Abstract
Introduction
Physical elder abuse is common and has serious health consequences but is under-recognised and under-reported. As assessment by healthcare providers may represent the only contact outside family for many older adults, clinicians have a unique opportunity to identify suspected abuse and initiate intervention. Preliminary research suggests elder abuse victims may have different patterns of healthcare utilisation than other older adults, with increased rates of emergency department use, hospitalisation and nursing home placement. Little is known, however, about the patterns of this increased utilisation and associated costs. To help fill this gap, we describe here the protocol for a study exploring patterns of healthcare utilisation and associated costs for known physical elder abuse victims compared with non-victims.
Methods and analysis
We hypothesise that various aspects of healthcare utilisation are differentially affected by physical elder abuse victimisation, increasing ED/hospital utilisation and reducing outpatient/primary care utilisation. We will obtain Medicare claims data for a series of well-characterised, legally adjudicated cases of physical elder abuse to examine victims’ healthcare utilisation before and after the date of abuse detection. We will also compare these physical elder abuse victims to a matched comparison group of non-victimised older adults using Medicare claims. We will use machine learning approaches to extend our ability to identify patterns suggestive of potential physical elder abuse exposure. Describing unique patterns and associated costs of healthcare utilisation among elder abuse victims may improve the ability of healthcare providers to identify and, ultimately, intervene and prevent victimisation.
Ethics and dissemination
This project has been reviewed and approved by the Weill Cornell Medicine Institutional Review Board, protocol #1807019417, with initial approval on 1 August 2018. We aim to disseminate our results in peer-reviewed journals at national and international conferences and among interested patient groups and the public.
Keywords: geriatric medicine, health economics, protocols & guidelines
Strengths and limitations of this study.
We explore patterns of healthcare utilisation and associated costs for known physical elder abuse victims, about common and serious phenomenon about which little is known.
We use Medicare claims data for a series of well-characterised, legally adjudicated cases of physical elder abuse to comprehensively examine victims’ healthcare utilisation before and after the date of abuse detection in comparison with non-victimised older adults algorithmically selected from Medicare claims.
We use machine learning approaches to better identify patterns suggestive of potential physical elder abuse exposure.
Though using legally adjudicated cases solves the important methodological challenge of ensuring that case subjects are actually victims of abuse, these cases represent a small percentage of all elder abuse cases, and their experience of abuse may differ in important ways from other victims.
Subjects must have been enrolled in Medicare Fee-for-Service rather than Medicare Advantage or another insurance for us to be able to examine their healthcare utilisation.
Introduction
Elder abuse is common and has serious health consequences but is under-recognised and under-reported. As many as 10% of US older adults experience elder abuse each year.1–6 This maltreatment may include physical abuse, sexual abuse, neglect, psychological abuse or financial exploitation, and many victims suffer from multiple types of abuse concurrently.1–5 Evidence suggests that elder abuse is associated with adverse health outcomes, including disability,7 dementia,8 depression8 and mortality.9–11 Despite its frequency, many elder abuse victims endure it for years before having it discovered or dying. Studies suggest that as few as 1 in 24 cases of elder abuse is reported to the authorities,1 3 12 and some of the associated morbidity and mortality is likely due to this delay in identification and intervention.13
As assessment by healthcare providers may represent the only outside contact for many older adults, so clinicians have a unique opportunity to identify suspected elder abuse and initiate intervention.14–20 Elder abuse victims have increased rates of emergency department (ED) use,14 17 hospitalisation21 and nursing home placement.22 23 Little is known, however, about the patterns of this increased utilisation and associated costs.5 24 Influential research in child abuse25–30 and intimate partner violence31 32 has focused on healthcare utilisation before identification, highlighting that many victims had multiple previous visits for likely abuse-related issues, suggesting ‘missed opportunities’ for identification and early intervention. Child abuse researchers have found that minor abusive injuries, ‘sentinel injuries’, are commonly found in children who are subsequently victims of severe child abuse but rare in those who are not.33 34 Strategies are being developed to capitalise on these findings to prevent morbidity and mortality for victims. Additionally, research has found that healthcare costs were significantly higher for victims of child abuse and intimate partner violence both in the short term35 36 and long term,35 37–40 compared with costs incurred by non-victims. These increased costs represent a key component of the overall economic burden of these phenomena,41–44 and related research findings have been critical in revealing the scope and impact of child abuse and intimate partner violence and in driving policymaking decisions. We know of no analogous research in elder abuse.
To help fill this gap in the literature, we describe here the protocol for a study designed to explore in detail patterns of healthcare utilisation and associated costs for known physical elder abuse victims compared with non-victims using analytic techniques including machine learning.
Methods and analysis
Conceptual framework and hypotheses
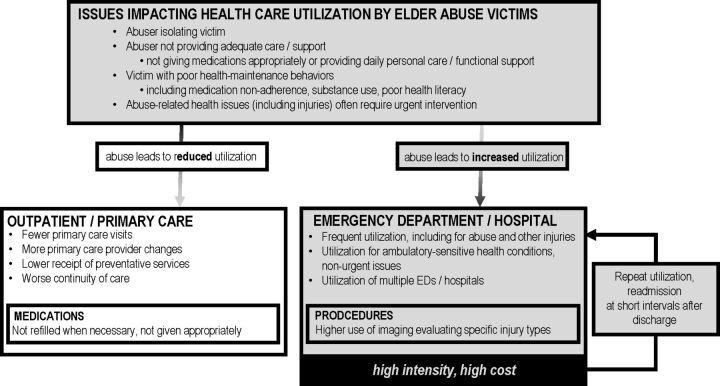
We hypothesise that various aspects of healthcare utilisation are differentially affected by physical elder abuse victimisation. Many issues related to physical elder abuse potentially increase ED/hospital utilisation and reduce outpatient/primary care utilisation. We have developed a conceptual framework (figure 1) to explain this pattern. This framework is informed by a model for elder abuse research that members of our team developed as part of the National Institutes of Health Workshop ‘Multiple Approaches to Understanding and Preventing Elder Abuse and Mistreatment: Prevention and Intervention’.45
Figure 1.
Conceptual framework for healthcare utilisation by elder abuse victims. EDs, emergency departments.
As shown in figure 1, we further hypothesise that physical elder abuse victims, due to their poor connection to primary care, will have increased utilisation of EDs/hospitals for ambulatory care-sensitive conditions (ACSCs) and for non-urgent issues. ACSCs are conditions that, if treated in a timely fashion with adequate primary care and managed properly on an outpatient basis, should not advance to the point where an ED visit or hospitalisation is required.46 Measuring the rate of use of high-intensity, high-cost services to treat these conditions is common in health services research to assess access to and quality of primary care.46–49 Similarly, use of the ED for non-urgent issues suggests inappropriate use in the absence of primary care.
We also hypothesise that physical elder abuse victims will have high rates of repeat ED visits and rehospitalisations within short intervals. This results from poor connections to primary care and poor adherence to outpatient follow-up care recommendations.50–53 We anticipate that physical elder abuse victims will also have higher use of the ED/hospital for issues directly related to abuse, including presentation for injuries and use of imaging to evaluate specific injury types. Based on anecdotal experiences by elder abuse experts,54 we also hypothesise that, compared with other older adults, physical elder abuse victims will more likely be seen at multiple EDs and hospitals. This ‘hospital hopping’ often occurs to avoid abuse detection.55
Conversely, we hypothesise that poor access to and less frequent use of primary care will be associated with more primary care provider changes, lower receipt of preventative services and worse continuity of care. More frequent changes in primary care providers result in fractured care and have been shown in previous claims-based research to be associated with child abuse.56 Receipt of preventative services has been used in previous studies to assess level of primary care utilisation among Medicare beneficiaries and has been shown to be lower in older adults with low primary care access including excess alcohol use and poor health literacy.57–61 We anticipate that physical elder abuse victims will have lower continuity of care, which has been shown in Medicare beneficiaries to be associated with increased rates of frequent ED use.62 Continuity of care assesses the dispersion of outpatient evaluation and management visits, examining how many unique doctors a patient visits within a specific timeframe.63
Fjnally, we also hypothesise that victims of physical elder abuse, partially due to poor connection to primary care, will have poorer adherence to medications for chronic conditions, such as diabetes medications and antihypertensives, which has been shown to impact high-intensity healthcare utilisation and cost.64 65
Study design
In this retrospective study, we will obtain Medicare claims data for a series of legally adjudicated cases of physical elder abuse to comprehensively examine victims’ healthcare utilisation before and after the date of abuse detection. We will also compare physical elder abuse victims to other non-victimised older adults. We will algorithmically select this comparison group from Medicare claims data to be matched to the physical elder abuse victims.
We will compare victims’ ED/hospital and outpatient primary care utilisation to that of the control groups. We will use machine learning approaches to extend our ability to identify patterns suggestive of potential physical elder abuse exposure.
This project has been reviewed and approved by the Weill Cornell Medicine Institutional Review Board, protocol #1807019417 (initially approved on 1 August 2018). The Institutional Review Board approved waiving the requirement to obtain informed consent from subjects in this retrospective study.
Study subjects
For this research, we plan to use a well-characterised series of 204 legally adjudicated cases of physical elder abuse from Brooklyn, New York, and Seattle, Washington. The methodological advantage of this series of cases is unique: because the perpetrators have pled guilty or been convicted, the presence of elder abuse has been verified and the time of detection is known. This dataset includes rich information about the abuse victims and perpetrators as well as details about the abuse history, when and how it was detected, and the surrounding circumstances. It was constructed using information from the legal case files, including: medical records, descriptions of emergency medical services personnel and police interactions with the victim and perpetrator, victim statements, adult protective services files, court documents and photographs of injuries.
Medicare data linkage
We will link these legally adjudicated cases to Medicare claims data using identifying information including social security numbers and/or a combination of last name, date of birth and residential ZIP code. Fee-for-service Medicare data are the largest single repository of patient healthcare data for US older adults,66 offering comprehensive information on utilisation of a broad range of healthcare services for continuously enrolled individuals. Medicare claims data hve been used successfully to analyse healthcare utilisation and costs and to inform interventions and policies for a variety of chronic diseases.67–70 Additionally, claims data have been used to examine the impact on utilisation and cost of sociomedical issues71 72 including excessive alcohol use.47 57 73 Medicare claims data have also been employed to provide insight into the characteristics of frequent users of specific health services, such as the ED62 74 and hospital.75
We plan to examine Medicare claims data for each case from 3 years before to 3 years after detection of elder abuse and will compare with controls. We will use files including: the Master Beneficiary Summary File (enrollee demographics, monthly enrolment information, chronic conditions, annual summary of costs and service utilisation), Medicare Provider Analysis and Review file (events of inpatient hospital and skilled nursing facility stays), Outpatient Claims, Carrier File (claims of physician services), Home Health Claims and the Part D (prescription drug) Event File.76
Measures
We describe the key measures of utilisation we plan to use in table 1. We intend to focus primarily on utilisation of high-intensity, high-cost healthcare services including ED visits and hospitalisations by elder abuse victims and non-victim control subjects. We will examine overall utilisation of these services and will also look at several characteristics of this utilisation. We will examine the frequency of ED use and hospitalisation among victims and compare utilisation of these services of victims and non-victim controls. We will focus on injury-related utilisation, using ICD codes and external cause of injury codes77 78 similar to previous work in child abuse.56 79 We will also examine frequent ED use, defined as four or more visits in a year, the cut-off accepted in the literature and used in previous Medicare research.62 74 80 81 We plan to measure the number of potentially avoidable low-urgency ED visits82 83 as well as ED visits and hospitalisations for ACSCs. We will define low urgency visits similar to previous literature82 83 using Medicare Current Procedural Terminology billing codes (99281 and 99282) indicating low severity and no additional procedures billed. For this research, we will use the 11 ACSCs established for use in Medicare data.46 We will also examine repeat ED visits and rehospitalisations within short intervals. Consistent with previous research, we will examine visits to the ED within 3 days, 7 days and 30 days of initial visit50 52 as well as repeat hospitalisations within 30 days and 90 days of initial hospitalisation.51 Additionally, we will explore use of multiple EDs and hospitals.
Table 1.
Selected key measures of healthcare utilisation
| Site/type | Utilisation measure |
| Emergency department (ED) |
|
| Hospital |
|
| Outpatient |
|
For outpatient care, we will examine the number of primary care visits and focus on injury-related visits for victims and controls. We will also examine changes in primary care providers. We plan to evaluate the continuity of care using the widely employed Continuity of Care Index (COCI).63 Given that the COCI requires multiple outpatient visits to be meaningfully calculated, we will only examine this variable for subjects with three or more outpatient visits, consistent with previous literature.62 84 85 We will measure whether physical elder abuse victims and control subjects received preventative services, including influenza vaccination, glaucoma screening, pneumonia vaccination and mammogram.57 We plan to examine adherence to medication for chronic conditions. To do this, we will measure the proportion of days covered86 87 and determine adherent versus non-adherent using 0.80 as a cut-off, a common research strategy in administrative claims data.87 88
We will examine demographic data, including age, gender and race/ethnicity. We will also use claims data for key health-related covariates to allow for further characterisation of physical elder abuse victims and comparison of subgroups. These include medical comorbidities, psychiatric comorbidities, dementia and frailty. For medical comorbidities, we plan to use chronic condition indicators within the Medicare Master Beneficiary file, and we will use psychiatric diagnoses within claims data. We will use an established approach35 89 90 to identify dementia. To identify frailty, we will use a recently developed algorithm designed for use in Medicare claims data.91 92
Non-victim control subjects
We will select a group of non-victim control subjects matched to the cases on age, race, gender and residential zip code at the time of detection of each elder abuse case. This control group will allow us to compare healthcare utilisation of elder abuse victims with that of a general older adult population. We will construct a second control group who, in addition to being matched to the cases on age, race, gender and ZIP code, visited the ED for an unintentional injury within 1 week of the victim’s abuse detection by law enforcement. This second control group will allow us to explore potential differences between older adults presenting to the ED for abuse-related injuries and those presenting with unintentional injuries, a key focus of our previous research.93 94 Findings from such comparisons may assist healthcare providers, particularly in the ED, to differentiate between physical elder abuse and unintentional injuries, informing future development of clinical algorithms to assist in this identification. Because we may have more controls than needed meeting the selection criteria within the first control cohort outlined above, we will further conduct propensity score matching to select controls that more closely match with the cases.
We recognise that older adults selected as control subjects may actually be victims of physical elder abuse. To minimise the likelihood of this, we will ensure that all selected controls have never received any elder maltreatment-related diagnosis within Medicare claims data.
Focus on physical abuse
Though physical elder abuse may occur less frequently than other types of mistreatment, we think that focusing on these cases is a strength of our approach. Researchers have recognised that elder mistreatment is not a monolithic phenomenon and that aetiologies, victim and perpetrator characteristics, risk factors, clinical features and sequelae likely differ in important ways between mistreatment types.95 An important reason that previous research has yielded inconsistent findings and little clinically useful information is likely that heterogeneous cases were analysed together. We have chosen to focus on physical abuse because this violent mistreatment may be particularly dangerous for an older adult. Our research focuses on healthcare utilisation for abuse victims and the potential for improving early identification in healthcare settings such as the ED. Given that physical abuse often causes acute injury that may trigger healthcare visits more commonly than other types of elder mistreatment, healthcare providers may have a particular opportunity to identify it. Linking known elder abuse cases to Medicare claims data to describe rates and patterns of healthcare utilisation may also be used to examine victims of other types of elder mistreatment though, and we plan to explore this in the future.
Analysis
We will conduct descriptive longitudinal analysis of healthcare utilisation up to 3 years before and 3 years after the detection of elder abuse (and among control cohorts). For each elder abuse case, we will determine the calendar month in which the case was detected (the ‘index month’). We will then group months before and after the index month into 3 month intervals/quarters. Our unit of analysis will be patient-quarter. We will plot measured outcomes over time (centred around the index month) and visualise level of utilisation in time blocks in relationship to the index month.
We will compare utilisation between physical elder abuse cases and non-victim control subjects using the key measures described above, focusing on identifying important differences. Comparisons will also specifically focus on rates of radiographic utilisation of maxillofacial CT scan and forearm X-rays as well as diagnoses including acute or chronic facial or chronic ulnar fracture, and chronic rib fracture as they have been found to be potential predictors of physical elder abuse.96 We will compare total costs between cases and controls and then examine in detail contributing costs associated with each type of utilisation.
We will also conduct statistical modelling of longitudinal healthcare utilisation outcomes to estimate adjusted differences between physical elder abuse victims and non-victims at various time points before and after the index month. For example, for the dichotomous outcome of any ED or inpatient admission in a quarter, we will estimate a mixed logistic regression where major covariates include victim status, time (relative to index month) and interaction of victim status and time, controlling for individual demographics and comorbidities. Random effects will be specified at the patient level (to account for repeated measures of the same individual) and zip code (to account for clustering of patients within the same zip code) levels.
We have conducted power calculations with these cases and controls, incorporating assumptions about Medicare linking rate (50% of cases), number of quarters of data contributed by each individual (six quarters), percentage of subjects with ≥1 ED visit in a quarter (12% of elder abuse victims and 6% of controls) and intracluster correlation (0.2, to account for clustering of quarters within the same individual). Using these assumptions, we have a power of 0.82, which is adequate to identify important differences in utilisation between cases and controls.
Using machine learning
The comparative statistical analysis described above will illuminate the trajectories of healthcare use one type at a time. It lacks the ability to integrate multidimensional data that, combined, forms unique patterns of care. Recent innovations in machine learning make it possible to use vast amounts of data, such as service utilisation, diagnoses received and procedures performed, to identify sequences and mix of clinical events likely to lead to particular outcomes or suggestive of an underlying disease process for different cohorts of patients.97–102 For example, sequential pattern mining has been used in child abuse to examine patterns of services provided to victims.103 104 To supplement the proposed statistical analysis, we propose to search for features within claims data that may be suggestive that an older adult is a victim of abuse. We will use Sequential PAttern Discovery using Equivalence classes,105 a well-established algorithm that identifies patterns that are observed more than a user-defined frequency threshold in a cohorts’ sequences of event. In addition, we will use Markov modelling106 to identify the probabilities of observed patterns and associated underlying status of abuse to better distinguish patterns that are unique to elderly abused patients. We may find, for example, that a significant percentage of abuse victims have two ED visits and a hospitalisation within a 3-month period and receive forearm X-rays and are diagnosed with a fracture, but this pattern is never seen in controls.
Patient and public involvement
We plan to involve older adults including victims of elder mistreatment in the reporting and dissemination for this research.
Timeline
This research was initiated in 2018, and we plan to report results by 2023.
Discussion
This ongoing work will address a significant gap in current knowledge about elder abuse by improving understanding of how physical abuse victims use healthcare services differently than non-victims as well as associated costs. We anticipate insights from our findings will generate hypotheses that may be tested in future studies in different populations and among victims of different types of elder mistreatment. We also expect that this work will lead to additional uses of claims data to explore the health consequences of elder abuse and to identify utilisation patterns with ‘red flags’ suggestive of exposure. Ultimately, we anticipate that knowledge gleaned will support the future development of a health informatics tool to identify potential victims.
An important limitation of our approach is the use of legally adjudicated cases. Though using this source solves the important methodological challenge of ensuring that case subjects are actually victims of abuse, legally adjudicated cases represent a small percentage of all cases, and abuse victims included may differ in important ways from other victims. They may have experienced more acute or severe abuse allowing identification, and subtle cases of abuse that are more challenging to detect may not have been included. Additionally, other circumstances surrounding the case including the availability of evidence, the willingness of the victim to participate and jurisdiction’s practice pattern may have impacted the decision to prosecute the perpetrator, significantly reducing potential generalisability. An important challenge in previous studies has been accurately classifying subjects as victims of mistreatment. This has likely contributed to inconsistent research findings. Our new potential approach will generate trustworthy results that may identify patterns and generate hypotheses that may be tested. We anticipate that rigorous studies such as ours will lay the necessary groundwork for future studies focused on identifying and examining more subtle cases.
Also, our research strategy relies on linking to Medicare Fee-for-Service records. If subjects were covered by Medicare Advantage or otherwise not covered by Medicare Fee-For-Service for any period, information about their healthcare utilisation would not be available during that period. We have incorporated this potential into our power calculation assumptions, however, and believe we will be able to identify important differences in utilisation.
Another important limitation is that selected control subjects may actually be unidentified cases, reducing the accuracy of our conclusions. Using elder mistreatment diagnoses within Medicare data is not an ideal method for ensuring controls are not cases, given that these diagnoses are infrequently and unreliably included. We hope to overcome this limitation by selecting multiple control cohorts, each with large numbers of controls. Using this approach, and performing sensitivity analyses on our findings, will allow us to identify patterns and draw meaningful conclusions even if a small number of controls are actually abuse victims.
Although we believe that machine learning techniques have enormous potential to find subtle patterns, it is possible that we will not identify any that are clinically identifiable or meaningful. Despite these potential limitations, we believe this research offers a unique opportunity to use a large series of well-characterised cases of physical elder abuse to help us understand the health-related markers that can be used to more validly predict elder abuse and thereby prevent it.
Improved understanding of patterns and associated costs of healthcare utilisation among elder abuse victims, which likely differs substantially from that of other older adults, is potentially very valuable. It may improve the ability of healthcare providers to identify, intervene and prevent victimisation. Furthermore, it may inform policy changes to reduce costs and help this vulnerable population. The research described here represents an important step in exploring the potential of examining healthcare utilisation to provide insight into elder abuse and how to address it.
Ethics and dissemination
This project has been reviewed and approved by the Weill Cornell Medicine Institutional Review Board, protocol #1807019417, with initial approval on 1 August 2018. We aim to disseminate our results in peer-reviewed journals at national and international conferences and among interested patient groups and the public.
Supplementary Material
Acknowledgments
We deeply appreciate the continued partnership of our colleagues/partners at the King’s Count District Attorney’s Office in Brooklyn, New York, and the King County Prosecuting Attorney’s Office in Seattle, Washington, without whom this work would not be possible.
Footnotes
Contributors: TR, YB, YZ, SC, AE, KP and ML conceived of the study. All authors contributed to the design of the study protocol. TR wrote the manuscript first draft. YB, YZ, SC, KW, AE, PJ, EB, DL, RK, JC, RB, TF, KP and ML contributed to and approved the final manuscript.
Funding: This work was supported by a grant from the National Institute on Aging (R01 AG060086). TR’s participation has also been supported by a Paul B. Beeson Emerging Leaders Career Development Award in Aging (K76 AG054866) from the National Institute on Aging. The funder has not been involved in the design or conduct of the research.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
References
- 1.Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National elder mistreatment study. Am J Public Health 2010;100:292–7. 10.2105/AJPH.2009.163089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lachs MS, Pillemer K. Elder abuse. Lancet 2004;364:1263–72. 10.1016/S0140-6736(04)17144-4 [DOI] [PubMed] [Google Scholar]
- 3.New York City Department for the Aging . Under the radar: new York state elder abuse prevalence study: self-reported prevalence and documented case surveys, 2012. Available: https://ocfs.ny.gov/main/reports/Under%20the%20Radar%2005%2012%2011%20final%20report.pdf [Accessed 10 Feb 2020].
- 4.National Research Council . Elder mistreatment: abuse, neglect and exploitation in an aging America. Washington, DC: The National Academies Press, 2003. [PubMed] [Google Scholar]
- 5.National Center for Elder Abuse . The elder justice roadmap: a Stakeholder initiative to respond to an emerging health, justice, financial, and social crisis. Available: https://www.justice.gov/file/852856/download [Accessed 10 Feb 2020].
- 6.Lachs MS, Pillemer KA. Elder abuse. N Engl J Med 2015;373:1947–56. 10.1056/NEJMra1404688 [DOI] [PubMed] [Google Scholar]
- 7.Schofield MJ, Powers JR, Loxton D. Mortality and disability outcomes of self-reported elder abuse: a 12-year prospective investigation. J Am Geriatr Soc 2013;61:679–85. 10.1111/jgs.12212 [DOI] [PubMed] [Google Scholar]
- 8.Dyer CB, Pavlik VN, Murphy KP, et al. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc 2000;48:205–8. 10.1111/j.1532-5415.2000.tb03913.x [DOI] [PubMed] [Google Scholar]
- 9.Lachs MS, Williams CS, O'Brien S, et al. The mortality of elder mistreatment. JAMA 1998;280:428–32. 10.1001/jama.280.5.428 [DOI] [PubMed] [Google Scholar]
- 10.Dong XQ, Simon MA, Beck TT, et al. Elder abuse and mortality: the role of psychological and social wellbeing. Gerontology 2011;57:549–58. 10.1159/000321881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker MW, LaCroix AZ, Wu C, et al. Mortality risk associated with physical and verbal abuse in women aged 50 to 79. J Am Geriatr Soc 2009;57:1799–809. 10.1111/j.1532-5415.2009.02429.x [DOI] [PubMed] [Google Scholar]
- 12.Pillemer K, Finkelhor D. The prevalence of elder abuse: a random sample survey. Gerontologist 1988;28:51–7. 10.1093/geront/28.1.51 [DOI] [PubMed] [Google Scholar]
- 13.Murphy K, Waa S, Jaffer H, et al. A literature review of findings in physical elder abuse. Can Assoc Radiol J 2013;64:10–14. 10.1016/j.carj.2012.12.001 [DOI] [PubMed] [Google Scholar]
- 14.Lachs MS, Williams CS, O'Brien S, et al. Ed use by older victims of family violence. Ann Emerg Med 1997;30:448–54. 10.1016/S0196-0644(97)70003-9 [DOI] [PubMed] [Google Scholar]
- 15.Bond MC, Butler KH. Elder abuse and neglect: definitions, epidemiology, and approaches to emergency department screening. Clin Geriatr Med 2013;29:257–73. 10.1016/j.cger.2012.09.004 [DOI] [PubMed] [Google Scholar]
- 16.Geroff AJ, Olshaker JS. Elder abuse. Emerg Med Clin North Am 2006;24:491–505. 10.1016/j.emc.2006.01.009 [DOI] [PubMed] [Google Scholar]
- 17.Dong X, Simon MA. Association between elder abuse and use of ED: findings from the Chicago health and aging project. Am J Emerg Med 2013;31:693–8. 10.1016/j.ajem.2012.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedman LS, Avila S, Tanouye K, et al. A case-control study of severe physical abuse of older adults. J Am Geriatr Soc 2011;59:417–22. 10.1111/j.1532-5415.2010.03313.x [DOI] [PubMed] [Google Scholar]
- 19.Heyborne RD. Elder abuse: keeping the unthinkable in the differential. Acad Emerg Med 2007;14:566–7. 10.1197/j.aem.2007.01.015 [DOI] [PubMed] [Google Scholar]
- 20.Chan KL, Choi WMA, Fong DYT, et al. Characteristics of family violence victims presenting to emergency departments in Hong Kong. J Emerg Med 2013;44:249–58. 10.1016/j.jemermed.2012.01.061 [DOI] [PubMed] [Google Scholar]
- 21.Dong X, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med 2013;173:911–7. 10.1001/jamainternmed.2013.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lachs MS, Williams CS, O'Brien S, et al. Adult protective service use and nursing home placement. Gerontologist 2002;42:734–9. 10.1093/geront/42.6.734 [DOI] [PubMed] [Google Scholar]
- 23.Dong X, Simon MA. Association between reported elder abuse and rates of admission to skilled nursing facilities: findings from a longitudinal population-based cohort study. Gerontology 2013;59:464–72. 10.1159/000351338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mouton CP, Rodabough RJ, Rovi SLD, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. Am J Public Health 2004;94:605–12. 10.2105/AJPH.94.4.605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jackson AM, Deye KP, Halley T, et al. Curiosity and critical thinking: identifying child abuse before it is too late. Clin Pediatr 2015;54:54–61. 10.1177/0009922814549314 [DOI] [PubMed] [Google Scholar]
- 26.Jenny C, Hymel KP, Ritzen A, et al. Analysis of missed cases of abusive head trauma. JAMA 1999;281:621–6. 10.1001/jama.281.7.621 [DOI] [PubMed] [Google Scholar]
- 27.King WK, Kiesel EL, Simon HK. Child abuse fatalities: are we missing opportunities for intervention? Pediatr Emerg Care 2006;22:211–4. 10.1097/01.pec.0000208180.94166.dd [DOI] [PubMed] [Google Scholar]
- 28.Letson MM, Cooper JN, Deans KJ, et al. Prior opportunities to identify abuse in children with abusive head trauma. Child Abuse Negl 2016;60:36–45. 10.1016/j.chiabu.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 29.Ravichandiran N, Schuh S, Bejuk M, et al. Delayed identification of pediatric abuse-related fractures. Pediatrics 2010;125:60–6. 10.1542/peds.2008-3794 [DOI] [PubMed] [Google Scholar]
- 30.Thorpe EL, Zuckerbraun NS, Wolford JE, et al. Missed opportunities to diagnose child physical abuse. Pediatr Emerg Care 2014;30:771–6. 10.1097/PEC.0000000000000257 [DOI] [PubMed] [Google Scholar]
- 31.Kothari CL, Rhodes KV. Missed opportunities: emergency department visits by police-identified victims of intimate partner violence. Ann Emerg Med 2006;47:190–9. 10.1016/j.annemergmed.2005.10.016 [DOI] [PubMed] [Google Scholar]
- 32.Willson P, Cesario S, Fredland N, et al. Primary healthcare provider's lost opportunity to help abused women. J Am Acad Nurse Pract 2001;13:565–70. 10.1111/j.1745-7599.2001.tb00327.x [DOI] [PubMed] [Google Scholar]
- 33.Lindberg DM, Beaty B, Juarez-Colunga E, et al. Testing for abuse in children with sentinel injuries. Pediatrics 2015;136:831–8. 10.1542/peds.2015-1487 [DOI] [PubMed] [Google Scholar]
- 34.Sheets LK, Leach ME, Koszewski IJ, et al. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics 2013;131:701–7. 10.1542/peds.2012-2780 [DOI] [PubMed] [Google Scholar]
- 35.Brown DS, Fang X, Florence CS. Medical costs attributable to child maltreatment a systematic review of short- and long-term effects. Am J Prev Med 2011;41:627–35. 10.1016/j.amepre.2011.08.013 [DOI] [PubMed] [Google Scholar]
- 36.Rovi S, Chen P-H, Johnson MS. The economic burden of hospitalizations associated with child abuse and neglect. Am J Public Health 2004;94:586–90. 10.2105/AJPH.94.4.586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Florence C, Brown DS, Fang X, et al. Health care costs associated with child maltreatment: impact on Medicaid. Pediatrics 2013;132:312–8. 10.1542/peds.2012-2212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones AS, Dienemann J, Schollenberger J, et al. Long-Term costs of intimate partner violence in a sample of female HMO enrollees. Womens Health Issues 2006;16:252–61. 10.1016/j.whi.2006.06.007 [DOI] [PubMed] [Google Scholar]
- 39.Peterson C, Xu L, Florence C, et al. The medical cost of abusive head trauma in the United States. Pediatrics 2014;134:91–9. 10.1542/peds.2014-0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller TR, Steinbeigle R, Lawrence BA. Lifetime cost of abusive head trauma at ages 0-4, USA. Prev Sci 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fang X, Brown DS, Florence CS, et al. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl 2012;36:156–65. 10.1016/j.chiabu.2011.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Max W, Rice DP, Finkelstein E, et al. The economic toll of intimate partner violence against women in the United States. Violence Vict 2004;19:259–72. 10.1891/vivi.19.3.259.65767 [DOI] [PubMed] [Google Scholar]
- 43.Thielen FW, Ten Have M, de Graaf R, et al. Long-Term economic consequences of child maltreatment: a population-based study. Eur Child Adolesc Psychiatry 2016;25:1297–305. 10.1007/s00787-016-0850-5 [DOI] [PubMed] [Google Scholar]
- 44.Yang J, Miller TR, Zhang N, et al. Incidence and cost of sexual violence in Iowa. Am J Prev Med 2014;47:198–202. 10.1016/j.amepre.2014.04.005 [DOI] [PubMed] [Google Scholar]
- 45.Teresi JA, Burnes D, Skowron EA, et al. State of the science on prevention of elder abuse and lessons learned from child abuse and domestic violence prevention: toward a conceptual framework for research. J Elder Abuse Negl 2016;28:263–300. 10.1080/08946566.2016.1240053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCall N. Centers for Medicare and Medicaid services. investigation of increasing rates of hospitalization for ambulatory care sensitive conditions among Medicare fee-for-service beneficiaries. Available: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/Downloads/McCall_2004_3.pdf [Accessed 10 Feb 2020].
- 47.Merrick ESL, Hodgkin D, Garnick DW, et al. Older adults' inpatient and emergency department utilization for ambulatory-care-sensitive conditions: relationship with alcohol consumption. J Aging Health 2011;23:86–111. 10.1177/0898264310383156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brownell J, Wang J, Smith A, et al. Trends in emergency department visits for ambulatory care sensitive conditions by elderly nursing home residents, 2001 to 2010. JAMA Intern Med 2014;174:156–8. 10.1001/jamainternmed.2013.11821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carter MW, Datti B, Winters JM. Ed visits by older adults for ambulatory care-sensitive and supply-sensitive conditions. Am J Emerg Med 2006;24:428–34. 10.1016/j.ajem.2005.12.012 [DOI] [PubMed] [Google Scholar]
- 50.Duseja R, Bardach NS, Lin GA, et al. Revisit rates and associated costs after an emergency department encounter: a multistate analysis. Ann Intern Med 2015;162:750–6. 10.7326/M14-1616 [DOI] [PubMed] [Google Scholar]
- 51.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–28. 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- 52.Liu SW, Obermeyer Z, Chang Y, et al. Frequency of ED revisits and death among older adults after a fall. Am J Emerg Med 2015;33:1012–8. 10.1016/j.ajem.2015.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA 2013;309:364–71. 10.1001/jama.2012.216219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahmad M, Lachs MS. Elder abuse and neglect: what physicians can and should do. Cleve Clin J Med 2002;69:801–8. 10.3949/ccjm.69.10.801 [DOI] [PubMed] [Google Scholar]
- 55.Rosen T, Stern ME, Elman A, et al. Identifying and initiating intervention for elder abuse and neglect in the emergency department. Clin Geriatr Med 2018;34:435–51. 10.1016/j.cger.2018.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Friedlaender EY, Rubin DM, Alpern ER, et al. Patterns of health care use that may identify young children who are at risk for maltreatment. Pediatrics 2005;116:1303–8. 10.1542/peds.2004-1988 [DOI] [PubMed] [Google Scholar]
- 57.Merrick EL, Hodgkin D, Garnick DW, et al. Unhealthy drinking patterns and receipt of preventive medical services by older adults. J Gen Intern Med 2008;23:1741–8. 10.1007/s11606-008-0753-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Asch SM, Sloss EM, Hogan C, et al. Measuring underuse of necessary care among elderly Medicare beneficiaries using inpatient and outpatient claims. JAMA 2000;284:2325–33. 10.1001/jama.284.18.2325 [DOI] [PubMed] [Google Scholar]
- 59.Klabunde CN, Meissner HI, Wooten KG, et al. Comparing colorectal cancer screening and immunization status in older Americans. Am J Prev Med 2007;33:1–8. 10.1016/j.amepre.2007.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ozminkowski RJ, Goetzel RZ, Shechter D, et al. Predictors of preventive service use among Medicare beneficiaries. Health Care Financ Rev 2006;27:5–23. [PMC free article] [PubMed] [Google Scholar]
- 61.Scott TL, Gazmararian JA, Williams MV, et al. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care 2002;40:395–404. 10.1097/00005650-200205000-00005 [DOI] [PubMed] [Google Scholar]
- 62.Colligan EM, Pines JM, Colantuoni E, et al. Factors associated with frequent emergency department use in the Medicare population. Med Care Res Rev 2017;74:311–27. 10.1177/1077558716641826 [DOI] [PubMed] [Google Scholar]
- 63.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care 1977;15:347–9. 10.1097/00005650-197704000-00010 [DOI] [PubMed] [Google Scholar]
- 64.Jha AK, Aubert RE, Yao J, et al. Greater adherence to diabetes drugs is linked to less hospital use and could save nearly $5 billion annually. Health Aff 2012;31:1836–46. 10.1377/hlthaff.2011.1198 [DOI] [PubMed] [Google Scholar]
- 65.Roebuck MC, Liberman JN, Gemmill-Toyama M, et al. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff 2011;30:91–9. 10.1377/hlthaff.2009.1087 [DOI] [PubMed] [Google Scholar]
- 66.Mues KE, Liede A, Liu J, et al. Use of the Medicare database in epidemiologic and health services research: a valuable source of real-world evidence on the older and disabled populations in the US. Clin Epidemiol 2017;9:267–77. 10.2147/CLEP.S105613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen J, Hsieh AF-C, Dharmarajan K, et al. National trends in heart failure hospitalization after acute myocardial infarction for Medicare beneficiaries: 1998-2010. Circulation 2013;128:2577–84. 10.1161/CIRCULATIONAHA.113.003668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fitch K, Pelizzari PM, Pyenson B. Inpatient utilization and costs for Medicare fee-for-service beneficiaries with heart failure. Am Health Drug Benefits 2016;9:96–104. [PMC free article] [PubMed] [Google Scholar]
- 69.Genao L, Durheim MT, Mi X, et al. Early and long-term outcomes of older adults after acute care encounters for chronic obstructive pulmonary disease exacerbation. Ann Am Thorac Soc 2015;12:1805–12. 10.1513/AnnalsATS.201504-250OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wetmore JB, Peng Y, Jackson S, et al. Patient characteristics, disease burden, and medication use in stage 4 - 5 chronic kidney disease patients. Clin Nephrol 2016;85:101–11. 10.5414/CN108626 [DOI] [PubMed] [Google Scholar]
- 71.Baicker K, Chandra A, Skinner JS, et al. Who you are and where you live: how race and geography affect the treatment of Medicare beneficiaries. Health Aff 2004;Variation:VAR-33–VAR-44. 10.1377/hlthaff.var.33 [DOI] [PubMed] [Google Scholar]
- 72.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 2011;305:675–81. 10.1001/jama.2011.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Merrick EL, Horgan CM, Hodgkin D, et al. Unhealthy drinking patterns in older adults: prevalence and associated characteristics. J Am Geriatr Soc 2008;56:214–23. 10.1111/j.1532-5415.2007.01539.x [DOI] [PubMed] [Google Scholar]
- 74.Colligan EM, Pines JM, Colantuoni E, et al. Risk factors for persistent frequent emergency department use in Medicare beneficiaries. Ann Emerg Med 2016;67:721–9. 10.1016/j.annemergmed.2016.01.033 [DOI] [PubMed] [Google Scholar]
- 75.Phongtankuel V, Johnson P, Reid MC. Risk factors for hospitalization of home hospice enrollees. Am J Hosp Palliat Care 2016:1049909116659439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.ResDAC Research Data Assistance Center . Data availability. Available: https://www.resdac.org/cms-data/file-availability [Accessed 10 Feb 2020].
- 77.Annest JL, Fingerhut LA, Gallagher SS, et al. Strategies to improve external cause-of-injury coding in state-based hospital discharge and emergency department data systems: recommendations of the CDC Workgroup for improvement of external Cause-of-Injury coding. MMWR Recomm Rep 2008;57:1–15. [PubMed] [Google Scholar]
- 78.Coben JH, Steiner CA, Barrett M, et al. Completeness of cause of injury coding in healthcare administrative databases in the United States, 2001. Inj Prev 2006;12:199–201. 10.1136/ip.2005.010512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Spivey MI, Schnitzer PG, Kruse RL, et al. Association of injury visits in children and child maltreatment reports. J Emerg Med 2009;36:207–14. 10.1016/j.jemermed.2007.07.025 [DOI] [PubMed] [Google Scholar]
- 80.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med 2010;56:42–8. 10.1016/j.annemergmed.2010.01.032 [DOI] [PubMed] [Google Scholar]
- 81.Locker TE, Baston S, Mason SM, et al. Defining frequent use of an urban emergency department. Emerg Med J 2007;24:398–401. 10.1136/emj.2006.043844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Davis JW, Fujimoto RY, Chan H, et al. Identifying characteristics of patients with low urgency emergency department visits in a managed care setting. Manag Care 2010;19:38–44. [PubMed] [Google Scholar]
- 83.Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 84.Bayliss EA, Ellis JL, Shoup JA, et al. Effect of continuity of care on hospital utilization for seniors with multiple medical conditions in an integrated health care system. Ann Fam Med 2015;13:123–9. 10.1370/afm.1739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liss DT, Chubak J, Anderson ML, et al. Patient-Reported care coordination: associations with primary care continuity and specialty care use. Ann Fam Med 2011;9:323–9. 10.1370/afm.1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hess LM, Raebel MA, Conner DA, et al. Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother 2006;40:1280–8. 10.1345/aph.1H018 [DOI] [PubMed] [Google Scholar]
- 87.Karve S, Cleves MA, Helm M, et al. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin 2009;25:2303–10. 10.1185/03007990903126833 [DOI] [PubMed] [Google Scholar]
- 88.Colantonio LD, Huang L, Monda KL, et al. Adherence to high-intensity statins following a myocardial infarction hospitalization among Medicare beneficiaries. JAMA Cardiol 2017;2:890–5. 10.1001/jamacardio.2017.0911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ostbye T, Taylor DH, Clipp EC, et al. Identification of dementia: agreement among national survey data, Medicare claims, and death certificates. Health Serv Res 2008;43:313–26. 10.1111/j.1475-6773.2007.00748.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Taylor DH, Fillenbaum GG, Ezell ME. The accuracy of Medicare claims data in identifying Alzheimer's disease. J Clin Epidemiol 2002;55:929–37. 10.1016/S0895-4356(02)00452-3 [DOI] [PubMed] [Google Scholar]
- 91.Faurot KR, Jonsson Funk M, Pate V, et al. Using claims data to predict dependency in activities of daily living as a proxy for frailty. Pharmacoepidemiol Drug Saf 2015;24:59–66. 10.1002/pds.3719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang HT, McGrath LJ, Wyss R, et al. Controlling confounding by frailty when estimating influenza vaccine effectiveness using predictors of dependency in activities of daily living. Pharmacoepidemiol Drug Saf 2017;26:1500–6. 10.1002/pds.4298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rosen T, Bloemen EM, LoFaso VM, et al. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. J Emerg Med 2016;50:518–26. 10.1016/j.jemermed.2015.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rosen T, LoFaso V, Bloemen EM. Injury patterns in physical elder abuse: preliminary findings from a pilot sample of highly adjudicated cases. San Diego: Society of Academic Emergency Medicine Annual Scientific Meeting, 2015. [Google Scholar]
- 95.Jackson S. Understanding elder abuse: new directions for developing theories of elder abuse occurring in domestic settings, 2013. Available: https://www.ncjrs.gov/pdffiles1/nij/241731.pdf [Accessed 10 Feb 2020].
- 96.Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J 2017;68:16–20. 10.1016/j.carj.2016.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang Y, Padman R. Paving the COWPath: learning and visualizing clinical pathways from electronic health record data. Carnegie Mellon University, 2015. [DOI] [PubMed] [Google Scholar]
- 98.Movahedi F, Carey L, Zhang Y. Care pathway after left ventricular assist devices (LVAD) implementation. San Diego, CA: International Society for Heart and Lung Transplantation, 2017. [Google Scholar]
- 99.Ghosh S, Li J, Cao L, et al. Septic shock prediction for ICU patients via coupled HMM walking on sequential contrast patterns. J Biomed Inform 2017;66:19–31. 10.1016/j.jbi.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 100.Kawamoto R, Nazir A, Kameyama A, et al. Hidden Markov model for analyzing time-series health checkup data. Stud Health Technol Inform 2013;192:491–5. [PubMed] [Google Scholar]
- 101.Watkins RE, Eagleson S, Veenendaal B, et al. Disease surveillance using a hidden Markov model. BMC Med Inform Decis Mak 2009;9:39. 10.1186/1472-6947-9-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang Y, Padman R. Innovations in chronic care delivery using data-driven clinical pathways. Am J Manag Care 2015;21:e661–8. [PubMed] [Google Scholar]
- 103.Duncan DF, Kum H-C, Weigensberg EC. Informing child welfare policy and practice: using knowledge discovery and data mining technology via a dynamic web site. Child Maltreat 2008;13:383–91. 10.1177/1077559508318951 [DOI] [PubMed] [Google Scholar]
- 104.Chung H, Wang W, Duncan D. ApproxMAP: approximate mining of consensus sequential patterns. Available: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.12.2633&rep=rep1&type=pdf [Accessed 10 Feb 2020].
- 105.Zaki MJ. Spade: an efficient algorithm for mining frequent sequences. Mach Learn 2001;42:31–60. 10.1023/A:1007652502315 [DOI] [Google Scholar]
- 106.Rabiner L. A tutorial on hidden Markov models and selected applications in speech recognition. IEEE, 1989. Available: http://www.ece.ucsb.edu/Faculty/Rabiner/ece259/Reprints/tutorial%20on%20hmm%20and%20applications.pdf [Accessed 10 Feb 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.