Abstract
Disparities in breast cancer mortality rates among older Black and Hispanic women are due in part to low participation in cancer screening. Participation in cancer screening could be affected by an array of factors including social support. Understanding the complex interplay between social support and breast cancer screening among older female adults, specifically among groups with higher mortality rates is extremely important for timely and appropriate interventions to increase survival rates. Thus, utilizing the social network theory as the conceptual framework, this study aims to examine effects of social support on receiving a mammogram among a representative sample of older adults, specifically African-American and Hispanic populations in the United States. Logistic regression models were conducted using the 2008 and 2012 Health and Retirement Study data. Findings from this study indicate that specific aspects of social support influence breast cancer screening participation among older Hispanic and non-Hispanic White women. However, this was not the case for the older Black women after adjusting for the socio-demographic factors. Given the role that family members play in the care of older adults, it is critical that social workers consider both the possible positive and negative interactions older women may have and how these interactions may affect their cancer screening behaviors. Findings can provide formative data to develop public health and social work interventions to increase positive social support and reduce negative social support by spouses and children to enhance breast cancer screening among older adults.
Keywords: social support, family support, older women, mammograms, Hispanics, Blacks, health promotion
Estimates indicate that over 1,760,000 new cases of cancer will be diagnosed, and more than 600,000 people will die from cancer in the United States in 2019 (American Cancer Society [ACS], 2019a). Approximately 21% of adults over age 65 die from all types of cancer (Centers for Disease Control and Prevention, 2017), however some racial and ethnic groups are affected more dramatically than others (ACS, 2018a, 2019a). According to the most recent data, the death rate for all cancers combined was 14% higher among African-American women compared to White women (ACS, 2016). Further, the American Cancer Society estimates that about one in three Hispanic women will be diagnosed with cancer in their lifetime (ACS, 2018b), and around 150,000 new cases of cancer were expected 2018 (ACS, 2018b).
Breast cancer
Among African-American women, breast cancer is the most commonly diagnosed cancer with 126.5 per 100,000 new cases diagnosed between 2011 and 2015 (ACS, 2019). Breast cancer death rates for African-American women are 41% higher than White women (ACS, 2019). Although White women experience higher incidence rates of breast cancer, African- American women are most likely to die from the disease (National Cancer Institute, 2018). Breast cancer is also the leading cause of cancer deaths among Hispanic women (ACS, 2018b). The female Hispanic population has a cancer diagnosis rate of 11.8 per 100,000 compared to 7.2 per 100,000 of non-Hispanic White American women (Mann, Foley, Tanner, Sun, & Rhodes, 2015). The probability of developing invasive breast cancer is five times higher among Hispanic women aged 50 and older compared to those aged 49 and younger (ACS, 2018b). These rates and estimations are a cause for concern as Hispanics and African-Americans are respectively expected to be the largest and second largest groups of older ethnic minority adults by 2050 (Passel & Cohn, 2008). Disparities in breast cancer mortality rates among specific groups are due in part to low participation in cancer screening (ACS, 2018b, 2019a). Evidence suggests that early diagnosis and treatment of breast cancer enhances survival rates (Documet et al., 2015). Participation in cancer screening could be affected by an array of factors including social support (Conway-Phillips & Janusek, 2014; Documet et al., 2015; Gamarra, Araujo Paz, & Griep, 2009).
Social Support and Breast Cancer Screening
Social support has long been suggested to have a powerful influence on health behaviors, health status, and decisions about health care (Berkman & Glass, 2000a; Heaney & Israel, 2008). Social science literature indicates that those with social support have higher health screening rates compared to those who do not have the support (Berkman & Glass, 2000a; Gamarra et al., 2009; Hvidberg, Wulff, Pedersen, & Vedsted, 2015). Social support is defined as an interactive process by which emotional, instrumental, or financial help can be obtained from the social network to which an individual belongs (Taylor, 2011; Wong & Leung, 2008). Emotional support may include listening, showing concern, enhancing esteem and building trust, while financial and instrumental supports may be provided through the sharing of money, time and labor.
The evidence on the effects of different aspects of social support on breast cancer screening has been mixed (Berkman & Glass, 2000a; Conway-Phillips & Janusek, 2014; Documet et al., 2015; Jensen, Pedersen, Andersen, & Vedsted, 2015; Messina et al., 2004a; Mishra, DeForge, Barnet, Ntiri, & Grant, 2012; Park, Kang, & Chadiha, 2018; Price et al., 2010; Rondet, Soler, Ringa, Parizot, & Chauvin, 2013). For example, social support in these studies have been operationalized as a determinant of social coherence (Conway et al., 2014) and was not predictive of mammography participation. However, Jensen et al. (2015) who defined social support as frequencies of contacts, instrumental support and emotional support found a positive association between low social support and low participation in breast cancer screening. Further, findings on Messina et al (2004a) indicated that lower levels of either emotional/informational support or positive social interactions, but not tangible support or affection, were significantly and independently associated with less frequent use of mammography. However, other studies did not find significant associations between these factors (Gamarra et al., 2009; Price et al., 2010). Possible reasons for the variance could include how social support is defined and how other factors such as age may play a role. Further, a review of the literature examining the effects of social support on breast cancer screening behavior of older adults was very limited, particularly among older African American and Hispanic women in the U.S. Much of the research that involved older women were non U.S based studies ( Farhadifar, Taymoori, Bahrami, & Zarea, 2015; Rondet et al., 2013). Further, those studies based in the U. S. were for younger populations or other ethnic populations (Documet et al., 2015; Dong, X., & Liu, 2017).
Understanding the complex interplay between social support and breast cancer screening among older adults, specifically among groups with higher mortality rates is extremely important for timely and appropriate interventions to increase survival rates. In this context, our study aims to examine effects of social support on receiving a mammogram among a representative sample of older adults, specifically African-American and Hispanic populations in the United States. We hypothesized that older female adults with positive social support from their spouses or children are more likely to receive a mammogram. Furthermore, we hypothesized that older female adults who experience negative social support from their spouses or children are less likely to receive a breast cancer screening.
Conceptual Framework
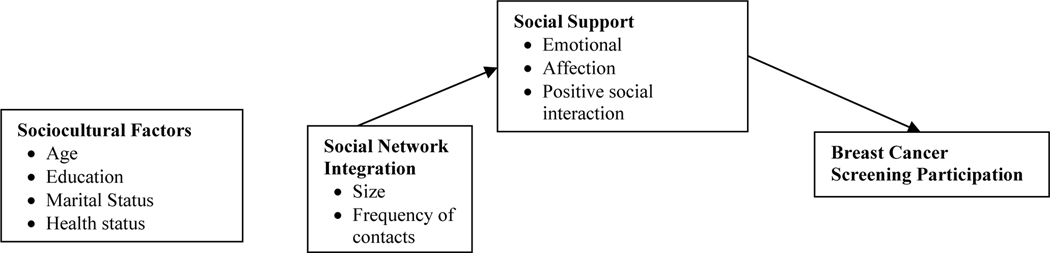
Social network theory provides the theoretical framework for this study. Social network theory seeks to explain individual behavior through examination of social network structures, including various interpersonal relationships (family, professional, religious) developed across the lifespan that “[shape] the flow of resources which determine access to opportunities and constraints on behavior” (Berkman & Glass, 2000b). To explain social networks’ influence on health behaviors, Berkman & Glass (2000b) conceptualize a model that accounts for macro level social forces/structures, mezzo level social networks and micro level “psychosocial mechanisms” which affect health through behavioral, psychological and physiological pathways. Social networks, they argue, inform behavior directly at the micro level through “(1) provision of social support, (2) social influence, (3) social engagement and attachment, and (4) access to resources and material goods” (p. 144). The micro level which includes social support is affected by the mezzo level that includes social networks and the macro level that includes socio-demographic factors. Thus, this study seeks to examine behavior at the micro level through the provision of social support to establish a baseline of knowledge instead of examining the other micro level mechanisms (social influence, social engagement and attachment, and access to resources and material goods). Social support is operationalized as emotional, affection, and positive social interaction consistent with previous literature (Jensen et al., 2015; Messina et al, 2004a). Specifically, this study will examine social support to under the impact on breast cancer screening behaviors.
While a substantial amount of evidence exists demonstrating the role of social support and cancer screening behaviors, less evidence exists to understand the role for older minority adults utilizing a national representative survey. Findings by previous work of the authors (Cadet, Burke, Stewart, Howard, & Schonberg (2017), Cadet, Stewart, & Howard, (2016), Cadet, T. (2015)) utilizing the participant sample from the Health and Retirement study indicates that psychosocial and cultural factors can both facilitate and inhibit cancer screening participation. However, it is not clear of the singular role that social support may play in cancer screening behaviors. These factors, the focus of the proposed study have been identified as potential contributing factors to health disparities, yet few studies have investigated these factors utilizing a nationally representative sample of Hispanic, African-American, and non-Hispanic White (NHW) populations. Therefore, the aim of this study is to examine the predictive effect of social support, from multiple family sources, on breast screening behaviors.
Study design and methods
This study was completed using data from the 2008 and 2012 waves of the Health and Retirement Study (HRS), a longitudinal panel study housed at The Institute for Social Research (ISR) at the University of Michigan and sponsored by the National Institute on Aging (NIA U01AG009740) HRS is a longitudinal household survey useful for the study of aging, retirement, and health among older populations in the United States (RAND Center for the Study of Aging, 2013), which includes 12 waves of data collected since 1992. Data from the HRS is publicly available at http://hrsonline.isr.umich.edu. (For further information about the HRS protocol, instrumentation, sampling strategy, statistical weighting procedures and psychosocial content, see Health and Retirement Study, 2009; Wallace & Herzog, 1995). Increased awareness of the impact of psychological and social factors on health outcomes led ISR to create the Psychosocial and Lifestyle Questionnaire in 2006, a comprehensive, self-administered survey which is distributed to half of participants every two years so that all participants complete the questionnaire once every four years (Smith et al., 2013). The Psychosocial and Lifestyle Questionnaire is included in HRS Core Survey data available at http://hrsonline.isr.umich.edu.
Health and retirement study sample.
This study utilized data from the 2008 and 2012 waves of the HRS to determine if there may be differences in participation rates across times and differences in responses to social support from family members. To be included in the analytic sample for this study, respondents were required to identify as (1) female, (2), African American/Black, Hispanic, White non-Hispanic, and (3) respond to the breast cancer screening and social support questions. The initial sample for 2008 was 43,982 and for 2012 was 51,935. The final sample for 2008 was 10,116 and for 2012 was 11,945. There was approximately 23% of missing data for the samples. Given the earlier discussion that approximately 50% of respondents would not have been selected to complete the psychosocial questionnaire of which the social support questions were part of, missing data was anticipated due to the sampling method.
Measures
Measures used in this study were extracted from the 2008 and 2012 HRS Core Survey Social support was assessed through 14 questions that referenced domestic situation (Do you have a husband, wife or partner with whom you live?), children (Do you have any children? What is the number of children in close relationship?), frequency of contact with children (How often do you meet up? Speak on the phone? Write or email?) and both negative and positive aspects of social support to evaluate the quality of participant relationships. Negative social support included four questions about social constraints: How often do they make too many demands on you? How much do they criticize you? How much do they let you know when you are counting on them? How much do they get on your nerves? Positive social support was assessed with three questions: How much do they really understand the way you feel about things? How much can you rely on them if you have a serious problem? How much can you open up to them if you need to talk about your worries? Social support questions were answered on a 1 to 4 scale with 1= a lot and 4 = not at all and were reverse coded according to HRS guidelines. Questions evaluating social network and perceived social support were developed based on (Schuster, Kessler, & Aseltine, 1990) research delineating positive and negative social support’s influence on health promotion and (Turner, Frankel, & Levin, 1983) suggestion that measures of social support and mental health outcomes must include items that identify subjective perceptions in addition to objective measures of social networks. The psychometric properties for positive social support for the spouse and children had an alpha coefficient of .82. For negative social support, the alpha coefficient was .79 for the spouse and .78 for children (Birditt, Newton, Cohen, 2004; Cranford, & Ryan, 2015; Rook, 2015; Uchino, 2009). Breast cancer screening participation was measured with one question that asked if participants had received a mammogram.
Statistical Analyses
All statistical analyses were performed using STATA 15 (StataCorp, 2015), and a p value < 0.05 was considered statistically significant. Analyses accounted for the complex multistage clustered design of the HRS sample, unequal probabilities of selection, nonresponse, and post-stratification to calculate weighted, nationally representative population estimates and standard errors to determine how specific social engagement variables influence participation in breast cancer screening. Due to the complex sample design, HRS recommends the use of weights to ensure findings from statistical analyses are representative of the U.S. population over the age of 50. The psychosocial questionnaire weight was applied to adjust for sample selection probability (Smith et al., 2013). A series of logistic regression models were conducted to examine and compare the role of social support and breast cancer screening participation for older Whites, Blacks, and Hispanics in 2008 and in 2012.
Exploratory and Bivariate Analyses
Descriptive analyses depict the sample’s characteristics. Summary statistics summarize all measures in 2008 and 2012 for participants in 2008 and 2012. See Table 1. Simple logistic regressions were conducted to determine the bivariate associations between respondent characteristics and their obtainment of a mammogram in 2008 and in 2012. See Table 2.
Table 1.
Demographic Descriptive Results
| Characteristics | 2008 (N=10,116) n (%) | 2012 (N=11,945) n (%) |
|---|---|---|
| Screening | ||
| Yes | 7,181 (71) | 8,003 (67) |
| No | 2,935 (29) | 3,942 (33) |
| Race/ Ethnicity | ||
| White | 7177 (71) | 8600 (72) |
| Black | 1761 (17) | 3106 (25) |
| Hispanic | 936 (9) | 1553 (13) |
| Marital Status | ||
| Never married | 258 (3) | 336 (3) |
| Widowed | 2651 (26) | 2608 (22) |
| Divorced | 1430 (14) | 1773 (14) |
| Married | 5768 (57) | 7229 (61) |
| Education | ||
| No degree | 1905 (19) | 1954 (16) |
| GED/ High School | 5646 (56) | 6468 (54) |
| 2–4 College | 1734 (17) | 2479 (21) |
| Master’s / Professional | 832 (8) | 1043 (9) |
| Health Status | ||
| Fair/Poor | 2783 (27) | 2689 (22) |
| Good | 3308 (33) | 3966 (33) |
| Excellent/Very Good | 4022 (40) | 5110 (43) |
Due to missing data, not all n’s add up to the N
Table 2:
Simple logistic regression model: sociodemographic factors and breast cancer screening in 2008 and 2012
| Predictor Variables | Mammogram 2008 (N=10,116) | Mammogram 2012 (N=11,945) | ||
|---|---|---|---|---|
| Category | O.R. (95% CI) | Category | O.R. (95% CI) | |
| Race/ethnicity | White | .927 (.798–1.08) | White | .888 (.758–1.04) |
| Black | 1.11 (.953–1.30) | Black | 1.24 (1.04–1.46) ** | |
| Hispanic | .797 (.668–.953) ** | Hispanic | .785 (.649–.950) ** | |
| Age | 50–64 |
.713 (.675–.754) *** | 50–64 |
.624 (.587–.665) *** |
| 65–74 |
65–74 |
|||
| 75–84 |
75–84 |
|||
| 85+ | 85+ | |||
| Marital Status | Never married |
1.47 (1.39–1.55) *** | Never married |
1.42 (1.34–1.51) *** |
| Widowed |
Widowed |
|||
| Divorced |
Divorced |
|||
| Married |
Married |
|||
| No |
No |
|||
| 1965–2014 | 1965–2014 | |||
| Education | No degree |
1.52 (1.42–1.64) *** | No degree |
1.56 (144–1.68) *** |
| (GED/HS) |
(GED/HS) |
|||
| 2–4 year college |
2–4 year college |
|||
| Masters / Professional |
Masters / Professional |
|||
| Spanish | Spanish | |||
| Health Status 2008 | Fair/ Poor |
1.34 (1.25–1.44) *** | Fair/ Poor |
1.35 (1.26–1.45) *** |
| Good |
Good |
|||
| Excellent / Very good | Excellent / Very good | |||
| Health Status 2012 | Fair/ Poor |
1.43 (1.34–1.54) *** | ||
| Good |
||||
| Excellent / Very good | ||||
indicates statistical significance at p < .05
indicates < .01
indicates p < 0.001
Multivariate Analyses
Utilizing logistic regression, we estimated 1) breast cancer screening participation in 2008 and in 2012; 2) the effect of social support factors on breast cancer screening participation in 2008 and in 2012; and 3) effects of sociodemographic characteristics on the relationship between social support factors and breast cancer screening participation in 2008 and in 2012. All predictor variables significant at the α = 0.05 level in the correlation analysis were entered in the analyses. The first analyses examined the unadjusted and adjusted effects of positive and negative social support from a husband, wife, or partner in obtaining a mammogram in 2008 among White, Black, and Hispanic participants (Table 2) or 2012 (Table 3). The second set of analyses examined the unadjusted and adjusted effects of positive and negative social support from children in obtaining a mammogram in 2008 among White, Black, and Hispanic participants (Table 4) or 2012 (Table 5). This approach provides the ability to control for sociodemographic variables, including age, marital status, education, and 2008 health status while assessing the effects of the main predictors. The odds of participating in breast cancer screening are presented and discussed.
Table 3:
Logistic Regression Examining 2008 Spousal Social Support among Participants as a Predictor of Mammogram in 2008 (N=10,116)
| Predictor Variables | White Respondents (N=7418) | White adjusteda,b | Black respondents (N=1761) | Black adjusteda | Hispanic respondents (N=937) | Hispanic adjusteda | |
|---|---|---|---|---|---|---|---|
| Positive Social Support | How much do they really understand the way you feel about things? | 1.18 (1.01–1.38) ** | 1.31 (.949–1.80) | 1.33 (.904–1.95) | 1.48 (.554–3.97) | 1.32 (.834–2.09) | 2.14 (.319–14.24) |
| How much can you rely on them if you have a serious problem? | 1.28 (1.08–1.52) ** | 1.49 (1.05–2.12) * | 1.20 (.805–1.79) | .738 (.286–1.90) | 1.65 (1.15–2.37) ** | .774 (.201–2.98) | |
| How much can you open up to them if you need to talk about your worries? | 1.27 (1.09–1.47) ** | 1.41 (1.04–1.91) * | 1.23 (.829–1.81) | .991 (.409–2.40) | 1.47 (1.01–2.14) * | 1.17 (.401–3.44) | |
| Negative Social Support | How often do they make too many demands on you? | .858 (.740-.995) * | .883 (.635–1.23) | .834 (.575–1.21) | .430 (.168–1.10) | .678 (.433–1.06) | .050 (.002–1.42) |
| How much do they criticize you? | .888 (.767–1.03) | .892 (.656–1.21) | .773 (.506–1.18) | .404 (.131–1.24) | 1.15 (.748–1.76) | .478 (.125–1.83) | |
| How much do they let you down when you are counting on them | .885 (.765–1.02) | .944 (.700–1.27) | .970 (.653–1.44) | .797 (.386–1.65) | .864 (.568–1.31) | .431 (.118–1.57) | |
| How much do they get on your nerves? | .881 (.746–1.04) | .935 (.659–1.33) | .653 (.435-.981) * | .583 (.226–1.50) | .859 (.555–1.33) | .411 (1.06–1.60) | |
-adjusted for age, marital status, education, and 2008 health status
-reference group
indicates statistical significance at p < .05
p <.01
indicates p < 0.001
Table 4:
Logistic Regression Examining 2008 Spousal Social Support among Participants as a Predictor of Mammogram in 2012 (N=11.945)
| Predictor Variables | White Respondents (N=8637) | White adjusteda,b | Black respondents (N=1750) | Black adjusteda | Hispanic respondents (N=1558) | Hispanic adjusteda | |
|---|---|---|---|---|---|---|---|
| Positive Social Support | How much do they really understand the way you feel about things? | 1.30 (1.11–1.53) *** | 1.26 (.914–1.73) | .781 (.526–1.16) | 1.13 (.545–2.36) | .954 (.605–1.50) | 1.09 (.339–3.49) |
| How much can you rely on them if you have a serious problem? | 1.36 (1.13–1.63) *** | 1.01 (.691–1.46) | 1.02 (.690–1.50) | 1.49 (.679–3.27) | 1.41 (.932–2.13) | 1.16 (.343–3.95) | |
| How much can you open up to them if you need to talk about your worries? | 1.33 (1.14–1.55) *** | 1.25 (.936–1.68) | .951 (.648–1.40) | 1.83 (.766–4.39) | 1.32 (.881–1.98) | 3.01 (.574–15.73) | |
| Negative Social Support | How often do they make too many demands on you? | .752 (.646-.875) *** | .792 (.594–1.06) | .677 (.467-.980) * | .845 (.373–1.92) | .608 (.387-.956) * | .073 (.012-.428) ** |
| How much do they criticize you? | .786 (.678-.911) *** | .813 (.607–1.09) | .861 (.581–1.28) | .988 (.383–2.55) | .897 (.583–1.38) | .087 (.016-.475) ** | |
| How much do they let you down when you are counting on them | .866 (.743–1.01) | 1.10 (.809–1.51) | 1.15 (.789–1.69) | 3.74 (1.34–10.48) | .849 (.531–1.36) | .319 (.047–2.18) | |
| How much do they get on your nerves? | .745 (.627–.884) *** | .856 (.608–1.21) | .844 (.570–1.25) | 1.07 (.395–2.90) | .910 (.581–1.43) | .639 (.237–1.73) | |
-adjusted for age, marital status, education, and 2008 health status
-reference group
indicates statistical significance at p < .05
p <.01
indicates p < 0.001
Table 5:
Logistic Regression Examining 2008 Social Support from Children among Participants as a Predictor of Mammogram in 2008 (N=10.116)
| Predictor Variables | White Respondents (N=7418) | White adjusteda,b | Black respondents (N=1761) | Black adjusteda | Hispanic respondents (N=937) | Hispanic adjusteda | |
|---|---|---|---|---|---|---|---|
| Positive Social Support | How much do they really understand the way you feel about things? | 1.09 (.956–1.23) | 1.13 (.854–1.49) | 1.18 (.857–1.63) | 1.42 (.801–2.53) | 1.04 (.738–1.46) | .782 (.399–1.53) |
| How much can you rely on them if you have a serious problem? | 1.02 (.900–1.16) | .997 (.781–1.27) | 1.34 (.970–1.84) | 1.12 (.635–1.98) | 1.03 (.726–1.47) | .852 (.476–1.53) | |
| How much can you open up to them if you need to talk about your worries? | .994 (.888–1.11) | 1.06 (.824–1.34) | 1.29 (.953–1.75) | 1.17 (.637–2.16) | 1.01 (.721–1.40) | .727 (.350–1.51) | |
| Negative Social Support | How often do they make too many demands on you? | .929 (.826–1.05) | .855 (.665–1.10) | .734 (.555–.972) * | .718 (.431–1.20) | .758 (.550–1.05) | .333 (.143–.774) * |
| How much do they criticize you? | .866 (.765–.980) * | .992 (.746–1.32) | .912 (.664–1.25) | 1.00 (.550–1.82) | 1.01 (.719–1.42) | .654 (.294–1.46) | |
| How much do they let you down when you are counting on them | .945 (.838–1.07) | .965 (.761–1.22) | .698 (.526–.927) * | .686 (.436–1.08) | .873 (.640–1.19) | .845 (.446–1.60) | |
| How much do they get on your nerves? | .939 (.827–1.06) | .943 (.719–1.24) | .717 (.542–.949) * | .897 (.510–1.58) | .803 (.580–1.11) | .505 (.233–1.09) | |
| Contact with Social Network | Meet up (include both arranged and chance meetings) | .868 (.807–.934) *** | .835 (.713–.978) * | .801 (.647–.993) * | .755 (.520–1.10) | .983 (.809–1.19) | .918 (.553–1.53) |
| Speak on the phone | 1.01 (.891–1.14) | .937 (.721–1.22) | .962 (.672–1.38) | .779 (.397–1.53) | .954 (.703–1.30) | .906 (.443–1.86) | |
| Write or email | .879 (.828–.932) *** | .851 (.743–.975) * | .954 (.814–1.12) | .893 (.674–1.18) | .866 (.729–1.03) | .715 (.413–1.24) | |
- adjusted for age, marital status, education, and 2008 health status
-reference group
indicates statistical significance at p < .05
p <.01
indicates p < 0.001
Results
Table 1 provides the study sample characteristics. More than one in every four older adults in our sample (n= 10,116) had not received a mammogram within the past two years in 2008, and one in every three older adults (n= 11,945), had not received a mammogram between 2010 and 2012. Slightly more than one-third of the sample were between the ages of 65 and 74 years of age in 2008 (37%) and in 2012 38%). The majority of the sample was married and the majority of the sample had received their GED or high school diplomas in both years (Married: 2008–57%; 2012–61%; GED/High School: 2008– 56%; 2012–54%).
Table 2 presents the results of simple logistic regression models examining socio-demographic factors and breast cancer screening participation. Hispanics were less likely than Whites to obtain a mammogram in both 2008 and in 2012 (OR=.80 [.67-.95], p<.01; OR=.79 [.65-.95], p<.01). With increasing age, there was a reduced likelihood of obtaining a mammogram in 2008 (OR=.71[.68-.75], p<.001) and in 2012 (OR=.62[.59–67], p<.001. With increasingly better health status, there was a higher likelihood of obtaining a mammogram in 2008 (OR=1.34 [1.25–1.44], p<.001) and in 2012 (OR=1.43 [1.34–1.54], p<.001.
Table 6 presents the results of the logistic regression models examining the role of spousal/partner support in 2008 and breast cancer screening participation in 2008. After controlling for the socio-demographic factors, White women had a higher likelihood of obtaining a mammogram with increasing feelings that they could rely on their spouses/partners if they had a serious problem (OR=1.49 [1.05 −2.12], p<.05) and that they could open up to spouses/partners if they needed to talk about their worries (OR=1.41[1.04–1.91], p<.05) compared to Black and Hispanic women. Prior to adjusting for socio-demographic factors, Hispanic women had also had a higher likelihood of obtaining a mammogram with increasing feelings that they could rely on their spouses/partners if they had a serious problem (OR=1.65 [1.15 −2.37], p<.01) and that they could open up to spouses/partners if they needed to talk about their worries (OR=1.47[1.01 −2.14], p<.05) compared to Whites. Also prior to adjusting for socio-demographic factors, Black women had a reduced likelihood of obtaining a mammogram with increasing feelings of spouses/partners getting on their nerves compared to Whites. However, for both Hispanic and Black women, these relationships were not significant after adjusting for socio-demographic factors.
Table 6:
Logistic Regression Examining 2008 Social Support from Children among Participants as a Predictor of Mammogram in 2012 (N=11.945)
| Predictor Variables | White Respondents (N=8637) | White adjusteda,b | Black respondents (N=1750) | Black adjusteda | Hispanic respondents (N=1558) | Hispanic adjusteda | |
|---|---|---|---|---|---|---|---|
| Positive Social Support | How much do they really understand the way you feel about things? | 1.02 (.887–1.17) | 1.43 (1.06–1.91) * | .931 (.675–1.28) | .958 (.474–1.93) | .829 (.570–1.21) | .715 (.348–1.47) |
| How much can you rely on them if you have a serious problem? | 1.04 (.908–1.20) | 1.35 (1.04–1.76) * | 1.00 (.698–1.43) | .866 (.450–1.67) | .761 (.507–1.14) | .632 (.331–1.20) | |
| How much can you open up to them if you need to talk about your worries? | .993 (.878–1.12) | 1.32 (1.03–1.70) * | 1.26 (.927–1.71) | 1.18 (.621–2.24) | .680 (.468–.989) * | .731 (.355–1.51) | |
| Negative Social Support | How often do they make too many demands on you? | 1.07 (.940–1.21) | .886 (.685–1.15) | .989 (.742–1.32) | .839 (.488–1.44) | .966 (.671–1.39) | .342 (.162–.719) ** |
| How much do they criticize you? | .917 (.802–1.05) | 1.04 (.773–1.41) | 1.13 (.848–1.51) | .913 (.499–1.67) | 1.01 (.711–1.42) | .550 (.257–1.18) | |
| How much do they let you down when you are counting on them | .926 (.813–1.05) | .908 (.697–1.18) | .838 (.628–1.12) | .845 (.498–1.43) | 1.12 (.790–1.59) | 1.12 (.585–2.16) | |
| How much do they get on your nerves? | .957 (.833–1.10) | .913 (.678–1.23) | .931 (.696–1.25) | 1.23 (.628–2.42) | 1.00 (.715–1.40) | .746 (.317–1.75) | |
| Contact with Social Network | Meet up (include both arranged and chance meetings) | .898 (.829–.974) ** | 1.05 (.869–1.27) | 1.04 (.850–1.28) | 1.02 (.717–1.46) | 1.05 (.843–1.31) | 1.00 (.600–1.68) |
| Speak on the phone | 1.00 (.873–1.15) | .987 (.725–1.34) | .837 (.617–1.13) | .786 (.380–1.63) | .775 (.490–1.23) | .747 (.384–1.46) | |
| Write or email | .841 (.790–.895) *** | .769 (.672–.880) *** | .854 (.733–.995) * | .775 (.568–1.06) | .947 (.785–1.14) | .794 (.523–1.20) | |
-adjusted for age, marital status, education, 2008 health status, and income
-reference group
indicates statistical significance at p < .05
p <.01
indicates p < 0.001
Table 6 presents the results of the logistic regression models examining the role of spousal/partner support in 2008 and breast cancer screening participation in 2012. After controlling for the socio-demographic factors, only Hispanic women had a reduced likelihood of obtaining a mammogram with increasing feelings that their spouse/partner made too many demands on them (OR=.07 [.01 −.43], p<.01) and criticized them (OR=.09 [.02-.48], p<.01. Prior to adjusting for socio-demographic factors, Black women had a reduced likelihood of obtaining a mammogram with increasing feelings that that their spouse/partner made too many demands on them (OR=.68 [.47-.98], p<.05) compared to Whites. Prior to adjusting for socio-demographic factors, White women had an increased likelihood of obtaining a mammogram for positive social support and decreased likelihood for negative social support compared to Blacks and Hispanics.
Table 4 presents the results of the logistic regression models of support from children in 2008 and breast cancer screening participation in 2008. While controlling for socio-demographic factors, Hispanic women had a reduced likelihood of obtaining a mammogram with increasing feelings that their children made too many demands on them (OR=.33 [.34–77], p<.05 compared to Whites. For White women, there was a reduced likelihood of obtaining a mammogram with increasing contact with children through meetings (OR=.84 [.71– .98], p<.05 and increasing letters or email (OR=.85 [.74–.98], p<.05 compared to Blacks and Hispanics. Prior to adjusting for socio-demographic factors, Black women had a reduced likelihood of obtaining a mammogram with increasing feelings of negative social support from their children and with increasing contacts with children with meetings compared to Whites.
Table 5 presents the results of the logistic regression models of support from children in 2008 and breast cancer participation in 2012. While controlling for socio-demographic factors, Hispanic women had a reduced likelihood of obtaining a mammogram (OR=.73 [.36– 1.51], p<.05 compared to Whites. For White women, after controlling for socio-demographic factors, each aspect of positive social support resulted in an increased likelihood of obtaining a mammogram with increasing positive social support. Specifically, with increasing feeling that their children understood them (OR=1.43 [1.06–1.91], p<.05), increasing feelings that they could rely on children if they had a serious problem (OR=1.35 [1.04–1.76], p<.05) and increasing feelings that they can open up to their children if they need to talk about their worries (OR=1.32 [1.03–1.70], p<.05), White women were more likely to obtain a mammogram compared to Blacks and Hispanics. Prior to adjusting for socio-demographic factors, Black women were less likely to obtain a mammogram with increasing contact with children through letters or email compared to Whites.
Discussion
Our findings partially confirmed the hypotheses of the study. Overall, findings are consistent with results from Messina and colleagues’ (2004b) and Jensen and colleagues’ (2015) studies, affirming a positive relationship between social support and breast cancer screening. Although there are not definitive conclusions in the literature about reasons for positive effects of social support on cancer screening behaviors, social network theory provides a framework to consider. Based on this theory, social networks can affect health behaviors through social support and social influence. For instance, pressure by the social network for cancer screening could increase the likelihood of receiving a mammogram (Documet et al., 2015). Moreover, social support can enhance self-esteem and consequently self-care, resulting in an increase in receiving a mammogram (Gamarra et al., 2009; Jensen et al., 2015). There are also discussions about diminishing effects of social support on stress and anxiety associated with breast cancer screening (Documet et al., 2015; Jensen et al., 2015).
Consistent with the conceptual framework, findings from this study indicate that specific aspects of social support influence breast cancer screening participation among older Hispanic and non-Hispanic White women. However, this was not the case for the older Black women in this sample after adjusting for the socio-demographic factors. The lack of a statistically significant relationship between social support and breast cancer screening among older African-American women could be partly due to limited indicators that we explored for social support and complexity of studies on preventive health behaviors among older adults (Burke et al., 2018; Caillet et al., 2011; Lee, Leipzig, & Walter, 2013). Further, it is well recognized that Black women tend to experience higher levels of stress than other women (Schulz et al., 2000). It is possible that questions about support do not precisely address the stress levels or that Black women experience emotional distancing as a result of stress which would support the lack of statistical significance in this study (Black & Woods-Giscombe, 2012).
In this study, consistent with the literature, suggests that social support may help to relieve the stress associated with cancer screening. Specifically, findings from this study suggest that indicators of positive social support by children and spouses were associated with an increase in odds of receiving a mammogram among non-Hispanic Whites. Moreover, indicators of negative social support by children and spouses including high levels of demands were associated with a decrease in odds of receiving a mammogram among Hispanic older adults. Hispanic women who feel pressure from their spouses and children may possibly feel too overwhelmed to consider their health needs and in this case getting a mammogram.
Interestingly, higher levels of contact with children were associated with lower likelihood of receiving a mammogram among older non-Hispanic White women in our sample. Higher levels of contact between older non-Hispanic White women and their children could be an indication of social burden instead of social support in terms of higher levels of demands from children. This perspective can explain the negative relationship between breast cancer screening and contact with children among older non-Hispanic White women in our sample.
Limitations
Results from this study should be interpreted with caution. Specifically, HRS does not provide information to ensure that respondents’ self-report of cancer screening or other health behaviors are accurate. In addition, findings may not be applicable to older Hispanic women, due to the diversity of the Hispanic population and self-selection of older Hispanics participating in the survey (Angel & Whitfield, 2007; Royner, Casten, & Harris, 2013). Empirical literature demonstrates that because of the representation of the range of countries from which Hispanics come, they have differing levels of health knowledge, beliefs, and patterns of service utilization that impact their health behaviors, such as cancer screening (Angel & Whitfield, 2007; Pinheiro et al., 2009). Further, we chose to examine factors in 2008 and their relationship to cancer screening behaviors in 2008 and 2012 to develop a baseline of knowledge to understand if previous factors affect future behaviors. Future research will examine similar factors using 2016 to gain a more comprehensive view of social support and cancer screening behaviors.
Social support is a complex concept and examined aspects of it in our study were limited to the available data in the selected secondary dataset. Moreover, although we controlled for demographic factors, other factors that we have may not accounted for could have moderated the impact of social support on breast cancer screening in our sample. In addition to factors that could have moderated the impact of social support, there may be additional factors that need to be considered within the context of social support especially in light of the non-significant findings for Black women.
Conclusions and Recommendations
Despite the limitations of this study, this study contributes to knowledge base on the possible roles of social support on receipt of mammograms for older women. Given the role that family members play in the care of older adults, it is critical that social workers consider both the possible positive and negative interactions older women may have and how these interactions may affect their cancer screening behaviors. Findings from this study can provide formative data to develop public health and social work interventions to increase positive social support and reduce negative social support by spouses and children to enhance breast cancer screening among older adults. Public health social workers have unique training to work with both the older adult, their family members and the community at large. Further, social workers should conduct comprehensive assessments to understand the dynamics of their relationships with family to determine if additional resources may be needed if the family interactions are not helpful. They can also provide psychosocial education and information to family members about the importance of healthy behaviors and the benefits which can include facilitating cancer screening participation. Finally, they can work with providers in community-based organization that may see older adults for other reasons to educate them about the findings from this study. Future interventions developed to increase cancer screening rates or adoption of other preventative health practices are encouraged to account for complex and varied influences of social support, informed by race/ethnicity, to increase the likelihood of positive outcomes.
Figure 1.
Conceptual models of how social networks impact health (Adapted from Berkman & Glass, 2000b).
Acknowledgements –
Simmons University Fund for Research and Simmons University School of Social Work Research Fellowship
Footnotes
Declaration of interest statement – The authors declare that they have no conflict of interest.
Contributor Information
Tamara Cadet, Simmons University School of Social Work, 300 The Fenway, Boston, MA 02115, 617-521-3981; Lecturer on Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Oral Health Policy and Epidemiology, Boston, MA.
Shanna L. Burke, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, AHC5 564, Miami, Florida 33199, 305-348-7462.
Mitra Naseh, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, AHC5 564, Miami, Florida 33199.
Adrienne Grudzien, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, AHC5 564, Miami, Florida 33199.
Rebecca S. Kozak, Simmons University School of Social Work, 300 The Fenway, Boston, MA 02115.
Jessica Romeo, Hope House Addiction Services, 8 Farnham Street, Boston, MA 02119.
Karen Bullock, Department Head, North Carolina State University, School of Social Work, 205 1911 Building 217, Campus Box 7639, Raleigh, NC 27695, 919-515-0438.
Cindy Davis, University of the Sunshine Coast, Professor of Social Work and Associate Dean of Learning & Teaching Faculty of Arts, Business & Law, D1.09, Queensland, Australia.
References
- American Cancer Society. (2018a). Cancer Facts & Figures 2018. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf
- American Cancer Society. (2018b). Cancer Facts & Figures for Hispanics/Latinos 2018–2020. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/cancer-facts-and-figures-for-hispanics-and-latinos-2018-2020.pdf
- American Cancer Society. (2019a). Cancer Facts & Figures for African Americans 2019–2021. American Cancer Society, 40. [Google Scholar]
- American Cancer Society. (2019b). Facts & Figures 2019: US Cancer Death Rate has Dropped 27% in 25 Years. Retrieved May 6, 2019, from https://www.cancer.org/latest-news/facts-and-figures-2019.html
- Angel JL, & Whitfield KE (2007). Setting the stage: Hispanic health and aging in America. In The health of aging Hispanics: The Mexican-origin population (pp. 1–14). New York, NY: Springer. [Google Scholar]
- Berkman L, & Glass T. (2000a). Social integration, social networks, social support, and health. In Berkman L & Kawachi I (Eds.), Social Epidemiology (pp. 137–173). Retrieved from https://scholar.google.com/scholar?hl=en&as_sdt=0%2C10&q=Social+integration%2C+social+networks%2C+social+support%2C+and+health&btnG= [Google Scholar]
- Berkman L, & Glass T. (2000b). Social integration, social networks, social support, and health. In Social Epidemiology (pp. 137–173). New York, NY: Oxford University Press. [Google Scholar]
- Birditt KS, Newton NJ, Cranford JA, & Ryan LH (2015). Stress and negative relationship quality among older couples: implications for blood pressure. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71(5), 775–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black AR, & Woods-Giscombe C. (2012). Applying the Stress and “Strength” Hypothesis to Black women’s breast cancer screening delays. Stress and Health : Journal of the International Society for the Investigation of Stress, 28(5), 389–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke SL, Hu T, Naseh M, Fava NM, O’Driscoll J, Alvarez D, … Duara R. (2018). Factors influencing attrition in 35 Alzheimer’s Disease Centers across the USA: A longitudinal examination of the National Alzheimer’s Coordinating Center’s Uniform Data Set. Aging Clinical and Experimental Research. 10.1007/s40520-018-1087-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadet T. (2015). The Relationship Between Psychosocial Factors and Breast Cancer Screening Behaviors of Older Hispanic Women. Social Work in Public Health, 30(2), 207–223. [DOI] [PubMed] [Google Scholar]
- Cadet T, Stewart K, & Howard T. (2016). Psychosocial Correlates of Cervical Cancer Screening Among Older Hispanic Women. Retrieved from https://ncbi.nlm.nih.gov/labs/articles/27960632/ [DOI] [PMC free article] [PubMed]
- Cadet TJ, Burke SL, Stewart K, Howard T, & Schonberg M. (2017). Cultural and emotional determinants of cervical cancer screening among older Hispanic women. Health Care for Women International, 38(12), 1289–1312. 10.1080/07399332.2017.1364740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caillet P, Canoui-Poitrine F, Vouriot J, Berle M, Reinald N, Krypciak S, … Paillaud E. (2011). Comprehensive Geriatric Assessment in the Decision-Making Process in Elderly Patients With Cancer: ELCAPA Study. Journal of Clinical Oncology, 29(27), 3636–3642. 10.1200/JCO.2010.31.0664 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Older Persons’ Heath. Retrieved May 20, 2019, from https://www.cdc.gov/nchs/fastats/older-american-health.htm
- Cohen S. (2004). Social relationships and health. American Psychologist, 59, 676–684. [DOI] [PubMed] [Google Scholar]
- Conway-Phillips R, & Janusek L. (2014). Influence of sense of coherence, spirituality, social support and health perception on breast cancer screening motivation and behaviors in African American women. ABNF Journal, 25(3), 72–79. [PubMed] [Google Scholar]
- Documet P, Bear TM, Flatt JD, Macia L, Trauth J, & Ricci EM (2015). The association of social support and education with breast and cervical cancer screening. Health Education & Behavior, 42(1), 55–64. 10.1177/1090198114557124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, & Liu A. (2017). Variations between sources of social support and cancer screen behaviors in US Chinese older adults. The Journals of Gerontology: Series A, 72(suppl_1), S26–S31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhadifar F, Taymoori P, Bahrami M, & Zarea S. (2015). The relationship of social support concept and repeat mammography among Iranian women. BMC women’s health, 15, 92. 10.1186/s12905-015-0253-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarra CJ, Araujo Paz EP, & Griep RH (2009). Social support and cervical and breast cancer screening in Argentinean women from a rural population. Public Health Nursing, 26(3), 269–276. 10.1111/j.1525-1446.2009.00779.x [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. (2009). Psychosocial and lifestyle data overview. Retrieved from http://hrsonline.isr.mich.edu
- Heaney CA, & Israel BA (2008). Social networks and social support. In Glanz K, Rimer BK, & Viswanath K (Eds.), Health behavior and health education: Theory, research, and practice (4th edition, p. 189). Retrieved from https://scholar.google.com/scholar?hl=en&as_sdt=0%2C10&q=Social+networks+and+social+support.+Health+behavior++and+health+education%3A+Theory%2C+research%2C+and+practice&btnG= [Google Scholar]
- HRS Staff. (2011). Sample Sizes and Response Rates. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf.
- HRS Staff. (2017). Sample Sizes and Response Rates. Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf
- Hvidberg L, Wulff CN, Pedersen AF, & Vedsted P. (2015). Barriers to healthcare seeking, beliefs about cancer and the role of socio-economic position. A Danish population-based study. Preventive Medicine, 71, 107–113. 10.1016/j.ypmed.2014.12.007 [DOI] [PubMed] [Google Scholar]
- Jensen LF, Pedersen AF, Andersen B, & Vedsted P. (2015). Social support and non-participation in breast cancer screening: A Danish cohort study. Journal of Public Health, 38(2), 335–342. 10.1093/pubmed/fdv051 [DOI] [PubMed] [Google Scholar]
- Lee SJ, Leipzig RM, & Walter LC (2013). “When will it help?” Incorporating lagtime to benefit into prevention decisions for older adults. JAMA, 310(24), 2609–2610. 10.1001/jama.2013.282612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann L, Foley KL, Tanner AE, Sun CJ, & Rhodes SD (2015). Increasing Cervical Cancer Screening Among US Hispanics/Latinas: A qualitative systematic review. Journal of Cancer Education, 30(2), 374–387. 10.1007/s13187-014-0716-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina CR, Lane DS, Glanz K, West DS, Taylor V, Frishman W, & Powell L. (2004a). Relationship of social support and social burden to repeated breast cancer screening in the women’s health initiative. Health Psychology, 23(6), 582–594. 10.1037/0278-6133.23.6.582 [DOI] [PubMed] [Google Scholar]
- Messina CR, Lane DS, Glanz K, West DS, Taylor V, Frishman W, & Powell L. (2004b). Relationship of Social Support and Social Burden to Repeated Breast Cancer Screening in the Women’s Health Initiative. Health Psychology, 23(6), 582–594. 10.1037/0278-6133.23.6.582 [DOI] [PubMed] [Google Scholar]
- Mishra SI, DeForge B, Barnet B, Ntiri S, & Grant L. (2012). Social determinants of breast cancer screening in urban primary care practices: A community-engaged formative study. Women’s Health Issues, 22(5), e429–e438. 10.1016/j.whi.2012.06.004 [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2018). Cancer Statistics. Retrieved May 15, 2019, from National Cancer Institute website: https://www.cancer.gov/about-cancer/understanding/statistics [Google Scholar]
- Ofstedal M, Weir D, Chen K, & Wagner J. (2011, June). Updates to HRS Sample Weights Report. Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/dr-013.pdf [Google Scholar]
- Park S, Kang JY, & Chadiha LA (2018). Social network types, health, and health-care use among South Korean older adults. Research on Aging, 40(2), 131–154. 10.1177/0164027516682814 [DOI] [PubMed] [Google Scholar]
- Passel JS, & Cohn D. (2008). U.S. Population Projections: 2005–2050 | Pew Research Center. Retrieved from Pew Research Center website: https://www.pewsocialtrends.org/2008/02/11/us-population-projections-2005-2050/
- Pinheiro PS, Sherman RL, Trapido EJ, Fleming LE, Huang Y, Gomez-Marin O, & Lee D. (2009). Pinheiro PS, Sherman RL, Trapido EJ, Fleming LE, Huang Y, Gomez-Marin O, & Lee D (2009). Cancer incidence in first generation U.S. Hispanics: Cubans, Mexicans,. [DOI] [PubMed] [Google Scholar]
- Price MA, Butow PN, Charles M, Bullen T, Meiser B, McKinley JM, … Phillips K-A (2010). Predictors of breast cancer screening behavior in women with a strong family history of the disease. Breast Cancer Research and Treatment, 124(2), 509–519. 10.1007/s10549-010-0868-1 [DOI] [PubMed] [Google Scholar]
- RAND Center for the Study of Aging. (2013). RAND HRS Data Documentation. Retrieved from RAND website: http://hrsonline.isr.umich.edu/index.php?p=showdesc
- Rondet C, Soler M, Ringa V, Parizot I, & Chauvin P. (2013). The role of a lack of social integration in never having undergone breast cancer screening: Results from a population-based, representative survey in the Paris metropolitan area in 2010. Preventive Medicine, 57(4), 386–391. 10.1016/j.ypmed.2013.06.016 [DOI] [PubMed] [Google Scholar]
- Rook KS (2015). Social networks in later life: Weighing positive and negative effects on health and well-being. Current Directions in Psychological Science, 24, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royner BW, Casten RJ, & Harris LF (2013). Cultural diversity and views on Alzheimer’s disease in older African Americans. Alzheimer Disease and Associated Disorders, 27(2), 133–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz A, Israel B, Williams D, Parker E, Becker A, & James S. (2000). Social inequalities, stressors and self reported health status among African American and white women in the Detroit metropolitan area. Social Science & Medicine, 51(11), 1639–1653. [DOI] [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, & Aseltine RH (1990). Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology, 18(3), 423–438. [DOI] [PubMed] [Google Scholar]
- Smith J, Fisher G, Ryan L, Clarke P, House J, & Weir D. (2013, February). Psychosocial and Lifestyle Questionnaire 2006–2010 Documentation Report Core Section LB. Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/HRS2006-2010SAQdoc.pdf
- StataCorp. (2015). Stata Statistical Software: Release 14. Retrieved from http://www.stata.com/new-in-stata/
- Taylor SE (2011). Social support: A review. In Friedman HS (Ed.), The Oxford handbook of health psychology (pp. 189–214). 10.1093/oxfordhb/9780195342819.013.0009 [DOI] [Google Scholar]
- Turner RJ, Frankel BG, & Levin DM (1983). Social support: Conceptualization, measurement, and implications for mental health. Research in Community & Mental Health, 3, 67–111. [Google Scholar]
- Uchino BN (2009). Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Sciences, 4, 236–255. [DOI] [PubMed] [Google Scholar]
- Wallace RB, & Herzog AR (1995). Overview of the Health Measures in the Health and Retirement Study. The Journal of Human Resources, 30, S84–S107. 10.2307/146279 [DOI] [Google Scholar]
- Wong DFK, & Leung G. (2008). The functions of social support in the mental health of male and female migrant workers in China. Health & Social Work, 33(4), 275–285. 10.1093/hsw/33.4.275 [DOI] [PubMed] [Google Scholar]