Abstract
Simple Summary
Brain metastases (BM) from colorectal cancer (CRC) are rare. There is little available information regarding incidence, risk factors, prognostic factors, treatment, and overall survival (OS). In this systematic review we performed a research of the current literature and exposed an average incidence of 2.10%. The most-reported risk factors for developing BM were KRAS mutations and lung metastases. The majority of patients with brain metastases did not show neurological symptoms. Treatment options included surgery, radiation, or chemotherapy. While patients who received surgery had prolonged survival, the best survival time was found with a multimodality treatment regimen including neurosurgery.
Abstract
Colorectal cancer (CRC) is the third most common malignancy worldwide. Most patients with metastatic CRC develop liver or lung metastases, while a minority suffer from brain metastases. There is little information available regarding the presentation, treatment, and overall survival of brain metastases (BM) from CRC. This systematic review and meta-analysis includes data collected from three major databases (PubMed, Cochrane, and Embase) based on the key words “brain”, “metastas*”, “tumor”, “colorectal”, “cancer”, and “malignancy”. In total, 1318 articles were identified in the search and 86 studies matched the inclusion criteria. The incidence of BM varied between 0.1% and 11.5%. Most patients developed metastases at other sites prior to developing BM. Lung metastases and KRAS mutations were described as risk factors for additional BM. Patients with BM suffered from various symptoms, but up to 96.8% of BM patients were asymptomatic at the time of BM diagnosis. Median survival time ranged from 2 to 9.6 months, and overall survival (OS) increased up to 41.1 months in patients on a multimodal therapy regimen. Several factors including age, blood levels of carcinoembryonic antigen (CEA), multiple metastases sites, number of brain lesions, and presence of the KRAS mutation were predictors of OS. For BM diagnosis, MRI was considered to be state of the art. Treatment consisted of a combination of surgery, radiation, or systemic treatment.
Keywords: brain metastases, cerebral metastases, BM, colorectal cancer, CRC, systematic review, meta-analysis
1. Introduction
Colorectal cancer (CRC) is the third most common type of malignant tumor worldwide, and in 2018, 880,792 deaths were reported due to CRC worldwide [1]. The incidence of CRC increases in an age-dependent manner, with the average age being 72–76 years at diagnosis [2]. Men are more frequently affected than women (23.6 cases vs. 16.3 cases per 100,000) [3]. Approximately 25% of patients present with distant metastases at time of diagnosis and another 25% will suffer from metastases further on [4]. Hepatic and pulmonary metastases are most common, while fewer patients develop brain metastases (BM). To date, there are standardized therapeutic pathways for the treatment of hepatic and pulmonary metastases which recommend surgical resection if complete resection is achievable. If the complete resection of metastases is not a therapeutic option, neoadjuvant chemotherapy is recommended with re-evaluation for surgery later on [5]. As BM are rare, there is a lack of data regarding management, with no guidelines for patients suffering from BM. Moreover, there seems to be a critical lack of information on presentation, treatment, and overall survival (OS) with regard to BM from CRC.
The aim of this systematic literature review and meta-analysis is to evaluate the incidence, common symptoms, overall survival, risk factors, and treatment strategies for BM due to CRC. Furthermore, based on the current literature we propose a clinical guideline for screening and treatment of BM from CRC.
2. Methods
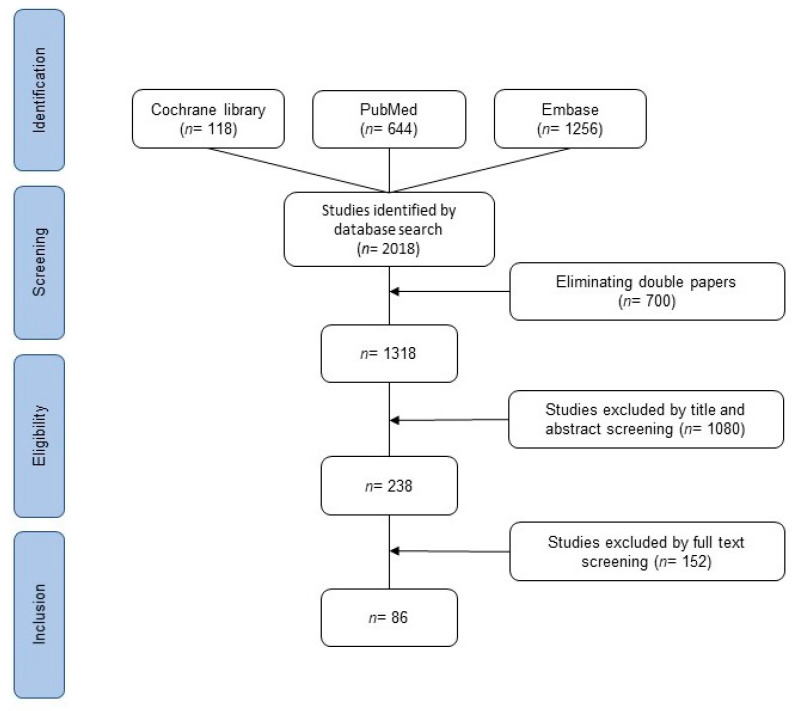
We searched PubMed database, Embase database, and Cochrane database on 30 November 2020. All types of studies published between 1 January 2000 and 30 November 2020 were included. Studies with available abstracts in German or English were included. Search terms included “brain”, “metastas*”, “tumor”, “colorectal”, “cancer”, and “malignancy” using “and” or “or”. All patients with BM from CRC were included in the analyses. Duplicates were automatically removed by the literature organization program in addition to manual control. Two independent reviewers (SM, FK) performed the screening of titles and abstracts of all studies. Potentially relevant articles were reviewed in full to determine eligibility for inclusion. Any disagreement on manuscripts was discussed and solved by consensus. The selection process can be seen in the PRISMA (TRANSPARENT REPORTING of SYSTEMATIC REVIEWS and META-ANALYSES) flowchart (Figure 1) [6]. In the case that two studies examined the same study population, the more recent study was included. The literature organization was performed with Endnote20. Charts and tables were created with Microsoft Word, Microsoft PowerPoint, and RevMan5. Statistical analysis was performed with SPSS26 and RevMan5. As a measure of effects, the odds ratio (OR) with the corresponding 95% confidence interval (95%CI) was calculated. Statistical heterogeneity was assessed by calculating the chi2 and I2 statistics.
Figure 1.
PRISMA flowchart of the search strategy.
3. Results
The database search identified 2018 articles. After removing duplicates, 1318 articles were left for further investigation. After screening by title and abstract for suitability, 328 manuscripts were left. Articles were read in full text to check for inclusion criteria. Eighty-six papers matched the inclusion criteria and were used to perform the meta-analysis. None of these were randomized controlled trials (RCTs), as they mostly involved retrospective analyses. Articles were grouped in different categories to perform the meta-analysis (Table 1).
Table 1.
Categories and numbers of articles that matched the regarding category (numerous articles matched more than one category). OS: overall survival; BM: bone metastases.
| Category | Articles Found |
|---|---|
| Incidence | 21 |
| Symptoms | 7 |
| Diagnosis | 4 |
| Risk factors for developing BM | 17 |
| Overall survival | 43 |
| Factors for poor OS | 25 |
| Treatment modalities | 18 |
3.1. Incidence
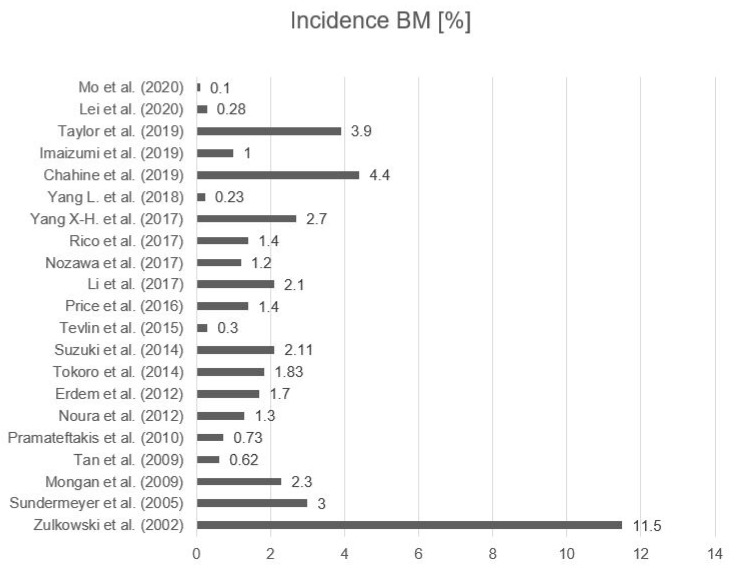
We identified 21 studies that reported on the incidence of BM due to CRC. Overall, 541,244 CRC cases were included, involving 1547 patients diagnosed with BM [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]. The overall average incidence of BM in CRC patients was 2.10% (95%CI 0.98–3.22) ranging from 0.1% up to 11.5% [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. Fifty-seven percent of patients were male and 43% were female (Figure 2 and Table 2). Two studies focused on subgroup analysis and are not included in the overall evaluation of incidence. In patients with metastatic CRC, Shindorf et al. described a BM incidence of 14.6% [28]. McGovern et al. divided patients into ethic subgroups and discovered an incidence of 7% in their Asian subpopulation, while other ethnicities had an incidence ranging from 0.6% to 3.2% [29].
Figure 2.
Incidence of BM (%) in all patients suffering from colorectal cancer (CRC) [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. The overall average incidence of BM in CRC patients was 2.10% (95% confidence interval (CI) 0.98–3.22).
Table 2.
Incidence and age distribution of patients with BM in included studies that reported on the number of patients with CRC, the number of patients with BM, the incidence of BM due to CRC, and percentage of male/female BM patients with BM [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. * only the abstract was available.
| Study | Number of CRC Patients | Number of BM Patients | Incidence (%) | Men | Women |
|---|---|---|---|---|---|
| Mo et al. (2020) | 142,343 | 122 | 0.1 | - | - |
| Lei et al. (2020) | 192,923 | 532 | 0.28 | - | - |
| Taylor et al. (2019) | 1346 | 52 | 3.9 | 52% | 48% |
| Imaizumi et al. (2019) | 7147 | 68 | 1 | 63% | 25% |
| Chahine et al. (2019) * | 538 | 24 | 4.4 | - | - |
| Yang L. et al. (2018) | 170,793 | 401 | 0.23 | 51% | 49% |
| Yang X.-H. et al. (2017) * | 1104 | 30 | 2.7 | - | - |
| Rico et al. (2017) | 4100 | 59 | 1.4 | 49% | 51% |
| Nozawa et al. (2017) | 2238 | 23 | 1.2 | - | - |
| Li et al. (2017) * | 1714 | 36 | 2.1 | 58% | 42% |
| Price et al. (2016) | 4100 | 59 | 1.4 | 49% | 51% |
| Tevlin et al. (2015) | 4219 | 11 | 0.3 | - | - |
| Suzuki et al. (2014) | 5345 | 113 | 2.11 | - | - |
| Tokoro et al. (2014) | 1364 | 25 | 1.83 | 52% | 48% |
| Erdem et al. (2012) | 878 | 15 | 1.7 | - | - |
| Noura et al. (2012) | 2299 | 29 | 1.3 | 79% | 21% |
| Pramateftakis et al. (2010) | 670 | 5 | 0.73 | - | - |
| Tan et al. (2009) | 4378 | 27 | 0.62 | 52% | 48% |
| Mongan et al. (2009) | 1620 | 39 | 2.3 | 54% | 46% |
| Sundermeyer et al. (2005) | 1020 | 33 | 3.2 | - | - |
| Zullkowskie et al. (2002) | 113 | 13 | 11.5 | - | - |
| Total | 550,252 | 1716 | 2.10 | 57% | 43% |
3.2. Symptoms
Six studies described symptoms in patients with BM from CRC. The initial symptoms of brain metastases were highly variable and were mostly not described in further detail. The most commonly reported symptoms were epileptic seizures, signs of increased intracranial pressure, or neurological symptoms [30,31,32,33,34,35]. Some patients did not show any symptoms at the time of diagnosis (Table 3). While Berghoff et al. found a ratio of 96.8% of asymptomatic patients, Kim D. et al. described only 5.3% of patients as being without symptoms [31,34]. Shindorf et al. performed a study that screened patients with metastatic CRC for BM, regardless of whether neurological symptoms were present. They showed that 76% of the patients with BM were asymptomatic [28].
Table 3.
Clinical characteristics of BM in studies analyzing asymptomatic patients with BM from CRC [28,30,31,32,33,34,35] (° no information about asymptomatic patients).
| Study | Number of BM Patients | Number and % of Asymptomatic Patients | Number and % with Epileptic Seizures |
|---|---|---|---|
| Berghoff et al. (2016) | 224 | 210 (96.8%) | 36 (14.6%) |
| Kim D. et al. (2018) | 19 | 1 (5.3%) | 1 (5.3%) |
| Shindorf et al. (2020) | 25 | 19 (76%) | - |
| Goto et al. (2014) | - | - | - |
| Nemec et al. (2017) | - | - | - |
| Hassan et al. (2018) | - | - | - |
| Total | 268 | 230 (85.8%) | - |
3.3. Diagnostic Techniques
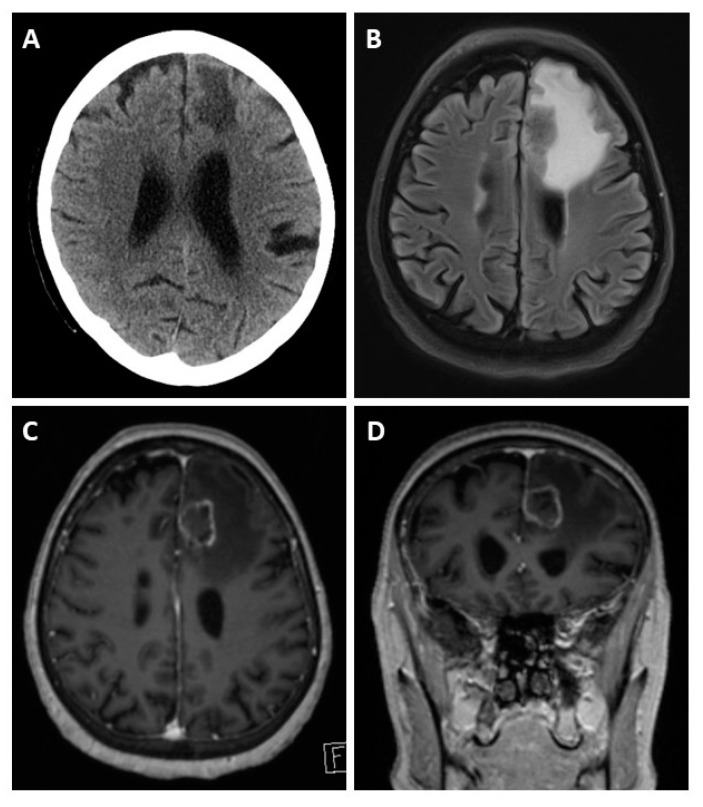
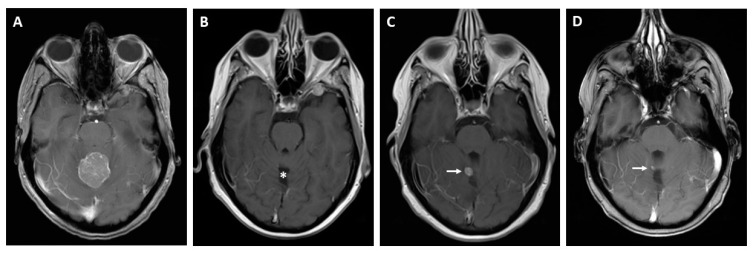
Possible imaging modalities for diagnosis of BM are CT, MRI, or PET-CT. FDG-PET-CT is commonly performed as a whole-body examination, in which BM can appear as an incidental finding. Screening for BM is usually performed with cranial MRI [36]. We identified two studies that compared whole-body PET-CT to whole-body MRI to detect metastases from CRC. In these studies, PET-CT was superior for identifying lymph node metastases, for example locoregional to the primary tumor, whereas MRI was superior for detecting lesions of <1cm, especially BM [37,38]. As even smaller lesions and a meningeal carcinomatosis can be missed by imaging, diagnostic spinal fluid examination is proposed to identify tumor cells or DNA [39,40] (see Figure 3).
Figure 3.
Cerebral CT and MRI scans of a patient with BM, a 62-year-old patient presenting with left frontal edema in computed tomography (A). The MRI scan reveals the actual extent of the edema in the fluid-attenuated inversion recovery (FLAIR) sequence (B). T1-weighted gadolinium post-contrast images in the axial (C) and coronal (D) orientation reveal causative left-frontal CRC metastasis.
3.4. Prognostic Factors
3.4.1. Overall
Nineteen studies depicted risk factors for developing BM; these studies are listed in Table 4. The majority of studies described an association of BM with lung metastases (LM) [13,21,22,41,42,43,44,45,46,47] or KRAS mutations [45,48,49,50,51]. Three studies reported that multiple extra cerebral metastases were related to the developing BM. Besides LM, bone metastases in particular were described as a risk factor [8,47,52,53]. Mo et al. and Yang X.-H. et al. identified a positive carcinoembryonic antigen (CEA) level as a risk factor for developing BM [7,13]. The primary CRC side might also have an association with an increased risk of developing BM. Prasanna et al., Yang X.-H. et al., and Christensen et al. reported a higher association between rectal cancer and BM [13,41,53]. Liu et al. described a correlation between KRAS mutations as well as BRAF mutations and BM, while Lee et al. depicted an association between ALK-translocation and BM [48,49]. In 2009 Mongan et al. described an association between BM development and chemokine receptor type 4 (CXCR4) [21].
Table 4.
Risk factors for developing BM. UICC: Union internationale contre le cancer; TNM: TNM classification; CEA: carcinoembryogenic antigen; CXCR4: chemokine receptor type 4 [7,8,13,21,22,29,41,42,43,44,45,46,47,48,49,50,51,52,53]. * only the abstract was available.
| CEA Level | Staging (TNM or UICC) |
Multiple Extra-Cerebral Metastases | Location of CRC | Bone Metastases | Lung Metastases | KRAS | Others | |
|---|---|---|---|---|---|---|---|---|
| Mo et al. (2020) | x | High N or High T | ||||||
| Lei et al. (2020) | UICC > III | x | ||||||
| Thurmaier et al. (2020) | UICC IV | x | x | x | ||||
| McGovern et al. (2019) * | Asian ethnicity | |||||||
| Prasanna et al. (2018) | Rectal cancer | x | ||||||
| Roussille et al. (2018) | x | x | ||||||
| Liu et al. (2018) | x | BRAF | ||||||
| Lee et al. (2017) * | x | ALK | ||||||
| Yang X.-H. et al. (2017) * | x | Rectal cancer | x | |||||
| Christensen et al. (2016) | Rectal cancer | x | ||||||
| Qiu et al. (2015) | x | |||||||
| Casagrande et al. (2015) | x | |||||||
| Yaeger et al. (2015) | x | |||||||
| Chang et al. (2015) * | x | |||||||
| Tanriverdi et al. (2014) * | x | |||||||
| Zoratto et al. (2013) * | x | x | ||||||
| Dhingani et al. (2012) * | UICC IV | x | x | |||||
| Mongan et al. (2009) | Left-sided CRC | x | CXCR4 | |||||
| Sundermeyer et al. (2005) | x |
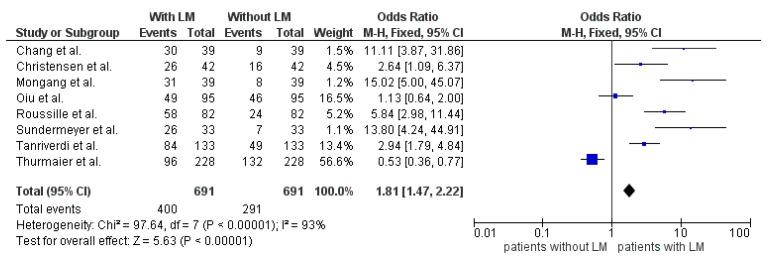
3.4.2. Lung Metastases
Eleven studies evaluated LM as a risk factor for developing brain metastases and reported a positive correlation (Table 5). In three of these studies only the abstracts were available but no full-text manuscripts. Eight studies were available in full text and are summarized in Figure 4. Altogether, 691 patients were examined. Of these patients, 400 had LM at diagnosis of BM, leaving 291 without LM at diagnosis of BM. The odds ratio was 1.81 (95%CI 1.47–2.22). Furthermore, a statistically significant difference was seen between the two groups (p <0.00001). The high heterogeneity may be caused by the small study populations (Figure 4).
Table 5.
Number of BM patients with and without lung metastases (LM) in association with BM patients. * only the abstract was available [13,21,22,41,42,43,44,45,46,47,52].
| Number of CRC Patients | Number of BM Patients | Number and % of BM and LM | Number and % of BM, no LM | Number of LM Patients |
|
|---|---|---|---|---|---|
| Thurmaier et al. (2020) | - | 228 | 96 (42.1%) | 132 (57.9%) | - |
| Roussille et al. (2018) | - | 82 | 58 (72%) | 24 (28%) | - |
| Yang X.-H. et al. (2017) * | 1104 | 30 | - | - | - |
| Christensen et al. (2016) | 480 | 42 | 26 (62%) | 16 (38%) | 156 |
| Qiu et al. (2015) | 46,027 | 95 | 49 (51.6%) | 46 (48.4%) | 1750 |
| Chang et al. (2015) * | - | 39 | 30 (76.9%) | 9 (23.1%) | - |
| Tanriverdi et al. (2014) * | 4864 | 133 | 84 (74%) | 49 (26%) | - |
| Zoratto et al. (2013) * | 623 | 26 | - | - | - |
| Dhingani et al. (2012) * | 301 | 52 | - | - | - |
| Mongang et al. (2009) | 1620 | 39 | 31 (78%) | 8 (22%) | - |
| Sundermeyer et al. (2005) | 1020 | 33 | 26 (78.8%) | 7 (21.2%) | 422 |
| Total | 56,039 | 799 | - | - | 2328 |
Figure 4.
Forest plot comparison of BM patients with LM and without LM.
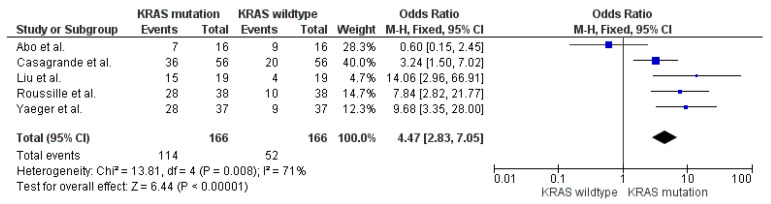
3.4.3. KRAS Mutation
In five studies KRAS mutation was investigated as a risk factor for developing BM (Table 6). In one of them only the abstract was available. Five studies which reported on the KRAS mutation status of BM patients are shown in Figure 5. A total of 166 patients had a KRAS mutation analysis. In total, 114 patients with BM had a KRAS mutation (68%) and 52 patients had a KRAS wild-type (32%). The odds ratio was 4.47 (95%CI 2.83–7.05). The overall effect showed a significant difference (p <0.00001). The high heterogeneity may be caused by the small study populations (Figure 5).
Table 6.
Number of BM patients with KRAS mutation and KRAS wild-type in association with BM patients. * only the abstract was available [45,48,49,50,51,54].
| Number of CRC Patients | Number of BM Patients | Number and % of BM + KRAS Mutations | Number and % of BM + KRAS Wild-Type | |
|---|---|---|---|---|
| Abo et al. (2019) * | - | 16 | 7 (43.7%) | 9 (56.3%) |
| Roussile et al. (2018) | - | 38 | 28 (74%) | 10 (26%) |
| Liu et al. (2018) | 461 | 19 | 15 (78.9%) | 4 (21.1%) |
| Lee et al. (2017) * | - | 11 | - | - |
| Yaeger et al. (2015) | - | 37 | 28 (75.7%) | 9 (24.3%) |
| Casagrande et al. (2015) | - | 56 | 36 (64.3%) | 20 (35.7%) |
Figure 5.
Forest plot comparison of BM patients with KRAS mutation and KRAS wild-type.
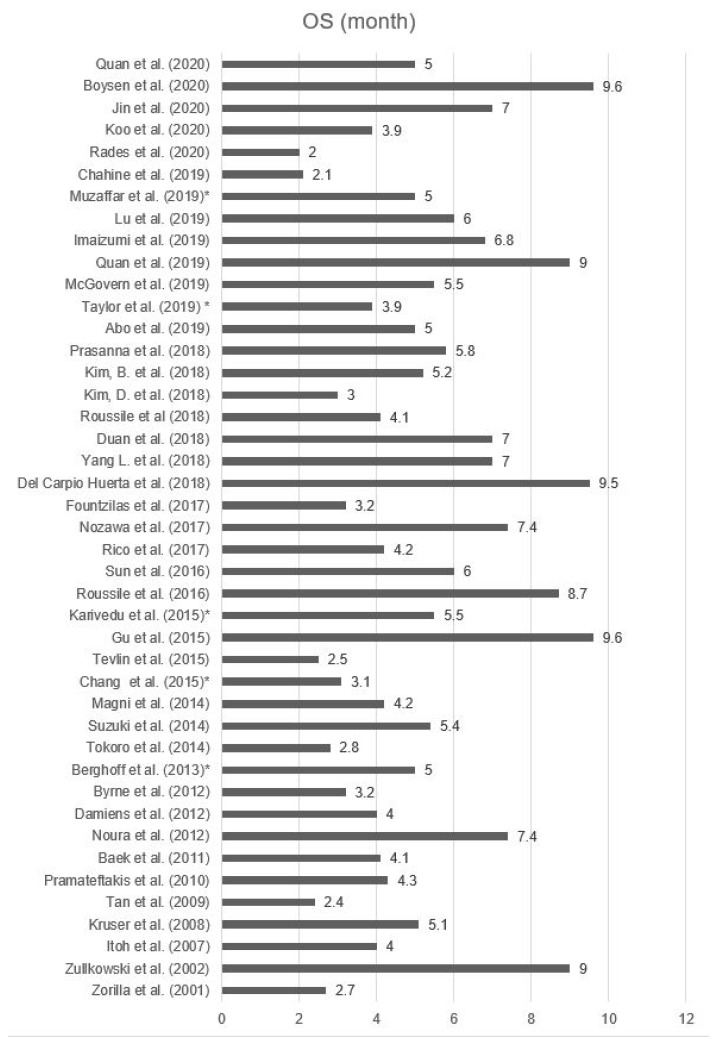
3.5. Survival
In 43 studies an overall survival (OS) with a range from 2 to 9.6 month from the time of BM diagnosis was determined. The median OS was 5.3 months (95%CI 4.6–5.9). In total there were 3611 patients with BM that were included in the OS analysis. The smallest study population reported on five patients, while the largest study included 475 patients with BM. The analyzed studies are shown in Figure 6 and Table 7 [9,10,11,12,14,15,18,20,23,24,25,26,27,29,34,45,46,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78].
Figure 6.
OS of patients with BM [9,10,11,12,14,18,20,23,24,25,26,27,29,34,45,46,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78]. * only the abstract was available.
Table 7.
Study characteristics and OS. Studies reported OS in months, the number of patients with CRC, and the number of patients with BM from CRC [9,10,11,12,14,18,20,23,24,25,26,27,29,34,45,46,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78]. *only the abstract was available.
| OS (Months) | Number of CRC Patients | Number of BM Patients | |
|---|---|---|---|
| Quan et al. (2020) | 5 | - | 371 |
| Boysen et al. (2020) | 9.6 | 38,131 | 235 |
| Jin et al. (2020) * | 7 | >30,000 | 104 |
| Koo et al. (2020) | 3.9 | - | 106 |
| Rades et al. (2020) | 2 | - | 57 |
| Chahine et al. (2019) * | 2.1 | 538 | 24 |
| Muzaffar et al. (2019) * | 5 | - | 475 |
| Lu et al. (2019) | 6 | - | 80 |
| Imaizumi et al. (2019) | 6.8 | 7147 | 68 |
| Quan et al. (2019) | 9 | - | 52 |
| McGovern et al. (2019) * | 5.5 | 76 | 5 |
| Taylor et al. (2019) * | 3.9 | - | 52 |
| Abo et al. (2019) * | 5 | - | 16 |
| Prasanna et al. (2018) | 5.8 | 5967 | 109 |
| Kim B. et al. (2018) * | 5.2 | - | 107 |
| Kim D. et al. (2018) | 3 | - | 19 |
| Roussile et al. (2018) | 4.1 | - | 82 |
| Duan et al. (2018) | 7 | - | 78 |
| Yang L. et al. (2018) | 7 | 170,793 | 401 |
| Del Carpio Huerta et al. (2018) | 9.5 | - | 28 |
| Fountzilas et al. (2017) | 3.2 | - | 40 |
| Nozawa et al. (2017) | 7.4 | 2238 | 23 |
| Rico et al. (2017) | 4.2 | 4100 | 59 |
| Sun et al. (2016) * | 6 | - | 45 |
| Roussile et al. (2016) * | 8.7 | - | 135 |
| Karivedu et al. (2015) * | 5.5 | - | 94 |
| Gu et al. (2015) | 9.6 | - | 93 |
| Tevlin et al. (2015) | 2.5 | 4219 | 11 |
| Chang et al. (2015) * | 3.1 | - | 39 |
| Magni et al. (2014) | 4.2 | - | 41 |
| Suzuki et al. (2014) | 5.4 | 5345 | 113 |
| Tokoro et al. (2014) | 28 | 1364 | 25 |
| Berghoff et al. (2013) * | 5 | - | 69 |
| Byrne et al. (2012) | 3.2 | 1304 | 52 |
| Damiens et al. (2012) | 4 | - | 48 |
| Noura et al. (2012) | 7.4 | 2299 | 29 |
| Baek et al. (2011) | 4.1 | - | 118 |
| Pramateftakis et al. (2010) | 4.3 | 670 | 5 |
| Tan et al. (2009) | 2.4 | 4378 | 27 |
| Kruser et al. (2008) | 5.1 | - | 49 |
| Itoh et al. (2007) | 4 | - | 5 |
| Zullkowski et al. (2002) | 9 | 113 | 13 |
| Zorilla et al. (2001) | 2.7 | - | 9 |
| Total | 5.3 | >278,682 | 3611 |
Twenty-five studies investigated factors of poor OS in patients with BM (Table 8). The most common factors were advanced age, low Karnofsky performance status (KPS), and extracranial metastases, as well as multiple BM. Four studies described a significant reduction in OS in patients with advanced age. Two studies did not report the exact OS. Duan et al. (>65 years: 4 months; <65 years: 10 months) and Quan et al. (>60 years: 4 months; <60 years: 8 months) described a survival benefit from 4 to 6 months [7,55,57,64]. Five studies evaluated KPS as a risk factor for poor OS. Two studies did not provide further specification on the OS. Lu et al. (KPS >70: 11 months; KPS <70: 4 months), Quan et al. (KPS >70: 7 months; KPS <70: 3 months), and Sun et al. (KPS >70: 2 months; KPS <70: 8 months) reported a survival benefit of 4–7 months [10,61,62,67,69]. Twelve studies investigated extracranial metastases as a prognostic factor for OS. Four did not report the exact OS. Three focused on a specific metastatic site and five evaluated extracranial metastases in general; these included the studies by Quan et al. (2020) (extracranial metastases: 4 months; no extracranial metastases: 6 months), Quan et al. (2019) (extracranial metastases: 7 months; no extracranial metastases: 28 months), Del Carpio Huerta et al. (extracranial metastases: 7.2 months; no extracranial metastases: 20.9 months), Gu et al. (extracranial metastases: 7 months; no extracranial metastases: 13 months), and Noura et al. (extracranial metastases: 8 months; no extracranial metastases: 24 months) [7,9,12,27,45,46,52,55,62,64,65,70]. Eleven studies reported multiple BM as a risk factor for poor OS. Four manuscripts did not provide the exact OS. Four studies compared one BM with more than one BM, those of Lu et al. (1: 9 months; >1: 5 months), Roussile et al. (2018) (1: 6.3 months, >1: 3.1 months), Roussile et al. (2016) (1: 12.3 months; >1: 4,9 months), and Gu et al. (1: 10 months; >1: 6 months). Duan et al. (1–2: 10 months; >2: 4 months), Sun et al. (1–2: 8 months; >2: 4 months), and Imaizumi et al. (1–3: 8.8 months; >3: 3.1 months) implemented different cut-offs [7,10,45,57,61,64,67,68,69,70,72]. Three studies reported that a positive CEA level was associated with a poor OS, but only Quan et al. reported a survival benefit of 3 months in patients with negative CEA levels [7,27,55].
Table 8.
Factors for poor OS [7,9,10,12,27,45,46,52,55,56,57,59,60,61,62,63,64,65,67,68,69,70,72,82,83]. * only the abstract was available. KPS: Karnofsky performance status.
| Positive CEA level | Low KPS |
Extracranial Metastases | Multiple BM | Age | Location of CRC | Others | Score | |
|---|---|---|---|---|---|---|---|---|
| Thurmaier et al. (2020) | Liver | |||||||
| Quan et al. (2020) | x | x | x | x | ||||
| Mo et al. (2020) | x | x | x | x | x | |||
| Boysen et al. (2020) | N2 | |||||||
| Jin et al. (2020) * | x | x | ||||||
| Rades et al. (2020) | x | |||||||
| Muzaffar et al. (2019) * | x | |||||||
| Lu et al. (2019) | x | x | ||||||
| Imaizumi et al. (2019) | x | x | History of chemotherapy | |||||
| Quan et al. (2019) | x | x | ||||||
| Taylor et al. (2019) * | Liver | |||||||
| Kim B. et al. (2018) * | x | |||||||
| Roussile et al. (2018) | Lung | x | PDL1+ | |||||
| Duan et al. (2018) | Bone | x | x | |||||
| Yang L. et al. (2018) | x | x | Pathology | |||||
| Del Carpio Huerta et al. (2018) | x | x | ||||||
| Berghoff et al. (2017) * | x | |||||||
| Sun et al. (2016) * | x | x | ||||||
| Nieder et al. (2016) | x | |||||||
| Roussile et al. (2016) * | x | |||||||
| Karivedu et al. (2015) * | x | x | ||||||
| Gu et al. (2015) | x | x | ||||||
| Chang et al. (2015) * | x | KRAS mutation | ||||||
| Berghoff et al. (2013) * | x | x | ||||||
| Noura et al. (2012) | x | x |
Other reported risk factors for poor OS are the site of the primary tumor, N2 lymph node status, history of chemotherapy for the initial CRC, and association between the histological type. Chang et al. reported an association between poor OS and KRAS mutation (KRAS mutation: 22 months, KRAS wildtype: 36 months), Roussile et al. described PDL1+ as a predictor of poor OS (PDL1+: 1.8 months; PDL1–: 4.2 months) [46,68]. Quan et al., Mo et al., Kim B. et al., and Rades et al. developed a scoring system to predict the OS in patients with newly diagnosed BM [7,62,63,79]. These scores included common prognostic factors like age, KPS, CEA level, extracranial metastases, and number of BM, additionally grouping patients to predict the survival rates. Aprile et al. and Mitra et al. reported cases of HER2/neu positivity in BM from CRC, while the original tumor sample was HER2/neu-negative. HER2/neu expression might also be associated with a potential negative prognostic value in BM (HER2/neu+: 4.6 months, HER2/neu–: 6.5 months) [80,81].
3.6. Treatment
Altogether 18 studies evaluated different treatment modalities (Table 9). They investigated the influence of the treatment on the OS. Common therapies were radiation, surgery, chemotherapy, or a combination of the latter [9,14,25,26,27,34,54,57,61,62,64,67,68,70,73,74,84,85].
Table 9.
OS in months for different treatment modalities [9,14,25,26,27,34,54,57,61,62,64,67,68,70,73,74,84,85]. * only the abstract was available. BSC: best supportive care. Rx: radiation therapy. Cx: chemotherapy. OP: surgery
| OS (month) | BSC | Rx | Cx | Rx + Cx | Op | Op + Rx | OP + Cx | OP + Rx + Cx | |
|---|---|---|---|---|---|---|---|---|---|
| Jin et al. (2020) * | 7 | 0.43 | 3.13 | - | 12.2 | 4.8 | 14 | - | 41.1 |
| Lu et al. (2019) | 6 | - | 3 | 5 | 10 | 10 | - | 17 | - |
| Quan et al. (2019) | 9 | - | 7 | 13 | - | 17 | 17 | - | - |
| Taylor et al. (2019) * | 3.9 | - | - | - | - | 1 | 4.4 | - | 12.3 |
| Abo et al. (2019) * | 5 | - | - | - | - | - | 17.4 | - | - |
| Kim D. et al. (2018) | 3 | - | 2.5 | - | - | - | 5 | - | - |
| Duan et al. (2018) | 7 | 2 | - | - | - | - | - | - | 14.1 |
| Del Carpio Huerta et al. (2018) | 9.5 | - | 4.6 | - | - | - | 12.1 | - | - |
| Rico et al. (2017) | 4.2 | - | 2.2 | - | - | - | 8.5 | - | - |
| Sun et al. (2016) * | 6 | - | 4 | 4 | 10 | 12 | - | - | - |
| Roussile et al. (2016) * | 8.7 | - | 4.9 | - | - | 14.8 | - | - | - |
| Gu et al. (2015) | 9.6 | - | - | - | - | 11 | 15.5 | - | - |
| Suzuki et al. (2014) | 5.4 | 1.2 | 5.1 | - | - | - | 10.5 | - | - |
| Tokoro et al. (2014) | 2.8 | 1.5 | 1.5 | - | - | 4.8 | - | - | - |
| Kim H. et al. (2013) | - | - | 5.6 | - | - | 16.2 | - | - | - |
| Byrne et al. (2012) | 3.2 | - | 3.4 | 1.7 | - | 13.2 | - | - | - |
| Damiens et al. (2012) | 4 | 2 | 4 | - | - | 3 | 13 | - | - |
| Noura et al. (2012) | 7.4 | - | 7.9 | - | - | 5.1 | 11.4 | - | - |
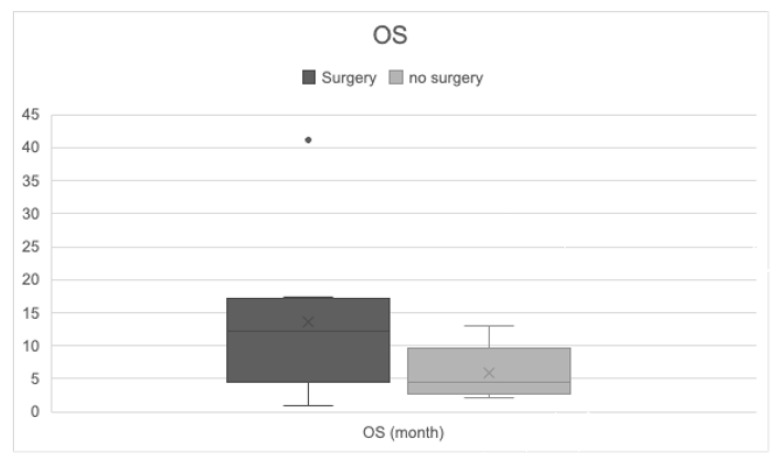
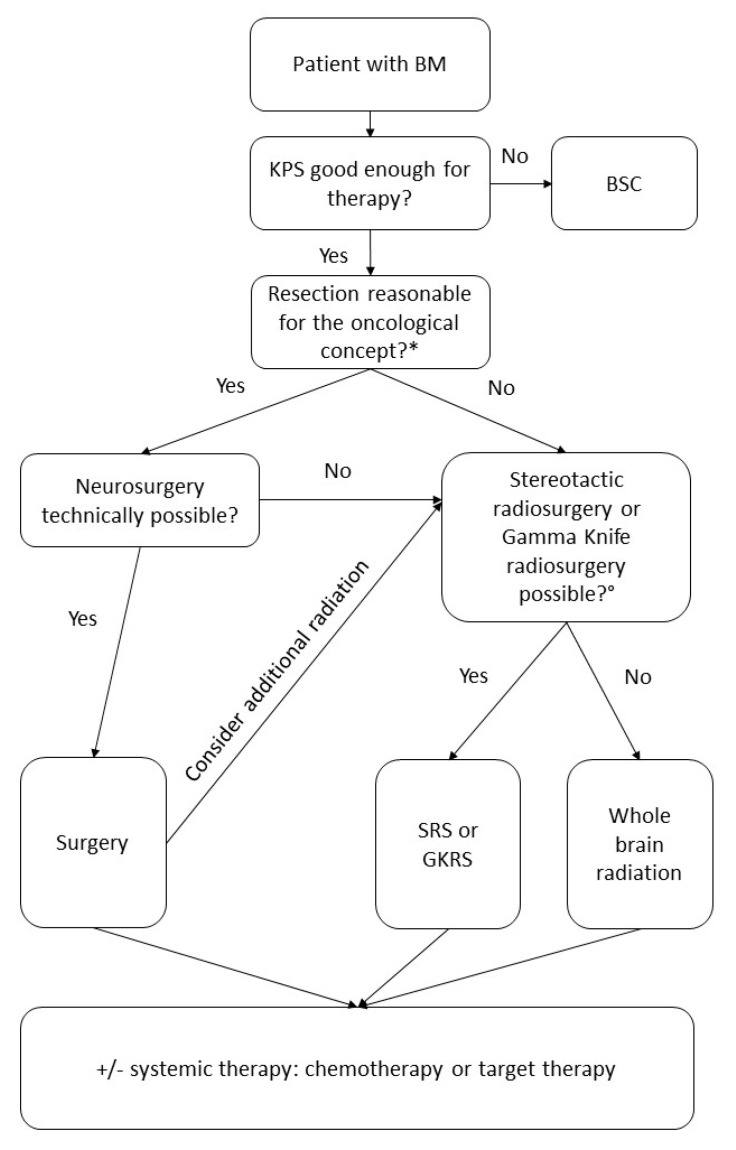
Patients who underwent surgical resection with or without additional radiation or chemotherapy had a longer OS (11.69 months; 95%CI 8.50–14.87) compared to patients without surgery (5.28 months; 95%CI 3.76–6.80). The best survival rates were reported in patients who were treated with neurosurgery with/without radiation or chemotherapy. Jin et al. showed that a multimodal therapy regime resulted in a longer OS (41.1 months) (Figure 7 and Figure 8) [57].
Figure 7.
OS in patients with and without surgical intervention. Comparison of OS in patients with neurosurgery and without neurosurgery—median OS: surgery 11.69 months (95%CI 8.50–14.87); no surgery 5.28 months (95%CI 3.76–6.80). t-test p = 0.001.
Figure 8.
MRI scan before and after neurosurgery in a 46-year-old patient with a large histologically proven CRC metastasis in the vermis, prior to (A) and after neurosurgery (B) (asterisk: resection defect). Recurrence of a small local tumorous lesion (C) (arrow) 12 months later. Significantly declining tumor nodule after chemotherapy (D) (arrow).
In patients treated with best supportive care the OS was the lowest, at 0.43–2 months [26,57,64].
If surgery was not possible, a procedure for local control such as stereotactic radiosurgery or gamma-knife radiosurgery provided better OS in patients with 1–3 metastases [86,87,88,89,90]. With these procedures, local control of BM was possible in up to 95% of patients [90].
Finkelmeier et al. and Berghoff et al. reported that a combination of chemotherapy or radiation with bevacizumab prolonged survival rates and reduced neurological symptoms [91,92]. A recently published study by Amin et al. showed that immunotherapy in combination with radiation led to a longer survival of 34%, but no further information about the type of immunotherapy was provided [93].
4. Discussion
In this study we reviewed the current literature to analyze incidence, risk factors, treatment strategies, and overall survival in patients with BM from CRC.
Our systematic review confirmed that BM are rare in colorectal cancer patients. The incidence in the included studies ranged from 0.1% up to 11.5%. Zullkowski et al. described an incidence of 11.5% in their study population, which differed greatly from the other studies. This divergence might be due to their patient selection and the small study collective. In patients with metastatic disease, one study reported a BM incidence of 14.6% [28]. This matches our results, which showed an association of BM with extracranial metastases. The wide range of values for reported incidence might be due to the large number of asymptomatic BM patients. A lack of symptoms like nausea, vomiting, headaches, or reduced vision can lead to a late diagnosis.
Therefore, in studies with restricted cranial imaging brain metastases may be undetected, whereas in studies that perform cranial imaging more generously BM might be detected earlier.
Accordingly, studies that evaluated a screening program for BM described 96% of BM patients as being asymptomatic [28,31].
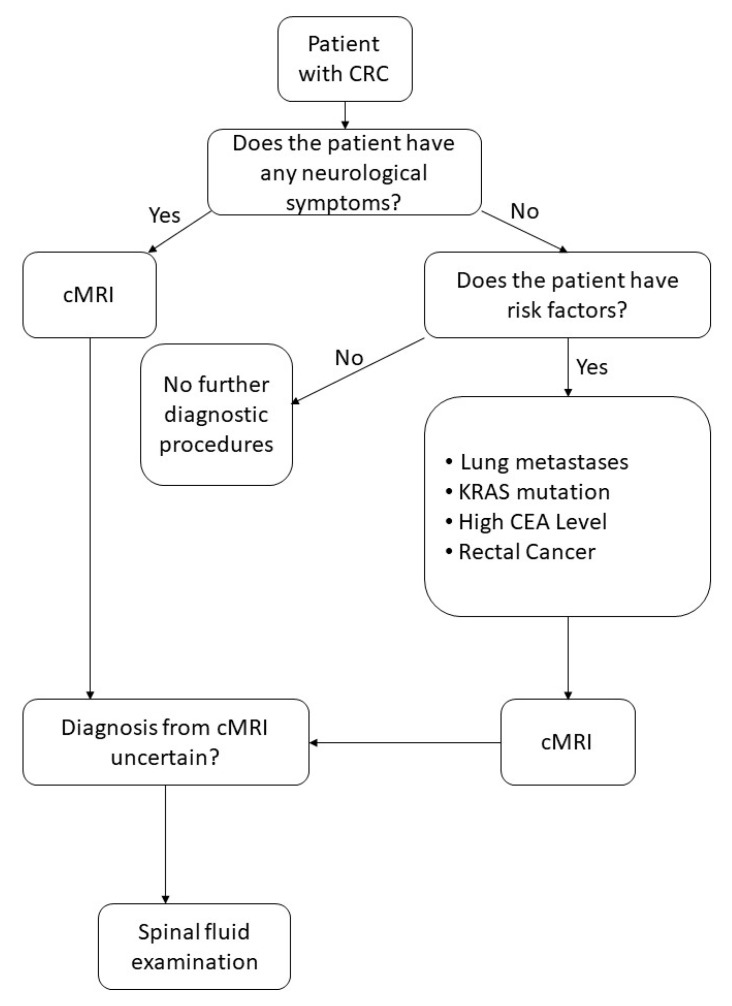
Considering these findings, we propose a systematic screening program for CRC patients (Figure 9). Performing cranial imaging on every patient with CRC would not only lead to great number of physiological MRIs but would also be a financial burden for the health system. Therefore, we recommend cranial imaging in patients with symptoms or if risk factors are present (KRAS mutation, pulmonary metastases, rectal cancer, or positive CEA level). Our screening strategy is shown in Figure 9.
Figure 9.
Assessment of screening for BM. (cMRI: cranial Magnetic resonance imaging)
For other malignant diseases that more frequently lead to BM like breast cancer, studies proved higher survival rates and better treatment options by detecting BM early. Cagney et al. recommend screening for BM in patients with metastatic breast cancer [94] and Komorowski et al. reported that asymptomatic patients with metastatic breast cancer and HER2-overexpression profited from BM screening [95]. Morikawa et al. proved in their analysis that early detection of asymptomatic BM from breast cancer was associated with higher survival rates [96].
In patients with non-small-cell lung cancer the ESMO (EUROPEAN SOCIETY.
FOR MEDICAL ONCOLOGY) guidelines recommend brain imaging to screen for BM [97]. In comparison, the ESMO guidelines for metastatic CRC do not provide a recommendation regarding screening for BM. The ESMO guidelines for rectal cancer recommend cranial imaging in symptomatic patients [5,98]. Knowing that early diagnosis of BM in CRC leads to better survival rates, a screening program in patients with more than one risk factor for developing BM should be evaluated according to our recommended screening strategy (Figure 9).
A meta-analysis by Li et al. evaluated the diagnostic criteria for BM in lung cancer patients. Gadolinium-enhanced MRI had a higher sensitivity than 18FDG PET/PET-CT for the diagnosis of BM [99]. Pope et al. described the high sensitivity of cranial MRI in detection of BM independently of the primary tumors, and therefore recommended it as first choice for diagnosis as well as monitoring of therapy response [100]. In line with the results of this meta-analysis we would advise screening for BM from CRC with cranial MRI.
In case of BM, a number of risk factors affect the OS. In this analysis we found that a positive CEA level, a low KPS, and the presence of extracranial metastases and multiple BM predicted a poor OS. Edwards et al. evaluated the OS of elderly patients with various solid tumors. There was a great association between poor KFS and shorter OS [101]. Hwang et al. described, besides other factors, the influence of low KPS on the OS in metastatic cancer patients [102]. Furthermore, a few studies described an association between CEA level and survival after curative treatment for BM [103,104,105]. CEA may be suggestive of metastatic disease which is associated with poor OS [106,107,108].
The best survival rates were found in patients with no extracranial metastases and a multimodal therapy regimen. If neurosurgical resection is possible, it leads to better OS rates if performed with additional radiation, chemotherapy, or targeted therapy. If neurosurgical resection is not possible, the number of BM is essential for defining the best treatment option. In patients with 1–3 BM, radiosurgery or gamma-knife radiosurgery is recommended, whereas patients with more than three BM should receive whole-brain radiation [86,87,88,89,90]. Our recommended treatment algorithm is shown in Figure 10.
Figure 10.
Assessment of therapy algorithm. BSC: best supportive care; SRS: stereotactic radiosurgery; GKRS: gamma knife radiosurgery; WBRT: whole-brain radiation. * Evaluate if neurosurgical resection is reasonable for the oncological therapeutic regime. The indication should be defined by an experienced neurosurgeon considering the size, number, and location of the metastases as well as symptomatology. ° The indication for SRS or GKRS should be considered individually for every patient. The DEGRO (Deutsche Gesellschafts für Radioonkologie) guidelines recommend SRS for a single BM <3 cm or 2–4 BM <2.5 cm for patients with life expectancy >3 months [109]. Lee et al. and Yamamoto et al. described how SRS for patients with up to 15 BM dependent on their position and size was associated with survival benefit and reduced risk of neurocognitive deterioration as compared to WBRT [110,111].
This study has some limitations. Not all articles that were suitable by abstract screening were available in full text. We included them anyway in our analysis if adequate data were available in the abstract. Furthermore, all suitable studies were performed retrospectively, which could lead to a publication bias. The majority of studies included a low number of patients, as seen in the study overview in the appendix.
As BM are rare in patients with CRC, a number of studies lasted more than 10 years to reach the calculated study population. As immunotherapy has developed and changed rather quickly over the last decade, treatment modalities and recommendations might have changed during the study duration, which can also pose a risk of bias. The time interval of each included study is shown in the study overview in the appendix.
5. Conclusions
BM due to CRC represent a rare condition, but if patients develop BM, their overall survival is poor. The vast majority of patients (up to 96%) are asymptomatic, which can lead to late diagnosis. Therefore, we encourage the use of a screening program for patients with risk factors for developing BM. This way, BM can be detected early on and therapy options are superior. A multimodal treatment strategy provides the best OS, and can include surgery with/without radiation, chemotherapy, or targeted therapy. Nevertheless, new studies with a higher number of patients are necessary to obtain valid information about incidence, OS, and the best treatment strategies.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study as the included studies had already undergone the ethical review and approval process.
Informed Consent Statement
Patient consent was waived as it had already been obtained by the primary authors of the included studies.
Data Availability Statement
The data presented in this study are openly available in PubMed, Embase, or Cochrane library.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization Cancer Today; Number of Incident Cases and Deaths Worldwide. [(accessed on 5 January 2021)]; Available online: https://gco.iarc.fr/today/online-analysis-multi-bars?v=2018&mode=cancer&mode_population=countries&population=900&populations=900&key=total&sex=0&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=10&group_cancer=1&include_nmsc=1&include_nmsc_other=1&type_multiple=%257B%2522inc%2522%253Atrue%252C%2522mort%2522%253Atrue%252C%2522prev%2522%253Afalse%257D&orientation=horizontal&type_sort=0&type_nb_items=%257B%2522top%2522%253Atrue%252C%2522bottom%2522%253Afalse%257D&population_group_globocan_id=#collapse-group-1-5.
- 2.Robert Koch Institute . Cancer in Germany 2015/2016—Colon and Rectum. Robert Koch Institute; Berlin, Germany: 2016. [Google Scholar]
- 3.World Health Organization Cancer Today; Fact Sheet Colorectal. [(accessed on 5 January 2021)]; Available online: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf.
- 4.World Health Organization Cancer Survival. [(accessed on 5 January 2021)]; Available online: https://gco.iarc.fr/survival/survmark/visualizations/viz8/?cancer=%22Colon+cancer%22&country=%22Australia%22&gender=%220%22&age_group=%2215-99%22&show_ci=%22%22&groupby=%22country%22.
- 5.Van Cutsem E., Cervantes A., Nordlinger B., Arnold D. Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2014;25(Suppl. 3):iii1–iii9. doi: 10.1093/annonc/mdu260. [DOI] [PubMed] [Google Scholar]
- 6.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mo S., Cai X., Zhou Z., Li Y., Hu X., Ma X., Zhang L., Cai S., Peng J. Nomograms for predicting specific distant metastatic sites and overall survival of colorectal cancer patients: A large population-based real-world study. Clin. Transl. Med. 2020;10:169–181. doi: 10.1002/ctm2.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lei S., Ge Y., Tian S., Cai B., Gao X., Wang N., Wang G., Wang L., Wang Z. Colorectal Cancer Metastases to Brain or Bone and the Relationship to Primary Tumor Location: A Population-Based Study. J. Gastrointest. Surg. 2020;24:1833–1842. doi: 10.1007/s11605-019-04308-8. [DOI] [PubMed] [Google Scholar]
- 9.Taylor N., Wong K., Jayamohan J., Shannon J., Karikios D., Nagrial A. Incidence, characteristics and prognosis in colorectal cancer with CNS metastases. Ann. Oncol. 2019;30:ix34–ix35. doi: 10.1093/annonc/mdz421.018. [DOI] [Google Scholar]
- 10.Imaizumi J., Shida D., Narita Y., Miyakita Y., Tanabe T., Takashima A., Boku N., Igaki H., Itami J., Kanemitsu Y. Prognostic factors of brain metastases from colorectal cancer. BMC Cancer. 2019;19:755. doi: 10.1186/s12885-019-5973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chahine G., Ibrahim T., Felefly T., El-Ahmadie A., Freiha P., El-Khoury L., Khalife-Saleh N., Saleh K. Colorectal cancer and brain metastases: An aggressive disease with a different response to treatment. Tumori J. 2019;105:427–433. doi: 10.1177/0300891618765541. [DOI] [PubMed] [Google Scholar]
- 12.Yang L., He W., Xie Q., Liu S., Kong P., Jiang C., Zhang B., Xia L. Brain metastases in newly diagnosed colorectal cancer: A population-based study. Cancer Manag. Res. 2018;10:5649–5658. doi: 10.2147/CMAR.S180173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang X.-H., Li A., Fu C.-G., Yu E. Risk factor analysis for brain metastasis after radical resection of colorectal cancer within 5 years. Acad. J. Second Mil. Med Univ. 2017;38:993–996. [Google Scholar]
- 14.Gonzalo T.R., Timothy J.P., Christos K., Cynthia P., Rob P., Amitesh R., Guy M., James M., Scott C., David R., et al. Brain metastasis in advanced colorectal cancer: Results from the South Australian metastatic colorectal cancer (SAmCRC) registry. Cancer Biol. Med. 2017;14:371–376. doi: 10.20892/j.issn.2095-3941.2017.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nozawa H., Ishihara S., Kawai K., Sasaki K., Murono K., Otani K., Nishikawa T., Tanaka T., Kiyomatsu T., Hata K., et al. Brain Metastasis from Colorectal Cancer: Predictors and Treatment Outcomes. Oncology. 2017;93:309–314. doi: 10.1159/000478661. [DOI] [PubMed] [Google Scholar]
- 16.Li B., Bai R., Li Y. Clinical characteristics and prognosis of brain metastasis in colorectal cancer. J. Pract. Oncol. 2017;32:416–420. [Google Scholar]
- 17.Tapia Rico G., Price T.J., Karapetis C., Piantadosi C., Padbury R., Roy A., Maddern G., Moore J., Carruthers S., Roder D., et al. Brain metastasis in advanced colorectal cancer: Results from the South Australian metastatic colorectal cancer (SAmCRC) registry. Ann. Oncol. 2016;27 doi: 10.20892/j.issn.2095-3941.2017.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tevlin R., Larkin J.O., Hyland J.M., O’Connell P.R., Winter D.C. Brain metastasis from colorectal carcinoma: A single cancer centre experience. Ir. J. Med Sci. 2015;184:673–675. doi: 10.1007/s11845-015-1272-y. [DOI] [PubMed] [Google Scholar]
- 19.Erdem D., Yücel I., Yilmaz B., Demirag G., Kut E., Cilingir F., Kemal Y., Teker F. Brain Metastases in Gastrointestinal Cancers. Ann. Oncol. 2012;23:ix221–ix222. doi: 10.1016/S0923-7534(20)33134-3. [DOI] [Google Scholar]
- 20.Pramateftakis M.G., Hatzigianni P., Kanellos D., Vrakas G., Kanellos I., Agelopoulos S., Ouzounidis N., Lazaridis C. Brain metastases in colorectal cancer. Tech. Coloproctology. 2010;14(Suppl. S1):S67–S68. doi: 10.1007/s10151-010-0624-x. [DOI] [PubMed] [Google Scholar]
- 21.Mongan J.P., Fadul C.E., Cole B.F., Zaki B.I., Suriawinata A.A., Ripple G.H., Tosteson T.D., Pipas J.M. Brain metastases from colorectal cancer: Risk factors, incidence, and the possible role of chemokines. Clin. Color. Cancer. 2009;8:100–105. doi: 10.3816/CCC.2009.n.016. [DOI] [PubMed] [Google Scholar]
- 22.Sundermeyer M.L., Meropol N.J., Rogatko A., Wang H., Cohen S.J. Changing Patterns of Bone and Brain Metastases in Patients with Colorectal Cancer. Clin. Color. Cancer. 2005;5:108–113. doi: 10.3816/CCC.2005.n.022. [DOI] [PubMed] [Google Scholar]
- 23.Zulkowski K., Kath R., Liesenfeld S., Patt S., Hochstetter A., Behrendt W., Hoffken K. Brain metastases from colorectal cancer. Med. Klinik. 2002;97:327–334. doi: 10.1007/s00063-002-1161-9. [DOI] [PubMed] [Google Scholar]
- 24.Tan W.-S., Ho K.-S., Eu K.-W. Brain Metastases in Colorectal Cancers. World J. Surg. 2009;33:817–821. doi: 10.1007/s00268-009-9919-3. [DOI] [PubMed] [Google Scholar]
- 25.Tokoro T., Okuno K., Hida J.-C., Ueda K., Yoshifuji T., Daito K., Sugiura F. Prognostic Factors for Patients With Advanced Colorectal Cancer and Symptomatic Brain Metastases. Clin. Color. Cancer. 2014;13:226–231. doi: 10.1016/j.clcc.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Suzuki Y., Yamaguchi T., Matsumoto H., Nakano D., Honda G., Shinoura N., Karasawa K., Takahashi K. Prognostic Factors and Treatment Effects in Patients with Curatively Resected Brain Metastasis from Colorectal Cancer. Dis. Colon Rectum. 2014;57:56–63. doi: 10.1097/01.dcr.0000436998.30504.98. [DOI] [PubMed] [Google Scholar]
- 27.Noura S., Ohue M., Shingai T., Fujiwara A., Imada S., Sueda T., Yamada T., Fujiwara Y., Ohigashi H., Yano M., et al. Brain metastasis from colorectal cancer: Prognostic factors and survival. J. Surg. Oncol. 2012;106:144–148. doi: 10.1002/jso.23055. [DOI] [PubMed] [Google Scholar]
- 28.Shindorf M.L., Jafferji M.S., Goff S.L. Incidence of Asymptomatic Brain Metastases in Metastatic Colorectal Cancer. Clin. Color. Cancer. 2020;19:263–269. doi: 10.1016/j.clcc.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGovern K., Rodriguez T., Smith M.H., Maloney A., Saif W.M. Investigation of an ethnic predisposition to developing brain metastases (BM) in Asian patients with colorectal cancer (CRC) J. Clin. Oncol. 2019;37:e15023. doi: 10.1200/JCO.2019.37.15_suppl.e15023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suzuki M., Komuro K., Ohara K. Olanzapine and Betamethasone Are Effective for the Treatment of Nausea and Vomiting due to Metastatic Brain Tumors of Rectal Cancer. Case Rep. Gastroenterol. 2014;8:13–17. doi: 10.1159/000358044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berghoff A.S., Schur S., Füreder L.M., Gatterbauer B., Dieckmann K., Widhalm G., Hainfellner J., Zielinski C.C., Birner P., Bartsch R., et al. Descriptive statistical analysis of a real life cohort of 2419 patients with brain metastases of solid cancers. ESMO Open. 2016;1:e000024. doi: 10.1136/esmoopen-2015-000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nemec J., Alnajjar A., Albarrak J., Al Otaibi M., Mohanty A. Brain Metastasis from Colorectal Adenocarcinoma: A Case Report. Gulf J. Oncol. 2017;1:70–72. [PubMed] [Google Scholar]
- 33.Hassan S.M., Mubarik A., Muddassir S., Haq F. Brain metastasis in colorectal cancer presenting as refractory hypertension. J. Community Hosp. Intern. Med. Perspect. 2018;8:215–219. doi: 10.1080/20009666.2018.1490138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim D.-Y., Ryu C.-G., Jung E.-J., Paik J.-H., Hwang D.-Y. Brain metastasis from colorectal cancer: A single center experience. Ann. Surg. Treat. Res. 2018;94:13–18. doi: 10.4174/astr.2018.94.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goto A., Ishimine Y., Hirata T., Naito T., Yabana T., Adachi T., Kondo Y., Kasai K. Colorectal carcinoma with hemiparesis due to isolated brain metastases as an initial symptom—A case report. Gan Kagaku Ryoho. 2014;41:1245–1249. [PubMed] [Google Scholar]
- 36.Wang Y., Wang X., Shen L. Clinical characteristics, diagnosis, and treatment of brain metastases from colorectal cancer. Chin. J. Clin. Oncol. 2016;43:962–966. [Google Scholar]
- 37.Schmidt G.P., Baur-Melnyk A., Haug A., Utzschneider S., Becker C.R., Tiling R., Reiser M.F., Hermann K.A. Whole-body MRI at 1.5 T and 3 T compared with FDG-PET-CT for the detection of tumour recurrence in patients with colorectal cancer. Eur. Radiol. 2009;19:1366–1378. doi: 10.1007/s00330-008-1289-y. [DOI] [PubMed] [Google Scholar]
- 38.Squillaci E., Manenti G., Mancino S., Cicciò C., Calabria F., Danieli R., Schillaci O., Simonetti G. Staging of colon cancer: Whole-body MRI vs. whole-body PET-CT—Initial clinical experience. Abdom. Imaging. 2008;33:676–688. doi: 10.1007/s00261-007-9347-5. [DOI] [PubMed] [Google Scholar]
- 39.Cheok S., Narayan A., Arnal-Estape A., Patel A., Nguyen D., Chiang V. 35. Evaluating Csf Circulating Tumor DNA in Intraparenchymal Brain Metastasis. Neuro Oncology Adv. 2020;2(Suppl. S2):ii6. doi: 10.1093/noajnl/vdaa073.023. [DOI] [Google Scholar]
- 40.Ali A., Ouyang T., Krishnamoorthy T., Aregawi D.G., Zacharia B., Glantz M.J. Role of cerebrospinal fluid (CSF) in the pathogenesis and treatment of patients with brain metastases. J. Clin. Oncol. 2018;36:e14006. doi: 10.1200/JCO.2018.36.15_suppl.e14006. [DOI] [Google Scholar]
- 41.Christensen T.D., Palshof J.A., Larsen F.O., Høgdall E., Poulsen T.S., Pfeiffer P., Jensen B.V., Yilmaz M.K., Christensen I.J., Nielsen D., et al. Risk factors for brain metastases in patients with metastatic colorectal cancer. Ann. Oncol. 2016;27 doi: 10.1093/annonc/mdw370.128. [DOI] [PubMed] [Google Scholar]
- 42.Qiu M., Hu J., Yang D., Cosgrove D.P., Xu R. Pattern of distant metastases in colorectal cancer: A SEER based study. Oncotarget. 2015;6:38658–38666. doi: 10.18632/oncotarget.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tanriverdi O., Kaytan-Saglam E., Ulger S., Bayoglu I.V., Turker I., Ozturk-Topcu T., Cokmert S., Turhal S., Oktay E., Karabulut B., et al. The clinical and pathological features of 133 colorectal cancer patients with brain metastasis: A multicenter retrospective analysis of the Gastrointestinal Tumors Working Committee of the Turkish Oncology Group (TOG) Med Oncol. 2014;31:152. doi: 10.1007/s12032-014-0152-z. [DOI] [PubMed] [Google Scholar]
- 44.Zoratto F., Loupakis F., Cremolini C., Salvatore L., Schirripa M., Antoniotti C., Marmorino F., Campenni G., Bergamo F., Zagonel V., et al. Risk for developing brain metastases from colorectal cancer in long-term survivors with lung metastases and KRAS mutations. J. Clin. Oncol. 2013;31:e14574. doi: 10.1200/jco.2013.31.15_suppl.e14574. [DOI] [Google Scholar]
- 45.Roussille P., Tachon G., Villalva C., Milin S., Frouin E., Godet J., Berger A., Emambux S., Petropoulos C., Wager M., et al. Pathological and Molecular Characteristics of Colorectal Cancer with Brain Metastases. Cancers. 2018;10:504. doi: 10.3390/cancers10120504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chang K.W.-L., Hernandez B., Michalek J., Crownover R.L., Floyd J., Mahalingam D. Clinical prognostic characteristics in predicting brain metastasis in patients with colorectal cancer: A single institution analysis. J. Clin. Oncol. 2015;33:e14640. doi: 10.1200/jco.2015.33.15_suppl.e14640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dhingani D., Daw H., Theethira T., Taylor H., Gohel T., Randhawa J., Randhawa M. Brain Metastases from Colorectal Cancer: A Retrospective Review of Possible Risk Factors. Am. J. Gastroenterol. 2012;107:S201. doi: 10.14309/00000434-201210001-00484. [DOI] [Google Scholar]
- 48.Liu J., Zeng W., Huang C., Wang J., Yang D., Ma D. Predictive and Prognostic Implications of Mutation Profiling and Microsatellite Instability Status in Patients with Metastatic Colorectal Carcinoma. Gastroenterol. Res. Pr. 2018;2018:4585802. doi: 10.1155/2018/4585802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee Y., Park K. P14.12 Molecular characteristics of metastatic brain tumor. Neuro-Oncology. 2017;19:iii104–iii105. doi: 10.1093/neuonc/nox036.399. [DOI] [Google Scholar]
- 50.Yaeger R., Cowell E., Chou J.F., Gewirtz A.N., Borsu L., Vakiani E., Solit D.B., Rosen N., Capanu M., Ladanyi M., et al. RAS mutations affect pattern of metastatic spread and increase propensity for brain metastasis in colorectal cancer. Cancer. 2015;121:1195–1203. doi: 10.1002/cncr.29196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Casagrande M., Rihawi K., Fontanella C., De Maglio G., Tuniz F., Ferrari L., Ongaro E., Bonotto M., Garattini S., Fanotto V., et al. 2153 Analysis ofthe molecular profile of brain metastases from colorectal cancer and concordance with matched primary tumors. Eur. J. Cancer. 2015;51:S384–S385. doi: 10.1016/S0959-8049(16)31074-7. [DOI] [Google Scholar]
- 52.Thurmaier J., Heinemann V., Engel J., Schubert-Fritschle G., Wiedemann M., Nüssler N.C., Ruppert R., Kleeff J., Schepp W., Löhe F., et al. Patients with colorectal cancer and brain metastasis: The relevance of extracranial metastatic patterns predicting time intervals to first occurrence of intracranial metastasis and survival. Int. J. Cancer. 2020 doi: 10.1002/ijc.33364. [DOI] [PubMed] [Google Scholar]
- 53.Prasanna T., Karapetis C.S., Roder D., Tie J., Padbury R., Price T., Wong R., Shapiro J., Nott L., Lee M., et al. The survival outcome of patients with metastatic colorectal cancer based on the site of metastases and the impact of molecular markers and site of primary cancer on metastatic pattern. Acta Oncol. 2018;57:1438–1444. doi: 10.1080/0284186X.2018.1487581. [DOI] [PubMed] [Google Scholar]
- 54.Abo Elseud Y., Mohanty A., Albarrak J. Colorectal cancer-related brain metastasis: A case series. Dis. Colon Rectum. 2019;62:e287–e288. [Google Scholar]
- 55.Quan J.-C., Guan X., Ma C.-X., Liu Z., Yang M., Zhao Z.-X., Sun P., Zhuang M., Wang S., Jiang Z., et al. Prognostic scoring system for synchronous brain metastasis at diagnosis of colorectal cancer: A population-based study. World J. Gastrointest. Oncol. 2020;12:195–204. doi: 10.4251/wjgo.v12.i2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Boysen A.K., Ording A.G., Astradsson A., Høyer M., Spindler K.-L. Metastasis directed treatment of brain metastases from colorectal cancer—A Danish population-based cohort study. Acta Oncol. 2020;59:1118–1122. doi: 10.1080/0284186X.2020.1769861. [DOI] [PubMed] [Google Scholar]
- 57.Jin Z., Breen W., Jin R., Brown P.D., Hubbard J.M. Multimodality management of brain metastasis from colorectal cancer. J. Clin. Oncol. 2020;38:204. doi: 10.1200/JCO.2020.38.4_suppl.204. [DOI] [Google Scholar]
- 58.Koo T., Kim K., Park H.J., Han S.-W., Kim T.-Y., Jeong S.-Y., Park K.J., Chie E.K. Prognostic factors for survival in colorectal cancer patients with brain metastases undergoing whole brain radiotherapy: Multicenter retrospective study. Sci. Rep. 2020;10:4340. doi: 10.1038/s41598-020-61354-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rades D., Nguyen T., Janssen S., Schild S.E. An Easy-To-Use Survival Score Compared to Existing Tools for Older Patients with Cerebral Metastases from Colorectal Cancer. Cancers. 2020;12:833. doi: 10.3390/cancers12040833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Muzaffar M., Naqash A.R. Synchronous brain metastasis and impact of primary tumor side in colorectal cancers. J. Clin. Oncol. 2019;37:712. doi: 10.1200/JCO.2019.37.4_suppl.712. [DOI] [Google Scholar]
- 61.Lu X., Cai Y., Xia L., Ju H., Zhao X. Treatment modalities and relative survival in patients with brain metastasis from colorectal cancer. Biosci. Trends. 2019;13:182–188. doi: 10.5582/bst.2019.01044. [DOI] [PubMed] [Google Scholar]
- 62.Quan J., Ma C., Sun P., Wang S., Zhuang M., Liu Z., Jiang Z., Chen H., Yang M., Zhao Z., et al. Brain metastasis from colorectal cancer: Clinical characteristics, timing, survival and prognostic factors. Scand. J. Gastroenterol. 2019;54:1370–1375. doi: 10.1080/00365521.2019.1686056. [DOI] [PubMed] [Google Scholar]
- 63.Kim B.H., Park H.J., Kim K., Han S.-W., Kim T.-Y., Jeong S.-Y., Park K.J., Chie E.K. Novel graded prognostic assessment for colorectal cancer patients with brain metastases. Int. J. Clin. Oncol. 2018;23:1112–1120. doi: 10.1007/s10147-018-1329-9. [DOI] [PubMed] [Google Scholar]
- 64.Duan H., He Z.-Q., Guo C.-C., Li J.-H., Wang J., Zhu Z., Sai K., Chen Z.-P., Jiang X.-B., Mou Y.-G. Bone metastasis predicts poor prognosis of patients with brain metastases from colorectal carcinoma post aggressive treatment. Cancer Manag. Res. 2018;10:2467–2474. doi: 10.2147/CMAR.S169563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Del Carpio Huerta L., Manrique A.C.V., Szafranska J., Martin-Richard M., Lopez-Bravo D.P., Garcia A.S., Mariscal I.E., Pons P.G., Granyo M.A., Joaquin A.B., et al. Brain metastases in colorectal cancer: Prognostic factors and survival analysis. Int. J. Color. Dis. 2018;33:1517–1523. doi: 10.1007/s00384-018-3107-6. [DOI] [PubMed] [Google Scholar]
- 66.Fountzilas C., Chang K., Hernandez B., Michalek J., Crownover R., Floyd J., Mahalingam D. Clinical characteristics and treatment outcomes of patients with colorectal cancer who develop brain metastasis: A single institution experience. J. Gastrointest. Oncol. 2017;8:55–63. doi: 10.21037/jgo.2016.12.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sun Z., Sun Y., Tan L., He J., Li X., She C., Li W. Clinical features and prognostic factors of brain metastasis from colorectal cancer. Zhonghua Zhong Liu Za Zhi. 2016;38:63–68. doi: 10.3760/cma.j.issn.0253-3766.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 68.Roussille P., Dior M., Locher C., Mabro M., Artru P., Tachon G., Frouin É., Berger A., Wager M., Goujon J.-M., et al. Clinical characteristics of colorectal cancer patients with brain metastases: An “Association des Gastro-Éntérologues Oncologues” (AGEO) multicenter study. Ann. Oncol. 2016;27 doi: 10.1093/annonc/mdw370.135. [DOI] [Google Scholar]
- 69.Karivedu V., Venur V.A., Kim I., Chao S.T., Suh J.H., Sohal D., Khorana A.A., Jia X., Ahluwalia M.S. Graded prognostic assessment index for colorectal cancer with brain metastases. J. Clin. Oncol. 2015;33:2049. doi: 10.1200/jco.2015.33.15_suppl.2049. [DOI] [Google Scholar]
- 70.Gu X.-D., Cai Y.-T., Zhou Y.-M., Li Z.-Y., Xiang J.-B., Chen Z.-Y. Prognostic factors and multidisciplinary treatment modalities for brain metastases from colorectal cancer: Analysis of 93 patients. BMC Cancer. 2015;15:902. doi: 10.1186/s12885-015-1933-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Magni E., Santoro L., Ravenda P.S., Leonardi M.C., Bonomo G., Monfardini L., Nolè F., Zampino M.G. Brain metastases from colorectal cancer: Main clinical factors conditioning outcome. Int. J. Color. Dis. 2014;29:201–208. doi: 10.1007/s00384-013-1781-y. [DOI] [PubMed] [Google Scholar]
- 72.Berghoff A.S. Clinical prognostic factors in brain metastases from colorectal cancer. Memo Mag. Eur. Med. Oncol. 2013;6:39. [Google Scholar]
- 73.Byrne B.E., Geddes T., Welsh F.K.S., John T.G., Chandrakumaran K., Rees M. The incidence and outcome of brain metastases after liver resection for colorectal cancer metastases. Color. Dis. 2012;14:721–726. doi: 10.1111/j.1463-1318.2011.02762.x. [DOI] [PubMed] [Google Scholar]
- 74.Damiens K., Ayoub J., Lemieux B., Aubin F., Saliba W., Campeau M., Tehfe M. Clinical features and course of brain metastases in colorectal cancer: An experience from a single institution. Curr. Oncol. 2012;19:254–258. doi: 10.3747/co.19.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baek J.Y., Kang M.H., Hong Y.S., Kim T.W., Kim D.Y., Oh J.H., Lee S.H., Park J.H., Kim J.H., Kim S.Y. Characteristics and prognosis of patients with colorectal cancer-associated brain metastases in the era of modern systemic chemotherapy. J. Neuro Oncol. 2011;104:745–753. doi: 10.1007/s11060-011-0539-z. [DOI] [PubMed] [Google Scholar]
- 76.Kruser T., Chao S., Elson P., Barnett G., Vogelbaum M., Toms S., Angelov L., Suh J. Multidisciplinary Management of Colorectal Cancer Brain Metastases: A Retrospective Study. Cancer. 2008;113:158–165. doi: 10.1002/cncr.23531. [DOI] [PubMed] [Google Scholar]
- 77.Itoh H., Nishijima K., Kurosaka Y., Takegawa S., Kiriyama M., Dohba S., Kojima Y., Ikeda K. Impact of combination therapy of neurosurgery and stereotatic radiosurgery for brain metastasis from colorectal cancer: Report of five cases. Chirurgia. 2007;20:19–24. [Google Scholar]
- 78.Zorrilla M., Alonso V., Herrero A., Corral M., Puértolas T., Trufero J.M., Artal A., Antón A. Brain metastases from colorectal carcinoma. Tumori J. 2001;87:332–334. doi: 10.1177/030089160108700511. [DOI] [PubMed] [Google Scholar]
- 79.Rades D., Dziggel L., Blanck O., Gebauer N., Bartscht T., Schild S.E. A Score to Identify Patients with Brain Metastases from Colorectal Cancer Who May Benefit from Whole-brain Radiotherapy in Addition to Stereotactic Radiosurgery/Radiotherapy. Anticancer. Res. 2018;38:3111–3114. doi: 10.21873/anticanres.12570. [DOI] [PubMed] [Google Scholar]
- 80.Mitra D., Clark J.W., Shih H.A., Oh K.S., Brastianos P.K., Wo J.Y., Strickland M.R., Curry W.T., Parikh A.R., Corcoran R.B., et al. Enrichment of HER2 Amplification in Brain Metastases from Primary Gastrointestinal Malignancies. Oncologist. 2019;24:193–201. doi: 10.1634/theoncologist.2018-0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Aprile G., De Maglio G., Menis J., Casagrande M., Tuniz F., Pisa E.F., Fontanella C., Skrap M., Beltrami A.C., Fasola G., et al. HER-2 Expression in Brain Metastases from Colorectal Cancer and Corresponding Primary Tumors: A Case Cohort Series. Int. J. Mol. Sci. 2013;14:2370–2387. doi: 10.3390/ijms14022370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Berghoff A.S., Ferreira P., Plazer H., Widhalm G., Birner P., Bartsch R., Prager G.W., Zielinski C., Preusser M. Primary tumor sidedness associates with prognosis of patients with brain metastases of colorectal cancer. J. Clin. Oncol. 2017;35:3562. doi: 10.1200/JCO.2017.35.15_suppl.3562. [DOI] [Google Scholar]
- 83.Nieder C., Hintz M., Grosu A.L. Predicted survival in patients with brain metastases from colorectal cancer: Is a current nomogram helpful? Clin. Neurol. Neurosurg. 2016;143:107–110. doi: 10.1016/j.clineuro.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 84.Del Carpio Huerta L.P., Tobeña M., Manrique A.V., Szafranska J., Martín-Richard M., Paez D., Espinoza I., Garcia A.S., Pons P.G., Granyo M.A., et al. Brain metastases (BM) in colorectal cancer (CRC): Prognostic factors and survival analysis. Ann. Oncol. 2016;27:vi195. doi: 10.1093/annonc/mdw370.133. [DOI] [Google Scholar]
- 85.Kim H.J., Huh J.W., Jung T.Y., Kim I.Y., Kim H.R., Jung S., Kim Y.J. Clinical outcome with gamma-knife surgery or surgery for brain metastases from colorectal cancer. J. Clin. Neurosci. 2013;20:1417–1421. doi: 10.1016/j.jocn.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 86.Paix A., Thillays F., Biau J., Vulquin N., Pop I., Debbi K., Grosu A., Noël G. PO-0815 Stereotactic radiation therapy in colorectal cancer brain metastasis: A multicentric cohort. Radiother. Oncol. 2019;133:S425–S426. doi: 10.1016/S0167-8140(19)31235-6. [DOI] [Google Scholar]
- 87.Nieder C., Hintz M., Grosu A.L. Colorectal cancer metastatic to the brain: Analysis of prognostic factors and impact of KRAS mutations on presentation and outcome. Clin. Transl. Oncol. 2016;18:88–92. doi: 10.1007/s12094-015-1340-9. [DOI] [PubMed] [Google Scholar]
- 88.Fokas E., Henzel M., Hamm K., Surber G., Kleinert G., Engenhart-Cabillic R. Multidisciplinary treatment of brain metastases derived from colorectal cancer incorporating stereotactic radiosurgery: Analysis of 78 patients. Clin. Colorectal Cancer. 2011;10:121–125. doi: 10.1016/j.clcc.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 89.Kahn E., Mondschein J., Chakravarthy A., Cmelak A., Berlin J., Thompson R., Weaver K., Li M., Xia F. Stereotactic Radiosurgery in the Treatment of Brain Metastases from Colorectal Cancer: Should Patients be Treated with Up-front Whole-brain Radiotherapy? Int. J. Radiat. Oncol. 2010;78:S273–S274. doi: 10.1016/j.ijrobp.2010.07.653. [DOI] [Google Scholar]
- 90.Hasegawa T., Kondziolka D., Flickinger J.C., Lunsford L.D. Stereotactic radiosurgery for brain metastases from gastrointestinal tract cancer. Surg. Neurol. 2003;60:506–514. doi: 10.1016/S0090-3019(03)00356-2. discussion 514–515. [DOI] [PubMed] [Google Scholar]
- 91.Berghoff A.S., Breckwoldt M.O., Riedemann L., Karimian-Jazi K., Loew S., Schlieter F., Furtner J., Cinci M., Thomas M., Strowitzki M.J., et al. Bevacizumab-based treatment as salvage therapy in patients with recurrent symptomatic brain metastases. Neuro Oncology Adv. 2020;2:vdaa038. doi: 10.1093/noajnl/vdaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Finkelmeier F., You S.-J., Waidmann O., Wolff R., Zeuzem S., Bähr O., Trojan J. Bevacizumab in Combination with Chemotherapy for Colorectal Brain Metastasis. J. Gastrointest. Cancer. 2016;47:82–88. doi: 10.1007/s12029-015-9795-z. [DOI] [PubMed] [Google Scholar]
- 93.Amin S., Baine M.J., Meza J.L., Lin C. Association of Immunotherapy with Survival Among Patients With Brain Metastases Whose Cancer Was Managed with Definitive Surgery of the Primary Tumor. JAMA Netw. Open. 2020;3:e2015444. doi: 10.1001/jamanetworkopen.2020.15444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cagney D.N., Martin A.M., Catalano P.J., Brown P.D., Alexander B.M., Lin N.U., Aizer A.A. Implications of Screening for Brain Metastases in Patients with Breast Cancer and Non–Small Cell Lung Cancer. JAMA Oncol. 2018;4:1001–1003. doi: 10.1001/jamaoncol.2018.0813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Komorowski A.S., Warner E., MacKay H.J., Sahgal A., Pritchard K.I., Jerzak K.J. Incidence of Brain Metastases in Nonmetastatic and Metastatic Breast Cancer: Is There a Role for Screening? Clin. Breast Cancer. 2020;20:e54–e64. doi: 10.1016/j.clbc.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 96.Morikawa A., Wang R., Patil S., Diab A., Yang J., Hudis C.A., McArthur H.L., Beal K., Seidman A.D. Characteristics and Prognostic Factors for Patients With HER2-overexpressing Breast Cancer and Brain Metastases in the Era of HER2-targeted Therapy: An Argument for Earlier Detection. Clin. Breast Cancer. 2018;18:353–361. doi: 10.1016/j.clbc.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 97.Postmus P.E., Kerr K.M., Oudkerk M., Senan S., Waller D.A., Vansteenkiste J., Escriu C., Peters S. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017;28(Suppl. S4):iv1–iv21. doi: 10.1093/annonc/mdx222. [DOI] [PubMed] [Google Scholar]
- 98.Glynne-Jones R., Wyrwicz L., Tiret E., Brown G., Rödel C., Cervantes A., Arnold D. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017;28:iv22–iv40. doi: 10.1093/annonc/mdx224. [DOI] [PubMed] [Google Scholar]
- 99.Li Y., Jin G., Su D. Comparison of Gadolinium-enhanced MRI and 18FDG PET/PET-CT for the diagnosis of brain metastases in lung cancer patients: A meta-analysis of 5 prospective studies. Oncotarget. 2017;8:35743–35749. doi: 10.18632/oncotarget.16182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pope W.B. Brain metastases: Neuroimaging. Handb. Clin. Neurol. 2018;149:89–112. doi: 10.1016/B978-0-12-811161-1.00007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Edwards B.J., Zhang X., Sun M., Song J., Khalil P., Karuturi M.S., Pang L., Geng Y., Dinney C.P., Valero V., et al. Overall survival in older patients with cancer. BMJ Support Palliat. Care. 2020;10:25–35. doi: 10.1136/bmjspcare-2018-001516. [DOI] [PubMed] [Google Scholar]
- 102.Hwang S.S., Scott C.B., Chang V.T., Cogswell J., Srinivas S., Kasimis B. Prediction of survival for advanced cancer patients by recursive partitioning analysis: Role of Karnofsky performance status, quality of life, and symptom distress. Cancer Investig. 2004;22:678–687. doi: 10.1081/CNV-200032911. [DOI] [PubMed] [Google Scholar]
- 103.Baqar A.R., Wilkins S., Staples M., Lee C.H.A., Oliva K., McMurrick P. The role of preoperative CEA in the management of colorectal cancer: A cohort study from two cancer centres. Int. J. Surg. 2019;64:10–15. doi: 10.1016/j.ijsu.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 104.Yang X.-Q., Li Y., Chen C., Peng C.-W., Liu S.-P., Liu Y. Preoperative serum carbohydrate antigen 125 level is an independent negative prognostic marker for overall survival in colorectal cancer. Med. Oncol. 2010;28:789–795. doi: 10.1007/s12032-010-9518-z. [DOI] [PubMed] [Google Scholar]
- 105.Gunawardene A., Larsen P., Shekouh A., Dennett E. Pre-operative carcinoembryonic antigen predicts survival following colorectal cancer surgery with curative intent. ANZ J. Surg. 2018;88:1311–1315. doi: 10.1111/ans.14723. [DOI] [PubMed] [Google Scholar]
- 106.Stojkovic Lalosevic M., Stankovic S., Stojkovic M., Markovic V., Dimitrijevic I., Lalosevic J., Petrovic J., Brankovic M., Markovic A.P., Krivokapic Z. Can preoperative CEA and CA19-9 serum concentrations suggest metastatic disease in colorectal cancer patients? Hell. J. Nucl. Med. 2017;20:41–45. doi: 10.1967/s002449910505. [DOI] [PubMed] [Google Scholar]
- 107.Ramphal W., Boeding J.R., Van Iwaarden M., Schreinemakers J.M., Rutten H.J., Crolla R.M., Gobardhan P.D. Serum carcinoembryonic antigen to predict recurrence in the follow-up of patients with colorectal cancer. Int. J. Biol. Markers. 2019;34:60–68. doi: 10.1177/1724600818820679. [DOI] [PubMed] [Google Scholar]
- 108.Takagawa R., Fujii S., Ohta M., Nagano Y., Kunisaki C., Yamagishi S., Osada S., Ichikawa Y., Shimada H. Preoperative Serum Carcinoembryonic Antigen Level as a Predictive Factor of Recurrence After Curative Resection of Colorectal Cancer. Ann. Surg. Oncol. 2008;15:3433–3439. doi: 10.1245/s10434-008-0168-8. [DOI] [PubMed] [Google Scholar]
- 109.Kocher M., Wittig A., Piroth M.D., Treuer H., Seegenschmiedt H., Ruge M., Grosu A.-L., Guckenberger M. Stereotactic radiosurgery for treatment of brain metastases. Strahlenther. Onkol. 2014;190:521–532. doi: 10.1007/s00066-014-0648-7. [DOI] [PubMed] [Google Scholar]
- 110.Yamamoto M., Serizawa T., Shuto T., Akabane A., Higuchi Y., Kawagishi J., Yamanaka K., Sato Y., Jokura H., Yomo S., et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi-institutional prospective observational study. Lancet Oncol. 2014;15:387–395. doi: 10.1016/S1470-2045(14)70061-0. [DOI] [PubMed] [Google Scholar]
- 111.Li J., Ludmir E., Wang Y., Guha-Thakurta N., McAleer M., Settle S., Yeboa D., Ghia A., McGovern S., Chung C., et al. Stereotactic Radiosurgery versus Whole-brain Radiation Therapy for Patients with 4-15 Brain Metastases: A Phase III Randomized Controlled Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020;108:S21–S22. doi: 10.1016/j.ijrobp.2020.07.2108. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are openly available in PubMed, Embase, or Cochrane library.