Abstract
Purpose of review
Mineworkers in South Africa experience a triple burden of disease due to their distinct work experience. Silicosis increases their risk of tuberculosis (TB), exacerbated by the HIV epidemic. Work-related factors are likely to increase transmission, severity, and post infection sequelae of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Understanding these relationships is important to control the impact of the epidemic.
Recent findings
SARS-CoV-2 infection rates among mineworkers exceed the population rates in the provinces in which those mines are located. Migrant work, living in crowded hostels, working in narrow poorly ventilated shafts mainly underground constitute important factors that increase transmission risk. Mineworkers continue to experience high levels of silica exposure. The prevalences of silicosis, HIV and pulmonary TB, remain high. Interstitial lung disease, pulmonary TB, and HIV have all been associated with poorer outcomes of SARS-CoV-2 infections. Mineworkers with post infection respiratory sequelae are likely to lose their jobs or lose income, due to the physically demanding nature of underground minework.
Summary
Further research into the unique work-related risk factors in mining that influence the COVID-19 epidemic is crucial for optimizing current interventions. Reducing SARS-CoV-2 infection transmission, health monitoring of infected and vulnerable workers, and following up of postinfection outcomes is essential to protect the respiratory health of miners.
Keywords: COVID-19, fitness-to-work, silica exposure, tuberculosis, vulnerability
INTRODUCTION
Since the 1860s South African mineworkers have experienced a substantial burden of respiratory diseases [1,2]. The high incidence of respiratory diseases in miners in the late 19th century was noted and investigated by South African researchers and led to the publication of seminal articles in the field on ‘phthisis’ – pulmonary tuberculosis (PTB) – and silicosis. That work culminated in the landmark 1930 International Silicosis Conference in Johannesburg [3].
In the 1980s, the HIV epidemic disproportionately affected the South African miner population [4]. The peculiarities of the South African mining industry once again provided ideal conditions for ensuring that this disease burden became endemic. The crowded hostels that housed many migrants and provided optimal social conditions for the spread of PTB also provided an optimal social environment for the spread of HIV [4].
It is within this context that the COVID-19 pandemic requires particular focus. This pandemic adds new complexities to the disease burden among miners: an environment conducive to spread of the infection, increased vulnerability for more severe complications of the disease, and the potential for chronic postinfection sequelae that is likely to impact on work ability of these miners.
The objective of this review was to explore the known and likely impacts of this new epidemic on mineworkers, and the inter-relatedness of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and existing chronic disease burden encountered in South African mineworkers.
Box 1.
no caption available
METHODS
Studies were identified from PubMed and MEDLINE using the following search strategy: (COVID-19 OR SARS-CoV-2) AND (TB or pulmonary tuberculosis) OR (HIV) OR (silicosis) OR (COPD) OR (silica exposure) OR (mining). Technical reports produced by government, industry, and research agencies in South Africa relevant to the review were sourced. Additional references published but not identified in the initial search were included.
THE COVID-19 EPIDEMIC IN SOUTH AFRICAN MINES
South Africa has had the highest morbidity and mortality due to COVID-19 on the African continent. In the mining industry, the first series of COVID-19 cases was reported in March 2020 (Fig. 1) [5]. There was a slow increase in cases until the end of April 2020, due to the national State of Disaster (The South African government instituted an Alert Level 5 ‘lockdown’ – the maximum ‘lockdown’ level). During alert level 5, the government did allow certain economic sectors deemed ‘essential’ to continue to function and included certain mining activities (gold, coal, and ‘essential mining’ was permitted) in that list despite potential high-risk exposures in underground mines due to narrow shafts and inadequate ventilation. By early May (alert level 4), the number of daily cases had increased steadily, reaching its peak in mid-July 2020. By 5 October 2020, 17 155 workers out of a workforce of 454 595 had tested positive and 184 deaths had been recorded. The proportion of positive cases (3.8%) in the mining population has been higher than the South African population (mine testing rates 11.6% compared with 7.2% in country), with a lower fatality rate (1.1%) than the national average (2.5%) [5].
FIGURE 1.
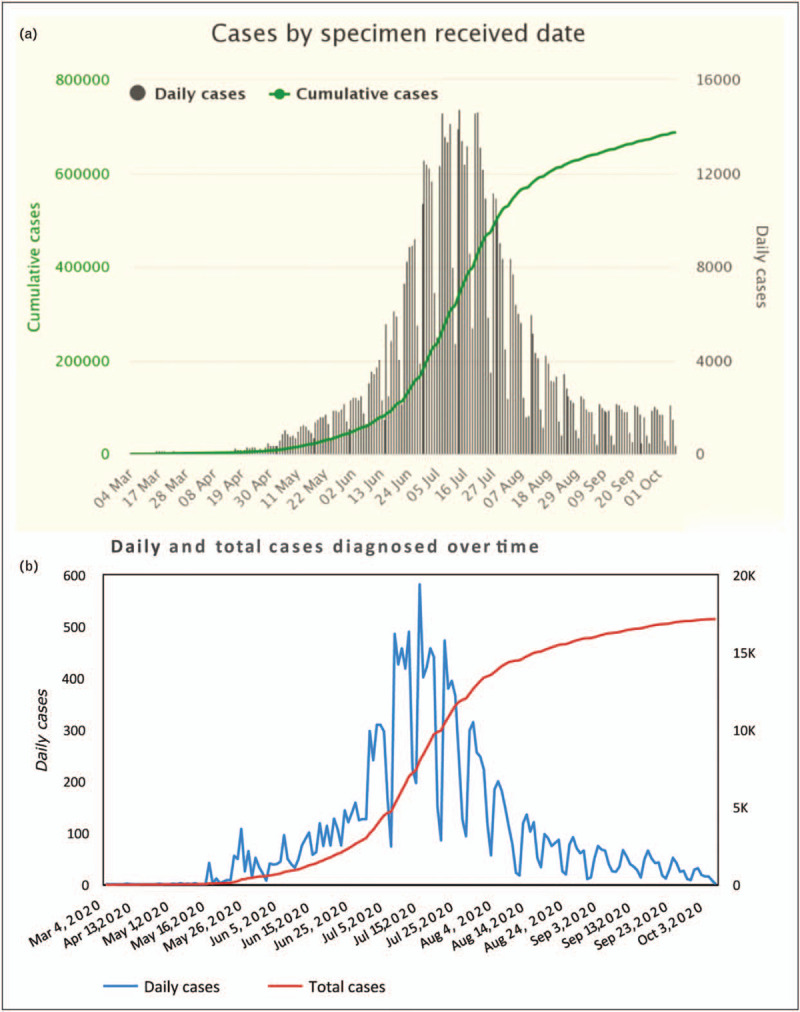
Daily and total COVID-19 cases diagnosed in (a) South African general population and (b) in the South African mining industry for the period March–October 2020. Source: (a) https://www.nicd.ac.za/wp-content/uploads/2020/10/NICD-Daily-Report-and-Commentary-08-10-2020-1.pptx, (b) https://www.mineralscouncil.org.za/minerals-council-position-on-covid-19 – last accessed 25 October 2020. Key dates: First South African case: 5 March 2020; Alert Level 5: 27 March 2020; Return of mineworkers: 30 April 2020; Alert Level 4: 30 April 2020; Alert Level 3: 1 June 2020.
The data on predictors of infection and risk factors for severe outcomes of COVID-19 among South African miners are still emerging. For miners, work-related exposures and chronic diseases coupled with their sociogeographic contexts could lead to increased risk for acquiring infection, greater vulnerability for severe acute outcomes, and a higher incidence of serious post infection sequelae (Table 1).
Table 1.
Work-related factors associated with SARS-COV-2 infection and COVID-19 disease in South African mining
| Potential risk factors for SARS-COV-2 infection |
| Migrant labor |
| Sociogeographic factors |
| Mining exposure-related factors |
| Vulnerability for more severe complications of COVID-19 disease |
| Silicosis and other interstitial lung diseases |
| Pulmonary TB |
| HIV infection |
| Chronic obstructive pulmonary disease |
| Other mining-related factors |
| Postinfection sequelae of COVID-19 |
| Progression to persistent/chronic lung disease |
| Fitness to work and work ability |
| Workers compensation |
TB, tuberculosis.
Potential risk factors for SARS-COV-2 infection
At least 20% of SARS-CoV-2 infections in adults are work-related [6], and 10% of the US workforce is employed in occupations that involve potential exposure at least once per week [7]. Canadian workers in low-income occupations, particularly women, immigrants, and members of visible minority groups are at greater risk of exposure to COVID-19 than other workers [8]. Miners fit categories of those at increased risk; their work is generally low paid, migrant in nature, and requires frequent close contact with coworkers [9]. The plurality of smoking males in this sector constitutes an additional risk factor [10–12]. In the South African mining context, certain work-related risk factors appear more prominent.
Migrant labor
The risk for SARS-CoV-2 infection has been linked to travel from ‘hotspots’ through international routes and to migration within a country. Initially, South Africa's early shutdown of international borders successfully controlled the foreign transmission. With the closure of the economy, many migrant workers returned to their homes, both in rural South Africa and in neighboring countries. During alert level 4 (Fig. 1), about 12 000 workers returned from neighboring countries. While strategies to screen for infection prior to leaving home, on entry into hostels, and at workplaces were pursued in hopes of limiting the spread of infection, the extent to which this migration contributed to infection transmission is unknown. However, the changing patterns of mineworker recruitment in the past decade, with increasing dependency on internal migrant workers closer to the mining regions (central and north-western South Africa) rather than foreigners [13], may have influenced transmission patterns.
Sociogeographic factors
The COVID-19 cases officially reported in South Africa have been geographically disparate across key mining provinces (North West, Mpumalanga, Limpopo, and Gauteng). With the reopening of mines, infection rates initially mirrored those of the local communities within which operations were located or the locations from which miners had migrated. The cumulative incidence over time, however, became higher in mines of all provinces except for the Western Cape (absent underground mining activity) (Fig. 2). Crowded hostels have historically provided the social conditions for the rapid spread of PTB and HIV [4], and approximately 30% of miners currently live in hostels. It is likely that these same housing factors have been a key factor in the transmission of COVID-19 and in the increased incidence of COVID-19 over time in this population.
FIGURE 2.
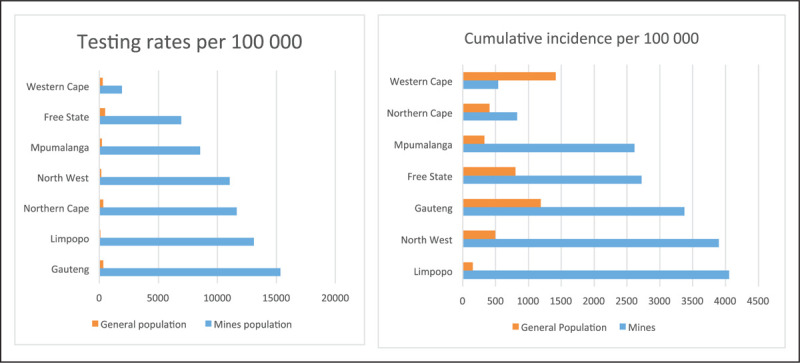
COVID-19 testing and cumulative incidence among South African miners for the period 1 March–31 July 2020. Source: Muchiri E., Charalambous S. Minerals Council COVID-19 response and surveillance progress report, 31 July 2020.
Mining exposure-related factors
Almost 80% of South African mineworkers are employed in platinum, gold, and coal mines, which are largely underground operations as opposed to open cast mines at which social distancing adherence may be easier. Platinum mining reported the highest cumulative incidence at 44.2 COVID-19 cases per 1000 workers screened, followed by diamond (38.9/1000), gold (32.8/1000), and coal mining (29.8/1000) (Fig. 3) [14]. The high cumulative incidence in the platinum industry, which employs 50% of all workers (and 73% of whom returned to work), could be due to large number of workers working in close contact. Gold and coal, employ only half the size of the platinum workforce (having similar testing rates) but are characterized by higher dust exposures, inadequate ventilation, and miners working in small groups in close proximity to each other – factors known to increase the risk of SARS-CoV-2 infection [15–17].
FIGURE 3.
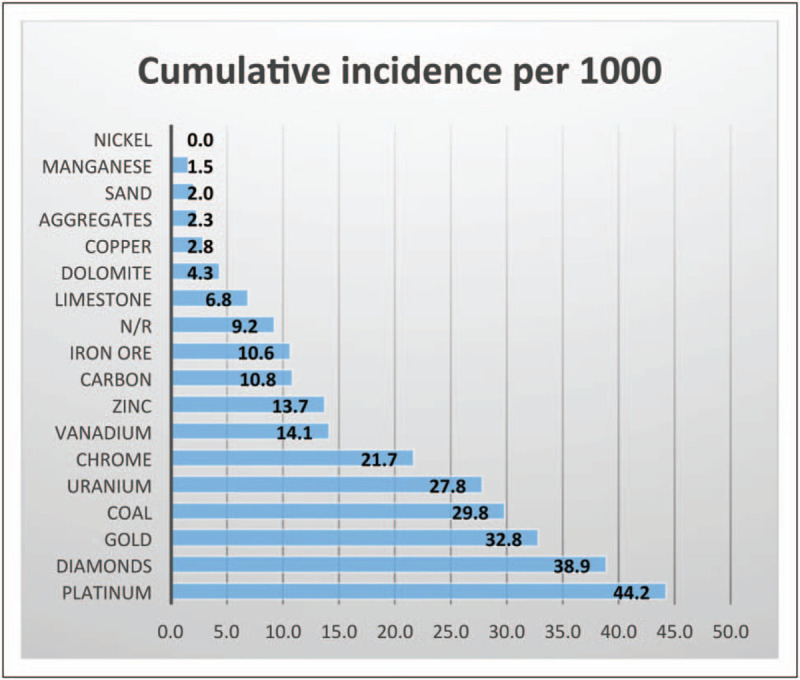
COVID-19 cumulative incidence by commodity among South African miners for the period 1 March–31 July 2020. Source: Muchiri E., Charalambous S. Minerals Council COVID-19 response and surveillance progress report, 31 July 2020.
Emissions generated by mining activities include particulates, such as PM10, PM2.5, and dust fallout. Historically, levels of respirable dust concentrations on South African mines have ranged from 1.04 mg/m3 among highly exposed shaft sinkers through to 0.2 mg/m3 among artisans [18]. Recent epidemiological studies have reported mean exposures of respirable silica of 0.05 mg/m3 (SD = 0.07 mg/m3), which is two-fold higher than the US Threshold Limit Values for crystalline silica [19▪]. In gold mines, silica quartz concentrations in dust ranged from 9 to 39%. Apart from the direct fibrotic effect of silica on lung tissue, its chronic and immunomodulatory character increases susceptibility to PTB, resulting in significantly higher TB incidence in silica-exposed populations [20]. Furthermore, chronic exposure to high PM2.5 levels results in overexpression of alveolar angiotensin-converting enzyme 2 (ACE-2) receptor, which can increase the viral load in individuals exposed to air pollutants [21].
Vulnerability for more severe complications of COVID-19 disease
As of October 2020, approximately 60% of South African miners who had died from COVID-19 were older than 50 years, and 86% had at least one comorbidity (Balfour T, Minerals Council South Africa, personal communication). This is similar to patterns seen elsewhere. A study representing 40% of all patients in England demonstrated those 60 years and older had a two-fold greater risk of COVID-19 death [22▪]. South African miners are subject to unique risk factors inherent to their work in addition to these factors known to be associated with increased vulnerability for severe outcomes of SARS-CoV-2 infection in the general population.
Silicosis and other interstitial lung diseases
Levels of radiological silicosis among South African goldminers have ranged from 19.9% in current miners [23] to 22.0–36.0% among exminers [24–26]. A very recent study of current miners published in 2020 reported a lower prevalence of silicosis (3.8%) [27▪].
Although evidence for pneumoconiosis as a risk factor for more severe outcomes of COVID-19 has yet to be presented, interstitial lung diseases (ILDs), which present with similar lung abnormality, have been associated with increased risk. In a case–controlled study, COVID-19-positive individuals with ILD had an adjusted mortality odds ratio (OR) of 4.3 [95% confidence interval (CI): 1.4–14.0] when compared with negative controls, with a mortality of 49% [28]. An international multicenter study also showed that patients with ILD are at increased risk of death from COVID-19, particularly those with poor lung function and obesity [29▪▪]. The pathophysiological bases for this outcome needs to be better understood given the protective response conferred against certain types of fibrosis by ACE-2 receptors, the entry point for SARS-CoV-2 into cells [30].
Pulmonary tuberculosis
The prevalence of PTB among South African mineworkers increased from 806 per 100 000 in 1991 to 3281 per 100 000 in 2004 [31], while in a recent TB cohort, a prevalence of 21.4% was observed [27▪]. This is also confirmed at autopsy (a legal requirement for South African miners); the prevalence among black miners increased from 4.6% in 1975 to a peak of 43.2% in 2007 and a subsequent decline to 27.3% in 2014 [32,33]. The decline has been attributed to several factors, including large-scale antiretroviral treatment campaigns, resulting in improved CD4 counts among HIV positive miners, in turn reducing their risk for acquiring TB. Major mining retrenchments in recent years, resulting in a ‘healthy worker effect’ [34], is also likely to contribute to this decline. The latter hypothesis is supported by the high prevalence of TB seen among exminers [35].
Based on available evidence, both current and past TB are likely to be risk factors for severe outcomes of SARS-CoV-2 infection. In a large study from the Western Cape province (n = 3460 932), current and previous PTB was associated with an increased COVID-19 mortality risk [adjusted hazard ratios of 2.70 (95% CI: 1.81; 4.04) and 1.51 (95% CI: 1.18; 1.93) respectively] [36▪]. In a meta-analysis of approximately 2765 cases of TB across six studies, the prevalence of PTB was two-fold higher (OR: 2.1; 95% CI: 0.6; 7.2) among those with severe COVID-19 [37]. In a longitudinal cohort analysis of 12 513 COVID-19 patients in the Philippines, current TB was also associated with a 2.2-fold higher risk of death (95% CI: 1.4–3.4), a 25% lower recovery rate (95% CI: 0.6–0.9) and a 20% higher risk of admission [38].
HIV infection
The prevalence of HIV in miners on South African mines was 1.3% in 1990, rising rapidly to 27% in 2000 [4], and currently reflects the rates seen in the general population (Balfour T, personal communication). The risk of TB among those with HIV and exposed to silica has been shown to be multiplicative [39]. The risk for adverse COVID-19 outcomes in the presence of positive HIV status is not consistently increased in those on antiretroviral treatment or with normal CD4 counts [40–42]. However, most of these studies used small convenience samples. A contrary finding was observed in the Western Cape study, which looked at 536 574 HIV-positive patients (16% of the total sample). An adjusted hazard ratio for COVID-19 mortality of 2.14 (95% CI: 1.7–2.7) was reported. This was independent of viral load and of immunosuppression [36▪].
Chronic obstructive pulmonary disease
Other chronic diseases such as chronic obstructive pulmonary disease (COPD) are likely to be prevalent due to high dust exposures in underground mining. The prevalence of emphysema reported among 43 030 autopsies conducted among Black miners between 1975 and 2014 was 12% [43]. A relative risk (RR) of 1.9 (95% CI: 1.4–2.4) for severe COVID-19 disease has been reported for those with COPD [44], with a pooled RR of 1.33 (0.77–2.31) for COVID-19-related mortality [45]. Tobacco smoking has also been associated with severe COVID-19 and adverse outcomes [46]. It is unclear, however, if smoking is an additive risk factor in addition to COPD [47].
Other mining-related factors
Other factors that may play a role include mining-related exposures associated with commodity type. Data reported from the Minerals Council in South Africa for the different mining commodities demonstrated that mortality rates varied from 2 to 0.9 to 0.7% across gold, platinum, and coal miners, respectively [5]. This was true despite a higher incidence of infection in platinum mine workers (44/1000) compared with gold mine workers (38/1000) (Fig. 3). Further analysis of these emerging trends is necessary to understand whether this may be due to exposures specific to the product being mined or due to demographic and health profiles that are unique to each type of mining.
Postinfectious sequelae of COVID-19
It is estimated that about 10% of individuals experience prolonged illness after COVID-19 and require ongoing health monitoring and support [48].
Progression to persistent/chronic lung disease
Due to the nascent nature of the disease, it is currently not possible to quantify the nature and degree of chronic lung outcomes in COVID-19 patients in general and mineworkers in particular. Emerging data, however, suggest that many experience persistent respiratory symptoms months after their initial illness [49,50]. Among 103 Italian patients, up to 52% had objective evidence of compromised activities of daily living after a mean of 16.1 days of hospitalization with COVID-19 [49]. Chronic respiratory outcomes included persistent cough, fibrotic lung disease, bronchiectasis, and pulmonary vascular disease [51,52]. This is supported by findings from long-term studies of previous Middle East Respiratory Syndrome and SARS coronavirus epidemics. In a study of 71 Middle East Respiratory Syndrome patients followed up over 15 years, 35% had reduced diffusion capacity and 38% had ground glass changes on computed tomography scans [53], whereas another study reported 52% with reduced diffusion capacity and that 12.2% had not returned to work 24 months after onset of illness [54]. Various studies show that those with preexisting chronic lung disorders are more likely to experience postinfectious sequelae and progression to chronicity of lung abnormality [29▪▪].
Fitness to work and work ability
These long-term effects of COVID-19 have a potential to adversely impact the return to work of workers in the mining sector due to the high levels of fitness required to work underground. The consequences for mineworkers with chronic disease and inability to work will be several-fold: an extended period of absence from work with loss of income, reassignment to alternate work appropriate to their level of fitness accompanied by loss of income, or permanent incapacity for work resulting in job loss. A successful recovery requires gradual rehabilitation and an individualized return to work plan [55], with comprehensive follow-up monitoring for persistent health impacts [56]. However, in a country with high levels of unemployment, such patients are likely to lose their jobs and the costs for such rehabilitation would have to be borne by patients themselves and by the public health sector.
Workers compensation
With studies showing at least 20% of COVID-19 cases estimated to be work-related [6], the South African government has accepted that, where evidence can be provided, mineworkers are entitled to compensation for a work-related infection to mitigate the consequences of acquiring the disease [57]. As of the beginning of November 2020, 3150 work-related COVID-19 claims had been submitted to the Compensation Fund by the mining sector [58]. This 6-month submission constitutes already a sizeable proportion (33%) of the overall total of 9670 claims for injuries and diseases submitted in 2018 [59]. Should a large proportion of those progressing to chronic disease also have substantial functional impairment, this will have substantial financial implications.
CONCLUSION AND AREAS FOR FUTURE RESEARCH
South African goldminers are experiencing a fourth major burden of respiratory disease as a result of their current work-related exposures, peculiar sociogeographic conditions, and health risk profile, which are likely to render them vulnerable to severe COVID-19 outcomes. Reducing SARS-CoV-2 infection transmission in the mines is essential, as are health monitoring of infected workers and close follow-up of postinfection outcomes in affected miners.
As the epidemic unfolds and knowledge of SARS-CoV-2 deepens, a better understanding of its impact on the health of mineworkers will evolve. Beyond individual factors that increase vulnerability for severe outcomes, further investigation is needed into workplace factors such as airborne transmission associated with concomitant dust exposure in different commodity sectors, ventilation, and social distancing work arrangements. The profile of the asymptomatic transmitter and the workplace factors that allow for such transmission also require further research. A better understanding of the risk of severe COVID-19 disease in miners with silicosis coexisting with other diseases (PTB, HIV, COPD) as well as the pathophysiological mechanisms involved is necessary. This is particularly important given the large examiner migrant population of those living in the rural areas of southern South Africa who continue to live with residual chronic occupational lung disease acquired in the mines.
Acknowledgements
The authors would like to thank Dr Thuthula Balfour of the Minerals Council South Africa for her assistance in obtaining access to the grey literature for the mining industry including some routine data and her comments on earlier versions of the article.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Oliver T. An address on Rand miners’ phthisis: delivered to the North of England Branch of the British Medical Association at Blyth. Br Med J 1905; 2:919–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Retief F. Chest disease in Rand miners. Lancet 1947; 1:536. [DOI] [PubMed] [Google Scholar]
- 3.Vincent M, Chemarin C, Cavalin C, et al. From the definition of silicosis at the 1930 Johannesburg conference to the blurred boundaries between pneumoconioses, sarcoidosis, and pulmonary alveolar proteinosis (PAP). Am J Ind Med 2015; 58:31–38. [DOI] [PubMed] [Google Scholar]
- 4.Rees D, Murray J, Nelson G, Sonnenberg P. Oscillating migration and the epidemics of silicosis, PTB, and HIV infection in South African gold miners. Am J Ind Med 2010; 53:398–404. [DOI] [PubMed] [Google Scholar]
- 5.Minerals Council of South Africa. COVID-19 dashboard. 2020; Johannesburg, South Africa: Minerals Council of South Africa, Available at: https://www.mineralscouncil.org.za/minerals-council-position-on-covid-19. [Last accessed 25 October 2020]. [Google Scholar]
- 6.Marinaccio A, Boccuni F, Rondinone BM, et al. Occupational factors in the COVID-19 pandemic in Italy: compensation claims applications support establishing an occupational surveillance system. Occup Environ Med 2020; 77:818–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One 2020; 15:e0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.St-Denis X. Sociodemographic determinants of occupational risks of exposure to COVID-19 in Canada. Can Rev Sociol 2020; 57:399–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Considerations for public health and social measures in the workplace in the context of COVID-19 (interim guidance). 2020; Geneva, Switzerland: WHO, Available at: https://www.who.int/publications/i/item/considerations-for-public-health-and-social-measures-in-the-workplace-in-the-context-of-covid-19. [Last accessed on 25 October 2020]. [Google Scholar]
- 10.Sood A, Pollard C, Le Suer K. Caring for miners during the coronavirus disease-2019 (COVID-19) pandemic. J Rural Health 2020; 37:165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calvimontes J, Massaro L, Araujo CHX, et al. Small-scale gold mining and the COVID-19 pandemic: conflict and cooperation in the Brazilian Amazon. Extr Ind Soc 2020; 7:1347–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godderis L, Luyten J. Challenges and opportunities for occupational health and safety after the COVID-19 lockdowns. Occup Environ Med 2020; 77:511–512. [DOI] [PubMed] [Google Scholar]
- 13.Ehrlich R, Montgomery A, Akugizibwe P, Gonsalves G. Public health implications of changing patterns of recruitment into the South African mining industry, 1973–2012: a database analysis. BMC Public Health 2017; 18:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muchiri E, Charalambous S. Minerals Council COVID-19 response and surveillance progress report. Johannesburg: Minerals Council; 2020. [Google Scholar]
- 15.Araya F. Modeling the spread of COVID-19 on construction workers: an agent-based approach. Saf Sci 2021; 133:105022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lan FY, Wei CF, Hsu YT, et al. Work-related COVID-19 transmission in six Asian countries/areas: a follow-up study. PLoS One 2020; 15:e0233588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond) 2020; 70:3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gibbs GW, Du Toit RSJ. Estimating the quartz exposure of South African gold miners. Ann Occup Hyg 2002; 46:597–607. [DOI] [PubMed] [Google Scholar]
- 19▪.Brouwer DH, Rees D. Can the South African milestones for reducing exposure to respirable crystalline silica and silicosis be achieved and reliably monitored? Front Public Health 2020; 8:107. [DOI] [PMC free article] [PubMed] [Google Scholar]; The article describes the current levels of exposure faced by mineworkers on South African mines, and their risks for pneumoconiosis.
- 20.Konecný P, Ehrlich R, Gulumian M, Jacobs M. Immunity to the dual threat of silica exposure and mycobacterium tuberculosis. Front Immunol 2018; 9:3069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Domingo JL, Marquès M, Rovira J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ Res 2020; 188:109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22▪.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584:430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study provides an important understanding of the risk factors for COVID-19 mortality, using a large database.
- 23.Churchyard GJ, Ehrlich R, teWaterNaude JM, et al. Silicosis prevalence and exposure-response relations in South African goldminers. Occup Environ Med 2004; 61:811–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steen TW, Gyi KM, White NW, et al. Prevalence of occupational lung disease among Botswana men formerly employed in the South African mining industry. Occup Environ Med 1997; 54:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trapido AS, Mqoqi NP, Williams BG, et al. Prevalence of occupational lung disease in a random sample of former mineworkers, Libode District, Eastern Cape Province, South Africa. Am J Ind Med 1998; 34:305–313. [DOI] [PubMed] [Google Scholar]
- 26.Park HH, Girdler-Brown BV, Churchyard GJ, et al. Incidence of PTB and HIV and progression of silicosis and lung function impairment among former Basotho gold miners. Am J Ind Med 2009; 52:901–908. [DOI] [PubMed] [Google Scholar]
- 27▪.Knight D, Ehrlich R, Cois A, et al. Predictors of silicosis and variation in prevalence across mines among employed gold miners in South Africa. BMC Public Health 2020; 20:829. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study provides a recent description of the risk for silicosis on South African mines.
- 28.Esposito AJ, Menon AA, Ghosh AJ, et al. Increased odds of death for patients with interstitial lung disease and COVID-19: a case–control study. Am J Respir Crit Care Med 2020; 202:1710–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29▪▪.Drake TM, Docherty AB, Harrison EM, et al. Outcome of hospitalization for COVID-19 in patients with interstitial lung disease: an international multicenter study. Am J Respir Crit Care Med 2020; 202:1656–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]; An international multicenter study, which demonstrated an increased COVID-19 mortality risk, particularly those with poor lung function and interstitial lung disease, which has important implications for miners with silicosis.
- 30.Wong AW, Fidler L, Marcoux V, et al. Practical considerations for the diagnosis and treatment of fibrotic interstitial lung disease during the coronavirus disease 2019 pandemic. Chest 2020; 158:1069–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glynn JR, Murray J, Bester A, et al. Effects of duration of HIV infection and secondary tuberculosis transmission on tuberculosis incidence in the South African gold mines. AIDS 2008; 22:1859–1867. [DOI] [PubMed] [Google Scholar]
- 32.Ndlovu N, Nelson G, Vorajee N, Murray J. 38 Years of autopsy findings in South African mine workers. Am J Ind Med 2016; 59:307–314. [DOI] [PubMed] [Google Scholar]
- 33.Ndlovu N, Musenge E, Park SK, et al. Four decades of pulmonary PTB in deceased South African miners: trends and determinants. Occup Environ Med 2018; 75:767–775. [DOI] [PubMed] [Google Scholar]
- 34.Ehrlich RI. Tuberculosis, mining and silica. Occup Environ Med 2018; 75:763–764. [DOI] [PubMed] [Google Scholar]
- 35.Maboso BM, Moyo DM, Muteba KM, et al. Occupational lung disease among Basotho ex-miners in a large outreach medical assessment programme. Occup Health Southern Afr 2020; 26:145–152. [Google Scholar]
- 36▪.Boulle A, Davies M, Hussey H, et al. Risk factors for COVID-19 death in a population cohort study from the Western Cape Province, South Africa. Clin Infect Dis 2020. ciaa1198.Available at: 10.1093/cid/ciaa1198. [Accessed 25 October 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]; The large population-based cohort study from South Africa outlining important information on vulnerability risk factors for COVID-19 mortality including pulmonary tuberculosis and HIV.
- 37.Gao Y, Liu M, Chen Y, et al. Association between tuberculosis and COVID-19 severity and mortality: a rapid systematic review and meta-analysis. J Med Virol 2021; 93:194–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sy KTL, Haw NJL, Uy J. Previous and active tuberculosis increases risk of death and prolongs recovery in patients with COVID-19. Infect Dis (Lond) 2020; 52:902–907. [DOI] [PubMed] [Google Scholar]
- 39.Corbett EL, Churchyard GJ, Clayton TC, et al. HIV infection and silicosis: the impact of two potent risk factors on the incidence of mycobacterial disease in South African miners. AIDS 2000; 14:2759–2768. [DOI] [PubMed] [Google Scholar]
- 40.Cooper TJ, Woodward BL, Alom S, Harky A. Coronavirus disease 2019 (COVID-19) outcomes in HIV/AIDS patients: a systematic review. HIV Med 2020; 21:567–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu Z, Zhang C, Wang FS. COVID-19 in people with HIV. Lancet HIV 2020; 7:e524–e526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gervasoni C, Meraviglia P, Riva A, et al. Clinical features and outcomes of HIV patients with coronavirus disease 2019. Clin Infect Dis 2020; 71:2276–2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mabila SL, Almberg KS, Friedman L, et al. Occupational emphysema in South African miners at autopsy, 1975–2014. Int Arch Occup Environ Health 2018; 91:981–990. [DOI] [PubMed] [Google Scholar]
- 44.Alqahtani JS, Oyelade T, Aldhahir AM, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS One 2020; 15:e0233147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ssentongo P, Ssentongo AE, Heilbrunn ES, et al. Association of cardiovascular disease and 10 other preexisting comorbidities with COVID-19 mortality: a systematic review and meta-analysis. PLoS One 2020; 15:e0238215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis 2020; 18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Zyl Smit R, Feldman C, Richards G, et al. South African Thoracic Society statement on obstructive airways disease and COVID-19. Afr J Thorac Crit Care Med 2020; 26:117–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Greenhalgh T, Knight M, A’Court C, et al. Management of postacute covid-19 in primary care. BMJ 2020; 370:m3026. [DOI] [PubMed] [Google Scholar]
- 49.Belli S, Balbi B, Prince I, et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived the hospitalisation. Eur Respir J 2020; 56:2002096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA 2020; 324:603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fraser E. Long term respiratory complications of covid-19. BMJ 2020; 370:m3001. [DOI] [PubMed] [Google Scholar]
- 52.National Health Service England, NHS England. Aftercare needs of inpatients recovering from COVID-19. 2020; Available at: https://www.pcrs-uk.org/sites/pcrs-uk.org/files/nhs-aftercarecovid.pdf. [Last accessed on 25 October 2020]. [Google Scholar]
- 53.Zhang P, Li J, Liu H, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res 2020; 8:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ngai JC, Ko FW, Ng SS, et al. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology 2010; 15:543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rayner C, Lokugamage A, Molokhia M. Covid-19: prolonged and relapsing course of illness has implications for returning workers. BMJ Opinion 2020; Available at: https://blogs.bmj.com/bmj/2020/06/23/covid-19-prolonged-and-relapsing-course-of-illness-has-implications-for-returning-workers/. [Last accessed on 25 October 2020]. [Google Scholar]
- 56.Gentile F, Aimo A, Forfori F, et al. COVID-19 and risk of pulmonary fibrosis: the importance of planning ahead. Eur J Prev Cardiol 2020; 27:1442–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Department of Employment and Labour. COIDA Directive on Compensation for workplace acquired corona virus disease (covid-19). 2020; Pretoria, South Africa: Department of Employment and Labour, Government Gazette 43540; available at: https://www.gov.za/sites/default/files/gcis_document/202003/43126gen193.pdf. [Last accessed on 25 October 2020]. [Google Scholar]
- 58.Department of Employment and Labour. Compensation Fund records sharp increase COVID-19 claims in the mining/iron and steel industries (official media release). Department of Employment and Labour. Johannesburg, South Africa. 2020 Available at: https://www.gov.za/speeches/employment-and-labour-continues-paying-rising-coronavirus-covid-19-claims-5-nov-2020-0000. [Last accessed on 23 November 2020]. [Google Scholar]
- 59.Rand Mutual Assurance. 2018 Annual integrated report. 2018; Johannesburg, South Africa: Rand Mutual Assurance, Available at: https://randmutual.co.za/Downloads#48935-integrated-reports. [Last accessed on 15 October 2020]. [Google Scholar]


