unspecified
Right Anterior Lower Leg
Right Lateral Lower Leg
Right Medial Lower Leg
Right Posterior Lower Leg
Right Lower Leg - Unspecified
Right Anterior Ankle
Right Lateral Ankle
Right Medial Ankle
Right Posterior Ankle
Right Ankle – Unspecified
Lower Extremity without Foot – Left (Right)
Left (Right) Anterior Thigh
Left (Right) Lateral Thigh
Left (Right) Medial Thigh
Left (Right) Posterior Thigh
Left (Right) Thigh - Unspecified
Left (Right) Anterior / Patellar Knee
Left (Right) Lateral Knee
Left (Right) Medial Knee
Left (Right) Posterior / Popliteal Knee
Left (Right) Knee – Unspecified
Left (Right) Anterior Lower Leg
Left (Right) Lateral Lower Leg
Left (Right) Medial Lower Leg
Left (Right) Posterior Lower Leg
Left (Right) Lower Leg - Unspecified
Left (Right) Anterior Ankle
Left (Right) Lateral Ankle
Left (Right) Medial Ankle
Left (Right) Posterior Ankle
Left (Right) Ankle - Unspecified
Upper Leg
Left Anterior Thigh
Left Lateral Thigh
Left Medial Thigh
Left Posterior Thigh
Left Thigh - Unspecified
Left Anterior / Patellar Knee
Left Lateral Knee
Left Medial Knee
Left Posterior / Popliteal Knee
Left Knee – Unspecified
Right Anterior Thigh
Right Lateral Thigh
Right Medial Thigh
Right Posterior Thigh
Right Thigh - Unspecified
Right Anterior / Patellar Knee
Right Lateral Knee
Right Medial Knee
Right Posterior / Popliteal Knee
Right Knee – Unspecified
Upper Leg – Left (Right)
Left (Right) Anterior Thigh
Left (Right) Lateral Thigh
Left (Right) Medial Thigh
Left (Right) Posterior Thigh
Left (Right) Thigh - Unspecified
Left (Right) Anterior / Patellar Knee
Left (Right) Lateral Knee
Left (Right) Medial Knee
Left (Right) Posterior / Popliteal Knee
Left (Right) Knee – Unspecified
Lower Leg without Foot
Left Anterior / Patellar Knee
Left Lateral Knee
Left Medial Knee
Left Posterior / Popliteal Knee
Left Knee – Unspecified
Left Anterior Lower Leg
Left Lateral Lower Leg
Left Medial Lower Leg
Left Posterior Lower Leg
Left Lower Leg - Unspecified
Left Anterior Ankle
Left Lateral Ankle
Left Medial Ankle
Left Posterior Ankle
Left Ankle - Unspecified
Right Anterior / Patellar Knee
Right Lateral Knee
Right Medial Knee
Right Posterior / Popliteal Knee
Right Knee – Unspecified
Right Anterior Lower Leg
Right Lateral Lower Leg
Right Medial Lower Leg
Right Posterior Lower Leg
Right Lower Leg - Unspecified
Right Anterior Ankle
Right Lateral Ankle
Right Medial Ankle
Right Posterior Ankle
Right Ankle – Unspecified
Lower Leg w/o Foot – Left (Right)
Left (Right) Anterior / Patellar Knee
Left (Right) Lateral Knee
Left (Right) Medial Knee
Left (Right) Posterior / Popliteal Knee
Left (Right) Knee – Unspecified
Left (Right) Anterior Lower Leg
Left (Right) Lateral Lower Leg
Left (Right) Medial Lower Leg
Left (Right) Posterior Lower Leg
Left (Right) Lower Leg - Unspecified
Left (Right) Anterior Ankle
Left (Right) Lateral Ankle
Left (Right) Medial Ankle
Left (Right) Posterior Ankle
Left (Right) Ankle - Unspecified
Thigh
Left Anterior Thigh
Left Lateral Thigh
Left Medial Thigh
Left Posterior Thigh
Left Thigh - Unspecified
Right Anterior Thigh
Right Lateral Thigh
Right Medial Thigh
Right Posterior Thigh
Right Thigh - Unspecified
Thigh – Left (Right)
Left (Right) Anterior Thigh
Left (Right) Lateral Thigh
Left (Right) Medial Thigh
Left (Right) Posterior Thigh
Left (Right) Thigh - Unspecified
Knee
Left Anterior / Patellar Knee
Left Lateral Knee
Left Medial Knee
Left Posterior / Popliteal Knee
Left Knee – Unspecified
Right Anterior / Patellar Knee
Right Lateral Knee
Right Medial Knee
Right Posterior / Popliteal Knee
Right Knee – Unspecified
Knee – Left (Right)
Left (Right) Anterior / Patellar Knee
Left (Right) Lateral Knee
Left (Right) Medial Knee
Left (Right) Posterior / Popliteal Knee
Left (Right) Knee – Unspecified
Lower Leg
Left Anterior Lower Leg
Left Lateral Lower Leg
Left Medial Lower Leg
Left Posterior Lower Leg
Left Lower Leg - Unspecified
Right Anterior Lower Leg
Right Lateral Lower Leg
Right Medial Lower Leg
Right Posterior Lower Leg
Right Lower Leg - Unspecified
Lower Leg – Left (Right)
Left (Right) Anterior Lower Leg
Left (Right) Lateral Lower Leg
Left (Right) Medial Lower Leg
Left (Right) Posterior Lower Leg
Left (Right) Lower Leg - Unspecified
Ankle
Left Anterior Ankle
Left Lateral Ankle
Left Medial Ankle
Left Posterior Ankle
Left Ankle - Unspecified
Right Anterior Ankle
Right Lateral Ankle
Right Medial Ankle
Right Posterior Ankle
Right Ankle - Unspecified
Ankle – Left (Right)
Left (Right) Anterior Ankle
Left (Right) Lateral Ankle
Left (Right) Medial Ankle
Left (Right) Posterior Ankle
Left (Right) Ankle – Unspecified
Foot/Toes
Left Dorsum of Foot
Left Lateral Foot
Left Medial Foot
Left Plantar Foot
Left Foot - Unspecified
Left Dorsal Surface of Toe(s)
Left Lateral Surface of Toe(s)
Left Medial Surface of Toe(s)
Left Plantar Surface of Toe(s)
Right Dorsum of Foot
Right Lateral Foot
Right Medial Foot
Right Plantar Foot
Right Foot - Unspecified
Right Dorsal Surface of Toe(s)
Right Lateral Surface of Toe(s)
Right Medial Surface of Toe(s)
Right Plantar Surface of Toe(s)
Foot/Toes – Left (Right)
Left Dorsum of Foot
Left Lateral Foot
Left Medial Foot
Left Plantar Foot
Left Foot - Unspecified
Left Dorsal Surface of Toe(s)
Left Lateral Surface of Toe(s)
Left Medial Surface of Toe(s)
Left Plantar Surface of Toe(s)
Footnotes
Conflicts of Interest: None other than the grants listed above
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health 2010. February;100(2):292–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lachs MS, Pillemer K. Elder abuse. Lancet 2004;364:1263–72. [DOI] [PubMed] [Google Scholar]
- 3.Under the radar: New York State Elder Abuse Prevalence Study: Self-Reported Prevalence and Documented Case Surveys 2012. Available at: https://ocfs.ny.gov/main/reports/Under%20the%20Radar%2005%2012%2011%20final%20report.pdf. Accessed on January 18, 2020.
- 4.Dyer CB, Pavlik VN, Murphy KP, Hyman DJ. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc 2000;48:205–8. [DOI] [PubMed] [Google Scholar]
- 5.Dong X, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA internal medicine 2013;173:911–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lachs MS, Williams CS, O’Brien S, Pillemer KA. Adult protective service use and nursing home placement. Gerontologist 2002;42:734–9. [DOI] [PubMed] [Google Scholar]
- 7.Dong X, Simon MA. Association between reported elder abuse and rates of admission to skilled nursing facilities: findings from a longitudinal population-based cohort study. Gerontology 2013;59:464–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lachs MS, Williams CS, O’Brien S, et al. The mortality of elder mistreatment. JAMA 1998;280:428–32. [DOI] [PubMed] [Google Scholar]
- 9.Dong XQ, Simon MA, Beck TT, et al. Elder abuse and mortality: the role of psychological and social wellbeing. Gerontology 2011;57:549–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker MW, LaCroix AZ, Wu C, et al. Mortality risk associated with physical and verbal abuse in women aged 50 to 79. J Am Geriatr Soc 2009;57:1799–809. [DOI] [PubMed] [Google Scholar]
- 11.Pillemer K, Finkelhor D. The prevalence of elder abuse: a random sample survey. Gerontologist 1988;28:51–7. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Elder Abuse. The Elder Justice Roadmap: A Stakeholder Initiative to Respond to an Emerging Health, Justice, Financial, and Social Crisis. Available at: https://www.justice.gov/file/852856/download. Accessed on January 18, 2020. [Google Scholar]
- 13.Mouton CP, Rodabough RJ, Rovi SL, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. Am J Public Health 2004;94:605–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American College of Emergency Physicians. Report on: The Future of Geriatric Care in our Nation’s Emergency Departments: Impact and Implications. 2008. [Google Scholar]
- 15.Roskos ER, Wilber ST. 210: The Effect of Future Demographic Changes on Emergency Medicine. Ann Emerg Med 2006;48:65. [Google Scholar]
- 16.Wilber ST, Gerson LW, Terrell KM, et al. Geriatric emergency medicine and the 2006 Institute of Medicine reports from the Committee on the Future of Emergency Care in the U.S. health system. Acad Emerg Med 2006;13:1345–51. [DOI] [PubMed] [Google Scholar]
- 17.National Research Council. Elder mistreatment: Abuse, neglect and exploitation in an aging America. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 18.Vandeweerd C, Paveza GJ. Verbal mistreatment in older adults:a look at persons with Alzheimer’s disease and their caregivers in the state of Florida. J Elder Abuse Negl 2005;17:11–30. [DOI] [PubMed] [Google Scholar]
- 19.Cooney C, Howard R, Lawlor B. Abuse of vulnerable people with dementia by their carers: can we identify those most at risk? Int J Geriatr Psychiatry 2006;21:564–71. [DOI] [PubMed] [Google Scholar]
- 20.Amstadter AB, Zajac K, Strachan M, et al. Prevalence and correlates of elder mistreatment in South Carolina: the South Carolina elder mistreatment study. J Interpers Violence 2011;26:2947–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy K, Waa S, Jaffer H, et al. A literature review of findings in physical elder abuse. Can Assoc Radiol J 2013;64:10–4. [DOI] [PubMed] [Google Scholar]
- 22.Lachs MS, Williams CS, O’Brien S, et al. ED use by older victims of family violence. Ann Emerg Med 1997;30:448–54. [DOI] [PubMed] [Google Scholar]
- 23.Bond MC, Butler KH. Elder abuse and neglect: definitions, epidemiology, and approaches to emergency department screening. Clin Geriatri Med 2013;29:257–73. [DOI] [PubMed] [Google Scholar]
- 24.Geroff AJ, Olshaker JS. Elder abuse. Emerg Med Clin North Am 2006;24:491–505, ix. [DOI] [PubMed] [Google Scholar]
- 25.Dong X, Simon MA. Association between elder abuse and use of ED: findings from the Chicago Health and Aging Project. Am J Emerg Med 2013;31:693–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedman LS, Avila S, Tanouye K, et al. A case-control study of severe physical abuse of older adults. J Am Geriatr Soc 2011;59:417–22. [DOI] [PubMed] [Google Scholar]
- 27.Heyborne RD. Elder abuse: keeping the unthinkable in the differential. Acad Emerg Med 2007;14:566–7. [DOI] [PubMed] [Google Scholar]
- 28.Chan KL, Choi WM, Fong DY, et al. Characteristics of family violence victims presenting to emergency departments in Hong Kong. J Emerg Med 2013;44:249–58. [DOI] [PubMed] [Google Scholar]
- 29.Stevens TB, Richmond NL, Pereira GF, et al. Prevalence of nonmedical problems among older adults presenting to the emergency department. Acad Emerg Med 2014;21:651–8. [DOI] [PubMed] [Google Scholar]
- 30.Collins KA. Elder maltreatment: a review. Arch Pathol Lab Med 2006;130:1290–6. [DOI] [PubMed] [Google Scholar]
- 31.Collins KA, Presnell SE. Elder neglect and the pathophysiology of aging. Am J Forensic Med Pathol 2007;28:157–62. [DOI] [PubMed] [Google Scholar]
- 32.Collins KA, Sellars K. Vertebral artery laceration mimicking elder abuse. Am J Forensic Med Pathol 2005;26:150–4. [PubMed] [Google Scholar]
- 33.Rosenblatt DE, Cho KH, Durance PW. Reporting mistreatment of older adults: the role of physicians. J Am Geriatri Soc 1996;44:65–70. [DOI] [PubMed] [Google Scholar]
- 34.Baldwin K, Pandya NK, Wolfgruber H, et al. Femur fractures in the pediatric population: abuse or accidental trauma? Clin Orthop Relat Res 2011;469:798–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pandya NK, Baldwin K, Wolfgruber H, et al. Child abuse and orthopaedic injury patterns: analysis at a level I pediatric trauma center. J Pediatr Orthop 2009;29:618–25. [DOI] [PubMed] [Google Scholar]
- 36.Kemp AM, Dunstan F, Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ 2008;337:a1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maguire S, Pickerd N, Farewell D, et al. Which clinical features distinguish inflicted from non-inflicted brain injury? a systematic review. Arch Dis Child 2009;94:860–7. [DOI] [PubMed] [Google Scholar]
- 38.Piteau SJ, Ward MG, Barrowman NJ, et al. Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systematic review. Pediatrics 2012;130:315–23. [DOI] [PubMed] [Google Scholar]
- 39.Maguire S, Mann MK, Sibert J, et al. Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Arch Dis Child 2005;90:182–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maguire S, Mann M. Systematic reviews of bruising in relation to child abuse-what have we learnt: an overview of review updates. Evid Based Child Health 2013;8:255–63. [DOI] [PubMed] [Google Scholar]
- 41.Sugar NF, Taylor JA, Feldman KW. Bruises in infants and toddlers: those who don’t cruise rarely bruise. Puget Sound Pediatric Research Network. Arch Pediatr Adolesc Med 1999;153:399–403. [DOI] [PubMed] [Google Scholar]
- 42.Valvano TJ, Binns HJ, Flaherty EG, et al. Does bruising help determine which fractures are caused by abuse? Child Maltreat 2009;14:376–81. [DOI] [PubMed] [Google Scholar]
- 43.Pierce MC, Kaczor K, Aldridge S, et al. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics 2010;125:67–74. [DOI] [PubMed] [Google Scholar]
- 44.Kemp AM, Joshi AH, Mann M, et al. What are the clinical and radiological characteristics of spinal injuries from physical abuse: a systematic review. Arch Dis Child 2010;95:355–60. [DOI] [PubMed] [Google Scholar]
- 45.Maguire S, Moynihan S, Mann M, et al. A systematic review of the features that indicate intentional scalds in children. Burns 2008;34:1072–81. [DOI] [PubMed] [Google Scholar]
- 46.Daria S, Sugar NF, Feldman KW, et al. Into hot water head first: distribution of intentional and unintentional immersion burns. Pediatr Emerg Care 2004;20:302–10. [DOI] [PubMed] [Google Scholar]
- 47.Maguire SA, Upadhyaya M, Evans A, et al. A systematic review of abusive visceral injuries in childhood--their range and recognition. Child Abuse Negl 2013;37:430–45. [DOI] [PubMed] [Google Scholar]
- 48.Kurrle S. Elder abuse. Aust Fam Physician 2004;33:807–12. [PubMed] [Google Scholar]
- 49.Yaffe MJ, Tazkarji B. Understanding elder abuse in family practice. Can Fam Physician 2012;58:1336–40, e695–8. [PMC free article] [PubMed] [Google Scholar]
- 50.Liao S, Mosqueda L. Physical abuse of the elderly: the medical director’s response. J Am Med Dir Assoc 2006;7:242–5. [DOI] [PubMed] [Google Scholar]
- 51.Bird PE, Harrington DT, Barillo DJ, et al. Elder abuse: a call to action. J Burn Care Rehabil 1998;19:522–7. [DOI] [PubMed] [Google Scholar]
- 52.Palmer M, Brodell RT, Mostow EN. Elder abuse: dermatologic clues and critical solutions. J Am Acad Dermatol 2013;68:e37–42. [DOI] [PubMed] [Google Scholar]
- 53.Chen AL, Koval KJ. Elder abuse: the role of the orthopaedic surgeon in diagnosis and management. J Am Acad Orthop Surg 2002;10:25–31. [DOI] [PubMed] [Google Scholar]
- 54.Senn DR, McDowell JD, Alder ME. Dentistry’s role in the recognition and reporting of domestic violence, abuse, and neglect. Dent Clin North Am 2001;45:343–63, ix. [PubMed] [Google Scholar]
- 55.Golden GS. Forensic odontology and elder abuse--a case study. J Calif Dent Assoc 2004;32:336–40. [PubMed] [Google Scholar]
- 56.Cowen HJ, Cowen PS. Elder mistreatment: dental assessment and intervention. Spec Care Dentist 2002;22:23–32. [DOI] [PubMed] [Google Scholar]
- 57.Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc 2009;57:1191–6. [DOI] [PubMed] [Google Scholar]
- 58.Ziminski CE, Wiglesworth A, Austin R, et al. Injury patterns and causal mechanisms of bruising in physical elder abuse. J Forensic Nurs 2013;9:84–91; quiz E1–2. [DOI] [PubMed] [Google Scholar]
- 59.Rosen T, Bloemen EM, LoFaso VM, et al. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. J Emerg Med 2016;50(3):518–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ziminski CE, Phillips LR, Woods DL. Raising the index of suspicion for elder abuse: cognitive impairment, falls, and injury patterns in the emergency department. Geriatr Nurs 2012;33:105–12. [DOI] [PubMed] [Google Scholar]
- 61.Sheets LK, Leach ME, Koszewski IJ, et al. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics 2013;131:701–7. [DOI] [PubMed] [Google Scholar]
- 62.von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. BMJ 2007;20:806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention. Elder Abuse: Definitions. Available at: https://www.cdc.gov/violenceprevention/elderabuse/definitions.html. Accessed on January 18, 2020.
- 64.Braitman LE, Davidoff F. Predicting clinical states in individual patients. Ann Intern Med 1996;125:406–12. [DOI] [PubMed] [Google Scholar]
- 65.Hollander JE, Singer AJ. An innovative strategy for conducting clinical research: the academic associate program. Acad Emerg Med 2002;9:134–7.67. [DOI] [PubMed] [Google Scholar]
- 66.Bloemen EM, Rosen T, Cline Schiroo JA, et al. Photographing injuries in the acute care setting: development and evaluation of a standardized protocol for research, forensics, and clinical practice. Acad Emerg Med 2016;23(5):653–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yaffe MJ, Wolfson C, Lithwick M, et al. Development and validation of a tool to improve physician identification of elder abuse: the Elder Abuse Suspicion Index (EASI). J Elder Abuse Negl 2008;20:276–300. [DOI] [PubMed] [Google Scholar]
- 68.Fulmer T, Paveza G, Vandeweerd C, et al. Neglect assessment in urban emergency departments and confirmation by an expert clinical team. J Gerontol A Biol Sci Med Sci 2005;60:1002–6. [DOI] [PubMed] [Google Scholar]
- 69.Rosen T, Clark S, Bloemen EM, et al. Geriatric assault victims treated at U.S. trauma centers: five-year analysis of the national trauma data bank. Injury 2016;47(12):2671–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shepherd JP, Al-Kotany MY, Subadan C, et al. Assault and facial soft tissue injuries. Br J Plast Surg 1987;40:614–9. [DOI] [PubMed] [Google Scholar]
- 71.Shepherd JP, Shapland M, Pearce NX, et al. Pattern, severity and aetiology of injuries in victims of assault. J R Soc Med 1990;83:75–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Le BT, Dierks EJ, Ueeck BA, et al. Maxillofacial injuries associated with domestic violence. J Oral Maxillofac Surg 2001;59:1277–83; discussion 83–4. [DOI] [PubMed] [Google Scholar]
- 73.Kemp AM, Maguire SA, Nuttall D, et al. Bruising in children who are assessed for suspected physical abuse. Arch Dis Child 2014;99:108–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J 2017;68(1):16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Green SM. When do clinical decision rules improve patient care? Ann Emerg Med 2013;62:132–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.