Abstract
Many people with dementia, supported by family carers, prefer to live at home and may rely on homecare support services. People with dementia are also often living with multimorbidities, including cancer. The main risk factor for both cancer and dementia is age and the number of people living with dementia and cancer likely to rise. Upskilling the social care workforce to facilitate more complex care is central to national workforce strategies and challenges. Training and education development must also respond to the key requirements of a homecare workforce experiencing financial, recruitment and retention difficulties. This systematic review of reviews provides an overview of dementia and cancer training and education accessible to the homecare workforce. Findings reveal there is a diverse range of training and education available, with mixed evidence of effectiveness. Key barriers and facilitators to effective training and education are identified in order to inform future training, education and learning development for the homecare workforce supporting people with dementia and cancer.
Keywords: homecare, multimorbidity, dementia and cancer, training and education
Introduction
Among people with dementia, there is an equally high prevalence of comorbid conditions (Bunn et al., 2016; Collerton, Davies, & Jagger, 2009). It is already established that advancing age increases the risk of dementia and that this parallels cancer (Cancer Research UK, 2015; Maddams, Utley, & Moller, 2012). While the number of people living with dementia and cancer is likely to rise, there is limited evidence documenting the implications for health and social care services (McWilliams et al., 2017, 2018). Many people with dementia prefer to remain at home for as long as possible (Alzheimer’s Society, 2016) and may rely on the support of homecare workers (Hussain & Manthorpe, 2012). While the full impact of dementia with cancer – and wider multimorbidity – is yet to be seen, people with dementia and cancer have greater healthcare needs and poorer clinical outcomes (McWilliams et al., 2017). This increases the demand for homecare services and enhances role-complexity. There is currently only very limited understanding of enhanced supportive care needs (Bunn et al., 2016; Hopkinson, Milton, & King, 2016; Wongrakpanich, Hurst, & Bustamante, 2017) and the training and education resources required by the homecare workforce. A better understanding of how to provide accessible, targeted and relevant training and educational is essential. This is particularly important given the demographics of the homecare workforce: the majority of homecare workers are predominately female, with a broad age range between 45 and 54 and with often limited education, low learner-confidence and few qualifications (Cooper, Cenko, Dow, & Rapaport, 2017).
The homecare sector
Upskilling the social care workforce is central to national workforce strategies and challenges (Department of Health, 2012; House of Commons, 2018; Scottish Government, 2017). Homecare delivery has rich potential for improving population health. Targeted training and education may significantly enhance the quality of care and lead to efficiency and cost savings in other parts of the health care system (Jefferson et al., 2018). Providing the tools necessary to engage fully with the homecare worker role may facilitate the more complex care required for people living with dementia and cancer and wider multimorbidities and reduce inequalities of outcomes (Bennett, Honeyman, & Bottery, 2018; Courtier, Milton, King, Tope, & Morgan, 2016; Finucane et al., 2018).
At the same time, training and education development must be cognisant of known difficulties within this sector. Homecare providers in the UK have a high staff turnover, are often risk-averse and unwilling to move away from time-and-task-based approaches to homecare delivery (Jefferson et al., 2018). While basic training may be provided, staff shortages may also prevent the release of staff for enhanced training, illustrating limited prioritisation and difficulties ring-fencing training and education (Clarkson et al., 2017). Low pay and poor working conditions combine to highlight a care system and workforce in crisis (Elliot, Stirling, Martin, Robinson, & Scott, 2016; National Audit Office, 2018; Samsi et al., 2017). The care market is also showing signs of stress in the face of unrealistic tenders and resultant market instability. Jefferson et al. (2018) report that more experienced providers are exiting this market sector. The ‘race to the bottom price’ means that homecare providers often bid for contracts on a lowest-fee-wins basis but then exit the local market when they find the margins are too small to deliver care (Hall et al., 2017). To some extent, exits are currently offset by new market entrants, mitigating full impact. The full effect of this is yet to be seen (Jefferson et al., 2018). Wider tensions include limited hospital and community care capacity and reliance on unpaid family care at home with homecare worker support (Scrutton & Brancati, 2016; Witham, Haigh, Mitchell, & Beddow, 2017).
Inadequate education for both family and professional carers is a key problem (Car et al., 2017). In the dementia and cancer fields, there is a current, fast-paced, demand for flexible, open-access (and often online) training and education for health and social care professionals providing care (Clarkson et al., 2017; Hughes, Preston, & Payne, 2016). In the Scottish social care sector, the workforce is now required (within a specified time period) to achieve qualifications which enable registration with the Scottish Social Services Council. The use of IT is often commended for consideration by employers who have to balance staff time with training . While this does not necessarily reflect the totality of training and education available, it does reflect a strong trend. At the same time, workforce readiness to engage in e-learning and technology-assisted training can be undermined by other difficulties (Clarkson et al., 2017). This may include lack of support, minimal or limited feedback and online access difficulties. Clarkson et al. (2017) in particular report difficulties attributable to the development of the e-tool, difficulties with software, limited understanding by the care provider and a workforce not yet ready to fully to engage in e-learning and technology-assisted education interventions. Technological knowledge and access requirements alongside lack of education support can be mediating factors negatively affecting learning motivation.
There is a need to better understand the facilitators and barriers to training and education; what works well for the homecare workforce; what works in the homecare context and what adaptations may be required for multimorbidities such as coexisting dementia and cancer. To our knowledge, no published study has explored the training and education needs of homecare workers supporting people with dementia and cancer. Understanding the current evidence will provide guidance on how training and education could be designed and delivered in future. In order to begin to address this gap in the evidence, this systematic review of reviews aims to:
Collate and synthesise the findings of systematic reviews on dementia and cancer training and education accessible to the homecare workforce.
Identify key themes, facilitators and barriers in the training and education for homecare workers.
Highlight potential gaps in provision for homecare workers, and areas for further development and research.
Methods
This is a systematic review of reviews (Smith, Devane, Begley, & Clarke, 2011). This ‘umbrella review’ (Loannidis, 2009) of reviews provides a wider picture of the research field and highlights where more research is needed (Thomson, Russell, Becker, Klassen, & Hartling, 2010). The review protocol was submitted to PROSPERO (CRD42018103963) prior to the search process. This ensured topic, approach and search strategy were clear a priori, any findings could be linked back to the given protocol and is recognised as good practice (Pieper, Puljak, Lorenzo, & Minozzi, 2018; Shea, Grimshaw, & Wells, 2017).
Search and selection strategy
The starting point was identified as two databases for systematic reviews: the Cochrane Database of Systematic Reviews (CDSR) and the Database of Reviews of Effects (DARE). The search was also broadened to other databases for more recent and interdisciplinary studies: (1) MEDLINE; (2) CINAHL Complete (2016); (3) Education Resource Information Centre (ERIC); (4) WebofScience; (5) PsycINFO; (6) Applied Social Science Index and Abstracts (ASSIA); (7) International Bibliography of Social Sciences (IBSS).
An explicit statement of the inclusion and exclusion criteria is provided in Table 1. The professional role focus taken necessarily excludes volunteer caregiving, informal or family caregiving, any education and training for informal or family caregivers, and any education or training for people with dementia, cancer or comorbidities. The start date of 2010 was chosen to align with key policy initiatives (Department of Health, 2009, 2012) and is within the timeline of the first Dementia Strategy in Scotland (Scottish Government, 2010), addressing the support needs of carers, adequacy of workforce skills and knowledge and need for increases in training and education provision. Reviews written in English, or with English translations, are included in the search strategy.
Table 1.
Search inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| Paid health and/or social care professional homecare workforce providing home/house care, mixed care, personalised, palliative or hospice at homecare. All types of dementia and cancer. Reporting the results of training and education interventions accessible to the homecare workforce. Systematic reviews and other analytical reviews. Published since 2009, in English or with English translation available. | Informal, volunteer or family caregiversTraining or education for informal, volunteer or family caregivers. Training or education for people with dementia or cancer or comorbidities. Scoping or non-systematic literature reviews. Published prior to 2010. Published in a language other than English or English translation. |
Explicit statement of the search terms can be found in Tables 2 and 3. For the general databases, an additional layer of searching was required to ensure the search narrowed to systematic reviews and reviews systematic in nature (Montori, Wilczynski, Morgan, & Haynes, 2005; Wilczynski, Haynes, & The Hedges team, 2007). As this is a review of reviews, employing strict analytical and intellectual rigour, grey literature was not included in the search protocol.
Table 2.
Search terms for CDSR & DARE.
| Dementia | Cancer | Education |
|---|---|---|
| Dementia | Cancer | Education |
| Alzheimer* | Comorbidities | Staff knowledge |
| Vascular dementia | Training | |
| Lewy body | Home health | |
| Frontotemporal | Homecare* |
CDSR: Cochrane Database of Systematic Reviews; DARE: Database of Reviews of Effects.*This acts as a placeholder or wildcard for other search terms that may relate or be similar, so will pick up.
Table 3.
Search terms for CINAHL, MEDLINE, PSYCHINFO, ERIC, Web of Science, ASSIA & IBSS.
| Systematic review | Dementia | Cancer | Education |
|---|---|---|---|
| Systematic review | Dementia | Cancer | Education |
| Review | Alzheimer* | Comorbidities | Staff knowledge |
| Vascular dementia | Training | ||
| Lewy body | Homecare* | ||
| Frontotemporal | Home health |
ASSIA: Applied Social Science Index and Abstracts; ERIC: Education Resource Information Centre, IBSS: International Bibliography of Social Sciences.*This acts as a placeholder or wildcard for other search terms that may relate or be similar, so will pick up.
Quality appraisal
Quality assessments were conducted independently (Pollock, Fernandes, & Hartling, 2017) by two project team members, with a process for reaching consensus in cases of disagreement. The AMSTAR 2 checklist was used to assess the quality of the selected reviews. To promote transparency (Pollock et al., 2017) a table is provided (Table 4) showing each review result, question by question, with first reviewer, second reviewer and the consensus outcomes reached.
Table 4.
AMSTAR 2 results.
| Authors | Clarkson et al. (2017)H | Cooper et al. (2017)M | Cummings et al. (2011) | D’Astous et al. (2017) M | Eggenberger et al. (2013) H | Elliot et al. (2012) M | Goeman and Koch (2016) M | Herber and Johnston (2013) M | Kim and Park (2017) H | Morgan et al. (2011) M | Raymond et al. (2014) M | Surr et al. (2017) M | Toot et al. (2017) M |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Did the research questions and inclusion criteria for the review include components of PICO? | Y YY | N N N | N N N | N N N | N N N | N N N | N N N | N N N | Y Y Y | N N N | P P P | P P P | P N P |
| (2) Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review? | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y YY |
| (3) Did the review authors explain their selection of the study designs for inclusion in the review? | Y Y Y | Y P P | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | N N N | Y N Y | P P P | P P P | Y Y Y | Y YY |
| (4) Did the review authors use a comprehensive literature search strategy? | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | P Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y YY |
| (5) Did the review authors perform study selection in duplicate? | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | CA CA CA | Y Y Y | CA CA CA | CA CA CA | YCAY | Y YY |
| (6) Did the review authors perform data extraction in duplicate? | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | PCACA | CA CA CA | CA CA CA | Y Y Y | Y Y Y | CA CA CA | Y Y Y | Y YY |
| (7) Did the review authors provide a list of excluded studies and justify the exclusion? | P Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | P Y P | Y Y Y | Y P P | N N N | P P P | Y Y Y | Y YY |
| (8) Did the review authors describe the included studies in adequate detail? | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y P P | Y Y Y | Y Y Y | Y YY |
| (9) Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review? | Y Y Y | N N N | Y Y Y | N N N | Y Y Y | PCAP | Y Y Y | Y Y Y | Y Y Y | N N N | CA CA CA | N P P | N N N |
| (10) Did the review authors report on the sources of funding for studies included in the review? | N N N | N N N | N N N | N N N | N N N | N N N | N N N | N N N | N N N | N N N | N N N | N N N | N N N |
| (11) If meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results? | NA NA NA | NA NA NA | Y Y Y | NA NA NA | NA NA NA | NA NA NA | NA NA NA | NA NA NA | Y Y Y | NA NA NA | NA NA NA | NA NA NA | Y Y Y |
| (12) If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis other evidence synthesis? | NA NA NA | NA NA NA | Y Y Y | NA NA NA | NA NA NA | NA NA NA | NA NA NA | NA NA NA | Y Y Y | NA NA NA | NA NA NA | NA NA NA | Y Y Y |
| (13) Did the review authors account for RoB in individual studies when interpreting discussing the results of the review? | N NN | N NN | Y Y Y | N NN | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | CA CA CA | CA CA CA | Y Y Y | N NN |
| (14) Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? | N N N | P P P | Y Y Y | Y N Y | Y Y Y | YNP | PYY | P P P | Y Y Y | P P P | Y Y Y | Y Y Y | P P P |
| (15) If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? | Y Y Y | NA NA NA | Y Y Y | NA NA NA | NA NA NA | NA NA NA | NA NA NA | NA NA NA | P P P | NA NA NA | NA NA NA | NA NA NA | N NN |
| (16) Did the review author’s report any potential sources of conflict of interest, including any funding they received for conducting the review? | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | Y Y Y | N N N | Y Y Y | Y Y Y | N NN | N NN | Y Y Y |
Y: Yes; P: partial yes; N: No; NA: not applicable; CA: cannot answer.
H = high confidence; M = moderate confidence; L = low confidence; CL = critically low.
Note: First Reviewer (NC), Second Reviewer, Consensus.
Analysis
Data extraction focused on key facilitators and barriers to training and education and outcomes. This is summarised in Table 4 (initial summary review) with information on the authors, topic summary, the number of papers reviewed by the systematic review and AMSTAR 2 confidence level (H = high; M = moderate; L = low; CL = critically low).
Analysis synthesises the results, ensuring new knowledge is grounded in the information gleaned from multiple research studies (Ryan, 2013; Smith et al., 2011). The fact that selected reviews have a broad focus makes the task of synthesis problematic in the traditional sense. Instead, a narrative synthesis was conducted using an adapted version of the procedures outlined by Popay et al. (2006) and reliant primarily on the use of words and text to summarise and explain the findings. This ensures the overarching themes are grounded in the studies identified, and a well-evidenced technique used in reviews focusing on a wide range of questions (Dixon-Woods et al., 2006; Popay et al., 2006). Stage 1 involved developing a theoretical model. As this is a systematic review of reviews, this theoretical work had been achieved in the preliminary exploration of how training and education in this field works, why and for whom. Theory-building and testing is often a neglected aspect of reviews. This work informs theory-building in relation to the identification of training and education facilitators and barriers. Stage 2 involved developing a preliminary synthesis whereby the results of the included studies are condensed so that patterns can be identified (Popay et al., 2006). Stage 3 developed this process, exploring relationships between and within studies. For this review, the relationships of interest (Popay et al., 2006) comprised the components and content of training and education reported and the facilitators and barriers affecting implementation, uptake, effectiveness and outcomes. Three main themes were identified and reported below. The final stage (Stage 4) provided an assessment of the strength of the evidence and synthesis for drawing conclusion and any generalisations that can be made (Popay et al., 2006). This forms the discussion and conclusion of this review.
Findings
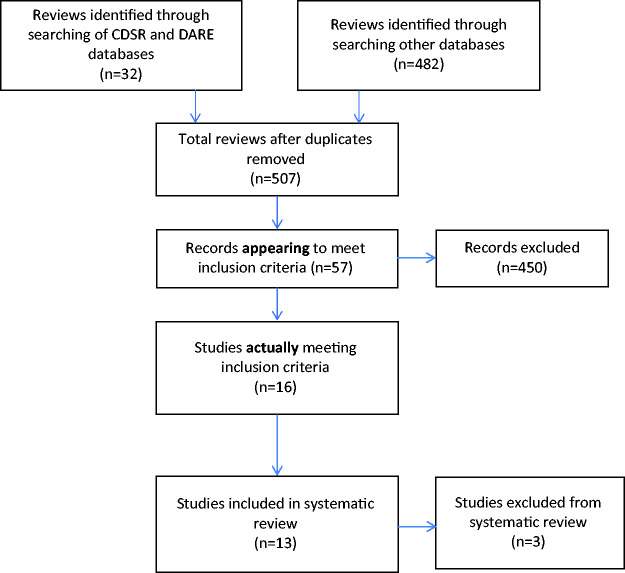
The initial search provided 507 review articles. The abstracts of these reviews were independently read and assessed by two project team members as to whether they met the inclusion criteria. A full PRISMA (Moher, Liberati, Tetzlaff, & Altman, 2009) statement outlining the stages of the search selection and rejection process is provided in Figure 1.
Figure 1.
PRISMA flow diagram.
This resulted in 450 reviews being excluded. The remaining 57 reviews were then independently read by two project team members resulting in 41 further reviews being excluded. During both these stages, the most common reasons for exclusion during were: (1) the review not being fully systematic in nature, most commonly scoping, literature or narrative reviews; (2) the review focused entirely on acute or long-term residential care as opposed to (or at least including) community at-home settings; and (3) the topic of workforce and professional education did not feature in a prominent way. Of the 16 remaining reviews, three (Kersten, Taminiau, Schuurman, Weggeman, & Embregts, 2018; Moyle, Hsu, Lieff, & Vernooij-Dassen, 2010; Spector, Revolta, & Orrel, 2016) were subsequently excluded because the primary focus was assisted-living or nursing care within assisted-living settings.
An initial summary of the 13 remaining reviews and their findings is provided in Table 5.
Table 5.
Initial summary review.
| Authors | Topic | No | AS | Facilitators | Barriers | Outcomes |
|---|---|---|---|---|---|---|
| (1) Clarkson et al. (2017) | Outcomes of home support interventions for older people with dementia and/or carers. | n = 70 | H | Emotional/social support skills. Behaviour management training. | Family carer-focused. Limited effective staff delivering training: nurses/nurse therapists overseeing. | Effective training and education delays care home admission. Interventions of variable quality: more research required. Paucity of research with social care/care-at-home focus. |
| (2) Cooper et al. (2017) | Effects of interventions to improve how homecare agencies deliver homecare. | n = 10 | M | Needs-based models of care. Group learning. Post-learning team meetings. Mentors, support. | Task-focused only. Lack of refresh. Lack of support. Poor teachers. Work-time-poor. Limited role flexibility. | Effective training reduces nursing/care home placement. Homecare workers experiences key challenges: solitary working, family contact, advice provision. The right training improves workforce wellbeing and retention. The right training may detect undiagnosed illnesses. Caution: evidence is not robust. |
| (3) Cummings et al. (2011) | Evaluating knowledge translation and cancer pain management interventions. | n = 26 | H | Multi-disciplinary team input. Multiple channels Learning over time. Group work and meetings. Feedback, refresh. Local follow-up. Local/community focus. Preconstructed materials/national guidelines. Minimum single learning session 2 hours; programme over 8 hours. | Lack of extensive learning follow-up and review. Lack of systematic approach to learning. Lack of monitoring and (ongoing) supervision. | Positive correlation between higher dose knowledge transfer comprehensive education programmes and change in outcomes: improved pain management knowledge, skills, attitudes for health professionals, patients and families. Cautious interpretation: risk of bias in trials evaluated. More research required. |
| (4) D’Astous et al. (2017) | Exploring experiences of homecare workers providing end-of-life care. | n = 12 | M | Multidisciplinary communication training. Group learning. Senior colleague liaison. Organisational learning ethos. | Task-focused only. Limited individual-client-needs focus. Limited emotional support training. Limited technical support. Limited access to other (healthcare professionals). | No effective components of training/support for homecare workers providing end of life care for people with dementia identified. Homecare Workers/non-professional staff have limited access to healthcare professional education and learning. Enhancing knowledge improves quality of care. Consideration should be given to ethnicity/migration status of care workers. |
| (5) Eggenberger et al. (2013) | Evaluating interventions to enhance communication in dementia care (focus residential and homecare; health care professionals and family caregivers). | n = 12 | H | Communication skills training. Didactic/teacher role. Supervision, support/feedback. Booster sessions: skill maintenance. Problem-based learning techniques. Motivational and/or reward systems. Training consultants to train family caregivers. | Open, experiential or student-led learning less effective. Single-dose interventions less effective. | Inconsistent results, mixed evidence. More evidence focusing on homecare required. Education effective with feedback/supportive culture. |
| (6) Elliot et al. (2012) | Whether training interventions build workers’ capacity and facilitate organisational change (primary, hospital, residential and community care, dementia units and hospital wards). | n = 6 | M | Group work. Supervisor support. Mentor/buddying. Instructional training modules. Communication skills. | Time-poor. Limited shift cover/workforce shortage. Learning not targeted to different skill/knowledge levels. No review or refresh. Lack of supervision. Job stress & burnout. Management support required. Limited training on relationship aspects of care role: privacy, dignity and boundaries ignored. Client attachment difficulties. | No studies found addressing worker/organisational outcomes in community setting. Barriers to care linked to lack of knowledge, workforce and organisational issues. Target training task-focused only. Negative workforce emotional wellbeing and burnout impacts on care and learning motivation. All studies: methodological concerns and mixed results. Instructional training common but no community-setting interventions. |
| (7) Goeman and Koch (2016) | Qualitative evaluation of components of dementia support worker type roles currently in operation to assist community dwelling. | n = 58 | M | Multidisciplinary learningPeople with dementia/family caregiver collaborationIndividualised, client-needs models. Supportive learning environment. Workplace learning network. | Limited learning evaluation/reflection. Task-based models. Lack of attention to workforce self-care and emotional de-briefing requirements. | Inconsistent results. Multi-interdisciplinary, individualised intervention over time with input from people with dementia, carers and family. Needs-based, not task-based education. Upskilling requires individualised needs-based education. |
| (8) Herber and Johnston (2013) | The role home and health support workers play in palliative and end of life care in the community and identifying challenges. | n = 9 | M | Theoretical and textbook training. Patient-centred care. Informal peer grief-support. Workforce group cohesiveness. Task-model dominant. Role-matching: trained with untrained. | Training too basic. Limited nationally recognised qualifications. Inadequate job preparation. Theoretical textbook training insufficient. On the job training from co-workers (with no formal training). Organisational challenges. Lack of supervision, mentors and support. | Theoretical/textbook training insufficient. Limited, on-the-job training common. No nationally recognised qualifications. Close support/supervision from district and community nurses required: role matching trained with untrained. Emotional and grief challenges. Community nurses to provide informal education. |
| (9) Kim and Park (2017) | Investigating the effectiveness of person-centred care (on people with dementia in long term care and homecare settings. | n = 19 | H | Learning over time. Patient-centred care. Needs-based care. Guidelines or manuals of care. Intensive, activity-based. | Lack of motivation and skills for (i) education and (ii) implementing PCC. Long-term staff education interventions lacked instruction detail. Focus on task-based | Insufficient data outside long term care settings: at-home outcomes could not be measured. Educational strategy required. Continuous education may be effective. Variable staff motivation for sustained education and training. Strong management and organisational structure required. More robust studies required. |
| (10) Morgan et al. (2011) | Evaluating dementia care and service provision in remote and rural settings (formal paid caregivers). | n = 46 | M | Adaptive technology effective; face to face preferred. Community sensitive trainers. Effective teachers. Local learning. Time for dissemination and implementation. Workforce views. Interdisciplinary. Partnership between educators and rural agencies. Review and refresh. | Cost. Lack of information. Travel distance. Workplace capacity. Technical abilities. Management. | Lack of dementia training and education reported for rural service providers, particularly independent sector. One-size education will not fit all. Specific rural needs in relation to technology (isolation), locale, access, staff shortage and capacity issues. Pain management training required. Dementia care training important for reducing job stress and improving job satisfaction. |
| (11) Raymond et al. (2014) | Synthesising information about management of end-of-life care in hospital, home and community settings. | n = 8 | M | Communication assessment tools to identify pain in people with dementia. | Lack of education = low professional and practice confidence in palliative dementia care. | Few reviews identify social care staff poorly paid; low status; limited access to training; non-professionally qualified; high turnover/staff shortages. Tension: calling for more training without recognising care for people with dementia falls on non-professional staff with generally less access to training than other care staff. Optimal management of pain in dementia is poorly understood. |
| (12) Surr et al. (2017) | Factors associated with effective dementia education and training for health and social care staff. | n= 152 | M | Group learning. Face-to-face. Didactic: classroom, lectures, discussion, video, activities. Effective combined multimedia online learning. Review, feedback, reflection. Activity-based: role-play/vignettes. Carer involvement. Learning materials: clear, concise and plain language. Structured tool/guidelines. Skilled trainers 8+ hours duration with individual sessions. | E-learning effective but technical and time intensive. Concurrent online. Not one size-fits-all. Role-play requires assessor relationship. In-service. Practice-based learning as sole approach not effective. Poor mentor engagement. Task-focused organisation. Hard copy or online written work. (Only) watching an individual or group. DVD/video. Reading/written resources. Lack of de-briefing in simulated training. | Combination learning has positive knowledge outcomes. Application of learning into practice requires staff champions. Requires method to guide practice change in a structured way. Positive staff outcomes via longer training/time for staff engagement in the overall training programme. Limited number of studies in community. More robust research required. Caution applying results out of care home and hospital context. |
| (13) Toot et al. (2017) | Factors associated with increased risk of nursing home placement for people with dementia. | n = 26 | M | Limited education focus. | Lack of physical and social needs learning models. Limited acute and chronic pain and conditions management. | Specialist multi-disciplinary teams should focus on cognitive enhancement strategies, assessment and management of behavioural and psychological symptoms of dementia, carer education. Effects of community support services unclear. |
AS: H = high confidence; M = moderate confidence; L = low confidence; CL = critically low.
Study characteristics
Two studies (Clarkson et al., 2017; Kim & Park, 2017) adopted Population, Intervention, Comparison, Outcome (PICO; Eden, Levit, Berg, & Morton, 2011) as an appraisal technique. Eleven reviews provided the characteristics of included studies, by means of a table of findings or narrative description. Elements highlighted included description of design, foci, method and sample size, illustrated objectives and research design or type of intervention.
All reviews performed a comprehensive literature search as expected of a systematic review. Ten reviews clearly affirmed study selection in duplicate. This was unclear in the remaining three studies (Herber & Johnston, 2013; Morgan, Innes, & Kosteniuk, 2011; Raymond et al., 2014). Similarly, only nine out of the 13 studies clearly stated data extraction was performed in duplicate. Only seven studies included a full and complete list of excluded studies, and justification for the exclusion. Morgan et al. (2011) provided no list at all while Goeman and Koch (2016), Kim and Park (2017) and Raymond et al. (2014) provided only partial lists.
Most studies described the included studies in adequate detail. For our purposes, this was an important element of quality appraisal. Likewise, provision of a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review is important and informs our training and education appraisal. A number of studies discussed methodological and statistical heterogeneity, for example: Cummings et al. (2011), Eggenberger, Heimer, and Bennett (2013) and Kim and Park (2017). Inconsistences were noted and include heterogeneity in inclusion criteria, study design and population, recruitment strategies and outcome measures. Mixed evidence regarding the effects of training and education may reflect methodological weaknesses and shortcomings in study design, diversity of method and foci of interest. Only five studies (Clarkson et al., 2017; Eggenberger et al., 2013; Goeman & Koch, 2016; Herber & Johnston, 2013; Kim & Park, 2017) included clear risk of bias assessment in the selected literature. Two studies (Elliot, Scott, Stirling, & Martin, 2012; Raymond et al., 2014) provided some risk assessment although not guided by clear protocol. The remaining studies (Cooper et al., 2017; Morgan et al., 2011; Surr, Gates, & Irving, 2017) provided no risk of bias assessment.
The AMSTAR 2 (Shea et al., 2017) appraisal process includes a method for interpreting weaknesses detected via critical and non-critical items. Two members of the project team conducted this process. Four reviews (Clarkson et al., 2017; Cummings et al., 2011; Eggenberger et al., 2013; Kim & Park, 2017) received high confidence appraisals, demonstrated via no, or only one, non-critical weakness. The remainder received moderate confidence appraisal, exhibiting more than one weakness but no critical flaws. Consideration was given as to whether, following these procedures and results, to exclude the findings of Toot, Swinson, Devine, Challis, and Orrell (2017). Toot et al. (2017) do not provide a specific focus on key components of training and education for the homecare workforce but do highlight that little is known about the effects of training and education and requirements for community support services and professionals. This review highlights that poor community support may have an association with increased risk of nursing home placement,particularly in relation to multimorbidity and was considered appropriate for inclusion.
Education and training: Delivery and method
While few reviews included a full evaluation of teaching approach and a degree of interpretive caution must be applied, some teaching methods can be identified as consistently successful learning facilitators across the reviews. This included a strong focus on face-to-face group work and shared-team or group learning (Cooper et al., 2017; D’Astous, Abrahams, Vandrevala, Samsi, & Manthorpe, 2017; Elliot et al., 2012; Herber & Johnston, 2013; Samsi et al., 2017; Surr et al., 2017). Good teaching delivery methods included the opportunity to share and exchange new learning and liaise with peers and senior colleagues for support, mentorship and knowledge-exchange. This method of learning and teaching delivery also enhanced group cohesiveness among the homecare workforce (D’Astous et al., 2017; Herber & Johnston, 2013; Samsi et al., 2017).
The effectiveness of tailored, role-focused teaching and learning methods was highlighted across 10 reviews. A one-size-fits-all teaching method appeared less successful and took very limited account of different skill levels and prior educational experience within this workforce (Clarkson et al., 2017; Cooper et al., 2017; D’Astous et al., 2017; Eggenberger et al., 2013; Elliot et al., 2012; Goeman & Koch, 2016; Herber & Johnston, 2013; Kim & Park, 2017; Morgan et al., 2011; Surr et al., 2017). This approach commonly comprised more didactic, standardised, work/manual/textbook, combination DVD learning, and often required reading and/or written responses. Online learning, when offered as student-led and with no, or very limited, offline-support, or combined with assisted group work, indicated high attrition and limited module completion rates (see Elliot et al., 2012; Surr et al., 2017).
Simulated, experiential and role play teaching produced weak or variable outcomes (Cummings et al., 2011; Eggenberger et al., 2013; Elliot et al., 2012; Goeman & Koch, 2016; Surr et al., 2017). One-off, single-delivery, traditional and more theory-led teaching methods were reported to be less effective, whether online or offline. Nine reviews also underlined the importance of reflection within teaching and learning, including timely learning refresh, audit, feedback or booster sessions. Cummings et al. (2011) identified learning over time, with feedback and audit, as cardinal elements of successful healthcare educational interventions for cancer pain management. This approach embedded knowledge delivered within professional practice, enhanced workforce skills and enabled the continuing implementation of learned knowledge. Ongoing motivational support and feedback incentivised learning and further enabled the maintenance of learning in practice (Cooper et al., 2017; Eggenberger et al., 2013; Elliot et al., 2012; Kim & Park, 2017; Surr et al., 2017).
Other key facilitators combined multi-disciplinary, integrated and collaborative teaching methods. This included contributions from known experts or specialists in the field, alongside input from, for example, people with dementia and their carers. Collaborative input from homecare professionals was also highlighted. This included the value of shared experiences and problem-based methods to resolve difficulties (D’Astous et al., 2017; Goeman & Koch, 2016; Morgan et al., 2011). Delivering teaching and education in a community setting also required the incorporation of local needs within training and education, as opposed to a more generic emphasis. This was particularly relevant within more rural, isolated locale (Cummings et al., 2011).
While effective teaching method facilitated learning, method alone was restrictive. Four reviews highlighted limited training and teaching delivery skills (Clarkson et al., 2017; Cooper et al., 2017; Herber & Johnston, 2013) often illustrated via the adoption of on-the-job training using co-workers with limited or no formal training and education delivery skills.
Workforce: Motivation and resilience
Cost, location, distance, travel and technical (computer) abilities were cited in seven reviews as learning motivation barriers and particularly relevant within a rural locale (Herber & Johnston, 2013). These issues are also known disinhibitors towards accessing education and learning for professional development more generally (Morgan et al., 2011). Poor quality of learning alongside limited nationally recognised accreditation were also identified as key workforce disincentives (Cooper et al., 2017; Cummings et al., 2011; D’Astous et al., 2017; Elliot et al., 2012; Goeman & Koch, 2016; Herber & Johnston, 2013; Surr et al., 2017). More specific learning motivation difficulties for the homecare workforce were further highlighted in four reviews (D’Astous et al., 2017; Elliot et al., 2012; Kim & Park, 2017; Raymond et al., 2014) and included limited educational experience, lower qualification levels and different skills that impacted on staff attitude, confidence and motivation towards training and education. Little evidence across the reviews provided any more detailed information about the particular skill and qualification levels of the homecare workforce.
There are further barriers for the homecare workforce that impact on learning motivation and the professional development. Eight reviews identified specific homecare workforce issues, including: low job satisfaction, burnout, emotional strain combined with limited emotional support and lack of preparation for death and end-of-life clients (see Elliot et al., 2012). This reaffirmed established links between stress, burnout and workforce retention. It is already known that homecare workers caring for individuals with memory impairment experienced higher levels of work-related stress compared to those caring for more functionally able clients (I-Ling, Kritika, Vandrevala, & Manthorpe, 2018). These issues have been raised earlier (see Elliot et al., 2012) and continue to be raised (see D’Astous et al., 2017; Goeman & Koch, 2016). The nature of homecare work may mean that strong, often meaningful relationships are formed, demanding time and effort (Herber & Johnston, 2013). If unprepared, the homecare worker may be more at risk of heightened grief and the associated effects (Boerner, Burack, Jopp, & Mock, 2015). For homecare workers, emotional support is key to the maintenance of workplace wellbeing and was highlighted in four reviews (D’Astous et al., 2017; Herber & Johnston, 2013; Kim & Park, 2017; Morgan et al., 2011). Lack of emotional training and preparation to manage the intimacies of close-caring, personal boundary issues alongside self-care was highlighted (D’Astous et al., 2017; Elliot et al., 2012). Workforce stress, low satisfaction and burnout enhanced negative learning motivation and individual capacity for extended learning. Five reviews (Cooper et al., 2017; D’Astous et al., 2017; Goeman & Koch, 2016; Herber & Johnston, 2013; Kim & Park, 2017) also highlighted workforce demand for person-centred, individual and/or needs-based care as opposed to task and time focused training provided.
Organisations: Supporting learning
Organisational attitudes are known predictors of educational success. Seven reviews identified the need to understand different organisational variables amid concerns over sector difficulties that restricted the implementation of more widespread learning programmes or inhibited staff from applying learned knowledge consistently in practice (Cooper et al., 2017; Cummings et al., 2011; Elliot et al., 2012; Herber & Johnston, 2013; Kim & Park, 2017; Morgan et al., 2011; Surr et al., 2017). Positive organisational learning ethos and management support that comprised continued mentoring and supervision was considered a strong facilitator for successful workforce training, education and learning. Discontinuity of management input alongside inappropriate management behaviour are reported as barriers to learning (Cooper et al., 2017; Elliot et al., 2012; Herber & Johnston, 2013; Morgan et al., 2011; Surr et al., 2017).
Task-focused organisations providing solely practical skills-based in-service learning posed the biggest barrier to staff development (Surr et al., 2017). Workforce shortage in general and staff shortages in-house (that prevented cover for those accessing training and education) reflect key organisational challenges highlighted consistently across reviews. Limited workforce role flexibility contributed to both stress and burnout but also, conversely, impacted on participation in the training and education that may help reduce stress and burnout (Cooper et al., 2017; Elliot et al., 2012; Surr et al., 2017).
Discussion
The aim of this review of reviews was to synthesise the findings of systematic reviews on dementia and cancer training and education accessible to the homecare workforce; identify key themes, facilitators and barriers in training and education for homecare workers; gaps in provision and areas for further development and research. Barriers and facilitators to effective training and education for the homecare workforce are illustrated within three key common themes identified. These themes are focused on (i) education and training: delivery and method; (ii) workforce: motivation and resilience and (iii) organisations: supporting learning.
One of the principal barriers highlighted was the identification of mixed, diverse, and variable outcome training and education accessible to the homecare workforce. With increases in the numbers of people choosing to receive care at home, alongside policy drivers aimed at enabling people to have the right to choose to remain – and die – at home, the role of the homecare worker is critical (D’Astous et al., 2017). Despite this, only five reviews (Clarkson et al., 2017; Cooper et al., 2017; D’Astous et al., 2017; Goeman & Koch, 2016; Herber & Johnston, 2013) focused solely on the community at-home setting. Only one review (Cummings et al., 2011) focused on cancer (pain management) interventions, and these were focused on healthcare providers, patients and family caregivers. While some reviews addressed some elements of homecare worker skills-training or education for dementia care, none addressed the overlap and complex care requirements when dementia and cancer, or other multimorbidities, co-exist. Surr et al. (2017) provide a strong review of effective dementia and education training, albeit this is considered across the health and social care workforce, does not focus on the specific needs of the homecare workforce and is limited to dementia-specific education and training for the management of challenging behaviour.
All reviews identify some key educational approaches that facilitate training and education and some of the key barriers negatively affecting training and education. Few reviews highlight or acknowledge that social care staff – and particularly the homecare workforce – have more limited access to this training than other care staff, are also poorly paid, insecure in employment and often considered lower status (Hussain & Manthorpe, 2012). It is important here to again emphasise that the majority of homecare workers are predominately female, with a broad age range between 45 and 54 and with often limited education, low learner-confidence and few qualifications (Cooper et al., 2017). Negative workforce emotional wellbeing, stress and burnout present barriers to care, workforce retention and also training, education and learning motivation. Training that does not respond to workforce self-care and emotional resilience requirements may further compound these difficulties. Significantly, no reviews explore the interrelationship between these factors.
As advances are made in disease recognition, technology and medical care, care support and provision at-home is becoming much more complex. People living with dementia who are over 65 have on average four multimorbidities, including cancer, while people without dementia have two on average (Poblador-Plou et al., 2014). This review highlights that training and education available and accessible to the homecare workforce may not fill the knowledge gaps required to be filled to avoid detriment. Further, some training and education provisions reviewed represent a passive learning style and this does not reflect best practice and more active learning approaches advocated across the spectrum of education research (Surr et al., 2017). Some reviews demonstrated a positive correlation between training and education in terms of effective method of delivery responsive to workforce needs and the continued implementation of new knowledge in practice. Strong organisational ethos supporting continued workforce training and education is a positive facilitator in the workplace. Currently, this ethos is compromised by key sector difficulties affecting the implementation of enhanced education beyond task-and-time focused skills training.
Conclusion
This review identifies some key training and education strategies and the components required to facilitate learning in the community homecare setting. A critical omission is lack of focus on providing the necessary training and education to support people living with dementia and cancer and wider multimorbidities. As yet, no study has explored the interrelationship between the training, education and learning needs of the homecare workforce, learning curricula and organisational and management ethos. A further weakness identified in the evidence-base is the lack of research exploring the motivations of the homecare workforce towards continued training and education development and the learning supports that may be required to encourage learning, workforce resilience and wellbeing.
In light of these findings, and while there may be no one-size-fits-all model of training and education, this review suggests that approaches to training and education that are responsive to these elements – and the connections between them – have the greatest potential. Training and education are mechanisms for change and it is important to also establish causal confidence that particular training and education has delivered the expected outcomes in a particular setting. Our conclusions remain tentative at this stage and underline the need to undertake further robust research examining these elements in more depth.
Limitations
The search process raised some questions concerning the search strategy. We implemented a search strategy using search terms around dementia AND cancer and dementia OR cancer. Most reviews focused on dementia alone. One review (Cummings et al., 2011) focused exclusively on cancer. 89 reviews that did focus on dementia and cancer were excluded because they did not meet the full inclusion criteria, for example, a review focused entirely on acute or residential care (for example, dementia with subsequent cancer as a cause of nursing home placement). No reviews met the full inclusion criteria and focused on coexisting dementia and cancer. While a limitation, this demonstrated a known scarcity of evidence recently documented (McWilliams et al., 2018).
Caution needs to be employed in interpreting the results because of the paucity of research conducted primarily in at-home community settings. Several reviews refer generically to ‘staff’, without delineating between qualified nursing, social care and homecare staff. This may hide or at best merge the specific education and training accessible to the homecare workforce. Despite this, the lack of information and evidence around homecare workforce training and education relating to dementia and cancer, or other multimorbidities, is evident.
There are generic limitations within a systematic review of reviews (Thomson et al., 2010). A systematic review of reviews is only as good as the systematic reviews within. Care was taken through robust research design and conduct to ensure parity across reviews and that particular individual studies were not over-used or over-represented, thereby distorting findings (Smith et al., 2011). Analysis and appraisal was performed by at least two researchers from the project team, so the chance of misinterpretation has been minimalised. However, questions concerning method, robustness and bias (for example see Cooper et al., 2017; Eggenberger et al., 2013; Elliot et al., 2012; Goeman & Koch, 2016) are also raised across the studies and cautious interpretation is underlined here.
Biography
Nicola Cunningham has a professional background in welfare, and a strong interest in developing teaching and learning opportunities for the welfare and social care sector. Supporting academic transition and widening access to university level education, learning and accreditation is a strong driver. Recent teaching has focused on the development and management of an innovative UK-wide online programme of learning for welfare and social care professionals. Current research progresses a rights-based approach to wellbeing and care at home, exploring the supportive needs of people affected by dementia, cancer and related co-morbidities and the training and education requirements of the homecare workforce.
Julie Cowie is a health services researcher with an interest in implementation science, exploring ways in which theoretically developed interventions are integrated into practice to maximise long-term continued use and effectiveness. Current research interests include: e-Interventions in healthcare settings. Her current focus is aiming to understand the contextual factors around the integration of interventions, and barriers and facilitators that impact on successful sustained implementation.
Karen Watchman Karen has an academic background is in social science, and a practice background in social care where she spent many years as Chief Executive of Down’s Syndrome Scotland. Current research in progress develops and delivers practice development courses focusing on post-diagnostic support for people with intellectual disability and dementia. Karen provides consultancy within the UK and Ireland to support an ageing population of people with an intellectual disability within social care settings.
Karen Methven currently combines teaching and research during her doctoral studies, teaching on the UG nursing programme for adult and mental health. Her doctoral studies explore the reasons for non-delivery of homecare from a service user’s perspective.
Footnotes
Contributors: Author 1 (corresponding author) reviewed abstracts, developed conceptualisation of study, contributed to synthesis, analysis and lead writer. Author 2 reviewed abstracts, contributed to synthesis, analysis, conceptualisation of study, contributed to writing. Author 3 conducted database search, reviewed abstracts, extracted data for table and contributed to writing. Author 4 contributed to conceptualisation of study, and contributed to writing.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics: This project received ethical approval from University of Stirling NICR Ethics committee on 24 April 2018 (NICR17/18: 36).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This independent research is supported by Chief Scientist Office, Grant number (CCA/18/09).
Contributor Information
Nicola Cunningham, Faculty of Health Sciences and Sport, University of Stirling, UK.
Julie Cowie, Glasgow Caledonian University, UK.
Karen Methven, University of Stirling, UK.
References
- Alzheimer’s Society. (2016). Fix dementia care homecare. London, UK: Alzheimer’s Society. [Google Scholar]
- Bennett L., Honeyman M., Bottery S. (2018). New models of home care. London, UK: The King's Fund. [Google Scholar]
- Boerner K., Burack O. R., Jopp D. S., Mock S. E. (2015). Grief after patient death: Direct care staff in nursing homes and homecare. Journal of Pain and Symptom Management, 49(2), 214–222. DOI: 10.1016/j.jpainsymman.2014.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunn F., Bun A.-M., Goodman C., Robinson L., Rait G., Norton S., … Brayne C. (2016). Comorbidity and dementia: A mixed-method study on improving healthcare for people with dementia (CoDem). University of Hertfordshire, UK. DOI: 10.3310/hsdr04080. [PubMed]
- Cancer Research UK. (2015). Cancer incidence by age. Secondary cancer incidence by age. Retrieved April 1, 2018 from http://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence/age#heading-Zero#VUVKIf7RwvZVzEZR.97
- Car L. T., El-Khatib M., Perneczky R., Papachristou N., Atun R., Rudan I., … Majeed A. (2017). Prioritizing problems in and solutions to homecare safety of people with dementia: Supporting carers, streamlining care. BMC Geriatrics, 17, 26. DOI: 10.1186/s12877-017-0415-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkson P., Hughes J., Roe B., Giebel C., Jolley D., Poland F., … Challis D. (2017). Systematic review: Effective home support in dementia care, components and impacts – Stage 2, effectiveness of home support interventions. Journal of Advanced Nursing, 74(3), 504–527. DOI: 10.1111/jan.13460. [DOI] [PubMed] [Google Scholar]
- Collerton J., Davies K., Jagger C. (2009). Health and disease in 85 year olds: Baseline findings from the Newcastle 85. + cohort study. The BMJ, 339. DOI:10.1136/bmj.b4904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C., Cenko B., Dow B., & Rapaport. (2017). A systematic review evaluating the impact of paid home carer training supervision and other interventions on the health and well-being of older home care clients. International Psychogeriatrics, 29(4), 595–604. DOI: 1017/s1041610216002386. [DOI] [PubMed] [Google Scholar]
- Courtier N., Milton R., King A., Tope R., Morgan S. (2016). Cancer & dementia: An exploratory study of the experience of cancer treatment in people with dementia. Psycho-Oncology, 25, 1079–1084. DOI: 10.1002/pon.4212. [DOI] [PubMed] [Google Scholar]
- Cummings G., Olivo S., Biondo P. D., Stiles C. R., Yurtseven O., Fainsinger R. L., Hagen N. (2011). Effectiveness of knowledge translation interventions to improve cancer pain management. Journal of Pain and Symptom Management, 41(5), 915–939. DOI: 10.1016/j.painsymman.2010.07.017. [DOI] [PubMed] [Google Scholar]
- D’Astous V., Abrahams R., Vandrevala T., Samsi K., Manthorpe J. (2017). Gaps in understanding the experiences of homecare workers providing care for people with dementia up to the end of life: A systematic review. Dementia, 1. DOI: 10.1177/1471301217699354. [DOI] [PubMed] [Google Scholar]
- Department of Health. (2009). Living well with dementia: A national dementia strategy. Strategic framework within for making quality improvements to dementia services and addressing health inequalities. Retrieved February 1, 2018 from https://www.gov.uk/government/publications/living-well-with-dementia-a-national-dementia-strategy
- Department of Health. (2012). Living well with dementia: A National Dementia Strategy. Good practice compendium – An assets approach. London, UK: Department of Health. Retrieved February 1, 2018 from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215822/dh_123475.pdf
- Dixon-Woods M., Cavers D., Agearwal S., Annandale E., Arthur A., Harvey J., … Sutton A. J. (2006). Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Medical Research Methodology, 6, 35. DOI: 10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eden J., Levit L., Berg A., Morton S. (2011). Finding what works in health care: standards for systematic reviews. Washington, DC: The National Academies Press. ISBN 978-0-309-16425-2 [PubMed] [Google Scholar]
- Eggenberger E., Heimer K., Bennett M. (2013). Communications skills training in dementia care: A systematic review of effectiveness, training content, and didactic methods in different care settings. International Psychogeriatrics, 25(3), 345–358. DOI: 10.1017/S1041610212001664. [DOI] [PubMed] [Google Scholar]
- Elliot K., Scott J., Stirling C., Martin A. (2012). Building capacity and resilience in the dementia care workforce: A systematic review of interventions targeting worker and organizational outcomes. International Psychogeriatrics, 24(6), 882–894. DOI: 10.1017/S1041610211002651. [DOI] [PubMed] [Google Scholar]
- Elliot K. J., Stirling C. M., Martin A. J., Robinson A. L., Scott J. L. (2016). We are not all coping: A cross-sectional investigation of resilience in the dementia care workforce. Health Expectations, 19(6), 1251–1264. DOI: 10.1111/hex.12419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finucane A. M., Carduff E., Lugton J., Fenning S., Johnston B., Fallon M., … Murray S. A. (2018). Palliative and end-of-life care research in Scotland. BMC Palliative Care, 17, 19. DOI: 10.1186/s12904-017-0266-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goeman E., Koch S. (2016). What is the effectiveness if the support worker role for people with dementia and their carers? A systematic review. BMC Health Services Research BMC Series, 16, 285. DOI: 10.1186/s129813-016-15312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall P., Jefferson I., Dale V., Bennett L., Birks Y., Bloor K., Murray R. (2017). Understanding domiciliary care in England. London, UK / York, UK, Partnership for responsive policy analysis and research. Retrieved December 12, 2018 from http://www.kingsfund.org.uk/publications/home-care-in-england [Google Scholar]
- Herber O., Johnston B. (2013). The role of healthcare support workers in providing palliative and end of life care in the community: A systematic literature review. Health and Social Care in the Community, 21(3), 225–235. DOI: 10.1111/j.1365-2524.2012.01092.x. [DOI] [PubMed] [Google Scholar]
- Hopkinson J. B., Milton R., King A. (2016). People with dementia: What is known about their experience of cancer treatment and cancer treatment outcomes? A systematic review. Psycho-oncology, 25, 1137–1146. DOI: 10.1002/pon.4185. [DOI] [PubMed] [Google Scholar]
- House of Commons. (2018, May). Committee of Public Accounts. The adult social care workforce in England. Thirty-eighth report of session 2017–2019 HC690. Retrieved October 22, 2018 from https://publications.parliament.uk/pa/cm201719/cmselect/cmpubacc/690/690.pdf
- Hughes S., Preston N., Payne S. (2016). Online learning in palliative care: Where are we now? European Journal of Palliative Care, 23(5), 1352–2779. [Google Scholar]
- Hussain S., Manthorpe J. (2012). The dementia social care workforce in England: Secondary analysis of a national workforce data set. Aging and Mental Health, 16(1), 110–118. DOI: 10.1080/13607863.2011.596808. [DOI] [PubMed] [Google Scholar]
- I-Ling Y., Kritika S., Vandrevala T., Manthorpe J. (2018). Constituents of effective support for homecare workers providing care to people with dementia at end of life. International Journal of Geriatric Psychiatry, 34(2), 352–359. [DOI] [PubMed]
- Jefferson L., Bennett L., Hall P., Cream J., Dale V., Honeyman M., … Murray R. (2018). Home care in England. Views from commissioners and providers. London, UK: The Kings Fund. [Google Scholar]
- Kersten M. C. O., Taminiau E. F., Schuurman M. I. M., Weggeman M. C. D. P., Embregts P. J. C. M. (2018). How to improve sharing and application of knowledge in care and support for people with intellectual disabilities? A systematic review. Journal of Intellectual Disability Research, 62(6), 496–520. DOI: 10.1111/jir.12491. [DOI] [PubMed] [Google Scholar]
- Kim S. K., Park M. (2017). Effectiveness of person-centred care on people with dementia: A systematic review and meta-analysis. Clinical Interventions in Aging, 12, 381–397. DOI: 10.2147/CIA.S117637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loannidis J. (2009). Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Canadian Medical Association Journal, 181(8), 487–493. DOI: 10.1503/cmaj.081086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams L., Farrell C., Grande G., Keady J., Swarbrick C., Yorke J. (2017). A systematic review of the prevalence of comorbid cancer and dementia and its implications for cancer-related care. Aging and Mental Health, 1–55. DOI: 10.1080/13607863.2017.1348476. [DOI] [PubMed] [Google Scholar]
- McWilliams L., Farrell C., Keady J., Swarbrick C., Burgess L., Grande G., … Yorke J. (2018). Cancer-related information needs and treatment decision-making experiences of people with dementia in England: A multiple perspective qualitative study. BMJ Open, 8, 4. DOI: 10.1136/bmjopen-2017-020250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddams J., Utley M., Moller H. (2012). Projections of cancer prevalence in the United Kingdom, 2010–2040. British Journal of Cancer, 107, 1195–1202. DOI: 10.1038/bjc.2012.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Medicine, 6. DOI: 10.1371/journal.pmed.1000097. [PMC free article] [PubMed] [Google Scholar]
- Montori V., Wilczynski N., Morgan D., Haynes B. (2005). Optimal search strategies for retrieving systematic reviews from Medline: Analytical survey. British Medical Journal, 330(68), DOI: 10.1136/bmj.38336.804167.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D., Innes A., Kosteniuk J. (2011). Dementia care in rural and remote settings: A systematic review of formal or paid care. Maturitas, 68, 34–46. DOI: 10.1016/j.maturitas.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Moyle W., Hsu M. C., Lieff S., Vernooij-Dassen M. (2010). Recommendations for staff education and training for older people with mental illness in long-term aged care. International Psychogeriatrics, 22(7), 1097–1106. DOI: 10.1017/S1041610210001754. [DOI] [PubMed] [Google Scholar]
- National Audit Office. (2018). The adult social care workforce in England. London, UK: National Audit Office. Retrieved February 8, 2018 from https://www.nao.org.uk/wp-content/uploads/2018/02/The-adult-social-care-workforce-in-England.pdf [Google Scholar]
- Pieper D., Puljak L., Lorenzo G., Minozzi S. (2018). Comparison of AMSTAR 2 with ROBIS in systematic reviews including randomized and non-randomized studies. Cochrane Colloqium Abstracts. Retrieved July 1, 2018 from https://abstracts.cochrane.org/2018-edinburgh/comparison-amstar-2-robis-systematic-reviews-including-randomized-and-non-randomized
- Poblador-Plou B., Calderon-Larranaga A., Marta-Moreno J., Hancco-Saavedra J., Sicras-Mainar A., Soljak M., Prados-Torres A. (2014). Comorbidity of dementia: A cross-sectional study of primary care older patients. BMC Psychiatry, 14(84). DOI: 10.1186/1471-244X-14-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock M., Fernandes R., Hartling L. (2017). Evaluation of AMSTAR to assess the methodological quality of systematic reviews in overviews of reviews of healthcare interventions. BMC Medical Research Methodology, 17(48). DOI: 10.1186/s12874-017-0325-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., … Duffy S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews: A product from the ESRC Methods Programme. Retrieved August 3, 2018 from https://www.researchgate.net/publication/2338666356_Guidance_on_the_conduct_of_narrative_synthesis_in_systematic_reviews_A_proddict_from_the_ESRC_Methods_Programme
- Raymond M., Warner A., Davies N., Nicholas N., Manthorpe J., Iliffe S. (2014). Palliative and end of life care for people with dementia: Lessons for clinical commissioners. Primary Health Care Research & Development, 15(4), 406–417. DOI: 10.1017/S146342361300039X. [DOI] [PubMed] [Google Scholar]
- Ryan R. (2013). Cochrane consumers and communication review group: Data synthesis and analysis. Retrieved January 3, 2018 from http://ccrg.cochrane.org
- Samsi K., Manthorpe J., Vandrevala R. T., Abrams R., L-Ling Y., D’Astous V. (2017). Working to the end: Experiences of the homecare workforce providing end-of-life care. In Alzheimer’s association international conference held in London, England 2017, 16–20 July.
- Scottish Government. (2010). Scotland’s National Dementia Strategy. Edinburgh, St. Andrews House, The Scottish Government. ISBN 978 0 7559 9534 9. Retrieved February 1, 2018 from https://www2.gov.scot/Resource/Doc/324377/0104420.pdf [Google Scholar]
- Scottish Government. (2017). National health and Social Care Workforce Plan. Phase 2 – A framework for improving workforce planning for social care in Scotland. Retrieved April 1, 2018 from https://www.gov.scot/binaries/content/documents/govscot/publications/publication/2017/12/national-health-social-care-workforce-plan-part-2-framework-improving/documents/00529319-pdf/00529319-pdf/govscot:document/ [Google Scholar]
- Scrutton J., Brancati C. U. (2016). Dementia and comorbidities: Ensuring parity of care from The International Longevity Centre supported by Pfizer. Retrieved February 1, 2018 from https://www.dementiastatistics.org/statistics/comorbidities/
- Shea B. J., Grimshaw J. M., Wells G. A. (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or nonrandomised studies of healthcare interventions, or both. The BMJ, 358. DOI: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed]
- Smith V., Devane D., Begley C., Clarke M. (2011). Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology, 11, 1–6. DOI: 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector A., Revolta C., Orrel M. (2016). The impact of staff training on staff outcomes in dementia care: A systematic review. International Journal of Geriatric Psychiatry, 31(11), 1172–1187. DOI: 10.1002/gps.4488. [DOI] [PubMed] [Google Scholar]
- Surr C., Gates C., Irving D. (2017). Effective dementia education and training for the health and social care workforce: A systematic review of the literature. Review of Educational Research, 87(5), 966–1002. DOI: 10:3102/0034654317723305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson D., Russell K., Becker L., Klassen T., Hartling L. (2010). The evolution of a new publication type: Steps and challenges of producing overviews of reviews. Research Synthesis Methods, 1, 198–211. DOI: 10.1002/jrsm.30/abstract. [DOI] [PubMed] [Google Scholar]
- Toot S., Swinson T., Devine M., Challis D., Orrell M. (2017). Causes of nursing home placement for older people with dementia: A systematic review and meta-analysis. International Psychogeriatrics, 29(2), 195–208. DOI: 10.1017/S1041610216001654. [DOI] [PubMed] [Google Scholar]
- Wilczynski N., Haynes B., & The Hedges Team. (2007). EMBASE search strategies achieved high sensitivity and specificity for retrieving methodologically sound systematic reviews. Journal of Clinical Epidemiology, 60, 29–33. DOI: 10.1016/j.jclinepi.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Witham G., Haigh C., Mitchell D., Beddow A. (2017). Carer experience supporting someone with dementia and cancer: A narrative approach. Qualitative Health Research, 1–11. DOI: 10.1177/1049732317736285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongrakpanich S., Hurst A., Bustamante J. (2017). Prognostic significance of dementia in older adults with solid tumours. Dementia and Geriatric Cognitive Disorders, 43(1–2), 38–44. DOI: 10.1159/000453449. [DOI] [PubMed] [Google Scholar]